Abstract
Background and purpose
Psoriasis (PS) is difficult to cure with a high incidence. Therefore, the quality of life (QOL) of people with Psoriasis has caused widespread concern. Universal scales respond poorly to subtle changes caused by specific diseases, which makes it challenging to fully understand the impact of QOL in patients with psoriasis. In view of the deficiencies of the universal scale and the lack of a specific scale suitable for Chinese cultural background, this study aims to develop the psoriasis scale among the system of QOL instruments for chronic diseases QLICD-PS (V2.0).
Methods
The scale QLICD-PS (V2.0) was developed based on the procedural decision-making approach and the experience of establishing scales at home and abroad. 122 patients with psoriasis were participated in measuring QOL 3 times before and after treatments. The reliability was assessed by test–retest reliability (Pearson’s correlation coefficients) and also internal consistency (Cronbach’s alpha coefficients). Qualitative analysis was adopted to evaluate content validity; item-domain correlation analysis, multi-dimensional scaling analysis, and factor analysis were adopted to evaluate the construct validity; the SF-36 scale was used as the criterion to evaluate the criterion-related validity due to lack of gold standard. Paired t tests were performed to evaluate the responsiveness on each domain/facet as well as the total of the scale, with Standardized Response Mean (SRM) being calculated.
Results
The QLICD-PS was composed of the general module including 3 domains (28 items) and the psoriasis specific module (13 items). The Cronbach's α of the specific module, the general module and the total scale of the QLICD-PS was 0.78, 0.87 and 0.74 respectively, the split-half reliability of the specific module, the general module and the total scale was 0.81, 0.91 and 0.81, respectively, both indicating high reliability. Correlation and factor analysis confirmed good construct validity and criterion-related validity. After treatments, the score changes in the total scale were statistically significant with SRM being 0.5, showing moderate responsiveness.
Conclusion
As the first psoriasis-specific QOL scale developed by the modular approach in Chinese, the QLICD-PS showed good reliability, validity and responsiveness, and could be used to measure the QOL of Patients with psoriasis specifically and sufficiently.
Similar content being viewed by others
Background
Psoriasis (PS) is a common chronic inflammatory immune-mediated skin disease caused by the interaction of genetic and environmental factors, etc. The incidence varies from regions and populations, and is related to factors such as race, geographic location, and environment [1]. Foreign surveys showed the incidence is 2% [2]. The Chinese epidemiological survey in 1984 showed that the total prevalence rate was 0.123%, with the prevalence rate in the north being higher than that in the south [3]. Due to the acceleration of China's urbanization, environmental pollution, intensified social competition and other factors, the current prevalence rate has increased to 0.47% [4]. In recent years, studies have shown that psoriasis is mainly related to infection, heredity, immune dysfunction, and endocrine disorders [5]. The disease has the characteristics of repeated attacks, skin damage, and long-lasting itching. It is a typical chronic psychosomatic disease, which has different degrees of impact on quality of life (QOL) of patients [6, 7].
With the transformation of the biomedical model to the bio-psycho-social model, the purpose of medicine was not simply to extend the survival of patients; the QOL had received more and more attention [8]. In the medical field, extensive QOL research began in the late 1970s with the purpose of exploring the influence of disease conditions and therapeutic interventions of patients, and thus the concept of health-related quality of life (HRQOL) was proposed [8, 9]. The term of HRQOL is often used to indicate QOL from the perspective of health care or medical services people experience. The WHO QOL Study Group defines QOL (in fact HRQOL) as individuals’ experience of life conditions related to their life goals, expectations, standards, and concerns in different cultures and value systems [10]. Generally speaking, QOL in medical field usually imply to HRQOL for short. Hence, the term of QOL and HRQOL are interchangeable in this study.
Psoriasis could systematic affect patients' health on various aspects, and thus QOL is needed. The purpose of the treatment of psoriasis was not only to relieve the symptoms of the patient's disease, but more importantly, to help the patient's psychological adaptation and improve the QOL. Therefore, to explore the QOL of patients with psoriasis and related influencing factors became an important problem in the prevention and treatment of psoriasis.
