Abstract
Background
Multiple sensitizations in early age have been reported to be a risk for development of asthma. This study evaluates the emergence and evolution of IgE to aeroallergens among a cohort of children with physician-diagnosed atopic dermatitis and/or showing food allergy symptoms and to examine the relation to asthma development.
Methods
Three-hundred and four children (median age 13.4 months at entry) with food allergy symptoms and/or atopic dermatitis without asthma at inclusion were analysed for IgE antibodies against food-, indoor- and outdoor-allergens and pet allergen components and correlated to the individuals’ outcome on asthma inception.
Results
At 2 years of follow-up, physician-diagnosed asthma was 19.7% (n = 49) and asthma diagnosed any time was 24% (n = 67). History of persistent cough and asthma of father, combination of milk- and wheat-allergy symptoms and dual sensitization to house dust mite and Japanese cedar were independent risk factors for asthma. Sensitization to dog was the most prevalent inhalant allergen at entry. Asthma children had a higher proportion of sensitization to dog, cat and horse allergens at entry compared with non-asthma children. Being sensitized to both food, house dust mite and pet allergens was strongly associated with asthma (p = 0.0006). Component resolved diagnosis for dog and cat allergens showed that IgE antibodies to Can f 1 and Fel d 1 was common even at very young age.
Conclusions
Early sensitization to inhalant allergens increases the risk of developing asthma as well as having milk and wheat allergy symptoms. Sensitization to dog, was common at an early age despite dog ownership. Sensitization to secretoglobin and lipocalins and less to serum albumins explained the pet sensitization.
Similar content being viewed by others
Background
The combination of atopic dermatitis and food allergy in young children reflect a strong risk for the development of asthma-like disease [1]. Symptomatic food allergy is especially associated with asthma among children with multiple or severe allergies [2]. Approximately one half of children with moderate to severe atopic dermatitis will have clinically relevant IgE antibodies to food allergens [3]. As atopic children grow older, the majority of allergen-specific IgE antibodies are directed against inhalant sources [4]. Sensitization to multiple allergens along with high IgE antibodies levels are features of severe atopic dermatitis in childhood. The knowledge that children with atopic dermatitis are at risk of developing asthma is poorly understood in general among health care providers. This is partially due to the fact that there is a wide variability in asthma development, 10–25%, in the risk estimate in longitudinal studies. A better recognition of the children at highest risk of developing asthma among the group of individuals with atopic dermatitis and food allergy is therefore needed.
At present, the identification of a child at high risk might not be possible with certainty. Current research points to some indicators including family history, history of asthma and allergies, early and severe sensitization to some food antigens and to aeroallergens and early viral infection associated with wheeze and adverse environmental exposures [5].
An atopic history of early life seems to be one of the key factors to identify an individual’s risk of persistent asthma. Illi et al. reported a cumulative prevalence of atopic dermatitis in the first 2 years of life of 21.5% among a general population of children [6]. When associated with allergic sensitization, atopic dermatitis was a good predictor of asthma at school age: the risk was not seen with atopic dermatitis in the absence of sensitization. Sensitization to hen’s egg seems to convey the greatest risk.
Birth cohorts in Europe, USA and Australia show that early sensitization and severe sensitization are risk factors for persistence of asthma [7–9]. Little is known about the timing and pattern of sensitization to individual aeroallergen in relation to the development of asthma in children with atopic dermatitis and food allergy. Sensitisation to animal and dust mite allergens are each a risk factor for the development of asthma. There seems to be a higher probability of wheeze for cat versus mite at a given IgE value among preschool children [10]. In the same study, summing IgE levels for mite, cat and dog at age 3 strengthened the risk for wheeze at age 5. Wisniewski et al. were not able to verify that multisensitization increase the risk for asthma [11]. Stoltz et al. have examined specific patterns of allergic sensitization in early childhood in relation to the risk of developing asthma and rhinitis [12]. They found that at 1 year of age only IgE antibodies to cat and dog were significantly associated with having asthma at age 6. Konradsen et al. have in a recent review stated that the prevalence of allergy to furry animal has been increasing in later years and allergy to cats, dogs or both is considered a major risk factor for the development of asthma and rhinitis [13].
