Abstract
Background
Contemporary challenges of prostate cancer (PCa) include overdiagnosis and overtreatment, entailing the need for novel clinical tools to improve risk stratification and therapy selection. PCa diagnosis and prognostication might be perfected using epigenetic biomarkers, among which aberrant DNA methylation of microRNA promoters has not been systematically explored. Herein, we identified aberrantly methylated microRNAs promoters in PCa and assessed its diagnostic and prognostic biomarker potential.
Methods
Using HumanMethylation450 BeadChip-based analysis differentially methylated CpGs in microRNA promoters were identified. Promoter methylation of six microRNAs (miR-34b/c, miR-129-2, miR-152, miR-193b, miR-663a and miR-1258) was analyzed by qMSP in three sets (180 prostatectomies, 95 urine sediments and 74 prostate biopsies). Biomarkers’ diagnostic (validity estimates) and prognostic [disease-free (DFS) and disease-specific survival (DSS)] performance was assessed.
Results
Significantly higher promoter methylation levels in PCa were confirmed for six candidate microRNAs. Except for miR-152, all displayed AUC values higher than 0.90, with miR-1258 and miR-193b disclosing the best performance (AUC = 0.99 and AUC = 0.96, respectively). In urine samples, miR-193b showed the best performance (91.6% sensitivity, 95.7% specificity, AUC = 0.96). Moreover, higher miR-129-2 independently predicted for shorter DSS and miR−34b/c methylation levels independently predicted for shorter DFS and DSS.
Conclusions
Quantitative miR-193b, miR-129-2 and miR-34b/c promoter methylation might be clinically useful PCa biomarkers for non-invasive detection/diagnosis and prognostication, both in tissue and urine samples.
Similar content being viewed by others
Background
Prostate cancer (PCa) is the most incident male cancer in western countries, constituting the second most common cause of cancer and the sixth leading cause of death by cancer among men worldwide [1]. For 2012, it was estimated that PCa alone accounted for 420,000 newly diagnosed cancer cases and 101,000 of all cancer-related deaths in European men [2]. PCa is age-related and very heterogeneous, both molecularly and clinically, ranging from relatively indolent to highly aggressive. It is typically asymptomatic at its earliest stages, when adequate treatment is mostly curative, in contrast with its late diagnosis, which usually impairs a curative-intent therapeutic strategy [3]. This led to the widespread use of serum PSA as screening tool for PCa. However, it is now commonly accepted that this entailed overdiagnosis and overtreatment, justifying the strong recommendation against PCa screening and prompting the search for more effective biomarkers [4].
DNA methylation is a chemically stable and easily quantified alteration [5]. We and others have previously reported on the use of quantitative promoter methylation of several protein-coding genes for early diagnosis and prognostication of PCa [6]. Although several gene methylation panels have been then developed [7, 8], both sensitivity and specificity must be perfected to allow for clinical translation.
MicroRNAs, a class of small (19–25 nucleotides) non-coding RNA, are involved in virtually all cellular processes and frequently deregulated in cancer cells [9], although its abrogation due to aberrant promoter methylation has been seldom reported [10]. Because this epigenetic alteration is likely to be highly cancer-specific, it might constitute an effective cancer biomarker. Thus, we aimed to explore the potential of microRNA-coding genes promoter methylation as diagnostic and prognostic biomarkers in PCa. Therefore, after genome-wide screening, a set of putative tumor-suppressor microRNAs (miR-34b/c, miR-129-2, miR-152, miR-193b, miR-663a and miR-1258) with increased promoter methylation levels in PCa compared to normal prostate tissues was identified and further validated in clinical samples.
Methods
Patients and samples collection
For the purposes of this study, three independent cohorts of PCa patients were defined.
PCa tissue samples were prospectively collected from 180 patients with clinically localized disease, consecutively diagnosed and submitted to radical prostatectomy (RP) from 2001 to 2006, at Portuguese Oncology Institute of Porto (Cohort #1). Fifteen control samples were obtained from cystoprostatectomy specimens with bladder cancer, not harbouring PCa nor prostatic involvement by urothelial carcinoma (morphologically normal prostate tissue, MNPT). After collection, tissue samples were fresh-frozen at −80 °C and subsequently cut in a cryostat for DNA extraction. Prostate biopsy samples were collected from 74 PCa suspects (elevated serum PSA), referred to Portuguese Oncology Institute - Porto from 2001 to 2003 (Cohort #2). In addition to standard diagnostic cores, a core was collected from the most suspicious area, fresh-frozen at −80 °C and subsequently cut in a cryostat for DNA extraction.
