Abstract
Introduction
People who use drugs (PWUD) are at increased risk for HIV infection. HIV self-testing (HIVST) is a promising method for identifying new infections, but optimal distribution strategies remain understudied.
Methods
To characterize PWUD by HIVST distribution strategy (peers vs. mail), we examined data from July 2022 to June 2023 collected from a real-world HIVST program led by the non-profit, Florida Harm Reduction Collective. We used descriptive statistics and Poisson regressions with robust error variance to compare those who received HIVST through peers or via mail by socio-demographics, Ending the HIV Epidemic (EHE) county designation, and HIV testing experience.
Results
Among 728 participants, 78% received HIVST from peers, 47% identified as cisgender female, 48% as heterosexual, and 45% as non-White; 66% resided in an EHE county, and 55% had no HIV testing experience. Compared to those who received an HIV self-test from peers, those who received tests via mail were less likely to be cisgender male (vs. cisgender female; prevalence ratio [PR] = 0.59, 95% confidence interval [CI]: 0.43, 0.81), non-Hispanic Black (vs. non-Hispanic White; PR = 0.57, 95% CI: 0.36, 0.89) or from EHE counties (vs. non-EHE counties; PR = 0.33, 95% CI: 0.25, 0.44). Those who received tests via mail were also more likely to identify their sexual orientation as “Other/Undisclosed” (vs. straight/heterosexual; PR = 2.00, 95% CI: 1.51, 2.66).
Conclusion
Our findings support the role of community-based HIVST distribution strategies in increasing HIV testing coverage among PWUD. Additional research could help inform the equitable reach of HIVST.
Similar content being viewed by others
Introduction
People who use drugs (PWUD) that are unregulated, such as fentanyl and methamphetamine, and share syringes, are at elevated risk for HIV infection [1,2,3,4]. Fentanyl, in particular, has been linked to increased injection frequency among people who inject opioids, which can increase the risk of transmission in the event of receptive syringe re-use from someone living with unsuppressed HIV [5, 6]. Additionally, stimulant use is associated with heightened sexual risk-taking (e.g., condomless sex with multiple partners) that can increase exposure to HIV [7, 8]. This combination of injection- and sexual-related risk behaviors causes a duality of HIV risk for PWUD that highlights the need for prevention strategies that can disrupt both transmission routes within the social networks of PWUD [9].
HIV testing is a key intervention prioritized by the United States’ Ending the HIV Epidemic (EHE) Initiative (under the “Diagnose” pillar) [10]. However, HIV testing coverage among PWUD remains low due to multiple factors, including high levels of substance use stigma and difficulty accessing healthcare services in traditional settings [11,12,13]. HIV self-testing (HIVST) is an evidence-based strategy that can overcome barriers to traditional clinic-based HIV testing for at-risk communities, including men who have sex with men (MSM) and transgender individuals [14, 15]. Evaluation research has shown that specific HIVST distribution strategies, such as by peers or through the mail, can promote the reach of HIVST and effectively increase HIV testing uptake in communities disproportionately affected by HIV [16,17,18,19,20,21,22,23,24,25]. Although the provision of HIVST through community-based organizations (including syringe services programs; SSPs) is a promising, feasible, and acceptable strategy for increasing HIV testing among PWUD [26,27,28], little research has investigated how to best expand the reach of HIVST for PWUD, particularly to individuals who do not have access to brick-and-mortar harm reduction services. Furthermore, there is scant research comparing the reach of peer- and mail-based HIVST distribution strategies in other communities [15, 29], and none, to our knowledge, has been conducted among PWUD. In the context of an innovative, decentralized HIVST program for PWUD in Florida, we aimed to characterize the socio-demographics, EHE counties, and HIV testing experiences of PWUD reached by peer- and mail-based HIVST distribution.
