Abstract
Purpose
This study was a quality-control study of resting and exercise Doppler echocardiography (EDE) variables measured by 19 echocardiography laboratories with proven experience participating in the RIGHT Heart International NETwork.
Methods
All participating investigators reported the requested variables from ten randomly selected exercise stress tests. Intraclass correlation coefficients (ICC) were calculated to evaluate the inter-observer agreement with the core laboratory. Inter-observer variability of resting and peak exercise tricuspid regurgitation velocity (TRV), right ventricular outflow tract acceleration time (RVOT Act), tricuspid annular plane systolic excursion (TAPSE), tissue Doppler tricuspid lateral annular systolic velocity (S’), right ventricular fractional area change (RV FAC), left ventricular outflow tract velocity time integral (LVOT VTI), mitral inflow pulsed wave Doppler velocity (E), diastolic mitral annular velocity by TDI (e’) and left ventricular ejection fraction (LVEF) were measured.
Results
The accuracy of 19 investigators for all variables ranged from 99.7 to 100%. ICC was > 0.90 for all observers. Inter-observer variability for resting and exercise variables was for TRV = 3.8 to 2.4%, E = 5.7 to 8.3%, e’ = 6 to 6.5%, RVOT Act = 9.7 to 12, LVOT VTI = 7.4 to 9.6%, S’ = 2.9 to 2.9% and TAPSE = 5.3 to 8%. Moderate inter-observer variability was found for resting and peak exercise RV FAC (15 to 16%). LVEF revealed lower resting and peak exercise variability of 7.6 and 9%.
Conclusions
When performed in expert centers EDE is a reproducible tool for the assessment of the right heart and the pulmonary circulation.
Similar content being viewed by others
Background
Exercise Doppler echocardiography (EDE) is standard practice for the evaluation of patients with coronary artery disease. The procedure is now increasingly used for the assessment of the right heart and the pulmonary circulation [1,2,3,4,5]. Echocardiography of the right heart mainly relies on estimates of right chambers dimensions (diameters/areas/volumes) and function (i.e. fractional area change, tricuspid annular plane systolic excursion (TAPSE) and of tissue Doppler–derived tricuspid lateral annular systolic velocity (S’) [2, 3]. Furthermore it estimates the components of the pulmonary vascular resistance equation, that is pulmonary artery pressure (PAP) from the maximum tricuspid regurgitation velocity (TRV), or the right ventricular outflow tract (RVOT) acceleration time (Act) of PA flow, wedged PAP from the ratio of transmitral flow E and mitral annulus e’ waves and cardiac output (CO) from the left ventricular outflow tract (LVOT) aortic flow. The RIGHT Heart International NETwork (RIGHT-NET) study was designed to comprehensively define limits of normal in right heart function and pulmonary circulation hemodynamics during EDE (diagnostic value) and to investigate the impact of abnormal responses on clinical outcome in individuals with overt or at risk of developing pulmonary hypertension (prognostic value) [6, 7]. The present report aims to provide a quality control analysis of left, right heart and pulmonary circulation resting and EDE measurements among 19 echocardiography laboratories with proven experience participating in the RIGHT-NET study [6, 7].
Methods
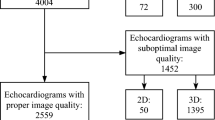
The echocardiography Core laboratory of the Institute of Clinical Physiology-CNR in Pisa (LG) coordinated the quality control procedure of all investigators at different centres participating in the RIGHT-NET study. Each center designated one operator that performed or reported at least 100 stress echocardiography studies per year. All readers were certified by national and/ or international societies. The quality control process was designed to be simple, reproducible and sustainable. The echocardiography Core laboratory issued a User Manual with a detailed description on how to measure each parameter, according to the most recent American and European Recommendations and Guidelines [8,9,10,11]. The User Manual was sent to all Participating Centers including the reference for transthoracic echocardiography assessment. All participating centers followed the recommended standard operational procedures in terms of data storage (data format, transfer procedure), and data processing (software used and measurement procedures). All operators performing and reading echocardiographic exams adhered to the quality control protocol. The echocardiography Core laboratory sent ten complete echocardiographic examinations in DICOM format through a safe file sharing platform (Fig. 1). All participating investigators were invited by email to join the platform, which was protected by user-specific passwords. The platform includes also detailed instructions on how to start the training and allows downloading and uploading of external files. Each reader was blinded to core laboratory measurements and to clinical history of the patients. All images and videos were completely anonymized to protect patients’ confidentiality’, in compliance with the EU’s General Data Protection Regulation 2018 [6].
