Abstract
Background
The aim was to establish a 10-year dyslipidemia incidence model, investigating novel anthropometric indices using exploratory regression and data mining.
Methods
This data mining study was conducted on people who were diagnosed with dyslipidemia in phase 2 (n = 1097) of the Mashhad Stroke and Heart Atherosclerotic Disorder (MASHAD) study, who were compared with healthy people in this phase (n = 679). The association of dyslipidemia with several novel anthropometric indices including Conicity Index (C-Index), Body Roundness Index (BRI), Visceral Adiposity Index (VAI), Lipid Accumulation Product (LAP), Abdominal Volume Index (AVI), Weight-Adjusted-Waist Index (WWI), A Body Shape Index (ABSI), Body Mass Index (BMI), Body Adiposity Index (BAI) and Body Surface Area (BSA) was evaluated. Logistic Regression (LR) and Decision Tree (DT) analysis were utilized to evaluate the association. The accuracy, sensitivity, and specificity of DT were assessed through the performance of a Receiver Operating Characteristic (ROC) curve using R software.
Results
A total of 1776 subjects without dyslipidemia during phase 1 were followed up in phase 2 and enrolled into the current study. The AUC of models A and B were 0.69 and 0.63 among subjects with dyslipidemia, respectively. VAI has been identified as a significant predictor of dyslipidemias (OR: 2.81, (95% CI: 2.07, 3.81)) in all models. Moreover, the DT showed that VAI followed by BMI and LAP were the most critical variables in predicting dyslipidemia incidence.
Conclusions
Based on the results, model A had an acceptable performance for predicting 10 years of dyslipidemia incidence. Furthermore, the VAI, BMI, and LAP were the principal anthropometric factors for predicting dyslipidemia incidence by LR and DT models.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Dyslipidemia is impaired lipid metabolism defined as increased levels of total cholesterol (TC), triglycerides (TG), and low-density lipoprotein cholesterol (LDL-C) and decreased levels of high-density lipoprotein cholesterol (HDL-C), that established as an independent predictor of cardiovascular and cerebrovascular occurrences [1, 2]. Cardiovascular disease (CVD) is responsible for substantial declines in both the quality of life and lifespan, while simultaneously imposing a considerable economic strain on healthcare systems worldwide [3]. The prevalence of dyslipidemia depends on geography; however, it has been estimated that more than 50% of adults (non-Hispanic white, non-Hispanic black, Mexican American, and urban and rural India) have dyslipidemia [4,5,6]. Also, the prevalence of dyslipidemia is noticeable in Iran, according to a meta-analysis that was published in 2014 with 29 articles and one unpublished data, the approximate prevalence of dyslipidemia in Iranian women and men, rural and urban populations for increased plasma concentration of triglyceride, cholesterol, LDL-C respectively were 46%, 41.6%, 35.5%; and for decreased HDL-C was 43.9% [7].
Dyslipidaemia is highly related to obesity [8]; anthropometric parameters have been employed for assessing obesity in both epidemiological and clinical investigations [9]. Significant differences in anthropometric parameters have been observed between individuals with dyslipidemia and those without, indicating a notable difference between the two groups, and a direct relationship between dyslipidemia and Body Mass Index (BMI) has been reported [10, 11], however, there are some controversies [12]. Novel anthropometric indices have been introduced for a better description of body shaping during the last decades [13,14,15]. It has been claimed that some of them are associated with all causes of mortality risk [16], cardio-metabolic risk [14], impaired glucose tolerance [17], and type 2 diabetes mellitus (T2DM) [18] dyslipidemia [19], but there are some controversies [20].
