Abstract
Cancer cells need constant supplies of lipids to survive and grow. Lipid dependence has been observed in various types of cancer, including high-grade serous ovarian carcinomas (HGSOC), which is a lethal form of gynecological malignancy. ANGPTL3, PCSK9, and Apo CIII are pivotal lipid-modulating factors, and therapeutic antibodies have been developed against each one (Evinacumab, Evolocumab and Volanesorsen, respectively). The roles -if any- of ANGPTL3, PCSK9, and Apo CIII in HGSOC are unclear. Moreover, levels of these lipid-modulating factors have never been reported before in HGSOC. In this study, circulating levels of ANGPTL3, PCSK9, and Apo CIII, along with lipid profiles, are examined to verify whether one or many of these lipid-regulating factors are associated with HGSOC.
Methods ELISA kits were used to measure ANGPTL3, PCSK9 and Apo CIII levels in plasma samples from 31 women with HGSOC and 40 women with benign ovarian lesions (BOL) before treatment and surgery. A Roche Modular analytical platform measured lipid panels, Apo B and Lp(a) levels.
Results ANGPTL3 levels were higher in women with HGSOC (84 ng/mL, SD: 29 ng/mL, n = 31) than in women with BOL (67 ng/mL, SD: 31 ng/mL, n = 40; HGSOC vs. BOL P = 0.019). Associations between the lipid panel and ANGPTL3, and the inverse relationship between HDL-cholesterol and triglycerides, were present in women with BOL but not with HGSOC. PCSK9 and Apo CIII were not associated with HGSOC.
Conclusions In this cohort of 71 women, ANGPTL3 levels were increased in HGSOC patients. The presence of HGSOC disrupted the classic inverse relationship between HDL and triglycerides, as well as the association between the lipid panel and ANGPTL3. These associations were only maintained in cancer-free women. Given the availability of Evinacumab, a therapeutic antibody against ANGPTL3, the current finding prompts an assessment of whether ANGPTL3 inhibition has therapeutic potential in HGSOC.
Similar content being viewed by others
Background
Ovarian cancer (OC) is an aggressive form of cancer, with fewer than half of women who will survive beyond the 5 years following their diagnosis [1]. There is an urgent need for new approaches to treat women diagnosed with OC. In addition to the actual standard of care combining surgery and chemotherapy, cholesterol-lowering drugs appear as promising add-on therapeutics to impede ovarian cancer progression [2,3,4].
Statins are inhibitors of hydroxymethylglutaryl-coenzyme A reductase, the rate-limiting step in cholesterol de novo synthesis, and have been extensively investigated for their protective role against cancers [5,6,7]. Several studies indicate decreased OC-related mortality in women using statins, especially lipophilic ones [8,9,10,11]. Due to a lack of prospective randomized trials, no consensus has been reached on the benefits of using statins as an adjuvant treatment [12,13,14,15,16].
The effects of non-statin cholesterol-lowering drugs on OC progression are scarcely documented. Apolipoprotein C-III (Apo CIII), angiopoietin protein-like 3 (ANGPTL3), proprotein convertase subtilisin/kexin type 9 (PCSK9) modify circulating lipid levels (Low-density Lipoprotein or LDL, and high-density lipoproteins or HDL levels) and thus modulate lipid supplies to extra-hepatic tissues, including cancer cells. Lipoprotein (a), or Lp(a), is an LDL particle with an Apo (a) and is gaining traction in the cardiovascular field, while little is known about its role in cancers. These hepatic-derived factors are the targets of a new generation of cholesterol-lowering drugs. Volanesorsen is an antisense oligonucleotide which targets Apo CIII and was developed in hyperchylomicronemia [17]. Evinacumab is a monoclonal antibody (mab) that inhibits ANGPTL3 and is approved for treating homozygous hypercholesterolemia [18]. Evolocumab, also a mab, blocks PCSK9 and is combined with a statin to reach Apo B targets (< 0,70 g/L) in patients with cardiovascular diseases [19].
The present study aims to measure and report circulating levels of ANGPTL3, PCSK9 and Apo CIII in women with ovarian carcinoma (OC); all three lipid-modulating factors are the target of clinically available therapeutical monoclonal antibodies or antisense oligonucleotide therapy. The central hypothesis of this article is that at least one of these factors will be modified in OC to meet the increased cholesterol requirements of OC.
The present study reports measurements of circulating levels of Lp(a), Apo CIII, ANGPTL3, and PCSK9 in women diagnosed with either an epithelial high-grade serous ovarian carcinoma (HGSOC) or a benign ovarian lesion (BOL). Additionally, correlations linking these lipid-related factors to the lipid profile and ovarian tumor biomarkers CA125 and HE4 are provided. Furthermore, specific patterns related to women with HGSOC are outlined. This study is the first to simultaneously measure all the parameters described above and compare their associations across cancer-free and cancer patients from a same cohort.
