Abstract
Cancer stem cells (CSCs), initially identified in leukemia in 1994, constitute a distinct subset of tumor cells characterized by surface markers such as CD133, CD44, and ALDH. Their behavior is regulated through a complex interplay of networks, including transcriptional, post-transcriptional, epigenetic, tumor microenvironment (TME), and epithelial-mesenchymal transition (EMT) factors. Numerous signaling pathways were found to be involved in the regulatory network of CSCs. The maintenance of CSC characteristics plays a pivotal role in driving CSC-associated tumor metastasis and conferring resistance to therapy. Consequently, CSCs have emerged as promising targets in cancer treatment. To date, researchers have developed several anticancer agents tailored to specifically target CSCs, with some of these treatment strategies currently undergoing preclinical or clinical trials. In this review, we outline the origin and biological characteristics of CSCs, explore the regulatory networks governing CSCs, discuss the signaling pathways implicated in these networks, and investigate the influential factors contributing to therapy resistance in CSCs. Finally, we offer insights into preclinical and clinical agents designed to eliminate CSCs.
Similar content being viewed by others
Introduction
Tumorigenesis and tumor progression are considered as complex and progressive processes that involve multiple levels of response and the accumulation of mutations. In the past several decades, many studies have emerged in the field of oncology regarding this topic. These studies have focused on tumor cells, the tumor microenvironment, tumor heterogeneity, etc., among which tumor heterogeneity is closely associated with tumorigenesis and the malignancy of tumors. As one of the theories to explain the underlying mechanism of tumor heterogeneity, cancer stem cells (CSCs) have received much attention [1].
CSCs were first found in the mid-1990s as a group of malignant tumor cells with the potential of self-renewal and differentiation, which were closely related to the tumorigenesis, metastasis and therapy resistance of tumors. They were identified in the blood of leukemia patients as a small specific subpopulation of cells which could initiate leukemia in immune-deficient mice [2]. In numerous studies, CSCs have consistently demonstrated their remarkable capacities for self-renewal, differentiation, sphere formation, and proliferation across various cancer types. These abilities are of significant relevance in the context of tumorigenesis. Moreover, CSCs possess the potential to drive tumor metastasis and confer resistance to therapy, thus playing pivotal roles in advancing tumor progression [3, 4]. Therefore, the study of CSCs is critical for understanding tumorigenesis and tumor progression, and many breakthroughs have already been made. To date, cell surface markers have been used to distinguish initial mutant cell populations of multiple tumors, including brain, prostate, breast, melanoma, lung and liver cancers [5,6,7,8,9,10]. However, it is still a challenge to find prospective markers to label CSCs in CSC-related studies. Generally, CSCs express CD133, CD44, EpCAM and ALDH [11, 12]. Nevertheless, CSC markers are slightly different across distinct cancer types due to tumor heterogeneity.
To gain a comprehensive understanding of CSCs and the intricate regulatory networks governing them, this review provides a comprehensive summary of the transcriptional, posttranscriptional, epigenetic modifications, tumor microenvironment (TME), and epithelial-mesenchymal transition (EMT) regulation of CSCs. Additionally, we delve into the signaling pathways intricately involved in these regulatory networks and explore influential factors contributing to therapy resistance in CSCs. Given that CSCs are increasingly recognized as promising targets in cancer treatment, we also spotlight CSC-associated targeting agents.
The origin of CSCs
Cancer stem cells (CSCs) are a subgroup of tumor cells that were first identified in leukemia in 1994. Dick and Bonnet isolated CSCs from leukemia and successfully differentiated this cell population into various hierarchies of leukemia cells in immune-deficient mice and showed that CSCs lead to the development of leukemia [13]. Increasing evidence has proved CSCs in a variety of solid tumors and these CSCs have subsequently demonstrated the potential of tumor-propagating and cell differentiation [14]. Breast cancer is the first solid tumor type in which CSCs were shown to exist [15]. Many other solid tumors have also been proven to contain CSCs, including colon cancer [16], pancreatic cancer [17] and brain cancers [18]. Besides, the presence of CSCs in various solid tumors exhibits considerable variability. Accordingly, the origin of CSCs is one of the hot topics in CSC research and is still elusive.
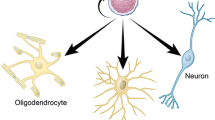
Various theories were proposed for the origin of stem cells, among which adult stem cells (ASCs)-origin theory and tumor cell-origin theory are the most mentioned [19]. For ASCs-origin theory in intestinal tumors, Dagmar Beier et al. had discovered that ASCs lost the APC gene in the long-term accumulation of transforming events, leading to carcinogenesis and the potential development of CSCs [20]. Tumor cell-origin theory indicated that CSCs originated from the stem-like tumor cells organized by the tumor heterogeneity [21]. Tumor heterogeneity refers to the fact that the cells of the tumor population itself exhibit phenotypic and functional differences [22]. In most cases, the different phenotypes of CSCs were a result of the tumor heterogeneity [23]. Conversely, CSCs were also identified as one of the primary factors contributing to tumor heterogeneity [24]. Furthermore, researches have shown that the potential mechanism by which tumor cells transform into CSCs involves genetic reprogramming or dynamic state switching [19]. However, there are several other possible origins of CSCs, including embryonal rest, somatic mutation, the cell fusion hypothesis, metabolic reprogramming, etc. [25].
Biological characteristics of CSCs
With gradual understanding of CSC characteristics, some breakthroughs have been made in tumor research. However, some CSC-related clinical problems in cancer treatments need to be further solved. Therefore, understanding the biological characteristics of CSCs is of great significance for exploring tumorigenesis and tumor development.
Self-renewal and differentiation are two representative characteristics of CSCs that could lead to tumorigenesis. Similar to ASCs, CSCs undergo both symmetric and asymmetric divisions stochastically with regulatory signaling pathways [26]. In symmetric division, one CSC divides into two to undergo self-renewal to replenish the CSC pool. Zhang et al. found that hTERThigh cells in prostate cancer exhibit stemness characteristics of CSCs by significantly increasing the proportion of symmetrically divided cells and realizing constant cell self-renewal [27]. Alternatively, asymmetric division produces transit-amplifying cells that terminally differentiate into tumorigenic potential cells and multilineage cells after stimulation. In glioblastoma, the endothelial differentiation function of CSCs contributes to tumor vasculature and promotes angiogenesis [28]. Additionally, CSCs also have sphere-formation and proliferation abilities. Studies had demonstrated that CSCs were distributed stochastically within a tumor and formed spheres even in serum deprivation [3, 29].
Surface markers play a crucial role in providing essential information for the understanding and investigation of CSCs. Over years of research, common surface markers have been well identified in CSCs across various tumor types. Generally, CSCs exhibit the expression of CD133, CD44, EpCAM, and ALDH in most cancers [11, 12]. Beyond these widely recognized markers, CSCs also display other non-classical markers such as CK17 and CD49f. For instance, CK17, a cytokeratin, has been reported to serve as a marker for CSCs in cervical cancer when co-expressed with OCT-4, NANOG, and SOX2 [30]. Additionally, CD49f, also known as Integrin Alpha 6, has emerged as a novel biomarker for CSCs. It is a transmembrane glycoprotein found in various tumors, including brain tumors, hepatocellular carcinoma (HCC), and lung cancer [31, 32]. However, it’s important to acknowledge that due to tumor heterogeneity, the surface markers of CSCs can exhibit slight variations in different types of cancer. For instance, Olfm4 and Ascl2 are highly expressed in gastrointestinal cancer but are absent in some hematological carcinomas [33]. CSCs from hematological carcinoma are usually positive for CD34, CD123, and CD33 but negative for CD38, CD90, CD117 and HLA-DR [34]. Brain cancers mostly express A2B5 and L1CAM, whereas cytokeratin 19 and OV-6 are specific markers for CSCs in HCC [35,36,37].
Regulatory networks of CSCs
Due to the inherent nature of stem cells, CSCs are proficient in self-renewal and differentiation. Additionally, they share some similar regulatory networks, such as transcription factors and posttranscriptional and epigenetic control. In addition, CSC characteristics are inseparable from complex interactions with the microenvironment. This section introduces the regulatory networks of CSCs based on five perspectives: transcriptional control, posttranscriptional control, epigenetic modification control, TME control and EMT control (Figs. 1 and 2).
Epigenetic modification, transcriptional control and posttranscriptional control of CSCs. Epigenetic modification, transcriptional control, and posttranscriptional control are three critical mechanisms within the CSC regulatory networks. These regulatory mechanisms play pivotal roles in maintaining CSC stemness, CSC-associated tumor metastasis, and CSC-associated therapy resistance. A The figure illustrates how methyl groups modify DNA and histones, influencing downstream gene expression at the epigenetic level. B Transcriptional control in CSCs is primarily attributed to six specific transcription factors: PBX1, Oct4, Sox2, c-Myc, KLF4, and Nanog. C Posttranscriptional control factors encompass RNA-binding proteins, N6-methyladenosine, A-to-I conversion, miRNAs, and lncRNAs
Tumor microenvironment control of CSCs. Various nontumor cells, including stromal cells and immune cells, and metabolic control which exist in the tumor microenvironment participate in CSC characteristic maintenance, CSC-associated tumor metastasis and CSC-associated therapy resistance. Cancer-associated fibroblasts (CAFs) are the most representative stromal cells, and tumor-associated macrophages (TAMs) are the most essential immune cells. They contribute to CSC characteristics maintenance by secreting particular cytokines. The detailed cytokines and corresponding factors that these cytokines influenced were all shown in the yellow boxes. In term of metabolic control which could participate in CSC characteristic maintenance, glycolysis, glutaminolysis, lipogenesis and hypoxia-inducible factors are the most representative four parts (red boxes)
Transcriptional control of CSCs
Transcription factors (TFs) are defined as a group of protein molecules whose unique binding to genes activate a vital process, transcription, and thereby, they inhibit or enhance gene expression [38]. To date, aberrant expression of TFs has been identified in cancer cell uncontrolled proliferation, metastasis, angiogenesis and survival [39,40,41,42,43]. Notably, numerous TFs drive CSC-specific characteristics, such as self-renewal and differentiation [44]. Among these key stemness TFs, six specific TFs participate specifically in the transcriptional control of CSCs: Oct4, Sox2, c-Myc, KLF4, Nanog and PBX1 [45,46,47]. In the following section, we will introduce each of them (Fig. 1).
Oct4
Oct4 (also called POU5F1 or Oct3) is a putative TF involved in CSC characteristic regulation. Both upregulation and downregulation of Oct4 are implicated in CSC self-renewal, CSC-associated tumor metastasis and CSC-associated therapy resistance.
Overexpressed Oct4 has been found in CSCs in clinical tumor samples, such as oral cavity squamous cell carcinomas, pancreatic cancer and glioma, which supports CSC self-renewal [48,49,50]. Moreover, the high Oct4 expression observed in CSCs from lung cancer not only maintains self-renewal but also promotes CSC-associated tumor metastasis [51]. Oct4-overexpressing CSCs transactivate the M-CSF promoter to upregulate M-CSF secretion, thereby resulting in tumor metastasis [52]. In addition, EMT-associated signals are positively correlated with high Oct4 expression, which also promotes CSC-associated tumor metastasis in lung cancer, as well as in HCC [53, 54]. Furthermore, Stella Chai et al. demonstrated that in HCC, Oct4 expression directly influences CSC-associated therapy resistance [55]. This phenomenon also exists in melanoma and cervical cancer [56, 57]. Conversely, Oct4 downregulation leads to gradual loss of stemness characteristics [58]. After the knockdown of the Oct4 gene, the likelihood of malignant transformation of CSCs from pancreatic cancer was significantly reduced [59].
Sox2
SRY (sex determining region Y)-Box-2 (Sox2) is a transcription factor expressed by CSCs [60]. Evidence is mounting that Sox2 expression is required for the sphere-formation ability of CSCs, CSC proliferation and CSC-related chemotherapeutic resistance [61, 62].
CSCs have strong sphere-formation ability, which has been proven decades ago. High Sox2 expression is observed in nearly half of the basal cell-like breast carcinomas and is associated with sphere-formation ability and CSC proliferation [63]. Furthermore, Sox2 expression is crucial for the proliferation of CSCs in lung cancer and glioma, as it sustains the bidirectional transition between the stem-like state and the differentiated state [64, 65]. Other studies have shown that Sox2 deletion results in the blockade of tumorigenesis and deletion of CSC proliferation genes [66]. Barone C et al. demonstrated that oligodendroglioma initiation and CSC proliferation were strongly arrested by knocking down Sox2 [67]. Moreover, Sox2 knockdown-dependent cell cycle arrest and a decrease in tumoroids have been shown in glioblastoma and breast cancer [68, 69]. In addition to CSC proliferation, Sox2 regulates CSC-associated therapy resistance. Increasing evidence has illustrated that in breast cancer, CSC resistance to tamoxifen, an ER antagonist, is attributed to the activation of Sox2 [70].
c-Myc
In normal cell activities, the Myc family plays a fundamental role in cell metabolism, the cell cycle, and cell differentiation. The Myc family includes c-Myc, L-Myc and N-Myc, which have different functions [71]. Since c-Myc is most closely related to CSCs, this section only focuses on how c-Myc regulates CSCs in cancers. The dysregulation of c-Myc could influence CSC stemness maintenance, CSC-associated tumor metastasis and therapy resistance [72].
Superoxide dismutase (SOD2) is a downstream target gene of c-MYC, which regulates cell stemness characteristics. In tongue squamous cell carcinoma, c-MYC combines with SOD2 and drives CSC generation [73,74,75]. In addition, increased c-Myc expression maintains CSC stemness and induces CSC-associated tumor metastasis through EMT in breast cancer [74]. Data have demonstrated that the overexpression of c-Myc can induce the ‘awakening’ of dormant CSCs and directly regulate downstream genes to activate EMT, leading to CSC-associated tumor metastasis in nasopharyngeal cancer [75]. While promoting the stemness of CSCs, c-Myc also increases the therapy resistance of CSCs. According to Jun‐Nian Zhou et al., blocking c-Myc results in CSCs from HCC becoming more sensitive to chemical agents [76].
KLF4
KLF4 is a TF that regulates diverse cellular processes, such as the cell cycle and differentiation. However, KLF4 is a bifunctional TF in human cancers. In the past few years, KLF4 has been described as an anticancer factor. Studies have demonstrated that KLF4 performs a tumor suppression function in gastrointestinal cancers [77, 78], T-cell acute lymphoblastic leukemia (T-ALL) [79], lung cancer [80], meningioma [81] and bladder cancer [82].
KLF4 was found to also act as an oncogene to promote carcinogenesis by affecting CSC stemness maintenance and CSC-associated tumor metastasis. In osteosarcoma and glioma, CSCs acquire a higher self-renewal and sphere-formation ability through the KLF4-activated MAPK signaling pathway [83, 84]. The same process has been observed in pancreatic cancer. Kress TR et al. showed that KLF4 overexpression also promoted CSC-associated tumor metastasis in pancreatic cancer [85]. The mechanism was demonstrated for the first time in 2017: KLF4 could induce perivascular cell plasticity, which promotes premetastatic niche formation for CSCs [86]. Moreover, CSCs can stabilize KLF4 expression by promoting the deubiquitinating process of KLF4 and further enhance CSC-associated tumor metastasis [87]. Conversely, the suppression of KLF4 directly decreased CSC-associated tumor metastasis from the breast to the brain [88].
Nanog
Nanog is also a CSC-associated TF that was first discovered in embryonic stem cells. Notably, Nanog is expressed at a low level in differentiated cells but is overexpressed in stem cells [89]. It plays a central role in CSC characteristic maintenance, CSC-associated metastasis and therapy resistance in cancers.
Data have shown that the suppression of Nanog is detrimental to CSC self-renewal, sphere-formation ability, and CSC generation in glioma [90]. Alternatively, the role of Nanog overexpression in maintaining CSC characteristics has been reflected in renal, ovarian and liver cancers [91,92,93]. In breast cancer, high-level expression of Nanog can not only maintain CSC stemness but also promote CSC-associated tumor metastasis [94]. Liu L et al. showed that in non-small cell lung cancer (NSCLC), Nanog regulated downstream signaling pathways and protein expression to promote the EMT process, which promoted CSC-associated tumor metastasis [53]. Furthermore, overexpression of Nanog also results in CSC-associated cancer therapy resistance. Emerging evidence has demonstrated that Nanoghigh CSCs are insensitive to gemcitabine, salinomycin and cisplatin treatments [53, 95].
PBX1
PBX1, a transcription factor, has been identified as a key player in both tumorigenesis and the self-renewal of CSCs [96]. Jung et al. discovered that PBX1 played a role in maintaining the characteristics of CSCs in ovarian cancer [97]. Additionally, PBX1 has been reported as a regulator of CSC self-renewal and contributes to CSC characteristics maintenance in leukemia [98, 99]. These findings suggest that PBX1 could potentially serve as a novel target for CSC therapy.
Posttranscriptional control of CSCs
In addition to TFs, posttranscriptional control can also maintain the characteristics of CSCs and regulate CSCs. Posttranscriptional control refers to the regulation of gene expression at the RNA level, these RNAs are mainly referred to as mRNAs currently [100, 101]. Abnormalities in posttranscriptional control can lead to uncontrolled cell proliferation, vascular sprouting, EMT and other tumorigenic processes [102]. Recently, posttranscriptional control of CSCs in cancers has attracted extensive attention. Among the diverse methods of posttranscriptional control, RNA-binding proteins (RBPs), adenosine modification and noncoding RNAs have been proved to be important (Fig. 1).
RNA-binding proteins (RBPs)-mediated control of mRNA
RNA-binding proteins (RBPs) are of the utmost importance in tumorigenic processes. They bind to mRNA molecules once transcription initiates and regulate subsequent processing. RBPs not only act on mRNA cleavage, splicing, capping and modification but also regulate cellular stability and protein translation [103], which can also be used by tumors. To date, thousands of RBPs have been discovered in several tumors and play a role in tumor development [104, 105]. This section will introduce two key RBPs in the control of mRNA in CSCs: MSI and LIN28.
MSI
MSI, which regulates sensory organ precursor cells to divide asymmetrically, was identified in Drosophila. The MSI family includes MSI1 and MSI2, both of which impact CSC characteristic maintenance [106]. Data have also shown the multiple roles of MISI1 in CSC self-renewal, proliferation and CSC-associated therapy resistance [107].
Argonaute2 (AGO2) is a MIS1-binding partner that binds to MSI1 in response to environmental stress and influences cell fate. Chen HY et al. suggested that in glioblastoma and pancreatic ductal adenocarcinoma, the MSI1/AGO2 complex repressed downstream mRNA by binding to its 3’UTR or coding sequence, which allowed CSCs to maintain self-renewal and proliferation [108]. MSI1 overexpression also promotes the proliferation of CSCs in colorectal cancer (CRC). In addition, the latest research on CRC highlighted the role of 5-fluorouracil (5-FU) in inducing CSC-associated therapy resistance by upregulating MSI1 [109, 110]. In glioblastoma, overexpression of MSI1 modifies transcripts of checkpoint proteins to hyperactivate the DNA damage repair mechanism, which results in CSC-associated irradiation resistance [111].
Similar to MSI1, MSI2 also contributes to CSC self-renewal and CSC-associated therapy resistance. Emerging evidence has shown that MSI2 plays an important role as a posttranscriptional regulator in hematologic cancer [112]. In leukemia, the increased RNA binding activity of MSI2 is positively correlated with CSC self-renewal ability [113, 114]. Fang T et al. demonstrated that MSI2 upregulated CSC-related TFs in HCC, which maintained the stemness of CSCs [115]. In addition, the MSI2 protein has been proven to impede CSC sensitivity to chemotherapy and radiotherapy in ovarian cancer [116].
