Abstract
Background
Chronic subdural hematoma (CSDH) is a common clinical situation in neurosurgical practice, but the optimal treatment option is controversial. This study aimed to evaluate the effect of cholesterol-lowering medications on and how they affected the prognoses of CSDH patients.
Methods
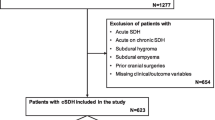
In this multi-institutional observational study performed in Korea, data from recently treated CSDH patients were gathered from 5 hospitals. A total of 462 patients were collected from March 2010 to June 2021. Patient clinical characteristics, history of underlying diseases and their treatments, radiologic features, and surgical outcomes were analyzed.
Results
Seventy-five patients experienced recurrences, and 62 had reoperations after the initial burr hole surgery. Among these, 15 patients with recurrences and 12 with reoperations were taking cholesterol-lowering medications. However, the use of medications did not significantly affect recurrence or reoperation rates (P = 0.350, P = 0.336, respectively). When analyzed by type of medication, no clinically relevant differences in total cholesterol (TC), triglyceride (TG), or low-density lipoprotein cholesterol (LDL-C) levels were identified. The combination of a statin drug and ezetimibe significantly elevated high-density lipoprotein cholesterol (HDL-C) levels (P = 0.004). TC, LDL-C, and TG levels did not significantly affect patient prognoses. However, HDL-C levels and recurrence (odds ratio (OR) = 0.96; 95% confidence interval (CI): 0.94–0.99; p = 0.010) were negatively correlated. An HDL-C level of 42.50 mg/dL was identified as the threshold for recurrence and reoperation.
Conclusions
In this study, using cholesterol-lowering medications did not significantly impact the prognosis of patients who underwent surgical management for a chronic subdural hematoma. However, the findings showed that the higher the HDL-C level, the lower the probability of recurrence and reoperation.
Similar content being viewed by others
Background
A chronic subdural hematoma (CSDH) is mostly caused by trauma. However, unlike an acute subdural hemorrhage, it is influenced by various processes, such as osmotic changes and inflammation [1, 2]. Blocking inflammation and immature angiogenesis with atorvastatin in a rat model led to rapid hematoma absorption [3, 4]. Hematoma drainage using burr hole trephination is an efficient method for reducing hematoma volume. However, the reported recurrence rate is as high as 21%, even with successful surgery [5,6,7,8,9]. Although surgical treatment is the mainstay treatment, research is being conducted on less-invasive treatment options, such as middle meningeal artery (MMA) embolization [10, 11] or the use of certain medications [2, 12,13,14,15,16,17,18,19,20].
Among the non-surgical treatment interventions for CSDH patients, a randomized controlled trial (RCT) demonstrated the beneficial effects of atorvastatin [16]. Statins (β-hydroxy β-methyl-glutaryl-CoA reductase inhibitors) were tested as a conservative method for treating CSDH patients because of their effects on reducing inflammation in the vessel wall [21] and mobilizing endothelial progenitor cells for vascular repair [22,23,24,25]. Based on an RCT that showed the use of atorvastatin reduced the volume of CSDH without surgical intervention, [16] the authors aimed to investigate whether the use of statins would affect recurrence and reoperation in patients who underwent burr hole trephination for a CSDH. This would be the largest published study on the effect of statins on the outcome of CSDH patients.
Methods
A retrospective analysis was conducted on a total of 462 patients who underwent burr hole trephination for a CSDH from March 2010 to June 2021 at 5 hospitals. The study investigated patient age, sex, the timing of surgery, and medical history of hypertension, diabetes, hyperlipidemia, liver disease, kidney disease, stroke, cardiovascular disease, and hematologic disorders. Lipid profiles, including total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglyceride (TG) levels, were analyzed, and the type and dose of medication were also collected. Every laboratory value, including LDL-C levels, was measured directly. All patients included in the study were followed for longer than 6 months to assess recurrence and reoperation. The time frame was set up to 6 months following a previous RCT that reported good functional outcomes after the treatment of CSDH patients [26]. An increase in hematoma volume during follow-up was defined as a recurrence, and a volume increase that required additional surgery was defined as a reoperation. Patients already taking a cholesterol-lowering medication on initial presentation were considered the medication group, and patients without cholesterol-lowering medication constituted the control group.