Voided urine samples from 95 PCa patients were collected from 1999 to 2002 (Cohort #3). The control set is composed of urine samples collected from 17 healthy donors and 29 patients without urological malignancy. Samples were centrifuged at 4,000 rpm for 20 min, washed in PBS 1× and the pellets were frozen at −80 °C.
Clinical data was retrieved from clinical charts. Survival data was collected for patients of Cohort #1 and of Cohort #2. Disease-specific survival (DSS) time was calculated as the time elapsed since diagnosis until death or the last follow-up. Disease-free survival (DFS) was calculated from the date of the radical prostatectomy or other curative treatment to the date of biochemical relapse, date of last follow-up, or death if relapse-free.
All patients enrolled (Tables 1 and 2) signed informed consent. This study was approved by institutional review board (CES-IPOPFG-EPE 019/08 and CES-IPOPFG-EPE 205/2013).
Nucleic acid isolation, bisulphite treatment, HumanMethylation 450 BeadChip and qMSP analysis
DNA extracted by phenol-chloroform as described elsewhere[11] was chemically modified using sodium bisulfite with EZ DNA Methylation-Gold™ Kit (Zymo Research, CA, USA) according to manufacturer’s protocol.
HumanMethylation450 BeadChip (Illumina, USA) allowed for gene methylation profiling of tissue samples (5 controls and 25 tumors), using 500 ng of bisulphite-converted DNA, according to manufacturer’s instructions. DNA methylation levels were depicted as beta-values ranging from 0–1.
Validation of all candidates was performed by quantitative methylation using KAPA SYBR FAST qPCR Kit (Kapa Biosystems, MA, USA). All reactions were run in triplicates in 384-well plates using Roche LightCycler 480 II, with β-actin (ACTB) as internal reference gene for normalization. Primer sequences (Additional file 1: Table S1) were designed using Methyl Primer Express 1.0 and purchased from Sigma-Aldrich (MO, USA).
Statistical analysis
For HumanMethylation 450 BeadChip data, a threshold intensity with P-value ≤ 0.01 was considered for further analysis. To identify consistently differentially methylated CpG sites, Wilcoxon rank sum paired test was performed for normalized beta-values. P-values were adjusted using false discovery rate, and CpGs with P-values <0.05 were selected.
In Cohort #1, pathological variables were categorized [Gleason score (GS): <7 and ≥7; pathological stage: pT2 and pT3]. Kruskall-Wallis and Mann–Whitney U tests allowed for comparisons among three or more groups and between two groups, respectively. For multiple comparisons P values were adjusted according to Bonferroni’s correction. Spearman nonparametric correlation was performed to ascertain association between methylation and PSA serum levels.
In Cohort #1 and Cohort #3, receiver operator characteristics (ROC) curves were constructed by plotting true positive rate (sensitivity) against false positive rate (1-specificity) and area under the curve (AUC) was calculated to assess diagnostic performance. Biomarker validity estimates [specificity, sensitivity, positive predictive value, negative predictive value and accuracy] were determined using as cut-off the highest value obtained through ROC curve analysis [sensitivity + (1-specificity)].
In Cohort #1 and Cohort #2, DSS and DFS curves were built using Kaplan–Meier method and the prognostic significance of clinicopathological variables (clinical stage, GS and serum PSA in both cohorts, and CAPRA Score in Cohort #2) was assessed using log-rank test. CAPRA score values were categorized as 0–2 (low-risk), 3–5 (intermediate risk) and 6–10 (high-risk) [12]. To test the prognostic significance of miR-34b/c and miR-129-2 promoter methylation, samples were categorized based on methylation levels of each miR (using percentile 75 as threshold) [11]. A Cox-regression model comprising all variables (multivariable analysis) was constructed. SPSS Statistics 20 (IBM, NY, USA) was used for all statistical analyses and graphics were assembled using GraphPad 5 Prism (GraphPad Software, CA, USA). P values <0.05 were considered statistically significant.