LIN28
Initially identified in Caenorhabditis elegans as a developmental regulator, LIN28 plays a role in various normal physiological processes, including cell development and proliferation. It exists in two paralog forms: LIN28a and LIN28b [117]. Emerging evidence suggests that LIN28 can regulate mRNA translation by binding to a ‘GGAGA’ motif, thereby influencing RNA splicing and processing. This is correlated with the maintenance of CSC characteristics and CSC-associated tumor metastasis [118].
Scientists have shown that LIN28 facilitates the expression of stemness-related TFs at the posttranscriptional level in several cancers, which could induce and maintain the stemness of CSCs [119, 120]. Yes-associated protein 1 (YAP1), which is the main downstream effector of the Hippo signaling pathway, is a newly discovered target of LIN28. Hailin Zou et al. have shown that LIN28 upregulates the expression of YAP1 to maintain CSC stemness and promote tumor growth in triple-negative breast cancer (TNBC) by inducing the mRNA decay of YAP1 upstream kinases [121, 122]. Furthermore, LIN28 alters the expression levels of vimentin and cadherins in breast cancer, which promote the sphere-formation ability of CSCs and CSC-associated tumor metastasis, respectively [123].
Adenosine modification-mediated control of mRNA
Apart from RBPs, adenosine modification of mRNA is another type of posttranscriptional control that maintains the stemness of CSCs and regulates carcinogenesis. Adenosine modification of mRNA refers to mRNA editing at the adenosine site, which changes the sequence information. N6-methyladenosine (m6A), adenosine-to-inosine (A-to-I) conversion and 5-methylcytosine (m5C) are three main forms of adenosine modification. However, the relationship between m5C and CSCs is uncertain. Therefore, this review focuses on m6A and A-to-I conversion in the remaining content.
N6-methyladenosine (m6A)
N6-methyladenosine (m6A) is methylation that occurs in the N6-position of adenosine, which is the most prevalent internal modification of mRNA. The action of m6A depends on three types of regulators, including m6A methyltransferase (METTLE), m6A demethylases, and m6A recognizer (the YTH and IMP families) [124]. Since m6A modifications are necessary for regulating cellular processing, it is not surprising that they are linked to CSC stemness maintenance, as well as CSC-associated therapy resistance.
Both m6A methylation and m6A demethylation can modify mRNAs at the posttranscriptional level to maintain CSC stemness. In terms of m6A methylation, reports have illustrated that YTHDF2 recognizes m6A installed by METTLE on the mRNA of several TFs to maintain CSC stemness [125,126,127,128]. In addition, suppressor of cytokine signaling 2 (SOCS2) is another target of METTLE for CSC stemness maintenance [129]. As a cytokine-inducible negative regulator, SOCS2 promotes CSC self-renewal and differentiation in HCC in a YTHDF2-dependent manner [130]. As for m6A demethylation, emerging evidence suggests that ALKBH5 removes m6A from FOXM1 mRNA in glioblastoma and maintains CSC stemness [117]. Furthermore, m6A demethylation shifts the alternative splicing of BCLX and NCOR2, which also contributes to glioma CSC self-renewal and tumor outgrowth [131,132,133]. Moreover, ALKBH5-dependent m6A demethylation of the TACC3 transcript is frequently modified in acute myeloid leukemia (AML), resulting in CSC stemness maintenance [134, 135].
Apart from functions in CSC stemness maintenance, m6A modification can also regulate CSC-associated therapy resistance. Scientists have suggested that m6A clearance decay induces CSC-associated radio-resistance in glioma [136, 137]. Furthermore, m6A clearance in leukemia induced by m6A demethylation modification has been proven to promote CSC-associated All-Trans Retinoic Acid therapy resistance [138,139,140].
Adenosine-to-inosine (A-to-I) conversion
Adenosine-to-inosine (A-to-I) conversion has also become a widespread part of the regulatory networks of CSCs. Initially, A-to-I conversion alters adenosine in double-stranded RNAs into inosine, and then inosine is recognized as guanine at the molecular level. This process is catalyzed by the adenosine deaminase (ADAR) family, which includes ADAR1, ADAR2 and ADAR3 [141]. Of note, A-to-I conversion makes it easy for CSCs to generate novel binding sites for tumor-regulating factors and produce new proteins with tumor-regulating effects [142, 143]. According to different ADARs, we will introduce how A-to-I conversion regulates the sphere-formation and proliferation ability of CSCs.
ADAR1 is actively and functionally expressed in various cancer types, such as liver, colorectal and thyroid cancers. For instance, ADAR1 catalyzes the A-to-I conversion of antizyme inhibitor 1 (AZIN1) mRNA in CSCs from HCC [144] and CRC [145], which is crucial to maintain the sphere-formation ability of CSCs. Otherwise, Cyclin-dependent serine/threonine protein kinase 13 (CDK13) is required for constitutive and alternative pre-mRNA splicing in thyroid cancer. Julia Ramírez‑Moya et al. demonstrated that ADAR1 catalyzed the A-to-I conversion at CDK13 mRNA to enhance CSC proliferation, which provides an advantage for thyroid cancer progression [146]. A similar phenomenon was also observed in HCC [147].
ADAR2 also participates in A-to-I conversion control of mRNA in CSCs. However, ADAR2 plays both promotive and inhibitory roles. Glutamate receptor subunit B (GRIA2) competitively binds calcium transporters to block calcium transportation and excitatory synaptic transmission [148]. In glioblastoma, ADAR2-catalyzed A-to-I conversion activates GRIA2 mRNA to promote CSC proliferation [149]. Conversely, ADAR2-mediated blocking of some genes also regulates CSCs. Increasing evidence has proven that ADAR2 can block CSC proliferation by inactivating podocalyxin-like (PODXL) in gastric cancer and inhibiting COPA (coatomer protein complex, subunit α) in HCC [150, 151]. In contrast to ADAR1 and ADAR2, ADAR3 is exclusively expressed in the brain and is not catalytically active. However, ADAR3 also regulates CSC proliferation in glioblastoma by directly competing with ADAR2 at the editing site of GRIA2 to inhibit ADAR2 [149].
Noncoding RNA-mediated control of mRNAs
Coding RNAs, also called mRNAs, represent the single-stranded RNAs that store genetic information and can be translated into proteins [152]. The remaining RNAs are known as noncoding RNAs, and they function in cellular mechanisms and gene regulation [153]. Noncoding RNAs include miRNAs, lncRNAs, rRNAs, tRNAs, snRNAs and snoRNAs [154]. Since most studies of CSCs are related to miRNAs and lncRNAs, in this review, we will only introduce these two types of noncoding RNA-mediated control of mRNA.
MicroRNAs (miRNAs)
MiRNAs are small noncoding RNAs. More than 2,000 miRNAs have been shown to regulate gene expression by recognizing cognate sequences and participating in transcriptional processes [155, 156]. To date, miRNAs have been largely identified in the fields of development and disease regulation, particularly in cancers [157]. Increasing evidence has illustrated the connection between various miRNAs and cancers, and these miRNAs can be divided into two classes: tumor suppressor class and tumor-promoting class.
On the one hand, the let-7 family and miR34 are members of the tumor suppressor class of miRNAs, which act in suppressing CSC stemness, reversing therapy resistance and inhibiting CSC-associated tumor metastasis [158]. Fengyan Yu et al. suggested that let-7 silenced the mRNAs of several oncogenes in breast cancer and negatively regulated CSC stemness [159]. Additionally, let-7-modulated mRNA silencing even arrested the G2-M phase of the CSC cell cycle in prostate cancer [160]. In gastric and ovarian cancers, let-7-induced posttranscriptional modification not only inhibits CSC self-renewal but also reverses chemoresistance [161, 162]. In addition to the let-7 family, miR34-a also has tumor suppressor functions. In various cancer types, miR-34a targets mRNAs of tumor-promoting genes to inhibit CSC self-renewal and proliferation [163, 164]. Apart from these findings, data also showed that the miR34-mediated inhibition of mRNAs of EMT-related TFs contributed to the inhibition of CSC-associated tumor metastasis in head and neck squamous cell carcinoma (HNSCC) and prostate cancer [165, 166].
On the other hand, miRNAs also have tumor-promoting functions. miR21 and miR221 are involved in this class of miRNAs that promote CSC stemness maintenance, CSC-associated tumor metastasis and CSC-associated therapy resistance [158]. MiR-21 is one of the first onco-miRNAs found to be overexpressed in multiple human cancers [167,168,169]. In pancreatic cancer and glioma, the posttranscriptional regulation of CSC-related TFs by miR-21 is an important step in maintaining CSC stemness [167, 170]. In breast cancer, miR-21 facilitates CSC metastasis by upregulating mesenchymal markers or synergistically regulating HIF-1α mRNA [171]. MiR-221 is another onco-miRNA. Quaking gene 5 (QKI-5) is an isoform of the QKI gene that can suppress the sphere-formation ability of CSCs and tumor formation. QKI-5 is downregulated in CRC through miR-221-dependent modulation [172, 173]. In addition, it has been reported that miR-221 promotes CSC-associated gemcitabine resistance at the posttranscriptional level in pancreatic cancer [170].
Long noncoding RNAs (lncRNAs)
Long noncoding RNAs (lncRNAs) are a class of transcripts encoded by the genome that are not translated into proteins. LncRNAs play key roles in various physiological and pathological processes, such as chromatin dynamics regulation, RNA processing, protein translation and stabilization [174]. Notably, aberrant expression and mutation of lncRNAs exist in most cancer types and play an essential role in the posttranscriptional control of CSCs [175]. Recently, increasing research has focused on the lncRNA-related posttranscriptional control of mRNAs in maintaining CSC stemness and proliferation ability [176]. This control could be classified into two ways, direct control and indirect control, and will be described separately in the following section.
Direct control of lncRNAs on mRNAs means that lncRNAs bind to target mRNA sequences directly to modulate mRNA stabilization or splicing. In breast cancer, lncRNA ROPM stabilizes PLA2G16 mRNA by binding to the 3’UTR terminal, activating the PI3K, WNT/β-catenin and Hippo signaling pathways to maintain CSC stemness and helping with tumor development [177]. Indirect control of lncRNAs on mRNAs involves two mechanisms. On the one hand, lncRNAs bind to mRNAs through RBPs as mediators. For example, the lncRNA KB-1980E6.3 regulation of c-Myc mRNA requires IMP1 as a mediator for combination and then maintains CSC stemness in breast cancer by upregulating stemness-related TF expression [178, 179]. On the other hand, lncRNAs act as “sponges” for miRNAs in the regulation of CSC properties. Emerging evidence demonstrates that lncRNA MALAT1 inhibits miR-375, miR-200c and miR-145 to promote stemness-related mRNA expression and maintain CSC stemness in various solid cancers [180,181,182,183]. LncRNA LOCCS blocks the activities of miR-93 to maintain the proliferation ability of CSCs in colon cancer [184]. Additionally, the overexpression of another lncRNA CCAT2 of CSCs in colon cancer plays the same role by inhibiting miR-145 [185].
Epigenetic modification control of CSCs
Epigenetic modifications mainly target genetic loci for transcriptional mechanisms and nucleosome remodeling without influencing the primary DNA sequence. DNA modification, histone modification and chromatin remodeling are three types of epigenetic modifications that maintain the stemness of CSCs [186]. Here, we only emphasize the functions of DNA modification and histone modification in this review (Fig. 1).
DNA modification
DNA methylation or demethylation is the most common DNA modification at the epigenetic level, and the modification site usually occurs at the guanine residues (CpG) [187]. DNA modification is crucial in cell development, apoptosis and differentiation [188]. In many cancer types, DNA methylation and demethylation change the expression level of some genes to regulate CSC characteristics [12].
Excessive DNA methylation can be achieved by the tumor itself and participate in CSC stemness maintenance and CSC-associated therapy resistance. For example, leucine-rich repeat containing G protein-coupled receptor (LGR5) is a well-known CSC marker in colon cancer [189]. DNA methylation-induced increased expression of LGR5 maintains the stemness of CSCs and promotes CSC-associated resistance to 5-fluorouracil [190]. Otherwise, gene mutations also lead to excessive DNA methylation of several enhancers at the epigenetic level. One study suggested that mutations in DNMT3 are related to aberrant stem cell gene expression and maintain CSC stemness in AML [191, 192].
Furthermore, DNA demethylation plays a role in regulating the sphere-formation ability of CSCs and CSC-associated therapy resistance. Hyun-Mi Kwon et al. demonstrated that DNMT1 inhibitors affect the sphere-formation ability of CSCs by effectively suppressing the expression of several TFs in pancreatic cancer, as well as in ovarian cancer and lung cancer [193,194,195]. In another study, DNMT1 inhibitor-mediated demethylation contributes to CSC resistance to sorafenib treatment [196].
Histone modification
Histone modification involves methylation, phosphorylation, acetylation, ubiquitination, adenylation and ADP ribosylation. Since most studies focus on the histone methylation control of CSCs, we only introduce this particular modification in the section. Histone methylation refers to the methylation of lysine (Lys, K) and arginine (Arg, R), which can be recognized by histone readers and initiate expression changes. Different amounts of methylation of histones at different sites may lead to gene activation or silencing [197].
The methylation of the Lys4 and Lys36 residues of histone H3 (H3K4me and H3K36me3) often results in targeted gene activation [198]. Increasing evidence has shown that the methylation of H3K4me can maintain CSC stemness and CSC-associated therapy resistance [198]. For example, scientists have found that the self-renewal characteristics of leukemia stem cells are maintained in a hyper-H3K4me3 state [199]. Several TFs genes are reported to be methylated at H3K4me in breast cancer, which maintains the stemness of CSCs [200]. In addition, H3K4me3 increased at the promoters of several stemness TFs and markers, which account for CSC self-renewal and proliferation in CRC [201]. Regarding CSC-associated therapy resistance, researches have demonstrated that GALNT10 facilitates CSC-associated platin resistance in ovarian cancer treatment through epigenetic modification in an H3K4me-dependent methylation manner [202, 203]. In addition, Qinghai Lin et al. indicated that H3K36me3-dependent histone modification of Oct4, Sox2 and Nanog at the promoter region is critical in maintaining CSC stemness in HCC [204].
Conversely, the methylation of H3K9me2 and H3K27me3 is generally associated with gene transcription repression, which also participates in CSC stemness maintenance [197]. In glioblastoma, H3K9me2 modification of CD133 and Sox2 is important in regulating CSC self-renewal [205]. Moreover, H3K27me3 modification promotes CSC self-renewal and differentiation in both EZH2 dependent and independent ways, thereby resulting in tumorigenesis in glioblastoma, ovarian cancer and prostate cancer [206,207,208].
Tumor microenvironment (TME) control of CSCs
The regulation of the tumor microenvironment (TME) is also one of the most important mechanisms within the regulatory networks of CSCs. The TME is the immune environment that affects tumor growth and metastasis due to the continuous interaction between tumor cells, nontumor cells (such as stromal cells, immune cells, endothelial cells, etc.) and noncellular factors (such as metabolism, etc.) [209]. Among the nontumor cells of the TME, cancer-associated fibroblasts (CAFs) are the most representative stromal cells, and tumor-associated macrophages (TAMs) are the most essential immune cells that control CSCs and promote tumor progression. Apart from that, metabolism is intricately linked to the TME, which was also related to CSCs characteristics maintenance. Hence, in this section, we mainly introduce the control of CSCs by CAFs, TAMs and metabolic factors (Fig. 2).
Cancer-associated fibroblasts (CAFs)
In the TME, CAFs are the most abundant stromal components, and other cells include undifferentiated mesenchymal stem cells (MSCs), endothelial cells and pericytes [210]. CAFs maintain CSC stemness, sphere-formation ability, CSC-associated tumor metastasis and CSC-associated therapy resistance by shaping the extracellular matrix [211].
For stemness maintenance, emerging evidence has demonstrated that CAF-induced STAT3 signaling activation leads to hepatocyte growth factor (HGF) and IL-6 over-secretion to enhance CD24 expression on CSCs in HCC [212]. Tsuyada A et al. indicated that in breast cancer, CAFs secrete CCL2 to promote tumor progression by maintaining the stemness and sphere-formation ability of CSCs [213]. In addition, CAFs also play a critical role in maintaining CSC-associated tumor metastasis via CAF-derived cytokine secretion and TF expression [214, 215]. Furthermore, CSC-associated chemoresistance can be realized by the CAFs-provided supporting tumor niche enriched with IL-6 and IL-8 in clinical samples of breast and lung cancers [216]. Furthermore, CSC-associated chemoresistance can also be achieved through CAF-induced signaling pathway activation in breast cancer and CRC, such as the TGF pathway and β-catenin pathway [217,218,219].
Tumor-associated macrophages (TAMs)
Generally, tumor-infiltrating immune cells include neutrophils, lymphocytes, monocytes, macrophages and their immature precursors [220]. It has been reported that macrophages have two phenotypes, M1 and M2, which are heterogenic [221]. The M1 phenotype triggers proinflammatory factors to activate antitumor properties, whereas M2 macrophages are tumor-associated macrophages (TAMs) that secrete chemokines and ligands to achieve the same purpose. Meanwhile, TAMs can specifically promote tumor growth by maintaining CSC stemness and proliferation [222].
For example, TAMs possibly influenced the binding between hyaluronic acid (HA) and CD44, thus maintaining CSC stemness via the PI3K/4EBP1/Sox2 pathway in HNSCC [223]. In pancreatic cancer, the stemness of CSCs is closely associated with TAM-secreted interferon-stimulated gene 15 (ISG15), a protein factor with immunomodulatory properties [224]. Moreover, TAMs physically interact with CSCs from breast cancer through EphA4/ezrin and CD90/CD11b to maintain the stemness of CSCs [225]. IL-6 secreted by TAMs plays an important role in the expression of CD44 and the proliferation of CSC, while blocking the IL6 receptor reverses this process [226]. Additionally, CAFs recruit TAMs in a CXCL12/CXCR4-dependent manner, which orchestrates EMT and CSC stemness in oral squamous cell carcinoma [227].
Metabolic controls of CSCs in TME
In addition to the regulation of CSCs by CAFs and TAMs, metabolic control also plays a crucial role in maintaining CSC characteristics within the TME [228]. Glycolysis, glutaminolysis, and lipogenesis are three significant metabolic characteristics of CSCs. First and foremost, tumor cells primarily rely on glucose as their primary fuel source, especially CSCs [229]. Upregulated glycolysis has been closely associated with CSC metabolism in breast cancer and glioblastoma [230, 231]. Furthermore, CSCs often exhibit a higher demand for glutamine, making glutaminolysis an essential factor in regulating CSCs [232]. Glutamine is known to be involved in nucleotide and amino acid biosynthesis in CSCs of neuroblastoma [233]. Additionally, in the metabolic regulation of HCC and CRC, glutaminolysis has been reported to play a role in maintaining CSC characteristics through demethylation and DNA damage repair [234, 235]. Furthermore, lipogenesis is another critical metabolic characteristic of CSCs [236]. Growing evidence suggests that upregulated lipogenesis is observed in CSCs derived from pancreatic cancer [237]. Additionally, scientists have discovered that increased fatty acid oxidation is crucial for maintaining CSCs in breast cancer [238] and leukemic cells [239].
Notably, hypoxia-inducible factor (HIF) is a critical factor in the TME that can influence these three metabolic characteristics of CSCs [240]. HIF has been shown to mediate a switch from oxidative to glycolytic metabolism in CSCs under hypoxic conditions, providing protection against oxidative damage in breast cancer [241]. In HCC, hypoxia was demonstrated to enhance the self-renewal ability of CSCs in an HIF-1α-dependent and HIF-2α-dependent manner [242]. Consequently, emerging research has identified metabolic agents as potential therapeutic agents for targeting CSCs, which will be discussed in detail in the following section.
