Abstract
Background
Blood lipids are essential components for cellular growth. An inverse association between serum lipid levels and risk of cancer has led to a controversy among previous studies. The aim of this prospective cohort study was to investigate the association between blood lipids change and risk of cancer incidence.
Methods
A cohort of 4130 Taiwanese adults from the Taiwanese Survey on the Prevalence of Hypertension, Hyperglycemia, and Hyperlipidemia database underwent repeated examinations in 2002 and 2007. Six groups were established based on the combined baseline (lower/higher) and interval change (decreasing/stable/increasing) in plasma lipid levels. Multivariable Cox proportional hazard model was used to investigate the relationship between lipids change and all-cause cancer incidence.
Results
Two hundred and forty cancer events developed over a median follow-up of 13.4 years. Comparing these with individuals with decreasing lower-baseline lipid levels, cancer risk reduction was demonstrated in those with increasing lower-baseline total cholesterol (adjusted hazard ratio [aHR], 0.48; 95% confidence interval [CI], 0.27 to 0.85), low-density lipoprotein cholesterol (LDL-C; aHR, 0.56; 95% CI, 0.35 to 0.92), and non–high-density lipoprotein cholesterol (non-HDL-C) (aHR, 0.54; 95% CI, 0.31 to 0.92) levels. A decreased risk for cancer incidence also presented in participants with stable lower-baseline, decreasing and increasing higher-baseline LDL-C levels, and with decreasing and stable higher-baseline non-HDL-C levels.
Conclusions
The interval decline in lower-baseline total cholesterol, LDL-C, and non-HDL-C levels was linked to a higher risk for all-cause cancer incidence. More attention to a potential cancer risk may be warranted for an unexplained fall in serum lipids.
Similar content being viewed by others
Background
Cancer has been the leading cause of death in Taiwan for several decades [1], and its incidence has been increasing. The number of cancer patients by age-standardized incidence rate increased from 191.6 per 100,000 people in 1996 to 309.8 in 2018 [2]. The well-known risk factors for malignant neoplasm included older age, family history, certain types of infection, and substance exposure such as alcohol or tobacco [3]. Furthermore, blood lipid metabolic dysregulation has also been correlated with increased carcinogenic risk [4]. Lipids are fundamental components in cellular homeostasis as they provide energy, stabilize the phospholipid bilayer in the plasma membrane, and are involved in various intracellular signal transduction pathways [4]. Dysregulation of lipid metabolism can activate several essential oncogenic signaling networks [5,6,7,8,9].
Different serum lipid components are associated with risk of various types of cancer. For example, higher total cholesterol (TC) levels are associated with higher risk of prostate and colon cancers in men and breast cancer in women [10]. Higher triglyceride levels and lower high-density lipoprotein cholesterol (HDL-C) levels are associated with breast and lung cancer risk [11, 12]. However, conflicting results in various studies suggest no relationship or even an inverse association between plasma lipids and cancer development [4, 13,14,15,16,17].
The high metabolic rate of cancer cell proliferation may have an impact on the serum lipid levels [4]. Earlier studies have demonstrated a decline in serum cholesterol levels during cancer development [18, 19]. Therefore, the effects of preclinical cancer could demonstrate normal or even lower serum cholesterol values among pre-existing cancer patients [14]. Most studies either compared baseline serum lipids with cancer risk or followed the study population for a relatively short duration. Hence, the effect of preclinical cancer could not be clarified. In addition, the different trajectories of serum lipid changes may differentially influence cell metabolism. Thus, studies focusing on the interval change of lipids before cancer diagnosis are of great value to elucidate the exact correlation between serum lipid and cancer risk. This prospective cohort study aimed to investigate the association of baseline and changes in various serum lipid levels on the risk of cancer incidence.
Methods
Study population and data source
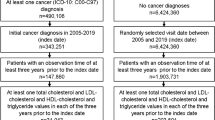
This is a population-based prospective cohort study. Participants were identified using population registries maintained in the Taiwanese Survey on Prevalence of Hypertension, Hyperglycemia, and Hyperlipidemia (TwSHHH) in 2002. TwSHHH 2002 was a general health survey launched for national population cohorts, and proposed a standard protocol for data collection. The follow-up evaluation was carried out from June 2007 to May 2008 in TwSHHH 2007. The dataset was also linked to Taiwan’s National Health Insurance Research Database (NHIRD). The NHIRD offered access to outpatient visits, hospitalization records, prescribed medications, and National Death Registry. The flow chart of the study design is shown in Fig. 1.
