Abstract
Background
The extent of surgery in patients with unilateral multifocal papillary thyroid microcarcinoma (UMPTMC) remains to be controversial. Aimed to improve surgical management of UMPTMC, this study was performed to identify the recurrence of UMPTMC and analyze its predictive factors.
Methods
This study was approved by the Ethical Committee of The First Hospital of the Jilin University, and written informed consent was given by participants for their clinical records to be used in this study. We retrospectively analyzed a total of 97 consecutive patients who underwent initial surgery for the treatment of UMPTMC at The First Hospital of Jilin University, between October 2005 and October 2006.
Results
Altogether, 97 patients of UMPTMC have been enrolled in our study, in which 57 cases were performed with hemithyroidectomy (HT) while other 40 cases with total thyroidectomy (TT). The sum diameter of all tumors >1 cm was more frequent in HT group than in TT group (40.35 vs 20%; p = 0.046). Positive central lymph nodes were found more frequently in the TT patients than in the HT patients (80 vs 59.65%; p = 0.046). Tumor recurrence was seen more frequently in the HT cases than in the TT cases (26 vs 5%; p = 0.007). The disease-free survival period was significantly shorter for the HT patients than for the TT patients (p = 0.0059 by the log-rank test). The disease-free survival rates at 5 and 10 years were 91.23 and 73.68%, respectively, in the HT group and 100 and 92.5%, respectively, in the TT group. Univariate analysis by Cox’s proportional hazards method showed male gender, sum diameter of all tumors >1 cm, and central lymph node metastases (CLNM) to be risk factors for recurrence of HT patients. Male gender and sum diameter >1 cm were factors identified for multivariate analysis by Cox’s proportional hazards method which yielded risk ratios of 3.037 [CI 1.026–8.988; p = 0.045] and 5.475 [CI 1.389–21.572; p = 0.015] in the HT group.
Conclusions
In summary, with an increased risk of recurrence, TT may be more reasonable as initial surgery in UMPTMC, especially with male gender and total tumor diameter greater than 1 cm.
Similar content being viewed by others
Background
Papillary thyroid carcinoma (PTC) is the most common type of thyroid carcinoma, and its incidence has been increasing around the world due to widespread use of ultrasonography-guided fine needle aspiration cytology (FNAC) for small lesions [1–3]. These increases are due mostly to the increase in the detection of papillary carcinomas <1 cm in size. PTC measuring 10 mm or less in the greatest diameter, which is called papillary thyroid microcarcinoma (PTMC), accounts for 39% of the cases of thyroid cancer in the USA [3] and 43.1% of the cases in Korea [4].
However, the extent of surgery in patients with PTMC continues to be controversial. According to American Thyroid Association guidelines in 2015, hemithyroidectomy (HT) alone is sufficient treatment for small, unifocal, intrathyroidal carcinomas in the absence of prior head and neck irradiation, familial thyroid carcinoma, or clinical detectable cervical lymph node metastasis [5]. Total thyroidectomy (TT) is performed when the nodule is preoperatively confirmed to be malignant in bilateral lobes by FNAC [5]. Nevertheless, as the 17–87% of PTC were multifocal [6], there were different opinions on how to manage the unilateral multifocal PTMC (UMPTMC). Most surgeons prefer to proceed with TT, which would be associated with the lowest risk of locoregional recurrence. However, the patient would receive high-dose lifelong thyroid hormone replacement and take the higher risks of recurrent laryngeal nerve injury and hypoparathyroidism. Others would be inclined to persuade UMPTMC patients to accept HT with a slightly higher risk of locoregional recurrence. Based on these disputes, we find it important to study the clinical and pathologic predictors of recurrence in UMPTMC. Similar studies that have been published on this subject were rare [7–9]; moreover, most of these reports do not provide detailed follow-ups of the contralateral nodule. According to previous studies [7–9], the 10-year recurrent and mortality rate of UMPTMC with different surgery strategies are still unknown; therefore, the cost-effectiveness of two different surgeries is hard to evaluate.
To help elucidate these matters further, we developed a retrospective cohort study of both the HT and TT strategies in the management of UMPTMC in order to facilitate decision-making for patients and surgeons. Firstly, the objective of this study was to identify the recurrence and mortality of UMPTMC and then to analyze its predictive factors.
