Abstract
Background
Clinical risk factors related to not administering thrombolysis to acute ischemic stroke patients with incidence dyslipidemia is not clear. This issue was investigated in telestroke and non-telestroke settings.
Methods
We analyzed retrospective data collected from a stroke registry to compare exclusion risk factors in the telestroke and non-telestroke. We performed multivariate analysis was performed to identify risk factors that may result in exclusion from rtPA. Variance inflation factors were used to examine multicollinearity and significant interactions between independent variables in the model, while Hosmer-Lemeshow test, Cox & Snell were used to determine the fitness of the regression models.
Results
A greater number of patients with acute ischemic stroke with incidence dyslipidemia were treated in the non-telestroke (285) when compared with the telestroke network (187). Although non-telestroke admitted more patients than the telestroke, the telestroke treated more patients with rtPA (89.30%) and excluded less (10.70%), while the non-telestroke excluded from rtPA (61.40%). In the non-telestroke, age (adjusted OR, 0.965; 95% CI, 0.942–0.99), blood glucose level (adjusted OR, 0.995; 95% CI, 0.99–0.999), international normalized ratio (adjusted OR, 0.154; 95% CI, 0.031–0.78),congestive heart failure(CHF) (adjusted OR, 0.318; 95% CI, 0.109–0.928), previous stroke (adjusted OR, 0.405; 95% CI, 0.2–0.821) and renal insufficiency (adjusted OR, 0.179; 95% CI, 0.035–0.908) were all directly linked to exclusion from rtPA. In the telestroke, only body mass index (adjusted OR, 0.911; 95% CI, 0.832–0.997) significantly excluded acute ischemic stroke patients with incidence dyslipidemia from thrombolysis therapy.
Conclusion
Despite having more patients with acute ischemic stroke that present incidence dyslipidemia, the non-telestroke patients had more clinical risk factors that excluded more patients from rtPA when compared with telestroke. Future studies should focus on how identified clinical risk factors can be managed to improve the use of rtPA in the non-telestroke setting. Moreover, the optimization of the risk-benefit ratio of rtPA by the telestroke technology can be advanced to the non-telestroke setting to improve the use of thrombolysis therapy.
Similar content being viewed by others
Background
The association between dyslipidemia and stroke is complicated and appears to vary depending on the stroke subtype, cholesterol levels, and lipid parameters [1]. For example, severe ischemic stroke and worse outcomes have been observed in patients that present with lower levels of cholesterol (TC) [2]. However, other studies [3, 4] found no association between levels of either TC or low-density lipoprotein (LDL-C), and stroke severity or outcome. In some studies, patients with lower total glyceride (TG) levels suffer more severe strokes [5, 6], while other studies showed higher TG levels in patients with a worse incidence stroke [7]. Contrarily, TG levels are not related to mortality and functional outcome [3, 8]. The conflicting results observed in dyslipidemia and ischemic stroke may be linked to the heterogeneity of stroke [9], and could affect the exclusion or inclusion of patients for recombinant tissue plasminogen (rtPA) irrespective of whether the patient is treated in the telestroke or non-telestroke setting.
A study comparing patients treated with rtPA in telestroke versus non-telestroke suggest that there is similarity in outcomes [10]; however, telestroke centers were shown to provide a twofold increase in the rates of rtPA [11]. Given the conflicting results of dyslipidemia’s effect on ischemic stroke, our first objective is to compare demographic and risk factors in patients with stroke that present with incidence dyslipidemia in the telestroke setting as compared with the non-telestroke. The presence or absence of specific risk factors in patients presenting with ischemic stroke and incidence dyslipidemia may contribute to the exclusion of patients from treatment with rtPA in either the telestroke or non-telestroke setting. One possibility is that acute ischemic stroke patients with incidence dyslipidemia are not present in the same proportions in the population of stroke patients in the telestroke and non-telestroke condition. For instance, since telestroke provided a twofold increase in the rates for rtPA, it is possible that more patients with acute ischemic stroke with incidence dyslipidemia may not receive thrombolytic therapy in the non-telestroke when compared with the telestroke. Therefore, the second objective investigated whether acute ischemic stroke patients that presented with a history of dyslipidemia are more susceptible to exclusion from rtPA in non-telestroke when compared with telestroke. Understanding the criteria for exclusion from rtPA in ischemic stroke patients with incidence dyslipidemia in the telestroke when compared with non-telestroke could provide an insight into the measurable risks that may be targeted to increase the usage of rtPA. Additionally, it could aid in identifying other potential research areas to increase eligibility for rtPA in the telestroke or non-telestroke network.