Results
MicroRNA promoter hypermethylation in Radical Prostatectomy samples (Cohort #1)
Using the 450 K array, we screened microRNA loci regulated by DNA methylation in PCa. The microarray dataset included 5 MNPT and 25 PCa tissue samples. Candidate miRNAs were selected according to adjusted P-values and differences in the methylated fraction between MNPT and PCa tissues. CpG sites displaying statistically significant differences with adjusted P-values and mean methylation <0.3 in MNPT were further considered relevant. Among these, methylation sites located in the promoter region and in proximity to transcription start sites (TSS) [1500 and 200 base pairs upstream of TSS (TSS200; TSS1500 region)] were identified. For the validation study, we selected microRNAs in which significant differences (P < 0.05) in methylation levels were observed at all CpG sites mapped and differences in methylated fractions were >0.12. Thus, six microRNAs - miR-34b/c, miR-129-2, miR-152, miR-193b, miR-663a, and miR-1258 (Fig. 1; Table 3), were selected for large scale validation in 15 MNPT and 180 PCa samples (Cohort #1). In this series, overall methylation levels remained significantly increased in PCa compared with MNPT (Fig. 2), confirming the results of the array analysis.
To assess the diagnostic potential of microRNA promoter methylation in PCa we performed ROC curve analysis (Fig. 2 and Table 4), which revealed AUC values ranging from 0.89 to 0.99, with miR-1258 (AUC = 0.99), miR-193b (AUC = 0.96) and miR-34b/c (AUC = 0.95) demonstrating the best performance. Because AUC for miR-152 was lower than 0.90, it was excluded from further analyses. Concerning validity estimates, miR-1258 promoter methylation levels displayed the highest values (97.8% sensitivity, 100% specificity) for PCa detection. Panels composed by two or more microRNAs did not improve performance (data not shown).
Then, we evaluated whether microRNA promoter methylation levels were associated with clinicopathological parameters. MiR-129-2 promoter methylation was associated with higher GS and pathological stage (P = 0.0248 and P = 0.0245, respectively), whereas, miR-34b/c, miR-663a and miR-1258 promoter methylation levels were only associated with higher pathological stage (P = 0.0055, P = 0.0386 and P = 0.0303, respectively) (Fig. 3).
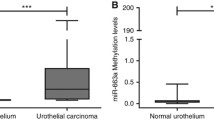
To determine whether microRNA promoter methylation was PCa-specific, malignant and benign tissue samples from bladder (43 and 7) and kidney (50 and 9) were analyzed. MiR-34b/c, miR-193b and miR-1258 promoter methylation levels were significantly higher in PCa tissues compared to all other samples tested. Interestingly, miR-129-2 and miR-663a showed higher methylation levels in bladder cancer and were, thus, considered unsuitable for accurate detection of PCa in urine sediments (Additional file 2: Figure S1).
MicroRNA promoter methylation in urine sediments (Cohort #3)
Best performing PCa-specific microRNAs - miR-34b/c, miR-193b and miR-1258 – were then tested in urine sediments, collected without previous prostatic massage, from PCa patients (n = 95, Cohort #3) and controls (n = 46). Higher miR-34b/c and miR-193b methylation levels and lower miR-1258 promoter methylation levels were depicted in PCa patients (Fig. 4). MiR-193b promoter methylation displayed the best performance with high sensitivity (91.6%) and specificity (95.7%), providing an overall accuracy of 92.9% (AUC = 0.96). Moreover, the panel including both miRs (miR-34b/c, miR-193b) augmented specificity (97.8%) and positive predictive value (98.9%) (Table 5). Addition of miR-34b/c promoter methylation did not improve biomarker performance. No associations between microRNAs’ promoter methylation levels and clinicopathological parameters were depicted in this series.
Box-plots and ROC curves of miR-34b/c, miR-193b and miR-1258 promoter methylation levels across urine sediments of controls (HD) and prostate cancer patients (PCa) from Cohort #3. Receiver operator characteristic (ROC) curves were constructed to evaluate the performance of the gene promoter methylation panel (miR-34b/c+miR-193b)
MicroRNA promoter methylation as prognostic biomarker (Cohorts # 1 & # 2)
Owing to its association with stage and GS, the prognostic value of miR-34b/c and miR-129-2 promoter methylation was further tested in the set of 180 radical prostatectomy (Cohort #1) and in a prospective group of 74 PCa suspects (Cohort #2).
