Abstract
Background
Hospital acquired fungal infections are defined as “never events”—medical errors that should never have happened. Systemic Candida albicans infections results in 30–50% mortality rates. Typically, adhesion to abiotic medical devices and implants initiates such infections. Efficient adhesion initiates formation of aggressive biofilms that are difficult to treat. Therefore, inhibitors of adhesion are important for drug development and likely to have a broad spectrum efficacy against many fungal pathogens. In this study we further the development of a small molecule, Filastatin, capable of preventing C. albicans adhesion. We explored the potential of Filastatin as a pre-therapeutic coating of a diverse range of biomaterials.
Methods
Filastatin was applied on various biomaterials, specifically bioactive glass (cochlear implants, subcutaneous drug delivery devices and prosthetics); silicone (catheters and other implanted devices) and dental resin (dentures and dental implants). Adhesion to biomaterials was evaluated by direct visualization of wild type C. albicans or a non-adherent mutant edt1 −/− that were stained or fluorescently tagged. Strains grown overnight at 30 °C were harvested, allowed to attach to surfaces for 4 h and washed prior to visualization. The adhesion force of C. albicans cells attached to surfaces treated with Filastatin was measured using Atomic Force Microscopy. Effectiveness of Filastatin was also demonstrated under dynamic conditions using a flow cell bioreactor. The effect of Filastatin under microfluidic flow conditions was quantified using electrochemical impedance spectroscopy. Experiments were typically performed in triplicate.
Results
Treatment with Filastatin significantly inhibited the ability of C. albicans to adhere to bioactive glass (by 99.06%), silicone (by 77.27%), and dental resin (by 60.43%). Atomic force microcopy indicated that treatment with Filastatin decreased the adhesion force of C. albicans from 0.23 to 0.017 nN. Electrochemical Impedance Spectroscopy in a microfluidic device that mimic physiological flow conditions in vivo showed lower impedance for C. albicans when treated with Filastatin as compared to untreated control cells, suggesting decreased attachment. The anti-adhesive properties were maintained when Filastatin was included in the preparation of silicone materials.
Conclusion
We demonstrate that Filastatin treated medical devices prevented adhesion of Candida, thereby reducing nosocomial infections.
Similar content being viewed by others
Background
Hospital acquired infections are described as “never events”—medical errors that should never have happened. These are largely preventable, serious events that have an adverse effect on public health. The CDC estimates that there are 1.7 million hospital acquired infections each year causing nearly 100,000 deaths, which costs the US healthcare system between 28 billion and 33 billion dollars each year [1]. Candida albicans, a normally human commensal organism, has become a significant cause of most nosocomial diseases of fungal origin [2,3,4]. The number of immunocompromised patients, the population “at risk” and susceptible to fungal diseases [5, 6], steadily increased worldwide at the beginning of the century due to better medical facilities and changes in life style. As expected, this had serious repercussions in the number of reported cases of C. albicans infections [7, 8]. In the United States alone, the estimated healthcare cost to treat C. albicans systemic infections is between $1.5 and $2 billion per year, which accounts for ∼70% of the total amount spent on systemic fungal infections [9,10,11]. This is in part due to a reduced number of antifungal drugs, a consequence of the fact that it is difficult to find fungi-specific drug targets that are not also present on host cells. Among the commercially available antifungals, azoles, polyenes and echinocandins are the most effective [12]. In the last few years strains resistant to fluconazole have been reported, and with it a new threat to public health [13,14,15,16]. Therefore, new methods to prevent hospital-acquired infections by this opportunistic fungus are becoming more important than ever.
Candida albicans is commonly found in the skin and urogenital tract of humans. However, it can become pathogenic causing localized infections such as thrush and vaginitis, the latter being suffered by 75% of females at least once in their lifetime [17, 18]. Furthermore, C. albicans can reach the bloodstream and cause systemic infections where the mortality rate can be as high as 50%, even with treatment [19, 20]. Individuals who contract systemic infections caused by this pathogen are typically immunocompromised, such as HIV-infected persons, transplant recipients, patients receiving chemotherapeutic agents, patients receiving large amounts of antibiotics for bacterial infection treatment, and low-birth weight infants [7, 8, 21,22,23,24], who are now at an increased risk due to drug resistant C. albicans [12, 25,26,27]. Treating such drug-resistant strains involves long term combination therapy that is often cost prohibitive.
