Abstract
It is reported that pulmonary fibrosis has become one of the major long-term complications of COVID-19, even in asymptomatic individuals. Currently, despite the best efforts of the global medical community, there are no treatments for COVID-induced pulmonary fibrosis. Recently, inhalable nanocarriers have received more attention due to their ability to improve the solubility of insoluble drugs, penetrate biological barriers of the lungs and target fibrotic tissues in the lungs. The inhalation route has many advantages as a non-invasive method of administration and the local delivery of anti-fibrosis agents to fibrotic tissues like direct to the lesion from the respiratory system, high delivery efficiency, low systemic toxicity, low therapeutic dose and more stable dosage forms. In addition, the lung has low biometabolic enzyme activity and no hepatic first-pass effect, so the drug is rapidly absorbed after pulmonary administration, which can significantly improve the bioavailability of the drug. This paper summary the pathogenesis and current treatment of pulmonary fibrosis and reviews various inhalable systems for drug delivery in the treatment of pulmonary fibrosis, including lipid-based nanocarriers, nanovesicles, polymeric nanocarriers, protein nanocarriers, nanosuspensions, nanoparticles, gold nanoparticles and hydrogel, which provides a theoretical basis for finding new strategies for the treatment of pulmonary fibrosis and clinical rational drug use.
Similar content being viewed by others
Introduction
Pulmonary fibrosis
Pulmonary fibrosis (PF) is a common, progressive, irreversible, fatal chronic pulmonary disease [1, 2] with a median survival of 2–4 years after diagnosis [3], which is characterized by excessive extracellular matrix deposition and scar in the lungs, resulting in functional failures, severe breathing problems and even death [4, 5]. It can be divided into secondary PF and idiopathic PF [6]. The relatively clear etiology and predisposing factors for PF are as follows: smoking, gastroesophageal reflux, genetic factors, some chemicals (e.g. organic or inorganic dust), some drugs (e.g. amiodarone and bleomycin), viral infections and some immune disorders (e.g. lupus erythematosus and scleroderma) [7] (Fig. 1).
Studies have concluded that the pathogenesis of PF is divided into three stages [7, 8]: (1) Injury: many factors can induce lung injuries, such as smoking, gastroesophageal reflux, genetic factors, some chemicals, some drugs, and viral infections. The destruction of epithelial and endothelial cells triggers the anti-fibrinolytic cascade reaction. Platelets are continuously activated, thrombin is enriched, and fibrin clots. (2) Alveolar inflammation: lung activated mesenchymal and infiltrating cells secrete transforming growth factor-β (TGF-β), tumor necrosis factor-α (TNF-α), chemotactic cytokines (CXC), and cell adhesion molecule (CAM). These cytokines promote an increase in inflammatory monoclonal factors. (3) Fibrosis with the excessive repair: fibroblast and myofibroblast activation, secretion of growth factors, interleukins (IL)-17A, and matrix metalloproteinases (MMPs), fibroblast growth factor receptor (FGFR), etc. Fibrosis occurs with the excessive repair of lung tissue and blood vessels, excessive proliferation of fibroblasts, and massive accumulation of extracellular matrix (Fig. 2). In late December 2019, COVID-19 outbroke and spread to several countries, resulting in a cumulative total of over 400 million confirmed cases, with the complications and sequelae of PF in critical and severe illnesses [8,9,10,11].
Treatments currently available of PF
However, there is a lack of effective clinical treatment to completely cure PF. Symptomatic treatment, such as the use of glucocorticoid and anti-infection therapy, is generally used. The prognosis of PF is unfavorable, which seriously threatens the life and health of human beings. In 2014, two anti-fibrotic drugs, pirfenidone and nintedanib, have been approved for use in humans by FDA [12], these drugs only can slow the decline of lung function but do not cure or reverse established fibrosis [13]. As a result, seeking a proper treatment for PF leads to a great deal of attention.
The latest international treatment guideline was presented by the Japanese Respiratory Society (JRS) in 2018, giving a conditional recommendation in PF treatments, containing pirfenidone combined with inhaled N-acetylcysteine therapy, inhaled N-acetylcysteine therapy, corticosteroid monotherapy, etc. (Fig. 3) [14]
Inhaled nano-based therapeutics for PF
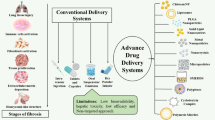
Notably, the long-term dosing and systemic administration of these drugs can cause serious side effects, such as diarrhea [15], nausea [16], vomiting [17] and rash/photosensitivity [18]. However, nano-based drug delivery systems can improve the solubility and bioavailability of anti-fibrotic drugs and immunotherapeutic agents, increase drug uptake by target cells, increase lung deposition rates, prolong the retention time in vivo and improve pharmacokinetic behavior, thereby significantly enhancing the therapeutic effect at low doses of anti-fibrotic drugs and reducing side effects [19, 20]. Inhalation nano-based drug delivery system as an emerging therapy offers a new way of treating PF, compared with traditional oral administration, inhalation administration can make the drug diffuse throughout the lung and promote bronchial relaxation. This kind of administration can greatly reduce the drug dosage, and the drug can reach the lung without passing through the blood circulation, with a high deposition rate in the lung.
Inhalation also has several meaningful advantages over injections, such as improved patient compliance, low therapeutic dose, safety, and treatment outcomes. Nano-based drug delivery system can wrap anti-fibrosis drugs in biocompatible materials. The nanomaterial shell has a protective effect, but also can effectively improve the stability of active ingredients and drugs. It has good biocompatibility and can improve bioavailability. After inhalation, the nanodrug first penetrates the lung barrier, and then accumulates to the target after endocytosis, and then releases the drug, and finally enters the blood circulation [21, 22]. This emerging delivery system can reduce the number of doses to achieve a sustained release therapeutic effect (Fig. 4A, Table 1).
A Series routes for the treatment of PF, including inhalation, intravenous, oral administration and lung transplantation. B Several biological barriers that need to be penetrated for inhaled nanomedicines to treat PF: the nanomedicines are inhaled and diffused into the alveoli, and then sequentially cross mucus, alveolar epithelial cells, interstitial tissues, capillary endothelial cells, plasma, and finally, reach the capillary red blood cells
On inhalation, the nanomedicines require the penetration of several physiological barriers: first inhaled and diffused into the alveoli, and then penetrate the mucus, alveolar epithelial cells, interstitial tissues, capillary endothelial cells, and plasma, and finally, reach the capillary red blood cells (Fig. 4B) [23, 24]. Unfortunately, little is known about the interaction of inhalation drug delivery with biological membrane, especially with extracellular polymeric substances (EPS) matrices [25], so there are still some safety issues with nano formulation, such as causing local inflammation and cytokine storms.