The median follow-up in Cohort #1 was 110.1 months (range: 2.8–169.1 months). Nine patients (5%) had died from PCa and 50 (28%) developed biochemical recurrence. Eighteen were never free of disease and were excluded from DFS analysis. In this cohort, pathological stage, GS and PSA levels significantly associated with DFS (Fig. 5A), whereas, only pathological stage and higher GS statistically associated with worse DSS (Fig. 6A). Remarkably, high miR-129-2 methylation levels associated with shorter DSS. In multivariable analysis, only GS and PSA levels for DFS and GS and miR-129-2 methylation for DSS retained prognostic value (Table 6).
a - Disease-free survival (DFS) curves based on pathological stage (upper left panel) and Gleason score (upper right panel), and miR-129-2 methylation levels (lower panel) in Cohort #1. b - Disease-free survival (DFS) curves based on clinical stage (upper left panel) and Gleason score (upper right panel), miR-34b/c (lower left) and miR-129-2 (lower right) methylation levels in Cohort #2
A - Disease-specific survival (DSS) curves based on pathological stage (upper left), Gleason Score (upper right), and miR-129-2 methylation levels (lower) in Cohort #1. B - Disease-specific survival (DSS) curves based on clinical stage (upper left), Gleason Score (upper center) CAPRA Score (upper left), miR-34b/c (lower left) and miR-129-2 (lower-right) methylation levels in Cohort #2
Regarding Cohort #2, the median follow-up was 114.9 months (range: 10.3–170.1 months). Thirteen patients (17.6%) had died from PCa and 29 (39.2%) developed biochemical recurrence. In 3 patients, serum PSA levels >0.2 ng/ml persisted following treatment and these were not further considered for DFS analysis. Advanced clinical stage, higher GS, higher miR-34b/c and miR-129-2 promoter methylation levels statistically associated with worse DFS (Fig. 5B). In multivariable analysis only higher clinical stage and high miR-34b/c promoter methylation levels independently predicted shorter DFS (Table 6). Except for serum PSA, all clinicopathological parameters tested, as well as miR-34b/c and miR-129-2 promoter methylation levels associated with DSS in univariable analysis (Fig. 6B). Similarly to DFS, in multivariable analysis only clinical stage and high miR-34b/c promoter methylation levels independently predicted shorter DSS (Table 6).
Discussion
PCa remains one of the most prevalent neoplasms and a leading cause of morbidity and mortality in men. Although PSA screening has decreased the number of men diagnosed with metastatic PCa, this was accomplished at the cost of overdiagnosis and overtreatment of a sizeable proportion of men carrying indolent/non-life threatening tumors [13]. Thus, a strong recommendation against serum PSA-based PCa screening has been issued [14], prompting the search for more effective biomarkers allowing for better risk stratification of PCa suspects. Herein, we aimed to tackle this clinical quest through discovery and preliminary validation of novel biomarkers for PCa detection and prognostication, using methylation analysis of microRNAs gene promoters.
Owing to our previous experience in DNA methylation analysis of PCa [6, 11], we searched for altered methylation patterns at the promoter regions of microRNAs deregulated in PCa. This information was then used to develop novel biomarkers, instead of microRNA expression levels, as previously attempted by other researchers [15]. Indeed, DNA methylation is easier to assess than microRNA expression, it is more specific and, importantly, more stable. Moreover, because microRNAs downregulation in cancer is more common than upregulation, it seemed likely that aberrant promoter methylation might constitute an underlying mechanism, similar to protein-coding genes [16]. Although several strategies might be used to identify microRNAs putatively downregulated due to promoter hypermethylation, high-throughput technologies such as methylation-array analysis are able to simultaneously pinpoint putative candidates [17] and the reliability of the results might be readily assessed through analysis of well-known hypermethylated loci. Indeed, results of the methylation array experiments confirmed the high prevalence of GSTP1 and APC promoter methylation (data not shown), as we previously demonstrated in PCa [18]. To increase the likelihood of finding robust candidate biomarkers, we used stringent conditions based on high fold-variation of methylation levels between cancerous and non-cancerous tissue samples. From methylation-array analysis, six candidate microRNAs, putatively deregulated by promoter hypermethylation were identified. MiR-1258, miR-193b and miR-34b/c were the most promising candidates, displaying substantial PCa-specificity compared with other urinary tract tumors, an attractive feature for testing in bodily fluids. MiR-129-2 and miR-663a showed modest results and their inability to discriminate PCa from bladder cancer rendered it unsuitable for testing in urine samples.
