Abstract
Introduction
We previously documented the beneficial effects of rice bran oil (RBO) on cardiac function and atherogenic cardiometabolic factors in men with coronary artery disease. Therefore, the existing evidence in this area aims to be expanded by investigating the impact of adding RBO to a daily standard diet on emerging insulin resistance surrogate markers, lipid peroxidation, antioxidant status, and metabolic disturbances in individuals with metabolic syndrome (MetSyn) through an open-label controlled trial.
Methods
A total of 50 overweight/obese adults (mean body mass index (BMI) = 31.08 kg/m2) with at least 3 MetSyn components were randomly allocated to either the control group, which received a standard diet plan, or the intervention group, which was supplemented with 30 g/d RBO for 8 weeks. BMI, MetSyn components, metabolic score for insulin resistance (METS-IR), triglyceride‒glucose‒BMI (TyG‒BMI), malondialdehyde (MDA), total antioxidant capacity (TAC), and plasma polyphenol levels were measured before and after this open-label trial.
Results
Analysis of covariance (ANCOVA) adjusted for baseline values revealed that, compared with patients who received only a standard diet, those who were supplemented with 30 g/d RBO presented significantly lower total cholesterol (P value = 0.005; effect size (ES):-0.92), LDL-cholesterol (P value = 0.048; ES:-0.62), fasting blood glucose (P value = 0.014; ES:-0.77), MDA (P value = 0.002; ES: -1.01), METS-IR (P value < 0.001; ES: -1.24), and TyG-BMI (P value = 0.007; ES:-0.85) after 8 weeks. Additionally, RBO consumption resulted in significantly higher levels of HDL-C (P value = 0.004; ES:0.94) and TAC (P value < 0.0001; ES:2.05). However, no significant changes were noted in BMI, waist circumference, serum triglycerides, plasma polyphenols, or blood pressure.
Conclusion
Although the current findings suggest that the hypocholesterolemic, antihyperglycemic, and antioxidative effects of 30 g/d RBO seem to be promising for MetSyn patients, they should be considered preliminary. Therefore, further well-designed clinical trials with larger sample sizes and longer durations are needed to confirm these findings.
Similar content being viewed by others
Introduction
Since it was originally defined by Reaven in 1988 [1], metabolic syndrome (MetSyn), commonly known as insulin resistance syndrome, or syndrome X, is now an important driver of the current global cardiovascular crisis [2]. A rising body of evidence indicates that this condition can accelerate atherosclerosis, which is caused by chronic inflammation and vascular endothelial dysfunction, and dramatically increases the risk of type 2 diabetes as well as cardiovascular-related mortality [3,4,5]. MetSyn is characterized by several cardiometabolic disorders, including obesity, insulin resistance, hypertension, atherogenic dyslipidemia (particularly hypertriglyceridemia, elevated low-density lipoprotein cholesterol (LDL-C) and low high-density lipoprotein cholesterol (HDL-C)), and a proinflammatory and prothrombotic state (such as increased levels of C-reactive protein (CRP), apo-lipoprotein B, and homocysteine) [6]. According to somewhat inconsistent clinical definitions and cutoff points for MetSyn components, several definitions and diagnostic criteria have been proposed. As reported by a recently published meta-analysis, the worldwide prevalence of MetSyn varied from 12.5% (95% confidence interval (CI): 10.2–15.0%) according to the Adult Treatment Panel III of the National Cholesterol Education Program (NCEP-ATP III) criteria to 31.4% (29.8–33.0%) according to the Joint Interim Statement definition [7].
Although several genetic and environmental factors can trigger different components of MetSyn, the pathogenesis underlying this complex condition is not well understood. Along with abnormal lipid metabolism, insulin resistance is the most broadly acknowledged pathophysiological factor associated with MetSyn [8,9,10]. Several reports documenting reduced antioxidant capacity together with greater concentrations of reactive oxygen (ROS) and nitrogen (RNS) species, oxidized LDL (OxLDL), and malondialdehyde (MDA) in MetSyn highlight the role of chronic low-grade inflammatory and pro-oxidative states in relation to visceral adiposity, as well as other potential pathophysiological mechanisms involved in this syndrome [8,9,10,11].
These mechanisms prompted us to apply novel strategies for ameliorating oxidative stress and lipid peroxidation combined with the accumulation of fat mass in MetSyn [8,9,10,11]. Notably, obese subjects have been shown to have a lower concentration of serum total antioxidant capacity (TAC) than normal subjects [12]. Thus, increasing the routine intake of dietary products that are able to enforce the antioxidative defense of the body can result in improved TAC and, in this way, combat visceral adiposity-related oxidative stress [12].
Therefore, herein, we aimed to explore the effects of a heart-friendly oil, rice bran oil (RBO), which has high phytochemical content and antioxidant properties, on the antioxidant capacity and lipid peroxidation of MetSyn together with overweight/obesity. Although accumulating evidence has shown that rice bran and its oil, as byproducts of the rice milling process, have therapeutic effects on several metabolic disorders [11, 13,14,15,16], few human studies are available regarding the ameliorative effects of RBO on lipid peroxidation and the antioxidant status [17].
We previously documented the modulating impact of RBO on atherogenic cardiometabolic factors through an open-label controlled trial in men with coronary artery disease (CAD), as it exerted hypolipidemic, hypoglycemic and anti-inflammatory effects. According to our previous results, daily consumption of 30 g of RBO, compared with sunflower oil, was able to increase the left ventricular ejection fraction to reduce the serum levels of uric acid, lipid profile (with the exception of HDL-C), blood glucose, and novel atherogenicity markers in correlation with ameliorated inflammatory markers (high-sensitivity C-reactive protein (hs-CRP) and tumor necrosis factor-alpha (TNF alpha)), although it failed to change body weight and blood pressure after the trial [18, 19]. Therefore, we aimed to expand the existing evidence by investigating the impact of incorporating RBO into the daily standard diet on various health markers in individuals with MetSyn through an open-label controlled trial. In this regard, changes in emerging insulin resistance surrogate markers (including the metabolic score for insulin resistance index (METS-IR) and triglyceride-glucose (TyG) BMI), lipid peroxidation (as reflected by MDA levels), and antioxidant status (as measured by TAC and total plasma polyphenol), in addition to anthropometric indices (as marked by body mass index (BMI) and waist circumference (WC)), blood pressure, and serum metabolic biomarkers (blood glucose and serum lipid profile), were explored following 8-week consumption of RBO within a standard diet vs. a standard diet alone. We hypothesized that the daily incorporation of RBO as a nutrient-rich fat source into a standard diet can reduce cardiometabolic risk, ameliorate insulin resistance and glycemic control, improve the lipid peroxidation rate, and enhance the antioxidant status in overweight/obese MetSyn patients in comparison to the standard diet alone.