EMT control of CSCs
Epithelial-mesenchymal transformation (EMT) is a dedifferentiation process that converts polarized epithelial cells into cells with a mesenchymal phenotype, which occurs by losing adhesion with neighboring cells [243]. The transition from the epithelial phenotype to the mesenchymal phenotype bestows cells with multiple capabilities, including stem cell properties [7]. The EMT process often occurs at the early stage of embryonic development; however, it is also linked to several pathological processes, such as cancers process [244]. Moreover, loss of E-cadherin is considered as the hallmark of EMT [245]. Increasing evidence suggests that EMT-inducing transcription factors (EMT-TFs), Snail, Slug, ZEB1 and Twist, downregulate E-cadherin expression and further promote the EMT process, which results in cancer cells losing epithelial properties but acquiring mesenchymal properties. And this process could promote stem markers expression, which could be the basic that EMT process maintains CSC stemness, CSC-associated tumor metastasis and CSC-associated therapy resistance [246].
Firstly, Snail is the most significant EMT-TF that plays a role in CSC stemness maintenance and CSC-associated tumor metastasis [245]. For CSC stemness maintenance, Sendurai A. Mani et al. demonstrated that in breast cancer, Snail-induced EMT process was responsible for the generation of CSC through the loss of E-cadherin expression. In addition, the transformed CSC acquires high CD44 expression to maintain stemness characteristics [247,248,249]. Apart from that, Slug can evoke similar functions as Snail and maintain CSC stemness in cancer [245]. In glioblastoma, overexpression of Slug induces cancer cells to lose E-cadherin then undergo EMT process, which switch cancer cells to CSC with self-renewal property and maintain CSC stemness through mesenchymal transformation-induced stem markers expression [250]. In addition, ZEB1-mediated EMT is also involved in maintaining CSC stemness [245]. Accumulating evidence in pancreatic cancer has demonstrated that ZEB1 regulates the EMT process, driving the transformation of cancer cells into CSCs with self-renewal properties [251]. Finally, Twist1 primes epithelial cells for stemness characteristics and maintains CSC stemness through EMT [245]. Novel research in HNSCC has revealed that the overexpression of Twist1 is essential for suppressing E-cadherin expression in cancer cells, inducing EMT, and thereby imparting cancer epithelial cells with stem cell properties, which help maintain CSC stemness [252]. Apart from CSC stemness maintenance, Twist also plays a role in CSC-associated therapy resistance. For example, it has been observed in colon cancer that E-cadherin downregulation induced by Twist promotes EMT process, which contributes to CSC phenotype transformation and is critical for CSC-associated irinotecan resistance [253].
However, CSC stemness does not parallel the degree of EMT, which means that extreme EMT leads to cells exhibiting a fully differentiated state rather than the stem-like phenotype [254, 255].
Regulation of signaling pathways in CSCs
Evidence suggests that many signaling pathways are involved in the regulatory networks of CSCs. Instead of relying on a single regulator, these processes are governed by intricate interwoven networks of signaling pathways, as depicted in Fig. 3. The networks include the Notch, WNT/β-catenin, Sonic hedgehog (Shh), TGF-β and JAK/STAT3 signaling pathways. Therefore, this section describes how these signaling pathways contribute to the maintenance of CSC characteristics, CSC-associated tumor metastasis and CSC-associated therapy resistance.
The signaling pathways controlling CSCs. Several signaling pathways play critical roles in malignancy transformation and tumor development, particularly within the CSC regulatory network. The accompanying figure introduces the five primary signaling pathways and outlines the mechanisms of signal transmission within each pathway. Notably, in the Notch signaling pathway, the core component, NICD, undergoes three cleavage events before entering the nucleus to promote gene transcription. Shh signaling can be activated in CSCs by inhibiting SMO-mediated Gli cleavage. WNT/β-catenin signaling is facilitated by the accumulation of inactive β-catenin, regulated by GSK-3β, and requires the involvement of Axin and Dishevelled. TGF-β recruits its receptors and initiates phosphorylation through serine/threonine kinase domains, subsequently translocating phosphorylated SMAD into the nucleus. In the JAK/STAT3 signaling pathway, signals are transmitted through transphosphorylation events downstream
Notch signaling
The Notch signaling pathway plays a crucial role in regulating cancer progression across various tumor types, with the Notch Intracellular Domain (NICD) serving as one of its key effectors. Following three sequential cleavage events mediated by furin, ADAM, and γ-secretase, Notch ICD translocates into the nucleus, where it functions as a TF [256]. However, Notch signaling can play either oncogenic or suppressive functions depending on specific condition [257]. Increasing evidence has demonstrated that aberrant Notch activation in CSCs is beneficial in stemness maintenance and CSC-associated tumor metastasis [258].
For instance, in breast cancer and pancreatic cancer, Notch signaling, which is activated by Sydecan-1 and ZEB, respectively, contributed to the maintenance of CSCs stemness [259, 260]. In addition, the Notch signaling pathway is activated by HIF-1α, which could promote CSC-associated tumor metastasis in lung cancer, ovarian cancer and breast cancer [261,262,263,264]. Contrary, it has been found that CSCs could regulate Notch signaling in turn. A few studies showed that many genes expressed by CSCs could activate Notch signaling. For instance, it has been demonstrated that overexpression of HIST2H2BF and STRAP in CSCs significantly contributes to the activation of Notch signaling and the release of NICD [265, 266].
WNT/β-catenin signaling
Classical WNT/β-catenin pathway requires the binding of WNT ligands to Frizzled and LRP receptors, which rescues the inhibition of β-catenin by APC, axin and GSK-3β [267]. The WNT/β-catenin signaling pathway has been found involved in many biological processes in decades. Meanwhile, the relationship between WNT/β-catenin signaling pathway and pathological processes, especially cancer development, has also been gradually revealed [268, 269]. In the study of the underlying mechanism, scientists have discovered that the WNT/β-catenin signaling pathway could be one of the key cascades in the regulation of CSCs [270]. Notably, hyperactivated WNT/β-catenin signaling in the CSC population is responsible for maintaining CSC stemness, promoting the sphere-forming ability of CSCs, and contributing to therapy resistance associated with CSCs [271].
For example, in colon cancer, p53 and myofibroblasts are critical in activating and maintaining CSC stemness through WNT/β-catenin signaling modulation [272, 273]. Moreover, WNT/β-catenin-dependent CD44 expression is positively correlated with CSC stemness in melanoma and breast cancer [274,275,276]. Additionally, TCF7, a member of the TCF/LEF family, is a downstream target of WNT and is essential for maintaining CSC stemness in pancreatic cancer [277]. In addition, scientists have identified that the activated WNT/β-catenin signaling is critical for both sphere-formation ability and CSC-associated chemo-/radio-resistance in gastric cancer [278,279,280]. The same phenomenon is found in CRC induced by overexpression of CD45 [281].
Sonic hedgehog (Shh) signaling
The Sonic Hedgehog (Shh) signaling networks include extracellular hedgehog ligands, the transmembrane protein receptor PTCH, the transmembrane protein SMO, intermediate transduction molecules and the downstream molecule Gli [282]. In the presence of Shh, SMO inhibition by PTCH is relieved, and full-length Gli activates different target genes for further transcription processes [283]. Similar to other signaling pathways, Shh signaling is also involved in several cancers, such as colorectal, breast and lung cancers [284]. Data have shown that Shh signaling is another key pathway in regulating CSC characteristics [270].
In thyroid tumors, Shh signaling regulates CSC stemness through Gli expression-mediated Bmi1 and Sox2 expression at the posttranscriptional and transcriptional levels [285]. In addition, increasing evidence has proven that several upstream regulators of the Shh-SMO-Gli axis are important in maintaining CSC stemness. For example, in CD138+ myeloma stem cells, Shh signaling is activated by RARα2 [286] Referring to the contribution of Shh signaling to CSC-associated tumor metastasis, the study has shown that the degradation of Gli by RUNX3-mediated ubiquitination could reduce CSC-associated tumor metastasis in CRC [287].
TGF- signaling
TGF-β is involved in multiple cellular processes, such as cell proliferation, development and homeostasis [288]. Mechanically, the TGF-β/type II receptor complex recruits the type I receptor and undergoes a phosphorylation event, followed by the recruitment and phosphorylation of the SMAD family that regulates downstream gene expression [289]. At the pathological level, it is a fundamental promoter of CSC self-renewal maintenance and CSC-associated tumor metastasis [290].
Data have illustrated that the TGF-β expression level is positively correlated with the CD44+ CSC population in breast and gastric cancers, which shows powerful self-renewal ability [291,292,293]. Moreover, Kim BN et al. demonstrated that TGF-β-mediated DNA demethylation of Slug and stemness-related TFs can promote CSC self-renewal ability [294, 295]. Apart from maintaining the self-renewal of CSCs, Yeh HW et al. emphasized the function of TGF-β signaling in regulating EMT and CSC-associated tumor metastasis in both liver and lung cancers by increasing Snail expression [296]. Moreover, TGF-β signaling can regulate CSC-associated tumor metastasis at the posttranscriptional modification level. In pancreatic cancer, TGF-β/SMAD signaling regulates CSCs by inducing miR-100 and miR-125b but blocking let-7a [297].
JAK/STAT3 signaling
The JAK/STAT3 signaling pathway participates in many physiological processes, including cell proliferation, immune regulation and differentiation [298]. The tyrosine kinase-related receptors, JAK and STAT3 are three main components within the signaling pathway. Cytokines and growth factors such as interferon, interleukin, EGF and PDGF transmit signals depending on this pathway. In most human cancers, JAK/STAT3 signaling is involved in CSC stemness maintenance and CSC-associated tumor metastasis [299].
Reports have illustrated that JAK2/STAT3 signaling upregulates cyclin D2 and stemness-related TFs to persistently maintain CSC stemness in cancers [300,301,302]. Moreover, a novel report showed that the critical role of oncostatin M in CSC stemness maintenance is realized through the JAK/STAT3 signaling pathway [303, 304]. Alternatively, data have revealed that inhibition of the JAK2/STAT3 signaling pathway results in the downregulation of CSC markers in cancers, which weakens the stemness characteristics of CSCs [305,306,307]. In addition to maintaining the stemness of CSCs, JAK/STAT3 signaling also leads to CSC-associated tumor metastasis by regulating the EMT process. It has been observed that the positive feedback autocrine loop between osteopontin and the JAK/STAT3 pathway results in the EMT process, which participates in the persistent enhancement of CSC-associated tumor metastasis [308, 309].
CSCs in cancer therapy resistance
In the last few decades, multiple therapeutic strategies have been applied in the treatment of cancer. These strategies fall into three categories: surgery, chemotherapy and radiotherapy [3, 310]. In clinical practice, these treatment strategies often face challenges, with one significant obstacle being CSCs-associated therapy resistance [311]. The CSC population consistently promotes a dynamic phenotypic switch between stem and non-stem states to resist cancer therapies [312]. Several factors can be utilized by CSCs to induce cancer therapy resistance: quiescence, reactive oxygen species (ROS) and aldehyde dehydrogenase (ALDH) (Fig. 4).
CSCs in cancer therapy resistance. CSCs demonstrate greater resistance to cancer therapy compared to regular cancer cells, making them more likely to evade radiotherapy and chemotherapy and increasing the risk of tumor relapse. Several factors contribute to the development of therapy resistance in CSCs. A CSCs can enter a quiescent state when exposed to environmental stress, such as therapy-induced stress, specific molecular stress, and DNA damage stress, enabling them to acquire resistance to radiotherapy and chemotherapy. B The disruption in the balance between ROS production and ROS scavenging in CSCs leads to CSC-related resistance to radiotherapy and chemotherapy. C High ALDH expression in CSCs enhances ROS scavenging and detoxification of toxic aldehydes, leading to multidrug resistance
Quiescence-mediated radiation and chemotherapeutic resistance
Quiescence is a cellular state observed in stem cells, wherein these cells remain in the nondividing G0 phase. Stem cells in this state could escape from stress and then switch their phenotype to increase the proliferation ability after the stress is over. For instance, CSCs remain quiescent in response to hypoxia, nutritional deprivation and other stresses, but can reawaken in favorable conditions, leading to tumor relapse [313]. Since most agents target the proliferated state of cancer cells, CSCs could take advantage of the quiescent state as a mechanism of therapy resistance, resulting in tumor relapse [314].
For instance, it has been reported that a slow-cycling quiescent CSC population can evade chemotherapy in cases of melanoma and chronic myeloid leukemia (CML), potentially leading to tumor relapse [315, 316]. Other reports have shown that p38-mediated MAPK1 activation or H4K20me3 methylation-dependent formation of tighter heterochromatin can lead to CSC quiescence, impacting therapy resistance in cancers [317, 318]. Moreover, the DNA damage response usually induces cell cycle arrest and cell death. In esophageal cancer and glioma, quiescent CSCs exhibit resistance to DNA damage induced by radiotherapy or chemotherapy [319, 320]. Additionally, in bladder cancer, it has been reported that quiescent CSCs re-enter the cell division cycle in response to damage caused by gemcitabine and cisplatin [321].
ROS-mediated radiation and chemotherapeutic resistance
Reactive oxygen species (ROS) are oxygen-containing molecules characterized by their short-lived and highly reactive properties. The production of ROS is linked to cellular physiological processes, including respiration, energy consumption, and enzyme activities [322]. ROS are typically regarded as harmful metabolites that can be involved in causing DNA damage and triggering the DNA damage response [323]. Compared with cancer cells, CSCs are much more responsive to variations in oxygen levels. Moreover, studies have demonstrated how CSCs use ROS to resist radio- and chemotherapy-derived oxidative stress [324].
Data have shown that CSCs from ovarian cancer led to an increase in Nrf2 levels [325], CSCs from HCC over-activate Prx2 expression [326], and CSCs from pancreatic cancer upregulate glycolysis-induced DCLK1 expression, all of which enhance ROS scavenging and lead to chemoresistance [327]. Moreover, CSCs exhibit radio-resistance properties not only by reducing ROS levels but also by enhancing ROS defenses in breast and some brain cancers [328]. These studies indicate that disruption of the redox balance in CSCs is a possible and promising strategy in cancer treatment.
ALDH-mediated multidrug resistance
Multidrug resistance (MDR) is a special kind of chemoresistance in which cancer cells resist chemotherapeutic agents with different structures and mechanisms of action. Aldehyde dehydrogenase (ALDH) is an enzyme with functions related to aldehyde detoxification and retinoic acid synthesis, playing vital roles in cellular mechanisms. It is also considered a potential selective marker for CSCs in various cancer types [329]. Currently, it is regarded as a target for CSC-associated multi-agent resistance.
At first, the CSC-associated multidrug resistance is positively correlated with ALDH expression level [330]. For instance, in various cancers, the ALDH1+ CSC population demonstrates resistance to chemotherapy [331]. ALDH can mediate multidrug resistance through the following two mechanisms. Firstly, it impacts ROS levels. Studies have revealed that ALDH helps maintain ROS levels low enough to prevent apoptosis induced by therapeutic agents in lung cancer CSCs [332]. Secondly, it facilitates the detoxification of toxic aldehydes. In gynecologic malignancies, ALDH in CSCs detoxifies toxic aldehydes into less harmful carboxy compounds, contributing to CSC-associated therapy resistance [333].
CSC-associated targeting agents for cancer
As mentioned above, cell surface markers, multiple regulatory networks and signaling pathways have tight connection with the modulation of CSC characteristics. Targeting these mechanisms is of utmost importance to eradicate both CSCs and the bulk tumor population. In this review, CSC-associated targeting agents are classified into five subgroups: agents targeting cell surface markers of CSCs, agents targeting transcriptional factors of CSCs, agents targeting the metabolism of CSCs, agents targeting CSC-associated signaling pathways and agents targeting epigenetic modifications. The summary of agents targeting CSCs in clinical and preclinical studies is presented in Table 1.
Agents targeting cell surface markers of CSCs
As specific biomarkers have been discovered at the surface of multiple cancer cells, they have already become common therapeutic targets in cancers, especially to identify and eradicate CSCs. Among them, CD123, CD44v6 and EpCAM are three common biomarkers of CSCs that are frequently utilized as therapeutic targets. Notably, the choice of targets can vary depending on the specific expression patterns of CSC surface markers in different types of tumors (NCT03869190, NCT02674763, NCT04430530 and NCT04216524).
IMGN632 has received a breakthrough agent designation from the FDA for the treatment of plasmacytoid dendritic cell tumors, targeting CD123 [347]. Subsequently, a study in acute lymphoblastic leukemia (ALL) showed a positive therapeutic effect of IMGN632 on B-ALL, characterized by high CD123 levels [348]. Many other agents could also recognize CD123 and then eradicate CSCs, such as talacotuzumab, flotetuzumab and tagraxofusp [349,350,351]. Furthermore, bivatuzumab mertansine is a humanized anti-CD44v6 monoclonal antibody (mAb) used for HNSCC treatment, but it has been associated with severe agent-related adverse effects [352, 353]. Catumaxomab is a specific EpCAM antibody used in the treatment of various solid tumors, with a focus on targeting CSCs [354,355,356,357].
Agents targeting transcriptional factors of CSCs
Oct4, Sox2, c-Myc, KLF4, Nanog, and PBX1 are specific transcription factors (TFs) associated with CSCs, and they have been considered as potential therapeutic targets for CSCs. While it is challenging to develop agents that target TFs, effective efforts have been made in preclinical models. For instance, Ivermectin, a polycyclic lactone pesticide, has been reported as an inhibitor with inhibitory effects on CSCs by targeting Oct4, Sox2, and Nanog [335]. Increasing evidence indicates that several inhibitors such as ZF-5985KD and Peptide aptamer P42 inhibit CSCs by targeting Sox2 [336]. Yangling Li et al. and Ruosi Yao et al. demonstrated respectively that statins significantly downregulated KLF4 and D347-2761 blocked c-Myc in CSCs derived from osteosarcoma [338, 339]. Moreover, T417 represents a novel potential agent that targets PBX1, thereby inhibiting CSCs in ovarian cancer [340].
Agents targeting the metabolism of CSCs
Metabolism is intricately linked to the TME and plays a crucial role in controlling CSCs. Emerging research has identified metabolic agents as potential therapeutic agents for targeting CSCs in a specific manner. These novel therapeutic agents in numerous preclinical and clinical studies can be categorized into two main groups: those that aim to hinder the metabolic characteristics of CSCs, such as glucose inhibitors, glutamine inhibitors, and lipid inhibitors, and those designed to alleviate hypoxia, such as HIF inhibitors.
Glucose inhibitors targeting glycolysis have demonstrated effectiveness. For instance, the antidiabetic medication Metformin has been reported to attenuate glycolysis in HCC [341]. Additionally, Michael et al. demonstrated that 2-deoxy-D-glucose reduced the proliferation of CSCs in colon cancer [358]. Glutamine represents another potential metabolic target for CSCs, and several glutamine inhibitors have been developed. For example, R-HepG2 has shown effectiveness in targeting glutamine in the treatment of CSCs in HCC [234]. Furthermore, CB-839 is a glutaminase inhibitor that has demonstrated clinical therapeutic efficacy in lung cancer [359]. Lipid inhibitors, such as omeprazole and cerulenin, have also been discovered with the potential to treat CSCs [360, 361]. On the other hand, increasing evidence suggests that HIF inhibitors, such as PT2385 and 32-134D, have therapeutic effects in various cancers by targeting CSCs [346, 362].