Methods
Overview
This evaluation study used routine program operation data from a decentralized HIVST program implemented by the Florida Harm Reduction Collective (FLHRC) between July 2022 and June 2023. The FLHRC is a statewide, non-profit organization based in St. Petersburg that supports harm reduction organizations across Florida. At the direction of their community advisory board, the FLHRC implemented a statewide HIVST program to increase access to HIV testing among PWUD regardless of their route of substance administration (i.e., the program was not limited to people who inject drugs). The program distributed FDA-approved, over-the-counter rapid HIVST kits (the OraQuick At-Home HIV test; OraSure Technologies, Inc.), which can be easily administered in community-based settings such as SSPs [30, 31]. To promote access to HIVST, the program used peer- and mail-based distribution strategies, as described below.
Procedures
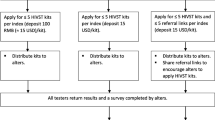
Peer-based distribution strategy
Approximately 10 peers with lived experience of substance use conducted outreach to distribute HIVST kits to PWUD in public parks, homeless encampments, and other venues where PWUD were known to spend time. However, the number of peers and venues varied between counties, and over time, as new peers were trained (or left), and people relocated or were involuntarily displaced by encampment sweeps [32]. Peers attended the Florida Department of Health’s 501/502 HIV training and were required to read and watch several training modules on HIV and the OraQuick At-Home HIV Test produced by the Centers for Disease Control and Prevention and OraSure Technologies Inc., respectively. Peers utilized engagement strategies, such as offering hygiene kits and condoms, to build trust and rapport with participants. If participants indicated an interest in HIVST, peers provided HIVST kits with informational postcards; acceptance of an HIVST kit was not required to receive engagement items. Participants could self-test immediately with the support of the peer distributor or take the kit with them to self-test later in private. If completed immediately, peers recorded test results and other relevant information (described below) using an anonymous HIPAA-compliant online survey delivered through a password-protected phone or laptop provided by the FLHRC (JotForm Inc., San Francisco, CA). Participants who chose to test later in private were given postcards with a QR code to an anonymous survey to report their results back to the FLHRC. Survey questions were consistent whether participants answered together with peers or in private.
Mail-based distribution strategy
The FLHRC also operates a robust mail-based naloxone distribution program that has been in operation since March 2022, which served as the primary marketing strategy for the mail-based HIVST kits. Postcards with information on how to order HIVST kits from the FLHRC were included in the naloxone kits. If participants chose to order HIVST kits, they could scan the QR code on the postcard or go directly to the FLHRC’s website to complete an anonymous survey (described below) and a separate form with mailing information for order fulfillment. In addition, the FLHRC collaborated with NEXT Distro, an online harm reduction organization that sends sterile syringes and other drug-use equipment, as well as naloxone, directly to PWUD [33, 34], where participants could access the link to FLRHC’s HIVST program.
Once order requests were received, the FLHRC sent an envelope packed with the following items: one HIVST kit; an informational postcard with a QR code to the FLHRC’s website; information on locally available resources participants could access depending on their test results (e.g., if non-reactive, information on HIV pre-exposure prophylaxis (PrEP) was provided); and another postcard with a QR code to a separate, optional anonymous survey to report their results back to the FLHRC. At the time of data collection, no contact information was collected on this optional follow-up survey for mail-based test recipients.
Survey measures
Our primary aim was to compare participants who received an HIVST kit from a trained peer to those who received a kit via mail. Characteristics of interest included gender identity, sexual orientation, race, ethnicity, EHE county designation, and prior HIV testing experience. In the survey, participants (or peers, depending on distribution strategy) could select from the following gender identities: cisfemale, cismale, transwoman, transman, non-binary, genderqueer, intersex, two-spirit, agender, pangender, intersex, questioning, other, unknown, and prefer not to answer, which were later categorized as “Cis-Female,” “Cis-Male,” and “Other/Undisclosed” (i.e., transwoman, transman, non-binary, genderqueer, intersex, two-spirit, agender, pangender, intersex, questioning, other, unknown, and prefer not to answer). Sexual orientation options included: straight/heterosexual, gay/lesbian, bi-sexual, polyamorous, queer, asexual, pansexual, questioning, other, unknown, and prefer not to answer, which were then categorized as “Straight/Heterosexual,” “Gay/Lesbian,” or “Other/Undisclosed” (i.e., bi-sexual, polyamorous, queer, asexual, pansexual, questioning, other, unknown, and prefer not to answer). For ethnicity, participants were asked if they identified as either “Hispanic” or “non-Hispanic.” For race, participants were asked if they identified as “Black,” “Latinx,” “Native American/Indigenous,” “Asian,” “Asian Subcontinent,” “White/Caucasian,” “Other,” or “Prefer not to answer.” For analysis purposes, ethnicity and race were combined into the following categories: “Non-Hispanic White,” “Non-Hispanic Black,” “Hispanic/Latinx,” and “Other/Undisclosed.” As designated by the Centers for Disease Control and Prevention (CDC), EHE counties in Florida include the following seven jurisdictions: Broward, Duval, Hillsborough, Miami-Dade, Orange, Palm Beach, and Pinellas [35]. All other Florida counties were considered non-EHE. Lastly, participants were asked to indicate whether they had any experience with HIV testing, which was dichotomized into “Yes” or “No,” with “Unsure” responses categorized as missing.