We hypothesised that early onset of sensitization to aeroallergen in children with atopic dermatitis and/or showing food allergy symptoms beginning within the first years of life is important in order to identify those at most risk of developing asthma.
The aim of this study was to evaluate the emergence and evolution of IgE antibodies to aeroallergens among a cohort of children with physician-diagnosed atopic dermatitis and/or showing food allergy symptoms and to examine the relation to asthma development during a 2-year follow up.
Methods
This study was based on children who participated in the IRAM (Impact of Rhinitis on Atopic March; UMIN000004157) cohort. The study was a prospective five visit study during 2 years. Beside medical history, children were also recorded for atopic dermatitis, allergic rhinitis, parents’ allergy/asthma and smoking history and age, gender, height and weight. Inclusion criteria for this study were confirmed atopic dermatitis and/or suspicion of food allergy. Suspicion of food allergy was based on clinical history of food-induced symptoms and corresponding sensitization to the food. In uncertain cases oral food challenges were added to determine allergy to the food in question following the procedure for food allergy diagnosis in the EAACI and Japanese guidelines [14]. As oral food challenges were not done in all children, the term “food allergy symptom” will be used instead of “food allergy” throughout this study combining the groups of children with confirmed food allergy and of children with suspicion of food allergy, respectively. The diagnosis of atopic dermatitis was made by the study physicians based on the criteria by Hanifin and Rajka [15]. Blood samples were taken for specific IgE antibody determinations (Table 1). Physician diagnosis of asthma, (at each visit), was based on the Japanese Paediatric Guideline for the treatment and management of bronchial asthma [16]. A previously known diagnosis of asthma was criteria for exclusion.
The informed consent was signed by a legal guardian and the protocol was reviewed and approved by the ethics committee in Mie National Hospital, Japan.
Serum samples were analysed for IgE antibodies using the ImmunoCAP® system according to the manufacturer’s guidelines (Phadia AB, Uppsala, Sweden).
Statistical analyses were performed using the SAS® 9.3 (SAS Institute Inc., Cary, USA) and R 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria,). All tests were two-sided and using significance level of 5%. The Chi square test or, when appropriate, Fischer’s exact test were used to compare proportions. The Mann–Whitney test was used to compare specific IgE levels at entry and after 2 year follow up. The effect of demographic variables, medical history and sensitisation to allergen components were jointly investigated using a logistic regression model.
Results
Number of patients and prevalence figures are presented in Table 1. The average number of allergens that a child was sensitized against was at entry 3.0 (SD 2.4; range 0–13) and after 2 years, 5.1 (3.2; 0–13). Amongst the children that were diagnosed with bronchial asthma anytime during the course of the study (n = 67), the corresponding figure at entry was 3.8 (2.8; 0–13) whilst in the group of children (n = 236) that did not develop asthma the mean number of positive allergens was 2.8 (2.2; 0–13) (p = 0.019). Corresponding figures after 2 years were 6.2 (3.4; 0–13) and 4.7 (3.1; 0–13) respectively (p = 0.025). At entry, among the children diagnosed with asthma 6% were not sensitized to any of the tested allergens, 16% were monosensitized, 30% were sensitized to two up to a maximum of three allergens and 48% to more than three allergens. Corresponding numbers for the non-asthma group were 11, 20, 39 and 30% respectively.
Forty-nine out of the 67 (73%) children that were diagnosed with asthma anytime during the 24 months follow-up time period had an asthma diagnosis at the last visit.
Asthma were significantly associated with persistent cough (OR 3.7, 95% CI 1.75–7.80), asthma of father (2.39, 1.14–5.04) and milk allergy symptoms (2.48, 1.22–5.05), when using >0.1 kUA/L as cut-off. When using >0.34 kUA/L as cut-off, house dust mites in addition to the same factors as mentioned above were associated with higher risk of asthma diagnosis (Table 2).