Since the 1980s, there had been an increasing number of researches on the QOL of patients with psoriasis. At first stage, some generic instruments such as SF-36 [11, 12], WHOQOL-100 [13, 14] were widely used for evaluating QOL of psoriasis. And then some dermatology scale were commonly used to assessment QOL of psoriasis including skin index (skindex) [15, 16], dermatology QOL index (DLQI) [17, 18], Dermatology QOL Scale(DQOLS) [19]. However, the specificity and sensitivity of these instruments were not strong enough when used for specific disease for they do not capture the symptoms and side effects specific to psoriasis.
Consequently, several disease-specific QOL measures for psoriasis have been developed including Psoriasis Disability Index (PDI) [20, 21], the psoriasis life stress inventory (PLSI) [22, 23], Salfore Psoriasis Index (SPI) [24], Psoriasis QOL Questionnaire 12 (PQOL-12) [25, 26], Psoriasis QOL Index (PSORQOL) [27], Psoriasis Stigma Experience Questionnaire (FSQ) [28] and so on (see Table 1 in detail).
However, no scale for psoriasis has been developed based on the modular approach (a general/core module plus specific modules). Moreover, no Chinese version of any of these instruments is available for use in psoriasis patients in China. Compared with foreign countries, the development of Psoriasis scale in China started late. Considering cultural dependence of QOL, it was necessary to develop suitable psoriasis assessment scale under Chinese cultural background. Consequently, a few scales have been developed in China including QOL Scale for Psoriasis Patients Treated with TCM by Zhou [29], the Psoriasis QOL Scale compiled with the connotation of Chinese medicine by Wang [30], the PQOLS (Psoriasis QOL Scale for Chinese Patients) compiled by Chen et al. [31]. However, they also have not been developed based on the modular approach, and most of them only used in traditional Chinese medicine [29, 30].
To solve these problems, we developed a QOL system called QLICD (Quality of Life Instruments for Chronic Diseases), which included a general module (QLICD-GM) that could be used for various diseases and some disease-specific modules [32]. At present, the latest version of the system was QLICD (V2.0), which contained 32 chronic disease-specific scales [33], including QLICD-CG [34], QLICD-PT [35], etc. The research mainly developed the specific module for patients with psoriasis, and then combined it with the general module that had been developed to form the Psoriasis Scale (QLICD-PS V2.0) in the System. This article aimed to report the development and validation of this scale.
Methods
Development of the QLICD-PS
General principles and steps of developing the QLICD-PS
The psoriasis disease-specific module was completed through the efforts of two independent groups. The nominal group consisted of 16 people, including 6 doctors, 2 nurses, 1 medical educator, and 7 teachers/researchers (2 QOL researcher, 2 psychologists, 2 sociologists, and 1 epidemiologist), which proposed the item pool using programmatic decision-making method. The focus group was composed of 10 experts, including 4 doctors, 1 medical educator and 5 teachers/researchers (2 QOL research scholars, 1 epidemiologist, 1 sociologist, and 1 psychologist), which proposed the conceptual framework using programmatic decision-making method and selects items proposed by the nominal group. In general, the nominal group was mainly responsible for reviewing the literature, referring to existed QOL scales for psoriasis patients and combining the clinical symptoms of psoriasis to propose items. The focus group was more specialized and refined, and was mainly responsible for screening, discussing and revising the items proposed by the nominal group. In the item selection process, both qualitative analysis methods such as group discussions, in-depth interviews as well as quantitative statistical methods such as variation analysis, correlation analysis, and factor analysis were used. Through a series of screening of the items, we had determined the specific module of the psoriasis scale, which were kept to 13 items (coded as PS1-PS13) and divided into 3 facets. It formed the QLICD-PS with the developed general module (QLICD-GM) (See Fig. 1 in detail).
