Abstract
Background
Identification of all possible HIV reservoirs is an important aspect in HIV eradication efforts. The urinary tract has however not been well studied as a potential HIV reservoir. In this pilot study we molecularly characterized HIV-1 viruses in urine and plasma samples to investigate HIV-1 replication, compartmentalization and persistence in the urinary tract.
Methods
Prospectively collected urine and blood samples collected over 12–36 months from 20 HIV-1 infected individuals were analysed including sampling points from prior to and after ART initiation. HIV-1 pol gene RNA and DNA from urine supernatant and urine pellets respectively were analysed and compared to plasma RNA viruses from the same individual.
Results
HIV-1 nucleic acid was detected in urine samples from at least one time point in 8/20 (40%) treatment-naïve subjects compared to 1/13 (7.7%) individuals on antiretroviral treatment (ART) during periods of plasma viral suppression and 1/7 (14.3%) individuals with virological failure. HIV-1 RNA was undetectable in urine samples after ART initiation but HIV-1 DNA was detectable in one patient more than 6 months after treatment initiation. There was co-clustering of urine-derived pol sequences but some urine-derived sequences were interspersed among the plasma-derived sequences.
Conclusions
Suppressive ART reduces HIV-1 replication in the urinary tract but HIV-1 DNA may persist in these cells despite treatment. A larger number of sequences would be required to confirm HIV compartmentalization in the urinary tract.
Similar content being viewed by others
Introduction
Persistent HIV reservoirs harbouring integrated, replication-competent proviral DNA serve as a source of viral rebound on interruption of antiretroviral therapy (ART), resulting in a requirement for lifelong ART. Independent replication and selection pressures at different anatomic sites coupled with restricted genetic exchange may result in distinct compartmentalized variants [1]. Determining the anatomic reservoirs responsible for persistent viremia and viral rebound and the types of cells involved is important in the current efforts for HIV eradication and identification of targets for new drugs.
Lymph nodes have been shown to harbour replication-competent virus in virally suppressed individuals [2]. Other tissues and organs including the gut, male and female genital tracts and central nervous system have also been identified as potential sources of HIV-1 persistence [3,4,5,6]. We have previously reviewed the mechanisms of HIV persistence during ART in these reservoirs [7]. However some potential reservoirs such as the urinary tract, which includes the urethra, bladder and kidneys, have not been well studied. There is a wide spectrum of HIV-associated renal disease including HIV-associated nephropathy and HIV immune-complex kidney disease, the pathogenesis of which has been linked to HIV-1 infection of renal epithelium [8, 9]. In African countries the prevalence of renal disease associated with HIV ranges from 6 to 45% [10]. HIV infection of renal tubular epithelial cells in patients on suppressive antiretroviral therapy has been reported [11,12,13], and HIV infection of kidney allografts after transplantation has also been detected in HIV positive recipients with undetectable HIV virus in plasma at the time of transplantation [14]. These findings highlight the kidneys as a potential HIV reservoir in virally suppressed individuals on ART. In this pilot study, we isolated and molecularly characterized HIV-1 viruses in urine samples collected prospectively from twenty HIV-1 infected individuals, before and after antiretroviral treatment initiation and compared them to blood-derived viruses to investigate HIV-1 replication, compartmentalization and persistence in the urinary tract.
Methods
Patients and samples
Twenty HIV-1 positive individuals were selected from the parent study, the Soweto Lung Cohort (n = 756) [15] recruited from patients in Soweto, South Africa between November 2008 and October 2012. This sub-study restricted participants to those with detectable viremia after at least 6 months on antiretroviral treatment initiation. Participants had scheduled 6 monthly clinic visits where blood and urine samples and clinical information were collected (Additional file 1: Table S1). Viral loads and CD4 counts were tested at each visit. If local eligibility criteria for ART initiation were met, patients were referred for initiation of ART. Virological failure was defined as VL > 1000 RNA copies/ml 6 months after starting ART. A total of 97 urine samples from 20 patients were identified and analysed from the archived specimens. Following collection, urine samples were clarified by centrifugation and stored at − 70 °C as supernatants and cell pellets. Virions were concentrated from 2 ml stored urine supernatant by high-speed centrifugation (25,000 rpm for 2 h) and the supernatant removed leaving ~ 200 µl for HIV-1 RNA extraction. Urine pellets were re-suspended in 200 µl phosphate buffered saline before HIV-1 proviral DNA extraction.