The challenges of inhalation drug delivery also has high demands on factors such as exposure time, dose, aggregation, concentration, particle size, surface area and charge are all closely related to nanotoxicity. The optimum particle size for inhalation is 100–500 nm (Fig. 5A), at around 100 nm, nanoparticles are more readily taken up by lung epithelial cells [26] and can be deposited in deep lung areas, particularly in alveolar structures near alveolar openings [27], if the mass median aerodynamic diameter (MMAD) of particles is less than or equal to approximately 500 nm, they are significantly deposited by diffusion based on Brownian motion [27], and if they exceed 500 nm, they are readily phagocytosed by macrophages and tend to be deposited in the alveolar lumen [27]. In addition, surface electrostatic charge is an important factor influencing the deposition of inhaled nanoparticles. Charged nanoparticles have a higher deposition efficiency compared to neutral charged nanoparticles [27].
A Comparison of optimal particle sizes for pulmonary inhalation drug delivery, e.g. lung retention time, lung tissue absorption, systemic exposure and pulmonary targeting efficiency, etc. [26]; B Charge selection for pulmonary inhalation drug delivery, e.g. cytocompatibility, lung retention time, systemic exposure and mucus penetration, etc. [28]
Zhao et al. [28] reported that negatively charged and neutral nanoparticles showed better lung cytocompatibility, higher cell viability and higher mucus permeability compared to positively charged nanoparticles (Fig. 5B). In contrast, cationic drug delivery systems typically showed cytotoxicity, which limited the dose administered [29].
It should not be ignored that inhaled nano-based drug delivery system has certain limitations, which requires high parameters such as particle shape, size and charge, so it has certain challenges in design. At the same time, changes in the physicochemical and structural properties of nanocarriers may be responsible for many material interactions, which may lead to toxicological effects [30], i.e. nanotoxicity, such as causing unwanted oxidative stress and cytotoxicity [31]. Efficient targeting of lung fibrotic cells and improving efficacy are key issues that need to be addressed by the new generation of inhaled nanoformulations. The above problems are the limitations of inhaled nanoformulations and need further research and improvement.
The review here presents the current application of inhaled nano-based therapeutics such as lipid-based nanocarriers, nanovesicles, polymeric nanocarriers, protein nanocarriers, nanosuspensions, nanoparticles, gold nanoparticles and hydrogel in the treatment and management of PF and future prospects of this emerging field (Fig. 6).
Lipid-based delivery system
Liposomes are one of the most successful inhalable nanocarriers among lipid matrix carriers. The hydrophilic drugs can be concentrated in the water core, while the hydrophobic drugs are mainly distributed in the lipid bilayer. Liposomes can improve intracellular uptake, prolong drug release, and reduce lung clearance rate. In addition, due to the biocompatibility and biodegradability of liposomes, there are nearly little local irritation and toxicological problems that occurs [37].
Liposomes
Liposomes are typically made from compounds that are structurally similar to those found in the lung, such as cholesterol and phospholipids [38]. This colloidal form includes self-assembled microvesicles consisting of an aqueous core surrounded by one or more lipid bilayers. Many studies have determined the high biodegradability and biocompatibility of liposome agents for drug delivery in the lungs [39]. Ivanova et al. [40] confirmed that liposome lung local delivery of prostaglandin E2 (PGE2), which prevents impaired expression of many genes associated with the development of IPF, significantly reduces inflammatory and fibrotic lung tissue damage, reduces hydroxyproline (HYP) accumulation in the lung, and virtually eliminates mortality in animals after tracheal bleomycin infusion. Lammers et al. [41] aid to increase anti-COVID-19 PF complications therapeutic efficiency by nano-formulating dexamethasone and giving it by inhalation by targeting the interleukin receptor, potentiating its anti-oedema activity and by utilizing its anti-fibrotic effects. It is striking that it may contribute to better control of the severity of PF and promote better management of life-threatening symptoms in the acute and intermediate stages.
In studies for the treatment of PF, natural medicines such as herbs have shown low adverse effects, stable anti-inflammatory and anti-fibrotic therapeutic effects and no significant drug dependence due to their natural properties. This makes them a promising therapeutic target for PF [42]. Jiang et al. [43] took advantages of the ball milling technique to prepare a salvianolic acids dry powder inhalation complex with l-arginine and lecithin. It brings out good flowing properties, excellent biocompatibility, high deposition in the lung. The lung tissue Area under the concentration–time curve between 0 and 1 h (AUC(0–1)) of the pharmacokinetic concentration—time curve was 2099.12 times higher than that of the intravenous administration group (Fig. 7). Chennakesavulu et al. [44] have reported liposomal dry powder inhalants of budesonide and colchicine complex. The encapsulation rate of lyophilized liposomes using mannitol as the carrier was 97.89–98.6%. The system also supplied prolonged drug retention (more than 24 h) at targeted sites and reduced systemic exposure. Kotta et al. [45] employed an endogenous surfactant-based liposome delivery system, encapsulating Naringin, which acts as an aerosol to support lung mechanics in the management of PF, showing a 79 ± 1.5% lung deposition rate as well as low toxicity. Zhou et al. [46] designed a nebulized paclitaxel liposome inhalation system for the treatment of bleomycin-induced PF in rats. The results show that inhaled paclitaxel liposomes can prevent severe PF. This method of administration has fewer systemic side effects and is safer than intravenous injection.
Schematic of salvianolic acid dry powder inhaler for the treatment of PF. Salvianolic acid, arginine and lecithin dry powder were prepared by ball milling technology and successfully delivered to the lungs after aerosolization. The study proved that the biocompatibility, bioavailability and lung deposition rate were improved [43]
Emerging targets represent a new breakthrough for the treatment of PF and can potentially be encapsulated in advanced drug delivery formulations for site-specific therapy [17]. Pandolfi et al. [47] modified liposome with hyaluronic acid, which plays a vital role in its specific receptor CD44, overexpressed in pulmonary fibrotic cells. The liposomes decreased pro-inflammatory cytokines IL-1β, IL-12 and anti-fibrotic VEGF transcripts, but increased TGF-β mRNA. Wang et al. [48] intratracheal administrated methyl-CpG-binding domain 2 (MBD2) siRNA liposomes to protect mice against bleomycin-induced PF. The entrapment efficiency of prepared liposomes displayed approximately 90% for loading siRNA. The toxicity of liposome-loaded siRNA in cell viability was not detected. Those liposomes that were administered intratracheal continued to accumulate in the lungs for at least 7 days. NIRF signals were only detected in the lungs but absent in other organs (Fig. 8). Polyethylene glycol (PEG)ylated liposomes may also be considered in formulations characterised by reduced renal filtration, reduced uptake by the reticuloendothelial system (RES, e.g. liver and spleen) and reduced enzymatic degradation. As a result, PEGylated drugs show an extended half-life in vivo, resulting in enhanced bioavailability [49].
Intratracheal administration of MBD2 siRNA-loaded liposomes protects mice from BLM-induced lung injury and fibrosis [48]. A IVIS images of the mouse after inhaled liposomes; B The distribution of liposomes in the body organs; C Confocal immunofluorescence image of liposome in mice with PF; D Temporal MBD2 expression changes in the lungs from liposome-administered mice; E Schematic for experimental design and administration time line; F Intratracheal administration of liposomes loaded with MBD2 siRNA protected mice from lung injury and fibrosis. Left: Representative results of staining. Right: Ashcroft scores associated with fibrosis severity. G Determination of HYP in mice after PF. H Western blot analysis of the expressions of MBD2, fibronectin, type I collagen, α-SMA and arginase 1 in lung tissue. I MBD2 selectively binds Ship promoter in macrophages, enhances PI3K/Akt signaling pathway and promotes macrophage M2 program by inhibiting Ship expression
Togami et al. [50] used a aerosolized drug delivery system with PEGylated liposomes to improve the pharmacokinetic properties of the drug, which could effectively prolong the distribution of the drug in the lungs and could be an effective delivery system for antifibrotic drugs.