Development of the QLICD-GM
The development of the QLICD-GM strictly followed the internationally recognized method of programmatic decision-making [32], and mainly included the following steps:(1) Establish a scale research team; (2) Define and decompose QOL measurement concepts to form a theoretical framework; (3) Propose a pool of candidate items; (4) Screen items to form a preliminary scale; (5) Screen pre-survey items to form a test scale; (6) Re-screen test surveys and items; (7) Evaluate the scale; (8) Form the formal scale. In the end, the QLICD-GM of 28 items was developed including 3 domains of physical function (9 items), mental function (11 items) and social function (8 items), which can be classified into 9 facets.
Creating the specific module of psoriasis
Using a similar procedure as described above, based on literature review, nominal group/focus group discussions, and patient interviews, we selected 20 items from the 40 item pool of the psoriasis-specific module. After pre-investigation and two stage screenings, the final module of 13 items (coded as PS1-PS13) was developed including 3 facets of specific symptoms (SPS), treatment side effects (TSE), and psychosocial impact of psoriasis (PSI) (Fig. 1).
Validation of the QLICD-PS
Data collection
A combination of the general module QLICD-GM and the newly developed psoriasis specific module was used to form the QLICD-PS. It was used for on-site investigation and evaluation of patients with psoriasis. The survey was conducted in the Dermatology Department of the First Affiliated Hospital of Zhengzhou University in China. The research objects were psoriasis patients with certain reading comprehension ability and ability to fill out the questionnaire independently. The investigators (doctors, nurses and medical graduate students) explained the purpose and significance of the study to the patients, and obtained the informed consent of the patients who agreed to participate in the study. The research protocol and informed consent form were approved by the ethics committee of the survey institution.
Each patient (n = 122) completed the first questionnaire before receiving treatment as the first round of assessment. After 1–2 days of treatments, the respondents (n = 110) participated in the second round of assessment. After 1 week of treatments, a total of 122 patients participated in the third round of assessment for responsiveness. Due to the lack of a recognized gold standard, we used the Chinese version of the SF-36 to collect data so as to evaluate the criterion-related validity of QLICD-PS.
The scoring method of the QLICD-PS
Each item of QLICD-PS was scored in a five-level Likert scoring system, that is, none, a little, average, fairly and very. Forward entries were scored from 1 to 5, while reverse entries were scored from 5 to 1. By adding up the domain/facet item scores, we obtained the raw scores of facet and domain. The total score of the scale was the sum of the scores in all domains. For comparison, the following equation was used to linearly convert all domain scores into standardized scores (SS) between 0 and 100: SS = (RS-Min) × 100/R, where RS, Min, and R represented the original score, the lowest score and score range (Table 2).
Based on scores, we completed the assessment of QLICD-PS from the perspectives of reliability (internal consistence and test–retest reliability), validity (construct validity, content validity, and criterion-related validity) and responsiveness.
Internal consistency (reliability)
This study evaluated the reliability of the scale from two aspects: internal consistent reliability and test–retest reliability. Cronbach’s alpha coefficient is common practice in scale development to evaluate the internal consistency of reliability, with coefficient between 0.70 and 0.95 being regarded as evidence of sufficient internal consistency [36]. Sehunemann [37] proposed that the test–retest reliability between 0.73and 0.95 was adequate. To assess internal consistency, Cronbach’s alpha coefficient and test–retest reliability was calculated separately for each domain/facet.
Content validity
The content validity refers to whether the designed item/scale could represent the content or topic to be measured. Qualitative analysis including by discussions of the nominal group and the focus group was adopted to evaluate content validity.
Construct validity
Item-domain correlation analysis and exploratory factor analysis were used to evaluate the construct validity of the scale in this study. We performed Pearson’s correlation coefficient r among items and domains with 0.40 or greater as the threshold [8, 36, 38]. We performed Exploratory factor analysis based on the eigenvalues > 1 criterion to examine the coincidence between components extracted from data and theoretical construct of the instrument, and to display and confirm the construct validity clearly by Varimax rotation with factor loadings greater 0.50 as criterion [8, 38]. Multi-trait scaling analysis (Pearson’s correlation analysis in fact) [36] was employed to test item convergent validity and discriminant validity, with the following criteria: convergent validity is supported when an item-domain correlation is greater 0.40; and discriminant validity is revealed when item-domain correlation is higher than that with other domains.
