Abstract
Background
The previous study showed that the Mandarin Tinnitus Questionnaire (MTQ) has satisfactory reliability and validity. We have also completed the classification of the severity of tinnitus based on MTQ scores. In clinical studies, efficacy is often judged by whether results are statistically significant; however, statistical significance does not necessarily equate to clinical significance, whereas the minimum clinically important difference (MCID) of the scale does. In the following project, we will explore the MCID of the MTQ.
Methods
We recruited participants aged 18 years and above who sought treatment for primary or secondary tinnitus at the Otorhinolaryngology Department of the Hearing Center of West China Hospital, Sichuan University from September 2020 to September 2021. The participants had to undergo the following four assessments of tinnitus severity: doctor evaluation, self-report, the MTQ, and the visual analog scale (VAS), all at baseline and at the follow-up. The MCIDs of the MTQ were established via anchor-based and distribution-based methods. The anchor method used the VAS and self-reported clinical impression as anchors and defined the treatment effectiveness by mean/median and receiver operating characteristic (ROC) curve, while methods of effect size (ES), standard error of measurement (SEM), and reliability change index (RCI) were used in distribution-based methods.
Results
A total of 115 patients were investigated in this study, 57.4% of whom were women. The average age was 43.2 ± 13.20 years. The average MTQ and VAS scores at baseline were 31.3 ± 14.90 and 5.03 ± 2.24, respectively, while the average MTQ and VAS scores at follow-up were 15.9 ± 11.70 and 3.58 ± 2.48, respectively. Moreover, in terms of self-reported clinical impressions, 19 patients indicated that they were cured (16.5%), 24 that it was much better (20.9%), 63 that there was no change (54.8%), and 9 that it was much worse (7.8%). The MCIDs for the change in total MTQ ranged from 6.29 to 19.00, those for improvement from 1.09 to 22.75, and those for deterioration from 3.50 to 7.64.
Conclusion
We selected an absolute value of 7.5 as the MCID for the MTQ score. An increase in MTQ score more than 7.5 was considered aggravation of tinnitus, and a decrease in MTQ score more than 7.5 was considered a reduction in tinnitus.
Similar content being viewed by others
Background
The global prevalence of tinnitus is approximately 14%, and more than 2% of people suffer from severe tinnitus [1], with 7.1% actively seeking medical attention and 2.5% requiring clinical intervention [2]. Tinnitus can cause a range of issues, including increased stress, anxiety, depression, sleep disorders, difficulty concentrating, and hearing impairment [3]. Approximately 26% of patients with tinnitus are affected by anxiety [4], 48% to 60% by sadness [5], and 76% by insomnia [6].
Subjective tinnitus can only be quantified indirectly since subjective tinnitus-induced suffering cannot be satisfactorily represented by psychoacoustic parameters (e.g., tinnitus loudness) [7]. Pinto et al. [8] reviewed 16 papers on the most prevalent psychiatric diagnostic criteria and measures of tinnitus annoyance and concluded that psychological diseases, tinnitus severity, and tinnitus distress in patients are all significantly associated. Tinnitus severity and tinnitus distress are strongly related to mental disease. As a result, a variety of tinnitus self-report questionnaires are available to assess the intensity of tinnitus by questioning patients about psychological disorders such as depression, anxiety, and stress to help explain the distress produced by tinnitus [9, 10].
The tinnitus questionnaire (TQ) was one of the first to be developed and the most commonly used [11]. It was developed by Hallam in 1987 and contains 52 items in five categories, namely emotional and cognitive stress, intrusiveness, auditory perceptual difficulties (APDs), somatic complaints, and sleep disturbance [12]. The original English version of the TQ has high internal consistency and reliability [12]. The TQ has been translated into German, Spanish, French, Dutch, Cantonese, and Mandarin [13]. The various translated versions have been widely used in the clinical setting, and their internal consistency and retest reliability have been demonstrated [13,14,15,16].
The Mandarin Tinnitus Questionnaire (MTQ) is a Mandarin version of the TQ derived via exploratory factor analysis [13]. It includes 37 questions each in five dimensions: cognitive distress, emotional distress, APDs, intrusiveness, and sleep disturbance. The MTQ and the English, German, and Cantonese TQs have consistent reliability and validity [13]. Logistic regression analysis resulted in the following classification of the severity of tinnitus based on MTQ scores: no tinnitus (a score of < 21), mild tinnitus (21–36), moderate tinnitus (37–47), and severe tinnitus (> 47) [17].