Statistical methods
For continuous variables, the authors examined the 1st to the 3rd quartile based on the median value. Percentiles were used to assess the proportion of patients with medical histories of other conditions compared to the overall patient population. Linear regression analysis was used to investigate the relationship between the intake of cholesterol-lowering medications and TC, HDL-C, LDL-C, and TG levels. Logistic regression analysis was used to examine the association between lipid levels and the occurrence of reoperation or recurrence. The odds ratio (OR) was used to determine the impact of these factors on prognoses of CSDH patients. Regression analysis was used to assess the differences in cholesterol levels between groups taking cholesterol-lowering medications and the effect of atorvastatin on cholesterol levels. HDL-C threshold levels were assessed using a receiver operating characteristics (ROC) curve. Finally, correlation analysis was performed to examine the influence of each medication on cholesterol levels. Statistical analyses were conducted using R studio, version 4.2.2, by the R Foundation for Statistical Computing in Vienna, Austria. A two-sided P-value of 0.05 was considered statistically significant.
Results
Table 1 describes the baseline characteristics of the patients. The median age of all patients was 75 years (range, 67–81 years), and the medication group was older than the control group (76 vs. 64 years; P = 0.003). Fewer male patients were included in the medication group than in the control group (55.36% vs. 71.14%; P = 0.003). A history of hypertension was identified in 74.11% of the patients in the medication group and 51.14% of the control group (P < 0.001). A history of diabetes mellitus was identified in 45.54% of the patients in the medication group and 25.43% of the control group (P < 0.001). Sixty-three patients took cholesterol-lowering medication due to hyperlipidemia, and 49 patients took cholesterol-lowering medication for the primary prevention of stroke, according to their medical histories. The history of liver disease, kidney disease, cancer, and hematologic disease did not differ between the medication group and the control group (P = 1.000, P = 0.469, P = 0.191, and P = 0.463, respectively). More patients had ischemic and/or hemorrhagic stroke in the medication group than in the control group (P = 0.005), and heart disease was also found more frequently in the medication group (P = 0.009).
Cholesterol levels in the patients included a median TC level of 152.0 mg/dL (131.20–178.00 mg/dL), a median HDL-C level of 47.0 mg/dL (38.00–56.00 mg/dL), a median LDL-C level of 87.0 mg/dL (71.75–108.00 mg/dL), and a median TG level of 94.0 mg/dL (72.00–139.20 mg/dL). In the medication group, the median TC level was 141.0 mg/dL (117.50–161.50 mg/dL), the median HDL-C level was 47.0 mg/dL (38.25–58.25 mg/dL), the median LDL-C level was 72.0 mg/dL (56.50–89.00 mg/dL), and median TG level was 97.5 mg/dL (72.00–136.00 mg/dL). In the control group, the median TC level was 159.0 mg/dL (137.50–187.50 mg/dL), the median HDL-C level was 46.00 mg/dL (38.00–56.00 mg/dL), the median LDL-C level was 92.0 mg/dL (76.00–112.00 mg/dL), and the median TG level was 96.5 mg/dL (72.00–141.20 mg/dL). No significant difference in TG levels was found between the medication group and the control group (P = 0.140). However, LDL-C and TC levels were significantly lower in the medication group (P < 0.001 and P = 0.002, respectively). HDL-C levels were not significantly different (P = 0.508).