Rodolfo Valdez et al., introduced the Conicity Index (C-Index) to evaluate obesity [13]. Thomas et al. suggested the Body Roundness Index (BRI) as a predictor of visceral adiposity tissue that can be used to evaluation of health status [15]. Visceral Adiposity Index (VAI) can be calculated from waist circumference [21] and BMI, along with assessing TG and HDL-C. So it is a convenient index for evaluating visceral fat dysfunction. As such, VAI could be beneficial in clinical practice, population studies, and estimating the cardio-metabolic risk linked to visceral obesity [14]. Lipid Accumulation Product [22] proved to be more efficacious than BMI for discerning United States adults at risk for CVD and it was defined by two measurements waist circumference (WC) and TG [23]. Abdominal Volume Index (AVI) has been demonstrated as a reliable and convenient anthropometric tool for estimating overall abdominal volume and has a strong correlation with Impaired Glucose Tolerance (IGT) and DM [18]. Also, AVI exhibited significant potential as a diagnostic tool for metabolic syndrome [24]. The association between AVI and atherogenic dyslipidemia has been reported [19].
A Body Shape Index (ABSI) has been developed as a new indicator [25]. It was a strong predictor for all causes of mortality [16]. One study showed that the reliability of this index and experimental measurement of lipid profile can be equal [26]. Body Adiposity Index (BAI) is a formula that estimates the adiposity of people without using weight [27]. Also, Weight-Adjusted-Waist Index (WWI) is a promising alternative marker for obesity and is associated with adverse health consequences [28]. Values pertaining to the Body Surface Area (BSA) are frequently employed within the medical domain, primarily for the purpose of computing the dosages of chemotherapeutic agents and determining the index of cardiac output [29].
To the best of our knowledge, there is no other predictive model for dyslipidemia incidence prediction, based on novel anthropometric indicators using artificial intelligence. According to the high prevalence of dyslipidemia and its relation to CVD, this study aimed to establish a 10-year predicting model for dyslipidemia based on novel anthropometric indices, using exploratory regression models and data mining.
Methods
Study population
This cohort study was conducted on all non-dyslipidemia participants from the Mashhad stroke and heart atherosclerotic disorder (MASHAD) cohort study; a 10-year cohort from northeastern Iran, in which all participants signed the written consent forms [30]. Among 9704 subjects of first phase of the MASHAD study, 2230 people did not have dyslipidemia. Of those, 1776 were evaluated in Phase 2 follow-up in 2019 (Fig. 1). The study protocol was approved by the Ethical Committee of Mashhad University of Medical Sciences (ID = IR.MUMS.MEDICAL.REC.1402.262).
Baseline examination
Dyslipidemia was defined as a serum TC <200 mg/dl (5.18 mmol/l), LDL-C 130 mg/dl (3.36 mmol/l), or TG 150 mg/dl (1.69 mmol/l), or HDL-C <40 mg/dl (1.03 mmol/l) in men and <50 mg/dl (1.30 mmol/l) in women [31]. If serum TG concentrations were lower than 400 mg/dl; LDL-C was computed from the serum TG, TC, and HDL-C concentrations expressed in mg/dl using the Friedewald formula [32].
A registered nurse measured anthropometric measurements such as weight, height, Hip Circumference (HC), Mid-arm Circumference (MAC), and WC. Waist-to-hip Ratio (WHR), BMI, BAI, C-Index, BRI, WWI, AVI, Lipid Accumulation Product (LAP), VAI, and BSA were computed utilizing the formulas presented in the Table of the Supplementary Appendix 1. Within measurements of height and weight wanted participants to wear light clothes and no shoes. According to the World Health Organization recommendations, a BMI between 25 and 29.99 kg/m2 was categorized as overweight and a BMI≥30 kg/m2 was classified as obese.
A current smoker was identified as one who smokes cigarettes daily, whereas an ex-smoker was defined as an individual who previously smoked daily, but no longer does so, and non-smoker subjects were acquired. Psychometric tests were conducted with Beck’s anxiety inventory to calculate an anxiety score, which was interpreted as follows: 0-7, minimal level of anxiety; 8-15, mild anxiety; 16-25, moderate anxiety; and 26-63, severe anxiety. The Beck’s Depression Inventory-II (BDI-II) was also employed to evaluate depression scores, with the following cut-offs: 0-13, minimal depression; 14-19, mild depression; 20-28, moderate depression; and 29-63, severe depression.