In clinical studies, efficacy is often judged by whether results are statistically significant; however, statistical significance does not necessarily equate to clinical significance, whereas the minimum clinically important difference (MCID) of the scale does [18, 19]. Thus, the MCID of the MTQ should be analyzed, and such studies are rare. Adamchic et al. [20] showed a 5-point decrease in the MCID for improvement and a 1-point increase in the MCID for worsening of the TQ score. Hall et al. [21] recommended using at least the median MCID of 12 (as determined in their study) to indicate a clinically meaningful change in the German TQ score. As different language versions of the TQ contain different numbers of items, the MCID should be determined for each.
In summary, there are few studies regarding efficacy assessment and determination of the MCID of different translated versions of the TQ, including the MTQ. We aimed to fill this clinical gap by analyzing the MCID of the MTQ. Our results may guide the scientific design of clinical treatment plans for patients with tinnitus.
Methods
Participants
In this study, we recruited participants aged 18 years and above who sought treatment for primary or secondary tinnitus at the Otorhinolaryngology Department of the Hearing Center of West China Hospital, Sichuan University from September 2020 to September 2021. Patients who were unable to complete the relevant assessment owing to cognitive impairment or difficulty in understanding, psychiatric disorders, or auditory hallucinations were excluded. This research was approved by the Biomedical Research Ethics Committee of West China Hospital (No. 2020 [311]). Participants were enrolled after they provided written informed consent.
Study design
We collected the demographic information (name, sex, age, telephone number), medical history (side of tinnitus), and tinnitus assessment data (assessment date and four assessment outcomes) of each participant at baseline. After 6 months, we followed them up telephonically. The different types of treatment interventions that participants underwent in different study centers were collected, and their self-reported clinical impression after treatment was recorded, as follows: cure/much better/no change/much worse. In addition, the participants had to undergo the following four assessments of tinnitus severity: doctor evaluation, self-report, the MTQ, and the visual analog scale (VAS), all at baseline and at the follow-up. The doctor's evaluation and the self-report were carried out independently.
Doctor evaluation and self-report
First, the doctors asked all patients the following five questions: (1) Do you feel anxious or nervous because of tinnitus? (2) Do you have difficulty in listening to others because of tinnitus? (3) Do you feel that you can never get away from tinnitus? (4) Is sleeping a problem because of tinnitus? (5) Does tinnitus result in headache, ear pain, or tension in the muscles of the head? Based on the answers to these five questions, the patients' tinnitus severity was classified as none, slight, mild, or severe. These five questions were designed to be analogous to emotional distress, auditory perceptual difficulties, cognitive distress, sleep disturbance, and intrusiveness [2]. Second, patients were asked to self-report on their current tinnitus severity according to the same four levels: none, slight, mild, and severe. The doctor’s evaluation and self-report were performed on the same day.
MTQ
The MTQ is a self-administered scale that consists of 37 questions, and the total score ranges from 0 (no distress) to 74 (very severe distress) [17]. This questionnaire indicates the degree of tinnitus-related psychopathological symptoms. According to the total MTQ score, patients are divided into four distress levels: none (0–20), mild (21–36), moderate (37–46), and severe (47–74). A higher score indicates a higher degree of tinnitus-induced distress.
VAS
The VAS is a very simple, subjective, psychometric response scale. The participants answered it last so that the results of the MTQ would not be influenced by any tiredness that the participants felt. In this study, patients conveyed their tinnitus-induced distress by indicating a position along a line marked 0 to 10. Zero indicated that the patient was not distressed, while 10 indicated that the patient was very severely distressed.
Statistical analysis
All continuous variables are presented as means (standard deviations [SDs]), and categorical data are presented as counts (percentages). Student’s t test or one-way analysis of variance was used for the comparison of continuous variables among groups, and the chi-squared test or Fisher’s exact test was used for the comparison of categorical variables between groups, as appropriate. Two regression models were used for flexibility in examining associations between the exposure and each outcome. The change in MTQ score from baseline was defined as ΔMTQ. An improvement in the MTQ score indicated a reduction in tinnitus severity (including much better, ΔVAS ≥ 1), while deterioration indicated exacerbation of tinnitus (including much worse, ΔVAS ≤ − 1).
