Abstract
Background
Intramural metastasis distant from the primary tumor is rare in colorectal cancer. Here, we present a notably rare and probably the first case of asynchronous intramural recurrence in the rectum after curative surgery for proximal sigmoid colon cancer.
Case presentation
A 44-year-old man underwent curative sigmoidectomy for proximal sigmoid colon cancer with T3N0M0, Stage IIA tubular adenocarcinomas. After 15 months, the tumor marker level had increased, and positron emission tomography-computed tomography (PET-CT) revealed abnormal fluorodeoxyglucose uptake in the rectum; colonoscopy revealed a submucosal tumor (SMT)-like lesion in the upper rectum, and biopsy revealed a tubular adenocarcinoma. We performed curative low anterior resection with tumor-specific mesorectal excision (TSME). The SMT-like tumor was located approximately 20 cm from the initial sigmoid colon anastomosis (i.e., at least 20 cm distal to the initial sigmoid colon cancer). The pathological findings revealed cancer cells with the same features as the initial sigmoid colon cancer, only in the intestinal wall but not in the mucosa and extramural tissue. Therefore, the lesion was determined to be an intramural recurrence.
After 24 months, lung recurrence, and local recurrence, which might have involved the lymph nodes in the preserved mesorectum after TSME at the bottom of the pelvis was detected on PET-CT. Hence, we started systemic chemotherapy.
Conclusions
This case report suggests that PET-CT and short-interval repeat colonoscopy may help detect a rare intramural recurrence. A long distal margin may be necessary to achieve local control in the rectal resection for intramural recurrence.
Similar content being viewed by others
Background
Intramural metastasis distant from the primary tumor is rare in colorectal cancer. Here, we present a notably rare case of asynchronous intramural recurrence in the rectum after curative surgery for proximal sigmoid colon cancer. To the best of our knowledge, this paper is the first case report of this type of recurrence.
Case presentation
A 44-year-old man with no specific medical or family history underwent curative sigmoidectomy for proximal sigmoid colon cancer with tubular adenocarcinoma. We performed standard regional lymph node dissection with high ligation of the inferior mesenteric artery and functional end-to-end anastomosis. The pathological diagnosis was T3N0M0, Stage IIA, according to the 8th Union for International Cancer Control classification. Moderate venous invasion was observed; however, lymphatic invasion was unnoted. Sufficient proximal and distal margins from the tumor were maintained (Fig. 1). Carcinoembryonic antigen (CEA) levels became normal after the surgery (from 11.0 to 3.3 ng/mL). No adjuvant chemotherapy was administered.
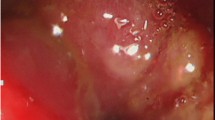
After 12 months, the CEA level increased to 9.0 ng/mL, although no recurrence was detected on computed tomography (CT) and colonoscopy. After another 3 months, the CEA level further increased to 17.2 ng/mL. We performed positron emission tomography-CT (PET-CT), and abnormal fluorodeoxyglucose uptake was detected in the rectum. Repeat colonoscopy revealed a submucosal tumor (SMT)-like lesion in the upper rectum (10–15 cm from the anal verge), and biopsy revealed tubular adenocarcinoma (Fig. 2). Lymph node and distant metastases were not identified on CT and PET-CT. We performed curative low anterior resection (LAR) with double-stapled anastomosis under the differential diagnosis of an atypical primary cancer or a rare case of intramural recurrence. We chose tumor-specific mesorectal excision (TSME) with a distal margin of 3 cm from the tumor. The postoperative course was uneventful. The SMT-like tumor was located approximately 20 cm from the initial sigmoid colon anastomosis in the specimen (i.e., at least 20 cm distal from the initial sigmoid colon cancer) (Fig. 3). Pathological findings revealed cancer cells with the same features as the initial sigmoid colon cancer, only in the intestinal wall but not in the mucosa and extramural tissue (Fig. 4). These findings were unlikely of primary cancer or lymph node recurrence, and likely of an intramural recurrence. Therefore, we determined that the lesion was an intramural recurrence from the initial sigmoid colon cancer. Severe venous invasion was also observed; however, lymphatic invasion was not observed. All resection margins were negative, and the CEA level became normal again (4.3 ng/mL). The RAS and BRAF statuses were both wild-type.
