Abstract
Background
The prognosis of patients under existing neoadjuvant chemotherapy or neoadjuvant chemoradiotherapy requires improvement. Whereas programmed cell death 1 (PD-1) inhibitors have shown promising response in advanced esophageal cancer, they have not been used in the perioperative treatment of resectable locally advanced esophageal cancer. Whether immunotherapy can be incorporated into neoadjuvant therapy has became a challenging question for researchers.
Case presentation
We present a case of a 65-year-old male who had a history of progressive dysphagia for approximately 1 month. He underwent pertinent studies including computed tomography (CT),gastroscopy,and pathological biopsy resulting in a diagnosis of medium-low differentiated squamous carcinoma of the thoracic segment of the esophagus (cT2N2M0 stage III). After 4 cycles of neoadjuvant chemotherapy combined with immunotherapy, gastroscopy showed the lesion in the esophagus was no longer present. Subsequently, the patient received thoracoscopic radical resection of esophageal cancer and achieved a pathological complete response (pCR) in postoperative pathological evaluation. During the whole treatment, no adverse effect was recorded and to date no evidence of recurrence has been recorded.
Conclusion
Our report suggest that neoadjuvant chemotherapy combined with immunotherapy not only improve the R0 resection and pCR rate in patients with resectable locally advanced esophageal cancer, but also the adverse effects are within the control range. However, the selection of therapeutic strategy, predictors of response to treatment, and interval time between neoadjuvant treatment and surgery still await more reliable evidence-based studies with large prospective samples.
Similar content being viewed by others
Background
Esophageal cancer is the seventh most common cancer worldwide, and has the sixth highest mortality rate among all malignancies [1]. Esophageal cancer is divided pathologically into two major types: adenocarcinoma and esophageal squamous cell carcinoma (ESCC), of which ESCC is more prevalent in Asian countries, especially in China [2]. Despite the development of multidisciplinary treatments such as surgery, radiotherapy, and chemotherapy, the prognosis of patients with esophageal cancer is still unsatisfactory.
Immune checkpoints enhance the tumor-killing function of immune cells by relieving the body's inhibitory effect on immune cells. Many clinical trials have been initiated to explore the immunotherapy of esophageal cancer [3], and immune checkpoint inhibitors (ICI) have been approved for The National Comprehensive Cancer Network (NCCN)/Chinese Society of Clinical Oncology (CSCO) first-line,second line and postoperative adjuvant therapy for esophageal cancer [4,5,6,7]. However, no reliable clinical studies showed the benefit of neoadjuvant immunotherapy in patients with esophageal cancer.
Neoadjuvant therapy refers to certain treatments that are given before radical treatment. It is used to improve the surgical R0 resection rate by reducing the tumor volume, size, or number of lymph nodes, and to reduce the recurrence rate by eliminating micrometastasis [8, 9]. In resectable locally advanced esophageal cancer, according to CROSS study [10], neoadjuvant chemoradiotherapy is approved as the standard treatment in western countries. While in Japan, perioperative neoadjuvant chemotherapy is preferred because of the positive results of the JCOG9907 study [11]. However, the 5-year recurrence rate is still as high as 40–50% [12]. This may be partly due to insufficient systemic therapy at either preoperative or postoperative period. For postoperative period, researches have confirmed only selected patients benefited from adjuvant therapy in clinical trails [13], and others enter surveillance until progression. So, enhancing preoperative treatments maybe a potential way to reduce the recurrence rate.
Neoadjuvant immunotherapy can induce a stronger immunological effect on tumor cells at an early stage of cancer by inducing T cell expansion with less impaired T-cell function compared with that induced by postoperative adjuvant immunotherapy [14,15,16]. In recent years, with approval of immunotherapy in the first line,second line treatment and postoperative adjuvant therapy, researchers have begun to study its efficacy in the perioperative period, including its positive impact on increasing surgical resection rates and improving long-term prognosis. Small sample clinical trials are already underway [17, 18], but have yet to confirm their reliability. In the present study, we report a case of a patient with locally advanced squamous esophageal cancer who underwent 4 cycles of immunotherapy combined with chemotherapy in the preoperative period and achieved a pCR on preoperative evaluation.
