Abstract
Background
Maternal probiotic supplementation has a promising effect on atopic dermatitis (AD) prevention in infancy. In the randomised controlled study, Probiotics in the Prevention of Allergy among Children in Trondheim (ProPACT), maternal probiotics reduced the cumulative incidence of AD in their offspring by 40% at 2 years of age. However, our understanding on how probiotics prevented AD is still limited, and the role of inflammatory proteins in infants following maternal probiotic supplementation is unclear. We hypothesised that maternal probiotics lowered pro-inflammatory proteins and increased anti-inflammatory proteins in their 2-year-old children as a mechanism of AD prevention. We aimed to explore this hypothesis and the association between these proteins and the presence of AD, severity of AD, and the degree of preventive effect of probiotics.
Methods
Plasma samples were collected from 2-year-old children (n = 202) during the ProPACT study, a randomised placebo-controlled trial of maternal probiotic supplementation. These samples were analysed for 92 inflammatory proteins using a multiplex proximity extension assay. Associations between inflammatory proteins and the presence and severity of AD, and the degree of preventive effect, was estimated individually using regression analysis and then collectively using unsupervised cluster analysis.
Results
Several proteins were observed to differ between the groups. The probiotic group had lower CCL11 and IL-17C, while children with AD had higher IL-17C, MCP-4, uPA, and CD6. Cytokine CCL20 and IL-18 had moderate correlation (r = 0.35 and r = 0.46) with the severity of AD. The cluster analysis revealed that children in the cluster of samples with the highest value of immune checkpoint receptors and inflammatory suppressor enzymes showed the greatest AD preventive effect from probiotics.
Conclusions
The proteins associated with both maternal probiotic supplementation and the presence and severity of AD warrant attention because of their potential biological relevance. Cluster analysis may provide a new insight when considering which subgroups benefit from probiotic supplementation. Larger studies are needed to confirm the results.
Trial registration number: The study was retrospectively registered at ClinicalTrials.gov (NCT00159523) on 12nd September 2005.
Similar content being viewed by others
Background
Allergic diseases have been increasing in prevalence worldwide [1]. Environmental factors such as industrialisation, modern lifestyle, and pollutants may play an important role in this increase [1, 2]. These changes are thought to have led to reduced exposure of microbiota in early life [3], and several studies have linked microbiota disruptions in the first months of life to the development of allergic diseases [4, 5]. Even with their increased prevalence [1], we have limited knowledge about effective preventive strategies for allergic diseases [6, 7]. Atopic dermatitis (AD), or eczema, is the most common allergy-related disease in childhood [2] affecting up to 1 in 3 children by the age of 8 in Europe [8]. The burden of AD can be significant due to sleep disruptions and risk of skin infections and effective strategies for prevention is limited, yet important [9].
Several clinical trials have found that probiotic supplementation around the time of birth may prevent AD [10, 11] especially when using combinations of strains and regimes that include pre- and postnatal supplementation [12]. However, our understanding of how probiotics prevent AD in childhood is still limited [10, 13], and systemic biomarkers may provide insights into the mechanism. Although probiotics are reported to reduce pro-inflammatory and increase anti-inflammatory serum biomarkers in adults [14], no previous study has investigated the effect of maternal probiotic supplementation on the level of proteins associated with inflammation in their offspring [15].
In the randomised placebo-controlled study, Probiotics in the Prevention of Allergy among Children in Trondheim (ProPACT), short-term administration of probiotic bacteria given to a nonselected population of pregnant women reduced the cumulative incidence of AD in their offspring by 40% at 2 years old [11]. We hypothesised that maternal probiotics reduced pro-inflammatory proteins and increased anti-inflammatory proteins in their 2-year-old children as a mechanism of AD prevention. Our primary aim was to explore whether probiotics influenced plasma inflammatory proteins in children at 2 years of age. As secondary aims, we investigated if individual proteins were correlated with the presence and severity of AD, and if the degree of preventive effect was associated with different inflammatory protein profiles.
Methods
Participants and sample collection
The ProPACT study followed 415 pregnant women randomised to receive probiotics or placebo milk from 36 weeks of gestation until 3 months post-delivery while breastfeeding [16, 17]. The pregnant women were recruited from a nonselected population, and a computer-generated randomisation sequence allocated them to probiotic or placebo milk. The probiotic milk corresponded to a daily dose of 5 × 1010 colony-forming units (CFU) Lactobacillus rhamnosus GG (LGG), 5 × 1010 CFU Bifidobacterium animalis subsp. lactis Bb-12 (Bb-12) and 5 × 109 CFU Lactobacillus acidophilus La-5 (La-5), whilst the placebo was fermented and pasteurised skim milk with similar taste and without probiotic bacteria. Information regarding demographics and risk factors for allergy-related diseases was obtained from questionnaires completed during pregnancy, and at the ages of 6 weeks, 1 year, and 2 years. A paediatrician examined all children at 2 years, and AD was defined using the U.K. working party’s diagnostic criteria for AD [18]. Additionally, children were encouraged to attend an examination by a trained nurse if they had an itchy rash for more than 4 weeks any time during the first year of life to ensure all cases were identified. The AD severity was assessed with the Nottingham Eczema Severity Score (NESS) [19].