Criterion-related validity
This study used the SF-36 as the Criterion to confirm criterion-related validity. The SF-36 includes eight subscales (domains): Physical Function (PF), Role-Physical (RP), Bodily Pain (BP), General Health (GH), Vitality (VT), Social Function (SF), Role-Emotional (RE) and Mental Health (MH). We calculated Pearson’s correlation coefficients between the similar domains of QLICD-PT and SF-36 to evaluate criterion-related validity.
Responsiveness
Responsiveness referred to the ability of the scale to detect small clinically important changes over time [39, 40]. This study mainly calculated the average scores of each domain/facet of the QLICD-PS at the first and third assessments (before and after treatments). The paired t test was used to evaluate responsiveness with calculating the standard responsiveness mean (SRM). The SRM was the ratio (absolute value) of the difference before and after treatment to the standard deviation of the difference. Husted [40] suggested that SRM above 0.8 indicated a very good responsiveness, SRM around 0.5 indicated a moderate responsiveness, and SRM around 0.2 indicated a low responsiveness.
Results
Socio-demographic characteristics of the sample
The age of 122 patients with psoriasis ranged from 21 to 57 years old, with an average age of 39.73 years. 78 cases (63.9%) were male and 117 cases (95.9%) were Han nationality. Most participants were married (84 cases, 68.9%) and 29 cases (23.8%) were widowed. In terms of educational level, 14 participants were graduated from primary school (11.5%), 43 graduated from secondary school (35.2%), 47 graduated from high school or technical secondary school (38.5%), and 18 graduated from college or university (14.8%). Among them, 45 were farmers (36.9), 34 were workers (27.9%), 3 were teachers (2.5%), and 5 were cadres (4.1%). Most of the forms of medical insurance were cooperative medical care (n = 57, 46.7%).
Internal consistency (reliability)
The Cronbach's α of each domain of the QLICD-PS was between 0.59 and 0.87. The Cronbach's α of the specific module, the general module and the total scale were 0.78, 0.87 and 0.74, respectively. The split-half reliability of each domain of the QLICD-PS was between 0.73 and 0.91. The split-half reliability of the specific module, the general module and the total scale were 0.81, 0.91 and 0.81, respectively. Both of these results showed good internal consistency reliability (see Table 3 in detail).
Test–retest reliability
Correlation analysis and paired t-tests were performed on various domains/facets, and the results showed that the differences of physical function, psychological function, social function and the general module as well as the total scale in the first and second evaluations were not statistically significant (P > 0.05). At the same time, the correlation analysis results showed that there was a significant correlation in each domain/facet (P < 0.001), with correlation coefficients being between 0.84 and 0.94. The test–retest reliability coefficient of the specific module and the total scale was 0.85 and 0.94, respectively. These results indicated that the QLICD-PS scale had good test–retest reliability (See Table 4 in detail).
Content validity
After repeated discussions by the nominal group and the focus group, the QLICD-PS was compiled according to a strict procedural method, with items including all the dimensions and assessment content. The scale included physical, psychological, social and clinical symptoms of patients with psoriasis, side effects of treatment, and special psychological characteristics of the disease. It fully reflected the connotation of the QOL of patients with psoriasis, indicating good content validity.
Construct validity
Correlation analyses displayed that there were sufficiently associations between items and their own domains/facets (most correlation coefficients are greater than 0.5), but weak associations between items across domains/facets and between domains/facets (Table 5). For example, correlation coefficients between items of GPH1–GPH9 (in bold) are greater than those across domains.