Statistical analysis
All data were analyzed using the R Statistical Software (v4.1.2; R Core Team 2021), The IBM SPSS Statistics (Version 27), and MedCalc statistical software version 13. All continuous data are expressed as mean ± SD and frequency (%) for categorical. All P-value < 0.05 was regarded as statistically significant. We used a t-test for continuous variables, and the Mann–Whitney test for non-normal data was employed to compare the mean or median of subjects with and without Dyslipidemia. The chi-square test was implemented to investigate the association between the categorical variables and the binary outcome, dyslipidemias. Data was split into train and test datasets using the holdout method as 75% and 25 % respectively.
Logistic Regression (LR) was performed with dyslipidemia incidents as the response variable and anthropometric factors. Some of these variables have collinearity, which in LR method were eliminated. To assess the multicollinearity between independent variables the variance inflation factor (VIF) as well as the computation of correlation coefficient was used. Generally, a correlation higher than 0.95 was considered a highly correlated variable that helps to recognize the possibility for multicollinearity. The logistic regression was used to compute the odds ratios (OR) with their 95% confidence interval. To compare the models and study the model’s goodness of fit test, the deviance as a likelihood ratio statistic was applied.
Decision tree model
The data put into a data mining approach and the Decision Tree (DT) was drawn to form a predictive model of anthropometric measurements. A decision tree is a non-parametric method named regarding the nature of the target variable. The aim of a decision tree is to form a predictive model in terms of predictor variables. This paper uses the CHIAD technique in DT. CHAID can be used for prediction as well as classification, and for detection of interaction between variables. There is a different algorithm written to assemble a decision tree, which can be utilized by the problem a few of the commonly used algorithms are (CART, ID3, C4.5, and CHAID). To find the most dominant feature, chi-square tests will use that is also called CHAID.
Data mining techniques were used to investigate the relationship between anthropometric predictors and binary response variables (dyslipidemia, and non-dyslipidemia). So, the main objective of this study was to anticipate dyslipidemias using the DT model and to determine their associated factors, especially anthropometric markers. For this purpose, the dataset was randomly split into two parts: training data, and test data (25%-75%). The training dataset was utilized to develop the DT model, which was then validated using test data (25%) that hadn't been used during training. DT algorithms use splitting criteria to break a node into branches to reduce the impurity of a node. This criterion provides a rate for every predictor variable.
Results
Characteristics of the study population
From the total study population of 9704 participants in phase 1, about 1776 non-dyslipidemia individuals whom were followed in phase 2 (10-year follow-up) enrolled to the study. As shown in Fig. 1, a total of 1097 subjects were dyslipidemic in the second phase of the study.
Table 1 shows that 1776 participants consisted of 679 with non-dyslipidemia and 1097 individuals suffered from dyslipidemia during phase 2 of the study. There were 876 (49.3%) females of whom 586 (53.4%) had dyslipidemia and 900 males (50.7%) of those 511(46.6%) had dyslipidemia. The serum glucose level was significantly higher in subjects with dyslipidemia than in non-dyslipidemias (P = 0.002). It is noticeable that close to 60% were overweight (37.3%) or obese (19.2%) with a significantly higher rate of dyslipidemia in overweight (39.1% vs 34.3%) and obese (22% vs 14.6%) participants. Apparently, smoking had no significant association with dyslipidemia (P = 0.949). The variables C-Index, BRI, VAI, LAP, and AVI all showed significantly higher in subjects with dyslipidemia compared to individuals without dyslipidemia (P < 0.001), and the rest of continuous variables were non-significant differences between the two groups.