Nano structured lipid carrier (NLC)
The NLC is made up of an aqueous phase with a surfactant and an unstructured solid lipid matrix (a combination of solid and liquid lipids). Because NLC uses lipid mixtures, it is not easy to form an orderly crystal structure, which can give more sealing space to the drug. NLC addresses the problems of low solid lipid nanoparticles (SLN) drug load and easy drug leakage while having the slow-release advantage of SLN [51]. For the effective treatment of idiopathic PF, Garbuzenko et al. [52] presented a prostaglandin E (PGE2) administered in combination with selected siRNAs (CCL12, MMP3, and HIF1A) by inhalation using Precirol ATO 5, which is a solid lipid as carrier. After treatment, the volume of fibrotic tissue in the lungs was reduced by 3.8-fold, which was essentially the same as the normal value (Fig. 9). The combination treatment also suppressed the expression of all pro-fibrotic genes, such as the expression of CTGF, TGFB1, TGFB2, TGFB3, TGFBR1, and TGFBR2 was downregulated. Keum et al. [53] evaluated the therapeutic efficacy of APTATstat3-9R, a high-affinity peptide conjugate that inhibits signal transducer and activator of transcription 3 (STAT3) phosphorylation via cell-penetrating 9-arginine motif modifications, a STAT3 phosphorylated cell-permeable peptide inhibitor, for the indication of improving PF. The biomimetic lipid nanocomplexes inhibits M2 polarization of lung epithelial and fibroblast differentiation into myofibroblasts and macrophages and penetrates the lung surfactant barrier and is taken up by lung epithelial cells. This work demonstrates a non-invasive, safe and effective approach to alleviate pulmonary fibrosis, but adverse effects such as cytotoxicity of uncertain mechanisms have emerged. But in general, the nanostructured lipid carrier has good biocompatibility [54], low toxicity [55], good inhalability [56], and slow-release control properties [57].
MRI and CT comparison of the development of PF in the healthy and untreated groups and in the PGE2 and siRNA nanostructured lipid carrier treatment groups. The areas with cyan color represent normal lung tissue. Yellow indicates normal connective tissue, while green indicates fibrotic tissue. After treatment, the volume of fibrotic tissue in the lungs was reduced by 3.8 times, which is almost the same as the normal value [52]
Nanovesicles
Nanovesicles have lately attracted a lot of attention due to their potential as a medicine delivery method [58]. They have distinct benefits as naturally occurring endogenous drug carriers, including low immunogenicity, high blood stability, high delivery efficiency, targeting ability, and improved permeability and retention impact. Dinh et al. [59] put forward using lung spheroid cell exosomes (LSC-Exo) inhalation to treat two models of PF induced by bleomycin and silica, respectively. By restoring normal alveolar structure, lowering collagen buildup and myofibroblast proliferation, enhancing AQP5+ and vWF+ cells, and decreasing αSMA+ cells, LSC-Exo treatment eased and reversed bleomycin- and silica-induced fibrosis. Inspiratory capacity and respiratory compliance are improved significantly after the LSC-Exo remedy. In addition, the therapeutic effect of LSC-Exo were superior to other components derived from mesenchymal stem cells (MSC), confirming the therapeutic potential of LSC-Exo inhalation for lung regeneration (Fig. 10). Li et al. [60] discovered that inhalation of four doses of the human lung spheroid cells-nanodecoy can effectively alleviate the inflammatory cells infiltration, reduce the degree of PF caused by COVID-19. This nanodecoy is highly translatable, so progenitor cells serve as a potential therapeutic approach for the treatment of PF. Additionally, Ashcroft score shows that this LSC-nanodecoy largely reduces fibrosis in primate cynomolgus macaques.
A Principal component analysis plots of LSC-exosome and MSC-exosome microRNA contents. B Quantification of fibrosis by Ashcroft score. The LSC-Exo treatment group showed therapeutic effects both in terms of maintaining normal lung structure and reducing fibrosis. C Quantification of pulmonary HYP levels; The LSC-Exo treatment group showed therapeutic effects in both reducing HYP levels and reducing collagen deposition. D LSC-Exo treatment group attenuated alveolar epithelial and vascular damage and reduced fibrosis, indicating an increase in AQP5+ and vWF+ cells and a decrease in αSMA+ cells [59]
Polymeric nanocarriers
Polymeric nanocarriers can be divided into polymeric nanoparticles, micelles, dendrimers, and polymeric drug complexes [61]. Polymeric nanoparticles are now being studied intensively for their exceptional potential as an anti-fibrosis medication delivery strategy. They’re made by encapsulating, dissolving, and entrapping the medication in biodegradable polymers or embedding the molecule in a polymeric matrix.
Chitosan nanoparticles are nowadays of great interest in nanomedicine and in the development of novel therapeutic drug delivery systems with higher bioavailability, by improving specificity and sensitivity and reducing pharmacological toxicity [62]. Chitosan nanoparticles combine the natural properties of polymers with the possibility of tunable size and surface modification according to tailored needs [63]. According to Rashidipour et al. [64] paraquat herbicide loaded on Pectin/Chitosan/Tripolyphosphate nanoparticles effectively reduced acute lung damage and PF, implying decreased apoptosis, oxidative stress, and α-smooth muscle actin (α-SMA) expression in lung tissue. The nanoparticles themselves displayed little or no harm, as evidenced by inflammatory and apoptotic indicators and histology scores. Zhang et al. [65] used amphoteric phosphorylcholine and chitosan to develop mimetic phosphorylcholine chitosan nanoparticles (PCCs-NPs) as a protein (msFGFR2c) delivery platform for the treatment of PF, which inhibited TGF-β1-induced α-SMA expression in fibroblasts, significantly reduced PF scores and collagen deposition, and significantly improved survival rates.
Poly(lactic-co-glycolic acid) is an FDA approved polymeric material with biodegradable and biocompatible characteristics [66]. Lee et al. [67] found that using an emulsification diffusion method prepared inhaled tacrolimus-loaded chitosan-coated-PLGA nanoparticles markedly reduced inflammation. The results showed tacrolimus extended release up to 5 days and demonstrated good localization and deposition rates in the lungs. This system is also perceived as an efficient sustained-release type inhalation system (Fig. 11). Elkomy et al. [68] developed a novel, non-invasive inhalable nifedipine-loaded chitosan-PLGA polymeric nanoparticles with the 61.81% entrapment efficiency and 50.4% sustained release profile over 24 h, which can regulate the TGF-β/β-catenin pathway in the rat model of bleomycin-induced PF.