Agents targeting CSC-associated signaling pathways
Targeting the signaling pathways involved in the regulation of CSC characteristics has become a comprehensive key technology for cancer therapy. Currently, the main related signaling pathways include the Notch, WNT/β-catenin, Shh, TGF-β and JAK/STAT3 signaling pathways. These pathways not only act independently but also interact with one another to maintain CSC characteristics.
Notch signaling pathway inhibitors
As mentioned before, the Notch signaling pathway is of the utmost importance in maintaining CSC characteristics. The tumor-promoting function of Notch signaling has been shown in glioma, colon cancer, breast cancer, gastric cancer, and myeloma [363]. Moreover, breakthroughs have been made in Notch-targeted cancer therapies through three major classes of Notch pathway inhibitors, including γ-secretase inhibitors, Notch receptor antibodies, and Notch ligand antibodies.
For instance, RO4929097 is a γ-secretase inhibitor with a high affinity for Notch signaling [364]. At present, over 30 clinical trials have used RO4929097 as an antitumor agent in various solid tumors (NCT01131234), sarcoma (NCT01154452) and melanoma (NCT01196416). In addition, MK-0752 shows well-tolerated antitumor activity against CSCs in breast cancer by inhibiting γ-secretase (NCT00645333) [365]. Additional selective γ-secretase inhibitors, including LY3039478 (NCT02836600), AL101 (NCT03691207), and BMS-906024 (NCT01292655), are currently undergoing clinical trials. Blocking Notch signaling through the inhibition of Notch receptors and ligands represents another strategy. Brontictuzumab is a Notch1 mAb, and its notable clinical benefits in Notch1-mutated adenoid cystic carcinoma (ACC) patients have been documented [366]. ABL001, on the other hand, targets DLL4, a prominent Notch ligand, thereby impeding angiogenesis in gastric cancer and colon cancer, while also reducing the population of CSCs [367, 368].
WNT/β-catenin signaling pathway inhibitors
Activation of WNT/β-catenin signaling in CSCs contributes to maintaining the characteristics of CSCs, promoting tumor processes and poor patient prognosis. At present, agents targeting the β-catenin and frizzled molecules of the WNT/β-catenin signaling pathway have been under clinical trials.
CWP232291 is a novel small molecule β-catenin inhibitor that aims to suppress β-catenin and potentially achieve clinical remission in prostate cancer [369]. Vantictumab and ipafricept have shown effectiveness in breast, ovarian, and pancreatic cancers by targeting and blocking frizzled receptors [370]. Additionally, other WNT/β-catenin signaling inhibitors have participated in various ongoing clinical trials, including PRI-724 (NCT01606579), OMP-54F28 (NCT01608867 and NCT02092363), ETC-1922159 (NCT02521844) and LGK974 (NCT01351103).
Shh signaling pathway inhibitors
Aberrant Shh signaling has been proven in various types of cancer. SMO is the most important component of the Shh signaling pathway that mediates TF transfer. Consequently, targeting SMO has become a primary strategy for inhibiting Shh signaling. It’s worth noting that SMO inhibitors exhibit greater effectiveness in treating basal cell carcinoma (BCC) and medulloblastoma compared to other cancer types [371].
Vismodegib is an FDA-approved SMO inhibitor for the treatment of advanced BCC. An American clinical trial indicated that 73% of BCC patients enrolled in the clinical trial had tumor shrinkage after vismodegib treatment (NCT00833417) [372]. However, the therapeutic effect of vismodegib was not satisfactory in other solid tumors (NCT01064622, NCT01209143). Increasing evidence has demonstrated that glasdegib contributes to a good therapeutic effect on AML by inhibiting Shh signaling (NCT01546038) [373, 374]. Other Shh inhibitors, such as BMS-833923, LDE225 and LEQ506, are also under investigation in clinical trials for various cancer treatments, and the effect remains to be confirmed.
Other signaling pathway inhibitors
Activation of the TGF-β signaling pathway and JAK/STAT3 signaling pathway has also been found in CSCs. TGF-β is a tumor promoter; therefore, blocking TGF-β has been a novel strategy in cancer therapy [375]. Vactosertib, a well-tolerated small molecule TGF-β inhibitor, has been tested in clinical trials of multiple cancer types (NCT03143985, NCT02160106). In addition, fresolimumab, galunisertib and AVID200 are other selective TGF-β inhibitors designed for various cancers [376]. In the JAK/STAT3 signaling pathway, AZD4205 and ruxolitinib have been discovered to be effective in the treatment of solid tumors and lymphoma [377,378,379]. Other agents related to CSC-associated signaling pathways in clinical trials are listed in Table 1.
Agents targeting epigenetic modifications
Epigenetic modification has garnered significant interest as a crucial component of the regulatory networks governing CSCs. Currently, epigenetic agents play vital roles in combatting CSC characteristics and targeting the overall tumor population. Two extensively researched epigenetic agents, DNMT inhibitors and HDAC inhibitors, are subjects of ongoing clinical cancer trials. In this section, we review agents that target epigenetic modifications, with a particular focus on DNMT and HDAC inhibitors, across various cancer types.
DNMTs are essential enzymes involved in DNA methylation, which in turn modulates CSC stemness. Decitabine and azacitidine are two major DNMT inhibitors used for cancer treatment. Decitabine is an FDA-approved DMNT inhibitor that has been applied in myelodysplastic syndrome, AML and solid tumors [380,381,382]. Azacitidine is another extensively studied DNMT inhibitor in clinical settings. Increasing evidence indicates its good tolerability and efficacy in AML, particularly among older patients [4, 383]. Furthermore, SGI-110, disulfiram, and Aza-TdC are additional DNMT inhibitors currently undergoing clinical trials for various cancer types.
HDACs remove acetyl groups, resulting in tighter binding between DNA and histones. Consequently, HDAC inhibitors have the potential to induce cell apoptosis [384]. To date, it has been found that givinostat can function in the treatment of Hodgkin’s lymphoma [385]. Vorinostat and romidepsin are two HDAC inhibitors specifically used for the treatment of cutaneous T-cell lymphoma (NCT01728805, NCT0148296). Moreover, a phase III clinical trial launched by Dr. Kim showed that a novel agent, mogamulizumab, significantly prolonged the progression-free survival of cutaneous T-cell lymphoma patients [386]. Apart from these agents, other HDAC inhibitors, such as belinostat, panobinostat, and chidamide, are also important in antitumor and anti-CSC therapies [387].
Moreover, more agents targeting CSC-associated regulatory networks and their clinical status can be found in Table 1.
Conclusions and perspectives
CSCs represent a subpopulation of stem cells characterized by their self-renewal capabilities and differentiation potential, contributing significantly to cell proliferation, metastasis, and tumor growth. The regulatory networks governing CSCs encompass transcriptional control, post-transcriptional control, epigenetic modifications, control by the tumor microenvironment (TME), and regulation by the epithelial-mesenchymal transition (EMT) process. This review also explores the roles of Notch, WNT/β-catenin, Sonic hedgehog (Shh), TGF-β, and JAK-STAT3 signaling pathways in CSC regulation. Additionally, several factors employed by CSCs are closely associated with therapy resistance. Promisingly, a variety of CSC-targeted therapies have been developed and are currently undergoing clinical trials, offering a hopeful outlook for the future of cancer treatment.
However, effectively eradicating CSCs faces several challenges. Firstly, the complete identification of surface markers specific to CSCs remains elusive, as CSCs can adapt by altering their surface markers to evade immune responses. Secondly, most current studies have isolated CSCs from the tumor microenvironment, which limits our understanding of how the tumor microenvironment influences CSCs, a crucial aspect of actual tumor development. Thirdly, irrespective of transcription factors, signaling pathways, or RNA and epigenetic modifications, there are regulatory networks that control both CSCs and normal cell physiological activities, posing limitations on targeted cancer therapies. Lastly, there is currently no effective therapy available for targeting the quiescent state of CSCs.
Availability of data and materials
All clinical trials mentioned in this current review are available in ClinicalTrials.gov (https://clinicaltrials.gov/); The figures in this article were created with BioRender.com.
Abbreviations
- ACC:
-
Adenoid cystic carcinoma
- ADAR:
-
Adenosine deaminase
- AGO2:
-
Argonaute2
- ALDH:
-
Aldehyde dehydrogenase
- AML:
-
Acute myeloid leukemia
- ASC:
-
Adult stem cell
- A-to-I:
-
Adenosine-to-inosine
- AZIN1:
-
Antizyme inhibitor 1
- BCC:
-
Basal cell carcinoma
- CAF:
-
Cancer-associated fibroblasts
- CDK13:
-
Cyclin-dependent serine/threonine protein kinase 13
- CML:
-
Chronic myeloid leukemia
- CSC:
-
Cancer stem cell
- EMT:
-
Epithelial-Mesenchymal Transformation
- EMT-TF:
-
EMT-inducing transcription factor
- 5-FU:
-
5-Fluorouracil
- GRIA2:
-
Glutamate receptor subunit B
- HA:
-
Hyaluronic acid
- HCC:
-
Hepatocellular carcinoma
- HGF:
-
Hepatocyte growth factor
- HIF:
-
Hypoxia-inducible factor
- HNSCC:
-
Head and neck squamous cell carcinoma
- ISG15:
-
Interferon-stimulated gene 15
- LGR5:
-
Leucine-rich repeat containing G protein-coupled receptor
- LncRNA:
-
Long noncoding RNA
- m6A:
-
N6-methyladenosine
- mAb:
-
Monoclonal antibody
- m5C:
-
5-Methylcytosine
- MDR:
-
Multidrug resistance
- MiRNA:
-
MicroRNA
- METTLE:
-
M6A methyltransferase
- NICD:
-
Notch ICD
- MSC:
-
Mesenchymal stem cell
- NSCLC:
-
Non-small cell lung cancer
- PODXL:
-
Podocalyxin-like
- QKI-5:
-
Quaking gene 5
- RBP:
-
RNA-binding protein
- ROS:
-
Reactive oxygen species
- Shh:
-
Sonic hedgehog
- SOCS2:
-
Suppressor of cytokine signaling 2
- SOD2:
-
Superoxide dismutase
- Sox2:
-
Sex determining region Y-Box-2
- T-ALL:
-
T-cell acute lymphoblastic leukemia
- TAM:
-
Tumor-associated macrophage
- TME:
-
Tumor Microenvironment
- TNBC:
-
Triple-negative breast cancer
- TF:
-
Transcription Factor
- YAP1:
-
Yes-associated protein 1
References
Nassar D, Blanpain C. Cancer stem cells: basic concepts and therapeutic implications. Annu Rev Pathol. 2016;11:47–76.
Bonnet D, Dick JE. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med. 1997;3(7):730–7.
Baumann M, Krause M, Hill R. Exploring the role of cancer stem cells in radioresistance. Nat Rev Cancer. 2008;8:545–54.
Toh TB, Lim JJ, Chow EKH. Epigenetics in cancer stem cells. Mol Cancer. 2017;16:29.
Singh SK, Clarke ID, Terasaki M, Bonn VE, Hawkins C, Squire J, Dirks PB. Identification of a cancer stem cell in human brain tumors. Cancer Res. 2003;63.
Li JJ, Shen MM. Prostate stem cells and cancer stem cells. Cold Spring Harb Perspect Med. 2019;9(6):a030395.
Dittmer J. Breast cancer stem cells: features, key drivers and treatment options. Semin Cancer Biol. 2018;53:59–74.
Yoganandarajah V, Patel J, van Schaijik B, Bockett N, Brasch HD, Paterson E, et al. Identification of cancer stem cell subpopulations in head and neck metastatic malignant melanoma. Cells. 2020;9(2):324.
Heng WS, Gosens R, Kruyt FAE. Lung cancer stem cells: origin, features, maintenance mechanisms and therapeutic targeting. Biochem Pharmacol. 2019;160:121–33.
Ma S, Chan KW, Hu L, Lee TKW, Wo JYH, Ng IOL, et al. Identification and characterization of tumorigenic liver cancer stem/progenitor cells. Gastroenterology. 2007;132(7):2542–56.
Wilson RJ, Thomas CD, Fox R, Roy DB, Kunin WE. Spatial patterns in species distributions reveal biodiversity change. Nature. 2004;432(7015):393–6.
Prasetyanti PR, Medema JP. Intra-tumor heterogeneity from a cancer stem cell perspective. Mol Cancer. 2017;16(1):41.
Trumpp A, Haas S. Cancer stem cells: the adventurous journey from hematopoietic to leukemic stem cells. Cell. 2022;185:1266–70.
Visvader JE, Lindeman GJ. Cancer stem cells in solid tumours: accumulating evidence and unresolved questions. Nat Rev Cancer. 2008;8:755–68.
Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. P Natl A Sci India B. 2003;100:3983–8.
Vermeulen L, Todaro M, de Sousa Mello F, Sprick MR, Kemper K, Perez Alea M, et al. Singlecell cloning of colon cancer stem cells reveals a multi-lineage differentiation capacity. P Natl A Sci India B. 2008;105:13427–32.
Hermann PC, Huber SL, Herrler T, Aicher A, Ellwart JW, Guba M, et al. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell. 2007;1(3):313–23.
Choi SA, Lee JY, Phi JH, Wang KC, Park CK, Park SH, et al. Identification of brain tumour initiating cells using the stem cell marker aldehyde dehydrogenase. Eur J Cancer. 2014;50(1):137–49.
Eun K, Ham SW, Kim H. Cancer stem cell heterogeneity: origin and new perspectives on CSC targeting. BMB Rep. 2017;50:117–25.
Barker N, Ridgway RA, Van Es JH, Van De Wetering M, Begthel H, Van Den Born M, et al. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature. 2009;457(7229):608–11.
Hausser J, Alon U. Tumour heterogeneity and the evolutionary trade-offs of cancer. Nat Rev Cancer. 2020;20:247–57.
Visvader JE. Cells of origin in cancer. Nature. 2011;469:314–22.
Melo FDSE, Vermeulen L, Fessler E, Medema JP. Cancer heterogeneity - a multifaceted view. EMBO Rep. 2013;14:686–95.
Sottoriva A, Verhoeff JJC, Borovski T, McWeeney SK, Naumov L, Medema JP, et al. Cancer stem cell tumor model reveals invasive morphology and increased phenotypical heterogeneity. Cancer Res. 2010;70(1):46–56.
Atashzar MR, Baharlou R, Karami J, Abdollahi H, Rezaei R, Pourramezan F, et al. Cancer stem cells: a review from origin to therapeutic implications. J Cell Physiol. 2020;235:790–803.
Marjanovic ND, Weinberg RA, Chaffer CL. Cell plasticity and heterogeneity in cancer. Clin Chem. 2013;59:168–79.
Zhang K, Guo Y, Wang X, Zhao H, Ji Z, Cheng C, et al. WNT/β-catenin directs self-renewal symmetric cell division of hTERThigh prostate cancer stem cells. Cancer Res. 2017;77(9):2534–47.
Ricci-Vitiani L, Pallini R, Biffoni M, Todaro M, Invernici G, Cenci T, et al. Tumour vascularization via endothelial differentiation of glioblastoma stem-like cells. Nature. 2010;468(7325):824–30.
Ricci-Vitiani L, Lombardi DG, Pilozzi E, Biffoni M, Todaro M, Peschle C, et al. Identification and expansion of human colon-cancer-initiating cells. Nature. 2007;445(7123):111–5.
Bigoni-Ordóñez GD, Ortiz-Sánchez E, Rosendo-Chalma P, Valencia-González HA, Aceves C, García-Carrancá A. Molecular iodine inhibits the expression of stemness markers on cancer stem-like cells of established cell lines derived from cervical cancer. BMC Cancer. 2018;18:1–12.
Toledo-Guzmán ME, Bigoni-Ordóñez GD, Hernández MI, Ortiz-Sánchez E. Cancer stem cell impact on clinical oncology. World J Stem Cells. 2018;10:183–95.
Krebsbach PH, Villa-Diaz LG. The role of integrin α6 (CD49f) in stem cells: more than a conserved biomarker. Stem Cells Dev. 2017;26(15):1090–9.
Lin SA, Barker N. Gastrointestinal stem cells in self-renewal and cancer. J Gastroenterol. 2011;46:1039–55.
Ho TC, LaMere M, Stevens BM, Ashton JM, Myers JR, O’Dwyer KM, et al. Evolution of acute myelogenous leukemia stem cell properties after treatment and progression. Blood. 2016;128(13):1671–8.
Auvergne R, Wu C, Connell A, Au S, Cornwell A, Osipovitch M, et al. PAR1 inhibition suppresses the self-renewal and growth of A2B5-defined glioma progenitor cells and their derived gliomas in vivo. Oncogene. 2016;35(29):3817–28.
Bao S, Wu Q, Li Z, Sathornsumetee S, Wang H, McLendon RE, et al. Targeting cancer stem cells through L1CAM suppresses glioma growth. Cancer Res. 2008;68(15):6043–8.
Li XF, Chen C, Xiang DM, Qu L, Sun W, Lu XY, et al. Chronic inflammation-elicited liver progenitor cell conversion to liver cancer stem cell with clinical significance. Hepatology. 2017;66(6):1934–51.
Bradner JE, Hnisz D, Young RA. Transcriptional addiction in cancer. Cell. 2017;168:629–43.
Labbé DP, Brown M. Transcriptional regulation in prostate cancer. Cold Spring Harb Perspect Med. 2018;8(11):a030437.
Cerezo M, Guemiri R, Druillennec S, Girault I, Malka-Mahieu H, Shen S, et al. Translational control of tumor immune escape via the eIF4F–STAT1–PD-L1 axis in melanoma. Nat Med. 2018;24(12):1877–86.
Boregowda RK, Medina DJ, Markert E, Bryan MA, Chen W, Chen S, et al. The transcription factor RUNX2 regulates receptor tyrosine kinase expression in melanoma. Oncotarget. 2016;7(20):29689–707.
Chen CH, Huang H, Ward CM, Su JT, Schaeffer LV, Guo M, et al. Modeling the initiation and progression of human acute leukemia in mice. Science (1979). 2007;316(5824):597–600.
Kuo YH, Landrette SF, Heilman SA, Perrat PN, Garrett L, Liu PP, et al. Cbfβ-SMMHC induces distinct abnormal myeloid progenitors able to develop acute myeloid leukemia. Cancer Cell. 2006;9(1):57–68.
Bushweller JH. Targeting transcription factors in cancer — from undruggable to reality. Nat Rev Cancer. 2019;19:611–24.
Okita K, Ichisaka T, Yamanaka S. Generation of germline-competent induced pluripotent stem cells. Nature. 2007;448(7151):313–7.
Van Schaijik B, Davis PF, Wickremesekera AC, Tan ST, Itinteang T. Subcellular localisation of the stem cell markers OCT4, SOX2, NANOG, KLF4 and c-MYC in cancer: a review. J Clin Pathol. 2018;71:88–91.
Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126(4):663–76.
Baillie R, Itinteang T, Yu HH, Brasch HD, Davis PF, Tan ST. Cancer stem cells in moderately differentiated oral tongue squamous cell carcinoma. J Clin Pathol. 2016;69:742–4.
Guo Y, Liu S, Wang P, Zhao S, Wang F, Bing L, et al. Expression profile of embryonic stem cell-associated genes Oct4, Sox2 and Nanog in human gliomas. Histopathology. 2011;59(4):763–75.
Wen J, Park JY, Park KH, Chung HW, Bang S, Park SW, et al. Oct4 and Nanog expression is associated with early stages of pancreatic carcinogenesis. Pancreas. 2010;39:622–6.
Jen J, Tang YA, Lu YH, Lin CC, Lai WW, Wang YC. Oct4 transcriptionally regulates the expression of long non-coding RNAs NEAT1 and MALAT1 to promote lung cancer progression. Mol Cancer. 2017;16(1):104.