Reading sessions
The echocardiography core laboratory randomly selected 10 cases including healthy subjects and at least one group of patients with overt and/or at risk of pulmonary hypertension (PH), according to clinical classification of PH (Table 1) [12]. Echocardiographic examinations were performed with commercially available equipment on all subjects (Vivid E9, GE Healthcare, Milwaukee, WI, USA). Data were collected on patients undergoing EDE on a semi-recumbent cycle ergometer with an incremental workload of 25 W every 2 min up to the symptom-limited maximal tolerated workload including resting, 50 W, peak stress and recovery acquisition, as previously described [6]. All operators directly measured the requested parameters by uploading the same ten cases from the web platform to their echocardiography machine. The DICOM format enabled to perform assessment of variables in the respective centres. All operators were then asked to enter their measurements in a dedicated excel file, which was then sent to the Coordinating Center for analysis. Table 2 provides the list of the left and the right heart parameters measured by all operators. The gold standard value for each measurement was established by the values measured by the echocardiography Core laboratory, according to the recommendations for echocardiographic assessment of the left and right heart by the American Society of Echocardiography/European Association of Cardiovascular Imaging [8,9,10,11].
Statistical analysis
Statistical analysis was performed using standard software (MedCalc version 14.8.1, MedCalc Software Ltd., Belgium; SPSS version 20.0, SPSS, Inc., Chicago, IL). Continuous variables were described by mean values ± standard deviation (SD). Normal distribution of the continuous values was assessed by the Kolmogorov-Smirnov test. Accuracy (in %) for each observer was estimated by comparison with the reference standard (core lab reading). Intra-class correlation coefficient (ICC) was calculated along with the 95% confidence interval, in order to quantify the reliability of measurement process. An ICC of > 0.8 indicated good agreement, ICC > 0.9 indicated excellent agreement with the core lab. Inter-observer variability among 19 observers were examined for resting and peak exercise TRV, RVOT Act, TAPSE, S’, right ventricular fractional area change (RV FAC), LVOT velocity time integral (VTI), mitral early inflow pulsed wave Doppler velocity (E), early diastolic mitral annular lateral and septal velocity by TDI (e’), left ventricular ejection fraction (LVEF). Data are presented as mean of the absolute and relative differences (in %) between measurements of all nineteen observers, and ICC for each single parameter was calculated along with the 95% confidence interval.
Intra-observer agreement was tested in 2 observers who volunteered to repeat the measurement session on 2 separate days and ICC was calculated.
Results
Nineteen observers completed all reading sessions. Figure 2 shows a summary of the accuracy (in %) of each center compared with the gold standard core lab for all parameters at rest and at peak of exercise. The average accuracy of 19 readers for all parameters was excellent in about 99.8% (range from 99.7 to 100%) (Table 3). ICC was > 0.9 for all observers. The average agreement of the 19 readers for all parameters was excellent (ICC = 0.98). Therefore there was no need to conduct personal feed-back and a second slot of measurements for anyone. Moreover the average agreement among readers remained excellent at rest and at peak exercise for all measurements (ICC = 0.98 and 0.99, respectively) (Table 4). Inter-observer variabilities among all observers for main exercise TTE measurements were reported in Table 5. Close inter-observer variabilities were found for both resting and peak exercise TRV (3.8 and 2.4%) (ICC = 0.97 and 0.98), RV S’ (2.9% for both) (ICC = 0.95 for both), E (5.7 and 8.3%) (ICC = 0.99 and 0.98) and e’ (6 and 6.5%) (ICC = 0.97 for both). Inter-observer variabilities of the RVOT Act and LVOT VTI were of 9.7% (ICC = 0.95) and 7.4% (ICC = 0.98) at rest, 12% (ICC = 0.92) and 9.6% (ICC = 0.97) at peak exercise, respectively. TAPSE showed less resting (5.3%) (ICC = 0.97) than peak exercise variability (8%) (ICC = 0.95). LVEF revealed lower resting and peak exercise mean relative differences of 7.6 and 9% (ICC = 0.99 and 0.98), respectively. Moderate inter-observer variability was found for resting and peak exercise RV FAC (15 and 16%, respectively) (ICC = 0.82 and 0.80) (Table 5).