Association between promoter methylation levels in tumor tissue samples and standard clinicopathological variables was also assessed. Higher miR-129-2 promoter methylation levels associated with higher GS and stage, suggesting prognostic value. MiR-34b/c, miR-663a and miR-1258 methylation levels also associated with pathological stage, but higher diagnostic performance underscores the potential for detecting PCa at early stages instead of prognostication, as we previously reported for EFEMP1 promoter methylation [19]. Nevertheless, in this series of radical prostatectomies (Cohort #1) higher miR-129-2 methylation conveyed independent prognostic information, although only for DSS. Importantly, these results are in line with previous observations concerning the association of higher gene promoter methylation levels with clinicopathological features of more aggressive disease [11, 20].
Urine is a key sample to evaluate DNA methylation biomarkers for PCa, as it is readily collected and biomarkers are diluted to a smaller extent than in plasma, providing higher sensitivity[21]. Nevertheless, the amount of DNA potentially deriving from prostatic cells is variable, usually low, entailing the use of a panel with limited number of biomarkers. Thus, only miR-34b/c, miR-193b and mir-1258, were tested in urine samples (Cohort #3). From these, Mir-193b was previously shown to be aberrantly methylated in PCa cell lines as well as in primary tumors, but no data is available regarding its performance as PCa detection biomarker [22, 23]. Indeed, Mir-193b performed best, with high AUC, sensitivity, specificity and PPV, whereas miR-34b/c performance was more modest.
Intriguingly, miR-1258, which showed the best performance in tissue samples (Cohort #1), displayed a strikingly different result in urines as its methylation levels were higher in controls than in PCa patients. The reason for this discrepant result is not immediately apparent, but it might be due to high miR-1258 promoter methylation in non-epithelial cells, such as leucocytes, which are relatively more abundant in urine than in tumor tissue samples. Moreover, median miR-1258 promoter methylation levels in urines from PCa were substantially inferior to those of miR-193b, impairing the robustness of the assay. It should be recalled that, contrarily to other studies, the urine samples we used were not collected following DRE or prostatic massage, which are usually employed in an attempt to increase sensitivity. Studies dealing with PCa biomarkers in urine vary in the method of urine collection and the real impact of prostatic massage has never been evaluated [24]. It could be argued that the distance from the peripheral zone to the urinary tract flow may render urinary based tests less sensitive, which would be an important issue since most malignancies arise from this zone. Nevertheless, studies on PCA3 did not find a difference in the levels of this biomarker between patients with peripheral versus transitional zone PCa [25, 26].
Currently, the performance of serum PSA and urinary PCA3, the only biomarkers approved for clinical use is rather limited. The reported performance of serum PSA as PCa biomarker is somewhat modest, with AUC ranging from 0.54 to 0.70 [27, 28]. Even other serum PSA-derived measurements, like PSA-density, free PSA percentage and PSA-velocity have not significantly improved performance [28]. Nonetheless, PCA3, which was reported to perform better than serum PSA both in urine and ejaculates but has not been approved for population-based screening, displays AUCs varying from 0.66 to 0.79 [27–30]. Additionally, although miRs’ expression has been extensively investigated in liquid biopsies, available data for urine samples is rather limited. Nevertheless, an AUC of 0.74 was reported for miR-107 [31] and simultaneous quantification of miR-107 and miR-574-3p in urine showed an AUC of 0.83, for PCa cancer detection [32]. We should emphasize that in our dataset, urinary miR-193b promoter methylation (AUC = 0.96) outperformed not the only currently approved clinical biomarkers, but also the previously mentioned miRs, constituting a promising tool for non-invasive PCa detection.