Patients and methods
Patients
Participants included in the present study were sampled prior to treatment, of female biological sex, aged between 39 and 83 years old (y.o.), and had not yet undergone surgical debulking. Forty participants were diagnosed with a BOL (benign ovarian cyst-like lesion: serous para-tubular adenofibromas or cystadenofibromas). Thirty-one participants had received an epithelial high-grade serous ovarian carcinoma (HGSOC) diagnosis. All diagnoses were performed at the Pathology Department of the CHU de Québec-Université Laval. Ovarian cancer grading was determined using biomarker levels and histological analyses of biopsies. Staging of ovarian tumors was established according to the Fédération Internationale de Gynécologie et d’Obstétrique (FIGO) system. Mean age and median age were similar between the two groups (Table 1).
Blood samples
Plasma specimens from 71 women newly diagnosed with HGSOC or BOL were collected between 2017 and 2020 and were registered in the biobank of The Cancer Research Network (RRCancer, Montréal, QC). Plasma samples collected in EDTA vacutainers were centrifuged, aliquoted into 500 μL fractions and then stored at − 80 °C. Aliquots were thawed only once, on the day of measurements. All clinical samples were anonymized before analysis to protect patients’ privacy. All methods described below were carried out in accordance with relevant ethical guidelines and regulations.
Lipid profile
Three-hundred μL of each sample were sent to the Core laboratory of the Hôpital de l’Enfant-Jésus (Quebec City, Canada) for measurements of apolipoprotein B (Apo B, in g/L), Lp(a) (nmol/L), total cholesterol (TC, in mmol/L), HDL-cholesterol (HDL, in mmol/L) and triglycerides (TG, in mmol/L) on a Cobas 8000 Modular analytical platform (Roche Diagnostics). Lp(a) measurements lower than the reportable range (Lp(a) < 10 nmol/L) were set to a default value of 3 nmol/L, corresponding to half of the lower limit of detection. LDL-cholesterol (LDL) was calculated with the Friedewald equation: LDL in mmol/L = TC – (TG/ 2.2) – HDL [20]. Non-HDL cholesterol was calculated by subtracting HDL-cholesterol from total cholesterol in mmol/L.
PCSK9, ANGPTL3 and Apo CIII
Using commercially available Enzyme-Linked Immunosorbent Assay (ELISA) kits, levels of ANGPTL3 (cat # ab254510, Abcam, Cambridge, MA, USA), PCSK9 (cat # 443107, Biolegend, San Diego, CA, USA) and Apo CIII (cat # ab154131, Abcam, Cambridge, MA, USA) were measured in 200 μL aliquots of plasma samples, in compliance with manufacturer’s instructions. All plasma samples were assayed in duplicate. Intra-assay (mean ± SD) & inter-assay coefficients of variation were: 4.0 ± 4.1% & 17.3% for ANGPTL3, 2.2 ± 1.9% & 15.1% for PCSK9 and 12.0 ± 10.7% & 23.4% for Apo CIII, respectively.
Tumor markers
Levels of tumor markers were tested at the time of specimen collection and were retrieved from the biobank database: measurements of Carbohydrate Antigen 125 (CA125) and Human Epididymis protein 4 (HE4) have been described elsewhere [21].
Statistical analysis
The minimal sample size for a statistical power of 80% and an alpha error of 0.05 was estimated using G*power software version 3.1. Forty women with a BOL and 31 women with a HGSOC formed the two study groups. BOL and HGSOC participants were age-matched (maximal difference of ±3 years) prior to paired-group analyses to limit the confounding effect of age on both cancer outcomes and blood lipid profiles. Two-group comparisons involved two-tailed tests admitting a type I error α = 0.05, performed using SAS software version 9.4 and R software version 4.2.0. Correlation coefficients between all variables were determined by Spearman’s rank order test, computed with the corx package (courtesy of Dr. James Conigrave, https://github.com/conig/corx). A small proportion of the analytes (13% for Apo CIII and 14% for HE4) were not successfully measured. Consequently, the number of subjects may vary depending on the applied statistical model. A flow chart of the analyses performed with adjustment for sparse data is provided in supplemental Fig. S1.
Results
Biological characteristics of the cohort
Participants’ age, menopausal status, tumor staging, tumor markers levels, lipid panel and lipid-related factors levels are listed in Table 1. Mean age was 64.2 ± 9.5 y.o. for the entire cohort and did not differ between women diagnosed with BOL vs women diagnosed with HGSOC (BOL: 63.7 ± 9.4 y.o., HGSOC: 64.8 ± 9.6 y.o., P-value BOL vs HGSOC =0.13). The majority of women were in postmenopausal status (80.4 and 91.3% for the BOL and HGSOC groups respectively). Menopausal statuses distribution was homogenous between groups (P-value of 0.29 with Fisher’s Exact Test).
