Abstract
Background
Venous thromboembolism represents the third most frequent acute cardiovascular syndrome worldwide. Its clinical manifestations are deep vein thrombosis and/or pulmonary embolism. Despite a considerable mortality, diagnosis is often missed.
Case presentation
We report the management of a female patient with high-risk pulmonary thromboembolism treated initially with thromboaspiration, complicated by embolus jailing in a patent foramen ovale. In this situation, left cardiac chambers and systemic circulation were jeopardized by this floating embolus.
Conclusions
High-risk pulmonary embolism requires reperfusion strategy but sometimes mechanical thromboaspiration may be not fully successful; transesophageal echocardiography led to a prompt diagnosis of this unexpected finding; in this very particular case, open surgery represented a bail-out procedure to avoid cerebral and systemic embolism.
Similar content being viewed by others
Background
Pulmonary embolism (PE) leads to variable symptoms, making the diagnosis challenging. Both American and European guidelines classify patients presenting with cardiac arrest or hemodynamic instability at high risk of mortality [1, 2]. Notably, in American guidelines, subjects with syncope or “thrombus in transit” at imaging are also considered at high risk. In this setting, reperfusion therapy is mandatory. This can be achieved by systemic thrombolysis or invasive approaches, such as catheter directed therapy or surgical embolectomy.
Patent foramen ovale (PFO) is defined as a small communication between right and left atrium at level of fossa ovale. This condition can be found in almost 25% of population, thus its correlation with cryptogenic stroke is still debated and no clear recommendations on its management exist [3].
Case presentation
A 55-year-old female patient was admitted to a peripheral hospital intensive care unit for type 1 respiratory failure complicated by shock and lactic acidosis (heart rate 106 bpm, blood pressure 60/30 mmHg, respiratory rate 25 breaths per minute and oxygen saturation 90% in air). No clinical signs of deep vein thrombosis (DVT) were observed. Blood exams revealed normal hemoglobin and red blood cell count, 12.000 white blood cells/µl, creatinine 1.8 mg/dl, NT-proBNP 19,800 pg/ml, D-dimer > 8000 ng/ml and lactates 8.6 mEq/l.
The patient had severe obesity [body mass index (BMI) 47 kg/m2] and no other cardiovascular risk factors. She complained effort-induced dyspnea in the last 2 days, and she was not on medications. The patient had an accidental fall with consequent cranial trauma in the previous month.
Urgent echocardiogram showed severe right ventricular systolic dysfunction and elevated systolic pulmonary artery pressure (80 mmHg). Unfractionated heparin infusion was started, and computed tomography pulmonary angiogram showed massive bilateral pulmonary embolism (Fig. 1A-B).
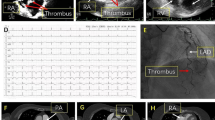
Urgent reperfusion strategy was mandatory due to hemodynamic instability, but systemic thrombolytic therapy was rejected because of recent head trauma; therefore, percutaneous thromboaspiration was performed. Although respiratory and hemodynamic parameters improved after the procedure, a transesophageal echocardiogram showed a new hyperechogenic mass in atrial septum, floating in both left and right atria and involving mitral valve (Fig. 2A-C, Additional file 1: Video 1, Additional file 2: Video 2, Additional file 3: Video 3, Additional file 4: Video 4 and Additional file 5: Video 5). The patient was immediately transferred to “Ospedale del Cuore” cardiac surgery department to remove the mass and avoid paradoxical embolism. During the intervention, a worm-shaped thrombus (10 × 1 cm) jailed in a 2 cm wide PFO was observed (Fig. 3A-B); consequently, thrombus was removed and PFO sutured.
A-C Transesophageal echocardiogram; inverted four chamber midesophageal scan (A-B) shows dilated right chambers and a thrombus involving left atrium, right atrium and mitral valve; short axis midesophageal scan (C) shows thrombus crossing the interatrial septum. AV = aortic valve. IA = interatrial septum. LA = left atrium. MV = mitral valve. RA = right atrium. Th = thrombus
Discussion and conclusions
In our case, PFO was discovered accidentally because of a large embolus was trapped inside it. This phenomenon could be facilitated by elevated right cardiac chambers pressure and mechanical thromboaspiration, but it is unclear whether to consider it a procedural complication or a new embolic manifestation. In this case, cardiac surgery was pursued due to high systemic and cerebral embolization risk.
Left popliteal vein thrombosis was found at ultrasound performed after the surgical intervention. The patient was weaned from inotropes and vasopressor after 1 week and discharged after 1 month with mild right ventricular systolic dysfunction and moderate pulmonary hypertension. Direct oral anticoagulant and home oxygen therapy was prescribed. She is currently on follow-up for chronic thromboembolic pulmonary hypertension (CTEPH) management.
High-risk pulmonary embolism is a life-threatening condition that must be managed with reperfusion strategy by medical or invasive approaches. Mechanical thromboaspiration could be complicated by incomplete emboli removal. In this case, a residual thrombus jailed in a PFO was successfully removed by a surgical procedure.
Availability of data and materials
All data generated or analysed during this study are included in this published article (and its supplementary information files).
Abbreviations
- BMI:
-
Body mass index
- CTEPH:
-
Chronic thromboembolic pulmonary hypertension
- DVT:
-
Deep vein thrombosis
- PAPs:
-
Systolic pulmonary artery pressure
- PE:
-
Pulmonary embolism
- PFO:
-
Patent foramen ovale
References
Konstantinides SV, Meyer G. The 2019 ESC Guidelines on the Diagnosis and Management of Acute Pulmonary Embolism. Eur Heart J. 2019;40(42):3453–5.
Rivera-Lebron B, McDaniel M, Ahrar K, et al. Diagnosis, Treatment and Follow Up of Acute Pulmonary Embolism: Consensus Practice from the PERT Consortium. Clin Appl Thromb. 2019;25:1076029619853037.
Pristipino C, Sievert H, D’Ascenzo F, et al. European position paper on the management of patients with patent foramen ovale. General approach and left circulation thromboembolism. EuroIntervention. 2019;40(38):3182–95.
Acknowledgements
We aknowledge the contribution of our colleagues from Hospital of Livorno (Tuscany, Italy), for referring the patient to our hospital and giving some important information to manuscript drafting.
Disclosures
Authors have no disclosure to declare.
Funding
Authors received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AR and FN collected patient’s data and cardiovascular imaging (ultrasound and fresh embolus) and drafted the manuscript; TG performed surgical procedure to remove the embolus and repair the POF; RA performed thromboaspiration intervention; BF and PR admitted the patient to intesive care unit and decided initial management; CP and EMP provided manuscript quality check; SS performed TEE and recorded ultrasound images; MS and SB supervised all the work. All authors approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The patient signed a written consent to publish this case report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Video 1. Inverted four chamber midesophageal scan. Anenlarged right ventricle and a floating thrombus between the right atrium andleft atrium can be observed.
Additional file 2: Video 2. Short axis midesophageal scan. A floatingthrombus, crossing the interatrial septum, can be observed.
Additional file 3: Video 3. Four chamber midesophageal scan. A thrombusinvolving the mitral valve can be observed.
Additional file 4: Video 4. Two chamber midesophageal scan. A thrombusinvolving the mitral valve can be observed.
Additional file 5: Video 5. 3D transesophageal echocardiogram showing thefloating thrombus.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rizza, A., Negro, F., Gasbarri, T. et al. Life-threatening paradoxical thromboembolism in a patient with patent foramen ovale. Cardiovasc Ultrasound 20, 28 (2022). https://doi.org/10.1186/s12947-022-00298-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12947-022-00298-x