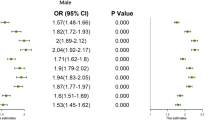
The association between anthropometric measurements and dyslipidemia using Logistic Regression (LR) model
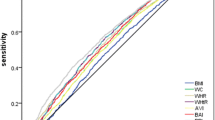
In Table 2, the result of LR is presented based on two models. Model A, including the variables VAI, BRI, and BMI, and Model B included all variables in Model A adjusted for physical activity level (PAL), age, sex, anxiety score, depression score, smoking status, percent of daily energy intake from fat, percent of energy intake from carbohydrate and percent of energy intake from protein. The LR applied to each anthropometrics variable with inclusion in the model based on a 20% level of significance (see Table 2 crude OR (95% CI)), the results lead to including the variables VAI, BRI, and BMI and they form model A. Furthermore, model B contains all variables in Model A plus the confounder variables explained above. The variable VAI is positively associated with dyslipidemias and significant in all 3 models (P < 0.001), but BRI and BMI are only significant in the crude model (P < 0.001). Clearly, the variable VAI is the most remarkable predictor of dyslipidemia. In model A, the odds of individuals with dyslipidemia for each unit increasing in VAI is 3.4 times of those without dyslipidemias (OR: 3.40, (95% CI: 2.63, 4.38)) adjusting for BRI and BMI. Similarly in model B, VAI is a significant predictor of dyslipidemias (OR: 2.81, (95% CI: 2.07, 3.81)) adjusting for all other variables. Moreover, it was found that model B has a significantly better fit than model A in terms of deviance (2139.2 vs 1460.6, P = < 0.001). The ROC curve in train and test in model A and model B are shown in Fig. 2 and Fig. 3 respectively. Also, the sensitivity of model A (87% for the train vs 87% for the test) is better than model B (86% for the train vs 81% for the test).
LR method for model A, in Table 2
LR method for model B, in Table 2
Supplementary Appendix 2 has summarized the association between anthropometric measurements and dyslipidemia using LR Model.
The Association between Anthropometric measurements and dyslipidemia using Decision Tree (DT) Model
Figure 4 and Fig. 5 shows the outcomes of the DT testing for anthropometry factors and anthropometry factors with confounding factors. In the first case, the DT algorithm determined the various dyslipidemia risk factors and categorized them into 2 layers. According to the DT model, the first variable [33] has the highest significance for classifying data, while the subsequent variables have lower significance. Figure 4 illustrates that VAI, followed by LAP, has the greatest impact on the dyslipidemia presence risk. Participants with VAI \(\le\) 0.64 had lower dyslipidemia, according to the DT model than those with higher VAI and LAP levels (0.5 vs. 0.5 incident rate). Higher VAI and LAP were more commonly associated with Dyslipidemia. Table 3 illustrates the specific dyslipidemia rules developed by the DT model. Therefore VAI and LAP were thus determined to be the most crucial variables in the DT model and to predict the dyslipidemia incidence.
In the second case (with disturbances) DT algorithm determined the various dyslipidemia risk factors with disturbances and categorized them into 3 layers. According to the DT model, the first variable [33] has the highest significance for classifying data, while the subsequent variables have lower significance. Figure 5 illustrates that VAI, followed by BMI, LAP, and depression score has the greatest impact on the dyslipidemia presence risk. Participants with VAI \(\le\) 0.63 had lower dyslipidemia, according to the DT model than those with higher BMI, LAP, and depression score levels (0.333 vs. 0.667 incident rate). Higher BMI and LAP were more commonly associated with dyslipidemia.
Variables with the best rate were selected to be included in the model. Table 4 illustrates the confusion matrix of the decision trees were used to evaluate the accuracy, precision, and specificity.
Discussion
Generally, this study has shown that VAI is the most important predictor for the incidence of dyslipidemia in all models. Moreover, BMI and LAP were identified as the most critical variables after VAI in the decision tree model to predict dyslipidemia incidence.
A 10-year predicting model for the incidence of dyslipidemia was established in the current study. To the best of our knowledge, there is no similar study that has a predictive model design, using artificial intelligence and includes novel anthropometric indicators. The results have shown that VAI is a strong predictor for 10-year anticipation of dyslipidemia. Although, BMI and LAP were identified as the most important variables in the prediction of dyslipidemia incidence.
The results of previous studies are in line with current study that introduced VAI as the most powerful prognosticator of atherogenic dyslipidemia [19]. Also, it has been found that LAP was a beneficial factor in predicting the incidence of dyslipidemia. Recently, Zhou, Y et al., showed that LAP was more associated with dyslipidemia than BMI among university staff in a cross-sectional study [34]. It has been stated that the BRI's potential role in predicting dyslipidemia is comparable with BMI but not stronger [35]. It has been shown that BRI can be a good indicator for dyslipidemia prediction in women but not in men [36]. Maybe this difference relates to the diversity of visceral adiposity between genders.