There is no standardized method to determine the ideal MCID. However, methodologists generally recommend triangulating the results of multiple methods [21]. In this study, the MCIDs of the MTQ were established via anchor-based and distribution-based methods.
MCIDs determined via an anchor-based method
MCID calculations should be based on patient-reported outcomes, e.g., the VAS score and self-reported clinical impression, which are correlated at r ≥ 0.30–0.35 and consist of appropriate patient-based and clinical anchors [22]. Thus, we calculated the Spearman rank correlation of self-reported clinical impression with the ΔMTQ scores and the Pearson correlation of the VAS score with the MTQ scores at baseline and at 6 months. These two methods were used as anchors to define the treatment effectiveness. Patients who differed by at least one point on the VAS at baseline and at 6 months were censored. The ΔMTQ score was calculated, and the mean (for normally distributed variables) or median (for non-normally distributed variables) absolute ΔMTQ score was recorded as the MCID. The VAS and self-reported clinical impression were used as the main anchors, and a receiver operating characteristic (ROC) curve was used to determine the optimal MCID cut-off point for the MTQ score.
MCIDs determined via a distribution-based method
A distribution-based approach was used to calculate the magnitude of small, intermediate, and large domain score differences [23]. On the basis of benchmark effect sizes (ESs) determined in a previous study (0.2, small; 0.5, intermediate; and 0.8 or greater, large) [24], small, intermediate, and large domain score differences in MTQ scores were calculated via the following equation:
In this equation, SD is the standard deviation of the baseline MTQ score. Domain score differences calculated with the above equation were compared with the observed differences in mean MTQ scores between the different clinical anchor states [25].
The standard error of measurement for the MTQ score was also computed, as follows:
where \(\alpha\) is the test–retest reliability of the MTQ, i.e., 0.93 [13]. We calculated 1.96 SEMs as an estimate of the MCID to reduce the probability of false positive results [26].
where the reliable change index (RCI) is the change in MTQ score divided by the square root of the SEM [27]. The RCI is an expression of the change in score in SD units, much like a z score. Therefore, we set this equal to 1.96 (the value on a standard normal curve associated with a 95% confidence interval) according to Beaton et al. [28], and solved for the change score in the numerator, to give the minimum change in MTQ score considered significantly different to no change at all (at p < 0.05).
Statistical software
All statistical tests were two-sided, and p < 0.05 was regarded as significant. All statistical analyses were performed by using open-source statistical analysis software (R version 4.0.5; The R Foundation for Statistical Computing, Vienna, Austria), IBM SPSS Statistics for Windows version 25 (IBM Corp., Armonk, New York, USA), and GraphPad Prism 8.3.0 software (GraphPad Software, San Diego, California, USA).
Results
Sociodemographic and clinical characteristics of patients with tinnitus
A total of 115 patients were investigated in this study, 57.4% of whom were women (Table 1). The average age was 43.2 ± 13.20 years. Among the patients, 40.0% complained of bilateral tinnitus, 33.0% of left-sided tinnitus, and 27.0% of right-sided tinnitus. The doctor-evaluated tinnitus severity was mostly slight, accounting for 69.6% at baseline and 60.9% at the follow-up. Nineteen patients self-reported that their tinnitus disappeared by the time of the follow-up. The average MTQ and VAS scores at baseline were 31.3 ± 14.90 and 5.03 ± 2.24, respectively, while the average MTQ and VAS scores at follow-up were 15.9 ± 11.70 and 3.58 ± 2.48, respectively. Moreover, in terms of self-reported clinical impressions, 19 patients indicated that they were cured (16.5%), 24 that it was much better (20.9%), 63 that there was no change (54.8%), and 9 that it was much worse (7.8%). The distributions of ΔMTQ scores in the four self-reported clinical impression groups (F = 11.47, p < 0.001) are illustrated in Fig. 1, including the median value and 5th–95th percentile.
MCIDs determined via the anchor-based method
The correlation coefficients between the self-reported clinical impression and ΔMTQ (r1), and VAS score and MTQ score at baseline (r2) were calculated using the self-reported clinical impression and VAS score as the main anchors. The correlation coefficients were as follows: r1 = 0.453 (p < 0.001) and r2 = 0.619 (p < 0.001).