Methods
Study design and participants
An open-label, randomized controlled trial was conducted to recruit a total of 80 adult subjects, with MetSyn from individuals who visited the cardiology outpatient clinic at Dr. Heshmat Hospital in Rasht, Iran, from May 2022 to August 2023. The following terms were applied to the inclusion criteria: adults aged between 20 and 70 years with a medical diagnosis of MetSyn [Three or more of the MetSyn components: 1. WC ≥ 102 cm for males and ≥ 88 cm for females; 2. systolic blood pressure (SBP) ≥ 130 mmHg or diastolic blood pressure (DBP) ≥ 85 mmHg; 3. Serum glucose ≥ 100 mg/dL; 4. HDL-C < 40 mg/dL for males and < 50 mg/dLfor females; and 5. Serum triglyceride ≥ 150 mmol/L]. The exclusion criteria were a history of kidney disease, urolithiasis, gastrointestinal disorders, autoimmune disorders, and cholelithiasis. Moreover, current drug or alcohol abuse, the administration of supplements that would interfere with the outcomes of the study (i.e., omega-3 fatty acids, antioxidants, fiber, vitamins and minerals), and any changes in drug therapy or treatment protocols. During the research, participants' willingness to proceed with the study was assessed. Any reluctance to continue, whether due to displeasure of the flavor of the oil or for any other reasons, was deemed grounds for exclusion from the study. Following the classification of eligible patients on the basis of their age range (one category: 20–45 years and the other category: 45–70 years), participants were randomly assigned to either the control group (n = 25) or the RBO group (n = 25) through a randomization method in which computer-generated random numbers were utilized. The randomization procedure was executed by one of the research team members who was not involved in the recruitment of subjects according to a stratified block design. The participants were organized into blocks of four, maintaining a 1:1 allocation ratio. The study lasted for 8 weeks in total, and participants were required to maintain their lifestyle and medications and were prescribed an individualized standard diet. An overview of the study procedure is depicted in Supplementary Fig. 1. The institutional review board of Research Affairs, affiliated with Guilan University of Medical Sciences (GUMS), reviewed and approved this research (registered with research code = 33733; 71214). Furthermore, the trial protocol was registered in the clinical trial registration system (“IRCT registration number: IRCT registration number = IRCT20180205038626N10, Registration date: 2021–11-25’, URL: https://irct.behdasht.gov.ir/trial/60160”). The ethics committee of the GUMS also approved this study (ethics code number = IR.GUMS.REC.1400.389). All research methods adhered to the principles mentioned in the Declaration of Helsinki as of 2013. In addition, written informed consent was obtained from all study subjects prior to participation.
Data collection and intervention
At baseline, all demographic, socioeconomic, medication and past medical history information was collected through face‒to-face interviews. Study assessments, including biochemical panels and measurements of blood pressure and anthropometry, were then carried out before and after the 8-week intervention. Furthermore, at the beginning of the trial and after the study, a registered dietitian of our research team interviewed all the participants. Standard individualized diets were then prescribed for all the subjects while considering their habitual dietary preferences and habits adjusted for excessive energy to be healthier. Energy and macronutrient requirements were then calculated for each participant on the basis of the “2010 United States Departments of Agriculture (USDA) dietary recommendations for American” [20]. The prescribed diet compositions were as follows: 50–55% carbohydrates, 30% fat and 15–20% protein. The participants were also provided with sample meal plans that illustrated the recommended diet, covering options for 6 meals per day, including breakfast, lunch, dinner, and three snacks, which were also given to the studied subjects. The patients in the control group were given a standard diet alone, whereas the intervention group subjects were additionally asked to consume RBO (30 g, equivalent ∼ 2 tablespoon per day). The participants’ adherence to the prescribed diets was assessed through the collection of 24 h diet recalls before and after 8 weeks, during which they were instructed to document their daily meals and snacks to food diaries. In addition, to ensure that they adhered well to the dietary plans, weekly follow-up phone calls were also scheduled to address any concerns and reiterate dietary guidelines.
The Giltaz Company manufactured RBO with no intervention in the study procedure. Its fatty acid content comprised 48.9% MUFAs (including C16:1 at 0.3%, C18:1—oleic acid at 48%, and C20:1 at 0.6%), 17.82% SFAs (comprising C14:0 at 0.4%, C16:0 at 15.12%, C18:0 at 1.6%, and C20:0 at 0.7%), and 32.53% PUFAs (including C18:2—linoleic acid at 30.33% and C18:3—linolenic acid at 2.2%). In terms of its bioactive contents, γ-oryzanol is found at a concentration of 1.65 g/100 g of RBO. In addition, its total amount of tocotrienols and tocopherols is approximately 0.281 mg/g, with γ-tocotrienol (0.175 mg/g RBO), followed by α-tocopherol (0.061 mg/g RBO), which is the most predominant form [18, 19].
Anthropometrics and blood pressure measurements
Weight and height were measured through the Seca 755 dial column medical scale and a standard stadiometer to the nearest 0.5 kg and 0.1 cm, respectively. The weight measurements were recorded to the nearest 0.5 kg, whereas the height measurements were taken to the nearest 0.1 cm. WC was measured through a nonstretchable tape placed at the midpoint between the last rib and upper part of the iliac crest. This WC measurement was also recorded to the nearest 0.1 cm. The assessments of body weight, WC, and blood pressure were conducted both before and after the 8-week intervention period. Systolic and diastolic blood pressure measurements were obtained via an automated sphygmomanometer (Supplementary Fig. 1).
Biological sample collection and analysis
Approximately 8 mL of blood sample was taken from each participant’s antecubital vein following an overnight fast, twice during the course of the investigation—once at baseline and once after the 8-week research period. To prevent coagulation, these samples were collected in sterile containers with sodium citrate. After blood centrifugation, the plasma and serum aliquots were stored at –70 °C until the end of the trials. Serum concentrations of total cholesterol (TC), HDL-C, LDL-C, triglycerides and fasting blood glucose (FBG) were determined via the enzymatic-colorimetric (CPO-POD) method via commercial kits according to the manufacturer’s instructions and using auto analyzers (Hitachi 917 (Hitachi High-Technologies Corporation, Tokyo, Japan); and Olympus 640 (Olympus Corporation, Tokyo, Japan). Moreover, the LDL-C level was calculated via the Friedewald formula [21]. Serum TAC was assessed via the Naxifer™-Total Antioxidant Capacity Assay Kit according to the manufacturer’s instructions (Novin Navand Salamat Pishtaz Company, Urmia, Iran). Additionally, the levels of plasma total phenol and serum MDA were evaluated via the Naphenol™-Total Phenol Assay Kit and the Nalondi™-Lipid Peroxidation Assay Kit-MDA, respectively (Novin Navand Salamat Pishtaz Company, Urmia, Iran) (Supplementary Fig. 1).