Filastatin was recently identified as a potential agent to prevent C. albicans filamentation and adhesion to abiotic and biotic surfaces [10], both of which contribute to biofilm formation and virulence [25, 28,29,30]. We have previously reported that Filastatin also inhibits the adhesion of C. dubliniensis, C. tropicalis and C. parapsilosis to polystyrene surfaces [10]. Here, we specifically focus on the antiadhesive properties of Filastatin, and propose its use as a pre-therapeutic coating for biomaterials, specifically, dental resin used in dentures and dental implants; silicone elastomers which is widely used as a biomaterial in catheters or as a component of implanted devices that contact the body; bioactive glass which is a component of some medical devices, such as cochlear implants or subcutaneous drug delivery devices that have embedded electronics, and used in prosthetic devices along with titanium to repair and replace diseased or damaged bone [31, 32]. These materials are at high risk of being contaminated with C. albicans due to their composition and physical properties [33, 34]. Even more, their common use in clinical settings makes them a suitable reservoir for nosocomial infections [35, 36]. Previous studies have demonstrated, to different extents, the efficiency of coating agents, such as chitosan [37], curcumin on dental resins [38], or the covalent immobilization of the antimicrobials vancomycin and caspofungin on titanium [39] preventing C. albicans adhesion and biofilm formation. Thus, we tested various biomaterials under steady-state laboratory conditions as well as physiological flow conditions where the abiotic surfaces were co-incubated or pre-treated with Filastatin. We used analytical techniques such as atomic force microscopy (AFM) to measure the force of adhesion to abiotic surfaces and electrochemical impedance spectroscopy (EIS) to measure the anti-adhesive properties of Filastatin on C. albicans under conditions that mimics physiological flow conditions. Finally, we tested silicone material where Filastatin was incorporated into its composition.
Methods
Strains and culture conditions
Candida albicans isolate, SC5314, obtained from a patient with disseminated candidiasis [40], an mCherry-tagged derivative [41], and the non-adherent mutant edt1 −/− [42] were used in this study. C. albicans cultures were stored at −80 °C and were propagated on synthetic complete media (SC) agar plates at 30 °C. A single colony obtained from the plates was used to prepare the inoculum in conical tubes containing 10 mL of tryptic soy broth (TSB) that allows cells to grow as planktonic cells. C. albicans cells were growth overnight (12–15 h) at 30 °C in a roller drum incubator (64 rpm).
Preparation of biomaterials
96 well polystyrene plates were used for assay development to test C. albicans adhesion. To measure the effect Filastatin wells were pre-treated with Filastatin using 198 µL of diH2O + 2 µL of DMSO, or 2 µL of 50 µM Filastatin in DMSO. The wells were washed 10 times in diH2O and dried using N2 gas. Treated surfaces were visually monitored since the nitrophenyl group on Filastatin absorbs in the visible spectrum (400 ηm).
Glass coupons (1.2 cm diameter) were cleaned using Piranha solution (30 of 35% H2O2 + 70% H2SO4) for 1 h, then washed with deionized water for at least 10 min, rinsed with ethanol wash and dried with N2 gas. Once dried, the coupons were oxygen plasma cleaned for 2 min, and then silane-coated using 1% APTMS (3-aminopropyltrimethoxysilane) in 96% ethanol (aqueous) for at least 6 h at room temperature and agitated at 60 rpm. The bioactive coupons were finally washed with ethanol, dried with N2 gas, and stored at 4 °C until use.
Dental implants resin coupons, made from a fast self-curing acrylic methacrylate resin using the Lang dental Jet Tooth Shade kit, were obtained from Dr. M. Noverr (LSUHSC, New Orleans, LA 70112).
Silicone coupons were made using a mix of polydimethylsiloxane elastomer (PDMS, a silicone elastomer). Briefly, 6 mL of polydimethylsiloxane elastomer were combined with 600 µL of silicone curing agent. After degassing the mix using vacuum for 2 h, the mix was poured on a plane surface and compressed into a fine pellicle of approx. 2 mm of height. Polymerization of the mix took place at 72 °C for 3 h. Coupons of 1.2 cm diameter were then cut from the PDMS pellicle. PDMS coupons including Filastatin were made adding 60 µL of 2.5 mM Filastatin in DMSO to the polydimethylsiloxane elastomer and curing agent mix. PDMS control coupons were made adding 60 µL of DMSO.
Dental resin and PDMS coupons treated with Filastatin prior exposure to cells were placed in a 1.5 mL of diH2O containing 50 µM Filastatin in 1% DMSO for 30 min at 37 °C. The coupons were vigorously washed with abundant diH2O, dried using N2 gas, and stored at 4 °C until use. The presence of Filastatin on the surface of the coupon was confirmed by the evident change of color to yellow.
Assay development for surface adhesion of C. albicans on polystyrene
SC5314 grown overnight were recovered by centrifugation at 1000g, 18 °C; washed twice with SC + 0.15%; and adjusted to 0.3 OD600 (equivalent to 9·106 cells mL−1). Cells were incubated in a polystyrene 96 well plate (198 µL per well) including 2 µL of DMSO (control) or 5, 2.5, or 1.25 mM Filastatin in DMSO for 2.5 h at 37 °C. The wells were emptied and 50 µL of crystal violet 0.5% aqueous solution was added to each well. After 45 min of incubation under static conditions the 96 well plate was washed 10 times with diH2O. 200 µL of 75% methanol were added to each well, and the absorbance was read at 590 nm in a plate reader (PerkinElmer, VICTOR3) [10]. The absorbance values obtained were used to calculate a relative absorbance. Typically, the relative absorbance was calculated per biological replicate by dividing each sample’s absorbance by the average of the DMSO control absorbance.