According to the change in self-reported clinical impression, 24 patients reported improvement and 9 reported deterioration; for these changes, the MCID values were 22.75 and 3.63, respectively. Twenty-eight patients changed one point on the VAS, and 65 patients changed at least one point on the VAS; their MCID values were 9.39 and 25.50, respectively. The mean and SD of the difference between the scores of MTQ under the two anchors were calculated, and the mean of the difference was recorded as the MCID (Table 2).
The results of the MCID for the MTQ score according to the ROC analyses are summarized in Table 3. The cut-off point for deterioration based on self-reported impression of change was 13.5, which corresponded to an area under the ROC curve of 0.775.
MCIDs determined via distribution-based methods
Distribution-based methods are used to estimate the MCID based on the observed distribution of score changes [29]. The results of the MCID for the MTQ score are presented in Tables 4 and 5, which were calculated by three variation indexes on two subjective criteria: the ES, SEM, and RCI. When ES = 0.5, the MCID values for improvement, deterioration, and total change according to self-reported clinical impression were 8.21, 7.64, and 8.07, respectively, and those for the VAS score were 1.09, 7.64, and 6.29, respectively (Table 4). Similarly, the MCIDs calculated for the MTQ score when 1.96SEM was used as the intermediary index according to self-reported clinical impression were 8.52, 7.93, and 8.37, respectively, and those calculated according to the VAS score were 1.13, 7.93, and 6.53, respectively (Table 5). The MCIDs calculated for the total when 1.96RCI was used as the intermediary index according to self-reported clinical impression were 12.04, 11,21, and 11.83, respectively, and those calculated according to the VAS score were 1.60, 11.21, and 9.23, respectively (Table 5).
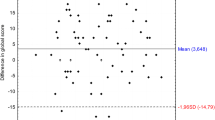
Results of various approaches combined
The MCIDs for the change in total MTQ ranged from 6.29 to 19.00, those for improvement from 1.09 to 22.75, and those for deterioration from 3.50 to 7.64 (Table 6 and Fig. 2).
Discussion
The MCID reflects the change in a score sufficient to indicate an impact of clinical treatment on a patient, and its primary function is to help clinical and research staff determine whether statistically significant score changes on a scale are clinically meaningful. In this study, we used both anchor-based and distribution-based methods to analyze the MCID of the MTQ to determine the smallest score change that was both statistically and clinically significant.
Selection of anchors in the anchoring method
Through correlation analysis, we discovered that self-reported clinical impression and VAS scores correlated best with changes in MTQ scores (r > 0.6), while physician evaluations correlated poorly with changes in MTQ scores (r < 0.6). This may be because the MTQ is a patient self-assessment scale, similar to the VAS and different to physicians' evaluations. This result emphasizes that the MTQ score accurately reflects patients' tinnitus.
Determination of the MCID value
The VAS and self-reported clinical impression were selected as anchors for analysis, and the mean/median and ROC curve were used for analysis and calculation of the MCID, respectively. The distribution-based method is used to estimate the MCID based on the observed distribution of score changes. Different MCID values were calculated (Table 6). The next objective was to determine the clinically most appropriate MCID values from the many calculated MCID values. We did this by comparing the results obtained via several analysis methods. We tried to minimize the placebo effect (which has a prevalence of up to 40% in tinnitus treatment [30]) by selecting the maximum MCID value as cut-off.
Considering that self-reported clinical impression is a qualitative variable and the VAS score is a quantitative variable, the VAS score more closely correlates with MTQ score changes. The MCID value for MTQ score improvement (7.50) calculated with the VAS score as anchor was similar to the MCID value for deterioration (7.64). Therefore, we decided to use the MCID value calculated with the VAS score as anchor. After treatment, the MTQ score of patients with tinnitus decreased by 7.5 or more than that before treatment. This result suggests that the treatment is effective in resolving or ameliorating tinnitus. Similarly, when the MTQ score increased by 7.5 or more compared with pretreatment, the patient’s tinnitus was considered aggravated.