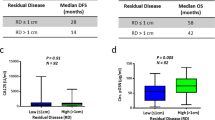
Lipid-related factors and malignancy
Plasma ANGPTL3 levels were higher in women with HGSOC compared to women diagnosed with a BOL (84 ± 29 ng/mL vs. 67 ± 31 ng/mL, P = 0.019; Table 1 and Fig. 1). The observed association remained when comparing age-matched BOL and HGSOC women (n = 31 per group, P = 0.030; Table 1). The presence of cancer did not modify Apo CIII and PCSK9 levels (see HGSOC and BOL, Table 1 and Fig. 1).
Lipid profile
Lipid profiles (TC or total cholesterol, HDL or High-density Lipoprotein cholesterol, TG or triglycerides, calculated LDL, calculated non-HDL, Apo B and Lp(a)) were similar between BOL and HGSOC groups (Table 1, all P-values > 0.05), with lipid levels comprised within the normal range [22]. A tight correlation between variables reflecting atherogenic particles (Apo B, non-HDL and LDL) was observed regardless of the group (all rho above 0.80, all P-values < 0.0001, Fig. 2). The classic inverse correlation between HDL and TG was seen in BOL (rho = − 0.70, P-value < 0.0001, Fig. 2A) and the entire cohort (rho = − 0.53, P-value < 0.0001, Fig. 2C). However, this correlation was not obtained (weak and non-significant) in HGSOC (rho = − 0.25, P-value > 0.05, Fig. 2B).
Pairwise Spearman’s correlation analyses between all variables. Pairwise correlations are presented for (A) benign ovarian lesion (BOL), (B) high-grade serous ovarian carcinoma (HGSOC) and (C) for the entire cohort (overall). In each matrix, correlation coefficients (rho) are displayed in the lower half-panel with color hues indicative of relationship strength (see rho coefficient scale) while significance is indicated in the upper half-panel (ns: non-significant, *: P < 0.05; **: P < 0.01; ***: P < 0.001; ****: P < 0.000 1)
Lipid-related factors and the lipid profile
A significant correlation between ANGPTL3 and several lipid parameters (HDL, total cholesterol, non-HDL cholesterol and LDL) was observed in BOL (Fig. 2A: HDL rho = 0.42, P-value < 0.01; TC rho = 0.45, P-value < 0.01; non-HDL rho = 0.36, P-value < 0.05; LDL rho = 0.40, P-value < 0.05) and in the entire cohort (Fig. 2C: HDL rho = 0.29, P-value < 0.05; TC rho = 0.37, P-value < 0.01; non-HDL and LDL both rho = 0.31, P-value < 0.01). No correlation between ANGPTL3 and lipid parameters were obtained in the HGSOC group (Fig. 2B). Similar correlations were obtained after age adjustment (Supplemental Fig. S2).
Apo CIII or PCSK9 levels were not correlated with the lipid profile in either group (Fig. 2). Nevertheless, Apo CIII levels correlated with TG levels in BOL and the entire cohort (Fig. 2A and C) but not in HGSOC (Fig. 2B). A weak correlation between PCSK9 and Lp(a) in BOL was also noticed (Fig. 2A).
Ovarian cancer tumor markers
CA125 and HE4 are established tumor markers of OCs and, as such, displayed significantly higher levels in HGSOC than in BOL (Table 1 and Supplemental Fig. S3). CA125 increased in HGSOC (422 ± 1358 U/mL, Table 1) vs. BOL (21 ± 12 U/mL, P-value = 1.4 × 10−7, Table 1). Likewise, HE4 levels were higher in HGSOC (539 ± 1185 pmol/L, Table 1) vs. BOL (66 ± 25 pmol/L, P-value = 2.2 × 10−7, Table 1). Also expected was the strong correlation between CA125 and HE4 in the entire cohort and HGSOC (Fig. 2C and B). Malignancy was strongly correlated with both CA125 (rho = 0.63, P < 0.0001, Fig. 2C) and HE4 (rho = 0.67, P < 0.0001, Fig. 2C) before adjusting for age as well as after (Supplemental Fig. S2C).
Discussion
Cholesterol and lipids are essential to ovarian carcinoma
It is increasingly recognized that cholesterol plays a role in cancer progression [4]. Lipids are essential to rapidly dividing cells, especially tumor cells [12, 23,24,25]. OCs are no exception: they require lipids and cholesterol for their growth [12, 23, 24]. Alterations in the various pathways (intracellular synthesis vs. dietary vs endogenous pathways) through which OCs acquire their lipids still need to be clarified [26]. The objective of the present study was to measure circulating levels of Lp(a), Apo CIII, ANGPTL3 and PCSK9 in women diagnosed either with a high-grade serous ovarian carcinoma (HGSOC) or a benign ovarian lesion (BOL), given the availability of monoclonal antibodies and antisense therapy targeting these lipid-related factors.