Flow chart of the participants in the study cohort. TwSHHH, Taiwanese Survey on Prevalence of Hypertension, Hyperglycemia, and Hyperlipidemia; TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; non-HDL-C, non-high-density lipoprotein cholesterol. Model adjusted for age, sex, body mass index, current smoking, alcohol drinking, betel nuts consumption, regular exercise, marital status, education level, income level, diabetes mellitus, hypertension, high-sensitivity C-reactive protein, menopause status, hormone replacement therapy and lipid-lowering agent use. Incidence rate is shown per 1000 person-years. TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; BMI, body mass index
This study excluded participants who were younger than 20 years, had prevalent cancer at or prior to the enrolment in TwSHHH 2007, reported pregnancy within 1 year prior to TwSHHH 2002 or TwSHHH 2007, and missing data. The final cohort population consisted of 4130 participants (2185 women and 1945 men). This study was in adherence with the Declaration of Helsinki. The protocol was reviewed and approved by the Research Ethics Committee of National Taiwan University Hospital. The committee complied with the Good Clinical Practice Guidelines (NTUH-REC number: 201901103 W [Institutional Review Board reference]).
Data collection
In TwSHHH 2002, all the participants responded to a standardized self-administered questionnaire and received routine examinations. The questionnaire included socio-demographic characteristics such as smoking status, alcoholic drinking, betel nuts consumption, exercise habits, menopause status, and medical and family history. Women participants were additionally interviewed with hormone replacement therapy use. Hypertension was diagnosed when systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg in consecutive measurements, or when on anti-hypertensive agents [20]. Diabetes mellitus was diagnosed with a fasting blood sugar level of ≥126 mg/dL and hemoglobin A1c level ≥ 6.5 mg/dL, or when on antidiabetic medication [21].
Blood samples were drawn after a 12 h of overnight fasting. Low-density lipoprotein cholesterol (LDL-C) was estimated using the Friedewald formula of “TC - HDL-C - (triglycerides/5)” in TwSHHH 2002 and was measured directly by homogeneous assays in TwSHHH 2007 [22]. TC and triglycerides were obtained using colorimetry [23]. HDL-C was obtained using electrophoresis. Non-HDL cholesterol (Non-HDL-C) was calculated as subtracting HDL-C from TC.
For the baseline analysis, participants were divided into quartiles according to the levels of each lipid component in TwSHHH 2002. For the interval changes in lipid levels between TwSHHH 2002 and 2007, participants were divided into six categories (low-decreased, low-stable, low-increased, high-decreased, high-stable, and high-increased). Low groups consisted of participants with baseline lipid levels categorized into quartiles 1 and 2, while high groups consisted of those with baseline lipid levels categorized into quartiles 3 and 4. The stable groups were defined as those with a lipid change of less than 0.25 standard deviation in baseline values of serum lipids. The increased groups were defined as those with a positive lipid change of greater than or equal to 0.25 standard deviation in baseline values of serum lipids. The decreased groups were defined as those with a negative lipid change of greater than or equal to 0.25 standard deviation in baseline values of serum lipids. Low-decreased group was defined as the reference group based on previous evidence that lower baseline or declining serum lipid level was associated with cancer development [18, 19].
Outcome identification and follow-up
The follow-up for each participant started since the index date in which blood samples were obtained in TwSHHH 2002 and ended on the date of cancer diagnosis, death, loss of follow-up, or administrative censoring (December 31, 2015). The outcomes were identified in accordance with the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD9-CM) codes. Both outpatient and inpatient records were used to confirm the diagnoses of outcomes. Cancer cases were identified with one or more diagnoses of ICD9-CM codes for malignant neoplasms, including 140–208 from the NHIRD registry database.