The intra-observer quality control analysis revealed an excellent ICC of 0.97 (95% Confidence Interval: 0.96 to 0.99). All ICC > 0.95 remained excellent at rest and at peak exercise for all measurements, except for RV FAC (ICC = 0.85 and 0.82, respectively). Each ICC showed p value < 0.0001.
Discussion
Before any acquisition of pooling echocardiographic data for research and clinical applications, a process of quality control and reading harmonization measurements should be undertaken [13,14,15,16]. The present results demonstrate that a rigorously designed protocol with a strong focus on quality assurance and certification can yield very strong ICC and limited variability among the 19 participant experienced centers to a large prospective EDE study of the right heart and the pulmonary circulation.
Previous studies
The inter-observer variability during EDE right heart and pulmonary circulation studies may be not negligible. Few such studies have been previously reported and all were mono-centric [3, 17]. Argiento et al. reported in 124 healthy subjects (62 women and 62 men; age 37 ± 13 yrs) (single center study) an inter-observer variability for pulmonary artery systolic pressure (PASP) and cardiac output (CO) estimates of 1.9 and 4.9% at rest, and 7.9 and 13.9% at maximum exercise, respectively [18]. D’Alto et al. reported in 90 healthy subjects (45 male, mean age 39 ± 13 years) inter-observer variabilities between two readers at rest and peak exercise of 1.9 and 7.9% for PASP, 4.9 and 13.9% for stroke volume, 2.6 and 6.8% for TAPSE, and 5.4 and 8.7% for S′, respectively [19]. Kusunose et al. reported in a subgroup of 15 randomly selected subjects with isolated moderate to severe mitral regurgitation a close inter- and intra-observer variability for resting TAPSE (8.8%) and exercise TAPSE (9.5%) [20]. As these data remain limited, more validation appeared necessary for a multi-centric study like the RIGHT-NET.
Uniqueness of the present study and clinical implications
To the best of our knowledge, this is the largest EDE multicenter study that comprehensively provides a detailed quality control analysis of both the right heart and the pulmonary circulation measurements. One major finding was that the accuracy and agreement were remarkably high among 19 experienced investigators, with no significant differences between resting and exercise measurements. These results provide a valid evidence of reliability of TRV, E/e’ ratio, LVOT VTI and LVEF during exercise. The inter-observer variability of RVOT Act was higher than that of TRV. RVOT Act measurements were collected during exercise, in keeping with a recent report advocating its combination with TRV for the assessment of the pulmonary pressures both at rest and during exercise [21]. The interest of this combination is that the feasibility rate of RVOT Act may be higher than that of TRV [22]. Furthermore our findings suggested that exercise TAPSE and S′ may be used as reproducible measures of the RV longitudinal systolic function. Larger resting and exercise variability of RV FAC may be caused by plane-dependency and reliance on a complex definition of the RV endocardial border [23].
Study limitations
Few study limitations need to be discussed. First, the present study did not validate the echocardiographic measurements against invasive gold standard evaluation of the pulmonary circulation (PAP, wedged PAP and cardiac output), and right ventricular function (indices derived from pressure-volume loops). Second, accuracy and precision were defined by comparison only with the core laboratory measurements. In this regard, it was not logistically possible to repeat the echocardiographic examination of the same patient in each participating center. Third, the study results could have been potentially influenced by the quality images acquired only by the echocardiography core laboratory. For this reason we randomly selected 10 cases with different clinical conditions from a large database to avoid possible bias of selection of best images. Fourth, the number of patients studied was relatively small (n = 10). However, each of the 19 participating centers provided a total of 35 left and right heart echo-Doppler variables at rest, peak exercise and after 5 min of recovery.
Conclusions
When protocols for acquisition and analysis are provided upfront and in experienced echocardiography laboratories EDE represents a reproducible tool to comprehensively assess the right heart and pulmonary circulation. This quality control study represents a solid bedrock for future RIGHT-NET studies, aiming to evaluate the diagnostic and prognostic role of EDE in the clinical settings of patients with cardiorespiratory diseases.
Availability of data and materials
The datasets analysed during the current study are available from the corresponding author on reasonable request.
References
Lewis GD, Bossone E, Naeije R, Grünig E, Saggar R, Lancellotti P, Ghio S, Varga J, Rajagopalan S, Oudiz R, Rubenfire M. Pulmonary vascular hemodynamic response to exercise in cardiopulmonary diseases. Circulation. 2013;128:1470–9.