In their 2012 MCID study on the TQ, Adamchic et al. [20] determined an MCID of − 5 and + 1 for the TQ, by using the Clinical Global Impression score as the ROC method in the anchoring method for calculation, taking response bias into account. In their 2018 study of the MCID for the German version of the TQ, Hall et al. [21] suggested a median of 12 as the MCID value, considering measurement bias and error. Therefore, we selected two subjective indicators with good correlations as anchors for the analysis and used the VAS score calculated based on the results as anchor.
A major limitation of this study was the following. For patients with tinnitus whose initial MTQ score was less than 7.5, we could not judge whether the treatment they received was effective in terms of the MCID. However, according to our previous study, a score of less than 21 on the MTQ is considered to indicate no problem with tinnitus [17]. When the initial score of the patient is less than 7.5, we believe that tinnitus has little impact on their quality of life. The next step is to expand the sample size in future studies to verify the adaptability of the MTQ in terms of treatment-related changes.
Conclusion
The change in MTQ score can be used as a clinical index to quantify the efficacy of tinnitus treatment and can be put into use in domestic studies related to tinnitus interventions, but physicians need to use it in conjunction with the severity of tinnitus experienced by the patient. The selected MCID for the MTQ score was an absolute value of 7.5. An increase in MTQ score more than 7.5 was considered aggravation of tinnitus, and a decrease in MTQ score more than 7.5 was considered a reduction in tinnitus.
The MCID of the MTQ score can guide the design of personalized clinical treatment plans for patients with tinnitus. The MTQ has been tested for reliability and validity and used for classification of tinnitus severity. Our results may assist in the development of relevant tinnitus questionnaires and guide their clinical use in China.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ES:
-
Effect size
- MCID:
-
Minimal clinically important difference
- MTQ:
-
Mandarin Tinnitus Questionnaire
- RCI:
-
Reliability change index
- ROC:
-
Receiver operating characteristic
- SEM:
-
Standard error of measurement
- TEQ:
-
Tinnitus evaluation questionnaire
- THI:
-
Tinnitus handicap inventory
- THI-CM:
-
Mandarin Chinese tinnitus handicap inventory
- THQ:
-
Tinnitus handicap questionnaire
- TQ:
-
Tinnitus questionnaire
- TRQ:
-
Tinnitus reaction questionnaire
- VAS:
-
Visual analogue scale
References
Jarach CM, Lugo A, Scala M, van den Brandt PA, Cederroth CR, Odone A, et al. Global prevalence and incidence of tinnitus: a systematic review and meta-analysis. JAMA Neurol. 2022;79:888–900.
Meng Z, Tao Y, Xu K, Li G, Zheng Y. Introduction of Mandarin version of the Tinnitus Questionnaire. J Audiol Speech Pathol. 2019;27:72–6.
Hall DA, Fackrell K, Li AB, Thavayogan R, Smith S, Kennedy V, et al. A narrative synthesis of research evidence for tinnitus-related complaints as reported by patients and their significant others. Health Qual Life Outcomes. 2018;16:61.
Bhatt JM, Bhattacharyya N, Lin HW. Relationships between tinnitus and the prevalence of anxiety and depression. Laryngoscope. 2017;127:466–9.
Sullivan MD, Katon W, Dobie R, Sakai C, Russo J, Harrop-Griffiths J. Disabling tinnitus. Association with affective disorder. Gen Hosp Psychiatry. 1988;10:285–91.
Schecklmann M, Pregler M, Kreuzer PM, Poeppl TB, Lehner A, Crönlein T, et al. Psychophysiological associations between chronic tinnitus and sleep: a cross validation of Tinnitus and Insomnia Questionnaires. Biomed Res Int. 2015;2015:461090.
Henry JA, Meikle MB. Psychoacoustic measures of tinnitus. J Am Acad Audiol. 2000;11:138–55.
Pinto PCL, Marcelos CM, Mezzasalma MA, Osterne FJV, de Melo Tavares de Lima MA, Nardi AE. Tinnitus and its association with psychiatric disorders: systematic review. J Laryngol Otol. 2014;128:660–4.
Henry JA. “Measurement” of Tinnitus. Otol Neurotol. 2016;37:e276-285.
Milerová J, Anders M, Dvořák T, Sand PG, Königer S, Langguth B. The influence of psychological factors on tinnitus severity. Gen Hosp Psychiatry. 2013;35:412–6.