Statistical analysis
We calculated descriptive statistics to characterize our sample overall and by HIVST distribution strategy (peer- or mailed-based). To compare those reached by each HIVST strategy, we used Poisson regressions with robust error variances to model HIVST distribution strategy (peer- vs. mail-based) as a function of participants’ characteristics (i.e., socio-demographics, EHE county designation, and HIV testing experience). We fit separate Poisson regression models with robust error variances for each characteristic to obtain prevalence ratios (PRs) and corresponding 95% confidence intervals (CIs). All analyses were conducted using R version 4.1.2.
Results
Among 728 total participants who were surveyed, 570 (78%) received an HIVST kit from a peer and 158 (22%) received an HIVST kit via mail. About half of participants identified as cisgender female (47%) and straight/heterosexual (48%). Most were non-Hispanic White (55%) and from an EHE county (66%). Importantly, most had no prior HIV testing experience (55%) and did not return their HIVST result (73%; Table 1). No participants receiving mail-based kits completed the optional follow-up survey to report their results. Therefore, all returned HIVST test results were from participants who received peer-distributed tests, with approximately 5% of these tests reported as reactive.
Compared to those who received HIVST kits from peers, those who received tests via mail were less likely to be cisgender male (vs. cisgender female; PR = 0.59, 95% CI: 0.43, 0.81), non-Hispanic Black (vs. non-Hispanic White; PR = 0.57, 95% CI: 0.36, 0.89), or from an EHE county (vs. non-EHE county; PR = 0.33, 95% CI: 0.25, 0.44). Additionally, compared to those who received tests from peers, those who received tests via mail were more likely to identify their sexual orientation as “Other/Undisclosed” (vs. straight/heterosexual; PR = 2.00, 95% CI: 1.51, 2.66). HIV testing experiences did not differ between those who received tests from peers vs. mail (PR = 0.86, 95% CI: 0.64, 1.16).
Discussion
We evaluated the first, to our knowledge, real-world implementation of HIVST for PWUD. HIVST is a promising intervention for overcoming barriers to traditional, clinic-based HIV testing for PWUD at risk for HIV infection [1,2,3,4], and could be particularly beneficial for our study population given that over half of our sample reported never being tested for HIV in the past. However, research on HIVST among PWUD remains scarce, and effective strategies for supporting the equitable delivery of HIVST to this community are understudied. Our findings highlight notable differences in the communities reached through peer- and mail-based distribution strategies, carrying implications for future HIVST program implementation for PWUD.
As noted above, over half of participants in this study reported that their HIVST kit from the FLHRC was the first HIV test they had ever received, and most resided in EHE counties, where HIV transmission is highest in the nation [35]. HIVST programs have historically reached individuals who have never or infrequently tested before but represent other key communities (i.e., MSM, transgender people, and female sex workers) for HIV prevention [14, 15]. A systematic review that compared HIVST to standard clinic-based HIV testing strategies among MSM and transgender individuals showed that HIVST increased testing uptake by 1.5 times and increased the mean number of HIV tests conducted by an organization by 2.6-fold over follow-up [15]. To our knowledge, this is the first study to highlight similar increases in HIV testing utilization for PWUD. Our findings support the need for further investment in HIVST for PWUD and its integration within harm reduction organizations such as SSPs. While SSPs initially evolved to address HIV transmission among PWUD at the onset of the HIV/AIDS epidemic in the U.S [36], funding and demand for HIV prevention within SSPs has diminished over time [37,38,39]. However, isolated HIV outbreaks among PWUD now threaten efforts to end the HIV epidemic and highlight the need for the implementation of additional HIV prevention services, including HIVST, within harm reduction spaces [40, 41].