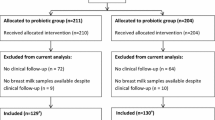
Children who attended the clinical examination and with available samples at 2 years were eligible for inclusion in the current study. Ultimately, 202 children were included, 101 from the probiotic group and 101 from the placebo group. All participating mothers signed a written consent. The study was approved by the Regional Committee for Medical Research Ethics in Central Norway (097–03) and registered at ClinicalTrials.gov (NCT00159523).
Plasma analyses
Heparin blood samples were collected from children at 2 years of age between December 2004 until April 2009 and diluted 1:1 with isotonic saline before plasma separation and storage at -80° C (further details in Additional file 1). Analysis of proteins were completed in October 2020.
Using the Olink® Target 96 Inflammation panel (Olink Proteomics, Uppsala, Sweden), 92 proteins associated with inflammation were analysed with a multiplex proximity extension (PEA) assay (complete list in Additional file 1: Table S1) [20]. The results were expressed as normalised protein expression (NPX) values which are arbitrary units on a Log2 scale, such that a one NPX unit increase corresponds to a doubling of the protein concentration for a given protein. As a relative quantification, the size of the NPX value can be compared within, but not between, proteins [21]. Different proteins with the same NPX value may still differ in their absolute concentrations.
Statistical analyses
The statistical analyses were performed using Stata/IC 17 (StataCorp) and RStudio (version R 4.1.3). Descriptive variables were presented as mean (standard deviation (SD)) for continuous variables, and frequency (percentage) for categorical variables. Differences between groups in the detectability of proteins were analysed with Fisher’s exact test for categorical data to compare the proportion of samples with detectable expression of proteins. In analyses comparing protein expression we included 64 proteins which were above the limit of detection (LOD) in at least 50% of samples. For samples with NPX values below the LOD for these 64 proteins, we still used the provided NPX value in the quantitative analyses, as recommended by Olink [22]. To explore whether maternal probiotics supplementation influenced individual plasma protein expression we used the Linear Models for Microarray Data (limma) package [23]. The results are presented with fold change and p-values. Pairwise Pearson or Spearman’s rank correlation was done to find which protein(s) that correlated to AD severity score by NESS.
We used unsupervised hierarchical clustering to identify plasma inflammatory profiles in the offspring. This analysis strategy results in information about clustering of both samples and proteins by identifying which samples are similar across the measured proteins, as well as which proteins are correlated with each other across samples. To distinguish between the clustering results for inflammatory protein expression of plasma samples from the children and 92 proteins measured, we use the term “sample clusters” and “groups of proteins” throughout the results and discussion. The cluster analysis was performed using Ward linkage in combination with squared Euclidean distances between samples and correlation distance between proteins [24], and was visualised using a heatmap produced by pheatmap package in R software and displaying hierarchical trees for both samples and proteins (Additional file 1: Fig. S1). Post cluster analysis and visual inspection of the hierarchical trees indicated four clusters of samples and three groups of proteins (see Additional file 1). To investigate whether maternal probiotic supplementation affected the overall inflammatory protein profile, we examined the association between sample clustering and randomisation group using Fisher’s exact test. Likewise, the association between the sample clusters and cumulative AD was assessed using Fisher’s exact test. The risk ratio (RR) of AD for children in the probiotic versus placebo group was also calculated within each sample cluster to determine if the degree of preventive effect differed between the overall inflammatory protein profile.
The expression of individual proteins was compared between the four sample clusters using linear regression (Additional file 1: Tables S5–S7) and the results are presented graphically (Fig. 2).
Results
A total of 202 plasma samples were included (Fig. 1). The probiotic group had more males and more often had siblings than placebo group. Consistent with the overall results from the ProPACT study, the probiotic group in these analyses had a lower cumulative incidence and prevalence of current AD at 2 years of age, as well as a slightly lower proportion with current asthma (Table 1).
Among the 92 proteins analysed, 28 were found to be below the LOD in ≥ 50% samples. Nine proteins were not detected in any samples, 14 proteins were detected in less than 10% of samples, and five were detected in between 11 to 50% of samples (Additional file 1: Table S1). There was no substantial difference in the proportion of samples with detectable expression between the probiotic and placebo groups (Additional file 1: Table S1).