ANGPTL3 levels increase in HGSOC
This study was conducted to investigate the impact of malignant ovarian tumors on lipid-related factors. The study found that ANGPTL3, a well-established proangiogenic and hyperlipidemic factor, was higher in women diagnosed with HGSOC (BOL: 67 ng/mL, HGSOC: 84 ng/mL, Table 1). However, this 25% increase in ANGPTL3 levels did not result in any change in the lipid profile. Presence of HGSOC disrupted the association between ANGPTL3 and the lipid profile (see Fig. 2). It was observed that the lipid profile was similar between women with BOL and HGSOC (Table 1). It is important to note that ANGPTL3 origin (liver vs HGSOC) cannot be identified through measurements from peripheral blood venipunctures. Yet, higher expression of ANGPTL3 was reported in biopsy-confirmed HGSOC tissues by Siamakpour-Reihani (discussed below), supporting a contribution of an HGSOC-derived ANGPTL3 secretion in addition to the liver ANGPTL3 secretion.
Lipoproteins and cholesterol levels in HGSOC
Lipids and their metabolic pathways have been linked to OCs [2, 27,28,29,30]. To establish whether malignant ovarian tumor influence circulating lipids in patients, the lipid profiles of women with BOL and HGSOC were compared. No significant change in TC, triglycerides, HDL, LDL, non-HDL, Apo B nor Lp(a) levels was observed between groups. These results concur with a study from 2007 reporting no difference in TC, LDL or HDL serum levels between 30 healthy controls and 32 patients of similar age with breast or ovarian cancers [31]. They contrast with a recent meta-analysis of 12 different studies reporting a decrease in TC and HDL in patients with ovarian tumors [32]. This discrepancy may be explained by the time separating blood sampling from diagnosis. A recent analysis of prospective case-control studies showed a possible inverse association between OC risk and TC levels when measured at least 2 years before diagnosis [33]. Furthermore, previous experimental and observational studies have proposed that levels of oxidized LDL, rather than total LDL, tend to show a stronger association with tumorigenesis and metastasis in OCs [31, 34, 35]. In the present study, oxidized LDL levels were not measured.
Another interesting observation was the lack of correlation between TG and HDL cholesterol levels in HGSOC patients (Fig. 2A vs. 2B for correlations; Supplemental Figs. S2A vs S2B for partial correlations with age-adjustment). In women without cancer, the expected strong and inverse correlation between HDL cholesterol and TG was present (rho = − 0.70, P-value < 0.000 1, n = 31, Fig. 2A). Meanwhile in women with OCs, no correlation was obtained between HDL cholesterol and TG (rho = − 0.25, non-significant P-value, n = 22, Fig. 2B). The latter observation goes against the well-established pathways linking HDL and TG. Nascent HDL emerge from the liver and acquire cholesterol from peripheral cells. Cholesteryl ester transfer protein (CETP) thereafter exchanges cholesterol esters from HDL to beta-lipoproteins for TG. As HDLs are enriched in TG, HDL cholesterol decreases, which explains the negative correlation commonly observed between HDL cholesterol and TG [36, 37]. A decoupling of lipoproteins metabolic pathways is portrayed by the disappearance of this correlation in women with HGSOC, perhaps involving ANGPTL3 or CETP.
ANGPTL3 and circulating lipids in HGSOC
ANGTPL3 inhibits both hepatic and extra-hepatic lipoprotein lipases. Since lipases are responsible for the hydrolysis of triglycerides, levels of triglycerides-rich lipoproteins such as very-low-density lipoproteins (VLDL), intermediate-density lipoproteins (IDL) and LDL are increased upon ANGPTL3-mediated lipase inhibition [38], contributing to higher circulating levels of lipids.
Changes in ANGPTL3 in OC were previously reported by Siamakpour-Reihani et al [39]: RNA microarray analyses performed on ovarian tissue specimens from 51 chemotherapy-naïve patients with advanced HGSOC revealed that higher expression of ANGPTL3 was associated with shorter survival. The results of higher circulating levels of ANGPTL3 in HGSOC compared to BOL (Table 1, Fig. 1) are, therefore, a finding that is in line with results described by Siamakpour-Reihani et al., but only to a certain extent, as survival data for HGSOC patients recruited between 2017 and 2020 are currently unavailable. Elevated levels of ANGPTL3 were not coupled to an elevation of HDL levels in HGSOC (Fig. 2B and Supplemental Fig. S2B). This observation is unexpected in light of known pathways governing the relationships between ANGPTL3, HDL and TG [40, 41]. Correlations between ANGPTL3 and other components of the lipid panel, namely TC and non-HDL (Fig. 2A, rho = 0.45, P-value < 0.01 and rho =0.36, P-value < 0.05 respectively), also weakened in the HGSOC group (Fig. 2B, rho = 0.32 and rho = 0.25 respectively, all P-values non-significant). These observations evoke a rupture in the interrelationship between ANGPTL3 and cholesterolemia in HGSOC.