Effectiveness of PF treatment after inhalation of TAC PLGA-NPs. A Morphologies of chitosan TAC PLGA-NPs by field-emission scanning electron microscopy (FE-SEM). The mean size of TAC PLGA-NPs and chitosan TAC PLGA-NPs was 320 ± 9.0 and 441 ± 11.9 nm. B This nanomedicine demonstrated good localization and deposition rates in the lungs. This system is also perceived as an efficient sustained-release type inhalation system [67]
Pirfenidone is the first licensed PF therapy, commonly used orally, and is known to mediate its anti-inflammatory and anti-fibrotic effects through modulation of cytokines and growth factors, but adverse effects such as gastrointestinal and photosensitivity are common in clinical trials, and dose limiting treatment leads to reduced effectiveness of the drug [69]. Therefore, the combination of pirfenidone and nanoparticles can be considered for inhalation administration to reduce side effects. Trivedi et al. [70] employed lactide-glycolide nanoparticles containing pirfenidone to ameliorate bleomycin-induced PF mice by intratracheal administration. The results indicated that the number of fibrotic cells, lymphocytes and neutrophils markedly decreased. These polymeric nanocarriers maintained delivery of pulmonary pirfenidone and enhance its antifibrotic efficacy.
The important role of the stromal cell-derived factor-1/chemokine receptor CXCR4 (SDF-1/CXCR4) axis in fibroblast recruitment and other pro-inflammatory and pro-fibrotic activities has been reported, and CXCR4 inhibition is a promising therapeutic target for PF [71,72,73]. Ding et al. [74] reported the development of a multimeric complex based on CXCR4 inhibition of poly(ethylimine) derivatives (PEI-C) for lung delivery of siRNA to silence fibrinogen activator inhibitor-1 (siPAI-1) in a combination therapy for PF, with fluorescence showing the longest drug retention time in the lung, significant downregulation of PAI-1 expression, and significant reduction in intrapulmonary collagen deposition.
Protein nanocarrier
Protein nanocarriers use proteins as carriers to deliver drugs by reacting with the amino carboxyl groups on the surface of the protein. It can improve the stability, bioavailability and pharmacokinetics of therapeutic proteins. Seo et al. [75] investigated a sustained release type of inhalable albumin nanoparticles binding tacrolimus with 85.3 ± 4.7% encapsulation efficiency, direct exposure, rapid absorption, long deposition. The system significantly decreased the extent of fibrotic and appeared similar to untreated lungs.
Zhang et al. [76] constructed an mRNA nano-delivery system co-loaded with matrix metalloproteinase 13 mRNA (mMMP13) and keratinocyte growth factor through dual functionalization modification. The system can be used to repair fibrotic lesions by synergistically promoting matrix degradation and alveolar epithelial reconstruction in PF lesions, providing a new idea for the treatment of PF diseases (Fig. 12). Bai et al. [22] developed a mucus-permeable nanoparticle system that combines siRNA against IL-11 and is regulated by inhibition of extracellular signal-regulated kinase and SMAD2. Thereby inhibiting fibroblastic differentiation and reducing excessive extracellular matrix deposition, significantly reducing fibrosis development.
A Feasibility of recombinant endogenous ribosome proteins being screened for mRNA delivery; A nano-based delivery system containing mMMP13 and keratinocyte growth factor (KGF) was prepared by dual functional modification; B The nano drug deposited in alveoli after inhalation releases outer KGF in response to the lesion site and promotes the proliferation of alveolar epithelial cells. After uptake of the recombinant ribosomal protein complex of mMMP13, in situ production of MMP13 accelerates the degradation of extracellular matrix in the alveolar cavity and promotes fibrosis lesion repair [76]
Nanosuspension
Nanosuspension drug delivery system refers to the medicinal dispersion system formed by suspending nano drugs in solvents. It has evolved in response to the numerous water-insoluble drug candidates that have emerged through high-throughput drug screening procedures that place a premium on fit into hydrophobic receptor pockets [77]. Su et al. [78] utilized high-pressure homogenization method and developed an inhalable tetrandrine-hydroxypropyl-β-cyclodextrin inclusion nanosuspension (640.3 ± 49.2 nm) for bleomycin-induced PF therapy, indicating faster uptake, higher solubilizing efficiency, reducing inflammation and fibrosis level, limiting the accumulation of HYP in the lungs, modulating proteins expressed in the development of fibrosis, and better postoperative survival (Fig. 13).
Schematic diagram of an inhalable powdered Tetrandrine-hydroxypropyl-β-cyclodextrin inclusion body nanosuspension for bleomycin-induced PF treatment [78]
Nanoparticles
Nanoparticles offer new possibilities for improving drug release properties and obtaining optimal results in the treatment of inflammatory lung diseases by modifying the physical properties of the inhaled drug delivery carriers, such as particle size, shape, density, surface charge and other surface modifications [79, 80]. Vartiainen et al. [81] fabricated a dry powder nanoparticle formulation that contained 29.4% of tilorone, 9.6% of leucine and 61.0% of mannitol for silica-induced PF treatment. The formulation promoted more stable penetration through the monolayer of lung cells. Additionally, it is important to note that there have been no studies on the pharmacokinetics of tirolone lung administration. Hemmati et al. [82] synthesized nano-curcumin with cyclodextrin as a neutral soluble carrier (275 nm), and the system can reduce the overall HYP content, TNF-α, TGF-β, platelet derived growth factor (PDGF) levels and increased IL-10 level. Compared to oral and conventional inhaled curcumin, nano-curcumin is more effective and has fewer side effects, significantly lower levels of inflammatory markers, and most importantly, inhalation of synthetic nano-curcumin can restore lung HYP levels. Zhou et al. [83] prepared inhalable gadofullerenol and fullerenol by a one-pot reaction, which obviously reduced collagen deposition caused by acute lung injury. This study revealed these nanoparticles’ antioxidant and anti-inflammatory function in regulating ROS-mediated inflammatory processes. Its therapeutic effects may be related to a synergistic mechanism of free radical scavenging and indirect regulation of TGF-β1 expression (Fig. 14).
Gold nanoparticles
Nanoscale gold surfaces have special effects. Therefore, gold nanoparticles can directly or indirectly produce different biological activities [84]. Codullo et al. [85] synthesized anti-CD44 imatinib-loaded gold nanoparticles, which acted on inhibition of proliferation and activity of pulmonary fibrotic cells, available reduction of IL-8 release, viability and polarization of M2 in alveolar macrophages (Fig. 15). Pandolfi et al. [86] have reported inhalable imatinib loading gold nanoparticles, which functionalized with antibody against CD44, demonstrating significant reduction tracheal lumen obliteration and apoptosis, and TGF-β-positive signal in surroundings.