Lu CS, Shiau AL, Su BH, Hsu TS, Wang CT, Su YC, et al. Oct4 promotes M2 macrophage polarization through upregulation of macrophage colony-stimulating factor in lung cancer. J Hematol Oncol. 2020;13(1):1–6.
Liu L, Zhu H, Liao Y, Wu W, Liu L, Liu L, et al. Inhibition of Wnt/β-catenin pathway reverses multi-drug resistance and EMT in Oct4+/Nanog+ NSCLC cells. Biomed Pharmacother. 2020;127:110225.
Yin X, Zhang BH, Zheng SS, Gao DM, Qiu SJ, Wu WZ, et al. Coexpression of gene Oct4 and Nanog initiates stem cell characteristics in hepatocellular carcinoma and promotes epithelial-mesenchymal transition through activation of Stat3/Snail signaling. J Hematol Oncol. 2015;8(1):23.
Chai S, Ng KY, Tong M, Lau EY, Lee TK, Wah Chan K, et al. Octamer 4/microRNA-1246 signaling axis drives Wnt/bcatenin activation in liver cancer stem cells. Hepatology. 2016;64(6):2062–76.
Kumar SM, Liu S, Lu H, Zhang H, Zhang PJ, Gimotty PA, et al. Acquired cancer stem cell phenotypes through Oct4-mediated dedifferentiation. Oncogene. 2012;31(47):4898–911.
Shao-Wen L, Wu XL, Dong CL, Xie XY, Wu JF, Zhang X. The differential expression of OCT4 isoforms in cervical carcinoma. PLoS One. 2015;10(3):e0118033.
Pesce M, Schöler HR. Oct-4: gatekeeper in the beginnings of mammalian development. Stem Cells. 2001;19(4):271–8. Available from: www.StemCells.com.
Lu Y, Zhu H, Shan H, Lu J, Chang X, Li X, et al. Knockdown of Oct4 and Nanog expression inhibits the stemness of pancreatic cancer cells. Cancer Lett. 2013;340(1):113–23.
Rodriguez-Pinilla SM, Sarrio D, Moreno-Bueno G, Rodriguez-Gil Y, Martinez MA, Hernandez L, et al. Sox2: a possible driver of the basal-like phenotype in sporadic breast cancer. Mod Pathol. 2007;20(4):474–81.
Novak D, Hüser L, Elton JJ, Umansky V, Altevogt P, Utikal J. SOX2 in development and cancer biology. Semin Cancer Biol. 2020;67:74–82.
Zhang S, Xiong X, Sun Y. Functional characterization of SOX2 as an anticancer target. Signal Transduct Target Ther. 2020;5(1):135.
Leis O, Eguiara A, Lopez-Arribillaga E, Alberdi MJ, Hernandez-Garcia S, Elorriaga K, et al. Sox2 expression in breast tumours and activation in breast cancer stem cells. Oncogene. 2012;31(11):1354–65.
Bass AJ, Watanabe H, Mermel CH, Yu S, Perner S, Verhaak RG, et al. SOX2 is an amplified lineage-survival oncogene in lung and esophageal squamous cell carcinomas. Nat Genet. 2009;41(11):1238–42.
Berezovsky AD, Poisson LM, Cherba D, Webb CP, Transou AD, Lemke NW, et al. Sox2 promotes malignancy in glioblastoma by regulating plasticity and astrocytic differentiation. Neoplasia (United States). 2014;16(3):193-206.e25.
Boumahdi S, Driessens G, Lapouge G, Rorive S, Nassar D, Le Mercier M, et al. SOX2 controls tumour initiation and cancer stem-cell functions in squamous-cell carcinoma. Nature. 2014;511(7508):246–50.
Barone C, Buccarelli M, Alessandrini F, Pagin M, Rigoldi L, Sambruni I, et al. Sox2-dependent maintenance of mouse oligodendroglioma involves the Sox2-mediated downregulation of Cdkn2b, Ebf1, Zfp423, and Hey2. Glia. 2021;69(3):579–93.
Battista S, Remboutsika E, Fleming A, Sampron nicolassampron N, Matheu andermatheu A, Garros-Regulez L, et al. Targeting SOX2 as a therapeutic strategy in glioblastoma. Glioblastoma Front Oncol. 2016;6:222.
Tuhin Das 1 RRN 2 3, RG 1 4, SP 1 2 3 4, MH 1 4, JB 1, SSM 2 4 5, SM 6 4 5. Actinomycin D down-regulates SOX2 expression and induces death in breast cancer stem cells. Anticancer Res. 2017:1655–63.
Piva M, Domenici G, Iriondo O, Rábano M, Simões BM, Comaills V, et al. Sox2 promotes tamoxifen resistance in breast cancer cells. EMBO Mol Med. 2014;6(1):66–79.
Stine ZE, Walton ZE, Altman BJ, Hsieh AL, Dang CV. MYC, metabolism, and cancer. Cancer Discov. 2015;5:1024–39.
Yoshida GJ. Emerging roles of Myc in stem cell biology and novel tumor therapies. J Exp Clin Cancer Res. 2018;37(1):173.
He Q, Liu Z, Zhao T, Zhao L, Zhou X, Wang A. Bmi1 drives stem-like properties and is associated with migration, invasion, and poor prognosis in tongue squamous cell carcinoma. Int J Biol Sci. 2015;11(1):1–10.
Liu M, Casimiro MC, Wang C, Shirley LA, Jiao X, Katiyar S, Ju X, Li Z, Yu Z, Zhou J, Johnson M, Fortina P, Hyslop T, Windle JJ, Pestell RG. p21CIP1 attenuates Ras- and c-Myc-dependent breast tumor epithelial mesenchymal transition and cancer stem cell-like gene expression in vivo. Proc Natl Acad Sci U S A. 2009;106(45):19035–9.
Yang J, Wu SP, Wang WJ, Jin ZR, Miao XB, Wu Y, et al. A novel miR-200c/c-myc negative regulatory feedback loop is essential to the EMT process, CSC biology and drug sensitivity in nasopharyngeal cancer. Exp Cell Res. 2020;391(2):111817.
Zhou JN, Zhang B, Wang HY, Wang DX, Zhang MM, Zhang M, et al. A functional screening identifies a new organic selenium compound targeting cancer stem cells: role of c-Myc transcription activity inhibition in liver cancer. Adv Sci. 2022;9(22):e2201166.
Ghaleb AM, Elkarim EA, Bialkowska AB, Yang VW. KLF4 suppresses tumor formation in genetic and pharmacological mouse models of colonic tumorigenesis. Mol Cancer Res. 2016;14(4):385–96.
Gu Cho Y, Song JH, Chang J, Kim S, Woo N, Yoo NJ, et al. Genetic and epigenetic analysis of the KLF4 gene in gastric cancer. All rights reserved. J Compilation C. 2007;115:802–10.
Shen Y, Chen TJ, Lacorazza HD. Novel tumor-suppressor function of KLF4 in pediatric T-cell acute lymphoblastic leukemia. Exp Hematol. 2017;53:16–25.
Yu T, Chen X, Zhang W, Liu J, Avdiushko R, Napier DL, et al. KLF4 regulates adult lung tumor-initiating cells and represses K-Ras-mediated lung cancer. Cell Death Differ. 2016;23(2):207–15.
Tang H, Zhu H, Wang X, Hua L, Li J, Xie Q, et al. KLF4 is a tumor suppressor in anaplastic meningioma stem-like cells and human meningiomas. J Mol Cell Biol. 2017;9:315–24.
Ohnishi S, Ohnami S, Laub F, Aoki K, Suzuki K, Kanai Y, et al. Downregulation and growth inhibitory effect of epithelial-type Krüppel-like transcription factor KLF4, but not KLF5, in bladder cancer. Biochem Biophys Res Commun. 2003;308(2):251–6.
Qi XT, Li YL, Zhang YQ, Xu T, Lu B, Fang L, et al. KLF4 functions as an oncogene in promoting cancer stem cell-like characteristics in osteosarcoma cells. Acta Pharmacol Sin. 2019;40(4):546–55.
Ganguly K, Krishn SR, Rachagani S, Jahan R, Shah A, Nallasamy P, et al. Secretory mucin 5AC promotes neoplastic progression by augmenting KLF4-mediated pancreatic cancer cell stemness. Cancer Res. 2021;81(1):91–102.
Kress TR, Sabò A, Amati B. MYC: connecting selective transcriptional control to global RNA production. Nature Publishing Group; 2015.
Murgai M, Ju W, Eason M, Kline J, Beury DW, Kaczanowska S, et al. KLF4-dependent perivascular cell plasticity mediates pre-metastatic niche formation and metastasis. Nat Med. 2017;23(10):1176–90.
Zou H, Chen H, Zhou Z, Wan Y, Liu Z. ATXN3 promotes breast cancer metastasis by deubiquitinating KLF4. Cancer Lett. 2019;467:19–28.
Okuda H, Xing F, Pandey PR, Sharma S, Watabe M, Pai SK, et al. miR-7 suppresses brain metastasis of breast cancer stem-like cells by modulating KLF4. Cancer Res. 2013;73:1434–44.
Chambers I, Colby D, Robertson M, Nichols J, Lee S, Tweedie S, et al. Functional expression cloning of Nanog, a pluripotency sustaining factor in embryonic stem cells. Cell. 2003;113:643–55.
Huang W, Zhong Z, Luo C, Xiao Y, Li L, Zhang X, et al. The miR-26a/AP-2α/Nanog signaling axis mediates stem cell self-renewal and temozolomide resistance in glioma. Theranostics. 2019;9(19):5497–516.
Zhang T, Sun H, Liu R, Cao W, Zhang T, Li E, et al. Nanog mediates tobacco smoke-induced enhancement of renal cancer stem cell properties. Environ Toxicol. 2020;35(11):1274–83.
Mahalaxmi I, Devi SM, Kaavya J, Arul N, Balachandar V, Santhy KS. New insight into NANOG: a novel therapeutic target for ovarian cancer (OC). Eur J Pharmacol. 2019;852:51–7.
Cao J, Zhao M, Liu J, Zhang X, Pei Y, Wang J, et al. RACK1 promotes self-renewal and chemoresistance of cancer stem cells in human hepatocellular carcinoma through stabilizing nanog. Theranostics. 2019;9(3):811–28.
Zhang C, Samanta D, Lu H, Bullen JW, Zhang H, Chen I, et al. Hypoxia induces the breast cancer stem cell phenotype by HIF-dependent and ALKBH5-mediated m6A-demethylation of NANOG mRNA. Proc Natl Acad Sci U S A. 2016;113(14):E2047–56.
Jia Z, Zhang Y, Yan A, Wang M, Han Q, Wang K, et al. 1,25-dihydroxyvitamin D3 signaling-induced decreases in IRX4 inhibits NANOG-mediated cancer stem-like properties and gefitinib resistance in NSCLC cells. Cell Death Dis. 2020;11(8):670.
Shepherd MS, Li J, Wilson NK, Oedekoven CA, Li J, Belmonte M, et al. Single-cell approaches identify the molecular network driving malignant hematopoietic stem cell self-renewal. Blood. 2018;132(8):791–803.
Jung J-G, Shih I-M, Park JT, Gerry E, Kim TH, Ayhan A, et al. Ovarian cancer chemoresistance relies on the stem cell reprogramming factor PBX1. Cancer Res. 2016;76:6351–61.
Shimabe M, Goyama S, Watanabe-Okochi N, Yoshimi A, Ichikawa M, Imai Y, et al. Pbx1 is a downstream target of Evi-1 in hematopoietic stem/progenitors and leukemic cells. Oncogene. 2009;28(49):4364–74.
Zhang H, Wan Y, Wang H, Cai J, Yu J, Hu S, et al. Prognostic factors of childhood acute lymphoblastic leukemia with TCF3::PBX1 in CCCG-ALL-2015: a multicenter study. Cancer. 2023;129(11):1691–703.
Grifone R, Shao M, Saquet A, Shi DL. RNA-binding protein Rbm24 as a multifaceted post-transcriptional regulator of embryonic lineage differentiation and cellular homeostasis. Cells. 2020;9(8):1891.
Herbert SP, Stainier DYR. Molecular control of endothelial cell behaviour during blood vessel morphogenesis. Nat Rev Mol Cell Biol. 2011;12:551–64.
Haruehanroengra P, Zheng YY, Zhou Y, Huang Y, Sheng J. RNA modifications and cancer. RNA Biol. 2020;17:1560–75.
Gehring NH, Wahle E, Fischer U. Deciphering the mRNP code: RNA-bound determinants of post-transcriptional gene regulation. Trends Biochem Sci. 2017;42:369–82.
Pereira B, Billaud M, Almeida R. RNA-binding proteins in cancer: old players and new actors. Trends Cancer. 2017;3:506–28.
Neelamraju Y, Gonzalez-Perez A, Bhat-Nakshatri P, Nakshatri H, Janga SC. Mutational landscape of RNA-binding proteins in human cancers. RNA Biol. 2018;15(1):115–29.
Mukohyama J, Shimono Y, Minami H, Kakeji Y, Suzuki A. Roles of microRNAs and RNA-binding proteins in the regulation of colorectal cancer stem cells. Cancers. 2017;9(10):143.
Okano H, Imai T, Okabe M. Musashi a translational regulator of cell fate. J Cell Sci. 2002;115(7):1355–9.
Chen HY, Wang ML, Laurent B, Hsu DCH, Chen MT, Lin LT, et al. Musashi-1 promotes stress-induced tumor progression through recruitment of AGO2. Theranostics. 2020;10(1):201–17.
Frau C, Jamard C, Delpouve G, Guardia GDA, Machon C, Pilati C, et al. Deciphering the role of intestinal crypt cell populations in resistance to chemotherapy. Cancer Res. 2021;81(10):2730–44.
Chiou GY, Yang TW, Huang CC, Tang CY, Yen JY, Tsai MC, et al. Musashi-1 promotes a cancer stem cell lineage and chemoresistance in colorectal cancer cells. Sci Rep. 2017;7(1):2172.
Lin JC, Tsai JT, Chao TY, Ma HI, Chien CS, Liu WH. MSI1 associates glioblastoma radioresistance via homologous recombination repair, tumor invasion and cancer stem-like cell properties. Radiother Oncol. 2018;129(2):352–63.
Kharas MG, Lengner CJ. Stem cells, cancer, and MUSASHI in blood and guts. Trends Cancer. 2017;3:347–56.
Nguyen DTT, Lu Y, Chu KL, Yang X, Park SM, Choo ZN, et al. HyperTRIBE uncovers increased MUSASHI-2 RNA binding activity and differential regulation in leukemic stem cells. Nat Commun. 2020;11(1):2026.
Kharas MG, Lengner CJ, Al-Shahrour F, Bullinger L, Ball B, Zaidi S, et al. Musashi-2 regulates normal hematopoiesis and promotes aggressive myeloid leukemia. Nat Med. 2010;16(8):903–8.
Fang T, Lv H, Wu F, Wang C, Li T, Lv G, et al. Musashi 2 contributes to the stemness and chemoresistance of liver cancer stem cells via LIN28A activation. Cancer Lett. 2017;384:50–9.
Löblein MT, Falke I, Eich HT, Greve B, Götte M, Troschel FM. Dual knockdown of musashi rna-binding proteins msi-1 and msi-2 attenuates putative cancer stem cell characteristics and therapy resistance in ovarian cancer cells. Int J Mol Sci. 2021;22(21):11502.
Shyh-Chang N, Daley GQ. Lin28: primal regulator of growth and metabolism in stem cells. Cell Stem Cell. 2013;12:395–406.
Mayr F, Heinemann U. Mechanisms of Lin28-mediated miRNA and mRNA regulation–a structural and functional perspective. Int J Mol Sci. 2013;14:16532–53.
Peng S, Maihle NJ, Huang Y. Pluripotency factors Lin28 and Oct4 identify a sub-population of stem cell-like cells in ovarian cancer. Oncogene. 2010;29(14):2153–9.
Qiu C, Ma Y, Wang J, Peng S, Huang Y. Lin28-mediated post-transcriptional regulation of Oct4 expression in human embryonic stem cells. Nucleic Acids Res. 2009;38(4):1240–8.
Hong AW, Meng Z, Guan KL. The Hippo pathway in intestinal regeneration and disease. Nat Rev Gastroenterol Hepatol. 2016;13:324–37.
Zou H, Luo J, Guo Y, Liu Y, Wang Y, Deng L, et al. RNA-binding protein complex LIN28/MSI2 enhances cancer stem cell-like properties by modulating Hippo-YAP1 signaling and independently of Let-7. Oncogene. 2022;41(11):1657–72.
Liu Y, Li H, Feng J, Cui X, Huang W, Li Y, et al. Lin28 induces epithelial-to-mesenchymal transition and stemness via downregulation of let-7a in breast cancer cells. PLoS One. 2013;8(12):e83083.
He L, Li H, Wu A, Peng Y, Shu G, Yin G. Functions of N6-methyladenosine and its role in cancer. Mol Cancer. 2019;18(1):176.
Zhang C, Huang S, Zhuang H, Ruan S, Zhou Z, Huang K, et al. YTHDF2 promotes the liver cancer stem cell phenotype and cancer metastasis by regulating OCT4 expression via m6A RNA methylation. Oncogene. 2020;39(23):4507–18.
Li T, Hu PS, Zuo Z, Lin JF, Li X, Wu QN, et al. METTL3 facilitates tumor progression via an m6A-IGF2BP2-dependent mechanism in colorectal carcinoma. Mol Cancer. 2019;18(1):112.
Visvanathan A, Patil V, Arora A, Hegde AS, Arivazhagan A, Santosh V, et al. Essential role of METTL3-mediated m 6 A modification in glioma stem-like cells maintenance and radioresistance. Oncogene. 2018;37(4):522–33.
Huang H, Weng H, Sun W, Qin X, Shi H, Wu H, et al. Recognition of RNA N 6 -methyladenosine by IGF2BP proteins enhances mRNA stability and translation. Nat Cell Biol. 2018;20(3):285–95.
LeRoith D, Nissley P. Knock your SOCS off. J Clin Investig. 2005;115(2):379–87.
Chen M, Wei L, Law CT, Ho-Ching Tsang F, Shen J, Lai-Hung Cheng C, et al. RNA N6-methyladenosine methyltransferase-like 3 promotes liver cancer progression through YTHDF2-dependent posttranscriptional silencing of SOCS2. Hepatology. 2018;67(6):2254–70.
Warren CFA, Wong-Brown MW, Bowden NA. BCL-2 family isoforms in apoptosis and cancer. Cell Death Dis. 2019;10(3):177.
Li CW, Dinh GK, Don CJ. Preferential physical and functional interaction of pregnane X receptor with the SMRTα isoform. Mol Pharmacol. 2009;75(2):363–73.
Li F, Yi Y, Miao Y, Long W, Long T, Chen S, et al. N6-methyladenosine modulates nonsense-mediated mRNA decay in human glioblastoma. Cancer Res. 2019;79(22):5785–98.
Akbulut O, Lengerli D, Saatci O, Duman E, Seker UOS, Isik A, et al. A highly potent TACC3 inhibitor as a novel anticancer drug candidate. Mol Cancer Ther. 2020;19(6):1243–54.
Shen C, Sheng Y, Zhu AC, Robinson S, Jiang X, Dong L, et al. RNA demethylase ALKBH5 selectively promotes tumorigenesis and cancer stem cell self-renewal in acute myeloid leukemia. Cell Stem Cell. 2020;27(1):64-80.e9.
Chai RC, Chang YZ, Chang X, Pang B, An SY, Zhang KN, et al. YTHDF2 facilitates UBXN1 mRNA decay by recognizing METTL3-mediated m6A modification to activate NF-κB and promote the malignant progression of glioma. J Hematol Oncol. 2021;14(1):109.