Because a major goal of this study was to discriminate clinically aggressive from indolent PCa, it was critical to test the prognostic value of microRNAs in a pre-therapeutic setting, which was accomplished in series of prospectively collected prostate biopsies (Cohort #3). In univariable analysis, most standard clinicopathological parameters associated with DFS and DSS, clinically validating this dataset. The same was demonstrated for higher miR-129-2 and miR-34b/c promoter methylation levels. The CAPRA score, however, only associated with DSS but not DFS. This was unexpected as its determination at diagnosis associated with DFS in patients with clinically localized disease submitted to RP [12]. Notwithstanding, our prostate biopsy series included PCa at diverse clinical stages, submitted to different therapeutic modalities (RP, radiotherapy, androgen-deprivation therapy), which might explain the apparent flaw of CAPRA score. In multivariable analysis, only clinical stage, amongst all clinicopathological parameters, retained independent prognostic value, both for DFS and DSS. Remarkably, high miR-34b/c promoter methylation levels also predicted shorter DFS and DSS, suggesting that it might constitute a useful PCa prognostic biomarker. These results suggest that high miR-34b/c promoter methylation levels identify clinically aggressive PCa, irrespective of disease extent at diagnosis.
It should be acknowledged that in spite of the excellent diagnostic performance of miR-193b promoter methylation in urine, additional patient sets must be tested. Furthermore, a larger cohort of patients submitted to biopsy and subjected to different therapies is required to further validate our observations. Ultimately, we plan to develop a multiplex assay to simultaneously assess miR-193b, miR-129-2 and miR34b/c promoter methylation, allowing for diagnostic and prognostic assessment of PCa suspects in a single analysis.
Conclusion
Through genome-wide screening, a set of methylation-based PCa biomarkers was identified and validated. MiR-193b demonstrated high sensitivity and specificity for detection of PCa, both in tissue and urine, whereas high miR-129-2 and miR-34b/c methylation levels independently predicted for shorter DSS and DFS or DSS, respectively. If confirmed in larger and independent datasets, quantitative promoter methylation of selected miRs might provide useful tools for clinical management of PCa patients. The authors would like to extend their appreciation to all the patients and control subjects that kindly provided the biological samples for this study.
Abbreviations
- ACTB:
-
β-actin
- ADT:
-
Androgen deprivation therapy
- APC:
-
Adenomatous polyposis coli
- AUC:
-
Area under the curve
- BlCa:
-
Bladder cancer
- CAPRA:
-
Cancer of the Prostate Risk Assessment
- CI:
-
Confidence interval
- DFS:
-
Disease-free survival
- DNA:
-
Deoxyribonucleic acid
- DSS:
-
Disease-specific survival
- EFEMP1:
-
EGF-containing fibulin-like extracellular matrix protein 1
- GS:
-
Gleason score
- GSTP1:
-
Glutathione S-transferase P
- HD:
-
Healthy donnors
- HR:
-
Hazard ratio
- MNPT:
-
Morphologically normal prostate tissue
- NBl:
-
Normal bladder
- NK:
-
Normal kidney
- NPV:
-
negative predictive value
- PBS:
-
Phosphate-buffered saline
- PCa:
-
Prostate cancer
- PCA3:
-
Prostate cancer antigen 3
- PPV:
-
Positive predictive value
- PSA:
-
Prostate-specific antigen
- RCT:
-
Renal cell tumor
- RNA:
-
Ribonucleic acid
- ROC:
-
Receiver operator characteristics
- RP:
-
Radical prostatectomy
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29.
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–386.
Hammerich K, Ayala GE, TM W. Anatomy of the prostate gland and surgical pathology of prostate cancer. In: Prostate Cancer Edited by Hedvig Hricak and Peter T. Scardino. Cambridge: Cambridge University Press; 2009. p. 1–14.
Costa-Pinheiro P, Patel HR, Henrique R, Jeronimo C. Biomarkers and personalized risk stratification for patients with clinically localized prostate cancer. Expert Rev Anticancer Ther. 2014;14:1349–58.
Duffy MJ, Napieralski R, Martens JW, Span PN, Spyratos F, Sweep FC, Brunner N, Foekens JA, Schmitt M, Group EP. Methylated genes as new cancer biomarkers. Eur J Cancer. 2009;45:335–46.
Jeronimo C, Henrique R. Epigenetic biomarkers in urological tumors: A systematic review. Cancer Lett. 2014;342:264–74.
Harden SV, Sanderson H, Goodman SN, Partin AA, Walsh PC, Epstein JI, Sidransky D. Quantitative GSTP1 methylation and the detection of prostate adenocarcinoma in sextant biopsies. J Natl Cancer Inst. 2003;95:1634–7.