Methods
Patient selection
We collected retrospective data for consecutive rtPA-treated acute ischemic stroke patients from a regional stroke registry to study the exclusion criteria in patients presenting with acute ischemic strokes with incidence dyslipidemia in a telestroke versus non-telestroke study design. We have described the registry in previous studies [12,13,14]. Briefly, eligibility for rtPA was based on the AHA inclusion guidelines for the management of patients with acute ischemic stroke [15], and all cases of stroke were confirmed by computed tomography (CT). This study was approved by the institutional Committee for Ethics and the Institutional Review Board of the Greenville Health System. Patient information was retrieved from a database, and those with final discharge diagnoses inconsistent with ischemic stroke or transient ischemic attack were excluded. We collected two years data (2014 and 2016) from patients in the telestroke and non-telestroke. Baseline characteristics collected included NIHSS score and pre-rtPA systolic/diastolic blood pressures. A history of comorbid risk factors, including hypertension, diabetes mellitus, a previous stroke or transient ischemic attack, and `atrial fibrillation was also collected. Other comorbidities included carotid artery stenosis, hypertension, prosthetic heart valve, renal insufficiency, smoking, sleep apnea, migraine, obesity, and peripheral vascular disease. Demographic data were also collected including age, sex, race, and ethnicity. The study excluded patients that received endovascular therapy in order to maintain the homogeneity of the data. Acute ischemic stroke patients with incidence dyslipidemia without medical records were excluded as well. Both groups of patients were treated within similar time frames and the telemedicine evaluations were performed by stroke neurologists at the hub hospital. In the first 24 h, consultations for stroke were available to the spoke hospital and local neurologists were utilized to provide follow-up care. A stroke nurse collected data from patients that presented with signs and symptoms that could indicate acute ischemic stroke with incidence dyslipidemia. To confirm the presence or absence of a stroke, imaging results were utilized and then symptoms indices were used to correlate the results. In our data analysis, we defined dyslipidemia using the description of the American Heart Association that are consistent with the 95th percentile in the population when total cholesterol is greater than 5.2 mmol/L (200 mg/dl), LDL greater than 3.4 mmol/L (130 mg/dl), HDL less than 0.9 mmol/L (35 mg/dl), or triglycerides greater than 1.7 mmol/L (150 mg/dl) or current treatments that involve using a drug to lower cholesterol [16].
Data analysis
We performed the initial exploratory data analyses using box plots, outlier estimation, and stem and leaf plots to discover extreme results, and missing variables were reviewed before analyses. All data were analyzed using the SPSS Statistics Software version 22.0 (Chicago, IL) and the significant level was determined at P < 0.05 for group comparisons. The patient data was de-identified and divided into the rtPA group and the no-rtPA group based on whether they received rtPA or not. The patient demographics, clinical variables, and comorbidities in the rtPA and no rtPA groups were compared by using two-tailed independent samples, and Student’s t-tests was considered for continuous variables. In addition, analysis were done to determine the mean, standard deviation, and range. For the categorical variables, Pearson’s Chi-Squared analysis was used, and the overall number of patients and percentage of patients for each variable was calculated. A regression analysis using Bayesian shrinkage was used to eliminate bias in variable selection and a relatively large number of potential covariates. The shrinkage enables reduced bias and stabilization of the model. To model the relationship between continuous variables and outcome, 25% of the total sample population was randomly selected and fractional polynomials were used to identify variables that provided the best fit in linearity. We retained variables if the resulting p-value was less than 0.001, and we excluded and eliminated stepwise all variables with p-values > 0.001. We re-added all previously eliminated variables and retained them in the model if the p < 0.001 criteria were fulfilled. For the final model, predicted parameters were estimated using standard errors and odds ratios. Additionally, all variables were calculated with a 95% asymptotic confidence interval. Variance inflation factors were utilized to evaluate multicollinearity and significant interactions between the independent variables.
Results
In this study, 285 acute stroke patients with incidence dyslipidemia were admitted in the non-telestroke network, while 187 were admitted in the telestroke network (Table 1). Of the 285 patients in the non-telestroke, 110 received rtPA and 175 did not receive rtPA. Of the 187 patients treated in the telestroke, 167 received rtPA and 20 did not.