Recurrence occurred in 16.02% and 13.39% of the medication and control groups, respectively (P = 0.381). Reoperation was performed in 13.42% of the total patients, and the proportion did not differ between the medication and control groups (10.71% vs. 14.29%; P = 0.426). Morbidity, including postoperative epidural hemorrhage, subarachnoid hemorrhage, and kidney injury, occurred in 3.25% of all patients, with 3.57% in the medication group and 3.14% in the control group (P = 0.767). No mortality was observed in the medication group, but 2.60% mortality was observed in the control group (P = 0.045).
One hundred and twelve patients were found to be taking cholesterol-lowering medication. Of these patients, 37 were taking atorvastatin, 18 were taking rosuvastatin, 8 were taking pitavastatin, 3 were taking simvastatin, one was taking fluvastatin, one was taking only ezetimibe, and 2 were taking fenofibrate. Eleven were taking a combination of ezetimibe and a statin drug. The medication type could not be confirmed in 31 cases (Fig. 1). An comparative analysis was conducted to identify differences in lipid levels among the medication types. There were no significant differences in TC and TG levels, but patients on combined medications showed elevated HDL-C levels (P = 0.004). Other medications were not associated with significant differences in HDL-C levels. Patients on pitavastatin showed higher LDL-C levels compared to other patients (P = 0.012) (Table 2).
Further analysis of patients taking atorvastatin was conducted for comparison to previous studies. The median TC level in patients taking atorvastatin was 137.0 mg/dL (115.00–162.00 mg/dL), the median HDL-C level was 46.0 mg/dL (39.50–61.00 mg/dL), the median LDL-C level was 66.0 mg/dL (56.00–86.00 mg/dL), and the median TG level was 89.5 mg/dL (67.75–113.50 mg/dL). TC and LDL-C levels were significantly lower in patients taking atorvastatin compared to the control group (P = 0.006 and P < 0.001), but there was no significant impact on TG and HDL-C levels (P = 0.205 and P = 0.649). Taking atorvastatin did not significantly impact recurrence or reoperation rates (P = 0.279 and P = 0.451).
Further analyses were conducted to investigate the effect of serum cholesterol levels on chronic subdural hematomas. In the analysis of the effect on recurrence, TC had an OR of 1.00 (0.99–1.02) and did not affect recurrence (P = 0.886). LDL-C levels had an OR of 0.99 (0.97–1.01) (P = 0.461), and TG levels had an OR of 1.00 (1.00–1.00), indicating no association with recurrence (P = 0.876). However, an OR of 0.96 (0.94–0.99) was found for HDL-C levels, indicating a negative correlation, where an increase in HDL-C levels was associated with a decrease in recurrence rates (P = 0.010). Similarly, for reoperation, TC levels had an OR of 1.01 (0.99–1.03) (P = 0.656), and LDL-C levels had an OR of 0.99 (0.96–1.01) (P = 0.526). TG had an OR of 1.00 (1.00–1.00), indicating no association with reoperation (P = 0.831). However, an OR of 0.96 (0.92–0.98) was found for HDL-C levels, indicating that an increase in HDL-C levels was associated with a decrease in reoperation rates (P = 0.007) (Table 3; Fig. 2). A threshold of 42.50 mg/dL HDL-C was obtained from the ROC curve (Fig. 3).
Odds ratios (ORs) of cholesterol for recurrence and reoperation. For recurrence, TC, HDL-C, LDL-C, and TG had ORs of 1.00 (0.99–1.02), 0.96 (0.92–0.99), 0.99 (0.97–1.01), and 1.00 (1.00–1.00), respectively. For reoperation, TC, HDL-C, LDL-C, and TG levels had ORs of 1.01 (0.99–1.03), 0.96 (0.92–0.98), 0.99 (0.96–1.01), and 1.00 (1.00–1.00), respectively. TC: total cholesterol, HDL-C: high-density lipoprotein cholesterol, LDL-C: low-density lipoprotein cholesterol, TG: triglycerides
Discussion
Previous studies analyzed the effects of statin medications on the reduction of chronic subdural hematoma volume and recurrence after surgery (Table 4).