Baden J, Adams S, Astacio T, Jones J, Markiewicz J, Painter J, Trust C, Wang Y, Green G. Predicting prostate biopsy result in men with prostate specific antigen 2.0 to 10.0 ng/ml using an investigational prostate cancer methylation assay. J Urol. 2011;186:2101–6.
Chen QW, Zhu XY, Li YY, Meng ZQ. Epigenetic regulation and cancer (review). Oncol Rep. 2014;31:523–32.
Lopez-Serra P, Esteller M. DNA methylation-associated silencing of tumor-suppressor microRNAs in cancer. Oncogene. 2012;31:1609–22.
Henrique R, Ribeiro FR, Fonseca D, Hoque MO, Carvalho AL, Costa VL, Pinto M, Oliveira J, Teixeira MR, Sidransky D, Jeronimo C. High promoter methylation levels of APC predict poor prognosis in sextant biopsies from prostate cancer patients. Clin Cancer Res. 2007;13:6122–9.
Cooperberg MR, Broering JM, Carroll PR. Risk assessment for prostate cancer metastasis and mortality at the time of diagnosis. J Natl Cancer Inst. 2009;101:878–87.
Chiam K, Ricciardelli C, Bianco-Miotto T. Epigenetic biomarkers in prostate cancer: Current and future uses. Cancer Lett. 2014;342:248–56.
Moyer VA, Force USPST. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157:120–34.
Lichner Z, Fendler A, Saleh C, Nasser AN, Boles D, Al-Haddad S, Kupchak P, Dharsee M, Nuin PS, Evans KR, et al. MicroRNA signature helps distinguish early from late biochemical failure in prostate cancer. Clin Chem. 2013;59:1595–1603.
Suzuki H, Maruyama R, Yamamoto E, Kai M. DNA methylation and microRNA dysregulation in cancer. Mol Oncol. 2012;6:567–78.
Gallego-Fabrega C, Carrera C, Muiño E, Montaner J, Krupinski J, Fernandez-Cadenas I. DNA methylation levels are highly correlated between pooled samples and averaged values when analysed using the Infinium HumanMethylation450 BeadChip array. Clin Epigenetics. 2015;7:48.
Valdes-Mora F, Clark SJ. Prostate cancer epigenetic biomarkers: next-generation technologies. Oncogene. 2015;34:1609–18.
Almeida M, Costa VL, Costa NR, Ramalho-Carvalho J, Baptista T, Ribeiro FR, Paulo P, Teixeira MR, Oliveira J, Lothe RA, et al. Epigenetic regulation of EFEMP1 in prostate cancer: biological relevance and clinical potential. J Cell Mol Med. 2014;18:2287–97.
Kristensen H, Haldrup C, Strand S, Mundbjerg K, Mortensen MM, Thorsen K, Ostenfeld MS, Wild PJ, Arsov C, Goering W, et al. Hypermethylation of the GABRE ~ miR-452 ~ miR-224 promoter in prostate cancer predicts biochemical recurrence after radical prostatectomy. Clin Cancer Res. 2014;20:2169–81.
Thuret R, Chantrel-Groussard K, Azzouzi AR, Villette JM, Guimard S, Teillac P, Berthon P, Houlgatte A, Latil A, Cussenot O. Clinical relevance of genetic instability in prostatic cells obtained by prostatic massage in early prostate cancer. Br J Cancer. 2005;92:236–40.
Kaukoniemi KM, Rauhala HE, Scaravilli M, Latonen L, Annala M, Vessella RL, Nykter M, Tammela TL, Visakorpi T. Epigenetically altered miR-193b targets cyclin D1 in prostate cancer. Cancer Med. 2015;4:1417–25.
Rauhala HE, Jalava SE, Isotalo J, Bracken H, Lehmusvaara S, Tammela TL, Oja H, Visakorpi T. miR-193b is an epigenetically regulated putative tumor suppressor in prostate cancer. Int J Cancer. 2010;127:1363–72.
Truong M, Yang B, Jarrard DF. Toward the detection of prostate cancer in urine: a critical analysis. J Urol. 2013;189:422–9.
Muller H, Brenner H. Urine markers as possible tools for prostate cancer screening: review of performance characteristics and practicality. Clin Chem. 2006;52:562–73.