Case presentation
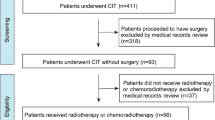
To protect patient's privacy, important patient information is withheld in the following description. The patient is a 65-year-old male with a 5-year history of previous coronary artery disease, who was implanted with a stent in 2016, 2017, and 2019, respectively, and has been taking aspirin, ticagrelor, and atorvastatin postoperatively. The patient denied a history of smoking and alcohol consumption. He was admitted to a hospital after suffering from progressive dysphagia for about 1 month, and was subjected to a gastroscopy, which showed an irregular bulge in the esophageal wall at 22~26 cm from the incisor, occupying 50% of the intestinal lumen (Fig. 1A, B). He was further referred to our hospital. The admission evaluation Eastern Cooperative Oncology Group (ECOG) Performance Status (PS) assessment was 1 point. Computed tomography (CT) of the chest + whole abdomen showed: (1) uneven thickening of the mid-thoracic wall of the esophagus, consistent with esophageal cancer, with a thickness of about 15 mm and a length of about 38 mm (Fig. 2A, B); (2) multiple swollen lymph nodes in the mediastinum, indicating metastasis, the larger one being 10 mm × 10 mm (Fig. 2C–E). Gastroscopy pathological biopsy (Fig. 3A, B) taken from the above hospital and further performed in our hospital showed that esophagus tumor cells showed single scattered or nest-like infiltrative growth, rich cytoplasm, red staining, localized keratinization, which was consistent with medium-low differentiation squamous cell carcinoma. Combined with the above examination, the patient was diagnosed as having (1) medium-low differentiated squamous carcinoma of the thoracic segment of the esophagus (cT2N2M0, stage III, according to the 8th [2017] edition of the American Joint Committee on Cancer staging system); (2) coronary artery disease; stable angina pectoris; and cardiac function class II status after coronary artery stent implantation. After obtaining the patient’s informed consent, four cycles of neoadjuvant chemotherapy combined neoadjuvant immunotherapy (Liposome 210 mg D1 + Nedaplatin 40 mg D1-3 + Tegafur 20 mg bid D1-7 + Pembrolizumab 200 mg D2) were performed from 18 November 2019 to 01 February 2020, 3 weeks a cycle (Fig. 4). After the fourth cycle, gastroscopy (Fig. 5A, B) showed that the lesion at 22~26 cm from the incisor in the esophagus was no longer present and local scar-like changes were also not obvious. Additionally, the patient received CT (Fig. 6A–E) and achieved CR (complete response) assessed by Response Evaluation Criteria in Solid Tumors (RECIST) V.1.1 [19]. On 16 March 2020, thoracoscopic radical resection of esophageal cancer was performed, and the procedure went smoothly. Postoperative pathological biopsy (Fig. 7A, B) showed (1) no clear cancer residue was seen in lymph nodes of groups 7, 8, 8a, 10L, and 12P; (2) no clear cancer residue was seen in all esophageal tissues sent for examination; (3) the tumor regression grading (TRG) was grade 0 according to guidelines of College of American Pathologists [20]. The whole treatment was well tolerated by the patient, and no adverse effects were observed during treatment. As of the date of publication of this article, the patient was still in CR status and PFS had not yet been achieved.
Post-treatment examination: postoperative histopathological findings (A, B). The images were obtained after H&E staining under a magnification of respectively 40× and 40×. The squamous epithelium is intact, and subepithelial proliferation of fibrous connective tissue with vasodilatation and inflammatory cell infiltration
Discussion
Although neoadjuvant chemotherapy or chemoradiotherapy combined with surgery helps to improve resection rate and survival in patients with locally advanced esophageal cancer, surgical R0 resection rate remains poor and most patients present with a recurrence pattern dominated by distant metastases. According to Shapiro et al., this recurrence pattern might result from insufficient intensity of systemic therapy [12]. Therefore,activation of immunity, a systemic therapy, might help to improve the failure pattern of high distant metastasis rate after the original neoadjuvant therapy. Based on the above theory, for the case staged as cT2N2M0, we performed neoadjuvant chemotherapy and added immunotherapy as a way to enhance systemic therapy. The patient achieved R0 resection, and there has been no recurrence so far.