For the time-dependent assay, cells were co-incubated with Filastatin following the protocol previously described in 96 well polystyrene plates for varying lengths of time: 5, 15, 30 min, and then every 30 min until 240 min. For Filastatin pre-treated polystyrene, 200 µL of the cell suspension was added to each well. Controls including 1% DMSO or 50 µM Filastatin in 1% DMSO in non-treated wells were also included, as well as a negative control of edt1 −/−. The 96 well plate was incubated for 4 h at 37 °C, without agitation and light exposure. Adherent cells were also quantified using crystal violet staining following extensive washing. Absorbance was normalized as described above.
Measurement of surface adhesion of C. albicans on various biomaterials
Adhesion was measured using direct cell counts. SC5314 or SC5314 mCherry grown overnight were washed with SC + 0.15% dextrose and adjusted to 0.3 OD600. APTMS-treated glass were incubated in a 24 well plates, each well containing 1.5 mL of the cell suspension and 15 µL of 5 mM Filastatin in DMSO, or an equal volume of the solvent as control. Cells were incubated for 2.5 h at 37 °C under static conditions (no agitation). Coupons were then recovered and washed twice with diH2O, 10 min each time. Fluorescent images were taken with an Axio Imager Z1 with ApoTome (Zeiss). Twenty images were obtained per coupon, and the cells per imaged field (0.15 mm2) were counted using ImageJ v1.49 m [43] and averaged. To visualize the non-tagged SC5314, after washing the coupons the cells were stained with Syto®9 and propidium iodide (PI) for 15 min (live/dead assay).
A similar protocol was used for other biomaterials. Briefly, a 24 well plate containing a 1.5 mL of a C. albicans cell suspension (0.3 OD600) per well was incubated at 37 °C using either APTMS-treated glass coupons, acrylic dental implants coupons, or PDMS coupons in presence and absence of 50 µM Filastatin in 1% DMSO. Acrylic dental coupons and PDMS treated with Filastatin; and PDMS coupons including Filastatin were only incubated with 1.5 mL of C. albicans (0.3 OD600). The coupons were recovered after 2.5 h, and were gently rinsed with diH2O. Then, the coupons were placed in a new plate containing 500 µL of crystal violet per well for a 45 min incubation. Subsequently, the coupons were rinsed in situ using 1000 µL of diH2O, three times. The crystal violet stain was recovered from the cells using 500 µL of an aqueous solution of 75% methanol, and the absorbance read at 590 nm.
Atomic Force Microscopy to measure adhesion force of C. albicans
AFM was used to quantify the adhesion force of single C. albicans cells to bioactive glass coupons. A 0.3 OD600 suspension of SC5314 cells was prepared using SC + 2% dextrose. Two tubes were filled with 2475 µL of cells and 25 µL of DMSO or 5 mM Filastatin in DMSO and incubated at 30 °C in a roller drum incubator. After 30 min the cells were centrifuged at 1000g for 5 min and 18 °C, and washed with PBS. A small volume of the cell suspension was pipetted on an agar plate, and using a cantilever coated with Concanavalin A (ConA) a single cell was picked up. This C. albicans cell was used for a series of ≥39 adhesion force measurements against a bioactive glass surface, with readings every 5 s using AFM (Asylum MFP-3D-BIO). As an additional control, the non-adherent edt1 −/− mutant was also tested for adhesion.
Electrochemical impedance spectroscopy of C. albicans under physiological microfluidic conditions
A microfluidic chamber of 4 mm × 6 mm × 1 mm was fabricated by casting PDMS into an aluminum chamber. Interdigitated micro electrodes (IDE) were fabricated from gold coated glass slides, with the electrode pattern carved using a VersaLaser VLS 2.30 CO2 laser cutter. Each sensor is comprised of a 4 × 6 mm active sensitive surface made of 4 pairs of microelectrodes (400 µm wide with 7.2 mm-long fingers, each finger separated by 400 µm). Before use, the IDE sensors were cleaned with piranha solution, washed for 10 min with abundant diH2O, sonicated for 5 min in 96% ethanol, and dried in a stream of N2 gas. IDEs were then activated with O2 plasma for 2 min and immersed overnight in a 1 mM cysteamine hydrochloride 3% triethylamine ethanoic solution at room temperature. The IDEs were then rinsed with 96% ethanol, submerged in 10% acetic acid in ethanoic solution, and rinsed with 96% ethanol before being dried with N2 gas.
A 0.3 OD600 suspension of SC5314 in SC + 0.15% dextrose with 50 µM Filastatin in 1% DMSO or 1% DMSO was pumped through the IDEs assembled microfluidic channels (each of 6 mm × 4 mm × 1 mm) at 120 µL min−1 for 3 h, and at 37 °C. A syringe pump (KD Scientific) and silicone tubing were used to maintain the continuous flow. EIS measurements were performed every 5 min over a frequency range of 4–100 kHz, 0 V DC bias and a 20 mV p–p sinusoidal excitation signal. Adhesion of C. albicans cells over time was measured indirectly by using impedance changes (Zreal at 4 kHz). The experiment was also performed for the non-adherent mutant edt1 −/− in presence of the DMSO vehicle (negative control). Each experiment consists of at least three biological replicates. Moreover, a single C. albicans cell is regarded as a dielectric component since it consists of biomaterials that have double-layer capacitance [44]. At higher frequencies, the electric current can penetrate the cell body and the impedance is independent of the frequency. At lower frequencies, the double layer capacitance of the cell body and EPS results in a high impedance. The EIS frequency used in biosensing research is usually below 1 MHz, at which there is greater sensitivity to biological bodies, such as cells [45]. In this microfluidic physiological flow [46] experiment, C. albicans cells flowing through the IDE were attached and detached from its surface over time due to the nature of the surface, flow shear stress and hydrodynamic forces [47, 48]. As expected, the attachment of cells on the IDE covered the IDE conductive surface and increased the impedance, while the detachment exposed the IDE conductive surface and thus decreased the impedance.