Possible implications of ANGPTL3 increase in HGSOC
Lipid profile similarity between BOL and HGSOC (Table 1), despite increased ANGPTL3 levels in HGSOC (Fig. 1), was compatible with the absence of correlation between lipids and ANGPTL3 in HGSOC (Fig. 2B). This implies that presence of OC disrupts the relationship between ANGPTL3 and lipid levels in this cohort. One explanation could be that circulating lipids are taken up by tumor cells, inducing an upregulation of the hepatic secretion of ANGPTL3 to maintain a preset cholesterolemia. Alternatively, increased levels of ANGPTL3 in HGSOC could reflect local production by the tumor itself [39]. In such context, ANGPTL3 may be secreted in the tumor microenvironment to mediate pro-angiogenic and pro-metastatic functions, as noted in other cancers [42, 43]. But the latter does not exclude other possible roles played by ANGPTL3, such as in lipolysis. The decoupling between circulating ANGPTL3 and lipid levels in OCs as well as the origin of ANGPTL3 increased secretion (tumoral vs hepatic) need to be further investigated.
Study limitations and strengths
The present work is a cross-sectional study and therefore precludes any causal association between higher ANGPTL3 levels and OC. Nonetheless, the analyses showed an increase of ANGPTL3 levels in women with HGSOC compared to women with BOL, a finding in line with previous data reported by Siamakpour-Reihani et al. Circulating atherogenic particles showed strong correlative association with each other (Apo B, LDL, non-HDL), providing an internal validation for all steps conducted (from measurements of lipid-related blood parameters to statistical analyses). In that regard, correlations between ANGPTL3 and circulating lipids in the control group is a finding that will likely be observed in a larger cohort of women [44] (Fig. 2A).
Plasma samples came from non-fasting participants, which may elevate TG levels and introduce bias in LDL values calculated with the Friedewald equation. Despite the use of non-fasting patients’ samples, measured TG levels were < 5 mmol/L [45], which means that calculated LDL levels were not biased by participants’ fasting/non-fasting status. The missing information included participants’ ethnicity, hormone-replacement therapy use [46] and cholesterol-lowering drugs [47], factors that could have affected the lipid profile and lipid-related factors.
Controls corresponded to women presenting a non-cancerous ovarian lesion. These lesions (fibromas and benign cysts) have not been associated with variations in lipid profile. Therefore, women diagnosed with BOL should not have lipid profiles different from lipid profiles of healthy women.
Women did not differ in age and had similar lipid profiles in the control vs. case groups (Table 1). Despite the absence of intergroup differences, age was considered as a potential biological confounder in analyses (see Table 1 for paired comparison, Supplemental Fig. S2 for partial correlation analyses).
The limited number of individuals belonging to tumor stages I, II and IV (Table 1, n = 3, n = 3 and n = 4, respectively) resulted in unequal group sizes and lack of statistical power in group comparisons, which did not permit to study ANGPTL3 and other analytes changes through the different stages. The observed low number of samples belonging to women in stage I and II is in line with the fact that HGSOC is frequently diagnosed at an advanced disease stage, contributing to the high lethality of HGSOC. A small number of participants increases the risk of dismissing real differences due to lower statistical power. Nevertheless, analyses on small groups represent a cost-effective step for identifying parameters worth further investigation, such as ANGPTL3 in OCs. The fact that well-established associations are observed in this cohort of 71 women (ex; the strong correlation between atherogenic measures LDL, Apo B and Non-HDL) suggests that the increase in ANGPTL3 in HGSOC is a real phenomenon which needs to be further investigated. Significant results with narrow confidence intervals generally have good predictive value for reproducibility in larger groups [48].
Conclusions
The main finding from this study was an elevation of plasma ANGPTL3 levels in women diagnosed with epithelial high-grade serous ovarian carcinoma, along with a decoupling between ANGPTL3 levels and the lipid profile in HGSOC. Given the availability of a monoclonal antibody against ANGPTL3 already used in patients with familial hypercholesterolemia, these results warrant further investigation of whether ANGPTL3 inhibition has therapeutic potential in ovarian cancers. Confirmation of ANGPTL3 inhibition as a therapeutical target will permit rapid repositioning of Evinacumab in OC.
Availability of data and materials
Datasets generated for this study are not publicly available for the sake of participants’ privacy and confidentiality surrounding current ancillary studies underway but may be made available by the corresponding author upon reasonable request.
Abbreviations
- ANGPTL3:
-
Angiopoietin protein-like 3
- Apo B:
-
Apolipoprotein B
- Apo CIII:
-
Apolipoprotein CIII
- BOL:
-
Benign ovarian lesion
- HDL:
-
High-density lipoprotein cholesterol
- HGSOC:
-
High-grade serous ovarian cancer
- IDL:
-
Intermediate density lipoprotein
- LDL:
-
Low-density lipoprotein cholesterol
- Lp(a):
-
Lipoprotein a
- mab:
-
Monoclonal antibody
- OC:
-
Ovarian cancer
- PCSK9:
-
Proprotein convertase subtilisin/kexin type 9
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- VLDL:
-
Very low-density lipoprotein
- y.o.:
-
Years old
References
Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD, Gaudet MM, Jemal A, Siegel RL. Ovarian Cancer statistics, 2018. CA-Cancer J Clin. 2018;68:284–96.