We found that a greater proportion of participants who received an HIVST kit via mail identified as cisgender female, non-Hispanic Black, reported their sexual orientation as “Other/Undisclosed,” and were from non-EHE counties. Mail-based distribution of HIVST may offer a higher degree of privacy and convenience than facility-based HIV testing and peer-based distribution of HIVST, which may be more appealing to cisgender females, people who identify as non-Hispanic Black, and individuals whose sexual identities are often stigmatized in traditional healthcare settings [42, 43]. Mail-based distribution of HIVST can, therefore, circumvent the need for PWUD to decide between HIV testing and facing discrimination. PWUD with these socio-demographic characteristics and from non-EHE counties might face additional barriers to accessing traditional healthcare settings because of geographical location, lack of transportation, or limited opportunities caused by structural disparities in access to care. Because HIV prevention resources are limited and targeted to EHE counties [10, 44], mail-based distribution of HIVST could provide a solution for PWUD at risk for HIV in non-EHE designations without the need for in-person HIV prevention infrastructure (e.g., Ryan White clinics). In Florida, all legal operational SSPs are in EHE jurisdictions and offer opt-out HIV testing, likely decreasing the need for HIVST in these communities [45].
One of the primary challenges encountered by HIVST programs is the effective management of returning test results to organizations providing the tests. In our sample, no participant who received an HIVST kit by mail returned their HIV test result. Based on the broader literature, we can assume that the HIV positivity rates for both peer- and mail-based delivery strategies are comparable [14, 15], suggesting that approximately 5% of mail-based test users in our sample could have had a reactive result. From a public health perspective, the return of HIV test results is desirable as it facilitates referrals to appropriate HIV-related clinical services (for treatment or prevention) and supports the cascade of contact tracing. Yet, this imperative for result return could potentially clash with the anonymity of HIVST. While the absence of any results here was somewhat unexpected, it aligns with findings from a meta-analysis of HIVST across various key communities for HIV prevention (e.g., MSM and female sex workers), which revealed that HIVST is associated with a 17% reduction in linkage to care compared to standard facility-based HIV testing [15]. These dynamics underscore the complex trade-offs between anonymity and the public health imperative to facilitate follow-up care and support for individuals with reactive test results, highlighting the need for innovative HIV prevention approaches that may involve a blend of peer-facilitated mail-delivery of HIVST.
Limitations
The implications of this work should be interpreted in the context of several limitations. First, our study considered a real-world HIVST program that was not implemented within a generalizable sample or location. Still, it provides an example of how an HIVST program for PWUD could function in other real-world settings. Similarly, the HIVST program was available to anyone accessing peer-based or online services offered by the FLRHC or NEXT Distro, meaning there were no strict eligibility criteria, and individuals who do not use drugs could have accessed the program. With that said, the FLHRC specifically trained peers to deliver services to PWUD, and NEXT Distro is a harm reduction organization known to serve this community. Moreover, there were no set schedules for outreach by trained peers across the FLHRC, which may have impacted the availability of services for specific communities. However, we do not anticipate this would have introduced differential bias by testing strategy. In addition, because the program was not created for research, our analyses could not include several characteristics that may also be associated with receipt of HIVST from a peer or via mail, such as housing status or income. Since the FLHRC’s HIVST program was anonymous there may be duplicates in our data, although the risk is low considering the timeframe of our assessment and the recommended frequency of HIV testing.