Results
Filastatin inhibits C. albicans adhesion in a time and concentration dependent manner
We have previously demonstrated that Filastatin inhibits adhesion of many fungal pathogens of the Candida spp. to polystyrene surfaces [10]. To further study its anti-adhesion properties we exposed C. albicans to increasing concentrations of Filastatin (Fig. 1a). Unbound cells were washed and attached cells were stained with crystal violet to measured absorbance at 590 nm and quantify adhesion. We measured the effect of 12.5, 25 and 50 µM Filastatin compared to the solvent (DMSO) control. Our results indicate that treatment with Filastatin significantly decreases adhesion by 58.7, 68.1 and 70.8%, respectively (p < 0.0001, one-way ANOVA) for C. albicans, as compared to the control (Fig. 1a).
Filastatin-mediated inhibition of C. albicans adhesion to abiotic surfaces is a dependent on its concentration and b increases over time. C. albicans were incubated in the presence of Filastatin. Adherent cells were stained with crystal violet and absorbance was measured. Relative absorbance values for each of the three biological replicates and standard error bars displayed, p < 0.0001. The edt1 −/− mutant lacking an adhesion protein is used as a negative control
In order to determine the exposure time required for Filastatin to trigger an anti-adhesion response in C. albicans, we performed a time course experiment from 5 to 240 min using 50 µM Filastatin. Our results showed that the anti-adhesion effect of Filastatin increases overtime (Fig. 1b). Significant reduction of C. albicans attachment was observed 15 min post Filastatin treatment as compared to control (DMSO solvent). The effect of Filastatin was exaggerated with increased exposure time: at 15 min post exposure 29.6% of cells were attached, 19.4% after 60 min, and less than a 6% after 240 min. Together these results indicate that effects of Filastatin are concentration and time dependent, and measurable as early as 15 min.
Filastatin decreases the force of attachment between C. albicans and abiotic surfaces
To measure the direct force of attachment of C. albicans to an abiotic surface we used AFM. Briefly, cells attached to a surface are probed to measure the force necessary to “pluck” them off the surface [49]. Wild type C. albicans was exposed to 50 µM Filastatin and control population was exposed to the solvent (DMSO) for 30 min. The force of attachment for wild type C. albicans was recorded at 0.23 nN compared to 0.017 nN when cells were treated with Filastatin (Fig. 2, p < 0.001, one-way ANOVA). This decreased force was comparable to the non-adherent edt1 −/− mutant cell attachment to surfaces. These physical measurements further support our previous observations that Filastatin decreases the force of attachment between C. albicans and an abiotic surface.
Atomic force microscopy (AFM) to measure adhesion force on C. albicans to abiotic surfaces. C. albicans cells were lifted with an AFM cantilever and probed against an abiotic surface to measure the adhesion force. The adhesion force of cells treated with Filastatin (white bar) is shown in contrast to untreated cells and the edt1 −/− non-adherent mutant (black bars). Each force measurement is calculated from 35–50 trials, standard error bars displayed, p < 0.001. The graphic shows one representative experiment
Filastatin inhibits adhesion of C. albicans to a variety of biomaterials
To establish the utility of Filastatin in preventing adhesion of C. albicans we tested biomaterials such as dental resin, bioactive glass, and silicone. We used 1.2 cm coupons composed of these biomaterials that fit at the bottom of 24 well plates. We standardized the protocol using bioactive glass where we measured adhesion by direct counting of cells attached to the surfaces (Fig. 3a), and spectroscopic measurement of crystal violet stained cells attached to the surface (Fig. 3b). As described earlier we exposed C. albicans to varying concentration of Filastatin (12.5, 25 and 50 µM) and allowed cells to attach to bioactive glass coupons. Our results indicate that there was a significant decrease (p < 0.0001) in the number of C. albicans cells attached to bioactive glass after treatment with Filastatin as compared to the untreated control (Fig. 3a). Similar results were obtained when adherent cells were stained and the absorbance at A590 was measured (Fig. 3b).