Methods
Patients
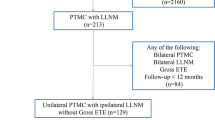
This study was approved by the Ethical Committee of The First Hospital of Jilin University, and written informed consent was given by participants for their clinical records to be used in this study. We retrospectively analyzed a total of 673 consecutive patients who underwent initial surgery for the treatment of thyroid carcinoma at The First Hospital of Jilin University, between October 2005 and October 2006. All patients recruited in the study met the following criteria: (a) patient information found in a hospital database and (b) patients with a postoperative pathological diagnosis of UMPTMC. (c) Patients underwent HT with unilateral prophylactic central lymph node dissection (CLND) or TT with bilateral prophylactic CLND. Patients were excluded from the study if they had pathological types of thyroid malignancies other than UMPTMC; preoperative confirmation of bilateral nodule, or obviously extrathyroidal invasion; preoperative confirmation of clinically positive (ultrasound positive or palpable positive) central and lateral lymph node; lack of a preoperative examination; and a history of neck radiotherapy, distant metastasis, and previous thyroid surgery. Finally, this study enrolled 97 patients with UMPTMC.
Initial treatment and contralateral lobe evaluation
Clinical diagnosis was initially made by examination of ultrasound and FNAC. Ultrasonography cervical mapping was done by experienced, specially trained radiologist. For the UMPTMC, TT or hemithyroidectomy was performed according to the patients’ willingness. Before that, surgeons have explained both the risks and benefits of each kind of operation and given informed consent form to patients.
Ultrasound (US) of thyroid and neck lymph node was performed by two physicians with more than 5-year experience in thyroid US (Dr. Shuai Xue and Dr. Peisong Wang); they were blinded to the previously obtained findings. If their results were inconsistent, another physician with more than 15-year experience of thyroid US (Dr. Jia Liu) was asked for consultation.
Clinicopathological variable
Demographic data on patient clinical features (gender, age at diagnosis), tumor histological characteristics (diameter of largest tumor, sum diameter of all tumors (according to histopathology reports), foci number, primary tumor laterality, extrathyroidal extension, TNM stage, presence of chronic thyroiditis), and central lymph node metastases (CLNM) were recorded.
Follow-up, recurrence, and reoperation
Until 2011, TSH-suppressive hormonal therapy was applied to postoperative patients and all cases did not receive radioactive iodine therapy. Postoperative physical examinations were performed every 3–6 months for 10 years. During the period of follow-up, all patients underwent ultrasound examinations of the neck as well as thyroid function test (including thyroglobulin level). We considered suspicious lymph node as recurrence using FNAC and washout fluid. Meanwhile, when nodule with diameter larger than 5 mm newly occurred in the contralateral lobe, FNAC was performed to these patients. If the result was thyroid carcinoma, we defined it as recurrence and recommended completion reoperation at the same time. We took the contralateral lobe and central and lateral compartment into account as the local regional recurrence. No patients had distant metastasis. A follow-up at least 10 years post-surgery was achieved for 89 patients.
Statistical analysis
To identify differences between groups for specific variables, SPSS version 16 software (SPSS Inc, Chicago, IL) was used for statistical analysis, which was performed by Pearson’s chi-square test or Student’s t test. Survival curves were drawn by Kaplan-Meier method and statistically analyzed by the log-rank test. To characterize UMPTMC, univariate analysis was performed by Cox’s proportional hazards method for disease-free survival. Factors analyzed were male gender, age (by year), diameter of the largest tumor (millimeters), sum diameter of all tumors, foci number, primary tumor laterality, extrathyroidal extension, TNM stage, presence of chronic thyroiditis, and CLNM. Multivariate analysis was performed by Cox’s proportional hazards method for disease-free survival and the risk factors. A p value <0.05 was considered statistically significant.