Table 2 presents the clinical characteristics that are associated with rtPA status for the telestroke and non-telestroke acute ischemic stroke patients that have a history of dyslipidemia. As shown in the table, 175 dyslipidemia stroke patients in the non-telestroke and 20 patients in the telestroke were excluded from rtPA. Dyslipidemia stroke patients excluded from receiving rtPA in the non-telestroke were older (71.8 yr. ± 12.6 yr. vs. 68.5 yr. ± 13.2 yr), ambulate independently (17.7% vs 5.4%), and had a history of a previous stroke (41.4% vs 28.2%), renal insufficiency (9.7% vs 2.7%), high blood glucose (162.1 ± 101.5 vs 136.8 ± 60.4), high creatinine (1.4 ± 1.1 vs 1.2 ± 0.6), high INR (1.2 ± 0.7vs 1.1 ± 0.1), and low diastolic blood pressure (78.8 ± 19.1 vs 84.4 ± 17.9). For the telestroke, excluded patients were not likely to be using cholesterol reducers (11.4% vs 73.7%), ambulate independently (5.4% vs 19.2%), and were admitted to the ED (5.4% vs 23.4%).
Data analysis using multivariate approach with Bayesian shrinkage (Table 3) showed that after adjustments for all risk factors and variables, obesity (adjusted OR, 3.059; 95% CI, 1.514–6.177), direct admission (adjusted OR, 30.346; 95% CI, 13.224–69.637) and rtPA administration (adjusted OR, 8.012; 95% CI, 3.26–19.687) were associated with the telestroke while systolic blood pressure (adjusted OR, 0.986; 95% CI, 0.973–0.999) was associated non-telestroke.
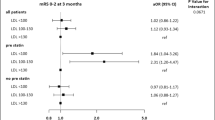
Further adjusted analysis with binary logistical regression was carried out to determine risk variables related to exclusion or inclusion for rtPA in the stroke population as a whole (telestroke and non-telestroke; Table 4). Our analyses identified NIH Stroke Scale Score (adjusted OR, 1.048; 95% CI, 1.011–1.085) and telestroke (adjusted OR, 13.904; 95% CI, 6.417–30.129) to be associated with inclusion for rtPA, while increasing age (adjusted OR, 0.974; 95% CI, 0.953–0.995), blood glucose level (adjusted OR, 0.996; 95% CI, 0.992–1), INR (adjusted OR, 0.194; 95% CI, 0.051–0.733), and renal insufficiency (adjusted OR, 0.349; 95% CI, 0.118–1.033) were related to exclusion from rtPA.
In patients treated in non-telestroke (Table 5), age (adjusted OR, 0.965; 95% CI, 0.942–0.99), blood glucose level (adjusted OR, 0.995; 95% CI, 0.99–0.999), INR (adjusted OR, 0.154; 95% CI, 0.031–0.78), CHF (adjusted OR, 0.318; 95% CI, 0.109–0.928), a previous stroke event (adjusted OR, 0.405; 95% CI, 0.2–0.821), and renal insufficiency (adjusted OR, 0.179; 95% CI, 0.035–0.908) were related to exclusion from rtPA. On the other hand, antiplatelet or anticoagulant (adjusted OR, 2.632; 95% CI, 1.288–5.38) was associated with rtPA inclusion in the acute ischemic stroke patients with incidence dyslipidemia. In the telestroke (Table 6), only BMI (adjusted OR, 0.911; 95% CI, 0.832–0.997) was related to exclusion from rtPA in stroke patients with incidence dyslipidemia.
Discussion
Four major findings arose from this study. First, within the same time frame, more patients presenting with acute ischemic stroke with incidence dyslipidemia were admitted to the non-telestroke when compared with the telestroke. Second, although non-telestroke admitted more patients than the telestroke, more patients received rtPA and fewer patients were excluded from rtPA in the telestroke. Third, more clinical variables were related to rtPA inclusion in the telestroke when compared with the non-telestroke. Finally, more risk factors were related to exclusion from rtPA in the non-telestroke when compared with the telestroke in patients with acute ischemic stroke with incidence dyslipidemia. The primary outcome of this analysis was rtPA exclusion of patients with acute ischemic stroke with incidence dyslipidemia. Other outcomes included individual components of the ischemic stroke and comorbidities associated with stroke or dyslipidemia.