Kowalski-Chauvel A, Lacore MG, Arnauduc F, Delmas C, Toulas C, Cohen-Jonathan-moyal E, et al. The m6a rna demethylase alkbh5 promotes radioresistance and invasion capability of glioma stem cells. Cancers (Basel). 2021;13(1):1–16.
Li Z, Weng H, Su R, Weng X, Zuo Z, Li C, et al. FTO plays an oncogenic role in acute myeloid leukemia as a N6-methyladenosine RNA demethylase. Cancer Cell. 2017;31(1):127–41.
Heuzé ML, Lamsoul I, Baldassarre M, Lad Y, Lévê S, et al. ASB2 targets filamins A and B to proteasomal degradation. Blood. 2008;112:5130–40.
dos Santos GA, Kats L, Pandolfi PP. Synergy against PML-RARa: targeting transcription, proteolysis, differentiation, and self-renewal in acute promyelocytic leukemia. J Exp Med. 2013;210:2793–802.
Han L, Diao L, Yu S, Xu X, Li J, Zhang R, et al. The genomic landscape and clinical relevance of A-to-I RNA editing in human cancers. Cancer Cell. 2015;28(4):515–28.
Laganà A, Paone A, Veneziano D, Cascione L, Gasparini P, Carasi S, et al. MiR-EdiTar: a database of predicted A-to-I edited miRNA target sites. Bioinformatics. 2012;28(23):3166–8.
Liao Y, Jung SH, Kim T. A-to-I RNA editing as a tuner of noncoding RNAs in cancer. Cancer Lett. 2020;494:88–93.
Chen L, Li Y, Lin CH, Chan THM, Chow RKK, Song Y, et al. Recoding RNA editing of AZIN1 predisposes to hepatocellular carcinoma. Nat Med. 2013;19(2):209–16.
Shigeyasu K, Okugawa Y, Toden S, Miyoshi J, Toiyama Y, Nagasaka T, et al. AZIN1 RNA editing confers cancer stemness and enhances oncogenic potential in colorectal cancer. JCI Insight. 2018;3(12):e99976.
Ramírez-Moya J, Miliotis C, Baker AR, Gregory RI, Slack FJ, Santisteban P. An ADAR1-dependent RNA editing event in the cyclin-dependent kinase CDK13 promotes thyroid cancer hallmarks. Mol Cancer. 2021;20(1):115.
Kim HE, Kim DG, Lee KJ, Son JG, Song MY, Park YM, et al. Frequent amplification of CENPF, GMNN and CDK13 genes in hepatocellular carcinomas. PLoS One. 2012;7(8):e43223.
Salpietro V, Dixon CL, Guo H, Bello OD, Vandrovcova J, Efthymiou S, et al. AMPA receptor GluA2 subunit defects are a cause of neurodevelopmental disorders. Nat Commun. 2019;10(1):3094.
Zhang Y, Wang K, Zhao Z, Sun S, Zhang K, Huang R, et al. ADAR3 expression is an independent prognostic factor in lower-grade diffuse gliomas and positively correlated with the editing level of GRIA2Q607R. Cancer Cell Int. 2018;18(1):196.
Chan THM, Qamra A, Tan KT, Guo J, Yang H, Qi L, et al. ADAR-mediated RNA editing predicts progression and prognosis of gastric cancer. Gastroenterology. 2016;151(4):637-650.e10.
Chan THM, Lin CH, Qi L, Fei J, Li Y, Yong KJ, et al. A disrupted RNA editing balance mediated by ADARs (Adenosine DeAminases that act on RNA) in human hepatocellular carcinoma. Gut. 2014;63(5):832–43.
Sonneveld S, Verhagen BMP, Tanenbaum ME. Heterogeneity in mRNA translation. Trends Cell Biol. 2020;30:606–18.
Djebali S, Davis CA, Merkel A, Dobin A, Lassmann T, Mortazavi A, et al. Landscape of transcription in human cells. Nature. 2012;489(7414):101–8.
Cech TR, Steitz JA. The noncoding RNA revolution - trashing old rules to forge new ones. Cell. 2014;157:77–94.
Chen L, Heikkinen L, Wang C, Yang Y, Sun H, Wong G. Trends in the development of miRNA bioinformatics tools. Brief Bioinform. 2019;20:1836–52.
He B, Zhao Z, Cai Q, Zhang Y, Zhang P, Shi S, et al. Mirna-based biomarkers, therapies, and resistance in cancer. Int J Biol Sci. 2020;16:2628–47.
Rupaimoole R, Slack FJ. MicroRNA therapeutics: towards a new era for the management of cancer and other diseases. Nat Rev Drug Discov. 2017;16:203–21.
Yong SL, Dutta A. MicroRNAs in cancer. Annu Rev Pathol Mech Dis. 2009;4:199–227.
Yu F, Yao H, Zhu P, Zhang X, Pan Q, Gong C, et al. let-7 regulates self renewal and tumorigenicity of breast cancer cells. Cell. 2007;131(6):1109–23.
Liu C, Kelnar K, Vlassov AV, Brown D, Wang J, Tang DG. Distinct microRNA expression profiles in prostate cancer stem/progenitor cells and tumor-suppressive functions of let-7. Cancer Res. 2012;72(13):3393–405.
Yang X, Cai H, Liang Y, Chen L, Wang X, Si R, et al. Inhibition of c-Myc by let-7b mimic reverses mutidrug resistance in gastric cancer cells. Oncol Rep. 2015;33(4):1723–30.
Yang N, Kaur S, Volinia S, Greshock J, Lassus H, Hasegawa K, et al. MicroRNA microarray identifies Let-7i as a novel biomarker and therapeutic target in human epithelial ovarian cancer. Cancer Res. 2008;68(24):10307–14.
Yunqing L, Guessous F, Ying Z, DiPierro C, Kefas B, Johnson E, et al. MicroRNA-34a inhibits glioblastoma growth by targeting multiple oncogenes. Cancer Res. 2009;69(19):7569–76.
Hermeking H. MicroRNAs in the p53 network: micromanagement of tumour suppression. Nat Rev Cancer. 2012;12:613–26.
Sun Z, Hu W, Xu J, Kaufmann AM, Albers AE. MicroRNA-34a regulates epithelial-mesenchymal transition and cancer stem cell phenotype of head and neck squamous cell carcinoma in vitro. Int J Oncol. 2015;47(4):1339–50.
Liu C, Kelnar K, Liu B, Chen X, Calhoun-Davis T, Li H, et al. The microRNA miR-34a inhibits prostate cancer stem cells and metastasis by directly repressing CD44. Nat Med. 2011;17(2):211–6.
Põlajeva J, Swartling FJ, Jiang Y, Singh U, Pietras K, Uhrbom L, et al. miRNA-21 is developmentally regulated in mouse brain and is co-expressed with SOX2 in glioma. BMC Cancer. 2012;12:378.
Elghoroury EA, ElDine HG, Kamel SA, Abdelrahman AH, Mohammed A, Kamel MM, et al. Evaluation of miRNA-21 and miRNA Let-7 as prognostic markers in patients with breast cancer. Clin Breast Cancer. 2018;18(4):e721–6.
Nagao Y, Hisaoka M, Matsuyama A, Kanemitsu S, Hamada T, Fukuyama T, et al. Association of microRNA-21 expression with its targets, PDCD4 and TIMP3, in pancreatic ductal adenocarcinoma. Mod Pathol. 2012;25(1):112–21.
Zhao Y, Zhao L, Ischenko I, Bao Q, Schwarz B, Nieß H, et al. Antisense inhibition of microRNA-21 and microRNA-221 in tumor-initiating stem-like cells modulates tumorigenesis, metastasis, and chemotherapy resistance in pancreatic cancer. Target Oncol. 2015;10(4):535–48.
Han M, Wang Y, Liu M, Bi X, Bao J, Zeng N, et al. MiR-21 regulates epithelial-mesenchymal transition phenotype and hypoxia-inducible factor-1α expression in third-sphere forming breast cancer stem cell-like cells. Cancer Sci. 2012;103(6):1058–64.
Darbelli L, Richard S. Emerging functions of the Quaking RNA-binding proteins and link to human diseases. Wiley Interdiscip Rev RNA. 2016;7(3):399–412.
Mukohyama J, Isobe T, Hu Q, Hayashi T, Watanabe T, Maeda M, et al. MiR-221 targets QKI to enhance the tumorigenic capacity of human colorectal cancer stem cells. Cancer Res. 2019;79(20):5151–8.
Bhan A, Soleimani M, Mandal SS. Long noncoding RNA and cancer: a new paradigm. Cancer Res. 2017;77:3965–81.
Jahangiri L, Ishola T, Pucci P, Trigg RM, Pereira J, Williams JA, et al. The role of autophagy and lncrnas in the maintenance of cancer stem cells. Cancers. 2021;13:1–30.
McCabe EM, Rasmussen TP. lncRNA involvement in cancer stem cell function and epithelial-mesenchymal transitions. Semin Cancer Biol. 2021;75:38–48.
Liu S, Sun Y, Hou Y, Yang L, Wan X, Qin Y, et al. A novel lncRNA ROPM-mediated lipid metabolism governs breast cancer stem cell properties. J Hematol Oncol. 2021;14(1):178.
Zhu P, He F, Hou Y, Tu G, Li Q, Jin T, et al. A novel hypoxic long noncoding RNA KB-1980E6.3 maintains breast cancer stem cell stemness via interacting with IGF2BP1 to facilitate c-Myc mRNA stability. Oncogene. 2021;40(9):1609–27.
Qin Y, Hou Y, Liu S, Zhu P, Wan X, Zhao M, et al. A novel long non-coding RNA lnc030 maintains breast cancer stem cell stemness by stabilizing SQLE mRNA and increasing cholesterol synthesis. Adv Sci. 2021;8(2):2002232.
Zhao L, Lou G, Li A, Liu Y. lncRNA MALAT1 modulates cancer stem cell properties of liver cancer cells by regulating YAP1 expression via miR-375 sponging. Mol Med Rep. 2020;22(2):1449–57.
Jiao F, Hu H, Han T, Yuan C, Wang L, Jin Z, et al. Long noncoding RNA MALAT-1 enhances stem cell-like phenotypes in pancreatic cancer cells. Int J Mol Sci. 2015;16(4):6677–93.
Xiao Y, Pan J, Geng Q, Wang G. LncRNA MALAT1 increases the stemness of gastric cancer cells via enhancing SOX2 mRNA stability. FEBS Open Bio. 2019;9(7):1212–22.
Han Y, Zhou L, Wu T, Huang Y, Cheng Z, Li X, et al. Downregulation of lncRNA-MALAT1 affects proliferation and the expression of stemness markers in glioma stem cell line SHG139S. Cell Mol Neurobiol. 2016;36(7):1097–107.
Yu X, Mi L, Dong J, Zou J. Long intergenic non-protein-coding RNA 1567 (LINC01567) acts as a “sponge” against microRNA-93 in regulating the proliferation and tumorigenesis of human colon cancer stem cells. BMC Cancer. 2017;17(1):716.
Yu Y, Nangia-Makker P, Farhana L, Majumdar APN. A novel mechanism of lncRNA and miRNA interaction: CCAT2 regulates miR-145 expression by suppressing its maturation process in colon cancer cells. Mol Cancer. 2017;16(1):155.
Dawson MA, Kouzarides T. Cancer epigenetics: from mechanism to therapy. Cell. 2012;150:12–27.
Dai X, Ren T, Zhang Y, Nan N. Methylation multiplicity and its clinical values in cancer. Expert Rev Mol Med. 2021;23:e2.
Angeloni A, Bogdanovic O. Sequence determinants, function, and evolution of CpG islands. Biochem Soc Trans. 2021;49:1109–19.
Tomita H, Hara A. Serrated lesions and stem cells on drug resistance and colon cancer. In Drug resistance in colorectal cancer: Molecular mechanisms and therapeutic strategies. Elsevier; 2020. p. 75–82.
Wong CC, Xu J, Bian X, Wu JL, Kang W, Qian Y, et al. In colorectal cancer cells with mutant KRAS, SLC25A22-mediated glutaminolysis reduces DNA demethylation to increase WNT signaling, stemness, and drug resistance. Gastroenterology. 2020;159(6):2163-2180.e6.
Lu R, Wang P, Parton T, Zhou Y, Chrysovergis K, Rockowitz S, et al. Epigenetic perturbations by Arg882-mutated DNMT3A potentiate aberrant stem cell gene-expression program and acute leukemia development. Cancer Cell. 2016;30(1):92–107.
Zhang J, Wang J, Liu Y, Sidik H, Young KH, Lodish HF, et al. Oncogenic Kras-induced leukemogeneis: hematopoietic stem cells as the initial target and lineage-specific progenitors as the potential targets for final leukemic transformation. Blood. 2009;113(6):1304–14.
Kwon H-M, Kang E-J, Kang K, Kim S-D, Yang K, Yi JM: Combinatorial effects of an epigenetic inhibitor and ionizing radiation contribute to targeted elimination of pancreatic cancer stem cell. Oncotarget. 2017;8:89005.
Tucker DW, Getchell CR, McCarthy ET, Ohman AW, Sasamoto N, Xu S, et al. Epigenetic reprogramming strategies to reverse global loss of 5-hydroxymethylcytosine, a prognostic factor for poor survival in high-grade serous ovarian cancer. Clin Cancer Res. 2018;24(6):1389–401.
Aoki N, Mochizuki K, Matsui Y. DNA methylation of the Fthl17 5’-upstream region regulates differential Fthl17 expression in lung cancer cells and germline stem cells. PLoS One. 2017;12(2):e0172219.
Wang Q, Liang N, Yang T, Li Y, Li J, Huang Q, et al. DNMT1-mediated methylation of BEX1 regulates stemness and tumorigenicity in liver cancer. J Hepatol. 2021;75(5):1142–53.
Black JC, Van Rechem C, Whetstine JR. Histone lysine methylation dynamics: establishment, regulation, and biological impact. Mol Cell. 2012;48:491–507.
Barski A, Cuddapah S, Cui K, Roh TY, Schones DE, Wang Z, et al. High-resolution profiling of histone methylations in the human genome. Cell. 2007;129(4):823–37.
Wong SHK, Goode DL, Iwasaki M, Wei MC, Kuo HP, Zhu L, et al. The H3K4-methyl epigenome regulates leukemia stem cell oncogenic potential. Cancer Cell. 2015;28(2):198–209.
Choi H, Park J, Park M, Won H, Joo H, Lee CH, et al. UTX inhibits EMT -induced breast CSC properties by epigenetic repression of EMT genes in cooperation with LSD 1 and HDAC 1. EMBO Rep. 2015;16(10):1288–98.
Ji G, Zhou W, Du J, Zhou J, Wu D, Zhao M, et al. PCGF1 promotes epigenetic activation of stemness markers and colorectal cancer stem cell enrichment. Cell Death Dis. 2021;12(7):633.
Zhang G, Lu J, Yang M, Wang Y, Liu H, Xu C. Elevated GALNT10 expression identifies immunosuppressive microenvironment and dismal prognosis of patients with high grade serous ovarian cancer. Cancer Immunol Immunother. 2020;69(2):175–87.
Zhao FY, Zhang Q, Wang JM, Jiang JY, Huyan LY, Liu BQ, et al. BAG3 epigenetically regulates GALNT10 expression via WDR5 and facilitates the stem cell-like properties of platin-resistant ovarian cancer cells. Biochim Biophys Acta Mol Cell Res. 2021;1868(9):119077.
Lin Q, Wu Z, Yue X, Yu X, Wang Z, Song X, et al. ZHX2 restricts hepatocellular carcinoma by suppressing stem cell-like traits through KDM2A-mediated H3K36 demethylation. EBioMedicine. 2020;53:102676.
Tao H, Li H, Su Y, Feng D, Wang X, Zhang C, et al. Histone methyltransferase G9a and H3K9 dimethylation inhibit the self-renewal of glioma cancer stem cells. Mol Cell Biochem. 2014;394(1):23–30.
Gardner AS, Moholdt G, Cogley JG, Wouters B, Arendt AA, Wahr J, et al. Inhibition of PRC2 activity by a gain-of-function H3 mutation found in pediatric glioblastoma. Science (1979). 2013;340(6134):852–7.
Zong X, Wang W, Ozes A, Fang F, Sandusky GE, Nephew KP. EZH2-mediated downregulation of the tumor suppressor DAB2IP maintains ovarian cancer stem cells. Cancer Res. 2020;80(20):4371–85.
Crea F, Hurt EM, Mathews LA, Cabarcas SM, Sun L, Marquez VE, et al. Pharmacologic disruption of Polycomb Repressive Complex 2 inhibits tumorigenicity and tumor progression in prostate cancer. Mol Cancer. 2011;10:40.
Jin MZ, Jin WL. The updated landscape of tumor microenvironment and drug repurposing. Signal Transduct Target Ther. 2020;5(1):166.
Poggi A, Varesano S, Zocchi MR. How to hit mesenchymal stromal cells and make the tumor microenvironment immunostimulant rather than immunosuppressive. Front Immunol. 2018;9:262.
Chen X, Song E. Turning foes to friends: targeting cancer-associated fibroblasts. Nat Rev Drug Discov. 2019;18:99–115.
Li Y, Wang R, Xiong S, Wang X, Zhao Z, Bai S, et al. Cancer-associated fibroblasts promote the stemness of CD24 + liver cells via paracrine signaling. J Mol Med. 2019;97(2):243–55.
Tsuyada A, Chow A, Wu J, Somlo G, Chu P, Loera S, et al. CCL2 mediates cross-talk between cancer cells and stromal fibroblasts that regulates breast cancer stem cells. Cancer Res. 2012;72(11):2768–79.
Suh J, Kim DH, Surh YJ. Resveratrol suppresses migration, invasion and stemness of human breast cancer cells by interfering with tumor-stromal cross-talk. Arch Biochem Biophys. 2018;643:62–71.
Nallasamy P, Nimmakayala RK, Karmakar S, Leon F, Seshacharyulu P, Lakshmanan I, et al. Pancreatic tumor microenvironment factor promotes cancer stemness via SPP1–CD44 axis. Gastroenterology. 2021;161(6):1998-2013.e7.
Su S, Chen J, Yao H, Liu J, Yu S, Lao L, et al. CD10+GPR77+ cancer-associated fibroblasts promote cancer formation and chemoresistance by sustaining cancer stemness. Cell. 2018;172(4):841-856.e16.
Cazet AS, Hui MN, Elsworth BL, Wu SZ, Roden D, Chan CL, et al. Targeting stromal remodeling and cancer stem cell plasticity overcomes chemoresistance in triple negative breast cancer. Nat Commun. 2018;9(1):2897.
Ohtsuka M, Ling H, Ivan C, Pichler M, Matsushita D, Goblirsch M, et al. H19 noncoding RNA, an independent prognostic factor, regulates essential Rb-E2F and CDK8-β-catenin signaling in colorectal cancer. EBioMedicine. 2016;13:113–24.
Ren J, Ding L, Zhang D, Shi G, Xu Q, Shen S, et al. Carcinoma-associated fibroblasts promote the stemness and chemoresistance of colorectal cancer by transferring exosomal lncRNA H19. Theranostics. 2018;8(14):3932–48.
Lin Y, Xu J, Lan H. Tumor-associated macrophages in tumor metastasis: Biological roles and clinical therapeutic applications. J Hematol Oncol. 2019;12(1):76.
Locati M, Curtale G, Mantovani A. Diversity, mechanisms, and significance of macrophage plasticity. Annu Rev Pathol. 2020;15:123–47.