The 64 proteins considered for the subsequent statistical analyses are presented in the Additional file 1: Table S2. Most proteins had lower expression in the probiotic group, including CCL11 (eotaxin-1) and interleukin-17C (IL-17C) which had p-values < 0.05 (Table 2 and Additional file 1: Table S3). Similarly, IL-17C, monocyte chemoattractant protein-4 (MCP-4), urokinase-type plasminogen activator (uPA), and cluster of differentiation 6 (CD6) had higher expression in children with AD (Table 2 and Additional file 1: Table S4).
There was a moderate positive correlation between AD severity (NESS score) and IL-18 with r = 0.35 (p = 0.043, 95% CI 0.010 – 0.613) and CCL20 with r = 0.46 (p = 0.007, 95% CI 0.138 – 0.687).
Using hierarchical cluster analysis, we identified four clusters of samples with closest similarities according to Ward linkage and squared Euclidean distance (Table 3). We found no clear evidence that probiotic supplementation influenced the clustering of samples (p = 0.420). On the other hand, a statistically significant difference in cumulative incidence of AD between clusters was found, ranging from 15% in cluster 3 to 42% in cluster 4 (p = 0.027, Table 3). The observed preventive effect of maternal probiotics supplementation differed between clusters, with cluster 1 and cluster 3 having reduced RR of getting AD in the probiotic group (Table 3). We observed that cluster 1 had the highest proportion of pets in the house, maternal history of atopy, as well as the lowest proportion with siblings and allergic sensitisation at 2 years.
The hierarchical clustering also identified three groups of proteins which closely correlated to each other (Table 4 and Fig. 2). Overall, group 1 was characterised by T cell surface proteins with immune checkpoint receptor (ICR) function and enzymes with anti-inflammatory effect. These proteins had highest expression in sample cluster 1 which in turn had the lowest proportion of children with allergic sensitisation and the lowest relative risk of AD in the probiotic group. Cluster 1 especially had significantly high expression of axis inhibition protein 1 (AXIN1), CD244, programmed death-ligand 1 (PD-L1), signal-transducing adaptor molecule-binding protein (STAMBP), and sirtuin-2 (SIRT2) (Fig. 2). Both protein group 2 and 3 consisted of mostly chemokines, cytokine receptors, and growth factors which many are observed to play role in AD. Sample cluster 2 had higher expression of most of these proteins in group 2 and 3 while also having the highest proportions of current AD and maternal smoking. In contrast, the lowest expression of group 2 and 3 proteins were found in sample cluster 4 which clinically had the highest frequency of cumulative AD in the children and atopy both in children and the family.
Discussion
In this study we have explored the role of multiple inflammatory proteins in the prevention of AD following maternal probiotic supplementation. We found that children in the probiotic group generally had lower expression of inflammatory proteins, especially CCL11 and IL-17C. The children with an AD diagnosis up to 2 years of age had higher expression of IL-17C, MCP-4, uPA, and CD6 whilst IL-18 and CCL20 may be moderately correlated with severity of AD in those children with AD. When considering the inflammatory protein profile collectively, we saw that the cluster of children with the greatest preventive effect following probiotic supplementation (sample cluster 1) also had higher expression of the protein group characterised by T cell surface proteins and enzymes with immunomodulatory functions (protein group 1).
Probiotics around the time of birth have been found to reduce the risk of AD both in the ProPACT study [11, 17] and meta-analyses [12], and the current study aimed to investigate if the preventive effect could be partially due to long term effects on the systemic inflammatory proteins of their offspring. Both CCL11 and IL-17C were observed to be lower in the probiotic group and they have previously been linked to AD, with the CCL11 playing an important role in AD severity [25]. The IL-17 cytokine family, which includes IL-17C, is produced by keratinocytes and is known to be overexpressed in AD skin lesions and serum [25,26,27]. While probiotics have been observed to reduce AD with suggested mechanism to be alterations of inflammatory markers in the breastmilk of the mothers [15], this is the first study to investigate the systemic inflammatory effect in offspring of mothers taking probiotic supplementation during pregnancy and while breastfeeding. A study in murine model observed that maternal probiotics suppressed the offspring’s IL-6, keratinocyte-derived cytokine (KC, also known as CXCL1), MCP-1, and IL-1β [28]. A small non-randomised and non-placebo-controlled study of 12-year-olds receiving probiotics did not find reduced plasma CCL11 or IL-17A (another member of the IL-17 family), yet reported reduced concentration levels of IL-12p40, IL-13, IL-15, IL-18, CCL2, and CCL24 [29]. Although these studies supported that probiotics may have an anti-inflammatory effect in the offspring, the changes were not observed in the same inflammatory biomarkers to those measured in our study and further research is needed.