Having a combination of milk and wheat allergy symptoms and house dust mite and cedar pollen sensitization had a likelihood of 38 and 45% respectively of being diagnosed with asthma anytime during follow-up (Table 3). Children with wheat allergic symptoms did not differ in their sensitization pattern at entry or at 2 year follow up compared to children with no wheat allergy symptoms. The results from the logistic regression were in line with this finding as sensitisation to Japanese cedar and wheat allergy symptoms were associated with increased probability of asthma diagnosis during follow-up, although they did not reach statistical significance (Table 2).
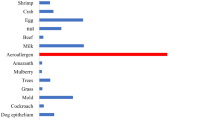
Children diagnosed with asthma at follow up were significantly more likely to be multi-sensitized to animals compared to the non-asthmatic children at entry (Fig. 1). Thirty-three percent of the asthma children were sensitized to two or more animals compared to 15% of the non-asthmatic children.
Sensitization to three different groups of allergens, pets, house dust mite and food, was analysed one by one or in combination in respect to asthma prevalence. Being sensitized to pet allergens and to house dust mite allergen independently of each other was associated with asthma (Fig. 2). Sensitization to all three groups in their combination was strongly associated with asthma (p = 0.0006).
Asthma prevalence in relation to sensitization to pets, HDM and food allergens. p Values were calculated when compared with the group without any sensitization, n.s. not significant. Not shown: Pets(+)HDM(−)Food(−), Pets(−)HDM(+)Food(−) and Pets(+)HDM(+)Food(−) because of too few number of observations in these combinations
Two hundred and ten children had atopic dermatitis at entry and 35 children were diagnosed with asthma at 2 years follow up. Totally 48 children were diagnosed with asthma anytime during the study. Mean number of positive allergens among these were 6.3 and 5.7 respectively. Corresponding figures in the non-asthmatic groups were 5.0 and 4.0 respectively. An increased risk of developing asthma (odds ratio = 1.22, CI 1.03–1.45, p = 0.02) was observed with increased number of positive allergens amongst the AD children.
Ninety-six percent (189/196) of the dog sensitized individuals had complete data set for measurements of IgE to Can f 1, Can f 2, Can f 3 and Can f 5 at entry. Overall sensitization to least one of these components was 37% (n = 69). Sensitization was highest for the lipocalins Can f 1/Can f 2 (30%, n = 56) followed by Can f 3 (15%, n = 29) and Can f 5 (13%, n = 25) (Fig. 3a). Fifteen percent were sensitized to at least two dog components whilst 7% were sensitized to all three components. Corresponding figures at 2 year follow up from 151 children with complete data set showed an overall sensitization to at least one component was 52% (n = 78). The most prevalent sensitization was found for Can f 1/Can f 2 (46%, n = 69) followed by Can f 3 (21%, n = 31) and Can f 5 (19%, n = 29) (Fig. 3b). At 2 year follow up, 23% were sensitized to at least two dog components whilst 11% were sensitized to all three components. Thirty-five (71%) of the asthma children were dog sensitized at entry. All these 35 children had complete data set for the dog components and 23 (47%) of them were positive to at least one of these components. In the group of non-asthmatic children after 2 years followed up 119 children were dog sensitized (62%) and 115 of them had complete data set. Fifty (29%) children were positive to at least one of the dog components.