HIV-1 amplification and pol gene sequencing
Total nucleic acid was extracted from 200 µl of sample and eluted in 50 µl of elution buffer using the automated NucliSENS easyMAG extraction system (Biomerieux, Boxtel, The Netherlands) with external lysis, and stored at − 20 °C until required for nucleic acid amplification. Extracted DNA was quantitated using the NanoDrop 2000 Spectrophotometer (Thermo Scientific). Genotyping of a 1084 base pair (bp) region of the HIV-1 pol gene covering the protease (PR) gene and codon 1–250 of the reverse transcriptase (RT) gene was performed using a one step reverse transcription polymerase chain reaction (RT-PCR) method [16]. Sequences were edited and assembled on Sequencher V 4.5 (Gene Codes Corporation, USA) and submitted to the Stanford HIVdb algorithm V 7.0. (http://hivdb.stanford.edu/) for subtyping, interpretation of resistance mutations and quality assessment. RNA and DNA viruses from urine samples were compared to RNA viruses from plasma samples detected from the same individual using phylogenetic analysis. Alignments were performed in MEGA6 and manually edited in BioEdit v 7.2.5 and neighbour joining trees constructed under the Kimura 2-parameter model with 1000 bootstrap values.
Results
Characteristics of subjects
Samples of 20 subjects meeting eligibility criteria were tested for the presence of HIV-1 nucleic acid in their longitudinal urine samples (Table 1). Study participants were followed up for between 12 and 36 months with a mean follow up period of 27 months (std: 8.81 months). Median CD4 count and plasma viral load at enrolment was 265 cells/µl and 4.17 log10 RNA copies/ml, respectively. Eighteen (90%) individuals had progressive HIV-1 disease defined as CD4 decline to < 300 cells/µl of whom 16 were initiated on ART during the study period. The other two individuals initiated ART at CD4 counts of 526 and 420 cells/µl.
Prevalence of HIV-1 nucleic acid detection in urine samples
HIV nucleic acid was detected in 27/97 (13.9%) of all urine samples representing 8 (40%) individuals (Table 2). Both HIV-1 RNA and proviral DNA were detected in urine supernatant and urine pellets, respectively, from 7 of the subjects, while only HIV-1 RNA was detected in the urine supernatant from subject 051.
To determine whether the detection of HIV-1 DNA in urine pellets associated with the amount of cells present in the urine, we compared the quantity of isolated genomic DNA (directly proportional to cell number) between urine pellet samples with and without detectable HIV nucleic acid. The mean DNA quantity was higher for urine pellets with detectable HIV nucleic acid compared to those with no detectable HIV nucleic acid (1.81 micrograms versus 0.37 μg; P = 0.01). For all urine samples, the frequency of detectable HIV RNA in supernatants and HIV proviral DNA in pellets were similar (13.4% and 14.4%, respectively). However, the frequency of detection for each individual over time varied substantially (Fig. 1).
CD4 T cell counts and viral loads over time in subjects showing detection of HIV nucleic acid in urine samples and plasma. Y-axis left: CD4 (cells/μl), black dotted line; Y-axis right: viral load (log10 copies/ml), red line. Subject IDs: Nucleic acid was detected in urine supernatant and pellet samples in all the subjects except Subject 051. In Subject 100, nucleic acid was detected in urine pellet during treatment period including period of virological failure (month 30) and period of undetectable viremia in blood (month 24). BL baseline (enrolment) sample, UP urine pellet, US urine supernatant, P plasma. Positive (Pos) samples are highlighted in green, negative (neg) in grey, ND not determined. Grey-shaded graph regions denote period of antiretroviral therapy
HIV-1 nucleic acid detection in urine samples during treatment period
To investigate if HIV detection in urine samples persists during treatment with antiretroviral therapy, we analysed urine samples obtained after treatment initiation. There were 26 urine samples tested (13 supernatant samples and 13 urine pellets) from 7 subjects that corresponded with periods of virological failure (VL > 1000 RNA copies/ml) in blood (Fig. 1). HIV-1 nucleic acid was detected in 1 urine pellet from subject 100. HIV-1 pol gene sequencing of the corresponding plasma samples did not detect resistance-associated markers from these samples. There were 42 samples tested (21 supernatant samples and 21 urine pellets) from 13 subjects that corresponded with periods of either undetectable viremia (Limit of detection 40 RNA copies/ml) or detectable viremia < 1000 RNA copies/ml in blood. HIV nucleic acid was detected in 1 urine pellet from subject 100 obtained more than 6 months after therapy initiation and during a period of undetectable viremia in blood.