Conclusion
This study underscores the potential of HIVST to increase testing uptake among PWUD, especially individuals without prior HIV testing experience and living in non-EHE jurisdictions where HIV prevention resources may be scarce. To maximize its public health impact, HIVST programs should tailor distribution strategies and follow-up supports to the specific needs and preferences of different communities of PWUD. Ultimately, HIVST holds promise to improve HIV detection and prevention efforts among PWUD, contributing to the broader goal of reducing incident HIV infections and ending the HIV epidemic in the United States. However, future research is needed to advance the equitable reach of HIVST, especially among communities of PWUD.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- PWUD:
-
People Who Use Drugs
- HIV:
-
Human Immunodeficiency Virus
- EHE:
-
Ending the HIV Epidemic
- HIVST:
-
HIV self-testing
- SSP:
-
Syringe Services Program
- MSM:
-
Men Who Have Sex with Men
- FLHRC:
-
Florida Harm Reduction Collective
- FDA:
-
U.S. Food and Drug Administration
- PR:
-
Prevalence Ratio
- CI:
-
Confidence Interval
- AIDS:
-
Acquired Immunodeficiency Syndrome
References
Vorobjov S, Uusküla A, Des Jarlais DC, Abel-Ollo K, Talu A, Rüütel K. Multiple routes of drug administration and HIV risk among injecting drug users. J Subst Abuse Treat. 2012;42(4):413–20.
Centers for Disease Control and Prevention. HIV and Injection Drug Use. In: Division of HIV/AIDS Prevention, editor. 2021.
Edeza A, Bazzi A, Salhaney P, Biancarelli D, Childs E, Mimiaga MJ, et al. HIV Pre-exposure Prophylaxis for people who inject drugs: the context of co-occurring injection- and sexual-related HIV risk in the U.S. Northeast. Subst Use Misuse. 2020;55(4):525–33.
Linley L, Johnson AS, Song R, Hu S, Wu B, Hall HI et al. Estimated HIV incidence and prevalence in the United States 2010–2019. 2021.
Alpren C, Dawson EL, John B, Cranston K, Panneer N, Fukuda HD, et al. Opioid use fueling HIV Transmission in an urban setting: an outbreak of HIV infection among people who inject Drugs-Massachusetts, 2015–2018. Am J Public Health. 2020;110(1):37–44.
Lambdin BH, Bluthenthal RN, Zibbell JE, Wenger L, Simpson K, Kral AH. Associations between perceived illicit fentanyl use and infectious disease risks among people who inject drugs. Int J Drug Policy. 2019;74:299–304.
Shoptaw S, Reback CJ. Associations between methamphetamine use and HIV among men who have sex with men: a model for guiding public policy. J Urban Health. 2006;83(6):1151–7.
Reback CJ, Fletcher JB. Elevated HIV and STI prevalence and incidence among methamphetamine-using men who have sex with men in Los Angeles County. AIDS Educ Prev. 2018;30(4):350–6.
Reddon H, Marshall BDL, Milloy MJ. Elimination of HIV transmission through novel and established prevention strategies among people who inject drugs. Lancet HIV. 2019;6(2):e128–36.
Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV Epidemic: a plan for the United States. JAMA. 2019;321(9):844–5.
Biancarelli DL, Biello KB, Childs E, Drainoni M, Salhaney P, Edeza A, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–6.
Meyerson K, Hoddinott G, Nicholson T, Meehan SA. Underlying reasons why some people haven’t tested for HIV - a discourse analysis of qualitative data from Cape Town, South Africa. Sahara j. 2021;18(1):105–12.
Motavalli D, Taylor JL, Childs E, Valente PK, Salhaney P, Olson J, et al. Health is on the Back Burner: Multilevel barriers and facilitators to Primary Care among people who inject drugs. J Gen Intern Med. 2021;36(1):129–37.
Johnson CC, Kennedy C, Fonner V, Siegfried N, Figueroa C, Dalal S, et al. Examining the effects of HIV self-testing compared to standard HIV testing services: a systematic review and meta-analysis. J Int AIDS Soc. 2017;20(1):21594.
Witzel TC, Eshun-Wilson I, Jamil MS, Tilouche N, Figueroa C, Johnson CC, et al. Comparing the effects of HIV self-testing to standard HIV testing for key populations: a systematic review and meta-analysis. BMC Med. 2020;18(1):381.