He J, Siu MKY, Ngan HYS, Chan KKL. Aberrant cholesterol metabolism in ovarian Cancer: identification of novel therapeutic targets. Front Oncol. 2021;11:738177.
Criscuolo D, Avolio R, Calice G, Laezza C, Paladino S, Navarra G, et al. Cholesterol homeostasis modulates platinum sensitivity in human ovarian Cancer. Cells. 2020;9.
Xu HJ, Zhou S, Tang QL, Xia HW, Bi F. Cholesterol metabolism: New functions and therapeutic approaches in cancer. Biochim Biophys Acta Rev Cancer. 2020;1874.
Gohlke BO, Zincke F, Eckert A, Kobelt D, Preissner S, Liebeskind JM, et al. Real-world evidence for preventive effects of statins on cancer incidence: a trans-Atlantic analysis. Clin Transl Med. 2022;12.
Revilla G, Cedo L, Tondo M, Moral A, Perez JI, Corcoy R, Lerma E, Fuste V, Reddy TS, Blanco-Vaca F, et al. LDL, HDL and endocrine-related cancer: from pathogenic mechanisms to therapies. Semin Cancer Biol. 2021;73:134–57.
Feng JL, Qin XW. Does adherence to lipid-lowering medications improve cancer survival? A nationwide study of breast and colorectal cancer, and melanoma. Br J Clin Pharmacol. 2021;87:1847–58.
Elmore RG, Ioffe Y, Scoles DR, Karlan BY, Li AJ. Impact of statin therapy on survival in epithelial ovarian cancer. Gynecol Oncol. 2008;111:102–5.
Akinwunmi B, Vitonis AF, Titus L, Terry KL, Cramer DW. Statin therapy and association with ovarian cancer risk in the New England case control (NEC) study. Int J Cancer. 2019;144:991–1000.
Froelich W. The role of lipophilic statins in reducing epithelial ovarian Cancer. Oncology. Times. 2020;42.
Feng JL, Dixon-Suen SC, Jordan SJ, Webb PM. Statin use and survival among women with ovarian cancer: an Australian national data-linkage study. Br J Cancer. 2021;125:766–71.
Kuzu OF, Noory MA, Robertson GP. The role of cholesterol in Cancer. Cancer Res. 2016;76:2063–70.
Ravnskov U, Rosch PJ, McCully KS. Statins do not protect against Cancer: quite the opposite. J Clin Oncol. 2015;33:810–1.
Nielsen SF, Nordestgaard BG, Bojesen SE. Statin use and reduced Cancer-related mortality. N Engl J Med. 2012;367:1792–802.
Wang AG, Aragaki AK, Tang JY, Kurian AW, Manson JE, Chlebowski RT, Simon M, Desai P, Wassertheil-Smoller S, Liu SM, et al. Statin use and all-cancer survival: prospective results from the Women’s Health Initiative. Br J Cancer. 2016;115:129–35.
Ravnskov U. Comment on ‘Statin use and all-cancer survival: prospective results from the Women’s Health Initiative. Br J Cancer. 2017;116.
Jones A, Peers K, Wierzbicki AS, Ramachandran R, Mansfield M, Dawson C, Ochoa-Ferraro A, Soran H, Jenkinson F, McDowell I, et al. Long-term effects of volanesorsen on triglycerides and pancreatitis in patients with familial chylomicronaemia syndrome (FCS) in the UK early access to medicines scheme (EAMS). Atherosclerosis. 2023;375:67–74.
Raal FJ, Rosenson RS, Reeskamp LF, Hovingh GK, Kastelein JJP, Rubba P, Ali S, Banerjee P, Chan KC, Gipe DA, et al. Evinacumab for homozygous familial hypercholesterolemia. N Engl J Med. 2020;383:711–20.
Gupta M, Mancini GBJ, Wani RJ, Ahooja V, Bergeron J, Manjoo P, Pandey AS, Reiner M, Beltran J, Oliveira T, Mackinnon ES. Real-world insights into Evolocumab use in patients with hyperlipidemia: Canadian analysis from the ZERBINI study. CJC Open. 2022;4:558–67.
Friedewald WT, Fredrickson DS, Levy RI. Estimation of concentration of low-density lipoprotein cholesterol in plasma, without use of preparative ultracentrifuge. Clin Chem. 1972;18:499−+.
Furrer D, Gregoire J, Turcotte S, Plante M, Bachvarov D, Trudel D, et al. Performance of preoperative plasma tumor markers HE4 and CA125 in predicting ovarian cancer mortality in women with epithelial ovarian cancer. PLoS One. 2019;14.
Eastern Ontario Regional Laboratory Association. EORLA regional biochemistry recommended reference intervals. [https://mcc.ca/objectives/normal-values/].
Ding X, Zhang W, Li S, Yang H. The role of cholesterol metabolism in cancer. Am J Cancer Res. 2019;9:219–27.