Comparison of HIV-1 viral populations in urine to variants in blood
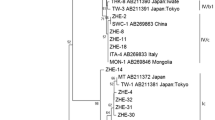
To compare HIV-1 viral populations in the urine to viruses in blood, a phylogenetic tree was constructed using the pol sequences obtained from the urine (supernatant and pellet samples) and from plasma (Fig. 2). Sequences included in the tree were from viruses from individuals where two or more sequences were obtained from urine samples. Co-clustering of urine-derived pol sequences among the plasma-derived sequences was observed while some urine-derived sequences were interspersed among the plasma-derived sequences. The co-clustering of urine-derived sequences in these individuals occurred between pellet-derived provirus sequences and sequences from free viruses in the urine supernatant. This is demonstrated in subject 747 for the 6 month sequences (6 M), subject 398 for the 12 month sequences (12 M) and in subject 376 for the 12 month (12 M) sequences (Fig. 2). Interspersing of urine-derived and plasma-derived sequences is shown in most of the sequences exemplified by urine-derived sequence 18 M and plasma-derived 6 M sequence which clustered.
Phylogenetic tree of the sequenced pol gene from the urine and blood viruses. The evolutionary history was inferred using the Neighbour-Joining method. The bootstrap values (1000 replicates) are shown next to the branches. The evolutionary distances were computed using the Kimura 2-parameter method. Evolutionary analyses were conducted in MEGA6. The sequence clusters from the 8 subjects with HIV-1 nucleic acid detected in urine are indicated. Red triangles—plasma RNA, blue squares—urine supernatant variants, empty blue squares—urine pellet variants. Sequences are named using time points (e.g. 6 M = 6 months, BL baseline)
Discussion
We analysed urine samples for HIV-1 shedding in the urinary tract before and after suppressive ART initiation. We have also investigated HIV-1 replication in the urinary tract, evidenced by detection of HIV-1 RNA in treatment naïve individuals, and HIV-1 compartmentalization by comparing HIV sequences from plasma-derived viruses to sequences derived from viruses in urine samples using phylogenetic analysis. We detected HIV-1 nucleic acid in urine samples from 40% of treatment-naïve subjects compared to 8% in the virally suppressed or low level viremia group and 14% in the virological failure group. Although phylogenetic analysis indicated co-clustering of provirus sequences and sequences from free viruses in the urine supernatant a larger number of sequences will be required to draw conclusions regarding virus compartmentalization in the urinary tract. We also detected viruses related to those circulating in blood resulting in equilibrium between blood and urinary tract viruses.
The low HIV-1 nucleic acid detection rates in urine samples from individuals on suppressive ART compared to treatment-naïve individuals indicates that suppressive ART is effective in blocking viral replication in the urinary tract. HIV-1 nucleic acid detection in urine samples from HIV positive treatment-naïve individuals has been reported in other studies [17, 18], followed by undetectable levels after treatment initiation [18]. Our data adds more information in that our cohort had a different subtype (C compared to B) and we analysed longitudinal samples instead of a single time point. In addition we looked at the pol gene instead of the env gene.
