Abstract
Background
Colistin resistance is mainly driven by alterations in the Gram-negative outer membrane lipopolysaccharides and is caused, in most cases, by mutations in mgrB gene. However, the recent emergence of plasmid-encoded colistin resistance among Enterobacteriaceae strains represents a serious threat to global public health. In this paper we have investigated the rates of colistin resistance and the underlying mechanisms in 450 Klebsiella pneumoniae and Escherichia coli isolates obtained from cancer patients in Egypt.
Methods
Colistin susceptibility and minimum inhibitory concentrations were determined according to the European Committee on Antimicrobial Susceptibility Testing, by broth microdilution, and by E-test. The mcr-1, mcr-2 and mgrB genes were detected by PCR and then sequenced. Clonal diversity in colistin-resistant K. pneumoniae was evaluated by multilocus sequence typing.
Results
Forty (8.8%) colistin-resistant isolates, including 22 K. pneumoniae and 18 E. coli, were isolated over 18 months. Of these, 50% were carbapenem-resistant, out of which nine were blaOXA-48 and seven blaNDM-1 positive. The mechanisms of colistin resistance could be revealed only in three of the 40 resistant strains, being represented by mcr-1 in one blaNDM-1-positive E. coli strain and in one K. pneumoniae ST11 and by mgrB mutations, detected in one K. pneumoniae isolate. None of the studied isolates harbored mcr-2.
Conclusions
Our results demonstrate a high frequency of colistin resistance in enterobacterial strains isolated from cancer patients, but a low prevalence of the most well known resistance mechanisms.
Similar content being viewed by others
Introduction
Antibiotic resistance is one of the most important public health issues worldwide. Severe infections due to multidrug-resistant bacteria, mainly carbapenem-resistant bacteria, in addition to lack of new antibiotics against gram-negative pathogens, have led to a reevaluation of old antibiotics [1]. In this light, colistin has gained clinical value as a last-line drug against serious bacterial infections, since it is effective against nearly all multidrug-resistant gram-negative bacteria. However, a gradual increase in the prevalence of colistin resistance has been noted in the last few years, and elucidation of underlying resistance mechanisms is critical.
Structural modifications of bacterial lipopolysaccharide are the main routes of colistin resistance in gram-negative bacteria. These modifications include addition of 4-amino-4-deoxy-l-arabinose or phosphoethanolamine following chromosomal mutations in genes encoding the two-component systems PhoPQ and PmrAB, or in mgrB, a negative regulator of PhoPQ [2]. The phosphoethanolamine transferase mcr-1, a recently identified horizontally transferable plasmid-mediated colistin resistance gene, is also worrisome, as it has been detected in over 20 countries within 3 months of its identification [2], including in Europe, Asia, South America, North America, and Africa [3,4,5,6,7]. In China, mcr-1 was detected in as many as 20% of animal strains and 1% of human strains [8]. Colistin resistance is most frequently observed in E. coli, but is present in various genera, including Escherichia, Klebsiella, Salmonella, Shigella, and Enterobacter [1]. In Egypt, mcr-1 was first reported in 2016 in an E. coli isolate recovered from the sputum of one patient [9]. The mcr-1 gene product adds phosphoethanolamine to the 4′ position of the lipid A moiety of lipopolysaccharides in the outer leaflet of the bacterial outer membrane, significantly reducing the affinity to colistin [10].
Subsequently, Wang et al. [11] described several other MCR homologs (MCR-2, MCR-3, MCR-4, and MCR-5. Two MCR homologs (MCR-6 and MCR-7) were placed into GenBank, and very recently, the mcr-7.1 gene was found in K. pneumoniae of chicken origin in China. mcr-2, which has about 76.7% nucleotide and 81% amino acid identity to mcr-1, the archetypal form. Hence, mcr-2 is a similar threat to public health as mcr-1, although its transfer, origin, and mechanism of resistance are not fully understood [12]. We have now evaluated the rates of colistin resistance in clinical enterobacterial infectious isolates from tertiary Cancer Hospital in Cairo, Egypt, to assess the presence of mcr-1 and mcr-2, as well as of mutations in mgrB.
Materials and methods
The study was conducted between January 2016 and June 2017 at the National Cancer Institute, Cairo University, Egypt, with approval from the local Ethical Committee. Enterobacterial samples described in this paper are from cultures obtained by the microbiology and clinical pathology department as part of routine care for hospitalized infected cancer patients. No additional clinical specimens were obtained for purposes of research; therefore, informed consent was not required.