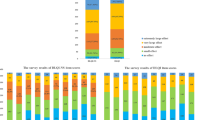
The Kaiser–Meyer–Olkin value of the specific module was 0.747, and Bartlett’s Tests of Sphericity was statistically significant (P < 0.005), supporting suitability of factor analysis. The factor analysis extracted 3 principal components from the 13 items of the specific module with the cumulative variance of 58.157%, reflecting 3 facets of this module (Table 6). The contribution rates of the first, second and third principal components were 24.793%, 17.690% and 15.674% respectively (Fig. 2).
By using the Varimax rotation method, it can be seen clearly that the 3 principal components reflected 3 different facets of the specific module. The first component represented the facet of Psychosocial impact with higher factor loadings on PS9 (0.71), PS10 (0.72), PS11 (0.84), PS12 (0.64) and PS13 (0.78); the second component reflected mainly treatment side effects with higher factor loadings on PS3 (0.63), PS4(0.70), PS5(0.61), PS7(0.65) and PS8(0.61); the third component mainly represented the specific symptoms with higher factor loadings on PS1(0.83) and PS2(0.58).
The above analysis results confirmed the theoretical construct, showing good construct validity.
Criterion-related validity
Correlation coefficients among the domain scores of the QLICD-PS and SF-36 were expressed in the Table 7, showing that the correlations between the same and similar domains are generally greater than those between different and non-similar domains. For example, the coefficient between the physical of QLICD-PS and physical function of SF-36 was 0.64, greater than any other coefficients in this row. It was considered that the criterion-related validity of the QLICD-PS was good.
Responsiveness
The results in Table 8 showed that all domains of the scale were statistically significant (P < 0.05). SRM in various domains ranged from 0.12 to 0.58, with that of the specific module and the total scale being 0.58 and 0.51, respectively. It could be seen that the responsiveness of the QLICD-PS was moderate (Table 8).
Discussions
Thoughts and characteristics of scale development
Based on the first version of QLICD-GM, the second version of QLICD-GM has made several improvements to increase the comprehensibility and accessibility [35]. By combining the improved general module QLICD-GM and the developed specific module for psoriasis, we developed a new QOL assessment scale for patients with psoriasis. The development process screened and modified the proposed item pool according to a rigorous procedural method, with 13 items being remained to form the final specific module. This modular approach unifies all disease-specific instruments of QLICDs under the same general module. Therefore, we can use QLICD-GM to capture general QOL in patients with different diseases, and then employ disease-specific modules such as QLICD-PT for pulmonary tuberculosis and QLICD-CG for Chronic Gastritis to catch the aspects of QOL that differentiate the different diseases. Therefore, the QLICD-PS is different from other QOL instruments for psoriasis.
Evaluation of QLICD-PS
Generally speaking, a practical QOL should be verified in at least three aspects: reliability, validity and responsiveness [32, 35]. In this study, the internal consistent reliability, the split-half reliability and the test–retest reliability were used to evaluate reliability of the QLICD-PS, with the results showing good reliability. Correlation analyses, multi-trait scaling analysis and factor analysis were employed to display validity, with the results confirming good validity on the whole.
The responsiveness results of the scale in this study showed that SRM ranged from 0.12 to 0.58, among which the SRM in the domains of mental function and social function were low (0.27 and 0.12 respectively). It might be because psoriasis was a chronic itchy skin disease, and its recurring characteristics had a profound impact on the QOL of patients, especially in terms of psychological and social functions which were difficult to be improved during a short hospital stay. It implies that psychological and social functions were not sensitive to short-term treatments. According to the evaluation criteria of responsiveness, SRM of the specific module and the total scale (0.51 and 0.54) could be rated as moderate responsiveness. Most probably, psoriasis was a chronic skin disease and the patient's hospital stay was short, the specific module was not expected to change significantly before and after treatments in a short period of time.