It has been shown that VAI serves as a significant tool for determining insulin sensitivity, and its elevation exhibits a robust correlation with the risk of developing cardio-metabolic disorders [14]. Insulin resistance plays a crucial role in the metabolism of very low-density lipoprotein (VLDL), including its effect of elevating the synthesis of hepatic VLDL triglycerides (VLDL-TGs) [37, 38]. The enhanced synthesis of VLDL-TGs is associated with the escalated production of hepatic Apolipoprotein B-100 (apo B-100) [37,38,39]. This leads to hypertriglyceridemia, increases in particle number exhibited by VLDL apo B-100 and decreased HDL-C concentrations [39]. Insulin resistance is also associated with an increase in hepatic triglyceride lipase (HTGL), which may result in the accelerated clearance of HDL-C and a reduction in HDL-C [40].
The reason for the difference between previous findings and current study results can be due to the difference in the included indicators of the studies and the statistical methods used.
Study strengths and limitations
This was a 10-year follow-up cohort study with a large population, using novel anthropometric indices for the prediction of dyslipidemia incidence. Using analytical techniques, including the machine learning algorithms such as the decision tree method and Logistic Regression Model was another robustness of the study. To the best of our knowledge, the design of previous studies was cross-sectional. There is no longitudinal study among subjects without dyslipidemia with a 10-year follow-up.
To explicate these findings the following limitations ought to be acknowledged: Possibly, some individuals with dyslipidemia were geriatric (aged ≥ 65 years); however, current research only comprised participants aged 35 to 65 years old. Also, some factors such as epigenetics, can be included in future studies.
Conclusion
The present study established a 10-year predicting model for dyslipidemia incidence, for the first time. Generally, current study has shown that in all models VAI is the most important predictor for dyslipidemia incidence. This finding emphasis on the importance of visceral obesity to dyslipidemia incidence and suggest to target the visceral obesity improvement for decreasing the incidence of dyslipidemia.
Availability of data and materials
The data will be available upon a reasonable request from the corresponding author.
References
Detection NCEPEPo, Adults ToHBCi. Third report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III): The Program; 2002.
Alloubani A, Nimer R, Samara R. Relationship between hyperlipidemia, cardiovascular disease and stroke: a systematic review. Curr Cardiol Rev. 2021;17(6):52–66.
Amini M, Zayeri F, Salehi M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-to-incidence ratio: results from global burden of disease study 2017. BMC Public Health. 2021;21(1):401.
Brown CD, Higgins M, Donato KA, Rohde FC, Garrison R, Obarzanek E, et al. Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res. 2000;8(9):605–19.
Joshi SR, Anjana RM, Deepa M, Pradeepa R, Bhansali A, Dhandania VK, et al. Prevalence of dyslipidemia in urban and rural India: the ICMR–INDIAB study. PLoS ONE. 2014;9(5):e96808.
O’Meara JG, Kardia SL, Armon JJ, Brown CA, Boerwinkle E, Turner ST. Ethnic and sex differences in the prevalence, treatment, and control of dyslipidemia among hypertensive adults in the GENOA study. Arch Intern Med. 2004;164(12):1313–8.
Tabatabaei-Malazy O, Qorbani M, Samavat T, Sharifi F, Larijani B, Fakhrzadeh H. Prevalence of dyslipidemia in Iran: a systematic review and meta-analysis study. Int J Prev Med. 2014;5(4):373.
Gidding SS. A perspective on obesity. Am J Med Sci. 1995;310:S68–71.
Organization WH. World Health Organization Obesity: preventing and managing the global epidemic. Report of a WHO consultation WHO Technical Report Series. 2000;894.
Madala MC, Franklin BA, Chen AY, Berman AD, Roe MT, Peterson ED, et al. Obesity and age of first non–ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2008;52(12):979–85.