Hall DA, Haider H, Szczepek AJ, Lau P, Rabau S, Jones-Diette J, et al. Systematic review of outcome domains and instruments used in clinical trials of tinnitus treatments in adults. Trials. 2016;17:270.
Hallam RS. Manual of the Tinnitus Questionnaire (TQ). London: Psychological Corporation; 1996
Meng Z, Chen Z, Xu K, Li G, Tao Y, Kwong JS-W. Psychometric properties of a Mandarin version of the tinnitus questionnaire. Int J Audiol. 2016;55:366–74.
Hiller W, Goebel G, Rief W. Reliability of self-rated tinnitus distress and association with psychological symptom patterns. Br J Clin Psychol. 1994;33:231–9.
Kam ACS, Cheung APP, Chan PYB, Leung EKS, Wong TKC, Tong MCF, et al. Psychometric properties of a Chinese (Cantonese) version of the Tinnitus Questionnaire. Int J Audiol. 2009;48:568–75.
Meeus O, Blaivie C, Van de Heyning P. Validation of the Dutch and the French version of the Tinnitus Questionnaire. B-ENT. 2007;3(Suppl 7):11–7.
Meng Z, Zhao F, Chen Z, Zheng Y. Categorization of tinnitus severity for the Mandarin Tinnitus Questionnaire. Ear Nose Throat J. 2021;100:NP33–8.
King MT. A point of minimal important difference (MID): a critique of terminology and methods. Expert Rev Pharmacoecon Outcomes Res. 2011;11:171–84.
Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–15.
Adamchic I, Tass PA, Langguth B, Hauptmann C, Koller M, Schecklmann M, et al. Linking the Tinnitus Questionnaire and the subjective clinical global impression: which differences are clinically important? Health Qual Life Outcomes. 2012;10:79.
Hall DA, Mehta RL, Argstatter H. Interpreting the Tinnitus Questionnaire (German version): what individual differences are clinically important? Int J Audiol. 2018;57:553–7.
Revicki D, Hays RD, Cella D, Sloan J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol. 2008;61:102–9.
Funk GF, Karnell LH, Smith RB, Christensen AJ. Clinical significance of health status assessment measures in head and neck cancer: what do quality-of-life scores mean? Arch Otolaryngol Head Neck Surg. 2004;130:825–9.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Lawrence Erlbaum Associates; 1988.
Samsa G, Edelman D, Rothman ML, Williams GR, Lipscomb J, Matchar D. Determining clinically important differences in health status measures: a general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics. 1999;15:141–55.
Crosby RD, Kolotkin RL, Williams GR. Defining clinically meaningful change in health-related quality of life. J Clin Epidemiol. 2003;56:395–407.
Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59:12–9.
Beaton DE, Bombardier C, Katz JN, Wright JG. A taxonomy for responsiveness. J Clin Epidemiol. 2001;54:1204–17.
Li F, Liu Y, Wan C, Zhou J, Tan J, Chen H. Establishing minimal clinically important differences for the quality of life instrument in patients with breast cancer QLICP-BR (V2.0) based on anchor-based and distribution-based methods. Front Oncol. 2022;12:753729.
Duckert LG, Rees TS. Placebo effect in tinnitus management. Otolaryngol Head Neck Surg. 1984;92:697–9.
Acknowledgements
The authors gratefully acknowledge Prof. Guanjian Liu at the Chinese Evidence-Based Medicine/Cochrane Center for excellent support with research design and statistical analysis.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Sichuan Province Health Department (130100).
Author information
Authors and Affiliations
Contributions
HG: Concept, design, literature search, and manuscript editing. CD: Data analysis, statistical analysis, and manuscript editing. JT, BY, JJ and MZ: Data acquisition. ZM: Supervision and manuscript review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Biomedical Research Ethics Committee of West China Hospital (No. 2020 [311]). All participants voluntarily signed an informed consent form for participation in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gu, H., Diao, C., Tang, J. et al. Minimal clinically important difference for the Mandarin version of the Tinnitus Questionnaire determined via anchor-based and distribution-based methods. Health Qual Life Outcomes 20, 157 (2022). https://doi.org/10.1186/s12955-022-02072-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-022-02072-z