Cruz PM, Mo H, McConathy WJ, Sabnis N, Lacko AG. The role of cholesterol metabolism and cholesterol transport in carcinogenesis: a review of scientific findings, relevant to future cancer therapeutics. Front Pharmacol. 2013;4:119.
Giacomini I, Gianfanti F, Desbats MA, Orso G, Berretta M, Prayer-Galetti T, Ragazzi E, Cocetta V. Cholesterol metabolic reprogramming in Cancer and its pharmacological modulation as therapeutic strategy. Front Oncol. 2021;11:682911.
Cheng CM, Geng F, Cheng X, Guo DL. Lipid metabolism reprogramming and its potential targets in cancer. Cancer Commun. 2018;38.
Iwahashi N, Ikezaki M, Fujimoto M, Komohara Y, Fujiwara Y, Yamamoto M, et al. Lipid droplet accumulation independently predicts poor clinical prognosis in high-grade serous ovarian carcinoma. Cancers. 2021;13.
Chen LM, Ma WL, Cheng WC, Yang JC, Wang HC, Su YT, Ahmad A, Hung YC, Chang WC. Targeting lipid droplet lysophosphatidylcholine for cisplatin chemotherapy. J Cell Mol Med. 2020;24:7187–200.
Sanz DJ, Raivola J, Karvonen H, Arjama M, Barker H, Murumagi A, et al. Evaluating targeted therapies in ovarian Cancer metabolism: novel role for PCSK9 and second generation mTOR inhibitors. Cancers. 2021;13.
Nieman KM, Kenny HA, Penicka CV, Ladanyi A, Buell-Gutbrod R, Zillhardt MR, Romero IL, Carey MS, Mills GB, Hotamisligil GS, et al. Adipocytes promote ovarian cancer metastasis and provide energy for rapid tumor growth. Nat Med. 2011;17:1498-U1207.
Delimaris L, Faviou E, Antonakos G, Stathopoulou E, Zachari A, Dionyssiou-Asteriou A. Oxidized LDL, serum oxidizability and serum lipid levels in patients with breast or ovarian cancer. Clin Biochem. 2007;40:1129–34.
Onwuka JU, Okekunle AP, Olutola OM, Akpa OM, Feng RN. Lipid profile and risk of ovarian tumours: a meta-analysis. BMC Cancer. 2020;20.
Trabert B, Hathaway CA, Rice MS, Rimm EB, Sluss PM, Terry KL, Zeleznik OA, Tworoger SS. Ovarian Cancer risk in relation to blood cholesterol and triglycerides. Cancer Epidemiol Biomark Prev. 2021;30:2044–51.
Scoles DR, Xu X, Wang HM, Tran H, Taylor-Harding B, Li A, Karlan BY. Liver X receptor agonist inhibits proliferation of ovarian carcinoma cells stimulated by oxidized low density lipoprotein. Gynecol Oncol. 2010;116:109–16.
Deng CF, Zhu N, Zhao TJ, Li HF, Gu J, Liao DF, et al. Involvement of LDL and ox-LDL in Cancer development and its Therapeutical potential. Front Oncol. 2022;12.
Marshall WJ. MLaAD: Clinical Chemistry. In: Clinical Chemistry. 8th ed. Elsevier; 2017. p. 298–9.
Barter PJ, Brewer HB, Chapman MJ, Hennekens CH, Rader DJ, Tall AR. Cholesteryl Ester Transfer Protein. Arterioscler Thromb Vasc Biol. 2003;23:160–7.
Kersten S. Angiopoietin-like 3 in lipoprotein metabolism. Nat Rev Endocrinol. 2017;13:731–9.
Siamakpour-Reihani S, Owzar K, Jiang C, Turner T, Deng YW, Bean SM, Horton JK, Berchuck A, Marks JR, Dewhirst MW, Secord AA. Prognostic significance of differential expression of angiogenic genes in women with high-grade serous ovarian carcinoma. Gynecol Oncol. 2015;139:23–9.
Christopoulou E, Elisaf M, Filippatos T. Effects of angiopoietin-like 3 on triglyceride regulation, glucose homeostasis, and diabetes. Dis Markers. 2019;2019.
Harada M, Yamakawa T, Kashiwagi R, Ohira A, Sugiyama M, Sugiura Y, et al. Association between ANGPTL3, 4, and 8 and lipid and glucose metabolism markers in patients with diabetes. PLoS One. 2021;16.
Zhong LJ, Tang L, He XX. Angiopoietin-like 3 (ANGPTL3) drives cell proliferation, migration and angiogenesis in cervical cancer via binding to integrin alpha v beta 3. Bioengineered. 2022;13:2971–80.
Wang YX, Yi Y, Pan SL, Zhang YH, Fu J, Wu XL, et al. Angiopoietin-like protein 3 promotes colorectal cancer progression and liver metastasis partly via the mitogen-activated protein kinase 14 pathway. Mol Carcinog. 2023;62.