Results
Altogether, 97 patients of UMPTMC have been enrolled in our study, in which 57 cases were performed with HT while other 40 cases with TT. The clinicopathological characteristics of the UMPTMC (n = 97) are shown in Table 1. The sum diameter of all tumors >1 cm was more frequent in HT group than in TT group (40.35 vs 20%; p = 0.046). Positive central lymph nodes were found more frequently in the TT patients than in the HT patients (80 vs 59.65%; p = 0.046). Tumor recurrence was seen more frequently in the HT cases than in the TT cases (26 vs 5%; p = 0.007). There were no significant differences between the two groups in terms of age, gender, extrathyroidal extension, diameter of the largest tumor, foci number, primary tumor laterality, TNM stage, presence of chronic thyroiditis, average follow-up period, and the number of disease-related death.
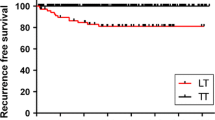
The disease-free survival period was significantly shorter for the HT patients than for the TT patients (p = 0.0059 by the log-rank test) (Fig. 1). Details of recurrent cases are shown in Table 2. The disease-free survival rates at 5 and 10 years were 91.23 and 73.68%, respectively, in the HT group and 100 and 92.5%, respectively, in the TT group. Survival curves did not differ statistically between groups (data shown in Table 1 and Fig. 2).
There were huge concerns about that most patients with UMPTMC may have microfoci of PTC in the contralateral lobe. They may believe that recurrent nodule is not newly occurred in the contralateral lobe but microfoci which not be detected at the time of diagnosis. We compared the characteristics of contralateral lobe between HT and TT groups. Fourteen recurrent cases were PTMC which is diagnosed by FNAC in HT group; meanwhile, only two cases had microfoci of PTC in the contralateral lobe in TT group at the time of diagnosis. p value was less than 0.05 (p = 0.037), and the difference was significant. Furthermore, we also analyzed the clinicopathological features in the contralateral lobe between HT and TT. The differences were not significant maybe owing to the small number of patients (data shown in Table 3).
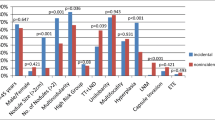
Univariate analysis by Cox’s proportional hazards method showed male gender, sum diameter of all tumors >1 cm, and CLNM to be risk factors for recurrence of HT patients (Table 4). Age, extrathyroidal extension, diameter of the largest tumor, foci number, primary tumor laterality, TNM stage, and presence of chronic thyroiditis were not predictors of recurrence. The risk ratio for male gender, sum diameter >1 cm, and positive CLNM were 5.676 [confidence interval (CI) 2.034–15.839; p = 0.001], 9.072 [CI 2.533–32.491; p = 0.001], and 4.951 [CI 1.114–21.998; p = 0.036] in the HT group. No other risk ratios obtained were of interest. Male gender and sum diameter >1 cm were factors identified for multivariate analysis by Cox’s proportional hazards method (Table 5) which yielded risk ratios of 3.037 [CI 1.026–8.988; p = 0.045] and 5.475 [CI 1.389–21.572; p = 0.015] in the HT group. Accordingly, male gender and sum diameter >1 cm were shown to be independent predictors of disease-free survival.
Discussion
Many studies have found that multifocal PTC comprised a more aggressive form of PTC since it was associated with more frequent N1a/N1b disease and occurs more frequently in T3/T4 patients [10]. TT was recommended to multifocal PTC patients for the reason multifocality was associated with an increased risk of disease recurrence or persistence [11, 12]. Nevertheless, PTMC was an inert form of PTC with low risk of recurrence and good prognosis. Therefore, how to manage the patients with UMPTMC remains controversial until now.
Therefore, we investigate clinical and pathologic characteristics of these two group patients, who received HT and TT, respectively. Compared between two groups, we find the disease-free survival period was significantly shorter for the HT patients than for the TT patients (p = 0.0059 by the log-rank test). Some researches demonstrated most PTMCs had excellent prognosis, and multifocality did not appear to have significant clinical importance in these tumors [12, 13]. Presence of heterogeneity in clinicopathological features and lack of long-time follow-ups lead to the identical disease-free survival period between unifocal and multifocal PTMC. Consistent with our study, Pyo et al. reported that tumor multifocality was significantly correlated with tumor recurrence in PTMCs (odds ratio, 2.002; 95% confidence interval, 1.475 to 2.719, p < 0.001) [14]. With an increased risk of recurrence, HT is not a reasonable operation for UMPTMC. If we recommend TT for all UMPTMCs, the patients would be informed about the need for lifelong thyroid hormone replacement and the risks of recurrent laryngeal nerve injury and hypoparathyroidism. Accordingly, by univariate and multivariate analysis by Cox’s proportional hazards methods, we try to ascertain clinical and pathologic predictors of recurrence in UMPTMC.