In terms of associations between individual inflammatory proteins and the presence and severity of AD, we observed that higher expression of IL-17C, MCP-4, uPA and CD6 were seen in children with AD, and IL-18 and CCL20 were positively correlated with severity. Among those proteins in our study which associated with the presence of AD, IL-17C is expressed in AD lesions as described above, while MCP-4 is an eosinophil-specific chemotactic factor related to AD [30], uPA activity is linked to transepidermal water loss in dry AD skin [31] and CD6 is a T cell surface protein found to be overexpressed in AD skin [32]. Higher expression of both the IL-17 family cytokines and CD6 have previously been reported in adults with AD [25, 32], and MCP-4 has been associated with AD severity [30]. The correlation between severity and IL-18 and CCL20 is also consistent with other studies, with both observed to be related to severity in adults [33, 34] and IL-18 in older children [35]. Our findings suggest that this association may also be present in 2-year-old children, although another small study found no clear correlation between CCL20 and AD severity in 4-month-old infants [36].
Moving beyond the assessment of individual proteins for our primary aim, we also used hierarchical cluster analysis to examine if the overall inflammatory protein profile was associated with probiotic supplementation, the degree of preventive effect, or the presence of AD. The preventive effect of probiotic supplementation appeared to be greatest in sample cluster 1, which also included the children with a comparatively high proportion with family and maternal history of atopy. This is somewhat contradictory with the previous ProPACT study where the preventive effect was primarily seen among children without a family history of atopy [11]. Cluster 1 had the highest expression of protein group 1 which was characterised by high expression of ICRs such as PD-L1 and CD244, and inflammatory suppressor enzymes. ICRs trigger immunosuppressive signalling by suppressing autoreactive cells, which prevents excessive inflammation [37]. No previous studies have specifically discussed the roles of ICRs in AD in children, but it was observed that deficiencies in these proteins resulted in increased inflammation in mild AD in murine models [38]. Similarly, the AXIN1 enzyme has been associated with barrier dysfunction and higher AXIN1 concentration levels associated with lower AD risk [39]. The enzymes SIRT2 and STAMBP, which were also highest in sample cluster 1, suppress inflammation and have anti-inflammatory effects [40, 41]. Although sample cluster 1 had neither the highest expression of all anti-inflammatory nor the lowest expression of pro-inflammatory proteins, the presence and severity of AD is likely due to a balance between pro- and anti-inflammatory proteins [42], and it is difficult to separate the nuances of these relationships from our data. Furthermore, it is not possible to determine if the greater preventive effect seen in the probiotic group in cluster 1 represents an underlying inflammatory protein profile, alterations in the protein profile in early infancy, or if the inflammatory protein profile is a result of the AD prevention.
While the children in sample cluster 1 showed the greatest preventive effect of AD from probiotics, those in cluster 3 had the lowest prevalence of AD. This cluster consistently showed low expression of most of the measured proteins, especially tumour necrosis factor ligand superfamily member 14 (TNFSF14) which has previously been found to correlate with AD severity in adults [43]. On the other hand, the children in sample cluster 2 and 4 had higher risks of being diagnosed with AD, although with contrasting expression of inflammatory protein profiles. Overall, samples in cluster 2 had the highest expression of protein groups 2 and 3, and those in cluster 4 had the lowest expression. However, because there were very few samples in cluster 4, the results were interpreted with caution. Cluster 2 had particularly high expression of group 2 proteins which mostly consisted of pro-inflammatory cytokines found in AD [30].
The key strengths of this study are the double-blinded randomised design for probiotics intervention and novel use of the modern proteomics technologies and statistical analysis strategies to examine a wide range of inflammatory proteins in 2-year-old children. This study provides insight into the systemic inflammatory protein profile of 2-year-old children after maternal probiotic supplementation. Blood protein profiles after maternal probiotic supplementation in young children are scarce [14, 15, 44]. Using detailed clinical information based on validated diagnostic methods, we were able to consider the inflammatory protein profile in relation to the presence and severity of AD. Lastly, this study used hierarchical clustering which is a suitable and useful method for classifying large data with similarities [45]. This enabled us to compare protein profiles and the degree of preventative effect following probiotic supplementation.