In the univariate analysis, triglycerides, total cholesterol, LDL-C, HDL-C, and lipids were not found to be significantly different in rtPA and non-rtPA groups for both the telestroke and non-telestroke settings. Lipid levels were higher in the non-telestroke than the telestroke. This effect was attenuated in the adjusted analysis indicating that the proportion of exclusion does not depend on the site of treatment, but on the stroke population with incidence dyslipidemia. We observed that elderly stroke patients with incidence dyslipidemia who present with a high blood glucose level, high INR, CHF, a previous incidence of stroke, and renal insufficiency were excluded from rtPA in the non-telestroke. High blood glucose [17], CHF [18, 19], high INR [20], and a prior stroke event in the last 3 months [21] are well documented risk factors for stroke that affect outcomes in thrombolysis therapy.
Although there are conflicting results on the effects that dyslipidemia has on acute ischemic stroke patients, our study reveals that elderly acute ischemic stroke patients with incidence dyslipidemia are associated with underlying risk factors, including high blood glucose levels, and are more likely to face exclusion from rtPA. Chronic hyperglycemia has been shown to be a major risk for stroke, and acute hyperglycemia related to a stroke is an indicator of poor patient diagnosis [22]. The immediate and robust control of chronic hyperglycemia may not provide added advantages and, at worst, could cause damage [23]. For this reason, a targeted and coordinated approach to diminish the risk of blood glucose in stroke patients with incidence dyslipidemia is important.
Our finding that patients with acute ischemic stroke with incidence dyslipidemia, who present with CHF are more likely to face rtPA exclusion is supported by reports that CHF is linked to an increased risk of thrombus formation and is also associated with an increased risk of stroke in a 3-fold [18, 24, 25]. In addition, stroke in CHF patients is linked to both higher mortality and poor treatment outcomes [26]. Therefore, it is possible that the complex interplay between CHF, dyslipidemia, and stroke may account for the observed risk posed by CHF during stroke [27]. The exclusion of patients with elevated INR, and patients presenting with a previous stroke event in the last 3 months in the non-telestroke setting is not surprising, as similar results have been proposed in previous studies [28,29,30]. It is possible that the combined effect of old age, coupled with elevated INR and a previous stroke event occurring in the last 3 months played a role in the exclusion criteria in patients with acute ischemic stroke with incidence dyslipidemia.
In general, more risk factors were linked to exclusion from rtPA in the non-telestroke when compared with the telestroke; because BMI was the only exclusion risk factor in the telestroke. When assessed individually, clinical risk factors that excluded patients in the non-telestroke group may not represent the likely predictors of risk of post-rtPA [31]. For this reason, identification of each clinical risk factor may not be an effective method to determine the patient eligibility for rtPA in either the telestroke or non-telestroke setting [32]. We observed that there are significant effects of clinical risk factors in excluding stroke patients with incidence dyslipidemia from rtPA in the non-telestroke group, whereas only BMI excluded patients from rtPA exclusion in the telestroke. The relationship between dyslipidemia and stroke is complicated and could affect the exclusion or inclusion of patients for rtPA irrespective of whether the patients are treated in the telestroke or non-telestroke setting. The fact that only BMI excluded patients from rtPA exclusion in the telestroke, suggests that the telestroke technology may optimize the risk-benefit ratio of rtPA to allow clinicians to accurately make good decisions in the treatment of acute ischemic stroke patients with incidence dyslipidemia.
There are several limitations in this study. An example of this is that data used in the study is retrospective, and suggest variability in the determination of confounding variables. Although we adjusted for confounding factors, our comparisons were focused on telestroke versus non-telestroke and not within the telestroke and non-telestroke groups. However, a strength of this study is its use of a large stroke center that monitors quality treatment in the telestroke and non-telestroke network. Because of this, our study is well equipped to evaluate both rtPA and exclusivity criteria in acute ischemic stroke patients with incidence dyslipidemia. Our study highlights the clinical significance of risk factors in elderly stroke patients (> 80) with incidence dyslipidemia, indicating that early identification of risk factors and treatment could improve outcomes with thrombolysis therapy.