In our study, univariate analysis showed male gender, sum diameter of all tumors >1 cm, and CLNM to be risk factors for recurrence of HT patients, as reported in previous studies by Kiriakopoulos et al. [10] and Huang et al. [15], although they focused on multifocal PTC. Kiriakopoulos et al. also found foci number correlates with male gender and lymph node metastases [10]. According to a consensus report of the European Society of Endocrine Surgeons, they recommended bilateral prophylactic CLND for patients with total tumor diameter (sum of the largest diameter of all foci) greater than 1 cm, because the frequency of subclinical CLNM is higher in multifocal PTC. Combining literatures on multifocal PTC and our study, we believe TT should be considered for UMPTMC, especially with male gender and total tumor diameter greater than 1 cm [6].
The gene(s) responsible for multifocal PTC have not yet been identified, and this disorder is now being investigated on a molecular level. Several researches found most of the patients with multifocal PTC had the BRAFV600E mutation in one or more tumor foci and all BRAFV600E-positive multifocal PTC showed more aggressive features [16, 17]. Moreover, many studies have investigated multifocal PTC clonality through a number of approaches, including X-chromosome inactivation, BRAF mutation, RET rearrangements, loss of heterozygosity, or allelic imbalances of distinct cancer foci [17–19]. High rate of independent clonality found in multifocal PTC patients lends support to the notion of field cancerization, whereby carcinogenic agents would affect a wide range of genetic susceptible cells, resulting in their simultaneous transformation [19]. Based on this theory, the contralateral lobe of UMPTMC has higher risk of recurrence attribute to genetic predispositions, environmental exposures, and epidemiological factors. That explains why we recommend TT for UMPTMC, especially with male gender and total tumor diameter greater than 1 cm.
Our study has several limitations. The first limitation is the small number of patients in the study population; due to the incidence of UMPTMC is low, and we want long duration of follow-up, we just summarized patients between October 2005 and October 2006. The second limitation is that until 2011, TSH-suppressive hormonal therapy was applied to postoperative patients and all cases did not receive radioactive iodine ablation. At that time, there was no guideline in China, which we could follow to recommend TSH-suppressive hormonal and radioactive iodine therapy. Finally, we did not use radioiodine whole body scan and PET scan routinely for all the TT patients. This might have some influence on the accuracy of diagnosis of recurrence in TT group, especially distant metastasis. However, the postoperative patients with negative US and thyroglobulin results are less likely to have positive radioiodine and PET scan. Despite these limitations, our study has important implications for UMPTMC management and provides significant information for PTMC guideline formation. Furthermore, to our knowledge, this study is the first report to recommend the optimal surgery strategy for UMPTMC patients.
Conclusions
Taken together, with an increased risk of recurrence, TT may be more reasonable as initial surgery in UMPTMC, especially with male gender and total tumor diameter greater than 1 cm. A multicentric pragmatic randomized controlled clinical trial with large population is needed to assess the effects on recurrence, quality of life, and cost-effectiveness outcomes of different treatments and follow-up regimen for UMPTMC.
Abbreviations
- BRAF:
-
B-Raf and v-Raf murine sarcoma viral oncogene homolog B
- CLND:
-
Central lymph node dissection
- CLNM:
-
Central lymph node metastases
- FNAC:
-
Fine needle aspiration cytology
- HT:
-
Hemithyroidectomy
- PTC:
-
Papillary thyroid carcinoma
- PTMC:
-
Papillary thyroid microcarcinoma
- RET:
-
Rearranged during transfection
- TT:
-
Total thyroidectomy
- UMPTMC:
-
Unilateral multifocal PTMC
References
Hirokawa M, Kudo T, Ota H, et al. Pathological characteristics of low-risk papillary thyroid microcarcinoma with progression during active surveillance. Endocr J. 2016;63:805–10.
Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006;295:2164–7.
Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg. 2014;140:317–22.
Lee JH, Shin SW. Overdiagnosis and screening for thyroid cancer in Korea. Lancet. 2014;384:1848.
Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26:1–133.
Iacobone M, Jansson S, Barczyński M, et al. Multifocal papillary thyroid carcinoma—a consensus report of the European Society of Endocrine Surgeons (ESES). Langenbecks Arch Surg. 2014;399:141–54.
Mehanna H, Al-maqbili T, Carter B, et al. Differences in the recurrence and mortality outcomes rates of incidental and nonincidental papillary thyroid microcarcinoma: a systematic review and meta-analysis of 21 329 person-years of follow-up. J Clin Endocrinol Metab. 2014;99:2834–43.
Soares P, Celestino R, Gaspar da Rocha A, et al. Papillary thyroid microcarcinoma: how to diagnose and manage this epidemic? Int J Surg Pathol. 2014;22:113–9.
Dideban S, Abdollahi A, Meysamie A. Thyroid papillary microcarcinoma: etiology, clinical manifestations, diagnosis, follow-up, histopathology and prognosis. Iran J Pathol. 2016;11:1–19.
Kiriakopoulos A, Petralias A, Linos D. Multifocal versus solitary papillary thyroid carcinoma. World J Surg. 2016;40:2139–43.
Kim HJ, Sohn SY, Jang HW, et al. Multifocality, but not bilaterality, is a predictor of disease recurrence/persistence of papillary thyroid carcinoma. World J Surg. 2013;37:376–84.
Wu ZG, Yan XQ, Su RS, et al. How many contralateral carcinomas in patients with unilateral papillary thyroid microcarcinoma are preoperatively misdiagnosed as benign? World J Surg. 2016. doi:10.1007/s00268-016-3701-0.
Kim KJ, Kim SM, Lee YS, et al. Prognostic significance of tumor multifocality in papillary thyroid carcinoma and its relationship with primary tumor size: a retrospective study of 2,309 consecutive patients. Ann Surg Oncol. 2015;22:125–31.
Pyo JS, Sohn JH, Kang G. Detection of tumor multifocality is important for prediction of tumor recurrence in papillary thyroid microcarcinoma: a retrospective study and meta-analysis. J Pathol Transl Med. 2016;50:278–86.
Huang G, Tian X, Li Y, et al. Clinical characteristics and surgical resection of multifocal papillary thyroid carcinoma: 168 cases. Int J Clin Exp Med. 2014;7:5802–7.
Ahn HY, Chung YJ, Kim BS, et al. Clinical significance of the BRAFV600E mutation in multifocal papillary thyroid carcinoma in Korea. Surgery. 2014;155:689–95.
Lin X, Finkelstein DS, Zhu B, et al. Molecular analysis of multifocal papillary thyroid carcinoma. J Mol Endocrinol. 2008;41:195–203.
Shattuck TM, Westra WH, Ladenson PW, et al. Independent clonal origins of distinct tumor foci in multifocal papillary thyroid carcinoma. N Engl J Med. 2005;352:2406–12.
Lu Z, Sheng J, Zhang Y, et al. Clonality analysis of multifocal papillary thyroid carcinoma by using genetic profiles. J Pathol. 2016;239:72–83.
Acknowledgements
None.
Funding
None.
Availability of data and materials
Please contact the author for data requests.
Authors’ contributions
PW participated in the design of the study, and JL performed the statistical analysis. GC conceived of the study and participated in its design, and SX drafted the manuscript. All authors read and approved the final manuscript.
Authors’ information
Guang Chen is a member of International Society of Surgery (ISS), a member of International Association of Endocrine Surgeon (IAES), and a council member of Asian Association of Endocrine Surgeon (AsAES).
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The ethics statement has been provided in Additional file 1.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
The ethics statement of our study by the Ethics Committee of Jilin University affiliated First Hospital. (DOC 58 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Xue, S., Wang, P., Liu, J. et al. Total thyroidectomy may be more reasonable as initial surgery in unilateral multifocal papillary thyroid microcarcinoma: a single-center experience. World J Surg Onc 15, 62 (2017). https://doi.org/10.1186/s12957-017-1130-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-017-1130-7