Yu L, Xu X, Yu W, Chen L, Zhang S, Li Y, et al. The effect of BMI on blood lipids and dyslipidemia in lactating women. Nutrients. 2022;14(23).
Manjareeka M, Nanda S, Mishra J, Mishra S. Correlation between anthropometry and lipid profile in healthy subjects of Eastern India. J Mid-life Health. 2015;6(4):164.
Valdez R. A simple model-based index of abdominal adiposity. J Clin Epidemiol. 1991;44(9):955–6.
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, et al. Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33(4):920–2.
Thomas DM, Bredlau C, Bosy-Westphal A, Mueller M, Shen W, Gallagher D, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity. 2013;21(11):2264–71.
Krakauer NY, Krakauer JC. Dynamic association of mortality hazard with body shape. PLoS ONE. 2014;9(2):e88793.
Keipert S, Voigt A, Klaus S. Dietary effects on body composition, glucose metabolism, and longevity are modulated by skeletal muscle mitochondrial uncoupling in mice. Aging Cell. 2011;10(1):122–36.
Guerrero-Romero F, Rodríguez-Morán M. Abdominal volume index. An anthropometry-based index for estimation of obesity is strongly related to impaired glucose tolerance and type 2 diabetes mellitus. Arch Med Res. 2003;34(5):428–32.
Busquets-Cortés C, López C, Paublini H, Arroyo Bote S, López-González ÁA, Ramírez-Manent JI. Relationship between atherogenic dyslipidaemia and lipid triad with different scales of overweight and obesity in 418,343 Spanish workers. J Nutr Metab. 2022;2022.
Afsar B, Elsurer R, Kirkpantur A. Body shape index and mortality in hemodialysis patients. Nutrition. 2013;29(10):1214–8.
Larson-Meyer DE, Heilbronn LK, Redman LM, Newcomer BR, Frisard MI, Anton S, et al. Effect of calorie restriction with or without exercise on insulin sensitivity, beta-cell function, fat cell size, and ectopic lipid in overweight subjects. Diabetes Care. 2006;29(6):1337–44.
Calmarza P, Trejo JM, Lapresta C, Lopez P. Lack of association between carotid intima-media thickness and apolipoprotein (a) isoforms in a sample of Spanish general population. J Cardiol. 2013;61(5):372–7.
Kahn HS. The" lipid accumulation product" performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison. BMC Cardiovasc Disord. 2005;5:1–10.
Khan SH, Shahid R, Fazal N, Ijaz A. Comparison of various abdominal obesity measures for predicting metabolic syndrome, diabetes, nephropathy, and dyslipidemia. J Coll Phys Surg Pak. 2019;29(12):1159–64.
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE. 2012;7(7):e39504.
Dhana K, Ikram MA, Hofman A, Franco OH, Kavousi M. Anthropometric measures in cardiovascular disease prediction: comparison of laboratory-based versus non-laboratory-based model. Heart. 2015;101(5):377–83.
Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, et al. A better index of body adiposity. Obesity. 2011;19(5):1083–9.
Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. 2018;8(1):16753.
Verbraecken J, Van de Heyning P, De Backer W, Van Gaal L. Body surface area in normal-weight, overweight, and obese adults. A comparison study. Metabolism. 2006;55(4):515–24.
Ghayour-Mobarhan M, Moohebati M, Esmaily H, Ebrahimi M, Parizadeh SM, Heidari-Bakavoli AR, et al. Mashhad stroke and heart atherosclerotic disorder (MASHAD) study: design, baseline characteristics and 10-year cardiovascular risk estimation. Int J Public Health. 2015;60(5):561–72.
Executive summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486–97.
Castelli WP, Garrison RJ, Wilson PW, Abbott RD, Kalousdian S, Kannel WB. Incidence of coronary heart disease and lipoprotein cholesterol levels: the Framingham study. JAMA. 1986;256(20):2835–8.