Schematic diagram of imatinib-loaded gold nanoparticles inhibiting the proliferation of fibroblasts and macrophages and ameliorating experimental bleomycin-induced PF in patients with systemic sclerosis [85]
Hydrogel-based delivery
Due to the high biocompatibility [87], drug protection [88], spatial and temporal control of drug release [88] and physicochemical customisability [89] offered by hydrogels hydrogels are increasingly investigated as topical drug delivery systems. Shamskhou et al. [90] innovated a hydrogel-based delivery system for recombinant interleukin-10 (IL-10) that breaks the half-life limit of free IL-10, which has the ability to reversibly bind IL-10 through the use of heparin without bleeding or other complications. This formulation is remarkably more effective than free IL-10 for both preventing and reducing collagen deposition in the lung parenchyma after 7 days of inhalation and has been shown to be used to prevent and reverse bleomycin-induced PF (Table 2).
Conclusions and future outlook
PF is one of the most dangerous interstitial lung disorders with the poorest prognosis. It is becoming increasingly regarded as a complication in individuals who have been infected with COVID-19, highlighting the importance of finding effective and site-specific therapeutics to reverse and maybe cure the disease [91, 92]. At present, all drugs that can be used for the treatment of PF are administered by systemic administration, with large toxic and side effects and poor patient compliance. Effective inhaled drugs are emerged and developed. However, inhaled free anti-fibrosis agents are highly toxic, easily cleared quickly, and their distribution in the lungs is not specific.
Inhaled nano-based drug delivery systems have many advantages over conventional drug or micron delivery systems for the treatment of PF [93]: (1) Targeted drug delivery [94]: increases the concentration of drug in the lungs, controls the release of drug, overcomes the lung barrier, reduces the dose of drug thus reducing the side effects of treatment and improving patient compliance; (2) Increased bioavailability of drug [95, 96]: allows better water solubility and protects it from degradation; (3) Rapid onset of action [97]: avoids first pass effects in the liver. Nanovaccines can exploit the large surface area of the lung and the rich environmental characteristics of antigen-presenting cells to elicit robust immune defense against various mucosal diseases [98]. A small number of inhaled nanomedicines for lung diseases have entered clinical trials, such as LQ036 nanobodies for moderate to severe asthma, but they have been terminated in Phase I [99], and mRNA VX-522 for cystic fibrosis for cystic fibrosis is in Phase I clinical trials [100]. However, inhaled nanomaterials for PF have not yet started clinical trials and need further research.
But still, the development of inhaled nano-based drug delivery system presents many challenges. In addition to the safety and efficacy of inhaled drugs in the lung, the lung biopharmaceutical properties should also be fully evaluated in drug design to ensure that inhaled nano-based drugs can maintain pharmacodynamic concentration in lung tissue for a long time. Noteworthy, actively-targeted inhaled nano-based drug delivery system in the treatment of PF ensure that all of these are in the investigational or unattended stage. Additionally, nanotechnology as a novel approach has not yet been approved for the clinical treatment of PF. Further investigation can focus on nanomedicines, immunotherapy and inhalable nanovaccines, which hold great promise for the treatment of PF. In conclusion, the use of inhaled nano-based drug delivery system has great potential when it comes to PF therapy, the safety, efficacy and industrial production of its clinical application still need to be further studied.
Data availability
The dataset supporting this review article is included within all the cited articles.
References
Wynn TA. Integrating mechanisms of pulmonary fibrosis. J Exp Med. 2011;208:1339–50.
Lederer DJ, Martinez FJ. Idiopathic pulmonary fibrosis. N Engl J Med. 2018;378:1811–23.
Ballester B, Milara J, Cortijo J. Idiopathic pulmonary fibrosis and lung cancer: mechanisms and molecular targets. Int J Mol Sci. 2019;20:593.
Deng Z, Fear MW, Choi YS, Wood FM, Allahham A, Mutsaers SE, Prêle CM. The extracellular matrix and mechanotransduction in pulmonary fibrosis. Int J Biochem Cell B. 2020;126:105802.
Martinez FJ, Collard HR, Pardo A, Raghu G, Richeldi L, Selman M, Swigris JJ, Taniguchi H, Wells AU. Idiopathic pulmonary fibrosis. Nat Rev Dis Primers. 2017;3:1–19.
Assad N, Sood A, Campen MJ, Zychowski KE. Metal-induced pulmonary fibrosis. Curr Environ Health Rep. 2018;5:486–98.
Sgalla G, Iovene B, Calvello M, Ori M, Varone F, Richeldi L. Idiopathic pulmonary fibrosis: pathogenesis and management. Respirs Res. 2018;19:1–18.
Vianello A, Guarnieri G, Braccioni F, Lococo S, Molena B, Cecchetto A, Giraudo C, De Marchi LB, Caminati M, Senna G. The pathogenesis, epidemiology and biomarkers of susceptibility of pulmonary fibrosis in COVID-19 survivors. Clin Chem Lab Med. 2022;60:307–16.
Zhang C, Wu Z, Li JW, Tan K, Yang W, Zhao H, Wang GQ. Discharge may not be the end of treatment: Pay attention to pulmonary fibrosis caused by severe COVID-19. J Med Virol. 2021;93:1378–86.
Ryan N, Meskell P. The experience of people with idiopathic pulmonary fibrosis living through the COVID-19 pandemic. J Adv Nurs. 2022;78(7):2232–44.
Carvalho LV, da Silva SC, Fontes JL, Cardoso L, Salomar M, Duarte-Neto AN, Figueira C, Brito R, Mesquita B, de Freitas LA. COVID-19 beyond DAD: persisting microcirculation thrombosis, hidden infections, and early pulmonary fibrosis as remaining challenges of the disease. Hum Pathol Rep. 2022;27:300607.
Covvey JR, Mancl EE. Recent evidence for pharmacological treatment of idiopathic pulmonary fibrosis. Ann Pharmacother. 2014;48:1611–9.
Skibba M, Drelich A, Poellmann M, Hong S, Brasier AR. Nanoapproaches to modifying epigenetics of epithelial mesenchymal transition for treatment of pulmonary fibrosis. Front Pharmacol. 2020;11:607689.
Homma S, Bando M, Azuma A, Sakamoto S, Sugino K, Ishii Y, Izumi S, Inase N, Inoue Y, Ebina M. Japanese guideline for the treatment of idiopathic pulmonary fibrosis. Respir Investig. 2018;56:268–91.
Kato M, Sasaki S, Nakamura T, Kurokawa K, Yamada T, Ochi Y, Ihara H, Takahashi F, Takahashi K. Gastrointestinal adverse effects of nintedanib and the associated risk factors in patients with idiopathic pulmonary fibrosis. Sci Rep-UK. 2019;9:1–9.
Hanta I, Cilli A, Sevinc C. The effectiveness, safety, and tolerability of Pirfenidone in idiopathic pulmonary fibrosis: a retrospective study. Adv Ther. 2019;36:1126–31.
Ghumman M, Dhamecha D, Gonsalves A, Fortier L, Sorkhdini P, Zhou Y, Menon JU. Emerging drug delivery strategies for idiopathic pulmonary fibrosis treatment. Eur J Pharm Biopharm. 2021;164:1–12.
Galli JA, Pandya A, Vega-Olivo M, Dass C, Zhao H, Criner GJ. Pirfenidone and nintedanib for pulmonary fibrosis in clinical practice: tolerability and adverse drug reactions. Respirology. 2017;22:1171–8.