Based on the case report, our article raises following questions that remain to be addressed.
Firstly, identification of metastatic lymph nodes. For patients diagnosed as locally advanced esophageal carcinoma without distant metastasis, the surgical approach and the potential application of neoadjuvant therapy are dependent on preoperative stage, especially N stage. However, 11~56% of lymph nodes were reported to falsely diagnosed as negative for metastasis [21]. Traditionally, only lymph nodes with short diameters > 10 mm, roundish and heterogenous internal density would be considered as metastasis. Nevertheless, Wakita et al. found that [22] 89% of the false negative lymph nodes did not exceed 8 mm in size. In our case, the diameter and shape of one lymph node was also not typical, but under the guidance of our experienced imaging expert, we identified the lymph node. For the vital issue above, maybe more explorations are needed to accurately identify metastatic lymph nodes.
Secondly, the new-emerging “neoadjuvant immunotherapy”, whether should it be used in combination with chemotherapy or chemoradiotherapy. Researches comparing two current and standard neoadjuvant therapy “chemotherapy and neoadjuvant chemoradiotherapy” in resectable locally advanced esophageal carcinoma have revealed no convincing evidence and unified conclusion [23,24,25]. For example, a retrospective analysis conducted by Koch showed clear advantage in overall survival for neoadjuvant chemoradiotherapy in comparison with chemotherapy [23], while Yamagata suggested that chemotherapy might be more effective than neoadjuvant chemoradiotherapy [24]. So,these two therapy strategies are still practiced according to respective institutional protocol. As for the new-emerging therapeutic strategy “neoadjuvant immunotherapy”, whether should it be used in combination with chemotherapy or chemoradiotherapy remains a significant question. ①Immunotherapy combined with chemotherapy. Chemotherapy can further activate the immune system by promoting tumor antigen presentation and destroying immunosuppressive factors [26, 27]. A pilot study combining immunotherapy with chemotherapy reported a satisfactory pCR rate of 31.3%, R0 resection rate of 93.8% and acceptable tolerance in locally advanced ESCC patients [28]. Similar result was also found in our case. ② Immunotherapy combined with chemoradiotherapy. The tumor microenvironment (TME) created by chemoradiotherapy might increase sensitivity to immunotherapy and promote anti-tumor immune response. One study has confirmed that overall survival in ICI combined with chemoradiotherapy was higher than that in the group of concurrent chemoradiotherapy without immunotherapy [17]. Nowadays,clinical trials comparing these two new emerging therapeutic strategies are underway. Therefore, typical application of neoadjuvant treatment in clinical case, would open new way and provide practical evidence for cancer treatment [29, 30].
Thirdly, selection of predictors for response to neoadjuvant immunotherapy. Some patients might exist as neoadjuvant therapy nonresponders, leading to tumor progression and delaying optimal treatment. Consequently, it is vital to screen the responding population with predictors. For example, for neoadjuvant chemotherapy, serum IgG level was found to be a satisfactory predictor [31]. For immunotherapy, researchers have focused on several biomarkers, mainly PD-L1 [32,33,34,35], the tumor mutation burden (TMB) [36,37,38], Mismatch repair (MMR) status [39], and tumor-infiltrating lymphocytes (TILs) [40,41,42]. In summary, PD-L1, TMB, MMR status, or TILs singly might not accurately predict the effect of immunotherapy, and whether to combine multiple predictors in neoadjuvant immunotherapy remains an outstanding question [43]. The case discussed in our study was not tested for these indicators before and after treatment, which is a shortcoming. If those expression could be characterized or quantified before treatment, they might provide solid evidence on predicting efficacy of neoadjuvant immunotherapy combined with chemotherapy.
Finally, the optimal time interval between neoadjuvant therapy and surgery is also concerned. In clinical trials, the standard time to surgery (TTS) after completed neoadjuvant chemoradiotherapy is 4–6 weeks. However, due to administration reasons or being not suitable for surgery, a significant number of patients underwent prolonged TTS after neoadjuvant therapy. Kuo has focused on such an issue concerning survival between standard TTS and prolonged TTS, and has detected no significant difference [44]. For the new emerging therapeutic strategy“neoadjuvant immunotherapy combined with chemotherapy or chemoradiotherapy”, we presented a TTS of 6 weeks. The optimal TTS still remains to be explored. Furthermore, more clinical trials should be performed to clarify differences in clinical benefit between TTS and prolonged TTS.