Nakanishi H, Groskopf J, Fritsche HA, Bhadkamkar V, Blase A, Kumar SV, Davis JW, Troncoso P, Rittenhouse H, Babaian RJ. PCA3 molecular urine assay correlates with prostate cancer tumor volume: implication in selecting candidates for active surveillance. J Urol. 2008;179:1804–9. discussion 1809–1810.
Ploussard G, de la Taille A. Urine biomarkers in prostate cancer. Nat Rev Urol. 2010;7:101–9.
Prensner JR, Rubin MA, Wei JT, Chinnaiyan AM. Beyond PSA: the next generation of prostate cancer biomarkers. Sci Transl Med. 2012;4:127rv123.brs.
Chevli KK, Duff M, Walter P, Yu C, Capuder B, Elshafei A, Malczewski S, Kattan MW, Jones JS. Urinary PCA3 as a predictor of prostate cancer in a cohort of 3,073 men undergoing initial prostate biopsy. J Urol. 2014;191:1743–8.
Roberts MJ, Chow CW, Schirra HJ, Richards R, Buck M, Selth LA, Doi SA, Samaratunga H, Perry-Keene J, Payton D, et al. Diagnostic performance of expression of PCA3, Hepsin and miR biomarkers inejaculate in combination with serum PSA for the detection of prostate cancer. Prostate. 2015;75:539–49.
Bryant RJ, Pawlowski T, Catto JW, Marsden G, Vessella RL, Rhees B, Kuslich C, Visakorpi T, Hamdy FC. Changes in circulating microRNA levels associated with prostate cancer. Br J Cancer. 2012;106:768–74.
Stuopelyte K, Daniunaite K, Bakavicius A, Lazutka JR, Jankevicius F, Jarmalaite S. The utility of urine-circulating miRNAs for detection of prostate cancer. Br J Cancer. 2016;115:707–15.
Acknowledgments
The authors are grateful to Mª Conceição Martins, BSc for the skilful technical support and would like to acknowledge to the Departments of Urology and Laboratory Medicine of the Portuguese Oncology Institute of Porto for their collaboration in urine collection.
Funding
The authors would like to acknowledge funding attributed to this study, namely research grants from Research Center of Portuguese Oncology Institute of Porto (CI-IPOP 4–2012; CI-IPOP 19–2016)) and by Federal funds through Programa Operacional Temático Factores de Competitividade (COMPETE) with co-participation from the European Community Fund (FEDER) and by national funds through Fundação para a Ciência e Tecnología (FCT) under the projects EXPL/BIM-ONC/0556/2012. JRC was supported by a FCT-Fundação para a Ciência e a Tecnologia fellowship (SFRH/BD/71293/2010).
Availability of data and materials
Not applicable.
Authors’ contributions
Conceived and designed the experiments: JR-C, RH, CJ. Performed the Experiments: JT-F, JR-C, AG, FDM, RF, JO, ME. Analyzed the data: J T-F, JR-C, LA, AG, RH, CJ. Contributed reagents/material/analysis: JT-F, LA, JO, RF, RH, CJ. All authors read and approved the final manuscript.
Competing interests
None of the authors have any conflict of interest to declare.
Consent for publication
All authors have agreed to publish this manuscript.
Ethics approval and consent to participate
All patients enrolled signed informed consent. This study was approved by institutional review board (CES-IPOPFG-EPE 019/08 and CES-IPOPFG-EPE 205/2013).
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1: Table S1.
Primer sequences used for reference gene and each microRNA promoter methylation analysis. (DOC 28 kb)
Additional file 2: Figure S1.
Distribution of miR’s promoter methylation levels in prostatic, vesical and renal tissues. MNPT - morphologically normal prostatic tissue; PCa - prostate cancer; NBl - normal bladder; BlCa - bladder cancer; NK - normal kidney; RCT – renal cell tumor. (TIF 1338 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Torres-Ferreira, J., Ramalho-Carvalho, J., Gomez, A. et al. MiR-193b promoter methylation accurately detects prostate cancer in urine sediments and miR-34b/c or miR-129-2 promoter methylation define subsets of clinically aggressive tumors. Mol Cancer 16, 26 (2017). https://doi.org/10.1186/s12943-017-0604-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12943-017-0604-0