Mu W, Chu Q, Liu Y, Zhang N. A review on nano-based drug delivery system for cancer chemoimmunotherapy. Nano-Micro Lett. 2020;12:1–24.
Thubelihle Ndebele R, Yao Q, Shi Y-N, Zhai Y-Y, Xu H-L, Lu C-T, Zhao Y-Z. Progress in the application of nano-and micro-based drug delivery systems in pulmonary drug delivery. BIO Integr. 2022;13:71–83.
Zhou Z, et al. Rational design of cancer nanomedicine: nanoproperty integration and synchronization. Adv Mater. 2017;29:1606628.
Bai X, Zhao G, Chen Q, Li Z, Gao M, Ho W, Xu X, Zhang XQ. Inhaled siRNA nanoparticles targeting IL11 inhibit lung fibrosis and improve pulmonary function post-bleomycin challenge. Sci Adv. 2022;8:eabn7162.
Camelo A, Dunmore R, Sleeman MA, Clarke DL. The epithelium in idiopathic pulmonary fibrosis: breaking the barrier. Front Pharmacol. 2014;4:173.
Wang JM, Robertson SH, Wang Z, He M, Virgincar RS, Schrank GM, Smigla RM, O’Riordan TG, Sundy J, Ebner L. Using hyperpolarized 129Xe MRI to quantify regional gas transfer in idiopathic pulmonary fibrosis. Thorax. 2018;73:21–8.
Fulaz S, Vitale S, Quinn L, Casey E. Nanoparticle–biofilm interactions: the role of the EPS matrix. Trends Microbiol. 2019;27:915–26.
Liu Q, Zhang X, Xue J, Chai J, Qin L, Guan J, Zhang X, Mao S. Exploring the intrinsic micro−/nanoparticle size on their in vivo fate after lung delivery. J Controll Release. 2022;347:435–48.
Praphawatvet T, Peters JI, Williams RO III. Inhaled nanoparticles—an updated review. Int J Pharmaceut. 2020;587:119671.
Zhao J, Qin L, Song R, Su J, Yuan Y, Zhang X, Mao S. Elucidating inhaled liposome surface charge on its interaction with biological barriers in the lung. Eur J Pharm Biopharma. 2022;172:101–11.
Fischer D, Li Y, Ahlemeyer B, Krieglstein J, Kissel T. In vitro cytotoxicity testing of polycations: influence of polymer structure on cell viability and hemolysis. Biomaterials. 2003;24:1121–31.
Murali S, Mangotra A. NanoToxicity—a bird's eye view of toxicological aspects. 2018.
Asati S, Sahu A, Jain A. Nanotoxicity: the dark side of nanoformulations. Curr Nanotoxicity Prev. 2021;1:6–25.
Wei Y, Zhao L. Passive lung-targeted drug delivery systems via intravenous administration. Pharm Dev Technol. 2014;19:129–36.
Molina-Molina M. The future of pharmacological treatment in idiopathic pulmonary fibrosis. Arch Bronconeumol. 2019;55:642–7.
George PM, Patterson CM, Reed AK, Thillai M. Lung transplantation for idiopathic pulmonary fibrosis. Lancet Resp Med. 2019;7:271–82.
Kuzmov A, Minko T. Nanotechnology approaches for inhalation treatment of lung diseases. J Controll Release. 2015;219:500–18.
Akçan R, Aydogan HC, Yildirim MŞ, Taştekin B, Sağlam N. Nanotoxicity: a challenge for future medicine. Turk J Med Sci. 2020;50:1180–96.
Gaber M, Medhat W, Hany M, Saher N, Fang J-Y, Elzoghby A. Protein-lipid nanohybrids as emerging platforms for drug and gene delivery: challenges and outcomes. J Controll Release. 2017;254:75–91.
Unida S, Ito Y, Onodera R, Tahara K, Takeuchi H. Inhalation properties of water-soluble drug loaded liposomes atomized by nebulizer. Asian J Pharm Sci. 2016;11:205–6.
Rudokas M, Najlah M, Alhnan MA, Elhissi A. Liposome delivery systems for inhalation: a critical review highlighting formulation issues and anticancer applications. Med Prin Pract. 2016;25:60–72.
Ivanova V, Garbuzenko OB, Reuhl KR, Reimer DC, Pozharov VP, Minko T. Inhalation treatment of pulmonary fibrosis by liposomal prostaglandin E2. Eur J Pharm Biopharm. 2013;84:335–44.
Lammers T, Sofias AM, Van der Meel R, Schiffelers R, Storm G, Tacke F, Koschmieder S, Brümmendorf TH, Kiessling F, Metselaar JM. Dexamethasone nanomedicines for COVID-19. Nat Nanotechnol. 2020;15:622–4.
Murthy P, Shaibie NA, Lim CL, Ling APK, Chye SM, Koh RY. An overview of herbal medicines for idiopathic pulmonary fibrosis. Processes. 2022;10:1131.
Jiang L, Li Y, Yu J, Wang J, Ju J, Dai J. A dry powder inhalable formulation of salvianolic acids for the treatment of pulmonary fibrosis: safety, lung deposition, and pharmacokinetic study. Drug Deliv Transl Res. 2021;11:1958–68.
Chennakesavulu S, Mishra A, Sudheer A, Sowmya C, Reddy CS, Bhargav E. Pulmonary delivery of liposomal dry powder inhaler formulation for effective treatment of idiopathic pulmonary fibrosis. Asian J Pharm Sci. 2018;13:91–100.
Kotta S, Aldawsari HM, Badr-Eldin SM, Binmahfouz LS, Bakhaidar RB, Sreeharsha N, Nair AB, Ramnarayanan C. Aerosol delivery of surfactant liposomes for management of pulmonary fibrosis: an approach supporting pulmonary mechanics. Pharmaceutics. 2021;13(11):1851.
Zhou Y, Zhu W, Cai X, Chen M. Atomized paclitaxel liposome inhalation treatment of bleomycin-induced pulmonary fibrosis in rats. Genet Mol Res. 2016;15:1–11.
Pandolfi L, Frangipane V, Bocca C, Marengo A, Tarro Genta E, Bozzini S, Morosini M, D’Amato M, Vitulo S, Monti M. Hyaluronic acid-decorated liposomes as innovative targeted delivery system for lung fibrotic cells. Molecules. 2019;24(18):3291.
Wang Y, Zhang L, Wu G-R, Zhou Q, Yue H, Rao L-Z, Yuan T, Mo B, Wang F-X, Chen L-M. MBD2 serves as a viable target against pulmonary fibrosis by inhibiting macrophage M2 program. Sci Adv. 2021;7:eabb6075.
Knop K, Hoogenboom R, Fischer D, Schubert US. Poly (ethylene glycol) in drug delivery: pros and cons as well as potential alternatives. Angew Chem Int Ed. 2010;49:6288–308.
Togami K, Maruta Y, Nanbu M, Tada H, Chono S. Prolonged distribution of aerosolized PEGylated liposomes in the lungs of mice with bleomycin-induced pulmonary fibrosis. Drug Dev Ind Pharm. 2020;46:1873–80.