We detected HIV-1 RNA in urine pellets more than 6 months after treatment was initiated highlighting that infected cells can be shed into the urinary tract during periods of both viral suppression and virological failure in blood. The individual had virological failure after a period of viral suppression in blood with detectable HIV-1 DNA in cells shed in urine. In another study, HIV-1 DNA was detected in the urine samples in 23% of virally suppressed subjects on ART [19]. This raises the question whether HIV-1 DNA in cells of the urinary tract is replication-competent and may be responsible for viral rebound upon treatment cessation or virological failure during treatment. HIV-1 infection of kidney allografts after transplantation in HIV positive recipients with undetectable HIV-1 virus in plasma has been reported [14] indicating that this HIV-1 DNA may be replication competent and the source of infection in renal transplants.
In individuals with detectable HIV-1 nucleic acid in urine, we noted that detection of the HIV-1 did not occur at all the time points tested regardless of the associated higher plasma viral loads. The frequency of detection for each individual over time varied substantially (Fig. 1), which suggests that specific factors may modulate the presence of HIV in urine. Firstly, HIV-1 shedding in the urogenital tract may be intermittent leading to absence of virus in some samples. Secondly, HIV detection may depend on the urine volumes used. Urine volumes of 2 ml were used for nucleic acid extraction in this study. Larger urine volumes resulted in higher HIV-1 RNA [13] and HIV-1 proviral DNA [17] detection rates. HIV-1 RNA detection rate was 50% in samples with a starting volume ranging from 35 to 630 ml [13] while there was HIV-1 DNA detection rate of 66.25% achieved using cell pellets obtained from 100 ml fresh urine samples [17]. Finally, the presence or degree of renal injury, which may affect the rate of shedding of renal epithelial cells, was unknown in our subjects. This information could help determine why HIV-1 nucleic acid could be detected in some individuals or at certain times as HIV-associated nephropathy has been associated with HIV-1 replication and compartmentalization [9, 19]. We however used the amount of DNA in urine pellets after nucleic acid extraction as an indicator of presence and amount of cells shed into the urogenital tract. Our results indicated that urine samples with detectable HIV-1 DNA had significantly higher numbers of cells (larger amount of host DNA extracted) compared to urine samples with no detectable HIV-1 nucleic acid which may be an indication of renal injury and HIV-1 replication at the time of sample collection. Although HIV-1 virus could have been intermittently shed in urine for some individuals, HIV-1 RNA and proviral DNA were consistently not detected in longitudinal urine samples taken over 18 months from some treatment-naïve individuals.
In conclusion, we have demonstrated that urine samples can be used as a non-invasive method to study HIV replication, persistence and compartmentalization in the urinary tract. Suppressive ART reduces HIV-1 replication in the urinary tract but HIV-1 DNA can persist and be shed from some cells in the urinary tract despite treatment. Our data suggests HIV-1 replication in the urinary tract but also direct virus importation from blood resulting in equilibrium between blood viruses and viruses shed from the urinary tract but a larger number of sequences would be required to confirm compartmentalization.
Availability of data and materials
Data generated or analysed during this study are included in this published article and its additional file. Additional datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DNA:
-
deoxyribose nucleic acid
- ART:
-
antiretroviral therapy
- RNA:
-
ribonucleic acid
- PR:
-
protease
- RT:
-
reverse transcriptase
- Pol:
-
polymerase
- VL:
-
viral load
- RT-PCR:
-
reverse transcription polymerase chain reaction
References
Nickle DC, Jensen MA, et al. Evolutionary indicators of human immunodeficiency virus type 1 reservoirs and compartments. J Virol. 2003;77:5540–6.
Rothenberger MK, Keele BF, Wietgrefe SW, et al. Large number of rebounding/founder HIV variants emerge from multifocal infection in lymphatic tissues after treatment interruption. PNAS. 2015;112(10):E1126–34.
Chun T, Nickle DC, Justement JS, et al. Persistence of HIV in gut-associated lymphoid tissue despite long-term antiretroviral therapy. J Infect Dis. 2008;197(5):714–20.
Politch JA, Mayer KH, Welles SL, et al. Highly active antiretroviral therapy does not completely suppress HIV in semen of sexually active HIV-infected men who have sex with men. AIDS. 2012;26:1535–43.
Dahl V, Gisslen M, Hagberg L, et al. An example of genetically distinct HIV type 1 variants in cerebrospinal fluid and plasma during suppressive therapy. J Infect Dis. 2014;209(10):1618–22.