The benefits of atorvastatin in treating CSDH have been repeatedly reported since 2016. Xu et al. reported favorable outcomes for patients treated with CSDH in conservative and postoperative settings (P = 0.045) [20]. However, only 7 patients were included in the conservative management group, and since these patients had relatively minor bleeding, the outcome may not have differed even without atorvastatin treatment. Chan et al. demonstrated that the risk of deterioration requiring further surgical treatment was lower in the atorvastatin group compared to a Glasgow Coma Scale or Markwalder’s Grading Scale-matched control group (P = 0.0447) [12]. However, since only 12 patients were included, further validation is mandatory. In 2018, Tang et al. reported a larger-scale retrospective study in post-surgical CSDH patients treated with atorvastatin. The study found less recurrence compared to the control group [18]. Finally, in 2018, Jiang et al. published the results of an RCT of 20 mg of atorvastatin compared to placebo for the conservative management of CSDH patients [16]. Patients taking atorvastatin showed greater reductions in hematoma volume (P = 0.003) and superior neurologic function improvement (P = 0.03). Fewer patients required surgery in the atorvastatin group compared to the placebo group (11.2% vs. 23.5%; P = 0.03). These CSDH studies on atorvastatin were exclusively performed in China.
Studies that were performed elsewhere were not uniformly treated with atorvastatin. Guidry et al. performed a study in the United States and also reported that statin use was associated with decreases in hematoma size [13]. Unique to this study, no significant difference in outcomes was found according to race. Klein et al. performed a study in Germany, and no evidence for the protective effect of statin medication was found in the treatment of CSDH patients [17]. Similarly, the present study results also showed no significant effect on recurrence or reoperation according to statin usage.
Many of the previously reported studies focused on the usage of atorvastatin medication and the outcome of CSDH patients. Various combinations of cholesterol-lowering drugs are used in daily clinical activities, and this makes interpretations more complex. The protective effect of atorvastatin in post-surgical patients still seems debatable, and evidence that atorvastatin is better than other cholesterol-lowering drugs for treating CSDH patients is scarce. To overcome this hurdle in data analysis, the authors gathered information on the type and dosage of cholesterol-lowering drugs used by the patients. TC, LDL-C, HDL-C, and TG blood chemistry results were collected to better identify which patients truly benefitted from CSDH management.
The results of this study failed to demonstrate the protective effect of statins on the recurrence and reoperation rates of CSDH patients. Even atorvastatin, which had been demonstrated multiple times to be effective, failed to show a significant impact on recurrence or reoperation rates. Notably, the analysis of serum cholesterol levels found that higher levels of HDL-C were associated with a lower incidence of recurrence and reoperation. The cut-off HDL-C value in the study was 42.50 mg/dL. A retrospective single-center study reported by Liu et al. in 2021 also attempted to identify the factors related to CSDH recurrence, including serum lipid levels. They found that CSDH recurrence was affected by risk factors including age, diabetes mellitus, midline shift, and HDL-C levels [27]. The reported an HDL-C cut-off value of 37.45 mg/dL, which was slightly lower than in this report.
Although this study did not find a significant difference in HDL-C levels between patients who used statins and those who did not, differences in HDL-C levels were found to depend on the type of medication used. When the type of medication used and the serum lipid profile levels were analyzed, only patients receiving combined medication with ezetimibe showed elevated HDL-C levels. Ezetimibe reduces atherogenic lipid profiles and increases HDL-C levels, which may explain why HDL-C levels were higher in patients who used a combination of these medications [28]. Even though this study failed to demonstrate it, statins are known to moderately increase HDL-C levels [29].