Khosa A, Reddi S, Saha RN. Nanostructured lipid carriers for site-specific drug delivery. Biomed Pharmacother. 2018;103:598–613.
Garbuzenko OB, Ivanova V, Kholodovych V, Reimer DC, Reuhl KR, Yurkow E, Adler D, Minko T. Combinatorial treatment of idiopathic pulmonary fibrosis using nanoparticles with prostaglandin E and siRNA (s). Nanomed-Nanotechnol. 2017;13:1983–92.
Keum H, Kim J, Yoo D, Kim TW, Seo C, Kim D, Jon S. Biomimetic lipid nanocomplexes incorporating STAT3-inhibiting peptides effectively infiltrate the lung barrier and ameliorate pulmonary fibrosis. J Controll Release. 2021;332:160–70.
Weber S, Zimmer A, Pardeike J. Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) for pulmonary application: a review of the state of the art. Eur J Pharm Biopharm. 2014;86:7–22.
Pardeike J, Weber S, Zarfl HP, Pagitz M, Zimmer A. Itraconazole-loaded nanostructured lipid carriers (NLC) for pulmonary treatment of aspergillosis in falcons. Eur J Pharm Biopharm. 2016;108:269–76.
Tiwari R, Pathak K. Nanostructured lipid carrier versus solid lipid nanoparticles of simvastatin: comparative analysis of characteristics, pharmacokinetics and tissue uptake. Int J Pharmaceut. 2011;415:232–43.
Patil-Gadhe A, Kyadarkunte A, Patole M, Pokharkar V. Montelukast-loaded nanostructured lipid carriers: Part II pulmonary drug delivery and in vitro–in vivo aerosol performance. Eur J Pharm Biopharm. 2014;88:169–77.
Estanqueiro M, Amaral MH, Conceição J, Lobo JMS. Nanotechnological carriers for cancer chemotherapy: the state of the art. Colloids Surf B. 2015;126:631–48.
Dinh P-UC, Paudel D, Brochu H, Popowski KD, Gracieux MC, Cores J, Huang K, Hensley MT, Harrell E, Vandergriff AC. Inhalation of lung spheroid cell secretome and exosomes promotes lung repair in pulmonary fibrosis. Nat Commun. 2020;11:1–14.
Li Z, Wang Z, Dinh P-UC, Zhu D, Popowski KD, Lutz H, Hu S, Lewis MG, Cook A, Andersen H. Cell-mimicking nanodecoys neutralize SARS-CoV-2 and mitigate lung injury in a non-human primate model of COVID-19. Nat Nanotechnol. 2021;16:942–51.
Abdelaziz HM, Gaber M, Abd-Elwakil MM, Mabrouk MT, Elgohary MM, Kamel NM, Kabary DM, Freag MS, Samaha MW, Mortada SM. Inhalable particulate drug delivery systems for lung cancer therapy: nanoparticles, microparticles, nanocomposites and nanoaggregates. J Controll Release. 2018;269:374–92.
Sharifi-Rad J, Quispe C, Butnariu M, Rotariu LS, Sytar O, Sestito S, Rapposelli S, Akram M, Iqbal M, Krishna A. Chitosan nanoparticles as a promising tool in nanomedicine with particular emphasis on oncological treatment. Cancer Cell Int. 2021;21:1–21.
Mohammed MA, Syeda JT, Wasan KM, Wasan EK. An overview of chitosan nanoparticles and its application in non-parenteral drug delivery. Pharmaceutics. 2017;9(4):53.
Rashidipour M, Rasoulian B, Maleki A, Davari B, Pajouhi N, Mohammadi E. Pectin/chitosan/tripolyphosphate encapsulation protects the rat lung from fibrosis and apoptosis induced by paraquat inhalation. Pestic Biochem Phys. 2021;178: 104919.
Zhang G, Mo S, Fang B, Zeng R, Wang J, Tu M, Zhao J. Pulmonary delivery of therapeutic proteins based on zwitterionic chitosan-based nanocarriers for treatment on bleomycin-induced pulmonary fibrosis. Int J Biol Macromol. 2019;133:58–66.
Makadia HK, Siegel SJ. Poly lactic-co-glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polymers. 2011;3:1377–97.
Lee C, Seo J, Hwang HS, Lee S, Lee ES, Lee EH, Choi H-G, Youn YS. Treatment of bleomycin-induced pulmonary fibrosis by inhaled tacrolimus-loaded chitosan-coated poly (lactic-co-glycolic acid) nanoparticles. Biomed Pharmacother. 2016;78:226–33.
Elkomy MH, Khallaf RA, Mahmoud MO, Sayed RR, El-Kalaawy AM, Abdel-Razik A-RH, Aboud HM. Intratracheally inhalable nifedipine-loaded chitosan-PLGA nanocomposites as a promising nanoplatform for lung targeting: snowballed protection via regulation of TGF-β/β-catenin pathway in bleomycin-induced pulmonary fibrosis. Pharmaceuticals. 2021;14(12):1225.
Gulati S, Luckhardt TR. Updated evaluation of the safety, efficacy and tolerability of pirfenidone in the treatment of idiopathic pulmonary fibrosis. Drug Healthc Patient. 2020;12:85–94.
Trivedi R, Redente EF, Thakur A, Riches DW, Kompella UB. Local delivery of biodegradable pirfenidone nanoparticles ameliorates bleomycin-induced pulmonary fibrosis in mice. Nanotechnology. 2012;23:505101.
Li F, Dai H, Geng J, Xu X. Inhibiting CXCR4/CXCL12 axis attenuates lung fibrosis both in vitro and in vivo. Eur Respir Soc. 2012.
Xu J, Mora A, Shim H, Stecenko A, Brigham KL, Rojas M. Role of the SDF-1/CXCR4 axis in the pathogenesis of lung injury and fibrosis. Am J Resp Cell Mol. 2007;37:291–9.
Shu H-KG, Yoon Y, Hong S, Xu K, Gao H, Hao C, Torres-Gonzalez E, Nayra C, Rojas M, Shim H. Inhibition of the CXCL12/CXCR4-axis as preventive therapy for radiation-induced pulmonary fibrosis. PLoS ONE. 2013;8(11):e79768.
Ding L, Zhu C, Yu F, Wu P, Chen G, Ullah A, Wang K, Sun M, Li J, Oupický D. Pulmonary delivery of polyplexes for combined PAI-1 gene silencing and CXCR4 inhibition to treat lung fibrosis. Nanomed-Nanotechnol. 2018;14:1765–76.
Seo J, Lee C, Hwang HS, Kim B, Lee ES, Oh KT, Lim J-L, Choi H-G, Youn YS. Therapeutic advantage of inhaled tacrolimus-bound albumin nanoparticles in a bleomycin-induced pulmonary fibrosis mouse model. Pulm Pharmacol Ther. 2016;36:53–61.
Zhang R, Jing W, Chen C, Zhang S, Mohamed M, Sun P, Wang G, You W, Yang Z, Zhang J. Inhaled mRNA nanoformulation with biogenic ribosomal protein reverses established pulmonary fibrosis in a bleomycin-induced murine model. Adv Mater. 2022;32(14):e2107506.