Statistical analyses
Analysis of variance for continuous variables and Chi-squared test for categorical variables were done to assess the differences among groups. The incidence rates of cancer were presented by the event numbers per 1000 person-years of follow-up. Log-rank test was used to compare the cancer incidence rates among different groups of lipid profiles. The multivariable Cox regression models were used to evaluate the relationship of lipid levels with cancer risks. The proportionality assumption was tested and verified [24]. Subgroup analyses were conducted to assess effect modification by age, sex, and body mass index (BMI). Sensitivity analyses were performed to determine the robustness of study findings: (1) excluding cancer cases or death in 1 year from index date of TwSHHH 2007, (2) excluding participants who used lipid-lowering agents, and (3) excluding extremely high triglyceride levels (> 400 mg/dL). An additional analysis was carried out to explore the correlation between the changes in body weight and blood lipids. A two-tailed P-value of < 0.05 was considered statistically significant differences. SAS version 9.4 (SAS Institute, Cary, North Carolina, U.S.) and Stata version 14 (Stata Corporation, College Station, Texas, USA) were used as analytics tools.
Results
Study characteristics
Table 1 shows the demographic characteristics of the study cohort categorized according to baseline serum LDL-C quartiles. A total of 4130 participants were included in this study. A total of 2,004,174 person-years at risk was recognized with a median follow-up period of 13.4 years. The mean age at study entry was 44.9 years. A higher LDL-C quartile was positively associated with age, BMI, regular exercise, married status, diabetes mellitus, hypertension, high-sensitivity C-reactive protein levels, menopause, use of lipid-lowering agents, and inversely associated with female gender and educational level. During follow-up, a total of 240 cancer events were ascertained.
Relationship between baseline and change of lipid levels and all-cancer incidence
The baseline lipid quartiles were not associated with total cancer incidence across all categories of lipid components (Table 2). Figure 2 demonstrates the relative risks of all-cause cancer incidence based on the interval changes of each lipid component. Participants in low-increased group of TC component exhibited a lower risk for all-cause cancer incidence compared to the low-decreased group (adjusted hazard ratio [aHR], 0.48; 95% confidence interval [CI], 0.27 to 0.85). For LDL-C component, compared to participants in the low-decreased group, those in the low-stable (aHR, 0.48; 95% CI, 0.24 to 0.93), low-increased (aHR, 0.56; 95% CI, 0.35 to 0.92), high-decreased (HR, 0.62; 95% CI, 0.41 to 0.94), and high-increased groups (aHR, 0.51; 95% CI, 0.30 to 0.85) showed lower risk of all-cause cancer incidence. After combining all other groups as a reference group, the low-decreased group for the LDL-C component also revealed a higher cancer risk with the adjusted hazard ratio of 1.59 (95% CI, 1.00–2.55) (Table S1 in Additional file 1). For non-HDL-C component, the results yielded a lower risk of all-cause cancer incidence for participants in the low-increased (aHR, 0.54; 95% CI, 0.31 to 0.92), high-decreased (aHR, 0.58; 95% CI, 0.35 to 0.95), and high-stable groups (aHR, 0.55; 95% CI, 0.30 to 0.98) in comparison to participants in the low-decreased group.
The effects of interval changes in various lipid components for all-cause cancer risk during median 13.4-year follow-up. Model adjusted for age, sex, body mass index, current smoking, alcohol drinking, betel nut consumption, regular exercise, marital status, education level, income level, diabetes mellitus, hypertension, high-sensitivity C-reactive protein, menopause status, hormone replacement therapy, and lipid-lowering agent use. Incidence rate is shown per 1000 person-years. CI, confidence interval; LDL, low density lipoprotein; HDL, high density lipoprotein
Subgroup and sensitivity analyses
The relative risks of all-cause cancer incidence based on the baseline quartiles and interval changes in TC and LDL-C components stratified by different variables are shown in Table S2 (Additional file 2) and Table 3, respectively. The results did not substantially vary when stratified by age, gender, or BMI for all categories of baseline lipid components. The effects of interval changes on the lipid levels were consistent across subgroups. The results of sensitivity analysis remained robust by excluding cancer events or death in 1 year from index date of TwSHHH 2007, excluding the participants using lipid-lowering agents and cases with extremely high triglyceride levels (> 400 mg/dL; Table S3 in Additional file 3). The additional analysis showed that the body weight of most participants remained constant or slightly increased between the follow-up intervals (Tables S4–1 and S4–2 in Additional file 4). The overall estimates also remained mostly stable for the TC, LDL-C, and Non-HDL-C components after excluding individuals with interval body weight loss (Table S4–3 in Additional file 4).