In China, although some scales were developed based on Chinese culture and demonstrated acceptable psychometric properties [29,30,31], there were still some shortcomings. Firstly, these scales were not systematically developed by the modular approach (combination of the general module and specific modules), and thus cannot be used to compare different diseases. Second, these scales lacked a unified standard, and the measurement method needed to be improved. Moreover, they did not involve the impact of drug side effects on patients enough, and most of them only used in traditional Chinese medicine [29, 30]. The PQOLS can be used in patients treated in Western medicine, but only has 4 items on symptoms of the disease and no item on side effects of the drug [31]. Therefore, it was necessary to develop a scientific, reasonable, reliable and suitable QOL measurement scale for Chinese psoriasis patients. In this study, a combination of the general module of recognized and well-developed system of QOL instruments for chronic diseases (QLICD) with the newly developed psoriasis specific module was used to form QLICD-PS. Compared with other scales in China, the QLICD-PS not only has good validity, reliability and responsiveness, but also can compare QOL across diseases by the general module, demonstrating both generic and specific properties. Moreover, it has a significant advantage that it consists of a moderate number of items with a clear hierarchical structure (items → facets → domains → overall) so that analysis of scores can be carried out not only at the domain and the overall levels but also at the different facet levels (12 facets in all) to detect changes in detail.
Strengths and limitations
Using the method of combining the general module of chronic diseases and the specific modules of diseases, the QOL assessment scale for psoriasis patients with Chinese cultural background was developed. Of course, this study was also subject to various restrictions. First, the sample size of the study was not very large for psoriasis is a skin disease with seasonal and regional characteristics, and the acquisition of samples was restricted by many unchangeable conditions such as seasons and regions. Furthermore, patients with psoriasis participated were limited to individuals who were able to read and understand the questionnaire in Chinese, the level of cultural proficiency should be carefully evaluated when translate QLICD-PS into other languages.
Conclusions
The QLICD-PS was developed under the Chinese cultural background by combining the recognized general module of chronic diseases and the specific module of psoriasis with several advantages. The QLICD-PS had good validity, reliability and responsiveness, and can be used to measure the QOL of Chinese patients with psoriasis.
Availability of data and materials
Please contact the authors for data requests.
References
Farber EM, Nail L. Epidemiology: natural history and genetics. In: Roenigk HR, Maibach HI, editors. Psoriasis. 3rd ed. New York: Marcel Dekker; 1998. p. 107–57.
Raychaudhuri S, Farber E. The prevalence of psoriasis in the world. J Eur Acad Dermatol Venereol. 2011;15(1):16–7. https://doi.org/10.1046/j.1468-3083.2001.00192.x.
Shao C, Zhang G, Bao Y, et al. National Psoriasis Epidemic Survey Report in 1984. Dermatol Venereol. 1989;01:60–72.
Ding X, Wang T, Shen Y, et al. Epidemiological survey of psoriasis in six provinces and cities in China. Chin J Dermatovenereol. 2010;24(07):598–601.
Zhang C. Factors affecting the quality of life of patients with psoriasis and nursing progress. Seek Med Ask Med. 2011;9(12):115–6.
He R, Qinxue Wu, Tian H, et al. Clinical research on integrated psychotherapy for psoriasis vulgaris. Pract Gener Med. 2008;02:131–2. https://doi.org/10.16766/j.cnki.issn.1674-4152.2008.02.073.
Chen J, Ren X. The effect of psychological intervention on the quality of life of patients with psoriasis. China J Leprosy Skin Diseases. 2007;23(4):315–6. https://doi.org/10.3969/j.issn.1009-1157.2007.04.018.
Hays RD, Anderson R, Revicki D, et al. Psychometric considerations in evaluating health-related quality of life measures. Qual Life Res. 1993;2(6):441–9. https://doi.org/10.1007/BF00422218.
Guyatt GH, Feeny DH, Patrick LD. Measuring health related quality of life. Ann Intern Med. 1993;118(8):622–9.
Bonomi AE, Patrick DL, Bushnell DM, Martin M. Validation of the United States’ version of the World Health Organization quality of life (WHOQOL) instrument. J Clin Epidemiol. 2000;53:1–12.