Naeije R, Saggar R, Badesch D, Rajagopalan S, Gargani L, Rischard F, Ferrara F, Marra AM, D’ Alto M, Bull TM, Saggar R, Grünig E, Bossone E. Exercise-induced pulmonary hypertension. Translating pathophysiological concepts into clinical practice. Chest. 2018;154(1):10–5.
Rudski LG, Gargani L, Armstrong WF, Lancellotti P, Lester SJ, Grunig E, D’Alto M, Aneq MA, Ferrara F, Saggar R, Saggar R, Naeije R, Picano E, Schiller NB, Bossone E. Stressing the cardiopulmonary vascular system: the role of echocardiography. JASE. 2018;31(5):527–50.
Bossone E, D'Andrea A, D'Alto M, Citro R, Argiento P, Ferrara F, Cittadini A, Rubenfire M, Naeije R. Echocardiography in pulmonary arterial hypertension: from diagnosis to prognosis. J Am Soc Echocardiogr. 2013;26(1):1–14.
Ferrara F, Gargani L, Ostenfeld E, D'Alto M, Kasprzak J, Voilliot D, Selton-Suty C, Vriz O, Marra AM, Argiento P, Stanziola AA, Cittadini A, D'Andrea A, Bossone E. Imaging the right heart pulmonary circulation unit: insights from advanced ultrasound techniques. Echocardiography. 2017 Aug;34(8):1216–31.
Ferrara F, Gargani L, Armstrong WF, Agoston G, Cittadini A, Citro R, D’ Alto M, D’ Andrea A, Dellegrottaglie S, De Luca N, Di Salvo G, Ghio S, Grünig E, Guazzi M, Kasprzak JD, Kolias TJ, Kovacs G, Lancellotti P, La Gerche A, Limongelli G, Marra AM, Moreo A, Ostenfeld E, Pieri F, Pratali L, Rudski LG, Saggar R, Saggar R, Scalese M, Selton-Suty C, Serra W, Stanziola AA, Voilliot D, Vriz O, Naeije R, Bossone E. The Right Heart International Network (RIGHT-NET): Rationale, Objectives, Methodology, and Clinical Implications. Heart Fail Clin. 2018;14(3):443–65.
Bossone E, Gargani L. The RIGHT Heart International NETwork (RIGHT-NET): A Road Map Through the Right Heart-Pulmonary Circulation Unit. Heart Failure Clin. 2018;14(3):xix:xx.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Popescu BA, Waggoner AD. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29(4):277–314.
Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713.
Lancellotti P, Pellikka PA, Budts W, Chaudhry FA, Donal E, Dulgheru R, Edvardsen T, Garbi M, Ha JW, Kane GC, Kreeger J, Mertens L, Pibarot P, Picano E, Ryan T, Tsutsui JM, Varga A. The clinical use of stress echocardiography in non-Ischaemic heart disease: recommendations from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr. 2017 Feb;30(2):101–38.
Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, Ghofrani A, Gomez Sanchez MA, Hansmann G, Klepetko W, Lancellotti P, Matucci M, McDonagh T, Pierard LA, Trindade PT, Zompatori M, Hoeper M, Aboyans V, Vaz Carneiro A, Achenbach S, Agewall S, Allanore Y, Asteggiano R, Paolo Badano L, Albert Barberà J, Bouvaist H, Bueno H, Byrne RA, Carerj S, Castro G, Erol Ç, Falk V, Funck-Brentano C, Gorenflo M, Granton J, Iung B, Kiely DG, Kirchhof P, Kjellstrom B, Landmesser U, Lekakis J, Lionis C, Lip GY, Orfanos SE, Park MH, Piepoli MF, Ponikowski P, Revel MP, Rigau D, Rosenkranz S, Völler H, Luis ZJ. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the joint task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67–119.
Pellikka PA, Nagueh SF, Elhendy AA, Kuehl CA, Sawada SG. American Society of Echocardiography recommendations for performance, interpretation, and application of stress echocardiography. J Am Soc Echocardiogr. 2015;20:1021–41.