Discussion
This prospective cohort study of initially healthy Taiwanese adults investigated the association of various lipid biomarkers and their interval changes with risk of all-cause cancer incidence during the median follow-up time of 13.4 years. The baseline serum lipid levels did not associate with incidence of total cancer. Participants with constantly stable or positively-changed cholesterol levels showed a lower cancer risk compared with those with initially low and subsequently decreased lipid levels. The association was mainly suggested from the components of TC, LDL-C, and non-HDL-C.
The evidence regarding the relationship between serum lipids and risk of cancer has been inconsistent. Several studies observed an inverse association, especially during first few years from the study onset [15, 17, 25,26,27,28]. The preclinical effect of cancer consuming more cholesterol on tumor growth could introduce potential reverse causality. However, some studies found the inverse association persisted even more than 10 years before the diagnosis of cancer, which could not be entirely attributed to the preclinical effect [10, 27].
Limited studies have explored the exact trajectories of serum lipid changes before the development of cancer. A Mendelian randomization study showed that lifelong low plasma LDL-C levels caused by gene polymorphisms are unrelated to increased cancer risk [29]. Similarly, this study found that the risk of cancer incidence was not associated with baseline lipid levels, but with their interval changes. Kritchevsky et al. in a cohort study with 103 middle-aged men found a decline in serum lipids approximately 2 years preceding cancer diagnosis, with LDL-C predominantly reflecting the decrease among lipoprotein fractions [18]. Winawer et al. in a case-control study with a modest sample size demonstrated an average decline of 13% in serum cholesterol occurring gradually during the 10 years prior to the diagnosis of colon cancer [19]. In this study, the depletion of serum lipids occurred more than 5 years before malignancy development in almost all cancer events. The median time for the diagnosis of cancer is around 7.7–10.6 years after the decline of serum lipids for various lipid components (Table S5 in Additional file 5). In addition, the exclusion of 1-year incident cases after index date of TwSHHH 2007 did not alter the findings. The results are in line with those of previous studies, that is, the preclinical effect does not entirely contribute to the inverse relationship between lipid change and cancer development.
In this study, the association between the decline in blood lipid levels and cancer risk did not change substantially after exclusion of lipid-lowering agent users. The mainstay of these agents, like statin, is believed to inhibit key enzymes in the cholesterol synthesis pathway and may disrupt oncogenesis [30]. Ambiguous results were obtained with respect to the relationship between the use of lipid-lowering agents and cancer risk. One meta-analysis concluded that reductions in LDL-C with statin treatment did not increase the cancer incidence during a median follow-up time of 5 years [31]. Another study indicated no difference in risk of colorectal cancer between statin continuers and discontinuers [32]. One Mendelian randomization study proposed that statins utilized a cholesterol-independent pathway to reduce the risk of malignancies [33]. In contrast, the association of decreasing blood lipids with cancer risk remained mostly consistent despite medical treatment in this study. Therefore, there may be an independent influence of endogenous metabolic depression on the processes of tumorigenesis and further research is warranted.
In this study, a higher risk of cancer incidence by depletion of serum lipids was mainly drawn from TC, LDL-C, and non-HDL-C components. The effects of TC and non-HDL-C on risk for cancer incidence appeared to be largely affected but could not be fully explained by LDL-C. The potential influence of remnant lipoprotein fractions or their binding apolipoproteins within the non-HDL-C component could not be concluded in the current study. Furthermore, the influence of LDL-C on cancer development may differ among various site-specific malignancies. While some studies found that low LDL-C levels may increase risk for hematological and esophageal cancers [34, 35], other studies reported marginal or non-significant association between LDL-C levels and the risk of breast cancer [36, 37]. The cholesterol requirement and basic constitution vary in different tissues; thus, the tissue origin of the neoplasm may also lead to discrepant observations [38].
The exact pathophysiology regarding the correlation between LDL-C and cancer development has remained inconclusive. The possibility that the depletion of LDL-C might merely act as a surrogate for body weight loss, which frequently occurs during cancer development, was proved to be marginal in this study. The oxidized LDL-C serves as a marker for lipid peroxidation, which could enhance carcinogenesis [34]. LDL particles transport cholesterol to surrounding tissues mainly through receptor-mediated pathways. An accelerated LDL receptor activity resulting in increased intracellular cholesterol influx also precedes the development of certain types of cancer [39, 40]. The activation of phosphatidylinositol 3-kinase/protein kinase B/mammalian target of rapamycin signaling pathway may mediate the upregulation of intracellular cholesterol levels, which is related to cell growth [38]. Furthermore, prolonged depletion of plasma cholesterol may contribute to tumorigenesis by promoting the activation of nuclear factor-κB [41]. It could also disrupt the homeostatic balance of lipid raft and dysregulate tumor cell growth [30]. Finally, the elimination of cholesterol by altered gut microbiota may also facilitate cancer development [30].