Acosta-Rodríguez VA, de Groot MHM, Rijo-Ferreira F, Green CB, Takahashi JS. Mice under caloric restriction self-impose a temporal restriction of food intake as revealed by an automated feeder system. Cell Metab. 2017;26(1):267-77.e2.
Zhou Y, Zhang J, Liu R-H, Xie Q, Li X-L, Chen J-G, et al. Association between health-related physical fitness and risk of dyslipidemia in university staff: a cross-sectional study and a roc curve analysis. Nutrients. 2022;14(1):50.
Zaid M, Ameer F, Munir R, Rashid R, Farooq N, Hasnain S, et al. Anthropometric and metabolic indices in assessment of type and severity of dyslipidemia. J Physiol Anthropol. 2017;36(1):1–10.
Zhang K, Zhao Q, Li Y, Zhen Q, Yu Y, Tao Y, et al. Feasibility of anthropometric indices to identify dyslipidemia among adults in Jilin Province: a cross-sectional study. Lipids Health Dis. 2018;17(1):1–10.
Grundy SM, Mok HY, Zech L, Steinberg D, Berman M. Transport of very low density lipoprotein triglycerides in varying degrees of obesity and hypertriglyceridemia. J Clin Investig. 1979;63(6):1274–83.
Kissebah AH, Alfarsi S, Adams PW. Integrated regulation of very low density lipoprotein triglyceride and apolipoprotein-B kinetics in man: normolipemic subjects, familial hypertriglyceridemia and familial combined hyperlipidemia. Metabolism. 1981;30(9):856–68.
Sparks JD, Sparks CE, Adeli K. Selective hepatic insulin resistance, VLDL overproduction, and hypertriglyceridemia. Arterioscler Thromb Vasc Biol. 2012;32(9):2104–12.
Baynes C, Henderson A, Anyaoku V, Richmond W, Hughes C, Johnston D, et al. The role of insulin insensitivity and hepatic lipase in the dyslipidaemia of type 2 diabetes. Diabet Med. 1991;8(6):560–6.
Acknowledgements
This study is part of a master thesis submitted by Alireza Takhttavous, funded by Mashhad University of Medical Sciences, Iran. )ID: IR.MUMS.MEDICAL.REC.1402.262)
Funding
This study was supported financially by Mashhad University of Medical Science (MUMS), Mashhad, Iran (Project Number: 4020349).
Author information
Authors and Affiliations
Contributions
Study Design, Maryam Alinezhad-Namaghi, Maryam Saberi-Karimian, Majid Ghayour-Mobarhan. Data Collection, Elham Amirfakhrian, Marzieh Hosseini. Statistical Analysis, Somayeh Ghiasi Hafezi, Habibollah Esmaily, Mark Ghamsary. Data Interpretation, Maryam Alinezhad-Namaghi, Maryam Saberi-Karimian, Majid Ghayour-Mobarhan. Manuscript Preparation, Maryam Alinezhad-Namaghi, Somayeh Ghiasi Hafezi, Maryam Saberi-Karimian, Majid Ghayour-Mobarhan Gordon A. Ferns. Literature Search, Maryam Alinezhad-Namaghi, Maryam Saberi-Karimian, Majid Ghayour-Mobarhan. Funds Collection, Majid Ghayour-Mobarhan.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Appendix 1.
Computed formula utilizing for calculation of novel anthropometric indices.
Additional file 2:
Supplementary Appendix 2. The association between anthropometric measurements and dyslipidemia using Logistic Regression (LR) Model. Table 1.Supp. Best Cut-off values of anthropometric indices maximizing sensitivity plus specificity using receiver operating characteristic analysis. Table 2.Supp. Association of the binary anthropometric indices with incident dyslipidemia based on optimal cutoff point. Figure 1.Supp. Model A based on optimal cutoff point, in Table 4. Figure 2.Supp. Model B based on optimal cutoff point, in Table 4.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Takhttavous, A., Saberi-Karimian, M., Hafezi, S.G. et al. Predicting the 10-year incidence of dyslipidemia based on novel anthropometric indices, using data mining. Lipids Health Dis 23, 33 (2024). https://doi.org/10.1186/s12944-024-02006-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02006-2