Ninety-four percent (102/108) of the cat sensitized children had complete data set for cat components Fel d 1, Fel d 2 and Fel d 4 (cut-off = 0.1 kUA/L). Overall sensitization to at least one of these components was 59% (n = 69). Sensitization to Fel d 1 was found to be most prevalent (39%, n = 30) followed by Fel d 4 (29%, n = 26) and Fel d 2 (25%, n = 26) (Fig. 3c). Twenty-five percent were sensitized to at least two cat components whilst 11% were sensitized to all three components. Corresponding figures after 2 years follow up from 115 children with complete data set showed an overall sensitization to at least one of the components of 72%. Sensitization to Fel d 1 was most prevalent (52%, n = 60) followed by Fel d 4 (33%, n = 38) and Fel d 2 (24%, n = 28) (Fig. 3d). Here, 26% were sensitized to at least two cat components whilst 11% were sensitized to all three components. In the group of the 49 children that eventually were diagnosed with asthma 31 (63%) were cat sensitized. All these 31 children had complete data set and 19 (61%) were found to be positive to at least one of the components. Forty-three percent (84/193) of the non-asthmatic children were cat sensitized after 2 years followed up and they all had complete data set. In this group 64 (76%) of the children were positive to at least one of these components.
Discussion
In this study we examined predictors of asthma among children with atopic dermatitis and/or food allergy symptoms. We found that being sensitized to both house dust mite and cedar pollen or having both milk and wheat allergy symptoms were associated with asthma development during a 2 year follow up. A high proportion were sensitized to dogs and cats and mainly due to sensitization to secretoglobin and lipocalins and less due to serum albumins.
Sensitization to cat and dog components per se were not better predictors of asthma development than sensitization to cat and dog whole allergens. However, Wisniewski et al. found that both Fel d 1 and Fel d 4 were identified as predictors of wheeze among cat sensitized children with atopic dermatitis [11]. One explanation to the different findings could be differences in age in the two study population. Median age in the American study was 7.5 years compared to the median age of 1.5 year in our study [11]. This means that the asthma diagnosis will be based on a much shorter observational period compared to the study of Wisniewski et al.
Having milk and wheat allergy symptoms in combination was associated with increased risk of asthma diagnosis during the follow up. Eighty-eight percent of the included children had food allergy symptoms and 47 of them had this milk- and wheat allergy symptoms combination, of which 40% developed asthma within 2 years. In comparison, out of the children with a single milk or wheat allergy symptom 23 and 18% developed asthma respectively. We know from the literature that especially egg but also milk sensitization are associated with development of IgE to respiratory allergens [17–19]. Few prospective studies have studied the impact of wheat allergy/sensitization on asthma development. Illi et al. showed that early atopic sensitization played a major role for the prognosis of atopic dermatitis and sensitization to wheat showed the strongest association. The group with early atopic dermatitis and wheeze showed sensitization to wheat, cat, mite, soy and birch. Nilsson et al. found that 72% of children with a challenge verified wheat allergy had or have had milk allergy and 75% reported asthma symptoms pointing to a relationship between milk- and wheat-allergy with asthma [20]. The reason why symptoms for egg allergy did not single out as a risk factor for asthma in our study is probably due to that most of the children included in the study had egg allergic symptoms at entry. We observed in our study that sensitization to HDM, pets and food was higher in children with asthma compared with the non-asthmatics. Furthermore we could see that there was a higher prevalence of sensitization to these allergen groups in children with AD than in the non-AD children (79 vs 21%, data not shown). Wisniewski et al. [11] also reported that the prevalence of sensitization to these allergens increased considerable in AD-children less than 2 years of age up to 15 years of age. Even though the follow up period in our study period was limited to 24 months, from 1 year of age to the age of around 3 years we could also observed a clear increase in the sensitization prevalence for many of these allergens. However, the short follow up period and the young age of the children in our study limits the possibility to compare our study results with other longitudinal studies with long follow up periods.