Definition of surrogate markers of insulin resistance
The indices of insulin resistance surrogate markers, including TyG-BMI and METS-IR, were estimated via the following calculations [22,23,24]:
-
\(\text{Metabolic score for insulin resistance index}\;\left(\mathrm{METS-IR}\right)=\)
-
\(\text{Triglyceride glucose}\;\left(\text {TyG}\right)-\text{BMI index = }((Ln\left.\left(\;\frac{\text {fasting triglycerides}\;\left(\frac{\text {mg}}{\textrm {dL}}\right)\times\;{\text {fasting glucose}}\;\left(\frac{\text {mg}}{\textrm{ dL}}\right)}2\right.\right))\;\times\;\text {BMI}).\)
Sample size calculation and statistical analysis
The sample size of the current trial was estimated on the basis of the abovementioned formula and considering the findings of our previous study [18], with 25 subjects in each study group, which accounted for an anticipated ∼15% dropout rate. Eighty percent statistical power with the aim of finding at least a 25 mg/dl reduction in serum LDL-C levels was also considered (α = 0.05, β = 0.20, standard deviation (SD) 1 = 19.52, SD2 = 36.51, and d = 25).
Statistical analysis was conducted in STATA version 16 (StataCorp LLC; College Station, TX, USA). Descriptive data were provided for all the variables. For categorical variables, the frequencies (counts) and percentages (%) were reported. For quantitative (continuous) variables, the mean and standard deviation (SD) were described. To compare the intervention group and the control group, in the case of continuous variables, the independent sample t test was employed. For categorical variables, the chi-square test was conducted. To analyze the effects of the intervention on the study outcomes, analysis of covariance (ANCOVA) was performed. The outcome variables included anthropometric data (BMI (in kg/m2) and WC (in cm)), blood pressure (SBP and DBP (in mmHg)), laboratory data (FBG, serum triglyceride, cholesterol, LDL-C and HDL-C levels (in mg/dL)), and serum levels of oxidant/antioxidant factors (MDA (in nmol/L), total plasma polyphenol (in Mg/ml), and TAC (in Mmol/L)). In addition, the METS-IR and TyG-BMI indices were also investigated as study outcomes reflecting the status of insulin resistance. The baseline values of each of these variables were also controlled for when conducting the ANCOVA models to explore treatment effects, allowing for a more accurate comparison of the intervention and control groups. The corresponding adjusted means and SDs take into account the initial values of the participants before the intervention are reported. Furthermore, the effect size for each outcome, known as Cohen's d [25], was calculated by dividing the mean difference after the intervention by the combined standard deviation. Cohen's d provides a standardized evaluation of the disparity between the intervention and control arms, facilitating a more insightful investigation of the effectiveness of the intervention. The magnitude of the effect sizes was classified via Cohen's d values [25]: negligible or trivial for d < 0.2, mild or weak for 0.20–0.49, moderate or medium for 0.50–0.79 and large or powerful for d > 0.80. Significance was considered when the P value was < 0.05, with two-tailed statistical analysis.
Results
Baseline characteristics of the participants
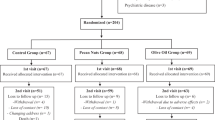
Out of 80 patients who were evaluated for eligibility, 50 were selected, and the study began. Two participants in the RBO group and 4 participants in the control group dropped out for various reasons. Accordingly, 44 individuals ended the trial, which is depicted comprehensively in Fig. 1. Table 1 summarizes the baseline characteristics of the studied participants, with average ages of 52 (10) and 53 (10) years in the intervention and control groups, respectively. The distributions of age, sex, and educational level were uniform among the participants in the two groups (Table 1). There were also no significant differences in terms of the MetSyn components of the participants in each group, except that the frequency of hypertriglyceridemia tended to be greater among patients in the intervention group than among the controls (96% vs. 71%, P value = 0.042) (Table 1).
The dietary energy and macronutrient intakes of the studied participants were also compared across the study groups, and no between-group differences were noted before or after the current randomized controlled trial (RCT) (Supplementary Table 1).
Effects of intervention on cardiometabolic risk factors, lipid peroxidation and antioxidant status markers
Between-group comparisons at enrollment revealed that the majority of the anthropometric, clinical, and biochemical data of the studied patients who were supplemented with RBO plus a standard diet or those who received only a standard diet were homogeneously distributed, except that the intervention group presented significantly lower WC, HDL-C, and TAC and greater triglyceride levels than did the other groups did (P value < 0.05) (Tables 2 and 3).
Regarding the effects of the study intervention on anthropometric measures, no significant differences were observed in either BMI or WC; however, a small, nonsignificant trend toward lower average BMI levels was observed in the patients in the RBO plus standard diet group than in those in the control arm. Additionally, with respect to the changes in blood pressure following the 8-week trial, only a moderate reduction in the level of SBP was observed in those who consumed RBO compared with controls, although this difference was marginally statistically significant (baseline adjusted mean (SD): 125.74 (7.14) mmHg vs 129.89 (7.32) mmHg; effect size: -0.58 (-1.18 – -0.03); P value = 0.064, using ANCOVA test) (Table 2).
At the 8th week, between-group comparisons of the levels of the serum lipid profile after taking into account the baseline values via ANCOVA revealed largely reduced TC (mean (SD): 144.57 (37.56) mg/dL vs. 178.99 (37.63) mg/dL; effect size: -0.92 (-1.53—-0.29); P value = 0.005) levels following the consumption of 30 g/d RBO plus a standard diet compared with the patients who received only a standard diet. Similarly, moderately decreased serum LDL-C concentrations were also detected in the intervention group, although the difference was marginally significant (mean (SD): 75.33 (31.28) mg/dL vs. 94.60 (31.29) mg/dL; effect size: -0.62 (-1.22—-0.01); P value = 0.048). Conversely, HDL-C levels were largely increased in the MetSyn patients who were administered RBO compared with those in the other groups (mean (SD): 42.49 (5.06) mg/dL vs. 37.75 (5.08) mg/dL; effect size: 0.94 (0.31–1.56); P value = 0.004). However, no significant effects on the serum triglyceride levels were noted after the trial (Table 2).