Popescu BA, Stefanidis A, Nihoyannopoulos P, Fox KF, Ray S, Cardim N, Rigo F, Badano LP, Fraser AG, Pinto F, Zamorano JL, Habib G, Maurer G, Lancellotti P, Andrade MJ, Donal E, Edvardsen T, Varga A. Updated standards and processes for accreditation of echocardiographic laboratories from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2014;15(7):717–27.
Patton DM, Enzevaie A, Day A, Sanfilippo A, Johri AM. A quality control exercise in the echo laboratory: reduction in inter-observer variability in the interpretation of pulmonary hypertension. Echocardiography. 2017 Dec;34(12):1882–7.
Armstrong AC, Ricketts EP, Cox C, Adler P, Arynchyn A, Liu K, Stengel E, Sidney S, Lewis CE, Schreiner PJ, Shikany JM, Keck K, Merlo J, Gidding SS, Lima JA. Quality control and reproducibility in M-mode, two-dimensional, and speckle tracking echocardiography acquisition and analysis: the CARDIA study, year 25 examination experience. Echocardiography. 2015;32(8):1233–40.
D'Andrea A, Stanziola AA, Saggar R, Saggar R, Sperlongano S, Conte M, D'Alto M, Ferrara F, Gargani L, Lancellotti P. Bossone E; RIGHT heart international NETwork (RIGHT-NET) investigators. Right ventricular functional Reserve in Early-Stage Idiopathic Pulmonary Fibrosis: an exercise two-dimensional speckle tracking Doppler echocardiography study. Chest. 2019;155(2):297–306.
Argiento P, Vanderpool RR, Mulè M, Russo MG, D’Alto M, Bossone E, et al. Exercise stress echocardiography of the pulmonary circulation: limits of Normal and sex differences. Chest. 2012;142(5):1158–65.
D’Alto M, Pavelescu A, Argiento P, Romeo E, Correra A, Di Marco GM, et al. Echocardiographic assessment of right ventricular contractile reserve in healthy subjects. Echocardiography. 2017;34:61–8.
Kusunose K, Popović ZB, Motoki H, Marwick TH. Prognostic significance of exercise-induced right ventricular dysfunction in asymptomatic degenerative mitral regurgitation. Circ Cardiovasc Imaging. 2013 Mar 1;6(2):167–76.
Wierzbowska-Drabik K, Picano E, Bossone E, Ciampi Q, Lipiec P, Kasprzak JD. The feasibility and clinical implication of tricuspid regurgitant velocity and pulmonary flow acceleration time evaluation for pulmonary pressure assessment during exercise stress echocardiography. Eur Heart J Cardiovasc Imaging. 2019 Sep 1;20(9):1027–34.
Naeije R, Torbicki A. More on the noninvasive diagnosis of pulmonary hypertension: Doppler echocardiography revisited. Eur Respir J. 1995 Sep;8(9):1445–9.
Ling LF, Obuchowski NA, Rodriguez L, Popovic Z, Kwon D, Marwick TH. Accuracy and interobserver concordance of echocardiographic assessment of right ventricular size and systolic function: a quality control exercise. J Am Soc Echocardiogr. 2012 Jul;25(7):709–13.
Acknowledgements
Not applicable.
Funding
No funding sources exist.
Author information
Authors and Affiliations
Consortia
Contributions
FF, LG, CC, EB analyzed and interpreted the patient data; CC, GA, PA, FB, RC, AC, RC, MD, AD, PD, SG, SG, AM, MM, AM, FP, LP, NP, MR, BR, AS, WS, DV, OV and KW analyzed the echocardiographic data; WA, FC, EG, MG, JK, TK, GL, CM, LR, RS, AS, MV and RN have drafted the work and substantively revised it; FF, LG, RN and EB have designed the study were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institution’s ethics board C.E. Campania Sud (parere n. 84 r.p.s.o.; determina n. 101 del 14-12-2015).
Informed consent was obtained from the participants prior to inclusion to the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
The RIGHT Heart International NETwork (RIGHT-NET) Investigators
Co-Principal Investigators: Eduardo Bossone (A Cardarelli Hospital, Naples, Italy), Luna Gargani (Institute of Clinical Physiology, CNR, Pisa, Italy), Robert Naeije (Free University of Brussels, Brussels, Belgium).
Study Coordinator: Francesco Ferrara (Cava de’ Tirreni and Amalfi Coast Division of Cardiology, University Hospital, Salerno, Italy).