The anti-inflammatory effect of HDL has been shown in many studies, [30, 31] and a relationship among HDL-C, vascular endothelial growth factor (VEGF), and CSDH was demonstrated. Weigel et al. proposed that VEGF contributes to hematoma growth and CT appearances in CSDH patients [32]. Petrov et al. reported imbalances in angiogenesis factors, including VEGF, in CSDH patients compared to healthy volunteers and that these imbalances were related to rebleeding [33]. A significant reduction in plasma VEGF concentrations was observed following statin therapy in a systemic review published in 2015 [34]. The effect was related to treatment duration, LDL-C lowering activity, the lipophilicity of statins, and the health status of studied individuals but not to the molar dose of statins. Epidemiological and prospective studies proved the vasculoprotective effects of HDL-C, which were presumably by regulating angiogenesis [35]. HDL-C increased endothelial proliferation, migration, and tube formation dose-dependently, consequently promoting angiogenesis via vascular endothelial growth factor 2 activation [36]. The findings in this study that elevated HDL-C levels were related to a lower incidence of CSDH recurrence and reoperation may have been due to the vasculoprotective effect of HDL-C via VEGF-promoting angiogenesis. According to the proposed mechanism mentioned above, there is also a possibility that postoperative CSDH patients may benefit clinically from elevating HDL-C levels with combined cholesterol-lowering medication, including ezetimibe.
Strengths of the study
This study analyzed the effects of cholesterol-lowering drugs on the outcome of patients with chronic subdural hematoma as a multi-institutional retrospective study. HDL-C levels rather than the usage of statin medication itself were identified to be associated with CSDH patient outcomes. This finding is consistent with the results of previously reported studies, that the impact of cholesterol-lowering drugs on chronic subdural hematoma is still debatable. Instead, patients’ HDL-C levels may be evaluated to better predict their prognoses.
Limitations
There were several limitations to this study besides its retrospective nature. The study was performed as a multi-center study to provide more diverse patient characteristics and treatment results. However, potential errors or differences in data collection may have been present. Further, the use of other drugs that affect cholesterol mechanisms, such as steroids or retinoids, could not be assessed. The case number was relatively large compared to previously published studies, but quantitative analysis of the dosage of each cholesterol-lowering medication failed to demonstrate statistically relevant results. Further studies with prospective designs are needed to overcome this limitation.
Conclusions
CSDH patients with elevated HDL-C levels are likely to have superior prognoses in terms of recurrence and reoperation. Thus, patients without elevated HDL-C levels should be carefully assessed during follow-up compared to those with elevated HDL-C levels. Moreover, attempts to elevate patients’ HDL-C levels may facilitate better prognoses.
Data Availability
Access to the datasets can be provided upon reasonable request the corresponding author.
Abbreviations
- CSDH:
-
Chronic subdural hematoma
- OR:
-
Odds ratio
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- LDL-C.:
-
Low-density lipoprotein cholesterol
- MMA:
-
Middle meningeal artery
- RCT:
-
Randomized controlled trial
- VEGF:
-
Vascular endothelial growth factor
References
Fan Y, Wang D, Rao C, Li Y, Rong H, Wang Z, et al. Atorvastatin combined with low-dose Dexamethasone Treatment protects endothelial function impaired by chronic subdural hematoma via the transcription factor KLF-2. Drug Des Devel Ther. 2020;14:3291–9.
Holl DC, Volovici V, Dirven CMF, Peul WC, van Kooten F, Jellema K, et al. Pathophysiology and nonsurgical treatment of chronic subdural hematoma: from past to Present to Future. World Neurosurg. 2018;116:402–11e2.
Li T, Wang D, Tian Y, Yu H, Wang Y, Quan W, et al. Effects of atorvastatin on the inflammation regulation and elimination of subdural hematoma in rats. J Neurol Sci. 2014;341(1–2):88–96.
Wang D, Li T, Wei H, Wang Y, Yang G, Tian Y, et al. Atorvastatin enhances angiogenesis to reduce subdural hematoma in a rat model. J Neurol Sci. 2016;362:91–9.
Jack A, O’Kelly C, McDougall C, Findlay JM. Predicting recurrence after chronic subdural haematoma drainage. Can J Neurol Sci. 2015;42(1):34–9.