Moreover, exploring the effects of supplementing the standard diet with RBO on glycemic control of the included MetSyn according to ANCOVA models adjusted for baseline levels revealed that the patients in the intervention group, compared with the controls, had moderately lower FBG levels (mean (SD): 107.67 (29.80) mg/dL vs. 130.59 (29.80) mg/dL; effect size: -0.77 (-1.38—-0.15); P value = 0.014). Interestingly, further analysis of the impact of the RBO intervention on novel insulin resistance markers, including the METS-IR and TyG-BMI indices, revealed significantly greater reductions in both markers after consumption of RBO plus a standard diet than after consumption of a standard diet alone (METS-IR baseline-adjusted mean (SD): 48.00 (3.42) vs. 52.30 (3.51); effect size: -1.24 (-1.88—-0.59); P value < 0.001; TyG-BMI index baseline-adjusted mean (SD): 273.00 (16.83) vs. 287.57 (17.25); effect size: -0.85 (-1.47—-0.23); P value = 0.007) (Tables 2 and 3 and Fig. 2).
Box plot of changes in insulin resistance surrogate markers (a triglyceride‒glucose (TyG) BMI and b metabolic score for insulin resistance index (METS − IR)) before and after intervention (consumption of standard diet + rice bran oil vs. standard diet alone) in a randomized controlled trial of patients with metabolic syndrome. The error bars depict the interquartile range. # indicates significant between-group differences according to ANCOVA adjusted for baseline values
With respect to the effects of RBO on lipid peroxidation and antioxidant status, the present findings revealed that serum MDA levels and TAC differed significantly between the intervention group and the control group after the 8-week trial. These significant improvements were reflected by largely reduced MDA levels and highly increased TAC after RBO consumption plus the standard diet in comparison with the standard diet alone (MDA adjusted mean (SD): 0.08 (0.03) nmol/ml vs. 0.11 (0.03) nmol/ml; effect size: -1.01 (-1.63—-0.37); P value = 0.002, TAC adjusted mean (SD): 0.45 (0.04) Mmol/L vs. 0.36 (0.04) Mmol/L; effect size: 2.05 (1.31 – 2.78); P value < 0.0001 via ANCOVA test). However, no significant differences were found in the levels of plasma polyphenols (Table 3).
Adverse effects
None of the patients in the RBO group experienced any adverse effects or complications following the consumption of RBO, and the oil was well tolerated.
Discussion
In line with our previous research on the impact of RBO on atherogenicity indices, cardiometabolic risk factors and biomarkers of the inflammatory state [18, 19], this study aimed to advance the current knowledge of the beneficial effects of RBO on MetSyn components, novel insulin resistance surrogate markers, antioxidant status, and lipid peroxidation in overweight and obese individuals, both men and women. The findings from the current study revealed that RBO supplementation within a standard diet resulted in a significant reduction in FBG, LDL-C, and TC and a significant improvement in HDL-C levels among individuals with MetSyn. Moreover, promising results have been shown for reinforcing antioxidant defense and inhibiting oxidative stress, as reflected by increased serum TAC, along with reduced levels of MDA, a well-known lipid peroxidation marker in serum.
Consistent with our findings, several reports on RBO have revealed lipid-lowering activities due to its high-value compounds [18, 19, 26,27,28,29,30,31,32,33,34]. A randomized control trial on hyperlipidemic subjects by Bumrungpert et al. demonstrated that 4 weeks of RBO supplementation (30 mL) could decrease LDL-C levels [27]. Moreover, a 4-week feeding study involving 50 volunteers who consumed a low-calorie diet based on 1400 kcal of energy with RBO was performed. The outcomes of a previous study corroborated earlier findings demonstrating the reduction in total and LDL cholesterol levels in humans caused by RBO [29]. Notably, recent systematic reviews and meta-analyses of RCTs confirmed our results by highlighting a significant improvement in the lipid profile through a reduction in the serum TC and LDL-C levels [26, 35]. Similarly, the results obtained in the present study on the effects of RBO on the lipid profile demonstrated that, compared with patients who received a standard diet plan, those who were supplemented with 30 g/d RBO presented reduced TC levels and elevated HDL-C levels with large effect sizes (effect sizes: -0.92 and 0.94, respectively; P value < 0.005). These subjects also showed a reduction in serum LDL-C levels with a moderate effect size, although the between-group difference was marginally significant (effect size: -0.62; P value = 0.048). Nonetheless, no significant differences in the serum triglyceride levels following the consumption of RBO were observed. Additionally, in a recent clinical trial by Prasertsri et al. [36], which involved 35 prehypertensive patients, no favorable changes in the serum TC, FBG, triglyceride, LDL-C or HDL-C levels were detected by the consumption of 1000 mg/day of Riceberry RBO or RBO (1000 mg/d), in contrast to our results [36].
Interestingly, in accordance with previous findings [18, 32, 34], the current results also support the efficacy of supplementing the standard diet with RBO, over the standard diet alone, in ameliorating glycemic control and insulin resistance indicators, as reflected by reduced FBG levels with moderate effect sizes (-0.77; P value = 0.014) and decreased values of insulin resistance surrogate markers, including METS-IR and the TyG-BMI index, with large effect sizes (-1.24 and -0.85, respectively; P value ≤ 0.007) in overweight/obese patients suffering from MetSyn. However, in contrast to the current evidence, some clinical trials have reported no significant changes in the glycemic profile following RBO consumption [30, 36].