Typical symptom patterns are important for the establishment of an asthma diagnosis. These include recurrent episodes of cough, wheeze, difficulty in breathing, chest tightness, and respiratory infections [21]. We found in our population that persistent cough was strongly associated with development of asthma. Cough is the most common cause for new visits in childhood ambulatory care and it is important to remember that this symptom is not pathognomonic for asthma and may occur as a result of several different conditions. Ongoing attempts are being made to simplify prediction tools for identifying children with wheeze or cough who are at risk for asthma. Pescatore et al. provided a simple, low-cost and non-invasive questionnaire based method to predict the risk of later asthma in symptomatic preschool children [22]. However, we do need objective biomarkers for diagnosing asthma in young children as cough and other symptoms may occur as a result of several different respiratory conditions. Being sensitized to both house dust mite and cedar pollen increased the risk significantly of developing asthma during the follow up period. A limitation of the study is that this finding is based on only eleven children sensitized at this early age and this finding has to be verified by others.
The high sensitization prevalence for dog was a surprise and no equivalent data has been found in the literature. This is surprisingly high as only 19% of the children were exposed to dog at home. One possible explanation is cross-reactions between bovine and pet albumins. However, Bos d 6 was positive in 23% of the children but Fel d 2 and Can f 3 were only positive in 9 and 8% respectively. This explanation could be partially true as we could document that monosensitisation to pet albumins decreased significantly over the study period, which might be an effect of development of milk tolerance. Instead the most likely explanation is that the majority of the animal sensitized individuals are genuinely sensitized to the secretoglobin (Fel d 1) and lipocalin (Can f 1). Eighteen percent were positive to the major dog component Can f 1 and 13% to Fel d 1, the major cat component already at entry. We have no similar data to compare this with but the picture looks very different from pet component pattern in older children. Bjerg et al. performed a population-based study of animal component sensitization, asthma and rhinitis in schoolchildren and found that 32% were sensitized to dog and 30% to cat [23]. Furthermore, only 5 and 4 of the children that developed asthma were sensitized to Can f 3 and Fel d 2 respectively, which gives a total different sensitization pattern to animal components. Simpson et al. have described patterns of IgE responses to multiple allergen components using latent variable modelling in association with different clinical symptoms [24]. They found that sensitization to the group with component from domestic pets was strongly associated with asthma. Uriatre and Sastre were able to associate IgE sensitization to the different animal molecules with asthma severity [25]. We could not verify this finding but found that if sensitized to two or more animals at an early age, you are more likely to develop asthma. This seems to be even more likely if you are also sensitized to house dust mite and food on the same time. However, our observation period was only 2 years, which is a drawback if studying asthma development in childhood.
Conclusions
We conclude that early sensitization to inhalant allergens increase the risk of developing asthma as well as having milk and wheat allergy symptoms. The most common inhalant allergens causing sensitisation was dog allergen, but prevalence and concentration remained stable over the 2 year follow up compared to house dust mite and cedar pollen. The dog and cat sensitisation was mainly explained by sensitisation to major allergens and not cross reactions to serum albumin.
Abbreviations
- Specific IgE:
-
specific immunoglobulin E
- SD:
-
standard deviation
- OR:
-
odds ratios
- kUA/L:
-
kilo units (arbitrary) per litre
- AD:
-
atopic dermatitis
References
Laan MP, Baert MR, Bijl AM, Vredendaal AE, De Waard-van der Spek FB, Oranje AP, Savelkoul HF, Neijens HJ. Markers for early sensitization and inflammation in relation to clinical manifestations of atopic disease up to 2 years of age in 133 high-risk children. Clin Exp Allergy. 2000;30:944–53.
Schroeder A, Kumar R, Pongracic JA, Sullivan CL, Caruso DM, Costello J, Meyer KE, Vucic Y, Gupta R, Kim JS, Fuleihan R, Wang X. Food allergy is associated with an increased risk of asthma. Clin Exp Allergy. 2009;39:261–70.
Eigenmann PA, Calza AM. Diagnosis of IgE-mediated food allergy among Swiss children with atopic dermatitis. Pediatr Allergy Immunol. 2000;11:95–100.
Fiocchi A, Pecora V, Petersson CJ, Dahdah L, Borres MP, Amengual MJ, Huss-Marp J, Mazzina O, Di Girolamo F. Sensitization pattern to inhalant and food allergens in symptomatic children at first evaluation. Ital J Pediatr. 2015;41:96.