We planned adjuvant chemotherapy with eight courses of capecitabine plus oxaliplatin (CapeOX). However, after three courses, the CEA levels increased again, and a single lung recurrence was detected; this lung lesion was resected and CapeOX therapy was not used. Twelve months after pneumonectomy, another lung recurrence and a local recurrence, which may have been related to recurrence in the lymph node in the preserved mesorectum after TSME at the bottom of the pelvis, were detected on CT and PET-CT (Fig. 5). We initiated FOLFIRI (5-fluorouracil, l-leucovorin, and irinotecan) plus panitumumab for unresectable recurrent colorectal cancer. Stable disease was maintained after 14 courses (51 months from the initial sigmoidectomy and 36 months from the secondary LAR).
Discussion and conclusions
In esophageal cancer, intramural metastasis is a well-known metastatic lesion in the gastrointestinal wall and is clearly distant from the primary tumor [1]. A similar etiology in colorectal cancer is known as distal intramural spread (DIS), which is sometimes an unexpected cancer in the distal intestinal wall under the normal mucosa; DIS comprises both continuous spread from the primary tumor and skip lesions [2,3,4]. DIS itself is not rare and is observed in approximately 25% of resected rectal cancer specimens, but the maximum DIS distance from the primary tumor is within 2 cm in almost all cases [2, 5]. Only a few case reports of distant DIS (approximately 6 cm) have been published [3, 4]. Furthermore, DIS is usually related to rectal cancer, not colon cancer, and there is only one case report regarding intramural cancer spread in colon cancer [6]. This report presented a rare case of asynchronous intramural recurrence in the rectum following curative surgery for proximal sigmoid colon cancer. Recurrence occurred from a very distant DIS, at least 20 cm from the primary tumor.
This type of recurrence due to distant DIS occurs from vessel (lymphatic and venous) invasion, although cancer cell implantation from an inadequate surgical procedure may result in intramural recurrence near the primary surgical site [2, 3, 7]. Moderate to severe venous invasion was observed in both the primary and recurrent tumors in our case. The venous pathway for long DIS is consistent with a high rate of hematogenous recurrence in the liver and lung after curative surgery for distant DIS cases in previous reports and lung recurrence in our case [3, 5].
The diagnostic flow of intramural recurrence in our case is important. The initial colonoscopy did not reveal any abnormal findings, but a repeat colonoscopy after only 3 months showed recurrence. Intramural cancer lesions, which usually grow as SMT-like lesions, are difficult to identify on colonoscopy as long as they result in mucosal changes. In fact, there are only a few case reports of the intramural spread of colorectal cancer that could be diagnosed via colonoscopy [7, 8]. Furthermore, significant changes in intramural lesions at short intervals, such as in our case, were also observed in a previous report, which reported the appearance of intramural lesions only 5 weeks after negative findings on initial colonoscopy [3]. To detect intramural recurrence without delay, other modalities such as PET-CT and short-interval repeat colonoscopy may be considered if there are compatible reasons (e.g., the inexplicable elevation of tumor markers such as in our case).
The appropriateness of our surgical procedure for intramural recurrence in the rectum, LAR with TSME, is another concern. Although a favorable sphincter-preserving surgery without postoperative complications was achieved, undesirable local recurrence, which might have involved the lymph nodes in the preserved mesorectum after TSME, was observed. In fact, distal cancer spread is observed not only intramurally (i.e., DIS), but also extramurally (i.e., mesorectum); thus, adequate resection of the distal mesorectum is key to avoiding local recurrence in rectal cancer surgery [9, 10]. Total mesorectal excision (TME), which involves the resection of the entire mesorectum and may sometimes contain unexpected cancer spread, is the conventional gold-standard procedure for rectal cancer [11, 12]. However, a high anastomotic leakage rate and unnecessary sphincter loss are serious concerns in TME; therefore, TSME with a 2–3-cm distal margin from the tumor is widely accepted, especially in upper rectal cancer [13]. Several studies have reported that distal cancer spread (both intramural and extramural) was within 2–3 cm from the primary tumor in almost all cases, indicating the appropriateness of TSME [9, 10, 14]. However, such a consensus is currently for normal primary cancer, and intramural recurrence, such as in our case, is expected to have a longer distal cancer spread than in usual cases. Although it is difficult to make a definitive diagnosis of intramural recurrence before surgery, TME may be the preferred procedure to achieve local control if intramural recurrence is noted from preoperative findings, even if abdominoperineal resection with permanent colostomy is required.
In conclusion, we present a rare case of asynchronous intramural recurrence in the rectum after curative surgery for proximal sigmoid colon cancer. We suggest the following two take-home messages from this report. First, PET-CT and short-interval repeat colonoscopy may be useful to detect intramural recurrence. Second, a longer distal margin than usual may be necessary to achieve local control in the rectal resection for intramural recurrence.