Comparison with other Asian countries
Cancer epidemiology and metabolic characteristics vary among different races and territories. The high prevalence of gastrointestinal cancer in Asian countries may affect the relationship between blood lipid levels and cancer risk. A Korean population-based cohort study found the correlation between TC and risk of all-cancer incidence differed largely by cancer site [10]. Other two Japanese studies indicated an inverse relationship between TC and cancer incidence [15, 25]. The inverse correlation was observed mainly for liver and stomach cancers. One study from China even showed a V-shaped relationship between LDL-C and cancer risk [42]. However, most previous studies lack information concerning change in the lipids before cancer development, which may partly constitute to the discrepancies. Moreover, while stomach cancer is markedly prevalent in most East Asian countries, liver cancer is relatively common in Taiwan [43, 44]. In this study, gastrointestinal cancer accounted for approximately 30%, which corresponded to the cancer epidemiology in Taiwan during the study period [45]. Unfortunately, the influence of metabolic depression on different site-specific cancers could not be studied in detail.
Study strength and limitations
This study has some important strengths. This prospective cohort study is the first to simultaneously evaluate the association between combined basic and interval changes of blood lipids and cancer risk in a population-based large cohort with a long follow-up time. Although the study population was relatively younger and metabolically healthier than the general population in Taiwan, the extrapolation of the results may still be appropriate due to the utilization of population-based representative databases. Second, this study used standardized measurements of variables. National registers also provided detailed information on cancer diagnosis or death. Third, this study collected comprehensive information on potential confounders.
However, it had a few limitations. First, due to the nature of observational design, a solid causal relationship could not be established. The relatively small number of cancer events and missing data may lessen the power of observed association and hinder further analysis for site-specific cancers. However, this study included various lipoprotein subfractions with a long follow-up time. The findings were consistent across various groups and with sensitivity analysis. Second, the Friedewald formula was used to estimate LDL-C level for the TwSHHH 2002 cohort. Nevertheless, the results did not change after exclusion of participants with extremely high triglyceride levels. Third, other residual confounding, such as diet, other medication history (like oral contraceptive or aspirin), and family history were lacking in this study.
Conclusions
In this population-based prospective cohort study, the interval decline of lower-baseline serum lipid levels was associated with increased risk for all-cause cancer incidence. The effect was mainly suggested by TC, LDL-C, and non-HDL-C components. The results provide novel evidence regarding the impact of plasma lipid dynamics on cancer development. Despite the protective role of lower plasma lipid levels in cardiovascular disease, an unexplained decline in serum lipids may imply a potential risk of cancer development. Therefore, clinicians may pay attention to monitoring and maintaining serum lipids for individuals with unexplained drop in serum lipids. Further research focusing on the effects of lipid change among different site-specific cancers is also warranted.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TC:
-
Total cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- TwSHHH:
-
Taiwanese Survey on Prevalence of Hypertension, Hyperglycemia, and Hyperlipidemia
- NHIRD:
-
Taiwan’s National Health Insurance Research Database
- LDL-C:
-
Low-density lipoprotein cholesterol
- Non-HDL-C:
-
Non-HDL cholesterol
- ICD9-CM:
-
International Classification of Diseases, Ninth Revision, Clinical Modification
- BMI:
-
Body mass index
- aHR:
-
Adjusted hazard ratio
- CI:
-
95% confidence interval
References
Chen CJ, You SL, Lin LH, Hsu WL, Yang YW. Cancer epidemiology and control in Taiwan: a brief review. Jpn J Clin Oncol. 2002;32(Suppl):S66–81. https://doi.org/10.1093/jjco/hye138.
2018 Cancer Registry Annual Report. Taipei City: Health Promotion Administration, Ministry of Health and Welfare; 2020. https://www.hpa.gov.tw/Pages/List.aspx?nodeid=269. Accessed 22 May 2021.
Risk Factors for Cancer. National Institutes of Health. 2015. https://www.cancer.gov/about-cancer/causes-prevention/risk. Accessed 16 Dec 2020.