Wu G, Ma Z, Cheng Y, Hu W, Deng C, Jiang S, et al. Targeting Gas6/TAM in cancer cells and tumor microenvironment. Mol Cancer. 2018;17(1):20.
Gomez KE, Wu FL, Keysar SB, Jason Morton J, Miller B, Chimed TS, et al. Cancer cell CD44 mediates macrophage/ monocyte-driven regulation of head and neck cancer stem cells. Cancer Res. 2020;80(19):4185–98.
Perng YC, Lenschow DJ. ISG15 in antiviral immunity and beyond. Nat Rev Microbiol. 2018;16:423–39.
Lu H, Clauser KR, Tam WL, Fröse J, Ye X, Eaton EN, et al. A breast cancer stem cell niche supported by juxtacrine signalling from monocytes and macrophages. Nat Cell Biol. 2014;16(11):1105–17.
Wan S, Zhao E, Kryczek I, Vatan L, Sadovskaya A, Ludema G, et al. Tumor-associated macrophages produce interleukin 6 and signal via STAT3 to promote expansion of human hepatocellular carcinoma stem cells. Gastroenterology. 2014;147(6):1393–404.
Li X, Bu W, Meng L, Liu X, Wang S, Jiang L, et al. CXCL12/CXCR4 pathway orchestrates CSC-like properties by CAF recruited tumor associated macrophage in OSCC. Exp Cell Res. 2019;378(2):131–8.
Deshmukh A, Deshpande K, Arfuso F, Newsholme P, Dharmarajan A. Cancer stem cell metabolism: a potential target for cancer therapy. Mol Cancer. 2016;15(1):69.
Liu PP, Liao J, Tang ZJ, Wu WJ, Yang J, Zeng ZL, et al. Metabolic regulation of cancer cell side population by glucose through activation of the Akt pathway. Cell Death Differ. 2014;21(1):124–35.
Mizushima E, Tsukahara T, Emori M, Murata K, Akamatsu A, Shibayama Y, et al. Osteosarcoma-initiating cells show high aerobic glycolysis and attenuation of oxidative phosphorylation mediated by LIN28B. Cancer Sci. 2020;111(1):36–46.
Zhou Y, Zhou Y, Shingu T, Feng L, Chen Z, Ogasawara M, et al. Metabolic alterations in highly tumorigenic glioblastoma cells: preference for hypoxia and high dependency on glycolysis. J Biol Chem. 2011;286(37):32843–53.
Pacifico F, Leonardi A, Crescenzi E. Glutamine metabolism in cancer stem cells: a complex liaison in the tumor microenvironment. Int J Mol Sci. 2023;24(3):2337.
Le Grand M, Mukha A, Püschel J, Valli E, Kamili A, Vittorio O, et al. Interplay between MycN and c-Myc regulates radioresistance and cancer stem cell phenotype in neuroblastoma upon glutamine deprivation. Theranostics. 2020;10(14):6411–29.
Lee ACK, Lau PM, Kwan YW, Kong SK. Mitochondrial fuel dependence on glutamine drives chemo-resistance in the cancer stem cells of hepatocellular carcinoma. Int J Mol Sci. 2021;22(7):3315.
Tran TQ, Hanse EA, Habowski AN, Li H, Gabra MBI, Yang Y, et al. α-Ketoglutarate attenuates Wnt signaling and drives differentiation in colorectal cancer. Nat Cancer. 2020;1(3):345–58.
De Francesco EM, Sotgia F, Lisanti MP. Cancer stem cells (CSCs): metabolic strategies for their identification and eradication. Biochem J. 2018;475:1611–34.
Brandi J, Dando I, Pozza ED, Biondani G, Jenkins R, Elliott V, et al. Proteomic analysis of pancreatic cancer stem cells: functional role of fatty acid synthesis and mevalonate pathways. J Proteomics. 2017;150:310–22.
Wang T, Fahrmann JF, Lee H, Li YJ, Tripathi SC, Yue C, et al. JAK/STAT3-regulated fatty acid β-oxidation is critical for breast cancer stem cell self-renewal and chemoresistance. Cell Metab. 2018;27(1):136-150.e5.
Ito K, Carracedo A, Weiss D, Arai F, Ala U, Avigan DE, et al. A PML-PPAR-δ pathway for fatty acid oxidation regulates hematopoietic stem cell maintenance. Nat Med. 2012;18(9):1350–8.
Mukha A, Dubrovska A. Metabolic targeting of cancer stem cells. Front Oncol. 2020;10:537930.
Semenza GL. Hypoxia-inducible factors: coupling glucose metabolism and redox regulation with induction of the breast cancer stem cell phenotype. EMBO J. 2017;36(3):252–9.
Cui CP, Wong CCL, Kai AKL, Ho DWH, Lau EYT, Tsui YM, et al. SENP1 promotes hypoxia-induced cancer stemness by HIF-1α deSUMOylation and SENP1/HIF-1α positive feedback loop. Gut. 2017;66(12):2149–59.
Wu MJ, Chen YS, Kim MR, Chang CC, Gampala S, Zhang Y, et al. Epithelial-mesenchymal transition directs stem cell polarity via regulation of mitofusin. Cell Metab. 2019;29(4):993-1002.e6.
Nieto MA. Epithelial plasticity: a common theme in embryonic and cancer cells. Science (1979). 2013;342(6159):1234850.
Markopoulos GS, Roupakia E, Marcu KB, Kolettas E. Epigenetic regulation of inflammatory cytokine-induced epithelial-tomesenchymal cell transition and cancer stem cell generation. Cells. 2019;8(10):1143.
Shibue T, Weinberg RA. EMT, CSCs, and drug resistance: the mechanistic link and clinical implications. Nat Rev Clin Oncol. 2017;14:611–29.
Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133(4):704–15.
Liu S, Kumar SM, Martin JS, Yang R, Xu X. Snail1 mediates hypoxia-induced melanoma progression. Am J Pathol. 2011;179(6):3020–31.
Dong C, Wu Y, Yao J, Wang Y, Yu Y, Rychahou PG, et al. G9a interacts with Snail and is critical for Snail-mediated E-cadherin repression in human breast cancer. J Clin Investig. 2012;122(4):1469–86.
Lin JC, Tsai JT, Chao TY, Ma HI, Liu WH. The STAT3/slug axis enhances radiation-induced tumor invasion and cancer stem-like properties in radioresistant glioblastoma. Cancers (Basel). 2018;10(12):512.
Wellner U, Schubert J, Burk UC, Schmalhofer O, Zhu F, Sonntag A, et al. The EMT-activator ZEB1 promotes tumorigenicity by repressing stemness-inhibiting microRNAs. Nat Cell Biol. 2009;11(12):1487–95.
Yang MH, Hsu DSS, Wang HW, Wang HJ, Lan HY, Yang WH, et al. Bmi1 is essential in Twist1-induced epithelial-mesenchymal transition. Nat Cell Biol. 2010;12(10):982–92.
Yang Y, Wang G, Zhu D, Huang Y, Luo Y, Su P, et al. Epithelial-mesenchymal transition and cancer stem cell-like phenotype induced by Twist1 contribute to acquired resistance to irinotecan in colon cancer. Int J Oncol. 2017;51(2):515–24.
Schmidt JM, Panzilius E, Bartsch HS, Irmler M, Beckers J, Kari V, et al. Stem-cell-like properties and epithelial plasticity arise as stable traits after transient twist1 activation. Cell Rep. 2015;10(2):131–9.
Celià-Terrassa T, Meca-Cortés Ó, Mateo F, De Paz AM, Rubio N, Arnal-Estapé A, et al. Epithelial-mesenchymal transition can suppress major attributes of human epithelial tumor-initiating cells. J Clin Investig. 2012;122(5):1849–68.
Li L, Tang P, Li S, Qin X, Yang H, Wu C, et al. Notch signaling pathway networks in cancer metastasis: a new target for cancer therapy. Med Oncol. 2017;34(10):180.
Andersson ER, Sandberg R, Lendahl U. Notch signaling: simplicity in design, versatility in function. Development. 2011;138:3593–612.
Aster JC, Pear WS, Blacklow SC. The varied roles of notch in cancer. Annu Rev Pathol Mech Dis. 2017;12:245–75.
Ibrahim SA, Gadalla R, El-Ghonaimy EA, Samir O, Mohamed HT, Hassan H, et al. Syndecan-1 is a novel molecular marker for triple negative inflammatory breast cancer and modulates the cancer stem cell phenotype via the IL-6/STAT3, Notch and EGFR signaling pathways. Mol Cancer. 2017;16(1):57.
Brabletz S, Bajdak K, Meidhof S, Burk U, Niedermann G, Firat E, et al. The ZEB1/miR-200 feedback loop controls Notch signalling in cancer cells. EMBO J. 2011;30(4):770–82.
Jiang N, Zou C, Zhu Y, Luo Y, Chen L, Lei Y, et al. HIF-1α-regulated miR-1275 maintains stem cell-like phenotypes and promotes the progression of LUAD by simultaneously activating Wnt/β-catenin and Notch signaling. Theranostics. 2020;10(6):2553–70.
Kao SH, Wu KJ, Lee WH. Hypoxia, epithelial-mesenchymal transition, and tet-mediated epigenetic changes. J Clin Med. 2016;5(2):24.
Sahlgren C, Gustafsson MV, Jin S, Poellinger L, Lendahl U. Notch signaling mediates hypoxia-induced tumor cell migration and invasion. Proc Natl Acad Sci U S A. 2008;105(17):6392–7.
Xing F, Okuda H, Watabe M, Kobayashi A, Pai SK, Liu W, et al. Hypoxia-induced Jagged2 promotes breast cancer metastasis and self-renewal of cancer stem-like cells. Oncogene. 2011;30(39):4075–86.
Jin L, Vu T, Yuan G, Datta PK. STRAP promotes stemness of human colorectal cancer via epigenetic regulation of the NOTCH pathwaya. Cancer Res. 2017;77(20):5464–78.
Qiu L, Yang X, Wu J, Huang C, Miao Y, Fu Z. HIST2H2BF potentiates the propagation of cancer stem cells via notch signaling to promote malignancy and liver metastasis in colorectal carcinoma. Front Oncol. 2021;11:677646.
Katoh M. Canonical and non-canonical WNT signaling in cancer stem cells and their niches: cellular heterogeneity, omics reprogramming, targeted therapy and tumor plasticity (Review). Int J Oncol. 2017;51:1357–69.
Gong A, Huang S. FoxM1 and Wnt/β-catenin signaling in glioma stem cells. Cancer Res. 2012;72:5658–62.
Fendler A, Bauer D, Busch J, Jung K, Wulf-Goldenberg A, Kunz S, et al. Inhibiting WNT and NOTCH in renal cancer stem cells and the implications for human patients. Nat Commun. 2020;11(1):929.
Takebe N, Miele L, Harris PJ, Jeong W, Bando H, Kahn M, et al. Targeting Notch, Hedgehog, and Wnt pathways in cancer stem cells: clinical update. Nat Rev Clin Oncol. 2015;12:445–64.
Reya T, Clevers H. Wnt signalling in stem cells and cancer. Nature. 2005;434(7035):843–50.
Cho YH, Ro EJ, Yoon JS, Mizutani T, Kang DW, Park JC, et al. 5-FU promotes stemness of colorectal cancer via p53-mediated WNT/β-catenin pathway activation. Nat Commun. 2020;11(1):5321.
Vermeulen L, De Sousa E Melo F, Van Der Heijden M, Cameron K, De Jong JH, Borovski T, et al. Wnt activity defines colon cancer stem cells and is regulated by the microenvironment. Nat Cell Biol. 2010;12(5):468–76.
Wei CY, Zhu MX, Yang YW, Zhang PF, Yang X, Peng R, et al. Downregulation of RNF128 activates Wnt/?-catenin signaling to induce cellular EMT and stemness via CD44 and CTTN ubiquitination in melanoma. J Hematol Oncol. 2019;12(1):21.
Rong Z, Zhang L, Li Z, Xiao Z, Duan Y, Ren X, et al. SIK2 maintains breast cancer stemness by phosphorylating LRP6 and activating Wnt/β-catenin signaling. Oncogene. 2022.
Jang GB, Kim JY, Cho SD, Park KS, Jung JY, Lee HY, et al. Blockade of Wnt/β-catenin signaling suppresses breast cancer metastasis by inhibiting CSC-like phenotype. Sci Rep. 2015;5:12465.
Hou P, Ma X, Zhang Q, Wu CJ, Liao W, Li J, et al. USP21 deubiquitinase promotes pancreas cancer cell stemness via Wnt pathway activation. Genes Dev. 2019;33(19–20):1361–6.
Mao J, Fan S, Ma W, Fan P, Wang B, Zhang J, et al. Roles of Wnt/β-catenin signaling in the gastric cancer stem cells proliferation and salinomycin treatment. Cell Death Dis. 2014;5(1):e1039.
Gadea G, Blangy A. Dock-family exchange factors in cell migration and disease. Eur J Cell Biol. 2014;93:466–77.
Chi HC, Tsai CY, Wang CS, Yang HY, Lo CH, Wang WJ, et al. DOCK6 promotes chemo- and radioresistance of gastric cancer by modulating WNT/β-catenin signaling and cancer stem cell traits. Oncogene. 2020;39(37):5933–49.
Park SY, Kim JY, Jang GB, Choi JH, Kim JH, Lee CJ, et al. Aberrant activation of the CD45-Wnt signaling axis promotes stemness and therapy resistance in colorectal cancer cells. Theranostics. 2021;11(18):8755–70.
Merchant AA, Matsui W. Targeting Hedgehog - a cancer stem cell pathway. Clin Cancer Res. 2010;16:3130–40.
Kong JH, Siebold C, Rohatgi R. Biochemical mechanisms of vertebrate hedgehog signaling. Development (Cambridge). 2019;146(10):dev166892.
Jeng KS, Chang CF, Lin SS. Sonic hedgehog signaling in organogenesis, tumors, and tumor microenvironments. Int J Mol Sci. 2020;21(3):758.
Lu Y, Zhu Y, Deng S, Chen Y, Li W, Sun J, Xu X. Targeting the Sonic Hedgehog Pathway to Suppress the Expression of the Cancer Stem Cell (CSC)-Related Transcription Factors and CSC-Driven Thyroid Tumor Growth. Cancers (Basel). 2021;13(3):418.
Yang Y, Shi J, Tolomelli G, Xu H, Xia J, Wang H, et al. RARα2 expression confers myeloma stem cell features. Blood. 2013;122(8):1437–47.
Kim BR, Na YJ, Kim JL, Jeong YA, Park SH, Jo MJ, et al. RUNX3 suppresses metastasis and stemness by inhibiting Hedgehog signaling in colorectal cancer. Cell Death Differ. 2020;27(2):676–94.
Morikawa M, Derynck R, Miyazono K. TGF- β and the TGF-β family: Context-dependent roles in cell and tissue physiology. Cold Spring Harb Perspect Biol. 2016;8(5):a021873.
Zhang Y, Alexander PB, Wang XF. TGF-β family signaling in the control of cell proliferation and survival. Cold Spring Harb Perspect Biol. 2017;9(4):a022145.
Colak S, ten Dijke P. Targeting TGF-β signaling in cancer. Trends Cancer. 2017;3:56–71.
Xu X, Zhang L, He X, Zhang P, Sun C, Xu X, et al. TGF-β plays a vital role in triple-negative breast cancer (TNBC) drug-resistance through regulating stemness, EMT and apoptosis. Biochem Biophys Res Commun. 2018;502(1):160–5.
Futakuchi M, Lami K, Tachibana Y, Yamamoto Y, Furukawa M, Fukuoka J. The effects of TGF-β signaling on cancer cells and cancer stem cells in the bone microenvironment. Int J Mol Sci. 2019;20(20):5117.
Yu D, Shin HS, Lee YS, Lee YC. MiR-106b modulates cancer stem cell characteristics through TGF-β/Smad signaling in CD44-positive gastric cancer cells. Lab Invest. 2014;94(12):1370–81.
Kim BN, Ahn DH, Kang N, Yeo CD, Kim YK, Lee KY, et al. TGF-β induced EMT and stemness characteristics are associated with epigenetic regulation in lung cancer. Sci Rep. 2020;10(1):10597.
Wang X, Wang J, Tsui YM, Shi C, Wang Y, Zhang X, et al. RALYL increases hepatocellular carcinoma stemness by sustaining the mRNA stability of TGF-β2. Nat Commun. 2021;12(1):1518.
Yeh HW, Hsu EC, Lee SS, Lang YD, Lin YC, Chang CY, et al. PSPC1 mediates TGF-β1 autocrine signalling and Smad2/3 target switching to promote EMT, stemness and metastasis. Nat Cell Biol. 2018;20(4):479–91.
Ottaviani S, Stebbing J, Frampton AE, Zagorac S, Krell J, De Giorgio A, et al. TGF-β induces miR-100 and miR-125b but blocks let-7a through LIN28B controlling PDAC progression. Nat Commun. 2018;9(1):1845.
Yu H, Lee H, Herrmann A, Buettner R, Jove R. Revisiting STAT3 signalling in cancer: new and unexpected biological functions. Nat Rev Cancer. 2014;14:736–46.
Jin W. Role of JAK/STAT3 signaling in the regulation of metastasis, the transition of cancer stem cells, and chemoresistance of cancer by epithelial-mesenchymal transition. Cells. 2020;9(1):217.
Park SY, Lee CJ, Choi JH, Kim JH, Kim JW, Kim JY, et al. The JAK2/STAT3/CCND2 axis promotes colorectal cancer stem cell persistence and radioresistance. J Exp Clin Cancer Res. 2019;38(1):399.
Kim SY, Kang JW, Song X, Kim BK, Yoo YD, Kwon YT, et al. Role of the IL-6-JAK1-STAT3-Oct-4 pathway in the conversion of non-stem cancer cells into cancer stem-like cells. Cell Signal. 2013;25(4):961–9.
Su YJ, Lai HM, Chang YW, Chen GY, Lee JL. Direct reprogramming of stem cell properties in colon cancer cells by CD44. EMBO J. 2011;30(15):3186–99.
Masjedi A, Hajizadeh F, Beigi Dargani F, Beyzai B, Aksoun M, Hojjat-Farsangi M, et al. Oncostatin M: a mysterious cytokine in cancers. Int Immunopharmacol. 2021;90:107158.
Junk DJ, Bryson BL, Smigiel JM, Parameswaran N, Bartel CA, Jackson MW. Oncostatin M promotes cancer cell plasticity through cooperative STAT3-SMAD3 signaling. Oncogene. 2017;36(28):4001–13.
Losuwannarak N, Maiuthed A, Kitkumthorn N, Leelahavanichkul A, Roytrakul S, Chanvorachote P. Gigantol targets cancer stem cells and destabilizes tumors via the suppression of the PI3K/AKT and JAK/STAT pathways in ectopic lung cancer xenografts. Cancers (Basel). 2019;11(12):2032.
Yang Y, Ding L, Hu Q, Xia J, Sun J, Wang X, et al. MicroRNA-218 functions as a tumor suppressor in lung cancer by targeting IL-6/STAT3 and negatively correlates with poor prognosis. Mol Cancer. 2017;16(1):141.
Kanno H, Sato H, Yokoyama TA, Yoshizumi T, Yamada S. The VHL tumor suppressor protein regulates tumorigenicity of U87-derived glioma stem-like cells by inhibiting the JAK/STAT signaling pathway. Int J Oncol. 2013;42(3):881–6.
Kothari AN, Arffa ML, Chang V, Blackwell RH, Syn WK, Zhang J, et al. Osteopontin—a master regulator of epithelialmesenchymal transition. J Clin Med. 2016;5(4):39.