Sample collection
Clinical samples were cultured on blood agar and MacConkey agar (Oxoid Co., England). Isolates were identified by standard microbiological techniques (Colonial morphology, Gram stain, oxidase and the use of several biochemical tests) andVITEK-2 Compact system (bioMerieux, Marcy l’E´toile, France), using E. coli ATCC 25922 as control strain. A total of 450 K. pneumoniae and E. coli strains were recovered.
Susceptibility testing, detection of ESBL, and determination of minimum inhibitory concentrations
Susceptibility to ampicillin/sulbactam, piperacillin/tazobactam, cefazolin, cefoxitin, ceftazidime, ceftriaxone, cefepim, meropenem, amikacin, gentamicin, tobramycin, ciprofloxacin, levofloxacin, and trimethoprim/sulfamethoxazole was determined by VITEK 2 Compact system. Susceptibility to colistin and tigecycline was evaluated by agar dilution method based on clinical break points defined by the European Committee on Antimicrobial Susceptibility Testing [13]. Minimum inhibitory concentrations for colistin were also measured by broth micro-dilution according to the same standards [13], as well as on E-test strips (bioMérieux, Marcy l’Etoile, France).
Multilocus sequence typing
Colistin-resistant K. pneumoniae isolates were typed by multilocus sequence typing, following the scheme established by the Pasteur Institute (www.pasteur.fr/mlst/Kpneumoniae.html; [14), which is based on the housekeeping genes gapA, infB, mdh, pgi, phoE, rpoB, and tonB.
Characterization of mcr-1 and mcr-2
Total DNA was extracted by Qiagen DNeasy DNA Extraction Kit (QIAGEN, Crawley, UK) from cultures left at 37 °C overnight in Luria–Bertani (LB) media. Isolates were identified by PCR amplification and sequencing of 16S rRNA, as previously described [15]. Isolates were tested by PCR for plasmid-encoded mcr-1, using primers CLR5-F (5′-CGGTCAGTCCGTTTGTTC-3′) and CLR5-R (5-CTTGGTCGGTCTGTAGGG-3′), as previously described [8]. Similarly, isolates were tested by PCR for mcr-2, using mcr-2 full Fw (5′-ATGACATCACATCACTCTTGG-3′) and mcr-2 full Rv (5′-TTACTGGATAAATGCCGCGC-3′) as previously described [16]. Amplified DNA fragments were purified using QIAquick PCR Purification Kit (QIAGEN, Crawley, UK) and sequenced in both directions. Nucleotide and deduced amino acid sequences were analyzed and compared by BLAST, as implemented by the National Center for Biotechnology Information web site (http://blast.ncbi.nlm.nih.gov/Blast.cgi).
Detection of carbapenem resistance genes
Isolates were screened for the carbapenemases NDM, VIM, IMP, SIM, GIM, SPM, OXA-48, and KPC by multiplex PCR, as previously described [17, 18].
Analysis of mgrB
Using primers mgrB-F (5′-AAGGCGTTCATTCTACCACC-3′) and mgrB-R (5′-TTAAGAAGGCCGTGCTATCC-3′), mgrB was amplified and sequenced in both directions to detect genetic alterations that may drive colistin resistance [19].
Results
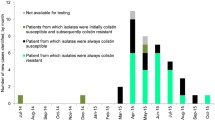
A total of 450 enterobacterial isolates (234 K. pneumoniae, 200 E. coli, and 16 Enterobacter) were collected from hospitalized cancer patients between January 2016 and June 2017, of whom 252 (56%) were males and 198 (44%) were females with age ranges from 1 to < 18 years (pediatrics) (37%), ≤ 55 years (35%) and > 55 years (28%). 440 had received antibiotics 1 month before isolating colistin-resistant Enterobacterial isolate, but none of them had been given colistin. The majority of isolates were from bloodstream infections (n = 263). None of the patients indicated travel within the preceding 12 months. Resistance to cefazolin (414/450; 92%), ceftriaxone (410/450; 91%), ceftazidime (400/450; 89%), cefepime (390/450; 86.5%), trimethoprim/sulfamethoxazole (383/450; 85%), ampicillin/sulbactam (378/450; 84%), levofloxacin (330/450; 73.5%), piperacillin/tazobactam (326/450; 72.5%), ciprofloxacin (321/450; 71.5%), meropenem (240/450; 53.5%), and tobramycin (231/450; 52%) were common, while resistance to gentamycin (202/450; 45%), amikacin (173/450; 38%), and tigecycline (45/450; 10%) was less common (Table 1). As tested by broth microdilution, 40 isolates were resistant to colistin (8.8%), of which 18 (45%) were meropenem-resistant. Similarly, E-tests showed that 36/450 (8%) of isolates were colistin-resistant. Finally, analysis on a VITEK 2 system showed that 140/450 (31%) of isolates produced extended-spectrum beta-lactamase. PCR screening for the most widespread carbapenemases revealed that 16 of the 40 colistin-resistant isolates harbored carbapenemases, with 9/40 positive for blaOXA-48 and 7/40 positive for blaNDM-1. No other carbapenemases (KPC, VIM, IMP, SIM, GIM, and SPM) were detected.