De Korte J, Mombers FM, Sprangers MA, et al. The suitability of quality-of-life questionnaires for psoriasis research: a systematic literature review. Arch Dermatol. 2002;138(9):1221–7. https://doi.org/10.1001/archderm.138.9.1221.
Wang Z, Zhang F. Research status of Quality of Life in patients with psoriasis. China J Leprosy Skin Diseases. 2007;07:601–3.
Skevington SM, Wright A. Changes in the quality of life of patients receiving antidepressant medication in primary care: validation of the WHOQOL-100. Br J Psychiatry. 2001;178(3):261–7. https://doi.org/10.1192/bjp.178.3.261.
The WHOQOL-SRPB Group. A cross-cultural study of spirituality, religion and personal beliefs as components of quality of life. Soc Sci Med. 2006;62(6):1486–97. https://doi.org/10.1016/j.socscimed.2005.08.001.
Nijsten TE, Sampoqna F, Chren MM, et al. Testing and reducing skindex-29 using Rasch analysis: skindex-17. Invest Dermatol. 2006;126(6):1244–50. https://doi.org/10.1038/sj.jid.5700212.
Tabolli S, Alessandroni L, Didona B, et al. A randomized controlled trial to evaluate short-term treatment with eosin vs. topical steroids in psoriasis. Clin Exp Dermatol. 2009;34(3):304–8. https://doi.org/10.1111/j.1365-2230.2008.02932.x.
Shikiar R, Bresnahan BW, Stone P, et al. Validity and reliability of patient reported outcomes used in Psoriasis: results from two randomized clinical trials. Health Qual Life Outcomes. 2003;8(1):53. https://doi.org/10.1186/1477-7525-1-53.
Basra MK, Fenech R, Gatt RM, et al. The Dermatology Quality of life Index 1994–2007: a comprehensive review of validation data and clinical results. Br J Dermatol. 2008;159(5):997–1035. https://doi.org/10.1111/j.1365-2133.2008.08832.x.
Yan XY, He GP. Research progress on the Quality of Life of patients with psoriasis. Pract Prevent Med. 2010;17(02):407–9.
Finlay AY. Quality of life measurement in dermatology: a practical guide. Br J Dermatol. 1997;136(3):305–14.
Lewis VJ, Finlay AY. Two decades experience of the Psoriasis Disability Index. Dermatology. 2005;210(4):261–8. https://doi.org/10.1159/000084748.
Krueger G, Koo J, Lebwohl M. The impact of psoriasis on quality of life: results of a 1998 National Psoriasis Foundation patient-membership survey. Arch Dermatol. 2001;137:280–4.
Gupta MA, Gupta AK. The psoriasis life stress inventory: a preliminary index of psoriasis-related stress. Acta Derm Venereol. 1995;75(3):240–3. https://doi.org/10.2340/0001555575240243.
Kirby B, Fortune DG, Bhushan M. The Salford Psoriasis Index: an holistic measure of psoriasis severity. Br J Dermatol. 2000;142(4):728–32. https://doi.org/10.1046/j.1365-2133.2000.03418.x.
Koo J, Kozma CM, Menter A. Development of a disease specific quality of life questionnaire: the 12-item Psoriasis Quality of Life Questionnaire (PQOL-12). Presented at the 61st Annual Meeting of the American Academy of Dermatology. San Francisco, March, 2003; 21–26.
Koo J, Menter A, Lebwohl M. The relationship between quality of life and disease severity: results from a large cohort of mild, moderate and severe psoriasis patients. Br J Dermatol. 2002;147:1077–9.
McKenna SP, Cook SA, Whalley D. Development of the PSORIQoL, a psoriasis-specific measure of quality of life designed for use in clinical practice and trials. Br J Dermatol. 2003;149(2):323–31. https://doi.org/10.1046/j.1365-2133.2003.05492.x.
Ginsburg IH, Link BG. Feelings of stigmatization in patients with psoriasis. J Am Acad Dermatol. 1989;20(1):53–63. https://doi.org/10.1016/s0190-9622(89)70007-4.