The analysis of the constituents in the current RBO applied in the present study revealed key functional ingredients, similar to those of the other RBO variants [37, 38]. Notably, high levels of oleic acid accounted for 48%, and linoleic acid accounted for 30.33% of the fatty acid content. Additionally, significant amounts of γ-oryzanol (1.65 g/100 g of RBO), γ-tocotrienol (0.175 mg/gram RBO), and α-tocopherol (0.061 mg/g RBO) were identified as predominant forms in this particular RBO variant [18, 19]. As such, the unsaturated fatty acid contents of RBO may contribute to the observed antihyperglycemic, cholesterol-lowering and antiantioxidative effects of this heart-friendly oil during this RCT [39, 40]. Interestingly, a clinical trial in which saturated fatty acids (SFAs) were substituted with MUFAs revealed significant reductions in the production rates of very-low-density lipoprotein (VLDL) apoB-100 and LDL apoB-100, along with decreases in non-HDL-C and LDL-C, whereas no significant changes in triglyceride-rich lipoprotein (apoB-48) were reported [41]. Furthermore, robust evidence revealed tocopherols, tocotrienols, and oryzanol as the main bioactive compounds of RBO that can meditate various metabolic pathways related to its health-promoting effects. Accordingly, numerous mechanisms have been delineated in this regard. It has been suggested that γ-oryzanol may downregulate β-hydroxy-β-methylglutaryl-CoA (HMG-CoA) reductase, a key rate-limiting enzyme involved in hepatic cholesterol synthesis, which can suppress cholesterol synthesis in the liver [29, 42, 43]. In addition, the γ-oryzanol complex might increase the flow of bile acid and its combination with cholesterol, which subsequently increases the levels of cholesterol and its metabolites in the feces and hinders intestinal absorbance [31, 44]. Moreover, the γ-oryzanol molecule contains sterols that may reduce cholesterol absorption [42]. Another important attribute of γ-oryzanol is its tangible effects on the stimulation of cholesterol 7-alpha-hydroxylase (CYP7A1), an essential enzyme that regulates cholesterol levels during its conversion to bile acid [26, 27, 45]. Above all, animal models have previously proposed that RBO has a profound effect on the lipid profile, particularly LDL-C, by increasing LDL-C receptor levels [46]. In addition, γ–oryzanol intervention has been reported to effectively improve insulin resistance and lipid profiles by modulating MetSyn-related biomarkers such as adiponectin [15, 47, 48]. Moreover, as determined by in vivo studies, the antihyperglycemic properties of RBO can be mediated mainly by its tocotrienol, γ-oryzanol, and ferulic acid (FA) contents through the inhibition of a-amylase and a-glucosidase, which are key enzymes that regulate the glucose concentration in the small intestine [18, 19, 49,50,51,52,53,54]. The considerable impact of macronutrients and bioactive ingredients of rice on the modulation of glucose transport, specifically, sodium-coupled glucose cotransporters (SGLT1) and glucose transporters (GLUT2), could also be another hypothesis that highlights glucose-lowering activities [52]. To further address this issue, it has been reported that tocotrienols are capable of binding to peroxisome proliferator-activated receptors (PPARs), which leads to insulin-mediated glucose uptake through the upregulation of glucose transporter 4 (GLUT4) [53]; in this way, tocotrienol content of RBO may increase insulin sensitivity and contribute to the alleviation of hyperglycemia [51, 54].
Although the available evidence regarding the effects of RBO as a MUFA-rich fat source on serum triglyceride levels seems to be conflicting [31, 55,56,57], in the present study, we failed to find any significant differences in triglyceride levels between the intervention and control groups after the trial, whereas favorable effects of RBO on cholesterol-related lipid factors were noted. These findings may be attributed in part to the significant differences in the baseline values of the serum triglyceride levels rather than a direct effect of the intervention, as the intervention group presented greater levels than did the controls. Thus, although triglyceride levels tended to decrease among RBO patients, taking into account the baseline values in ANCOVA models revealed no significant effects of consuming the oil compared with those in the control group.
Additionally, the present study was designed to evaluate the efficacy of RBO on lipid peroxidation and antioxidant defense. Compared with receiving only the standard diet plan, consuming RBO resulted in largely ameliorated levels of the lipid peroxidation marker MDA and improved antioxidant status, as manifested by highly elevated TAC (large effect sizes: -1.01 and 2.05, respectively; P value ≤ 0.002). The evidence reported by other research groups may support our findings in terms of lipid peroxidation and oxidative stress, as indicated by changes in MDA and TAC [18, 27, 36, 51, 58]. Similarly, an 8-week RCT on prehypertensive females reported that both RBO and rice berry rice bran oil ameliorated MDA and TNF-alpha [36]. Research by Bumrungpert et al. revealed significant improvements in antioxidant status, as defined by ferric reducing antioxidant power (FRAP) and oxygen radical absorbance capacity (ORAC), after the consumption of a diet with RBO compared with the consumption of a diet with soybean oil [27]. From an overall perspective, it is not surprising that the levels of MDA, a secondary product of lipid peroxidation, would be modulated by the potent antiliplipidemic properties of RBO [51, 59]. The antioxidant properties of RBO, a polyphenol-enriched byproduct of rice processing, are delineated by its ability to increase the activities of several antioxidant enzymes, such as glutathione peroxidase (GPx), superoxide dismutase (SOD), catalase (CAT), quinone oxidoreductase, and nicotinamide adenine dinucleotide phosphate reduced form (NADPH), in addition to disrupting proinflammatory cytokine secretion [51, 59]. Likewise, RBO has shown promising potential protective effects against oxidative damage by donating a hydrogen atom to different free radicals and converting them to less reactive species as a consequence of its radical-scavenging activity [15, 58, 60]. Notably, γ-oryzanol seemed to have additional MetSyn by reducing the intracellular levels of CRP, triglycerides, and interleukin-6 and the expression of stearoyl coenzyme-A desaturase-1 [15, 47, 48].
With respect to the effects of RBO on blood pressure and anthropometric indices in our study, only a moderate reduction in the level of SBP was observed in those who consumed RBO compared with controls, although this difference was marginally significant (moderate effect size: -0.58). However, a recent randomized clinical trial on hypercholesteremia in overweight/obese adults provided insight into the blood pressure-reducing effects of defatted rice bran, a byproduct of RBO production, not only through reducing SBP but also DBP [32]. Nonetheless, consuming RBO did not result in significant effects on DBP, WC, or BMI in our trial, although it did lead to a small, nonsignificant trend toward lower average BMI levels than the standard diet alone (small effect size: -0.40). In parallel, the currently available body of research has failed to show a definitive impact of RBO on anthropometric indices, particularly weight [18, 29, 32]. The absence of the anticipated effect and controversial results of prior studies might be the result of several small differences beyond lifestyle, physical activity, and caloric intake.
Strengths and limitations
This study's primary strength lies in its inclusive recruitment of both male and female participants, providing a comprehensive analysis across genders. Research conducted on overweight/obese MetSyn patients underscores the potential of RBO as a therapeutic agent. However, the study is not without limitations. Prominently, the open-label design of the study, in addition to the lack of placebo oil, may complicate the interpretation of the findings, making it difficult to isolate the effects of RBO. Additionally, the 8-week intervention period may also be viewed as a limitation. Moreover, while some outcomes showed effect sizes greater than 0.20, they did not reach statistical significance, suggesting that the sample size and, therefore, the study power might have been inadequate. In addition, in the current investigation, we adopted a comprehensive set of statistical and methodological approaches to minimize the potential impact of confounding variables on the effects of RBO consumption. These approaches included a randomization process, the enforcement of a standardized dietary regimen for participants, and guidelines for patients to refrain from altering their daily activities, encompassing physical activity and medication consumption, throughout the study. We also employed ANCOVA models in which the baseline values of each outcome of interest were controlled for. Nonetheless, it is crucial to note that we were unable to completely eliminate all potential confounders. As a result, unmeasured influences, such as other environmental factors and variations in patients' medication or physical activity levels, may affect the outcomes. Therefore, caution is warranted in interpreting the findings, given the potential for residual confounding.