Mutilocus sequence typing of colistin-resistant K. pneumoniae revealed seven ST101 strains and three ST383 isolates. Two isolates each of ST147, ST11, ST16, and ST1399 were also detected, along with one isolate each of ST22, ST37, ST785, and ST2193 (Table 2).
Genotypic surveys for plasmid-encoded mcr-1 and mcr-2 showed that two of 40 (5%) colistin-resistant isolates harbor mcr-1, including one of 18 E. coli isolates and one of 22 K. pneumoniae isolates, which is ST11. These genes were 100% identical to the known mcr-1 sequence (Genbank: NG_050417.1, Liu et al., 2016). The minimum inhibitory concentrations for colistin was 4 mg/L for both isolates. mcr-2 was not detected.
Sequencing of the PhoP/PhoQ regulator mgrB in 25 select isolates revealed a missense mutation in only one (4%) colistin-resistant K. pneumoniae, the genotype of which was ST1399. This mutation (GCC > GAC) mutates proline 178 to tyrosine. Two additional silent mutations were observed with high confidence in this isolate, namely a TAA > CAA mutation at position 144 and a TCC > CCC mutation at position 156. All other isolates harbor wild-type mgrB (Fig. 1).
Discussion
Colistin has become the only viable antimicrobial against aggressive infections due to multidrug-resistant bacteria, and the emergence of plasmid-mediated colistin resistance in Enterobacteriaceae severely compromises its use [10]. Hence, we surveyed colistin resistance rates in multidrug-resistant K. pneumoniae and E. coli isolated from hospitalized cancer patients at National Cancer Institute, Cairo, Egypt. National Cancer Institute is a tertiary referral hospital, so patients come from different governates in Egypt. The underlying mechanisms driving colistin resistance were investigated by amplification and sequencing of chromosomal mgrB and plasmid-encoded mcr-1 and mcr-2. In the current study, a total of 450 clinical isolates were recovered from cancer patients with hematological malignancies and solid tumors during the study period. More than half of the isolates were obtained from blood stream infections (58%). Gram-negative bacilli causing blood stream infections are frequently detected in cancer patients, and are associated with high mortality. Bacterial bloodstream infections are the leading in case of infectious complications in the course of neutropenia in cancer patients [20]. In line with other studies conducted worldwide, 8.8% of isolates were colistin-resistant, as assessed by broth microdilution. E-test and broth microdilution results were consistent in 36 cases, but the former failed to detect colistin resistance in four isolates, highlighting the reliability of the latter as a reference method for testing colistin susceptibility. Indeed, broth microdilution was found to be the most reliable method for testing colistin susceptibility, as colistin resistance is underestimated by other methods such as agar dilution and disk diffusion. Colistin-resistant K. pneumoniae was reported in eastern India [21], and at frequencies of 5.8% and 6.6% in Lao PDR and Thailand, respectively [22]. Similarly, minimum inhibitory concentrations of 3–64 mg/L were reported in 2.4% and 0.7% of isolates in France and Nigeria [22]. mcr-1 was first detected in human isolates in 2011 in Denmark, Germany, Italy, the Netherlands, Spain, Sweden, and the United Kingdom [23]. mcr-1 has since been detected in clinical isolates in Malaysia [7], South Africa [24], Egypt [9], the US [25], and China [26, 27]. Accordingly, this plasmid-encoded gene is of special concern to public health, because it is more easily transmissible than chromosomal colistin resistance genes. In our samples, mcr-1 was present in only two (5%) isolates (E. coli and K. pneumoniae), implying that colistin resistance is mainly due to chromosomal elements. The minimum inhibitory concentration was 4 µg/mL for both. The E. coli isolate, recovered from the site of surgery in a patient, was also carbapenem-resistant, with minimum inhibitory concentration 8 µg/mL. In addition, this isolate harbored the metallo-β-lactamase gene blaNDM-1. On the other hand, the K. pneumoniae isolate, obtained from a patient with bacteremia, did not harbor carbapenemase genes. Since colistin is not used in the hospital to treat community-acquired infections, this may account for the low prevalence of mcr.