Sly PD, Boner AL, Bjorksten B, Bush A, Custovic A, Eigenmann PA, Gern JE, Gerritsen J, Hamelmann E, Helms PJ, Lemanske RF, Martinez F, Pedersen S, Renz H, Sampson H, von Mutius E, Wahn U, Holt PG. Early identification of atopy in the prediction of persistent asthma in children. Lancet. 2008;372:1100–6.
Illi S, von Mutius E, Lau S, Nickel R, Gruber C, Niggemann B, Wahn U, Multicenter Allergy Study G. The natural course of atopic dermatitis from birth to age 7 years and the association with asthma. J Allergy Clin Immunol. 2004;113:925–31.
Peat JK, Salome CM, Woolcock AJ. Longitudinal changes in atopy during a 4-year period: relation to bronchial hyperresponsiveness and respiratory symptoms in a population sample of Australian schoolchildren. J Allergy Clin Immunol. 1990;85:65–74.
Rhodes HL, Thomas P, Sporik R, Holgate ST, Cogswell JJ. A birth cohort study of subjects at risk of atopy: twenty-two-year follow-up of wheeze and atopic status. Am J Respir Crit Care Med. 2002;165:176–80.
Sherrill D, Stein R, Kurzius-Spencer M, Martinez F. On early sensitization to allergens and development of respiratory symptoms. Clin Exp Allergy. 1999;29:905–11.
Simpson A, Soderstrom L, Ahlstedt S, Murray CS, Woodcock A, Custovic A. IgE antibody quantification and the probability of wheeze in preschool children. J Allergy Clin Immunol. 2005;116:744–9.
Wisniewski JA, Agrawal R, Minnicozzi S, Xin W, Patrie J, Heymann PW, Workman L, Platts-Mills TA, Song TW, Moloney M, Woodfolk JA. Sensitization to food and inhalant allergens in relation to age and wheeze among children with atopic dermatitis. Clin Exp Allergy. 2013;43:1160–70.
Stoltz DJ, Jackson DJ, Evans MD, Gangnon RE, Tisler CJ, Gern JE, Lemanske RF Jr. Specific patterns of allergic sensitization in early childhood and asthma & rhinitis risk. Clin Exp Allergy. 2013;43:233–41.
Konradsen JR, Fujisawa T, van Hage M, Hedlin G, Hilger C, Kleine-Tebbe J, Matsui EC, Roberts G, Ronmark E, Platts-Mills TA. Allergy to furry animals: new insights, diagnostic approaches, and challenges. J Allergy Clin Immunol. 2015;135:616–25.
Urisu A, Ebisawa M, Ito K, Aihara Y, Ito S, Mayumi M, Kohno Y, Kondo N. Japanese guideline for food allergy 2014. Allergol Int. 2014;63:399–419.
Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol Suppl (Stockh). 1980;92:44–7.
Hamasaki Y, Kohno Y, Ebisawa M, Kondo N, Nishima S, Nishimuta T, Morikawa A, Aihara Y, Akasawa A, Adachi Y, Arakawa H, Ikebe T, Ichikawa K, Inoue T, Iwata T, Urisu A, Ohya Y, Okada K, Odajima H, Katsunuma T, Kameda M, Kurihara K, Sakamoto T, Shimojo N, Suehiro Y, Tokuyama K, Nambu M, Fujisawa T, Matsui T, Matsubara T, Mayumi M, Mochizuki H, Yamaguchi K, Yoshihara S. Japanese pediatric guideline for the treatment and management of bronchial asthma 2012. Pediatr Int. 2014;56:441–50.
Illi S, von Mutius E, Lau S, Niggemann B, Gruber C, Wahn U, Multicentre Allergy Study G. Perennial allergen sensitisation early in life and chronic asthma in children: a birth cohort study. Lancet. 2006;368:763–70.