Rabinow BE. Nanosuspensions in drug delivery. Nat Rev Drug Discov. 2004;3:785–96.
Su W, Liang Y, Meng Z, Chen X, Lu M, Han X, Deng X, Zhang Q, Zhu H, Fu T. Inhalation of tetrandrine-hydroxypropyl-β-cyclodextrin inclusion complexes for pulmonary fibrosis treatment. Mol Pharmaceut. 2020;17:1596–607.
Wang K, Lei Y, Xia D, Xu P, Zhu T, Jiang Z, Ma Y. Neutrophil membranes coated, antibiotic agent loaded nanoparticles targeting to the lung inflammation. Colloids Surf B. 2020;188:110755.
Card JW, Zeldin DC, Bonner JC, Nestmann ER. Pulmonary applications and toxicity of engineered nanoparticles. Am J Physiol-Lung C. 2008;295:L400–11.
Vartiainen V, Raula J, Bimbo LM, Viinamäki J, Backman JT, Ugur N, Kauppinen E, Sutinen E, Joensuu E, Koli K. Pulmonary administration of a dry powder formulation of the antifibrotic drug tilorone reduces silica-induced lung fibrosis in mice. Int J Pharmaceut. 2018;544:121–8.
Hemmati AA, Karampour NS, Dahanzadeh S, Sharif B, Makhmalzadeh AR, Ghafourian M. The protective effects of nebulized nano-curcumin against bleomycin-induced pulmonary fibrosis in rats. Jundishapur J Nat Pharma Prod. 2021;16:e106961.
Zhou Y, Zhen M, Ma H, Li J, Shu C, Wang C. Inhalable gadofullerenol/[70] fullerenol as high-efficiency ROS scavengers for pulmonary fibrosis therapy. Nanomed-Nanotechnol. 2018;14:1361–9.
Ko W-C, Wang S-J, Hsiao C-Y, Hung C-T, Hsu Y-J, Chang D-C, Hung C-F. Pharmacological role of functionalized gold nanoparticles in disease applications. Molecules. 2022;27:1551.
Codullo V, Cova E, Pandolfi L, Breda S, Morosini M, Frangipane V, Malatesta M, Calderan L, Cagnone M, Pacini C. Imatinib-loaded gold nanoparticles inhibit proliferation of fibroblasts and macrophages from systemic sclerosis patients and ameliorate experimental bleomycin-induced lung fibrosis. J Controll Release. 2019;310:198–208.
Pandolfi L, Fusco R, Frangipane V, D’Amico R, Giustra M, Bozzini S, Morosini M, D’Amato M, Cova E, Ferrario G. Loading Imatinib inside targeted nanoparticles to prevent Bronchiolitis Obliterans Syndrome. Sci Rep-UK. 2020;10:1–10.
Naahidi S, Jafari M, Logan M, Wang Y, Yuan Y, Bae H, Dixon B, Chen P. Biocompatibility of hydrogel-based scaffolds for tissue engineering applications. Biotechnol Adv. 2017;35:530–44.
Li J, Mooney DJ. Designing hydrogels for controlled drug delivery. Nat Rev Mater. 2016;1:1–17.
Loessner D, Meinert C, Kaemmerer E, Martine LC, Yue K, Levett PA, Klein TJ, Melchels FP, Khademhosseini A, Hutmacher DW. Functionalization, preparation and use of cell-laden gelatin methacryloyl-based hydrogels as modular tissue culture platforms. Nat Protoc. 2016;11:727–46.
Shamskhou EA, Kratochvil MJ, Orcholski ME, Nagy N, Kaber G, Steen E, Balaji S, Yuan K, Keswani S, Danielson B. Hydrogel-based delivery of Il-10 improves treatment of bleomycin-induced lung fibrosis in mice. Biomaterials. 2019;203:52–62.
Ojo AS, Balogun SA, Williams OT, Ojo OS. Pulmonary fibrosis in COVID-19 survivors: predictive factors and risk reduction strategies. BMC Pulm Med. 2020;2020(5):1–10.
Alhiyari MA, Ata F, Alghizzawi MI, Bilal ABI, Abdulhadi AS, Yousaf Z. Post COVID-19 fibrosis, an emerging complicationof SARS-CoV-2 infection. IDCases. 2021;23:e01041.
Patra JK, Das G, Fraceto LF, Campos EVR, Rodriguez-Torres MdP, Acosta-Torres LS, Diaz-Torres LA, Grillo R, Swamy MK, Sharma S. Nano based drug delivery systems: recent developments and future prospects. J Nanobiotechnol. 2018;16:1–33.
Forest V, Pourchez J. Nano-delivery to the lung-by inhalation or other routes and why nano when micro is largely sufficient? Adv Drug Deliver Rev. 2022;183:114173.
Lee W-H, Loo C-Y, Traini D, Young PM. Inhalation of nanoparticle-based drug for lung cancer treatment: advantages and challenges. Asian J Pharm Sci. 2015;10:481–9.
Gulati N, Chellappan DK, MacLoughlin R, Dua K, Dureja H. Inhaled nano-based therapeutics for inflammatory lung diseases: recent advances and future prospects. Life Sci. 2021;285:119969.
Hädrich G, Boschero RA, Appel AS, Falkembach M, Monteiro M, da Silva PEA, Dailey LA, Dora CL. Tuberculosis treatment facilitated by lipid nanocarriers: can inhalation improve the regimen? Assay Drug Dev Technol. 2020;18:298–307.
Tang W, Zhang Y, Zhu G. Pulmonary delivery of mucosal nanovaccines. Nanoscale. 2022;14:263–76.
U.S. National Library of Medicine. Clinical Trials.gov. First-in-human study to evaluate the safety, tolerability, immunogenicity, and pharmacokinetics of LQ036 [EB/OL]. (2023-04-13) [2023-05-19] https://beta.clinicaltrials.gov/study/NCT04993443.
U.S. National Library of Medicine. Clinical Trials.gov. A phase 1 study of VX-522 in participants with cystic fibrosis (CF) [EB/OL]. (2023-05-01) [2023-05-04] https://clinicaltrials.gov/ct2/show/record/NCT05668741.
Acknowledgements
This work was supported by the National Science Foundation of China (No. 22075247), and the Zhejiang provincial Natural Foundation of China (No. LGF21C100001).
Figures were created with BioRender.com.
Author information
Authors and Affiliations
Contributions
QW was responsible for writing the manuscript, while corresponding author XS was responsible for conceptualizing the ideas, and XZ, DZ, RX, YC and KZ all made suggestions. All authors edited and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
We have included 10 figures (Figs. 5, 7, 8, 9, 10, 11, 12, 13, 14 and 15) from previously published literature with required copyright permission from the copyright owners. We have mentioned this in the manuscript with appropriate citations.
Competing interests
The authors declare that they have no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wan, Q., Zhang, X., Zhou, D. et al. Inhaled nano-based therapeutics for pulmonary fibrosis: recent advances and future prospects. J Nanobiotechnol 21, 215 (2023). https://doi.org/10.1186/s12951-023-01971-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12951-023-01971-7