mcr-2 was not detected at all, in line with other studies. Indeed, mcr-2 was detected only in Belgium [28], indicating that it is probably dispersed via a different mechanism as mcr-1 [28]. Another possibility is that mcr genes are not transmitted from animal and environmental strains to human strains. Additionally, reproducibility of tests for polymyxin/colistin resistance, as well as inconsistencies between assays, as we and others have noted, may hinder detection of isolates with mcr-1 and mcr-2 [29]. Future work will be conducted to screen the other mcr variants (mcr-3, mcr-4 and mcr-5) in infectious enterobacterial isolates recovered from cancer patients.
Cancer patients are frequently subjected to prolonged antibiotic therapy due to neutropaenia. Proven enterobacterial infection requires adminstration of antimicrobial therapy for up to 10 days; this increases the rates of resistance to antimicrobials. High rates of antimicrobial resistance were observed in our samples. For example, 53.5% of isolates were meropenem-resistant. Carbapenem resistance was mediated primarily by blaOXA-48 (9/40) and blaNDM-1 (7/40), which are the most common carbapenemases in Egypt [30]. Other carbapenemases (KPC, VIM, IMP, SIM, GIM, and SPM) were not detected. In contrast, resistance to tigecycline was rarer (10%), although increasing use of tigecycline to treat life-threatening infections may eventually escalate resistance rates among multidrug-resistant gram negative bacteria. Importantly, the resistance phenotypes of the studied colistin resistant isolates were not identical therefore each isolate was different.
Analysis of mgrB in 25 selected colistin-resistant isolates identified 13 with wild-type mgrB and one with a missense mutation in mgrB. The gene was not detected in the remaining 11 isolates (Table 2). Although the apparently minor role of mgrB mutations in colistin resistance among our isolates was unexpected, we note that operons involved in lipopolysaccharide modification are regulated by determinants other than PmrB/MgrB, such as CrrABTCRS [31]. Alternatively, other resistance mechanisms such as accumulation of capsular polysaccharide or efflux pumps may contribute to resistance [32].
Colistin-resistant K. pneumoniae isolates in our collection belong to various clones, as assessed by multilocus sequence typing, suggesting considerable genetic diversity present in the same hospital. Of these, ST101 is a major drug-resistant strain, not only in Egypt, but also worldwide [33, 34]. Strikingly, we seem to have found the first mcr-1 positive ST11 strain in Egypt.
Conclusions
Multidrug resistance is becoming significantly more prevalent in high-risk patients, with the prevalence of colistin resistance increasing at alarming rates in Egypt. Indeed, the plasmid-borne colistin resistance gene mcr-1 was detected in two isolates and is spreading worldwide like plasmid-mediated carbapenemases. Thus, vigilant surveillance of colistin and carbapenem resistance should continue to limit further spread. This is the first report of mcr-1 in K. pneumoniae ST11 in Egypt, in a strain recovered from the bloodstream of a hospitalized cancer patient. This is also the first survey for mcr-2 in clinical isolates in the country, although it was not detected. In addition, mgrB mutations appear to play only a minor role in driving colistin resistance in this study. The lack of funding is one of the reasons behind the limited investigation of all the possible colistin resistance mechanisms in this study. Thus, chromosomal mutations of the pmrAB, and phoPQ must be investigated immediately, and further work is needed to fully understand the molecular mechanisms mediating colistin resistance in human enterobacterial isolates.
Availability of data and materials
All data analysed during this study are included in this published article.
Abbreviations
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- MLST:
-
multi locus sequence typing
- ST:
-
sequence type
- WT:
-
wild type
References
Falagas ME, Kaiakou SK. Colistin: the revival of polymyxins for the management of multidrug-resistant gram negative bacterial infections. Clin Infect Dis. 2005;40:1333–41.