Robciuc MR, Maranghi M, Lahikainen A, Rader D, Bensadoun A, Öörni K, Metso J, Minicocci I, Ciociola E, Ceci F, et al. Angptl3 deficiency is associated with increased insulin sensitivity, lipoprotein lipase activity, and decreased serum free fatty acids. Arterioscler Thromb Vasc Biol. 2013;33:1706–13.
Nordestgaard BG, Langsted A, Mora S, Kolovou G, Baum H, Bruckert E, Watts GF, Sypniewska G, Wiklund O, Borén J, et al. Fasting is not routinely required for determination of a lipid profile: clinical and laboratory implications including flagging at desirable concentration cut-points—a joint consensus statement from the European Atherosclerosis society and European Federation of Clinical Chemistry and Laboratory Medicine. Eur Heart J. 2016;37:1944–58.
Ghosh M, Galman C, Rudling M, Angelin B. Influence of physiological changes in endogenous estrogen on circulating PCSK9 and LDL cholesterol. J Lipid Res. 2015;56:463–9.
Reeskamp LF, Tromp TR, Huijgen R, Stroes ESG, Hovingh GK, Grefhorst A. Statin therapy reduces plasma angiopoietin-like 3 (ANGPTL3) concentrations in hypercholesterolemic patients via reduced liver X receptor (LXR) activation. Atherosclerosis. 2020;315:68–75.
Hackshaw A. Small studies: strengths and limitations. Eur Respir J. 2008;32:1141–3.
Acknowledgements
The authors express their gratitude to the study participants, to Mrs. Magdalena Batchvarova for her help with samples selection and to the staff from the Core Laboratories of the Hôpital de l’Enfant-Jésus and Centre Hospitalier de l’Université Laval, especially to Mrs. Josée Letourneau and Mr. Eric Perron-Malenfant, for their help with analytes measurements on automated platforms (ex: lipid profile). Plasma samples were provided by the tissue biobank repository and database of the Réseau de Recherche sur le Cancer, the Cancer Research Center of the CHU de Québec-Université Laval and the Fonds de Recherche du Québec en Santé (FRQS). E.WC. was partly supported by a donation from an anonymous family to the Oncology research axis of the CHU de Québec-Université Laval. This work has been made possible through an establishment grant from the Oncology Research axis of the CHU de Québec-Université Laval Research Center and the Medicine faculty of Laval University.
Funding
This project was funded with an establishment grant for new investigators of the Oncology research axis from the CHU de Québec.
Author information
Authors and Affiliations
Contributions
A. G. provided the funding for the present work, devised the hypothesis, rationale of the project, the main conceptual ideas and the logistic details related to plasma lipids profiling on clinical platforms. P. D. and D. B. provided plasma samples needed for all the experiments. F–H. J. undertook the required procedures to obtain the institutional ethics committee’s approval to perform the study. F–H. J. and E. WC. performed ELISA assays. C. D., A-C. B. and E. WC. performed the statistical analyses. A. G. and E. WC. wrote the manuscript with input from all authors. E. WC., F–H. J., P.D., D.B., C. D., F. C., A-C. B., J. B., SOA.L, NG. S. and A. G. revised and discussed all results and contributed to the final manuscript within their scope of expertise. All author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Plasma samples analyzed in the present study were from women who had signed an informed consent to participate to the “FRQ-S – Réseau de Recherche sur le Cancer (RRCancer) - Biobanque des tumeurs gynécologiques” biobank registry (biobank reference no 2012–846). Ethics approval for the present study was obtained from relevant research ethics committees of the CHU de Québec (2022–6170).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Fig. S1.
Flow chart of analyses performed on the study population. Fig. S2. Pairwise Spearman’s partial correlation analyses between all variables, with age-adjustment. Partial correlations based on age-adjustment are presented for (A) benign ovarian lesions (BOL), (B) high-grade serous ovarian carcinoma (HGSOC) and (C) the entire cohort (overall). Correlation coefficients (rho) are displayed in each matrix lower half-panel with color hues indicative of relationship strength (see rho coefficient scale). Correlation significance is expressed in upper half-panel (ns: non-significant, *: P < 0.05; **: P < 0.01; ***: P < 0.001; ****: P < 0.000 1). Fig. S3. CA125 and HE4 plasma levels between BOL and HGSOC. Significant level increase of tumor markers CA125 (BOL: n = 40, HGSOC: n = 31, P = 1.4E-7) and HE4 (BOL: n = 38, HGSOC: n = 23, P = 2.2E-7) was found in HGSOC compared to BOL. ****: P < 0.000 1.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wong Chong, E., Joncas, FH., Douville, P. et al. Pre-operative levels of angiopoietin protein-like 3 (ANGPTL3) in women diagnosed with high-grade serous carcinoma of the ovary. Lipids Health Dis 23, 59 (2024). https://doi.org/10.1186/s12944-024-02038-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02038-8