Potential limitations of this study include the low level of detection of some proteins, the use of panel with a fixed set of proteins, and the relatively small samples size compared to the number of proteins analysed. Whilst the panel used in our study included several proteins previously related to AD and or type 2 inflammation, some of these could not be included in the analyses because of a low level of detection in a large number of samples. These included IL-4 and TSLP were detected in 1% and 3%, respectively, despite previous serum studies in young children reporting absolute concentrations above the LOD for the highly sensitive PEA technology used in the current study [25, 46]. Similarly, IL-5 and IL-13 were detected in only 4% and 3% of samples, respectively, and no samples had detectable levels of IL-33. The low levels of these proteins in our study may be due to sample dilution, the type of sample used (plasma), the children’s age [47], mild severity for most children with AD [48], and storage duration which might influence the concentrations found for some protein [49]. We note in particular, that some proteins which were reported as detectable in other studies of AD and healthy children but the proteins under LOD in our study also have been measured in peripheral blood mononuclear cells (PBMCs) [50] or serum [25, 51, 52] rather than plasma, or in plasma samples from older children [53,54,55]. In addition to the proteins below LOD, potentially interesting proteins were not available on the commercial panel, including some AD-related proteins (CCL17, CCL18, CCL22, and CCL27) and others associated with type 2 inflammation (IL-3, IL-9, IL-25, IL-31, and the eotaxins, CCL24 and CCL26) [56]. We cannot rule out that we would have found more differences or different patterns if these additional proteins could have been included, or if alternative collection, storage, and analysis methods allowed for quantification of the proteins found to have low levels of detection. Another limitation of this study is the comparison of multiple inflammatory markers in a relatively small number of participants in both the probiotics and placebo group. Due to the exploratory nature of the study, no statistical adjustment was performed for these multiple comparisons. The results should therefore be interpreted cautiously and still need to be confirmed in larger studies. Finally, we have no information about consumption of probiotic-containing food by mothers or infants between 3 months and 2 years of age when the samples were collected, however we have no reason to believe this would be different between the trial arms.
Conclusion
In this randomised placebo-controlled exploratory study, maternal perinatal probiotic supplementation resulted in mostly lower expression of the measured plasma inflammatory biomarkers in the offspring at 2 years of age, especially CCL11 and IL-17C, while IL-17C, MCP-4, uPA and CD6 correlated with the presence and CCL20 and IL-18 with the severity of AD. Additionally, children with the greatest preventive effect of probiotics had the highest expression of the group of proteins characterised by T cell surface proteins with ICR function and suppressor enzyme of inflammation. Cluster analysis may provide a new insight when considering which subgroups benefit from probiotic supplementation. Further larger studies are needed to confirm the results.
Availability of data and materials
Primary patient data can be shared upon reasonable request to the corresponding author.
Abbreviations
- AD:
-
Atopic Dermatitis
- AXIN1:
-
Axis inhibitor protein 1
- CCL:
-
C–C motif chemokine ligand
- CD:
-
Cluster of differentiation
- CFU:
-
Colony-forming units
- CI:
-
Confidence interval
- CXCL:
-
C-X-C motif chemokine ligand
- ICRs:
-
Immune checkpoint receptors
- IL:
-
Interleukin
- LGG:
-
Lactobacillus rhamnosus GG
- Limma :
-
Linear Models for Microarray Data
- LOD:
-
Limit of detection
- NESS:
-
Nottingham Eczema Severity Score
- NPX:
-
Normalised protein expression
- PBMCs:
-
Peripheral blood mononuclear cells
- PD-L1:
-
Programmed cell death ligand 1
- PEA:
-
Proximity extension assay
- ProPACT:
-
Probiotics in the Prevention of Allergy among Children in Trondheim
- RR:
-
Relative risk
- SD:
-
Standard deviation
- SIRT2:
-
NAD-dependent protein deacetylase sirtuin-2
- STAMBP:
-
Signal-transducing adaptor molecule-binding protein
- TSLP:
-
Thymic stromal lymphopoietin
- uPA:
-
Urokinase-type plasminogen activator
References
Doll RJ, Joseph NI, McGarry D, Jhaveri D, Sher T, Hostoffer R. Epidemiology of allergic diseases. Allergy and asthma: the basics to best practices. Cham: Springer International Publishing; 2019. p. 31–51.
Mu Z, Zhang J. The role of genetics, the environment, and epigenetics in atopic dermatitis. In: Chang C, Lu Q, editors. Epigenetics in allergy and autoimmunity. Singapore: Springer Singapore; 2020. p. 107–40.
Sbihi H, Boutin RC, Cutler C, Suen M, Finlay BB, Turvey SE. Thinking bigger: How early-life environmental exposures shape the gut microbiome and influence the development of asthma and allergic disease. Allergy. 2019;74(11):2103–15.
Arrieta MC, Stiemsma LT, Dimitriu PA, Thorson L, Russell S, Yurist-Doutsch S, et al. Early infancy microbial and metabolic alterations affect risk of childhood asthma. Sci Transl Med. 2015;7(307):307ra152.
Chatenoud L, Bertuccio P, Turati F, Galeone C, Naldi L, Chatenoud L, et al. Markers of microbial exposure lower the incidence of atopic dermatitis. Allergy. 2020;75(1):104–15.
Natsume O, Ohya Y. Recent advancement to prevent the development of allergy and allergic diseases and therapeutic strategy in the perspective of barrier dysfunction. Allergol Int. 2018;67(1):24–31.
Prescott SL, Tang M. Position statement: Allergy prevention in children. 2004.