Baron S, Hadjadj L, Rolain JM, Olaitan AO. Molecular mechanisms of polymyxin resistance: knowns and unknowns. Int J Antimicrob Agents. 2016;48:583–91.
Zurfuh K, Poirel L, Nordmann P, Nüesch-Inderbinen M, Hächler H, Stephan R. Occurrence of the plasmid-borne mcr-1 colistin resistance gene in extended spectrum-β-lactamase-producing Enterobacteriaceae in river water and imported vegetable samples in Switzerland. Antimicrob Agents Chemother. 2016;60:2594–5.
Grami R, Mansour W, Mehri W, Bouallègue O, Boujaâfar N, Madec JY, et al. Impact of food animal trade on the spread of mcr-1-mediated colistin resistance, Tunisia, July 2015. Euro Surveill. 2016;21:30144.
Battisti A. Antibiotic resistance—Italy: colistin, MCR-1, E. coli, turkeys 2014. ProMED mail. 2016;20160113.3933461.
Ruppé E, Le Chatelier E, Pons N, Andremont A, Ehrlich SD. Dissemination of the mcr-1 colistin resistance gene. Lancet Infect D is. 2016;16:290–1.
Yu CY, Ang GY, Chin PS, Ngeow YF, Yin WF, Chan KG. Emergence of mcr-1- mediated colistin resistance in Escherichia coli in Malaysia. Int J Antimicrob Agents. 2016;47:504–5.
Liu YY, Wang Y, Walsh TR, Yi LX, Zhang R, Spencer J, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16:161–8.
Elnahriry SS, Khalifa HO, Soliman AM, Ahmed AM, Hussein AM, Shimamoto T, et al. Emergence of plasmid-mediated colistin resistance gene mcr-1 in a clinical Escherichia coli isolate from Egypt. Antimicrob Agents Chemother. 2016;60:3249–50.
Schwarz S, Johnson AP. Transferable resistance to colistin: a new but old threat. J Antimicrob Chemother. 2016;71:2066–70.
Wang X, Wang Y, Zhou Y, Li J, Yin W, Wang S, et al. Emergence of a novel mobile colistin resistance gene, mcr-8, in NDM-producing Klebsiella pneumonia. Emerg Microbes Infect. 2018;7:122.
Xavier BB, Lammens C, Ruhal R, Kumar-Singh S, Butaye P, Goossens H, et al. Identification of a novel plasmid mediated colistin-resistance gene, mcr-2, in Escherichia coli, Belgium. Euro Surveill. 2016;21:30280.
European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters, version 7.1; 2017. http://www.eucast.org.
Diancourt L, Passet V, Verhoef J, Grimont PA, Brisse S. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J Clin Microbiol. 2005;43:4178–82.
Petrov K, Petrova P. Isolation and molecular identification of Klebsiella pneumoniae strains, producing diols from glycerol. Biotechnol Biotechnol Equip. 2009;23:814–7.
Liassine N, Assouvie L, Descombes MC, Tendon VD, Kieffer N, Poirel L, et al. Very low prevalence of MCR-1/MCR-2 plasmid-mediated colistin resistance in urinary tract Enterobacteriaceae in Switzerland. Int J Infect Dis. 2016;51:4–5.
Ellington MJ, Kistler J, Livermore DM, Woodford N. Multiplex PCR for rapid detection of genes encoding acquired metallo-beta-lactamases. J Antimicrob Chemother. 2007;59:321–2.
Poirel L, Walsh TR, Cuvillier V, Nordmann P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis. 2011;70:119–23.
Cannatelli A, D’Andrea MM, Giani T, Di Pilato V, Arena F, Ambretti S, et al. In vivo emergence of colistin resistance in Klebsiella pneumoniae producing KPC-type carbapenemases mediated by insertional inactivation of the PhoQ/PhoP mgrB regulator. Antimicrob Agents Chemother. 2013;57:5521–6.
Gustinetti G, Mikulska M. Bloodstream infections in neutropenic cancer patients: a practical update. Virulence. 2016;7(3):280–97.
Goel G, Hmar L, De Sarkar M, Bhattacharya S, Chandy M. Colistin-resistant Klebsiella pneumoniae: report of a cluster of 24 cases from a new oncology center in eastern India. Infect Control Hosp Epidemiol. 2014;35:1076–7.