Conclusion
Although the role and interactive effects of individual risk factors in the exclusion from rtPA is not clear, the interaction between these factors and dyslipidemia suggests aggressive multiple risk-reduction measures for acute ischemic stroke patients with incidence dyslipidemia. This study contributes to existing literature in stroke and dyslipidemia by showing that the telestroke technology excluded fewer stroke patients with incidence dyslipidemia when compared with non telestroke, offering clues for thrombolysis therapy optimization in the treatment of acute ischemic stroke with incidence dyslipidemia.
Abbreviations
- Adjusted OR-:
-
Adjusted odd ratio
- BMI:
-
Body mass index
- CHF:
-
Congestive heart failure
- CI:
-
Confidence interval
- INR:
-
International normalized ratio
- LDL-C:
-
Low-density lipoprotein
- rtPA:
-
Recombinant tissue plasminogen
- TC:
-
Total cholesterol
- TG:
-
Total glyceride
References
Pol T, Held C, Westerbergh J, Lindbäck J, Alexander JH, Alings M, Erol C, Goto S, Halvorsen S, Huber K, Hanna M, Lopes RD, Ruzyllo W, Granger CB, Hijazi Z. Dyslipidemia and risk of cardiovascular events in patients with atrial fibrillation treated with Oral anticoagulation therapy: insights from the ARISTOTLE (Apixaban for reduction in stroke and other thromboembolic events in atrial fibrillation) trial. J Am Heart Assoc. 2018;7.3:1–11.
Koton S, Schneider ALC, Rosamond WD, Shahar E, Sang YY, Gottesman RF, et al. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA. 2014;312(3):259–68.
Jain M, Jain A, Yerragondu N, Brown RD, Rabinstein A, Jahromi B. The triglyceride paradox in stroke survivors: a prospective study. Neurosci J. 2013;12:34–41.
Lu D, Li P, Zhou YY, Xu XI XL, Liu LP, Tian Z. Association between serum non-high-density lipoprotein cholesterol and cognitive impairment in patients with acute ischemic stroke. BMC Neurol. 2016;16:154.
Dziedzic T, Pera J, Slowik A, Gryz-Kurek EA, Szczudlik A. Hypoalbuminemia in acute ischemic stroke patients: frequency and correlates. Eur J Clin Nutr. 2007;61(11):1318–22.
Weir CJ, Sattar N, Walters MR, Lees KR. Low triglyceride, not low cholesterol concentration, independently predicts poor outcome following acute stroke. Cerebrovasc Dis. 2003;16(1):76–82.
Simundic AM, Nikolac N, Topic E, Basic-Kes V, Demarin V. Are serum lipids measured on stroke admission prognostic? Clin Chem Lab Med. 2008;46(8):1163–7.
Tuttolomondo A, Di Raimondo D, Pedone C, Pinto A, Licata G. Effects of clinical and laboratory variables at admission and of in-hospital treatment with cardiovascular drugs on short term prognosis of ischemic stroke. The GIFA study. Cerebrovasc Dis. 2013;35:619.
Boehme AK, Esenwa C, Elkind MSV. Stroke risk factors, genetics, and prevention. Circ Res. 2017;120(3):472–95.
Bladin CF, Cadilhac DA. Effect of Telestroke on emergent stroke care and stroke outcomes. Stroke. 2014;45(6):1876.
Sairanen T, Soinila S, Nikkanen M, Rantanen K, Mustanoja S, Farkkila M, et al. Two years of Finnish Telestroke thrombolysis at spokes equal to that at the hub. Neurology. 2011;76(13):1145–52.
Nathaniel TI, Cochran T, Chaves J, Fulmer E, Sosa C, Yi S, et al. Co-morbid conditions in use of recombinant tissue plasminogen activator (rt-PA) for the treatment of acute ischaemic stroke. Brain Inj. 2016;30(10):1261–5.
Colello MJ, Ivey LE, Gainey J, Faulkner RV, Johnson A, Brechtel L, et al. Pharmacological thrombolysis for acute ischemic stroke treatment: gender differences in clinical risk factors. Adv Med Sci. 2018;63(1):100–6.
Gainey J, Brechtel L, Konklin S, Madeline L, Lowther E, Blum B, et al. In a stroke cohort with incident hypertension; are more women than men likely to be excluded from recombinant tissue-type plasminogen activator (rtPA)? J Neurol Sci. 2018;387:139–46.