Filastatin inhibits attachment of C. albicans to bioactive glass. C. albicans was incubated in varying concentrations of Filastatin in 24 well plates containing bioactive glass coupons. a Direct cell counts were obtained by propidium iodide and Syto9® staining. Black bars represent the number of wild type cells (control) or non-adherent cells (edt1 −/−) that attach to untreated bioactive glass. Grey and white bars represent wild-type cells treated with varying concentrations of Filastatin. Standard error bars displayed, p < 0.0001. b Crystal violet staining to determine adhered cells to the surface of bioactive glass coupons
To determine whether Filastatin affects viability of the cells, we used a live-dead assay (Syto9® and PI) where metabolically active and live cells fluoresce green (Syto9®) and dead cells fluoresce red (PI). These studies indicate that adherent C. albicans cells treated with Filastatin or those removed from the media containing Filastatin are viable. A representative microscopy image of a coupon surface with fluorescent stained cells is shown in Fig. 4a. To test whether the continuous exposure to Filastatin is needed to disrupt adhesion, we exposed C. albicans to 50 µM Filastatin, washed them, and then tested cell adhesion on bioactive glass. The experimental design is outlined in Fig. 4b. Briefly, surface adhesion of C. albicans cells was measured after continuous exposure to Filastatin or DMSO compared to that of cells that were washed and recovered in fresh media after Filastatin treatment. Our results (Fig. 4c) indicated that continuous exposure to Filastin decreased surface adhesion by 78% as compared to short exposure to Filastatin where adhesion was decreased by 24%. These results suggest that Filastatin is more effective when present continuously. This prompted us to consider Filastatin as a pre-therapeutic coating for biomaterials.
The anti-adhesion effect of Filastatin depends on a continuous exposure to the drug and does not affect C. albicans viability. a C. albicans cells are viable upon exposure to Filastatin. Microscopic imaging of untreated cells attached to bioactive glass (top panel, labeled control) indicate that cells were viable but were unable to attach when treated with Filastatin (bottom panel). Filastatin treated cells were removed from the incubation media and stained for viability to ascertain that 100% of the cells were accounted for. b Experimental design to compare SC5314 cells pretreated with Filastatin vs those under continuous exposure to Filastatin. Step 1 Cells were incubated with 1% DMSO (i), untreated (ii), or 50 µM Filastatin in 1% DMSO (iii). Step 2 After 15 min, all the cells were washed three times. Step 3 Adhesion assay using cell suspensions (i control, ii continuous exposure to Filastatin, or iii pre-treated with Filastatin). Yellow represents Filastatin in the media, or cells that were exposed to Filastatin. c C. albicans cells exposed to Filastatin either as a pre-treatment (hatched) or continuously (white) were unable to attach to bioactive glass as compared to the untreated cells (black). The decrease in adhesion is more dramatic when Filastatin is present continuously. Standard error bars displayed, p < 0.0001. Cell adhesion was measured using the crystal violet assay
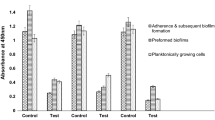
Filastatin, can serve as a pre-therapeutic coating for various biomaterials
Since Filastatin is most effective when present continuously we wanted to test whether it can be used as pre-therapeutic for biomaterials that pose a high risk of contamination with C. albicans. C. albicans cells incubated on 50 µM Filastatin-treated polystyrene wells showed 24.5% of cell adhesion when compared to the DMSO solvent control. A similar result was obtained when Filastatin was co-incubated (25.37% of cells adhered) with cells. 74% of cells adhered to DMSO solvent treated polystyrene wells, while the positive control edt1 −/− mutant strain, registered a 6.77% of cell adhesion (Fig. 5).
Filastatin-treatment of polystyrene prevents C. albicans attachment. a Diagram representing the experimental setup. Step 1 Polystyrene surfaces were untreated (i, ii), treated with the DMSO solvent (iii), or treated with Filastatin (iv). Step 2 Washing. Step 3 Incubation with C. albicans in the presence of solvent (i), Filastatin (ii), or none (iii, iv). b Crystal violet staining to determine C. albicans attachment to Filastatin-treated polystyrene. The black bars (control and edt1 −/−) represent C. albicans attachment to untreated polystyrene. The white bar represents Filastatin treated C. albicans attachment to untreated polystyrene. The grey bar represents adhesion of C. albicans to polystyrene exposed to the solvent only, and the grey hatched bar represents C. albicans adhesion to Filastatin-treated polystyrene
Similar decrease in adhesion was observed when silicone surfaces and dental resin were incubated with C. albicans cells in presence of 50 µM Filastatin. Cell attachment was decreased by 87.27 and 60.43% as compared to DMSO solvent controls, respectively (Fig. 6a, b).
Biomaterials treated with Filastatin prevent C. albicans attachment. a Adhesion of wild type C. albicans cells incubated with or without Filastatin on silicone coupons; or b on acrylic dental resin coupons. c C. albicans incubated on Filastatin-treated silicone coupons, or DMSO-exposed silicone coupons (control); or d on Filastatin-treated acrylic dental resin coupons. C. albicans adhesion measured using the crystal violet assay. Standard error bars displayed. ***p < 0.001, ****p < 0.0001
Silicone and dental resin coupons were also pretreated with 50 µM Filastatin for 30 min prior to exposure to C. albicans. Silicone surfaces where Filastatin was chemisorbed showed a 62.7% of reduction of adhesion of C. albicans, while similarly treated dental resin showed a 79.7% (Fig. 6c, d). Together these results indicate that biomaterials such as silicone and dental resin when superficially treated with Filastatin prevent attachment of C. albicans. These results further establish the utility of Filastatin as a pre-therapeutic for biomaterials. The anti-adhesion effect of Filastatin is lost after treatment with harsh chemicals such as methanol. Binding of C. albicans to methanol-treated coupons was similar when compared to untreated resin surfaces. These observations informed our next experiments to incorporate Filastatin into the matrix of biomaterials.