Im Choi S, Yoen Kim S, Ha Lee J, Yul Kim J, Wie Cho E, Kim IG. Osteopontin production by TM4SF4 signaling drives a positive feedback autocrine loop with the STAT3 pathway to maintain cancer stem cell-like properties in lung cancer cells. Oncotarget. 2017;8(60):101284–97.
Zhou BBS, Zhang H, Damelin M, Geles KG, Grindley JC, Dirks PB. Tumour-initiating cells: challenges and opportunities for anticancer drug discovery. Nat Rev Drug Discov. 2009;8:806–23.
Yang L, Shi P, Zhao G, Xu J, Peng W, Zhang J, et al. Targeting cancer stem cell pathways for cancer therapy. Signal Transduct Target Ther. 2020;5(1):8.
Batlle E, Clevers H. Cancer stem cells revisited. Nat Med. 2017;23:1124–34.
Sharma NS, Gnamlin P, Durden B, Gupta VK, Kesh K, Garrido VT, et al. Long non-coding RNA GAS5 acts as proliferation “brakes” in CD133+ cells responsible for tumor recurrence. Oncogenesis. 2019;8(12):68.
Li L, Bhatia R. Stem cell quiescence. Clin Cancer Res. 2011;17:4936–41.
Roesch A, Fukunaga-Kalabis M, Schmidt EC, Zabierowski SE, Brafford PA, Vultur A, et al. A temporarily distinct subpopulation of slow-cycling melanoma cells is required for continuous tumor growth. Cell. 2010;141(4):583–94.
Takeishi S, Matsumoto A, Onoyama I, Naka K, Hirao A, Nakayama KI. Ablation of Fbxw7 eliminates leukemia-initiating cells by preventing quiescence. Cancer Cell. 2013;23(3):347–61.
Kobayashi A, Okuda H, Xing F, Pandey PR, Watabe M, Hirota S, et al. Bone morphogenetic protein 7 in dormancy and metastasis of prostate cancer stem-like cells in bone. J Exp Med. 2011;208(13):2641–55.
Ye S, Ding YF, Jia WH, Liu XL, Feng JY, Zhu Q, et al. SET domain-containing protein 4 epigenetically controls breast cancer stem cell quiescence. Cancer Res. 2019;79(18):4729–43.
Chen Y, Li D, Wang D, Liu X, Yin N, Song Y, et al. Quiescence and attenuated DNA damage response promote survival of esophageal cancer stem cells. J Cell Biochem. 2012;113(12):3643–52.
Bao S, Wu Q, McLendon RE, Hao Y, Shi Q, Hjelmeland AB, et al. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature. 2006;444(7120):756–60.
Kurtova AV, Xiao J, Mo Q, Pazhanisamy S, Krasnow R, Lerner SP, et al. Blocking PGE2-induced tumour repopulation abrogates bladder cancer chemoresistance. Nature. 2015;517(7533):209–13.
Scherz-Shouval R, Elazar Z. Regulation of autophagy by ROS: physiology and pathology. Trends Biochem Sci. 2011;36:30–8.
Kangasjärvi S, Kangasjärvi J. Towards understanding extracellular ROS sensory and signaling systems in plants. Adv Bot. 2014;2014:1–10.
Srinivas US, Tan BWQ, Vellayappan BA, Jeyasekharan AD. ROS and the DNA damage response in cancer. Redox Biol. 2019;25:101084.
Mizuno T, Suzuki N, Makino H, Furui T, Morii E, Aoki H, et al. Cancer stem-like cells of ovarian clear cell carcinoma are enriched in the ALDH-high population associated with an accelerated scavenging system in reactive oxygen species. Gynecol Oncol. 2015;137(2):299–305.
Son YW, Cheon MG, Kim Y, Jang HH. Prx2 links ROS homeostasis to stemness of cancer stem cells. Free Radic Biol Med. 2019;134:260–7.
Zhao H, Duan Q, Zhang Z, Li H, Wu H, Shen Q, et al. Up-regulation of glycolysis promotes the stemness and EMT phenotypes in gemcitabine-resistant pancreatic cancer cells. J Cell Mol Med. 2017;21(9):2055–67.
Diehn M, Cho RW, Lobo NA, Kalisky T, Dorie MJ, Kulp AN, et al. Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature. 2009;458(7239):780–3.
Toledo-Guzmán ME, Hernández MI, Gómez-Gallegos ÁA, Ortiz-Sánchez E. Aldh as a stem cell marker in solid tumors. Curr Stem Cell Res Ther. 2019;14(5):375–88.
Huang CP, Tsai MF, Chang TH, Tang WC, Chen SY, Lai HH, et al. ALDH-positive lung cancer stem cells confer resistance to epidermal growth factor receptor tyrosine kinase inhibitors. Cancer Lett. 2013;328(1):144–51.
Dinavahi SS, Bazewicz CG, Gowda R, Robertson GP. Aldehyde dehydrogenase inhibitors for cancer therapeutics. Trends Pharmacol Sci. 2019;40:774–89.
Raha D, Wilson TR, Peng J, Peterson D, Yue P, Evangelista M, et al. The cancer stem cell marker aldehyde dehydrogenase is required to maintain a drug-tolerant tumor cell subpopulation. Cancer Res. 2014;74(13):3579–90.
Muralikrishnan V, Hurley TD, Nephew KP. Targeting aldehyde dehydrogenases to eliminate cancer stem cells in gynecologic malignancies. Cancers. 2020;12(4):961.
Juarez M, Schcolnik-Cabrera A, Dueñas-Gonzalez A. The multitargeted drug ivermectin: from an antiparasitic agent to a repositioned cancer drug. Am J Cancer Res. 2018;8(2):317–33.
Dominguez-Gomez G, Chavez-Blanco A, Medina-Franco JL, Saldivar-Gonzalez F, Flores-Torrontegui Y, Juarez M, et al. Ivermectin as an inhibitor of cancer stem-like cells. Mol Med Rep. 2018;17(2):3397–403.
Stolzenburg S, Rots MG, Beltran AS, Rivenbark AG, Yuan X, Qian H, et al. Targeted silencing of the oncogenic transcription factor SOX2 in breast cancer. Nucleic Acids Res. 2012;40(14):6725–40.
Liu K, Xie F, Zhao T, Zhang R, Gao A, Chen Y, et al. Targeting SOX2 protein with peptide aptamers for therapeutic gains against esophageal squamous cell carcinoma. Mol Ther. 2020;28(3):901–13.
Li Y, Xian M, Yang B, Ying M, He Q. Inhibition of KLF4 by statins reverses adriamycin-induced metastasis and cancer stemness in osteosarcoma cells. Stem Cell Rep. 2017;8(6):1617–29.
Yao R, Zhang M, Zhou J, Liu L, Zhang Y, Gao J, et al. Novel dual-targeting c-Myc inhibitor D347–2761 represses myeloma growth via blocking c-Myc/Max heterodimerization and disturbing its stability. Cell Commun Signal. 2022;20(1):73.
Shen YA, Jung J, Shimberg GD, Hsu FC, Rahmanto YS, Gaillard SL, et al. Development of small molecule inhibitors targeting PBX1 transcription signaling as a novel cancer therapeutic strategy. iScience. 2021;24(11):103297.
Hu L, Zeng Z, Xia Q, Liu Z, Feng X, Chen J, et al. Metformin attenuates hepatoma cell proliferation by decreasing glycolytic flux through the HIF-1α/PFKFB3/PFK1 pathway. Life Sci. 2019;239:116966.
Zannella VE, Pra AD, Muaddi H, McKee TD, Stapleton S, Sykes J, et al. Reprogramming metabolism with metformin improves tumor oxygenation and radiotherapy response. Clin Cancer Res. 2013;19(24):6741–50.
Wei R, Hackman RM, Wang Y, Mackenzie GG. Targeting glycolysis with epigallocatechin-3-gallate enhances the efficacy of chemotherapeutics in pancreatic cancer cells and xenografts. Cancers (Basel). 2019;11(10):1496.
Calvert AE, Chalastanis A, Wu Y, Hurley LA, Kouri FM, Bi Y, et al. Cancer-associated IDH1 promotes growth and resistance to targeted therapies in the absence of mutation. Cell Rep. 2017;19(9):1858–73.
Cho H, Du X, Rizzi JP, Liberzon E, Chakraborty AA, Gao W, et al. On-target efficacy of a HIF-2α antagonist in preclinical kidney cancer models. Nature. 2016;539(7627):107–11.
Wicks EE, Semenza GL. Hypoxia-inducible factors: cancer progression and clinical translation. J Clin Invest. 2022;132(11):e159839.
DiPippo AJ, Wilson NR, Pemmaraju N. Targeting CD123 in BPDCN: an emerging field. Expert Rev Hematol. 2021;14:993–1004.
Angelova E, Audette C, Kovtun Y, Daver N, Wang SA, Pierce S, et al. CD123 expression patterns and selective targeting with a CD123-targeted antibody-drug conjugate (IMGN632) in acute lymphoblastic leukemia. Haematologica. 2019;104(4):749–55.
Montesinos P, Roboz GJ, Bulabois CE, Subklewe M, Platzbecker U, Ofran Y, et al. Safety and efficacy of talacotuzumab plus decitabine or decitabine alone in patients with acute myeloid leukemia not eligible for chemotherapy: results from a multicenter, randomized, phase 2/3 study. Leukemia. 2021;35(1):62–74.
Uy GL, Aldoss I, Foster MC, Sayre PH, Wieduwilt MJ, Advani AS, et al. Flotetuzumab as salvage immunotherapy for refractory acute myeloid leukemia. Blood. 2021;137:751–62.
Cangini D, Silimbani P, Cafaro A, Giannini MB, Masini C, Di Rorà AGL, et al. Tagraxofusp and anti-cd123 in blastic plasmacytoid dendritic cell neoplasm: a new hope. Minerva Med. 2020;111(5):467–77.
Sauter A, Kloft C, Gronau S, Bogeschdorfer F, Erhardt T, Golze W, Schroen C, Staab A, Riechelmann H, Hoermann K. Pharmacokinetics, immunogenicity and safety of bivatuzumab mertansine, a novel CD44v6-targeting immunoconjugate, inpatients with squamous cell carcinoma of the head and neck. Int J Oncol. 2007;30(4):927–35.
Tijink BM, Buter J, De Bree R, Giaccone G, Lang MS, Staab A, et al. A phase I dose escalation study with anti-CD44v6 bivatuzumab mertansine in patients with incurable squamous cell carcinoma of the head and neck or esophagus. Clin Cancer Res. 2006;12(20 PART 1):6064–72.
Krishnamurthy A, Jimeno A. Bispecific antibodies for cancer therapy: a review. Pharmacol Ther. 2018;185:122–34.
Knödler M, Körfer J, Kunzmann V, Trojan J, Daum S, Schenk M, et al. Randomised phase II trial to investigate catumaxomab (anti-EpCAM × anti-CD3) for treatment of peritoneal carcinomatosis in patients with gastric cancer. Br J Cancer. 2018;119(3):296–302.
Sehouli J, Reinthaller A, Marth C, Reimer D, Reimer T, Stummvoll W, et al. Intra- and postoperative catumaxomab in patients with epithelial ovarian cancer: safety and two-year efficacy results from a multicentre, single-arm, phase II study. Br J Cancer. 2014;111(8):1519–25.
Bezan A, Hohla F, Meissnitzer T, Greil R. Systemic effect of catumaxomab in a patient with metastasized colorectal cancer: a case report. BMC Cancer. 2013;13:618.
Lea MA, Qureshi MS, Buxhoeveden M, Gengel N, Kleinschmit J, Desbordes C. Regulation of the proliferation of colon cancer cells by compounds that affect glycolysis, including 3-bromopyruvate, 2-deoxyglucose and biguanides. Anticancer Res. 2013;33(2):401–7.
Best SA, Gubser PM, Sethumadhavan S, Kersbergen A, Negrón Abril YL, Goldford J, et al. Glutaminase inhibition impairs CD8 T cell activation in STK11-/Lkb1-deficient lung cancer. Cell Metab. 2022;34(6):874-887.e6.
Jin UH, Lee SO, Pfent C, Safe S. The aryl hydrocarbon receptor ligand omeprazole inhibits breast cancer cell invasion and metastasis. BMC Cancer. 2014;14(1):498.
Yasumoto Y, Miyazaki H, Vaidyan LK, Kagawa Y, Ebrahimi M, Yamamoto Y, et al. Inhibition of fatty acid synthase decreases expression of stemness markers in glioma stem cells. PLoS One. 2016;11(1):e0147717.
Chen W, Hill H, Christie A, Kim MS, Holloman E, Pavia-Jimenez A, et al. Targeting renal cell carcinoma with a HIF-2 antagonist. Nature. 2016;539(7627):112–7.
Tolcher AW, Messersmith WA, Mikulski SM, Papadopoulos KP, Kwak EL, Gibbon DG, et al. Phase I study of RO4929097, a gamma secretase inhibitor of notch signaling, in patients with refractory metastatic or locally advanced solid tumors. J Clin Oncol. 2012;30(19):2348–53.
Wu J, LoRusso PM, Matherly LH, Li J. Implications of plasma protein binding for pharmacokinetics and pharmacodynamics of the γ-secretase inhibitor RO4929097. Clin Cancer Res. 2012;18(7):2066–79.
Schott AF, Landis MD, Dontu G, Griffith KA, Layman RM, Krop I, et al. Preclinical and clinical studies of gamma secretase inhibitors with docetaxel on human breast tumors. Clin Cancer Res. 2013;19(6):1512–24.
Ferrarotto R, Eckhardt G, Patnaik A, LoRusso P, Faoro L, Heymach JV, et al. A phase I dose-escalation and dose-expansion study of brontictuzumab in subjects with selected solid tumors. Ann Oncol. 2018;29(7):1561–8.
Kim DH, Lee S, Kang HG, Park HW, Lee HW, Kim D, et al. Synergistic antitumor activity of a DLL4/VEGF bispecific therapeutic antibody in combination with irinotecan in gastric cancer. BMB Rep. 2020;53(10):533–8.
Yeom DH, Lee YS, Ryu I, Lee S, Sung B, Lee HB, et al. Abl001, a bispecific antibody targeting vegf and dll4, with chemotherapy, synergistically inhibits tumor progression in xenograft models. Int J Mol Sci. 2021;22(1):1–14.
Pak S, Park S, Kim Y, Park JH, Park CH, Lee KJ, et al. The small molecule WNT/β-catenin inhibitor CWP232291 blocks the growth of castration-resistant prostate cancer by activating the endoplasmic reticulum stress pathway. J Exp Clin Cancer Res. 2019;38(1):342.
Fischer MM, Cancilla B, Yeung VP, Cattaruzza F, Chartier C, Murriel CL, et al. WNT antagonists exhibit unique combinatorial antitumor activity with taxanes by potentiating mitotic cell death. Sci Adv. 2017;3(6):e1700090.
Justilien V, Fields AP. Molecular pathways: novel approaches for improved therapeutic targeting of hedgehog signaling in cancer stem cells. Clin Cancer Res. 2015;21:505–13.
Sekulic A, Migden MR, Oro AE, Dirix L, Lewis KD, Hainsworth JD, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. New Engl J Med. 2012;366:2171–9.
Sarkaria SM, Heaney ML. Glasdegib in newly diagnosed acute myeloid leukemia. Expert Rev Anticancer Ther. 2021;21:573–81.
Cortes JE, Heidel FH, Hellmann A, Fiedler W, Smith BD, Robak T, et al. Randomized comparison of low dose cytarabine with or without glasdegib in patients with newly diagnosed acute myeloid leukemia or high-risk myelodysplastic syndrome. Leukemia. 2019;33(2):379–89.
Kim BG, Malek E, Choi SH, Ignatz-Hoover JJ, Driscoll JJ. Novel therapies emerging in oncology to target the TGF-β pathway. J Hematol Oncol. 2021;14:1–20.
Teicher BA. TGFβ-directed therapeutics: 2020. Pharmacol Ther. 2021;217:107666.
Su Q, Banks E, Bebernitz G, Bell K, Borenstein CF, Chen H, et al. Discovery of (2 r)- n-[3-[2-[(3-methoxy-1-methyl-pyrazol-4-yl)amino]pyrimidin-4-yl]-1 h-indol-7-yl]-2-(4-methylpiperazin-1-yl)propenamide (azd4205) as a potent and selective janus kinase 1 inhibitor. J Med Chem. 2020;63(9):4517–27.
Verstovsek S, Mesa RA, Gotlib J, Levy RS, Gupta V, DiPersio JF, et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med. 2012;366(9):799–807.
Dao KHT, Gotlib J, Deininger MMN, Oh ST, Cortes JE, Collins RH Jr, et al. Efficacy of ruxolitinib in patients with chronic neutrophilic leukemia and atypical chronic myeloid leukemia. J Clin Oncol. 2019;38(10):1006–18.
DiNardo CD, Pratz K, Pullarkat V, Jonas BA, Arellano M, Becker PS, et al. Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood. 2019;133(1):7–17.
Nie J, Liu L, Li X, Han W. Decitabine, a new star in epigenetic therapy: The clinical application and biological mechanism in solid tumors. Cancer Lett. 2014;354:12–20.
Tian J, Lee SO, Liang L, Luo J, Huang CK, Li L, et al. Targeting the unique methylation pattern of androgen receptor (AR) promoter in prostate stem/progenitor cells with 5-aza-2′-deoxycytidine (5-AZA) leads to suppressed prostate tumorigenesis. J Biol Chem. 2012;287(47):39954–66.
Pollyea DA, Winters A, McMahon C, Schwartz M, Jordan CT, Rabinovitch R, et al. Venetoclax and azacitidine followed by allogeneic transplant results in excellent outcomes and may improve outcomes versus maintenance therapy among newly diagnosed AML patients older than 60. Bone Marrow Transplant. 2022;57(2):160–6.
Giovarelli M, Zecchini S, Catarinella G, Moscheni C, Sartori P, Barbieri C, et al. Givinostat as metabolic enhancer reverting mitochondrial biogenesis deficit in Duchenne Muscular Dystrophy. Pharmacol Res. 2021;170:105751.
Locatelli SL, Cleris L, Stirparo GG, Tartari S, Saba E, Pierdominici M, et al. BIM upregulation and ROS-dependent necroptosis mediate the antitumor effects of the HDACi Givinostat and Sorafenib in Hodgkin lymphoma cell line xenografts. Leukemia. 2014;28(9):1861–71.
Kim YH, Bagot M, Pinter-Brown L, Rook AH, Porcu P, Horwitz SM, et al. Mogamulizumab versus vorinostat in previously treated cutaneous T-cell lymphoma (MAVORIC): an international, open-label, randomised, controlled phase 3 trial. Lancet Oncol. 2018;19(9):1192–204.
West AC, Johnstone RW. New and emerging HDAC inhibitors for cancer treatment. J Clin Investig. 2014;124:30–9.
Acknowledgements
Not applicable.
Funding
This work was supported by National Natural Science Foundation of China (82273297), National Science Fund for Excellent Young Scholars (No. 32122052), National Natural Science Foundation Regional Innovation and Development (No. U19A2003).
Author information
Authors and Affiliations
Contributions
Min Luo offered main direction and significant guidance of this manuscript. Zhen Zeng drafted the manuscript. Mingyang Fu illustrated the figures and tables for the manuscript. Yuan Hu revised the manuscript and drafted the point-to-point response letter. Yuquan Wei and Xiawei Wei provided suggestions on the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zeng, Z., Fu, M., Hu, Y. et al. Regulation and signaling pathways in cancer stem cells: implications for targeted therapy for cancer. Mol Cancer 22, 172 (2023). https://doi.org/10.1186/s12943-023-01877-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12943-023-01877-w