Kuzu OF, Noory MA, Robertson GP. The role of cholesterol in Cancer. Cancer Res. 2016;76(8):2063–70. https://doi.org/10.1158/0008-5472.CAN-15-2613.
Hooper JE, Scott MP. Communicating with hedgehogs. Nat Rev Mol Cell Biol. 2005;6(4):306–17. https://doi.org/10.1038/nrm1622.
Huang P, Nedelcu D, Watanabe M, Jao C, Kim Y, Liu J, et al. Cellular Cholesterol Directly Activates Smoothened in Hedgehog Signaling. Cell. 2016;166:1176–87.e14.
Luchetti G, Sircar R, Kong JH, Nachtergaele S, Sagner A, Byrne EF, et al. Cholesterol activates the G-protein coupled receptor smoothened to promote hedgehog signaling. Elife. 2016;5. https://doi.org/10.7554/eLife.20304.
Sheng R, Chen Y, Yung Gee H, Stec E, Melowic HR, Blatner NR, et al. Cholesterol modulates cell signaling and protein networking by specifically interacting with PDZ domain-containing scaffold proteins. Nat Commun. 2012;3:1249.
Vaquero J, Nguyen Ho-Bouldoires TH, Claperon A, Fouassier L. Role of the PDZ-scaffold protein NHERF1/EBP50 in cancer biology: from signaling regulation to clinical relevance. Oncogene. 2017;36(22):3067–79. https://doi.org/10.1038/onc.2016.462.
Kitahara CM. Berrington de Gonzalez a, freedman ND, Huxley R, Mok Y, Jee SH, et al. Total cholesterol and cancer risk in a large prospective study in Korea. J Clin Oncol. 2011;29(12):1592–8. https://doi.org/10.1200/JCO.2010.31.5200.
Han C, Zhang HT, Du L, Liu X, Jing J, Zhao X, et al. Serum levels of leptin, insulin, and lipids in relation to breast cancer in China. Endocrine. 2005;26(1):19–24. https://doi.org/10.1385/ENDO:26:1:019.
Lin X, Lu L, Liu L, Wei S, He Y, Chang J, et al. Blood lipids profile and lung cancer risk in a meta-analysis of prospective cohort studies. J Clin Lipidol. 2017;11(4):1073–81. https://doi.org/10.1016/j.jacl.2017.05.004.
Gaard M, Tretli S, Urdal P. Risk of breast cancer in relation to blood lipids: a prospective study of 31,209 Norwegian women. Cancer Causes Control. 1994;5(6):501–9. https://doi.org/10.1007/BF01831377.
Heir T, Falk RS, Robsahm TE, Sandvik L, Erikssen J, Tretli S. Cholesterol and prostate cancer risk: a long-term prospective cohort study. BMC Cancer. 2016;16(1):643. https://doi.org/10.1186/s12885-016-2691-5.
Iso H, Ikeda A, Inoue M, Sato S, Tsugane S. Serum cholesterol levels in relation to the incidence of cancer: the JPHC study cohorts. Int J Cancer. 2009;125(11):2679–86. https://doi.org/10.1002/ijc.24668.
Strasak AM, Pfeiffer RM, Brant LJ, Rapp K, Hilbe W, Oberaigner W, et al. Time-dependent association of total serum cholesterol and cancer incidence in a cohort of 172,210 men and women: a prospective 19-year follow-up study. Ann Oncol. 2009;20(6):1113–20. https://doi.org/10.1093/annonc/mdn736.
Cem HASSOY, Ahmet E. ERBAYCU, Aydan ÇAKAN, Ayşe ÖZSÖZ1, Filiz HEKİMGİL. Serum lipid profile in cases with lung cancer. Göğüs Hastanesi Dergisi. 2003;17:11–8.
Kritchevsky SB, Wilcosky TC, Morris DL, Truong KN, Tyroler HA. Changes in plasma lipid and lipoprotein cholesterol and weight prior to the diagnosis of cancer. Cancer Res. 1991;51(12):3198–203.
Winawer SJ, Flehinger BJ, Buchalter J, Herbert E, Shike M. Declining serum cholesterol levels prior to diagnosis of colon cancer. A time-trend, case-control study. Jama. 1990;263(15):2083–5. https://doi.org/10.1001/jama.1990.03440150091032.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension (Dallas, Tex : 1979). 2003;42(6):1206–52.