Garcia-Aymerich J, Benet M, Saeys Y, Pinart M, Basagaña X, Smit HA, et al. Phenotyping asthma, rhinitis and eczema in MeDALL population-based birth cohorts: an allergic comorbidity cluster. Allergy. 2015;70(8):973–84.
Foisy M, Boyle RJ, Chalmers JR, Simpson EL, Williams HC. Overview of reviews the prevention of eczema in infants and children: an overview of Cochrane and non-Cochrane reviews. Evid Based Child Health. 2011;6(5):1322–39.
Cao L, Wang L, Yang L, Tao S, Xia R, Fan W. Long-term effect of early-life supplementation with probiotics on preventing atopic dermatitis: a meta-analysis. J Dermatolog Treat. 2015;26(6):537–40.
Dotterud CK, Storro O, Johnsen R, Oien T. Probiotics in pregnant women to prevent allergic disease: a randomized, double-blind trial. Br J Dermatol. 2010;163(3):616–23.
Sun S, Chang G, Zhang L. The prevention effect of probiotics against eczema in children: an update systematic review and meta-analysis. J Dermatolog Treat. 2021;33:1–11.
D’Elios S, Trambusti I, Verduci E, Ferrante G, Rosati S, Marseglia GL, et al. Probiotics in the prevention and treatment of atopic dermatitis. Pediatr Allergy Immunol. 2020;31(Suppl 26):43–5.
Milajerdi A, Mousavi SM, Sadeghi A, Salari-Moghaddam A, Parohan M, Larijani B, et al. The effect of probiotics on inflammatory biomarkers: a meta-analysis of randomized clinical trials. Eur J Nutr. 2020;59(2):633–49.
Kwok KO, Fries LR, Silva-Zolezzi I, Thakkar SK, Iroz A, Blanchard C. Effects of probiotic intervention on markers of inflammation and health outcomes in women of reproductive age and their children. Front Nutr. 2022;9: 889040.
Oien T, Storro O, Jenssen JA, Johnsen R. The impact of a minimal smoking cessation intervention for pregnant women and their partners on perinatal smoking behaviour in primary health care: a real-life controlled study. BMC Public Health. 2008;8:325.
Simpson MR, Dotterud CK, Storrø O, Johnsen R, Øien T. Perinatal probiotic supplementaion in the prevention of allergy related disease: 6 year follow up of a randomised controlled trial. BMC Dermatol. 2015;15:13.
Williams HC, Burney PG, Hay RJ, Archer CB, Shipley MJ, Hunter JJ, et al. The U.K. Working Party’s Diagnostic Criteria for Atopic Dermatitis. I. Derivation of a minimum set of discriminators for atopic dermatitis. Br J Dermatol. 1994;131(3):383–96.
Emerson RM, Charman CR, Williams HC. The Nottingham Eczema Severity Score: preliminary refinement of the Rajka and Langeland grading. Br J Dermatol. 2000;142(2):288–97.
Assarsson E, Lundberg M, Holmquist G, Bjorkesten J, Thorsen SB, Ekman D, et al. Homogenous 96-plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. PLoS ONE. 2014;9(4): e95192.
Olink. What is NPX? 2022. https://www.olink.com/question/what-is-npx/. Accessed 7 Mar 2022.
How is the limit of detection (LOD) estimated and how is this handled in the data analysis? 2021. https://www.olink.com/faq/how-is-the-limit-of-detection-lod-estimated-and-handled/#:~:text=Limit%20of%20detection%20(LOD)%20is,product%20validation%20for%20every%20panel. Accessed 28 Sep 2021.
Ritchie ME, Phipson B, Wu D, Hu Y, Law CW, Shi W, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43(7): e47.
Mooi E, Sarstedt M, Mooi-Reci I. Cluster analysis. Market research The process, data, and methods using stata 2018. p. 313–66. https://doi.org/10.1007/978-981-10-5218-7_9
Bakker DS, de Graaf M, Nierkens S, Delemarre EM, Knol E, van Wijk F, et al. Unraveling heterogeneity in pediatric atopic dermatitis: Identification of serum biomarker based patient clusters. J Allergy Clin Immunol. 2022;149(1):125–34.
Guttman-Yassky E, Krueger JG. IL-17C: A Unique Epithelial Cytokine with Potential for Targeting across the Spectrum of Atopic Dermatitis and Psoriasis. J Invest Dermatol. 2018;138(7):1467–9.
Leonardi S, Cuppari C, Manti S, Filippelli M, Parisi GF, Borgia F, et al. Serum interleukin 17, interleukin 23, and interleukin 10 values in children with atopic eczema/dermatitis syndrome (AEDS): association with clinical severity and phenotype. Allergy Asthma Proc. 2015;36(1):74–81.