Clinical relevance of the current findings
These findings shed light on the promising effects of RBO, as incorporating this healthy oil into the standard diet in overweight/obese patients with MetSyn might lead to enhancements in hyperglycemia and high cholesterol levels while increasing HDL-C levels. Moreover, the ability of the body to protect against oxidative stress might also be improved. Considering these findings, healthcare providers can recommend a daily intake of approximately 30 g of RBO within a healthy dietary pattern for MetSyn patients. Moreover, unhealthy fat sources should also be limited as part of a comprehensive strategy to address the underlying factors contributing to MetSyn and improve overall health outcomes for affected individuals.
Future direction
Future studies should consider a larger sample size to improve the statistical power and definitively assess the effects of RBO. Furthermore, extending the duration of intervention periods could be beneficial for understanding the long-term effects of regular RBO consumption, as well as any potential adverse effects that may arise. In addition, isolating the active compounds found in RBO (including oleic acid, linoleic acid, γ-oryzanol, tocotrienols, and tocopherols) and investigating their effects in future clinical trials would provide substantial value in differentiating and comparing the benefits of the various constituents of this healthy oil. Additionally, incorporating direct measurements of γ-oryzanol levels and alterations in fatty acid profiles in the plasma or tissues of the studied patients would offer important insights into the mechanisms by which RBO may influence metabolic disturbances and oxidative stress pathways.
Conclusion
Overall, current findings from an 8-week open-label RCT provide important insights into the effects of RBO, including its hypocholesterolemic, antihyperglycemic, and antioxidative effects, together with alleviating lipid peroxidation associated with MetSyn. While these findings imply the potential of RBO to mitigate MetSyn and its related risks, they should be considered preliminary and need to be validated by future studies. Thus, well-structured clinical trials with larger sample sizes and longer follow-up periods and additional strategies to further minimize confounding effects are necessary. Additional experimental studies should also clarify the potential mechanisms by which RBO and its components can improve metabolic disturbances and oxidative stress.
Availability of data and materials
The datasets of the current study are available from the corresponding author on reasonable request.
Abbreviations
- RBO:
-
Rice bran oil
- MetSyn:
-
Metabolic syndrome
- BMI:
-
Body mass index
- METS-IR:
-
Metabolic score for insulin resistance
- TyG-BMI:
-
Triglyceride–glucose–BMI index
- MDA:
-
Malondialdehyde
- TAC:
-
Total antioxidant capacity
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- CRP:
-
C-reactive protein
- ROS:
-
Reactive oxygen species
- RNS:
-
Reactive nitrogen species
- OxLDL:
-
Oxidized LDL
- hs-CRP:
-
High-sensitivity C-reactive protein
- TNF alpha:
-
Tumor necrosis factor-alpha
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- USDA:
-
United States Departments of Agriculture
- WC:
-
Waist circumference
- SD:
-
Standard deviation
- CYP7A1:
-
Cholesterol 7-alpha-hydroxylase
- FA:
-
Ferulic acid
- PPAR:
-
Peroxisome proliferator-activated receptor
- GPx:
-
Glutathione peroxidase
- SOD:
-
Superoxide dismutase
- CAT:
-
Catalase
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate reduced form
References
Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37(12):1595–607.
Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. 2006;119(10):812–9.
Lakka H-M, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288(21):2709–16.
Laaksonen DE, Lakka H-M, Niskanen LK, Kaplan GA, Salonen JT, Lakka TA. Metabolic syndrome and development of diabetes mellitus: application and validation of recently suggested definitions of the metabolic syndrome in a prospective cohort study. Am J Epidemiol. 2002;156(11):1070–7.
Sattar N, Gaw A, Scherbakova O, Ford I, O’Reilly DSJ, Haffner SM, et al. Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation. 2003;108(4):414–9.
Haffner SM. The metabolic syndrome: inflammation, diabetes mellitus, and cardiovascular disease. Am J Cardiol. 2006;97(2):3–11.
Noubiap JJ, Nansseu JR, Lontchi-Yimagou E, Nkeck JR, Nyaga UF, Ngouo AT, et al. Geographic distribution of metabolic syndrome and its components in the general adult population: A meta-analysis of global data from 28 million individuals. Diabetes Res Clin Pract. 2022;188:109924. https://doi.org/10.1016/j.diabres.2022.109924.
Roberts CK, Hevener AL, Barnard RJ. Metabolic syndrome and insulin resistance: underlying causes and modification by exercise training. Compr Physiol. 2013;3(1):1.
Tylutka A, Morawin B, Walas Ł, Michałek M, Gwara A, Zembron-Lacny A. Assessment of metabolic syndrome predictors in relation to inflammation and visceral fat tissue in older adults. Sci Rep. 2023;13(1):89.
Esposito K, Giugliano D. The metabolic syndrome and inflammation: association or causation? Nutr Metab Cardiovasc Dis. 2004;14(5):228–32.
Quetglas-Llabrés MM, Monserrat-Mesquida M, Bouzas C, Gómez C, Mateos D, Ripoll-Vera T, et al. Inflammatory and Oxidative Stress Markers Related to Adherence to the Mediterranean Diet in Patients with Metabolic Syndrome. Antioxidants (Basel). 2022;11(5):901. https://doi.org/10.3390/antiox11050901.
Anaya-Morua W, Villafan-Bernal JR, Ramírez-Moreno E, García-Ortiz H, Martínez-Portilla RJ, Contreras-Cubas C, et al. Total Antioxidant Capacity in Obese and Non-Obese Subjects and Its Association with Anthropo-Metabolic Markers: Systematic Review and Meta-Analysis. Antioxidants. 2023;12(8):1512.
Cravotto G, Binello A, Merizzi G, Avogadro M. Improving solvent-free extraction of policosanol from rice bran by high-intensity ultrasound treatment. Eur J Lipid Sci Technol. 2004;106(3):147–51.
Orthoefer FT, Eastman J. Rice bran oil. Bailey’s industrial oil and fat products. 2005;2(7):465–89.
Sohail M, Rakha A, Butt MS, Iqbal MJ, Rashid S. Rice bran nutraceutics: A comprehensive review. Crit Rev Food Sci Nutr. 2017;57(17):3771–80.
Sivamaruthi BS, Alagarsamy K, Thangaleela S, Bharathi M, Kesika P, Chaiyasut C. Composition, Microbiota, Mechanisms, and Anti-Obesity Properties of Rice Bran. Foods. 2023;12(6):1300.