The anti-adhesive properties of Filastatin persists when incorporated into the chemical composition
To be used as a pre-therapeutic Filastatin may also be incorporated into the composition of the biomaterial. For this purpose, we choose to test silicone since it is a versatile biomaterial specifically used in catheters, a surface that often initiates a candida infection. Our results indicate that incorporation of 25 µM filastatin into the composition of silicone coupons decreased adhesion of C. albicans by 6.5-fold when compared to untreated silicone coupons (Fig. 7, p < 0.001). These results demonstrate that Filastatin retains its biological activity when it is incorporated into the silicone material, despite of being exposed at 72 °C for 3 h.
Filastatin incorporated into silicone during formulation confers anti-adhesive properties against C. albicans. Crystal violet assay results for C. albicans attached to silicone surfaces prepared with Filastatin (white bar) or including the DMSO solvent (black bar). Standard error bars displayed, p < 0.001
The anti-adhesive properties of Filastatin persist in physiological flow conditions
The effectiveness of Filastatin in a dynamic flow system that mimics physiological conditions was assessed using EIS to measure surface impedance. Higher impedance is indicative of more C. albicans cells being attached to surfaces. EIS is widely used in biosensing [50] to measure impedance on amine-terminated IDE (a schematic of the IDE is shown in Fig. 8a, b). Through the course of this microfluidic experiment, the cells experience a continuous flow rate of 120 µL min−1 for 3 h, mimicking the conditions in the circulatory system of the mammalian host [46]. C. albicans cells continually attached and detached from the surface of the electrode during the experiment. Due to the double-layer capacitance nature of the cells at low frequency range, attachment of the cells on IDE surface is recorded as an increase in impedance changes and detachment of the cells exposes the electrode’s conductive surface and is recorded as a decrease in the impedance [44, 45]. This allows us to measure the impedance as a readout for cell attachment and to determine the effects of Filastatin. C. albicans cells treated with Filastatin showed lower impedance as compared to untreated cells. The impedance of the non-adherent mutant edt1 −/− was measured as a positive control (Fig. 8c). Indeed, these results indicate that Filastatin is effective under dynamic flow conditions and supports the finding that Filastatin reduces attachment of C. albicans to abiotic surfaces.
Filastatin prevents the attachment of C. albicans under flow conditions. a Schematic of the interdigitated gold microelectrodes for sensing impedance upon C. albicans attachment. b Schematic of the assembly of electron impedance spectroscopy (EIS) device in the microfluidic chamber that mimics physiological flow of bodily fluids. c Normalized impedance ratio results for C. albicans in SC + 0.15% dextrose and 50 µM Filastatin at 4 kHz. EIS measurements were performed every 10 min using a 20 mV p–p sinusoidal excitation signal. The adhesion over time was measured by using impedance changes (Zreal). SC5314 was used for the positive control and Filastatin treatments, and edt1 −/− is the negative control
Discussion
Over the last few decades the number of cases of systemic candidiasis has increased, outpacing the development of antifungal drugs to fight it. As an opportunistic pathogen, C. albicans is responsible for common clinical problems including oral thrush and vaginitis, but can also lead to life-threatening systemic infections in immunocompromised individuals [51], resulting in 30–50% mortality rates [52, 53]. A contributing factor to these statistics is the ability of C. albicans to develop resistance to antifungal drugs. In fact, fluconazole-resistant Candida strains were more frequently reported [27] and with it the fear of a new threat. The Center for Disease Control (CDC) recently declared drug-resistant C. albicans as a major public health threat [13,14,15,16, 54]. With the Pharmaceutical industry reporting a low inventory of antimicrobials [55], the search for non-traditional methods to prevent and manage nosocomial fungal infections is becoming more important than ever.
Inhibitors of adhesion are excellent lead compounds for pre-therapeutic and therapeutic drug development because (1) adhesion is the first step of an infection, and (2) inhibition of a general property such as fungal adhesion are likely to have a broad spectrum and affect other fungal pathogens. Efficient adhesion is required for formation of aggressive biofilms, which in turn make Candida a successful pathogen [56]. Therefore, adhesion is a pivotal step in fungal pathogenesis, but to our knowledge, one that has not yet been targeted by small molecules.
The discovery of Filastatin and other small molecules with attachment and biofilm disrupting properties [57] can lead to new alternatives for the prevention of nosocomial infections. Here, we further tested the effects of Filastatin on C. albicans, showing promising uses as a pre-therapeutic material and even as a composition additive for silicone-based devices.