Mori K, Maeda M. Surgical treatment of chronic subdural hematoma in 500 consecutive cases: clinical characteristics, surgical outcome, Complications, and recurrence rate. Neurol Med Chir (Tokyo). 2001;41(8):371–81.
Nakaguchi H, Tanishima T, Yoshimasu N. Factors in the natural history of chronic subdural hematomas that influence their postoperative recurrence. J Neurosurg. 2001;95(2):256–62.
Ramachandran R, Hegde T. Chronic subdural hematomas–causes of morbidity and mortality. Surg Neurol. 2007;67(4):367–72. discussion 72 – 3.
Yamamoto H, Hirashima Y, Hamada H, Hayashi N, Origasa H, Endo S. Independent predictors of recurrence of chronic subdural hematoma: results of multivariate analysis performed using a logistic regression model. J Neurosurg. 2003;98(6):1217–21.
Ironside N, Nguyen C, Do Q, Ugiliweneza B, Chen CJ, Sieg EP, et al. Middle meningeal artery embolization for chronic subdural hematoma: a systematic review and meta-analysis. J Neurointerv Surg. 2021;13(10):951–7.
Srivatsan A, Mohanty A, Nascimento FA, Hafeez MU, Srinivasan VM, Thomas A, et al. Middle meningeal artery embolization for chronic subdural hematoma: Meta-Analysis and systematic review. World Neurosurg. 2019;122:613–9.
Chan DY, Chan DT, Sun TF, Ng SC, Wong GK, Poon WS. The use of atorvastatin for chronic subdural haematoma: a retrospective cohort comparison study(). Br J Neurosurg. 2017;31(1):72–7.
Guidry BS, Kelly KA, Yengo-Kahn AM, Lan M, Tang AR, Chotai S, et al. Statins as a medical Adjunct in the Surgical Management of Chronic Subdural hematomas. World Neurosurg. 2021;149:e281–e91.
He C, Xia P, Xu J, Chen L, Zhang Q. Evaluation of the efficacy of atorvastatin in the treatment for chronic subdural hematoma: a meta-analysis. Neurosurg Rev. 2021;44(1):479–84.
Huang J, Gao C, Dong J, Zhang J, Jiang R. Drug treatment of chronic subdural hematoma. Expert Opin Pharmacother. 2020;21(4):435–44.
Jiang R, Zhao S, Wang R, Feng H, Zhang J, Li X, et al. Safety and efficacy of atorvastatin for chronic subdural hematoma in Chinese patients: a Randomized ClinicalTrial. JAMA Neurol. 2018;75(11):1338–46.
Klein J, Mauck L, Schackert G, Pinzer T. Do statins reduce the rate of revision Surgery after chronic subdural hematoma drain? Acta Neurochir (Wien). 2021;163(7):1843–8.
Tang R, Shi J, Li X, Zou Y, Wang L, Chen Y, et al. Effects of Atorvastatin on Surgical treatments of chronic subdural hematoma. World Neurosurg. 2018;117:e425–e9.
Qiu S, Zhuo W, Sun C, Su Z, Yan A, Shen L. Effects of atorvastatin on chronic subdural hematoma: a systematic review. Med (Baltim). 2017;96(26):e7290.
Xu M, Chen P, Zhu X, Wang C, Shi X, Yu B. Effects of Atorvastatin on Conservative and Surgical treatments of chronic subdural hematoma in patients. World Neurosurg. 2016;91:23–8.
Potey C, Ouk T, Petrault O, Petrault M, Berezowski V, Salleron J, et al. Early treatment with atorvastatin exerts parenchymal and vascular protective effects in experimental cerebral ischaemia. Br J Pharmacol. 2015;172(21):5188–98.
Araujo FA, Rocha MA, Mendes JB, Andrade SP. Atorvastatin inhibits inflammatory angiogenesis in mice through down regulation of VEGF, TNF-alpha and TGF-beta1. Biomed Pharmacother. 2010;64(1):29–34.