Choko AT, Corbett EL, Stallard N, Maheswaran H, Lepine A, Johnson CC, et al. HIV self-testing alone or with additional interventions, including financial incentives, and linkage to care or prevention among male partners of antenatal care clinic attendees in Malawi: an adaptive multi-arm, multi-stage cluster randomised trial. PLoS Med. 2019;16(1):e1002719.
Choko AT, Fielding K, Johnson CC, Kumwenda MK, Chilongosi R, Baggaley RC, et al. Partner-delivered HIV self-test kits with and without financial incentives in antenatal care and index patients with HIV in Malawi: a three-arm, cluster-randomised controlled trial. Lancet Global Health. 2021;9(7):e977–88.
Fistonich GM, Troutman KM, Visconti AJ. A pilot of Mail-Out HIV and Sexually Transmitted Infection Testing in Washington, District of Columbia during the COVID-19 pandemic. Am J Prev Med. 2021;61(5 Suppl 1):S16–25.
Okoboi S, Lazarus O, Castelnuovo B, Nanfuka M, Kambugu A, Mujugira A, et al. Peer distribution of HIV self-test kits to men who have sex with men to identify undiagnosed HIV infection in Uganda: a pilot study. PLoS ONE. 2020;15(1):e0227741.
Eshun-Wilson I, Jamil MS, Witzel TC, Glidded DV, Johnson C, Le Trouneau N, et al. A systematic review and network Meta-analyses to assess the effectiveness of human immunodeficiency virus (HIV) self-testing distribution strategies. Clin Infect Dis. 2021;73(4):e1018–28.
Gichangi A, Wambua J, Mutwiwa S, Njogu R, Bazant E, Wamicwe J, et al. Impact of HIV Self-Test distribution to Male partners of ANC clients: results of a Randomized Controlled Trial in Kenya. J Acquir Immune Defic Syndr. 2018;79(4):467–73.
Masters SH, Agot K, Obonyo B, Napierala Mavedzenge S, Maman S, Thirumurthy H. Promoting Partner testing and couples testing through secondary distribution of HIV Self-Tests: a Randomized Clinical Trial. PLoS Med. 2016;13(11):e1002166.
Napierala S, Bair EF, Marcus N, Ochwal P, Maman S, Agot K, et al. Male partner testing and sexual behaviour following provision of multiple HIV self-tests to Kenyan women at higher risk of HIV infection in a cluster randomized trial. J Int AIDS Soc. 2020;23(Suppl 2):e25515–e.
Thirumurthy H, Bair EF, Ochwal P, Marcus N, Putt M, Maman S, et al. The effect of providing women sustained access to HIV self-tests on male partner testing, couples testing, and HIV incidence in Kenya: a cluster-randomised trial. Lancet HIV. 2021;8(12):e736–46.
Lightfoot MA, Campbell CK, Moss N, Treves-Kagan S, Agnew E, Kang Dufour M-S et al. Using a Social Network Strategy to distribute HIV Self-Test kits to African American and latino MSM. JAIDS J Acquir Immune Defic Syndr. 2018;79(1).
Delaney KP, DiNenno EA. HIV Testing Strategies for Health Departments to end the epidemic in the U.S. Am J Prev Med. 2021;61(5 Suppl 1):S6–15.
Peiper NC, Shamblen S, Gilbertson A, Guest G, Kopp M, Guy L, et al. Acceptability of a HIV self-testing program among people who use illicit drugs. Int J Drug Policy. 2022;103:103613.
Ballard AM, Haardöerfer R, Prood N, Mbagwu C, Cooper HLF, Young AM. Willingness to participate in At-Home HIV Testing among Young adults who use Opioids in Rural Appalachia. AIDS Behav. 2021;25(3):699–708.
Figueroa C, Johnson C, Verster A, Baggaley R. Attitudes and acceptability on HIV Self-Testing among Key populations: a Literature Review. AIDS Behav. 2015;19(11):1949–65.
U.S. Food and Drug Administration. OraQuick In-Home HIV Test. 2012.
Stekler DKMGJHCFJ, editor. Acceptability and Ease of Use of Home Self-Testing for HIV among Men Who Have Sex with Men. Conference on retroviruses and opportunistic infections (CROI 2012); 2012; Seattle, Washington.