AFM measurements revealed that Filastatin-exposed C. albicans cells were unable to attach to abiotic surfaces and resembled those of the non-adherent edt1 −/− mutant cells. The effect of Filastatin is most dramatic when it is continuously present, because cells that were washed to remove Filastatin were capable of binding abiotic surfaces again, albeit with reduced efficiency. These results led us to explore surface-treatment with Filastatin. For this purpose, three biomaterials were tested for co-incubations with Filastatin, and surface-treatment experiments: polystyrene, silicone and acrylic dental resin. In each case, materials treated with Filastatin showed a dramatic decrease in the number of cells adhered and correlated well with results of experiments where cells were co-incubated with Filastatin. The extent of adhesion of cells co-incubated with Filastatin was greater in polystyrene and silicone compared to acrylic dental resin. These results might be caused by DMSO, due to its moderate compatibility/solubility with PDMS and polystyrene [58]. In this present report, the nature of Filastatin attachment to surfaces is ill understood. We conducted preliminary studies using Quartz Crystal Microbalance with Dissipation monitoring technology (QCM-D), which showed Filastatin covering the surface of an APTMS-treated crystal. Future studies will focus on better methods to tether Filastatin to biomaterials.
Our results involving bioactive glass surfaces and plastics confirmed the efficacy of Filastatin as a potent anti-adhesion molecule for C. albicans in concentrations as low as 12.5 µM while in co-incubation. Moreover, this effect also extents to C. dubliniensis, C. parapsilosis and C. tropicalis [10]. Due to its potential use as a pre-therapeutic drug, IES and a microfluidics bioreactor were used to determine the effect of Filastatin under a microenvironment that mimics physiological flow conditions of bodily fluids. The impedance readings can be interpreted as a disruption on the adhesive properties of C. albicans cells in the presence of Filastatin, reinstating not only the efficacy of this molecule under steady conditions but also under flow conditions.
It is known that C. albicans cell surface interacts directly with host cells and is highly dynamic [59]. Its protein composition changes in the presence of environmental stresses, during switching between budded and hyphal morphologies and also when treated with antifungal agents [59, 60]. Notably, cell surface proteins, nutrient sensing and uptake, morphological switching, and biofilm formation are interrelated factors that contribute directly to the virulence and fitness of C. albicans within the host environment [59, 61,62,63]. Therefore, discovery of compounds that block adhesion, perturb morphological switching and reduce biofilm formation or limit uptake of essential nutrients by C. albicans would be an important first step towards developing new antifungal therapeutics.
Conclusion
We have shown that Filastatin is an effective agent against C. albicans adhesion to multiple surfaces under steady and dynamic conditions. Furthermore, C. albicans was unable to attach to biomaterials treated with Filastatin. Future studies will focus on the molecular targets of Filastatin and tethering to biomaterials, as well as in safety and of Filastatin as a pre-therapeutic coating.
Abbreviations
- AFM:
-
atomic force microscopy/microscope
- APTMS:
-
(3-aminopropyl) trimethoxysilane
- CDC:
-
Center for Disease Control
- diH2O:
-
deionized water
- DMSO:
-
dimethyl sulfoxide
- EIS:
-
electrochemical impedance spectroscopy
- HIV:
-
human immunodeficiency virus
- IDE:
-
interdigitated electrode
- PDMS:
-
polydimethylsiloxane
- PI:
-
propidium iodide
- QCM-D:
-
quartz crystal microbalance with dissipation monitoring
- SC:
-
synthetic complete (media)
- TSB:
-
tryptic soy broth
References
Scott RD. The direct medical costs of healthcare-associated infections in US hospitals and the benefits of prevention: Division of Healthcare Quality Promotion National Center for Preparedness, Detection, and Control of Infectious Diseases, Centers for Disease Control and Prevention; 2009.
Pfaller MA. Nosocomial candidiasis: emerging species, reservoirs, and modes of transmission. Clin Infect Dis. 1996;22(Suppl 2):S89–94.
Kabir MA, Hussain MA, Ahmad Z. Candida albicans: a model organism for studying fungal pathogens. ISRN Microbiol. 2012;2012:538694.
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis. 2004;39(3):309–17.
Low CY, Rotstein C. Emerging fungal infections in immunocompromised patients. F1000 Med Rep. 2011;3:14.
Barnes RA. Early diagnosis of fungal infection in immunocompromised patients. J Antimicrob Chemother. 2008;61(Suppl 1):i3–6.
Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev. 2007;20(1):133–63.
Schelenz S. Management of candidiasis in the intensive care unit. J Antimicrob Chemother. 2008;61(Suppl 1):i31–4.
Miceli MH, Diaz JA, Lee SA. Emerging opportunistic yeast infections. Lancet Infect Dis. 2011;11(2):142–51.
Fazly A, Jain C, Dehner AC, Issi L, Lilly EA, Ali A, Cao H, Fidel PL Jr, Rao RP, Kaufman PD. Chemical screening identifies filastatin, a small molecule inhibitor of Candida albicans adhesion, morphogenesis, and pathogenesis. Proc Natl Acad Sci USA. 2013;110(33):13594–9.
Wilson LS, Reyes CM, Stolpman M, Speckman J, Allen K, Beney J. The direct cost and incidence of systemic fungal infections. Value Health. 2002;5(1):26–34.
Spampinato C, Leonardi D. Candida infections, causes, targets, and resistance mechanisms: traditional and alternative antifungal agents. Biomed Res Int. 2013;2013:204237.