Lowe AJ, Abramson MJ, Hosking CS, Carlin JB, Bennett CM, Dharmage SC, Hill DJ. The temporal sequence of allergic sensitization and onset of infantile eczema. Clin Exp Allergy. 2007;37:536–42.
Lowe AJ, Hosking CS, Bennett CM, Carlin JB, Abramson MJ, Hill DJ, Dharmage SC. Skin prick test can identify eczematous infants at risk of asthma and allergic rhinitis. Clin Exp Allergy. 2007;37:1624–31.
Nilsson N, Sjolander S, Baar A, Berthold M, Pahr S, Vrtala S, Valenta R, Morita E, Hedlin G, Borres MP, Nilsson C. Wheat allergy in children evaluated with challenge and IgE antibodies to wheat components. Pediatr Allergy Immunol. 2015;26:119–25.
Papadopoulos NG, Arakawa H, Carlsen KH, Custovic A, Gern J, Lemanske R, Le Souef P, Makela M, Roberts G, Wong G, Zar H, Akdis CA, Bacharier LB, Baraldi E, van Bever HP, de Blic J, Boner A, Burks W, Casale TB, Castro-Rodriguez JA, Chen YZ, El-Gamal YM, Everard ML, Frischer T, Geller M, Gereda J, Goh DY, Guilbert TW, Hedlin G, Heymann PW, Hong SJ, Hossny EM, Huang JL, Jackson DJ, de Jongste JC, Kalayci O, Ait-Khaled N, Kling S, Kuna P, Lau S, Ledford DK, Lee SI, Liu AH, Lockey RF, Lodrup-Carlsen K, Lotvall J, Morikawa A, Nieto A, Paramesh H, Pawankar R, Pohunek P, Pongracic J, Price D, Robertson C, Rosario N, Rossenwasser LJ, Sly PD, Stein R, Stick S, Szefler S, Taussig LM, Valovirta E, Vichyanond P, Wallace D, Weinberg E, Wennergren G, Wildhaber J, Zeiger RS. International consensus on (ICON) pediatric asthma. Allergy. 2012;67:976–97.
Pescatore AM, Dogaru CM, Duembgen L, Silverman M, Gaillard EA, Spycher BD, Kuehni CE. A simple asthma prediction tool for preschool children with wheeze or cough. J Allergy Clin Immunol. 2014;133(111–8):e1–13.
Bjerg A, Winberg A, Berthold M, Mattsson L, Borres MP, Ronmark E. A population-based study of animal component sensitization, asthma, and rhinitis in schoolchildren. Pediatr Allergy Immunol. 2015;26:557–63.
Simpson A, Lazic N, Belgrave DC, Johnson P, Bishop C, Mills C, Custovic A. Patterns of IgE responses to multiple allergen components and clinical symptoms at age 11 years. J Allergy Clin Immunol. 2015;136:1224–31.
Uriarte SA, Sastre J. Clinical relevance of molecular diagnosis in pet allergy. Allergy. 2016;71:1066–8.
Authors’ contributions
TF and MN conceived the idea and designed this study. MN, MS, and YK collected the data and CJP, SN, and PD performed the statistical analyses. CJP and MPB drafted the manuscript and all co-authors gave input and agreed to the final submitted version. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank Mr. Yoshiki Segawa at Institute for Clinical Research, Mie National Hospital for his excellent technical assistance and Dr. Yuji Tohda at Department of Respiratory Medicine and Allergology, Kinki University School of Medicine for his general support for the study.