Conclusion
In resectable locally advanced esophageal cancer, neoadjuvant chemotherapy or chemoradiotherapy combined with surgery has been used as the standard treatment; however, its therapeutic efficacy still needs to be improved. Although neoadjuvant immunotherapy is still at the stage of exploration in small samples, the available clinical data show that its efficacy is significant and its safety and adverse effects are within the control range. In future, neoadjuvant immunotherapy is expected to provide a new treatment strategy for patients with locally advanced esophageal cancer. In addition, based on clinical trial of large prospective samples, the selection of therapeutic strategy, predictors of response to treatment, and interval time between neoadjuvant treatment and surgery will be the essential research directions of neoadjuvant therapy.
Availability of data and materials
All the data are available in the patient’s medical record.
Abbreviations
- ESCC:
-
Esophageal squamous cell carcinoma
- PD-1:
-
Programmed cell death 1
- ICIs:
-
Immune checkpoint inhibitors
- pCR:
-
Pathological complete response
- TRG:
-
Tumor regression grading
- ECOG:
-
Eastern Cooperative Oncology Group
- PS:
-
Performance status
- CT:
-
Computed tomography
- NCCN:
-
National Comprehensive Cancer Network
- CSCO:
-
Chinese Society of Clinical Oncology
- TME:
-
Tumor microenvironment
- TMB:
-
The tumor mutation burden
- MMR:
-
Mismatch repair
- TILs:
-
Tumor-infiltrating lymphocytes
- MSI-H:
-
Microsatellite instability-high
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Thrift AP. The epidemic of oesophageal carcinoma: where are we now? Cancer Epidemiol. 2016;41:88–95.
Alderton GK, Bordon Y. Tumour immunotherapy--leukocytes take up the fight. Nat Rev Immunol. 2012;12(4):237.
Kato K, Cho BC, Takahashi M, Okada M, Lin CY, Chin K, et al. Nivolumab versus chemotherapy in patients with advanced oesophageal squamous cell carcinoma refractory or intolerant to previous chemotherapy (ATTRACTION-3): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(11):1506–17.
Kojima T, Shah MA, Muro K, Francois E, Adenis A, Hsu CH, et al. Randomized phase III KEYNOTE-181 study of pembrolizumab versus chemotherapy in advanced esophageal cancer. J Clin Oncol. 2020;38(35):4138–48.
Luo H, Lu J, Bai Y, Mao T, Wang J, Fan Q, et al. Effect of camrelizumab vs placebo added to chemotherapy on survival and progression-free survival in patients with advanced or metastatic esophageal squamous cell carcinoma: the ESCORT-1st randomized clinical trial. Jama. 2021;326(10):916–25.
Ilson DH. Adjuvant nivolumab in esophageal cancer - a new standard of care. N Engl J Med. 2021;384(13):1269–71.
Leng XF, Daiko H, Han YT, Mao YS. Optimal preoperative neoadjuvant therapy for resectable locally advanced esophageal squamous cell carcinoma. Ann N Y Acad Sci. 2020;1482(1):213–24.
Schermers B, Franke V, Rozeman EA, van de Wiel BA, Bruining A, Wouters MW, et al. Surgical removal of the index node marked using magnetic seed localization to assess response to neoadjuvant immunotherapy in patients with stage III melanoma. Br J Surg. 2019;106(5):519–22.
van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366(22):2074–84.
Ando N, Kato H, Igaki H, Shinoda M, Ozawa S, Shimizu H, et al. A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol. 2012;19(1):68–74.
Shapiro J, van Lanschot JJB, Hulshof MCCM, van Hagen P, van Berge Henegouwen MI, Wijnhoven BPL, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015;16(9):1090–8.
Xu Y, Yu X, Chen Q, Mao W. Neoadjuvant versus adjuvant treatment: which one is better for resectable esophageal squamous cell carcinoma? World J Surg Oncol. 2012;10:173.