Co-Investigators: William F. Armstrong, Theodore John Kolias (University of Michigan, Ann Arbor, USA); Eduardo Bossone, Rosangela Cocchia, Ciro Mauro, Chiara Sepe (A Cardarelli Hospital, Naples, Italy); Filippo Cademartiri, Brigida Ranieri, Andrea Salzano (IRCCS SDN, Diagnostic and Nuclear Research Institute, Naples, Italy); Francesco Capuano (Department of Industrial Engineering, Università di Napoli Federico II, Naples, Italy); Rodolfo Citro, Rossella Benvenga, Michele Bellino, Ilaria Radano (University Hospital of Salerno, Salerno, Italy); Antonio Cittadini, Alberto Marra, Roberta D’Assante, Salvatore Rega (Federico II University of Naples, Italy); Michele D’Alto, Paola Argiento (University of Campania “Luigi Vanvitelli”, Naples, Italy); Antonello D’Andrea (Umberto I° Hospital Nocera Inferiore, Italy); Francesco Ferrara, Carla Contaldi (Cava de’ Tirreni and Amalfi Coast Hospital, University Hospital of Salerno, Italy); Luna Gargani, Matteo Mazzola, Marco Raciti (Institute of Clinical Physiology, CNR, Pisa, Italy); Santo Dellegrottaglie (Ospedale Medico-Chirurgico Accreditato Villa dei Fiori, Acerra - Naples, Italy); Nicola De Luca, Francesco Rozza, Valentina Russo (Hypertension Research Center, University Federico II of Naples, Italy); Giovanni Di Salvo (University of Padova, Italy; Imperial College, London, UK); Stefano Ghio, Stefania Guida (I.R.C.C.S. Policlinico San Matteo, Pavia, Italy); Ekkerard Grunig, Christina A. Eichstaedt (Heidelberg University Hospital, Germany); Marco Guazzi, Francesco Bandera, Valentina Labate (IRCCS Policlinico San Donato, University of Milan, Milan, Italy); André La Gerche (Baker Heart and Diabetes Institute, Melbourne, Australia); Giuseppe Limongelli, Giuseppe Pacileo, Marina Verrengia (University of Campania “Luigi Vanvitelli”, Naples, Italy); Jaroslaw D. Kasprzak, Karina Wierzbowska-Drabik (Bieganski Hospital, Medical University of Lodz Poland); Gabor Kovacs, Philipp Douschan (Medical University of Graz, Graz, Austria); Antonella Moreo, Francesca Casadei, Benedetta De Chiara, (Niguarda Hospital, Milan, Italy); Robert Naeije (Free University of Brussels, Brussels, Belgium); Ellen Ostenfeld (Lund University, Skåne University Hospital, Sweden); Gianni Pedrizzetti (Department of Engineering and Architecture, University of Trieste); Francesco Pieri, Fabio Mori, Alberto Moggi-Pignone (Azienda Ospedaliero-Universitaria Careggi, Florence, Italy); Lorenza Pratali (Institute of Clinical Physiology, CNR, Pisa, Italy); Nicola Pugliese (Department of Clinical and Experimental Medicine, University of Pisa, Italy); Rajan Saggar (UCLA Medical Center,Los Angeles, USA); Rajeev Saggar (Banner University Medical Center, Phoenix, Arizona, USA); Christine Selton-Suty, Olivier Huttin, Clément Venner (University Hospital of Nancy, France); Walter Serra, Francesco Tafuni (University Hospital of Parma, Italy); Anna Stanziola, Maria Martino, Giovanna Caccavo (Department of Respiratory Disease, Federico II University, Monaldi Hospital, Naples, Italy); István Szabó (University of Medicine and Pharmacy of Târgu Mureș, Târgu Mureș, Romania); Albert Varga, Gergely Agoston, (University of Szeged, Szeged, Hungary); Darmien Voilliot (Centre Hospitalier Lunéville, France); Olga Vriz (Heart Centre, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia); Mani Vannan, Sara Mobasseri, Peter Flueckiger, Shizhen Liu (Piedmont Heart Institute, USA).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ferrara, F., Gargani, L., Contaldi, C. et al. A multicentric quality-control study of exercise Doppler echocardiography of the right heart and the pulmonary circulation. The RIGHT Heart International NETwork (RIGHT-NET). Cardiovasc Ultrasound 19, 9 (2021). https://doi.org/10.1186/s12947-021-00238-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12947-021-00238-1