Improving Care and Promoting Health in Populations: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S7-s13.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. https://doi.org/10.1093/clinchem/18.6.499.
Bucolo G, David H. Quantitative determination of serum triglycerides by the use of enzymes. Clin Chem. 1973;19(5):476–82. https://doi.org/10.1093/clinchem/19.5.476.
Ng'andu NH. An empirical comparison of statistical tests for assessing the proportional hazards assumption of Cox's model. Stat Med. 1997;16(6):611–26. https://doi.org/10.1002/(SICI)1097-0258(19970330)16:6<611::AID-SIM437>3.0.CO;2-T.
Asano K, Kubo M, Yonemoto K, Doi Y, Ninomiya T, Tanizaki Y, et al. Impact of serum total cholesterol on the incidence of gastric cancer in a population-based prospective study: the Hisayama study. Int J Cancer. 2008;122(4):909–14. https://doi.org/10.1002/ijc.23191.
His M, Zelek L, Deschasaux M, Pouchieu C, Kesse-Guyot E, Hercberg S, et al. Prospective associations between serum biomarkers of lipid metabolism and overall, breast and prostate cancer risk. Eur J Epidemiol. 2014;29(2):119–32. https://doi.org/10.1007/s10654-014-9884-5.
Strohmaier S, Edlinger M, Manjer J, Stocks T, Bjørge T, Borena W, et al. Total serum cholesterol and cancer incidence in the metabolic syndrome and Cancer project (me-can). PLoS One. 2013;8(1):e54242. https://doi.org/10.1371/journal.pone.0054242.
Ulmer H, Borena W, Rapp K, Klenk J, Strasak A, Diem G, et al. Serum triglyceride concentrations and cancer risk in a large cohort study in Austria. Br J Cancer. 2009;101(7):1202–6. https://doi.org/10.1038/sj.bjc.6605264.
Benn M, Tybjærg-Hansen A, Stender S, Frikke-Schmidt R, Nordestgaard BG. Low-density lipoprotein cholesterol and the risk of cancer: a mendelian randomization study. J Natl Cancer Inst. 2011;103(6):508–19. https://doi.org/10.1093/jnci/djr008.
Vona R, Iessi E, Matarrese P. Role of cholesterol and lipid rafts in Cancer signaling: a promising therapeutic opportunity? Front Cell Dev Biol. 2021;9:622908. https://doi.org/10.3389/fcell.2021.622908.
Emberson JR, Kearney PM, Blackwell L, Newman C, Reith C, Bhala N, et al. Lack of effect of lowering LDL cholesterol on cancer: meta-analysis of individual data from 175,000 people in 27 randomised trials of statin therapy. PLoS One. 2012;7(1):e29849. https://doi.org/10.1371/journal.pone.0029849.
Mamtani R, Lewis JD, Scott FI, Ahmad T, Goldberg DS, Datta J, et al. Disentangling the association between statins, cholesterol, and colorectal Cancer: a nested case-control study. PLoS Med. 2016;13(4):e1002007. https://doi.org/10.1371/journal.pmed.1002007.
Carter P, Vithayathil M, Kar S, Potluri R, Mason AM, Larsson SC, et al. Predicting the effect of statins on cancer risk using genetic variants from a Mendelian randomization study in the UK biobank. Elife. 2020;9. https://doi.org/10.7554/eLife.57191.
Wulaningsih W, Garmo H, Holmberg L, Hammar N, Jungner I, Walldius G, et al. Serum Lipids and the Risk of Gastrointestinal Malignancies in the Swedish AMORIS Study. J Cancer Epidemiol. 2012;2012:792034.
Shor R, Wainstein J, Oz D, Boaz M, Matas Z, Fux A, et al. Low serum LDL cholesterol levels and the risk of fever, sepsis, and malignancy. Ann Clin Lab Sci. 2007;37(4):343–8.
Touvier M, Fassier P, His M, Norat T, Chan DS, Blacher J, et al. Cholesterol and breast cancer risk: a systematic review and meta-analysis of prospective studies. Br J Nutr. 2015;114(3):347–57. https://doi.org/10.1017/S000711451500183X.
Ozturk MA, Keçeci M, Komoglu S, Eryılmaz M, Sertbaş Y, Sertbaş M, et al. Association between hyperlipidemia and mammographic breast density in post-menopausal women. South Clin Istanbul Eurasia. 2018;29:110–4.