Versluis JM, Long GV, Blank CU. Learning from clinical trials of neoadjuvant checkpoint blockade. Nat Med. 2020;26(4):475–84.
Blank CU, Rozeman EA, Fanchi LF, Sikorska K, van de Wiel B, Kvistborg P, et al. Neoadjuvant versus adjuvant ipilimumab plus nivolumab in macroscopic stage III melanoma. Nat Med. 2018;24(11):1655–61.
Forde PM, Chaft JE, Smith KN, Anagnostou V, Cottrell TR, Hellmann MD, et al. Neoadjuvant PD-1 blockade in resectable lung cancer. N Engl J Med. 2018;378(21):1976–86.
Zhang W, Yan C, Zhang T, Chen X, Dong J, Zhao J, et al. Addition of camrelizumab to docetaxel, cisplatin, and radiation therapy in patients with locally advanced esophageal squamous cell carcinoma: a phase 1b study. Oncoimmunology. 2021;10(1):1971418.
Li C, Zhao S, Zheng Y, Han Y, Chen X, Cheng Z, et al. Preoperative pembrolizumab combined with chemoradiotherapy for oesophageal squamous cell carcinoma (PALACE-1). Eur J Cancer. 2021;144:232–41.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Shi C, Berlin J, Branton PA. Protocol for the examination of specimens from patients with carcinoma of the esophagus (Version 4.0.0.0). College Am Pathologists Cancer Protocols. 2017:1–17.
McGuill MJ, Byrne P, Ravi N, Reynolds J. The prognostic impact of occult lymph node metastasis in cancer of the esophagus or esophago-gastric junction: systematic review and meta-analysis. Dis Esophagus. 2008;21(3):236–40.
Wakita A, Motoyama S, Sato Y, Kawakita Y, Nagaki Y, Terata K, et al. Evaluation of metastatic lymph nodes in cN0 thoracic esophageal cancer patients with inconsistent pathological lymph node diagnosis. World J Surg Oncol. 2020;18(1):111.
Koch OO, Weitzendorfer M, Varga M, Tschoner A, Partl R, Perathoner A, et al. Perioperative chemotherapy versus neoadjuvant chemoradiation for patients with adenocarcinoma of the distal esophagus in Austria: a retrospective analysis. World J Surg Oncol. 2019;17(1):146.
Yamagata Y, Saito K, Hirano K, Oya M. Long-term outcomes and safety of radical transmediastinal esophagectomy with preoperative docetaxel, cisplatin, and 5-fluorouracil combination chemotherapy for locally advanced squamous cell carcinoma of the thoracic esophagus. World J Surg Oncol. 2020;18(1):252.
Kumar T, Pai E, Singh R, Francis NJ, Pandey M. Neoadjuvant strategies in resectable carcinoma esophagus: a meta-analysis of randomized trials. World J Surg Oncol. 2020;18(1):59.
Bracci L, Schiavoni G, Sistigu A, Belardelli F. Immune-based mechanisms of cytotoxic chemotherapy: implications for the design of novel and rationale-based combined treatments against cancer. Cell Death Differ. 2014;21(1):15–25.
Chen G, Emens LA. Chemoimmunotherapy: reengineering tumor immunity. Cancer Immunol Immunother. 2013;62(2):203–16.
Yang P, Zhou X, Yang X, Wang Y, Sun T, Feng S, et al. Neoadjuvant camrelizumab plus chemotherapy in treating locally advanced esophageal squamous cell carcinoma patients: a pilot study. World J Surg Oncol. 2021;19(1):333.
Japan Esophageal S. Japanese Classification of Esophageal Cancer, 11th Edition: part I. Esophagus. 2017;14(1):1–36.
Japan Esophageal S. Japanese Classification of Esophageal Cancer, 11th Edition: part II and III. Esophagus. 2017;14(1):37–65.
Nakaya S, Ogawa R, Hayakawa S, Fujihata S, Okubo T, Sagawa H, et al. Serum IgG level is a predicting factor for the response to neoadjuvant chemotherapy in patients with esophageal squamous cell carcinoma. World J Surg Oncol. 2021;19(1):217.
Camidge DR, Schenk EL. Blood-Based Biomarkers for Predicting Immunotherapy Benefit in Lung Cancer. Cell. 2020;183(2):303–4.