Schwamm LH, Fonarow GC, Reeves MJ, Pan W, Frankel MR, Smith EE, et al. Get with the guidelines-stroke is associated with sustained improvement in Care for Patients Hospitalized with Acute Stroke or transient ischemic attack. Circulation. 2009;119(1):107–U206.
Kavey REW, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. J Pediatr. 2003;142(4):368–72.
Yao M, Ni J, Zhou L, Peng B, Zhu Y, Cui L. Elevated fasting blood glucose is predictive of poor outcome in non-diabetic stroke patients: a sub-group analysis of SMART. PLoS ONE. 2016;11(8):1–10.
Boovalingam P, Chunduri A, Berberic S, Brawn L, Blake M, O'Kane D, et al. Assessment of severity and clinical outcome of acute Ischemic stroke in patients with diabetes compared with patients with chronic heart failure: retrospective case series. Diabet Med. 2017;34:93.
Ois A, Gomis M, Cuadrado-Godia E, Jimenez-Conde J, Rodriguez-Campello A, Bruguera J, et al. Heart failure in acute ischemic stroke. J Neurol. 2008;255(3):385–9.
Tanne JH. Study shows what INR level is best for preventing stroke in patients with atrial fibrillation. Br Med J. 2003;327(7416):638.
Thacker EL, Wiggins KL, Rice KM, Longstreth WT, Bis JC, Dublin S, et al. Short-term and long-term risk of incident ischemic stroke after transient ischemic attack. Stroke. 2010;41(2):239–43.
Chen R, Ovbiagele B, Feng WW. Diabetes and stroke: epidemiology, pathophysiology, pharmaceuticals and outcomes. Am J Med Sci. 2016;351(4):380–6.
Duncan AE. Hyperglycemia and perioperative glucose management. Curr Pharm Des. 2012;18(38):6195–203.
Haeusler KG, Laufs U, Endres M. Chronic heart failure and ischemic stroke. Stroke. 2011;42(10):2977–U483.
Witt BJ, Gami AS, Ballman KV, Brown RD, Meverden RA, Jacobsen SJ, et al. The incidence of ischemic stroke in chronic heart failure: a meta-analysis. J Card Fail. 2007;13(6):489–96.
Scherbakov N, Haeusler KG, Doehner W. Ischemic stroke and heart failure: facts and numbers. Esc Heart Fail. 2015;2(1):1–4.
Rundek T, Sacco RL. Risk factor management to prevent first stroke. Neurol Clin. 2008;26(4):1007–45.
Demaerschalk. Scientific rationale for the inclusion and exclusion criteria for intravenous Alteplase in acute ischemic stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association (vol 47, pg 581, 2016). Stroke. 2016;47(11):E262-E.
Buchan AM. Why are stroke patients excluded from tPA therapy? An analysis of patient eligibility - reply. Neurology. 2001;57(9):1739–40.
Chuanjie WU, Di WU JC, Chuanhui L, Xunming J. why not intravenous thrombolysis in patients with recurrent stroke within 3 months? Ageing Dis. 2018;9(2):309–16.
Whiteley WN, Slot KB, Fernandes P, Sandercock P, Wardlaw J. Risk factors for intracranial hemorrhage in acute ischemic stroke patients treated with recombinant tissue plasminogen activator a systematic review and meta-analysis of 55 studies. Stroke. 2012;43(11):2904–U235.
Miller DJ, Simpson JR. Silver B Safety of Thrombolysis in Acute Ischemic Stroke: A Review of Complications, Risk Factors, and Newer Technologies. Neurohospitalist. 2011;13:138–47.
Acknowledgements
We thank the stroke unit of Greenville Health system for helping in data collection. This study was funded by Fullerton Foundation Grant.
Funding
This study was funded by the Fullerton Foundation Grant.
Availability of data and materials
Data and material in this study are available for use from the corresponding author.
Author information
Authors and Affiliations
Contributions
JD, BB and TIN designed the concept, experimental design and data analysis. LM, EL, RB and KC critically revised the drafts read and approved the last version of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is a retrospective data analysis, and was approved by Institutional Review Board of Greenville Health System and the institutional Committee for Ethics.
Consent for publication
All co-authors agreed to the submission of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gainey, J., Blum, B., Bowie, B. et al. Stroke and dyslipidemia: clinical risk factors in the telestroke versus non-telestroke. Lipids Health Dis 17, 226 (2018). https://doi.org/10.1186/s12944-018-0870-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-018-0870-x