Selim S, Hussein E, Abdel-Megeid NS, Melebary SJ, Al-Harbi MS, Saleh AA. Growth Performance, Antioxidant Activity, Immune Status, Meat Quality, Liver Fat Content, and Liver Histomorphology of Broiler Chickens Fed Rice Bran Oil. Animals (Basel). 2021;11(12):3410. https://doi.org/10.3390/ani11123410.
Mahdavi-Roshan M, Salari A, Ghorbani Z, Nikpey Z, Haghighatkhah M, Fakhr Mousavi A, et al. The effects of rice bran oil on left ventricular systolic function, cardiometabolic risk factors and inflammatory mediators in men with coronary artery disease: a randomized clinical trial. Food Funct. 2021;12(10):4446–57.
Mahdavi-Roshan M, Salari A, Vakilpour A, Savar Rakhsh A, Ghorbani Z. Rice bran oil could favorably ameliorate atherogenicity and insulin resistance indices among men with coronary artery disease: post hoc analysis of a randomized controlled trial. Lipids Health Dis. 2021;20(1):153.
Dietary Guidelines Advisory Committee. Dietary Guidelines for Americans 2010; US Department of Health and Human Services. US Department of Agriculture: Washington, DC; 2010.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502.
Bello-Chavolla OY, Almeda-Valdes P, Gomez-Velasco D, Viveros-Ruiz T, Cruz-Bautista I, Romo-Romo A, et al. METS-IR, a novel score to evaluate insulin sensitivity, is predictive of visceral adiposity and incident type 2 diabetes. Eur J Endocrinol. 2018;178(5):533–44.
Yu X, Wang L, Zhang W, Ming J, Jia A, Xu S, et al. Fasting triglycerides and glucose index is more suitable for the identification of metabolically unhealthy individuals in the Chinese adult population: A nationwide study. J Diabetes Investig. 2019;10(4):1050–8.
Er L-K, Wu S, Chou H-H, Hsu L-A, Teng M-S, Sun Y-C, et al. Triglyceride Glucose-Body Mass Index Is a Simple and Clinically Useful Surrogate Marker for Insulin Resistance in Nondiabetic Individuals. PloS one. 2016;11(3):e0149731-e.
Cohen J. The Effect Size. Statistical Power Analysis for the Behavioral Sciences. Abingdon: Routledge; 1988:77–83.
Jolfaie NR, Rouhani MH, Surkan PJ, Siassi F, Azadbakht L. Rice Bran Oil Decreases Total and LDL Cholesterol in Humans: A Systematic Review and Meta-Analysis of Randomized Controlled Clinical Trials. Horm Metab Res. 2016;48(7):417–26.
Bumrungpert A, Chongsuwat R, Phosat C, Butacnum A. Rice Bran Oil Containing Gamma-Oryzanol Improves Lipid Profiles and Antioxidant Status in Hyperlipidemic Subjects: A Randomized Double-Blind Controlled Trial. J Altern Complement Med. 2019;25(3):353–8.
Minhajuddin M, Beg ZH, Iqbal J. Hypolipidemic and antioxidant properties of tocotrienol rich fraction isolated from rice bran oil in experimentally induced hyperlipidemic rats. Food Chem Toxicol. 2005;43(5):747–53.
Zavoshy R, Noroozi M, Jahanihashemi H. Effect of low calorie diet with rice bran oil on cardiovascular risk factors in hyperlipidemic patients. J Res Med Sci. 2012;17(7):626–31.
Lai MH, Chen YT, Chen YY, Chang JH, Cheng HH. Effects of rice bran oil on the blood lipids profiles and insulin resistance in type 2 diabetes patients. J Clin Biochem Nutr. 2012;51(1):15–8.
Salar A, Faghih S, Pishdad GR. Rice bran oil and canola oil improve blood lipids compared to sunflower oil in women with type 2 diabetes: A randomized, single-blind, controlled trial. J Clin Lipidol. 2016;10(2):299–305.
Saphyakhajorn W, Sirirat R, Sapwarobol S. Effect of defatted rice bran supplementation on metabolic parameters and inflammatory status in overweight/obese adults with hypercholesterolemia: a randomized, placebo-controlled intervention. BMC Nutr. 2022;8(1):94.
Eady S, Wallace A, Willis J, Scott R, Frampton C. Consumption of a plant sterol-based spread derived from rice bran oil is effective at reducing plasma lipid levels in mildly hypercholesterolaemic individuals. Br J Nutr. 2011;105(12):1808–18.
Haldar S, Wong LH, Tay SL, Jacoby JJ, He P, Osman F, et al. Two Blends of Refined Rice Bran, Flaxseed, and Sesame Seed Oils Affect the Blood Lipid Profile of Chinese Adults with Borderline Hypercholesterolemia to a Similar Extent as Refined Olive Oil. J Nutr. 2020;150(12):3141–51.
Pourrajab B, Sohouli MH, Amirinejad A, Fatahi S, Găman M-A, Shidfar F. The impact of rice bran oil consumption on the serum lipid profile in adults: a systematic review and meta-analysis of randomized controlled trials. Crit Rev Food Sci Nutr. 2022;62(22):6005–15.
Prasertsri P, Boonla O, Vierra J, Yisarakun W, Koowattanatianchai S, Phoemsapthawee J. Effects of Riceberry Rice Bran Oil Supplementation on Oxidative Stress and Cardiovascular Risk Biomarkers in Older Adults with Prehypertension. Prev Nutr Food Sci. 2022;27(4):365–75.
Rukmini C, Raghuram TC. Nutritional and biochemical aspects of the hypolipidemic action of rice bran oil: a review. J Am Coll Nutr. 1991;10(6):593–601.
Reis N, Castanho A, Lageiro M, Pereira C, Brites CM, Vaz-Velho M. Rice Bran Stabilisation and Oil Extraction Using the Microwave-Assisted Method and Its Effects on GABA and Gamma-Oryzanol Compounds. Foods. 2022;11(7):912.
Devarajan S, Singh R, Chatterjee B, Zhang B, Ali A. A blend of sesame oil and rice bran oil lowers blood pressure and improves the lipid profile in mild-to-moderate hypertensive patients. J Clin Lipidol. 2016;10(2):339–49.
Purushothama S, Raina PL, Hariharan K. Effect of long term feeding of rice bran oil upon lipids and lipoproteins in rats. Mol Cell Biochem. 1995;146(1):63–9.
Desjardins LC, Brière F, Tremblay AJ, Rancourt-Bouchard M, Drouin-Chartier JP, Corbeil J, et al. Substitution of dietary monounsaturated fatty acids from olive oil for saturated fatty acids from lard increases low-density lipoprotein apolipoprotein B-100 fractional catabolic rate in subjects with dyslipidemia associated with insulin resistance: a randomized controlled trial. Am J Clin Nutr. 2024;119(5):1270–9.