Bednar MM, Sturdevant CB, Tompkins LA, et al. Compartmentalization, viral evolution, and viral latency of HIV in the CNS. Curr HIV/AIDS Rep. 2015;12(2):262–71.
Mzingwane ML, Tiemessen CT. Mechanisms of HIV persistence in HIV reservoirs. Rev Med Virol. 2017;27:e1924.
Wyatt CM, Meliambro K, Klotman PE. Recent progress in HIV-associated nephropathy. Annu Rev Med. 2012;63:147–59.
Marras D, Bruggeman LA, Gao F, et al. Replication and compartmentalization of HIV-1 in kidney epithelium of patients with HIV-associated nephropathy. Nat Med. 2002;8:522–6.
Moosa MR, van der Walt I, Naicker S, Meyers AM. Important causes of chronic kidney disease in South Africa. S Afr Med J. 2015;105(4):320.
Winston JA, Bruggeman LA, Ross MD, et al. Nephropathy and establishment of a renal reservoir of HIV type 1 during primary infection. N Engl J Med. 2001;344:1979–84.
Chen P, Chen BK, Mosoian A, et al. Virological synapses allow HIV-1 uptake and gene expression in renal tubular epithelial cells. J Am Soc Nephrol. 2011;22:496–507.
Blasi M, Balakumaran B, Chen P, et al. Renal epithelial cells produce and spread HIV-1 via T-cell contact. AIDS. 2014;28:2345–53.
Canaud G, Dejucq-Rainsford N, Avettand-Fenoël V, et al. The kidney as a reservoir for HIV-1 after renal transplantation. J Am Soc Nephrol. 2014;25(2):407–19.
Gupte AN, Wong ML, Msandiwa R, et al. Factors associated with pulmonary impairment in HIV-infected South African adults. PLoS ONE. 2017;12(9):e0184530.
Zhou Z, Wagar N, DeVos JR, et al. Optimization of a low cost and broadly sensitive genotyping assay for HIV-1 drug resistance surveillance and monitoring in resource-limited settings. PLoS ONE. 2011;6(11):e28184.
Li JJ, Huang YQ, Poiesz BJ, Zaumetzger-Abbot L, Friedman-Kien AE. Detection of human immunodeficiency virus type 1 (HIV-1) in urine cell pellets from HIV-1 seropositive individuals. J Clin Microbiol. 1992;30(5):1051–5.
Blasi M, Carpenter JH, Balakumaran B, Cara A, Feng G, Klotman ME. Identification of HIV-1 genitourinary tract compartmentalization by analysing the env gene sequences in urine. AIDS. 2015;29(13):1651–7.
Chakrabarti AK, Caruso L, Ding M, et al. Detection of HIV-1 RNA/DNA and CD4 mRNA in feaces and urine from chronic HIV-1 infected subjects with and without antiretroviral therapy. AIDS Res Ther. 2009;6:20.
Acknowledgements
Not applicable.
Funding
This work is based on the research supported by grants awards from South African Research Chairs Initiative of the Department of Science and Technology and National Research Foundation of South Africa. The Longitudinal Study of HIV-Associated Lung Infections in Soweto was funded by the National Institutes of Health, USA (R01HL090312 and P30AI094189: R. E. Chaisson). The funding bodies had no contribution in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
MM, SB, GH and CT conceived and planned the project. CT, RC and NM enrolled study participants, and were responsible for the collection and storage of the blood and urine samples used in the study. MM, MK, AB and JL were responsible for nucleic acid extraction, sequencing and phylogenetic analysis. RL analysed the data and constructed the figures and tables. MM and KR drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The parent study was approved by the University of the Witwatersrand Human research ethics committee (Medical); clearance certificate number M140926 and all participants provided informed consent for sample collection.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
Study subjects and time points at which urine samples were tested.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mzingwane, M.L., Hunt, G., Lassauniere, R. et al. Detection and molecular characterization of urinary tract HIV-1 populations. Ann Clin Microbiol Antimicrob 18, 27 (2019). https://doi.org/10.1186/s12941-019-0326-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-019-0326-9