Ding X, Zhang W, Li S, Yang H. The role of cholesterol metabolism in cancer. Am J Cancer Res. 2019;9(2):219–27.
Henriksson P, Eriksson M, Ericsson S, Rudling M, Stege R, Berglund L, et al. Hypocholesterolaemia and increased elimination of low-density lipoproteins in metastatic cancer of the prostate. Lancet. 1989;2(8673):1178–80. https://doi.org/10.1016/s0140-6736(89)91790-x.
Vitols S, Gahrton G, Björkholm M, Peterson C. Hypocholesterolaemia in malignancy due to elevated low-density-lipoprotein-receptor activity in tumour cells: evidence from studies in patients with leukaemia. Lancet. 1985;2(8465):1150–4. https://doi.org/10.1016/s0140-6736(85)92679-0.
Calleros L, Lasa M, Toro MJ, Chiloeches A. Low cell cholesterol levels increase NFkappaB activity through a p38 MAPK-dependent mechanism. Cell Signal. 2006;18(12):2292–301. https://doi.org/10.1016/j.cellsig.2006.05.012.
Yang X, So W, Ko GT, Ma RC, Kong AP, Chow CC, et al. Independent associations between low-density lipoprotein cholesterol and cancer among patients with type 2 diabetes mellitus. Cmaj. 2008;179(5):427–37. https://doi.org/10.1503/cmaj.071474.
Kuo C-N, Liao Y-M, Kuo L-N, Tsai H-J, Chang W-C, Yen Y. Cancers in Taiwan: practical insight from epidemiology, treatments, biomarkers, and cost. J Formos Med Assoc. 2020;119(12):1731–41. https://doi.org/10.1016/j.jfma.2019.08.023.
Ng CJ, Teo CH, Abdullah N, Tan WP, Tan HM. Relationships between cancer pattern, country income and geographical region in Asia. BMC Cancer. 2015;15(1):613. https://doi.org/10.1186/s12885-015-1615-0.
Huang YC, Chen YH. Cancer incidence characteristic evolution based on the National Cancer Registry in Taiwan. J Oncol. 2020;2020:1408793.
Acknowledgements
We would like to thank Editage (https://www.editage.com.tw/) for editing and proofreading this manuscript.
Authors‘contributions
Y.-C.C.: Conceptualization, designing the study, analysing and interpreting the data, drafting and revising the article. C.-J.L.: Conceptualization, designing the study, revising the article. T.-L.Y.: Conceptualization, designing the study, data acquisition. M.-C.T.: Conceptualization, designing the study, data acquisition. L.-Y.H.: Data acquisition and analysing the data. K.-L.C.: Conceptualization, designing the study. H.-Y.H.: Conceptualization, designing the study, data acquisition, analysing and interpreting the data, revising the article. All authors read and approved the final manuscript.
Funding
None declared.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was in adherence with the Declaration of Helsinki. The protocol was reviewed and approved by the Research Ethics Committee of National Taiwan University Hospital. The committee complied with the Good Clinical Practice Guidelines (NTUH-REC number: 201901103 W [Institutional Review Board reference]).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1
: Adjusted relative risks and 95% confidence intervals of all-cause cancer incidence in the low-decreased group against all other groups for the LDL-C component.
Additional file 2: Table S2
: Subgroup analysis for the adjusted relative risks and 95% confidence intervals of all-cause cancer incidence according to quartiles of TC and LDL-C components.
Additional file 3: Table S3
: Sensitivity analysis for the adjusted relative risks and 95% confidence intervals of all-cause cancer incidence according to quartiles and interval changes of each lipid component.
Additional file 4: Table S4–1
: Distribution of BMI values for interval changes in the LDL-C component in the cohort population. Table S4–2: BMI change between TwSHHH 2002 and TwSHHH 2007 for the LDL-C component in the cohort population. Table S4–3: Sensitivity analysis for the adjusted relative risks and 95% confidence intervals of all-cause cancer incidence according to the interval changes in each lipid component.
Additional file 5: Table S5
: Time distribution of cancer diagnosis after TwSHHH 2002 according to the interval changes in each lipid component.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chang, YC., Lin, CJ., Yeh, TL. et al. Lipid biomarkers and Cancer risk - a population-based prospective cohort study in Taiwan. Lipids Health Dis 20, 133 (2021). https://doi.org/10.1186/s12944-021-01570-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-021-01570-1