Olaitan AO, Diene SM, Kempf M, Berrazeg M, Bakour S, Gupta SK, et al. Worldwide emergence of colistin resistance in Klebsiella pneumoniae from healthy humans and patients in Lao PDR, Thailand, Israel, Nigeria and France owing to inactivation of the PhoP/PhoQ regulator mgrB: an epidemiological and molecular study. Int J Antimicrob Agents. 2014;44:500–7.
European Centre for Disease Prevention and Control. Rapid risk assessment: plasmid-mediated colistin resistance in Enterobacteriaceae, 15 June 2016. https://ecdc.europa.eu.
Coetzee J, Corcoran C, Prentice E, Moodley M, Mendelson M, Poirel L, et al. Emergence of plasmid-mediated colistin resistance (mcr-1) among Escherichia coli isolated from South African patients. S Afr Med J. 2016;106:35–6.
McGann P, Snesrud E, Maybank R, Corey B, Ong AC, Clifford R, et al. Escherichia coli harboring mcr-1 and blaCTX-M on a novel IncF plasmid: first report of mcr-1 in the United States. Antimicrob Agents Chemother. 2016;60:4420–1.
Yu H, Qu F, Shan B, Huang B, Jia W, Chen C, et al. Detection of mcr-1 colistin resistance gene in carbapenem-resistant Enterobacteriaceae from different hospitals in China. Antimicrob Agents Chemother. 2016;60:5033–5.
Zhang XF, Doi Y, Huang X, Li HY, Zhong LL, Zeng KJ, et al. Possible transmission of mcr-1-harboring Escherichia coli between companion animals and human. Emerg Infect Dis. 2016;22:1679–81.
Sun J, Xu Y, Gao R, Lin J, Wei W, Srinivas S, et al. Deciphering MCR-2 colistin resistance. MBio. 2017;8:e00625-17.
Hindler JA, Humphries RM. Colistin MIC variability by method for contemporary clinical isolates of multidrug-resistant gram-negative bacilli. J Clin Microbiol. 2013;51:1678–84.
ElMahallawy HA, Zafer MM, Amin MA, Ragab MM, Al-Agamy MH. Spread of carbapenem resistant Enterobacteriaceae at tertiary care cancer hospital in Egypt. Infect Dis. 2018;50:560–4.
Haeili M, Javani A, Moradi J, Jafari Z, Feizabadi MM, Babaei E. MgrB alterations mediate colistin resistance in Klebsiella pneumoniae isolates from Iran. Front Microbiol. 2017;8:2470.
Olaitan AO, Morand S, Rolain J-M. Mechanisms of polymyxin resistance: acquired and intrinsic resistance in bacteria. Front Microbiol. 2014;5:643.
Potron A, Poirel L, Rondinaud E, Nordmann P. Intercontinental spread of OXA-48 beta-lactamase-producing Enterobacteriaceae over a 11-year period, 2001 to 2011. Euro Surveill. 2013;18:20549.
ElMahallawy H, Zafer MM, Al-Agamy M, Amin MA, Mersal MM, Booq RF, et al. Dissemination of ST101 blaOXA-48 producing Klebsiella pneumoniae at tertiary care setting. J Infect Dev Ctries. 2018;12:422–7.
Acknowledgements
The authors thank the Deanship of Scientific Research at King Saud University for funding this work through Project No. RGP-038.
Funding
Mohamed Alagamy received Research grants for Research at King Saud University, with Grant Number RGP-038.
Author information
Authors and Affiliations
Contributions
MZ and HE contributed to study design, literature review, and manuscript writing; AA collected isolates and performed experiments; MA contributed to study design and critically reviewed the manuscript; MHA and HR performed molecular analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethical committee of the National Cancer Institute as the Enterobacterial samples described in this paper are from cultures obtained by the microbiology and clinical pathology department as part of routine care for hospitalized infected cancer patients. No additional clinical specimens were obtained for purposes of research; therefore, informed consent was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zafer, M.M., El-Mahallawy, H.A., Abdulhak, A. et al. Emergence of colistin resistance in multidrug-resistant Klebsiella pneumoniae and Escherichia coli strains isolated from cancer patients. Ann Clin Microbiol Antimicrob 18, 40 (2019). https://doi.org/10.1186/s12941-019-0339-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-019-0339-4