Sasaki J, Takada Y, Handa K, Kusuda M, Tanabe Y, Matsunaga A, et al. Effects of gamma-oryzanol on serum lipids and apolipoproteins in dyslipidemic schizophrenics receiving major tranquilizers. Clin Ther. 1990;12(3):263–8.
Sapwarobol S, Saphyakhajorn W, Astina J. Biological Functions and Activities of Rice Bran as a Functional Ingredient: A Review. Nutr Metab Insights. 2021;14:11786388211058560.
Chou TW, Ma CY, Cheng HH, Chen YY, Lai MH. A rice bran oil diet improves lipid abnormalities and suppress hyperinsulinemic responses in rats with streptozotocin/nicotinamide-induced type 2 diabetes. J Clin Biochem Nutr. 2009;45(1):29–36.
Pullinger CR, Eng C, Salen G, Shefer S, Batta AK, Erickson SK, et al. Human cholesterol 7alpha-hydroxylase (CYP7A1) deficiency has a hypercholesterolemic phenotype. J Clin Invest. 2002;110(1):109–17.
Chen CW, Cheng HH. A rice bran oil diet increases LDL-receptor and HMG-CoA reductase mRNA expressions and insulin sensitivity in rats with streptozotocin/nicotinamide-induced type 2 diabetes. J Nutr. 2006;136(6):1472–6.
Wang O, Liu J, Cheng Q, Guo X, Wang Y, Zhao L, et al. Effects of ferulic acid and γ-oryzanol on high-fat and high-fructose diet-induced metabolic syndrome in rats. PLoS ONE. 2015;10(2): e0118135.
Ohara K, Uchida A, Nagasaka R, Ushio H, Ohshima T. The effects of hydroxycinnamic acid derivatives on adiponectin secretion. Phytomedicine. 2009;16(2–3):130–7.
Sobhy R, Eid M, Zhan F, Liang H, Li B. Toward understanding the in vitro anti-amylolytic effects of three structurally different phytosterols in an aqueous medium using multispectral and molecular docking studies. J Mol Liq. 2019;283:225–34.
Jung EH, Kim SR, Hwang IK, Ha TY. Hypoglycemic effects of a phenolic acid fraction of rice bran and ferulic acid in C57BL/KsJ-db/db mice. J Agric Food Chem. 2007;55(24):9800–4.
Ahmed MA, Mohamed MA, Rashed LA, Abd Elbast SA, Ahmed EA. Rice Bran Oil Improves Insulin Resistance by Affecting the Expression of Antioxidants and Lipid-Regulatory Genes. Lipids. 2018;53(5):505–15.
Pereira C, Lourenço VM, Menezes R, Brites C. Rice Compounds with Impact on Diabetes Control. Foods. 2021;10(9):1992.
Fang F, Kang Z, Wong C. Vitamin E tocotrienols improve insulin sensitivity through activating peroxisome proliferator-activated receptors. Mol Nutr Food Res. 2010;54(3):345–52.
Vafa M, Haghighat N, Moslehi N, Eghtesadi S, Heydari I. Effect of Tocotrienols enriched canola oil on glycemic control and oxidative status in patients with type 2 diabetes mellitus: A randomized double-blind placebo-controlled clinical trial. J Res Med Sci. 2015;20(6):540–7.
Kuriyan R, Gopinath N, Vaz M, Kurpad AV. Use of rice bran oil in patients with hyperlipidaemia. Natl Med J India. 2005;18(6):292–6.
Tan SY, Peh E, Siow PC, Marangoni AG, Henry CJ. Effects of the physical-form and the degree-of-saturation of oil on postprandial plasma triglycerides, glycemia and appetite of healthy Chinese adults. Food Funct. 2017;8(12):4433–40.
Yang L, Yang C, Chu C, Wan M, Xu D, Pan D, et al. Beneficial effects of monounsaturated fatty acid-rich blended oils with an appropriate polyunsaturated/saturated fatty acid ratio and a low n-6/n-3 fatty acid ratio on the health of rats. J Sci Food Agric. 2022;102(15):7172–85. https://doi.org/10.1002/jsfa.12083.
Kalita P, Ahmad AB, Sen S, Deka B, Hazarika QK, Kapil MJ, et al. High-Value Compounds and Bioactivity of Rice Bran, Rice Bran Protein: A review. Recent Adv Food Nutr Agric. 2022. https://doi.org/10.2174/2772574X14666221227151558.
Ghatak SB, Panchal SJ. Investigation of the immunomodulatory potential of oryzanol isolated from crude rice bran oil in experimental animal models. Phytother Res. 2012;26(11):1701–8.
Saji N, Francis N, Schwarz LJ, Blanchard CL, Santhakumar AB. The Antioxidant and Anti-Inflammatory Properties of Rice Bran Phenolic Extracts. Foods. 2020;9(6):829.
Acknowledgements
The authors would like to thank the Giltaz Company which donated the oils with no conflict of interest. The donating company was not involved in study design, acquiring data, statistical analysis, results interpretation, or publication. None of the authors had any affiliation to this company. We also extend our gratitude to the patients who participated in the study.
Funding
This study was financially supported by Guilan University of Medical Sciences (GUMS), Rasht, Iran (research code = 3733; 71214).
Author information
Authors and Affiliations
Contributions
MMR, and ZGh: Conceptualization, funding acquisition, methodology, project administration and supervision. ZGh, MMR and NSh: Formal analysis, validation, visualization and writing original draft. MMR, MA, AS, AS, ZA, ZGh and NSh: Methodology, investigation and resources. MMR, ZGh, NSh, MA, AS, AS, and ZA: Writing review, editing and approving the final draft.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The institutional review board of Research Affairs, affiliated with Guilan University of Medical Sciences (GUMS), reviewed and approved this research (registered with research code = 3733; 71214). Furthermore, the trial protocol was registered in the clinical trial registration system (“IRCT registration number: IRCT registration number = IRCT20180205038626N10, Registration date: 2021–11-25’, URL: https://irct.behdasht.gov.ir/trial/60160”). The ethics committee of the GUMS also approved this study (ethics code number = IR.GUMS.REC.1400.389). All research methods adhered to the principles mentioned in the Declaration of Helsinki as of 2013. In addition, written informed consent was obtained from all study subjects prior to participation.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mahdavi-Roshan, M., Shoaibinobarian, N., Evazalipour, M. et al. An open label randomized controlled trial of the effects of rice bran oil on cardiometabolic risk factors, lipid peroxidation and antioxidant status in overweight/obese adults with metabolic syndrome. Lipids Health Dis 23, 273 (2024). https://doi.org/10.1186/s12944-024-02260-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02260-4