Zhou M. Preliminary establishment of the Life of Quality Scale for psoriasis patients treated with traditional Chinese Medicine. Guangzhou: Guangzhou University of Traditional Chinese Medicine; 2008. p. 3–4.
Wang C. Research on the establishment of a Quality of Life Scale for patients with psoriasis [dissertation]. Changsha: Hunan University of Traditional Chinese Medicine; 2006. p. 25–7.
Chen X, Cheng Y, Zhang M. Development and evaluation of Quality of Life Scale for patients with psoriasis in China. J Clin Dermatol. 2014;43(10):590–3. https://doi.org/10.16761/j.cnki.1000-4963.2014.10.012.
Wan C, Tu X, Messing S, et al. Development and validation of the general module of the system of quality of life instruments for chronic diseases and its comparison with SF-36. J Pain Symptom Manag. 2011;42:93–104. https://doi.org/10.1016/j.jpainsymman.2010.09.024.
Wan CH, Li XM, Yang Z, et al. Development and Applications of the system of Quality of Life Instruments for Chronic Diseases QLICD (in Chinese). China Sci Technol Achiev. 2019;20(17):26–8.
Quan P, Yu L, Yang Z, et al. Development and validation of Quality of Life instruments for chronic diseases-chronic gastritis version 2 (QLICD-CG V2.0). PLoS ONE. 2018;13(11):e0206280. https://doi.org/10.1371/journal.pone.0206280.
Sun Y, Yang Z, Wan C, Xu C, Chen L, Xu L, Zhang X, Yan F. Development and validation of the pulmonary tuberculosis scale of the system of Quality of Life Instruments for Chronic Diseases (QLICD-PT). Health Qual Life Outcomes. 2018;16(1):137. https://doi.org/10.1186/s12955-018-0960-5.
Hays RD, Hayashi T. Beyond internal consistency reliability: Rationale and use’s guide for multi-trait analysis program on the microcomputer. Behav Res Methods Instrum Compu. 1990;22:167–75.
Schunemann HJ, Sperati F, Barba M, et al. An instrument to assess quality of life in relation to nutrition: generation item reduction and initial validation. Health Qual Life Outcomes. 2010;8:26. https://doi.org/10.1186/1477-7525-8-26.
Wan C, Li H, Fan X, Yang R, Pan J, Chen W, Zhao R. Development and validation of the coronary heart disease scale under the system of quality of life instruments for chronic diseases QLICD-CHD: combinations of classical test theory and Generalizability Theory. Health Qual Life Outcomes. 2014;12:82. https://doi.org/10.1186/1477-7525-12-82.
Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. https://doi.org/10.1016/j.jclinepi.2006.03.012.
Husted JA, Cook RJ, Farewell VT, et al. Methods for assessing responsiveness: a critical review and recommendations. J Clin Epidemiol. 2000;53(5):459–68. https://doi.org/10.1016/s0895-4356(99)00206-1.
Acknowledgements
In carrying out this research project, we have received substantial assistance from the First Affiliated Hospital of Zhengzhou University and the Affiliated Hospital of Guangdong Medical University. We sincerely appreciate all the support we received.
Funding
This research was funded by the National Natural Science Foundation of China (Project Number: 71373058, 30860248).
Author information
Authors and Affiliations
Contributions
CW, JT, Qiongling Liu and Li Feng designed this study. Li Feng performed the data collection and data analysis. Li Feng drafted the manuscript. Qiongling Liu and Chonghua Wan and Li Feng revised the manuscript deeply. All authors contributed to interpreting the data. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research protocol was approved by the Institutional Review Board of the investigators’ institutions. The respondents were anonymous, voluntary and provided consent for participation.
Consent for publication
No individual’s personal data has been included.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Q., Feng, L., Wan, C. et al. Development and validation of the psoriasis scale among the system of quality of life instruments for chronic diseases QLICD-PS (V2.0). Health Qual Life Outcomes 20, 68 (2022). https://doi.org/10.1186/s12955-022-01970-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-022-01970-6