Lu J, Lu L, Yu Y, Baranowski J, Claud EC. Maternal administration of probiotics promotes brain development and protects offspring’s brain from postnatal inflammatory insults in C57/BL6J mice. Sci Rep. 2020;10(1):8178.
Cabrera SM, Coren AT, Pant T, Ciecko AE, Jia S, Roethle MF, et al. Probiotic normalization of systemic inflammation in siblings of type 1 diabetes patients: an open-label pilot study. Sci Rep. 2022;12(1):3306.
Mizutani H. Cytokines in atopic dermatitis (Eczema). In: Ring J, Przybilla B, Ruzicka T, editors. Handbook of atopic eczema. Berlin: Springer, Berlin Heidelberg; 2006. p. 350–6.
Oszukowska M, Michalak I, Gutfreund K, Bienias W, Matych M, Szewczyk A, et al. Role of primary and secondary prevention in atopic dermatitis. Postepy Dermatol Alergol. 2015;32(6):409–20.
Saaf AM, Tengvall-Linder M, Chang HY, Adler AS, Wahlgren CF, Scheynius A, et al. Global expression profiling in atopic eczema reveals reciprocal expression of inflammatory and lipid genes. PLoS ONE. 2008;3(12): e4017.
Trzeciak M, Glen J, Bandurski T, Sokolowska-Wojdylo M, Wilkowska A, Roszkiewicz J. Relationship between serum levels of interleukin-18, IgE and disease severity in patients with atopic dermatitis. Clin Exp Dermatol. 2011;36(7):728–32.
Brunner PM, Guttman-Yassky E, Leung DY. The immunology of atopic dermatitis and its reversibility with broad-spectrum and targeted therapies. J Allergy Clin Immunol. 2017;139(4S):S65–76.
Wrzask M, Machura E, Mazur B, Chrobak E, Ziora K. Serum macrophage-derived chemokine and interleukin 18 concentrations are associated with disease severity in children with atopic dermatitis. Eur J Pediatr Dermatol. 2015;25(2):71–7.
Hulshof L, Overbeek SA, Wyllie AL, Chu M, Bogaert D, de Jager W, et al. Exploring immune development in infants with moderate to severe atopic dermatitis. Front Immunol. 2018;9:630.
Morita H, Saito H, Matsumoto K. Immune checkpoint molecules on ILC2s as potential therapeutic targets for allergic diseases. J Allergy Clin Immunol. 2022;149(1):60–2.
Elishmereni M, Fyhrquist N, Singh Gangwar R, Lehtimaki S, Alenius H, Levi-Schaffer F. Complex 2B4 regulation of mast cells and eosinophils in murine allergic inflammation. J Invest Dermatol. 2014;134(12):2928–37.
Mukherjee N. Role of breastfeeding duration, maternal smoking during pregnancy, and DNA-methylation for the risk of eczema. [Electronic Theses and Dissertations.]: University of Memphis; 2018.
Bednash JS, Johns F, Patel N, Smail TR, Londino JD, Mallampalli RK. The deubiquitinase STAMBP modulates cytokine secretion through the NLRP3 inflammasome. Cell Signal. 2021;79: 109859.
Sun K, Wang X, Fang N, Xu A, Lin Y, Zhao X, et al. SIRT2 suppresses expression of inflammatory factors via Hsp90-glucocorticoid receptor signalling. J Cell Mol Med. 2020;24(13):7439–50.
Narbutt J, Lesiak A, Sysa-Jedrzeiowska A, Zakrzewski M, Bogaczewicz J, Stelmach I, et al. The imbalance in serum concentration of Th-1- and Th-2-derived chemokines as one of the factors involved in pathogenesis of atopic dermatitis. Mediators Inflamm. 2009;2009: 269541.
Kotani H, Masuda K, Tamagawa-Mineoka R, Nomiyama T, Soga F, Nin M, et al. Increased plasma LIGHT levels in patients with atopic dermatitis. Clin Exp Immunol. 2012;168(3):318–24.
Brunner PM, He H, Pavel AB, Czarnowicki T, Lefferdink R, Erickson T, et al. The blood proteomic signature of early-onset pediatric atopic dermatitis shows systemic inflammation and is distinct from adult long-standing disease. J Am Acad Dermatol. 2019;81(2):510–9.
Arnau V, Mars S, Marin I. Iterative cluster analysis of protein interaction data. Bioinformatics. 2005;21(3):364–78.
Olink®. Olink® Inflammation Validation Data 2021. https://www.olink.com/content/uploads/2021/09/olink-inflammation-validation-data-v3.0.pdf. Accessed 11 Oct 2022.
Decker ML, Grobusch MP, Ritz N. Influence of age and other factors on cytokine expression profiles in healthy children-a systematic review. Front Pediatr. 2017;5:255.