The authors would also like to thank the IRAM study investigators who actively participated in the study: Dr. Satoko Usui (Department of Otorhinolaryngology, Mie National Hospital), Dr. Ogura Kanae (Department of Pediatrics, Kyoto Yawata Hospital), Drs. Yutaka Suehiro and Yukiko Hiraguchi and Yuko Ebishima and Saeko Shimodera (Department of Pediatrics, Osaka Prefectual Medical Center for Respiratory and Allergic Deseases), Drs. Makoto Kameda and Yuri Takaoka and Tomoki Nishikido and Hiroko Yajima and Mineko Ikeoka (Department of Pediatrics, Osaka Prefectual Medical Center for Respiratory and Allergic Deseases), Drs. Hideo Ogura and Yukiko Ogura (Department of Pediatrics, Kochi National Hospital), Dr. Gyokei Murakami (Murakami Pediatric & Allergy Clinic), Drs. Toshimi Nakamura and Yoko Yamashita (Department of Pediatrics, Kanazawa Medical University Hospital), Dr. Yoko Kawasaki (Hotarugawa Clinic), Drs. Taku Oishi and Hiroaki Hisakawa and Akihiko Hisakawa and Hiroshi Wakiguchi (Department of Pediatrics, Kochi University), Dr. Hiroyasu Okahata (Department of Pediatrics, Kure Kyousai Hospital), Drs. Ikuo Okafuji and Shigeta Shimizu (Kobe City Medical Center General Hospital), Drs. Naomi Kondo and Eiko Matsui and Kazuo Kubota (Department of Pediatrics, Gifu University Hospital), Dr. Yutaka Morisawa (Kera Child & Allergy Clinic), Dr. Mitsuhiko Nambu (Department of Pediatrics, Tenri Hospital), Dr. Miki Takao (Department of Pediatrics, Takashige Memorial Hospital), Dr. Yoshinori Matsuwaki (Department of Otorhinolaryngology, Ota General Hospital), Drs. Yuichi Adachi and Toshiko Itazawa (Department of Pediatrics, Toyama University), Dr. Youichi Onoue (Onoue Pediatric Clinic), Dr Osamu Higuchi (Department of Pediatrics, Kurobe City Hospital), Dr. Yoko Adachi (Department of Pediatrics, Takaoka Minami Hospital), Dr. Akihiko Terada (Terada Kid’s Allergy & Asthma Clinic), Dr. Yoko Osawa (Department of Otorhinolaryngology, Tannan Regional Medical Center), Dr. Rentaro Abumi (Abumi Clinic), Drs. Tatsuya Fuchizawa and Junko Yamamoto (Saiseikai Takaoka Hospital), Drs. Motokazu Nakabayashi and Masaharu Kasei (Department of Pediatrics, Kouseiren Takaoka Hospital), Drs. Takanori Abe and Mayumi Sugimoto (Department of Pediatrics, Japanese Red Cross Kochi Hospital), Dr. Hisashi Kondo (Kondo Pediatrics Clinic), Drs. Akiko Toga and Nobuyuki Doichi (Department of Pediatrics, Fukui-ken Saiseikai Hospital).
Competing interests
Takao Fujisawa and Mizuho Nagao received lecture fees from Thermo Fisher Scientific, Siemens Healthcare Diagnostics, MSD KK, Glaxo SmithKline, and Kyorin Pharmaceutical. Magnus P Borres, Carl Johan Petersson, Satoshi Nakayama and Patrik Dykiel are employed by ThermoFisher Scientific, Uppsala, Sweden. All other authors have declared they have no competing interests.
Availability of data
Data supporting our findings is stored on a secure database in the Allergy Center and Department of Clinical Research, Mie National Hospital, Tsu, Mie, Japan. If further information is required, please contact us directly as it is currently secured to maintain confidentiality.
Ethics approval and consent to participate
Written consent was obtained from the parents. Ethics approval was given by the Ethics Committee of Mie National Hospital, Tsu, Japan (21-9).
Funding
This study was supported, in part, by unconditional grant from Kyorin Pharmaceutical Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Nagao, M., Borres, M.P., Sugimoto, M. et al. Sensitization to secretoglobin and lipocalins in a group of young children with risk of developing respiratory allergy. Clin Mol Allergy 15, 4 (2017). https://doi.org/10.1186/s12948-017-0061-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12948-017-0061-8