Availability of data and materials
Not applicable.
Abbreviations
- CEA:
-
Carcinoembryonic antigen
- CT:
-
Computed tomography
- PET-CT:
-
Positron emission tomography-computed tomography
- SMT:
-
Submucosal tumor
- LAR:
-
Low anterior resection
- TSME:
-
Tumor-specific mesorectal excision
- DIS:
-
Distal intramural spread
- TME:
-
Total mesorectal excision
References
Okamura A, Watanabe M, Kozuki R, Toihata T, Takahashi K, Imamura Y, et al. Significance of intramural metastasis in patients with esophageal squamous cell carcinoma: an indicator of aggressive cancer behavior. World J Surg. 2019;43:1997–2005.
Nakagoe T, Yamaguchi E, Tanaka K, Sawai T, Tsuji T, Shibasaki S, et al. Distal intramural spread is an independent prognostic factor for distant metastasis and poor outcome in patients with rectal cancer: a multivariate analysis. Ann Surg Oncol. 2003;10:163–70.
Sato H, Shiota M, Okabe A, Tsukamoto T, Honda K, Morise Z, et al. Rectal cancer with extensive distal intramural spread treated by abdominoperineal resection. Int Cancer Conf J. 2020;9:9–13.
Munakata S, Murai Y, Koizumi A, Kato H, Yamamoto R, Ueda S, et al. Abdominoperineal resection for unexpected distal intramural spreading of rectal cancer. Case Rep Gastroenterol. 2018;12:297–302.
Williams NS, Dixon MF, Johnston D. Reappraisal of the 5 centimetre rule of distal excision for carcinoma of the rectum: a study of distal intramural spread and of patients’ survival. Br J Surg. 1983;70:150–4.
Abe T, Sakai H, Hayashi M, Nakamura S, Takesue S, Sada M, et al. Intramural metastasis to the appendix from ascending colon cancer: a case report. Surg Case Rep. 2020;6:69.
Tsumura A, Yokoyama S, Takifuji K, Hotta T, Matsuda K, Watanabe T, et al. Endoscopically observable white nodule caused by distal intramural lymphatic spread of rectal cancer: a case report. World J Surg Oncol. 2012;10:216.
Toda K, Kawada K, Hasegawa S, Yamada M, Kawamura J, Sakai Y. Intramural metastasis of T1 rectal cancer: report of a case report. World J Surg Oncol. 2015;13:337.
Shimada Y, Takii Y, Maruyama S, Ohta T. Intramural and mesorectal distal spread detected by whole-mount sections in the determination of optimal distal resection margin in patients undergoing surgery for rectosigmoid or rectal cancer without preoperative therapy. Dis Colon Rectum. 2011;54:1510–20.
Shirouzu K, Isomoto H, Kakegawa T. Distal spread of rectal cancer and optimal distal margin of resection for sphincter-preserving surgery. Cancer. 1995;76:388–92.
Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery--the clue to pelvic recurrence? Br J Surg. 1982;69:613–6.
Enker WE, Thaler HT, Cranor ML, Polyak T. Total mesorectal excision in the operative treatment of carcinoma of the rectum. J Am Coll Surg. 1995;181:335–46.
Lowry AC, Simmang CL, Boulos P, Farmer KC, Finan PJ, Hyman N, et al. Consensus statement of definitions for anorectal physiology and rectal cancer. ANZ J Surg. 2001;71:603–5.
Scott N, Jackson P, al-Jaberi T, Dixon MF, Quirke P, Finan PJ. Total mesorectal excision and local recurrence: a study of tumour spread in the mesorectum distal to rectal cancer. Br J Surg. 1995;82:1031–3.
Acknowledgements
The authors would like to thank Editage (www.editage.com) for the English language editing.
Funding
This report did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
YA participated in all aspects of this report: management of the patient, conceptualization of the report, and writing of the draft. KC reported the pathological findings. KY and JT managed the patient. NK and SI managed the patient and supervised the study. All authors have read and approved the final manuscript and agree to be held accountable for all aspects of the report.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal upon request.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Asada, Y., Chinen, K., Yamataka, K. et al. Intramural cancer recurrence in the rectum after curative surgery for proximal sigmoid colon cancer: a case report. World J Surg Onc 20, 332 (2022). https://doi.org/10.1186/s12957-022-02794-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02794-w