Hodi FS, Chiarion-Sileni V, Gonzalez R, Grob J-J, Rutkowski P, Cowey CL, et al. Nivolumab plus ipilimumab or nivolumab alone versus ipilimumab alone in advanced melanoma (CheckMate 067): 4-year outcomes of a multicentre, randomised, phase 3 trial. The Lancet Oncology. 2018;19(11):1480–92.
Wu YL, Lu S, Cheng Y, Zhou C, Wang J, Mok T, et al. Nivolumab versus docetaxel in a predominantly chinese patient population with previously treated advanced NSCLC: CheckMate 078 randomized phase III clinical trial. J Thorac Oncol. 2019;14(5):867–75.
Liu X, Guo CY, Tou FF, Wen XM, Kuang YK, Zhu Q, et al. Association of PD-L1 expression status with the efficacy of PD-1/PD-L1 inhibitors and overall survival in solid tumours: A systematic review and meta-analysis. Int J Cancer. 2020;147(1):116–27.
Wu Y, Xu J, Du C, Wu Y, Xia D, Lv W, et al. The predictive value of tumor mutation burden on efficacy of immune checkpoint inhibitors in cancers: a systematic review and meta-analysis. Front Oncol. 2019;9:1161.
Marabelle A, Fakih M, Lopez J, Shah M, Shapira-Frommer R, Nakagawa K, et al. Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol. 2020;21(10):1353–65.
Samstein RM, Lee CH, Shoushtari AN, Hellmann MD, Shen R, Janjigian YY, et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat Genet. 2019;51(2):202–6.
Cortes-Ciriano I, Lee S, Park WY, Kim TM, Park PJ. A molecular portrait of microsatellite instability across multiple cancers. Nat Commun. 2017;8:15180.
Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJ, Robert L, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515(7528):568–71.
Uryvaev A, Passhak M, Hershkovits D, Sabo E, Bar-Sela G. The role of tumor-infiltrating lymphocytes (TILs) as a predictive biomarker of response to anti-PD1 therapy in patients with metastatic non-small cell lung cancer or metastatic melanoma. Med Oncol. 2018;35(3):25.
Mariathasan S, Turley SJ, Nickles D, Castiglioni A, Yuen K, Wang Y, et al. TGFβ attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature. 2018;554(7693):544–8.
Lu S, Stein JE, Rimm DL, Wang DW, Bell JM, Johnson DB, et al. Comparison of biomarker modalities for predicting response to PD-1/PD-L1 checkpoint blockade: a systematic review and meta-analysis. JAMA Oncol. 2019;5(8):1195–204.
Kuo YH, Chien YW, Chen PR, Feng CL, Li CC, Chien CR. Impact of the interval between neoadjuvant concurrent chemoradiotherapy and esophagectomy in the modern era: a population-based propensity-score-matched retrospective cohort study in Asia. World J Surg Oncol. 2019;17(1):222.
Acknowledgements
The authors thank the patient’s family for their approval for publication.
Funding
This work was funded by Guangdong Basic and Applied Basic Research Regional Combination The Youth Foundation (2019A1515110155); Guangdong Natural Science Foundation Surface Project (2021A1515010807); Shenzhen Natural Science Foundation Basic Research Surface Project (JCYJ20210324123012035); Guangdong Medical Scientific Technology Foundation (A2019529); the Fundamental Research Funds for the Central Universities, Sun Yat-sen University (Grant No. 22qntd3702).
Author information
Authors and Affiliations
Contributions
Jiehao Liao and Tingwei Li collected and assembled the data. Huiru Dai drafted the manuscript. Huiru Dai, Minling Liu, and Xueying Li contributed to manuscript writing. Wensheng Huang collected, assembled and analyzed CT images, and provided constructive guidance. Shuo Fang and Yun Li designed the study and provided final approval of the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editors-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dai, H., Liu, M., Li, X. et al. A case study of combined neoadjuvant chemotherapy and neoadjuvant immunotherapy in resectable locally advanced esophageal cancer. World J Surg Onc 20, 267 (2022). https://doi.org/10.1186/s12957-022-02732-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02732-w