Buttmann M, Lorenz A, Weishaupt A, Rieckmann P. Atorvastatin partially prevents an inflammatory barrier breakdown of cultured human brain endothelial cells at a pharmacologically relevant concentration. J Neurochem. 2007;102(4):1001–8.
Liu Y, Wei J, Hu L, Hu S. Beneficial effects of statins on endothelial progenitor cells. Am J Med Sci. 2012;344(3):220–6.
Sobrino T, Blanco M, Perez-Mato M, Rodriguez-Yanez M, Castillo J. Increased levels of circulating endothelial progenitor cells in patients with ischaemic Stroke treated with statins during acute phase. Eur J Neurol. 2012;19(12):1539–46.
Santarius T, Kirkpatrick PJ, Ganesan D, Chia HL, Jalloh I, Smielewski P, et al. Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: a randomised controlled trial. Lancet. 2009;374(9695):1067–73.
Liu WC, Lin QQ, Jin J, Wang M, You WD, Gu J, et al. An association of low high-density lipoprotein levels with recurrence of chronic subdural hematoma. Acta Neurochir (Wien). 2021;163(4):1061–8.
Othman RA, Myrie SB, Mymin D, Roullet JB, Steiner RD, Jones PJH. Effect of ezetimibe on low- and high-density lipoprotein subclasses in sitosterolemia. Atherosclerosis. 2017;260:27–33.
McTaggart F, Jones P. Effects of statins on high-density lipoproteins: a potential contribution to cardiovascular benefit. Cardiovasc Drugs Ther. 2008;22(4):321–38.
Barker G, Winer JR, Guirgis FW, Reddy S. HDL and persistent inflammation immunosuppression and catabolism syndrome. Curr Opin Lipidol. 2021;32(5):315–22.
Grao-Cruces E, Lopez-Enriquez S, Martin ME, Montserrat-de la Paz S. High-density lipoproteins and immune response: a review. Int J Biol Macromol. 2022;195:117–23.
Weigel R, Hohenstein A, Schilling L. Vascular endothelial growth factor concentration in chronic subdural hematoma fluid is related to computed tomography appearance and exudation rate. J Neurotrauma. 2014;31(7):670–3.
Petrov A, Ivanov A, Dryagina N, Petrova A, Samochernykh K, Rozhchenko L. Angiogenetic factors in chronic subdural Hematoma Development. Diagnostics (Basel). 2022;12(11).
Sahebkar A, Ponziani MC, Goitre I, Bo S. Does statin therapy reduce plasma VEGF levels in humans? A systematic review and meta-analysis of randomized controlled trials. Metabolism. 2015;64(11):1466–76.
Tan JT, Ng MK, Bursill CA. The role of high-density lipoproteins in the regulation of angiogenesis. Cardiovasc Res. 2015;106(2):184–93.
Jin F, Hagemann N, Sun L, Wu J, Doeppner TR, Dai Y, et al. High-density lipoprotein (HDL) promotes angiogenesis via S1P3-dependent VEGFR2 activation. Angiogenesis. 2018;21(2):381–94.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: EJ, PJ-SData curation: EJ, AS, LMH, CJ-G, KYI, CCB, PJ-SFormal analysis: EJ, PJ-SInvestigation: EJ, AS, LMH, CJ-G, KYI, CCB, PJ-S Methodology: EJ, PJ-SWriting - original draft: EJ, PJ-SWriting - review: All.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was approved by the Institutional Review Board of The Catholic University of Korea (IRB No.: XC22RDI0012). Informed consent was waived because of the retrospective nature of this study.
Consent for publication
No individual patient data were included in this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Eun, J., Ahn, S., Lee, M.H. et al. Potential impact of high-density lipoprotein cholesterol in the postoperative outcomes of chronic subdural hematoma patients: multi-institutional study in Korea. Lipids Health Dis 22, 197 (2023). https://doi.org/10.1186/s12944-023-01970-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-023-01970-5