Barocas JA, Nall SK, Axelrath S, Pladsen C, Boyer A, Kral AH, et al. Population-Level Health effects of Involuntary Displacement of people Experiencing Unsheltered Homelessness who inject drugs in US cities. JAMA. 2023;329(17):1478–86.
Distro NEXT. N.D. Available from: https://nextdistro.org/.
Yang C, Favaro J, Meacham MC. NEXT harm reduction: an online, mail-based naloxone distribution and harm-reduction program. Am J Public Health. 2021;111(4):667–71.
Centers for Disease Control and Prevention (CDC). Ending the HIV Epidemic in the U.S. (EHE) Jurisdictions. 2022.
Des Jarlais DC. Harm reduction in the USA: the research perspective and an archive to David Purchase. Harm Reduct J. 2017;14(1):51.
Broz D, Carnes N, Chapin-Bardales J, Des Jarlais DC, Handanagic S, Jones CM, et al. Syringe Services Programs’ role in ending the HIV Epidemic in the U.S.: why we cannot do it without them. Am J Prev Med. 2021;61(5 Suppl 1):S118–29.
Centers for disease Control and Prevention. Federal Funding for Syringe Services Programs. In: National Center for HIV VH, STD, and TB Prevention, editor. 2019.
Jones CM. Syringe services programs: an examination of legal, policy, and funding barriers in the midst of the evolving opioid crisis in the U.S. Int J Drug Policy. 2019;70:22–32.
Gonsalves GS, Crawford FW. Dynamics of the HIV outbreak and response in Scott County, IN, USA, 2011-15: a modelling study. Lancet HIV. 2018;5(10):e569–77.
Alves J, Stewart J, Ruiz-Mercado G, Taylor JL. When Perfect is the enemy of tested: a call to Scale Rapid HIV Testing for people who inject drugs. J Gen Intern Med. 2022;37(11):2851–2.
Rivenbark JG, Ichou M. Discrimination in healthcare as a barrier to care: experiences of socially disadvantaged populations in France from a nationally representative survey. BMC Public Health. 2020;20(1):31.
Ayhan CHB, Bilgin H, Uluman OT, Sukut O, Yilmaz S, Buzlu S. A systematic review of the discrimination against sexual and gender minority in Health Care settings. Int J Health Serv. 2020;50(1):44–61.
Centers for Disease Control and Prevention (CDC). Current and Past Funding for Ending the HIV Epidemic in the U.S. 2023.
Bartholomew TS, Tookes HE, Bullock C, Onugha J, Forrest DW, Feaster DJ. Examining risk behavior and syringe coverage among people who inject drugs accessing a syringe services program: a latent class analysis. Int J Drug Policy. 2020;78:102716.
Acknowledgements
We want to acknowledge and thank the Florida Department of Health for in-kind HIV self-testing kits and the NEXT Distro team for their support and operation of the mail-based platform. We would also like to thank the Florida Harm Reduction Collective’s Community Advisory Board for expressing the need for HIV self-testing kits.
Funding
This work was supported by funding from the National Institute on Drug Abuse (NIDA): T32DA023356 and R34DA058389; The Center for Disease Control and Prevention (CDC) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $199,113 with 100 percent funded by CDC/HHS. The contents are those of the authors and do not necessarily represent the official views of, nor endorsement by, CDC/HHS, NIDA, or the U.S. Government.
Author information
Authors and Affiliations
Contributions
Conceptualization, Methodology: WHE, TSB; Data validation and curation: WHE and AM; Data analysis: WHE and TSB; Original manuscript draft: WHE, AM, TSB, HET, ARB; Resources and project administration: TS, SM, TSB. All authors contributed to the interpretation of results, manuscript revisions, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was deemed exempt by the University of Miami Institutional Review Board (IRB).
Consent for publication
All participants consented to the collection of their information, and all authors have read the final draft of this manuscript and agreed to have it published.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Eger, W.H., Mutchler, A., Santamour, T. et al. Decentralized HIV testing: comparing peer and mail-based distribution strategies to improve the reach of HIV self-testing among people who use drugs in Florida. Harm Reduct J 21, 116 (2024). https://doi.org/10.1186/s12954-024-01031-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12954-024-01031-9