He H, Del Duca E, Diaz A, Kim HJ, Gay-Mimbrera J, Zhang N, et al. Mild atopic dermatitis lacks systemic inflammation and shows reduced nonlesional skin abnormalities. J Allergy Clin Immunol. 2021;147(4):1369–80.
Enroth S, Hallmans G, Grankvist K, Gyllensten U. Effects of long-term storage time and original sampling month on biobank plasma protein concentrations. EBioMedicine. 2016;12:309–14.
Czarnowicki T, Gonzalez J, Shemer A, Malajian D, Xu H, Zheng X, et al. Severe atopic dermatitis is characterized by selective expansion of circulating TH2/TC2 and TH22/TC22, but not TH17/TC17, cells within the skin-homing T-cell population. J Allergy Clin Immunol. 2015;136(1):104-15.e7.
Berdat PA, Wehrle TJ, Kung A, Achermann F, Sutter M, Carrel TP, et al. Age-specific analysis of normal cytokine levels in healthy infants. Clin Chem Lab Med. 2003;41(10):1335–9.
Raes M, Scholtens PA, Alliet P, Hensen K, Jongen H, Boehm G, et al. Exploration of basal immune parameters in healthy infants receiving an infant milk formula supplemented with prebiotics. Pediatr Allergy Immunol. 2010;21(2 Pt 2):e377–85.
Timmons BW, Tarnopolsky MA, Snider DP, Bar-Or O. Immunological changes in response to exercise: influence of age, puberty, and gender. Med Sci Sports Exerc. 2006;38(2):293–304.
Dorn LD, Gayles JG, Engeland CG, Houts R, Cizza G, Denson LA. Cytokine patterns in healthy adolescent girls: heterogeneity captured by variable and person-centered statistical strategies. Psychosom Med. 2016;78(6):646–56.
Fujisawa T, Fujisawa R, Kato Y, Nakayama T, Morita A, Katsumata H, et al. Presence of high contents of thymus and activation-regulated chemokine in platelets and elevated plasma levels of thymus and activation-regulated chemokine and macrophage-derived chemokine in patients with atopic dermatitis. J Allergy Clin Immunol. 2002;110(1):139–46.
Haddad EB, Cyr SL, Arima K, McDonald RA, Levit NA, Nestle FO. Current and emerging strategies to inhibit type 2 inflammation in atopic dermatitis. Dermatol Ther (Heidelb). 2022;12(7):1501–33.
Acknowledgements
We are thankful to the parents and the participants of the study, the project assistants Guri Helmersen, Else Bartnes and Liv Ryan, the midwives of the Trondheim region for their help in the recruitment, paediatrician Rakel Berg who examined the children.
Funding
Open access funding provided by Norwegian University of Science and Technology. This study was funded by the Liaison Committee between the Central Norway Regional Health Authority and NTNU—Norwegian University of Science and Technology, and the Norwegian Research Council (grant reference number 2019/38881). Tine BA sponsored the study through supply and distribution of the study milk. Funding sources had no role in the study design, data collection, analysis, interpretation of the results, nor writing of the manuscript.
Author information
Authors and Affiliations
Contributions
DPZ: Conceptualization, Methodology, Writing—Original Draft, Data Curation, Formal analysis, Visualization; ADBR.: Writing—Review & Editing, Supervision, Funding acquisition, Interpretation of Results; VV: Writing—Review & Editing, Supervision, Interpretation of Results; TØ: Writing—Review & Editing, Supervision, Funding acquisition, Interpretation of Results; MRS: Writing—Review & Editing, Data Curation, Visualization, Supervision, Funding acquisition, Interpretation of Results. All authors read and approved the final manuscript except ADBR who passed away before the final version of manuscript was submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Regional Committee for Medical Research Ethics in Central Norway (097–03). The collected information was kept confidential and used only for research purposes. Informed consent to participate in the study was obtained from all the participants or their parent or legal guardian in the case of children under 18.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Additional documentation. Table S1. Percentage of detectable Normalised Protein eXpression (NPX) levels of proteins. Table S2. Descriptive statistics of blood plasma proteins included in the statistical analyses. Table S3. Limma results for Probiotics and Placebo. Table S4. Limma results for Cumulative AD and Non-AD in children. Table S5. Expressions of proteins in first group by sample clusters. Table S6. Expressions of proteins in second group by sample clusters. Table S7. Expressions of proteins in third group by sample clusters. Figure S1. Inflammatory proteins of 2-year-old children following maternal probiotics suplementation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zakiudin, D.P., Rø, A.D.B., Videm, V. et al. Systemic inflammatory proteins in offspring following maternal probiotic supplementation for atopic dermatitis prevention. Clin Mol Allergy 21, 5 (2023). https://doi.org/10.1186/s12948-023-00186-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12948-023-00186-3