Giusiano G, Mangiaterra M, Garcia Saito V, Rojas F, Gomez V, Diaz MC. Fluconazole and itraconazole resistance of yeasts isolated from the bloodstream and catheters of hospitalized pediatric patients. Chemotherapy. 2006;52(5):254–9.
Wang Y, Liu JY, Shi C, Li WJ, Zhao Y, Yan L, Xiang MJ. Mutations in transcription factor Mrr2p contribute to fluconazole resistance in clinical isolates of Candida albicans. Int J Antimicrob Agents. 2015;46:552.
Rosana Y, Yasmon A, Lestari DC. Overexpression and mutation as a genetic mechanism of fluconazole resistance in Candida albicans isolated from human immunodeficiency virus patients in Indonesia. J Med Microbiol. 2015;64(9):1046–52.
Zhang SQ, Miao Q, Li LP, Zhang LL, Yan L, Jia Y, Cao YB, Jiang YY. Mutation of G234 amino acid residue in Candida albicans drug-resistance-related protein Rta2p is associated with fluconazole resistance and dihydrosphingosine transport. Virulence. 2015;6(6):611–9.
Sobel JD. Vaginitis. N Engl J Med. 1997;337(26):1896–903.
Ruhnke M, Maschmeyer G. Management of mycoses in patients with hematologic disease and cancer—review of the literature. Eur J Med Res. 2002;7(5):227–35.
Pappas PG, Rex JH, Lee J, Hamill RJ, Larsen RA, Powderly W, Kauffman CA, Hyslop N, Mangino JE, Chapman S, et al. A prospective observational study of candidemia: epidemiology, therapy, and influences on mortality in hospitalized adult and pediatric patients. Clin Infect Dis. 2003;37(5):634–43.
Sexton JA, Brown V, Johnston M. Regulation of sugar transport and metabolism by the Candida albicans Rgt1 transcriptional repressor. Yeast. 2007;24(10):847–60.
Pfaller MA. Epidemiology of nosocomial candidiasis: the importance of molecular typing. Braz J Infect Dis. 2000;4(4):161–7.
Jarvis WR. Epidemiology of nosocomial fungal infections, with emphasis on Candida species. Clin Infect Dis. 1995;20(6):1526–30.
Leroy O, Gangneux JP, Montravers P, Mira JP, Gouin F, Sollet JP, Carlet J, Reynes J, Rosenheim M, Regnier B, et al. Epidemiology, management, and risk factors for death of invasive Candida infections in critical care: a multicenter, prospective, observational study in France (2005–2006). Crit Care Med. 2009;37(5):1612–8.
Barberino MG, Silva N, Reboucas C, Barreiro K, Alcantara AP, Netto EM, Albuquerque L, Brites C. Evaluation of blood stream infections by Candida in three tertiary hospitals in Salvador, Brazil: a case-control study. Braz J Infect Dis. 2006;10(1):36–40.
Chandra J, Kuhn DM, Mukherjee PK, Hoyer LL, McCormick T, Ghannoum MA. Biofilm formation by the fungal pathogen Candida albicans: development, architecture, and drug resistance. J Bacteriol. 2001;183(18):5385–94.
Mathe L, Van Dijck P. Recent insights into Candida albicans biofilm resistance mechanisms. Curr Genet. 2013;59(4):251–64.
Antifungal Resistance. http://www.cdc.gov/fungal/antifungal-resistance.html.
Palanisamy SK, Ramirez MA, Lorenz M, Lee SA. Candida albicans PEP12 is required for biofilm integrity and in vivo virulence. Eukaryot Cell. 2010;9(2):266–77.
Samaranayake YH, Cheung BP, Yau JY, Yeung SK, Samaranayake LP. Human serum promotes Candida albicans biofilm growth and virulence gene expression on silicone biomaterial. PLoS ONE. 2013;8(5):e62902.
de Vasconcellos AA, Goncalves LM, Del Bel Cury AA, da Silva WJ. Environmental pH influences Candida albicans biofilms regarding its structure, virulence and susceptibility to fluconazole. Microb Pathog. 2014;69–70:39–44.
Bronzino JD. The biomedical engineering handbook 1. Berlin: Springer; 2000.
Srivatsan TS. Processing and fabrication of advanced materials, XVII: part 8: polymer-based composites and nano composites, vol. 2. New Delhi: I.K. International Publishing House; 2009.
Ellepola AN, Samaranayake LP. Adhesion of oral Candida albicans isolates to denture acrylic following limited exposure to antifungal agents. Arch Oral Biol. 1998;43(12):999–1007.
Nevzatoglu EU, Ozcan M, Kulak-Ozkan Y, Kadir T. Adherence of Candida albicans to denture base acrylics and silicone-based resilient liner materials with different surface finishes. Clin Oral Invest. 2007;11(3):231–6.
Ramage G, Martinez JP, Lopez-Ribot JL. Candida biofilms on implanted biomaterials: a clinically significant problem. FEMS Yeast Res. 2006;6(7):979–86.
O’Grady NP, Alexander M, Dellinger EP, Gerberding JL, Heard S, Maki D, Masur H, McCormick R, Mermel L, Pearson M. Draft guideline for the prevention of intravascular catheter-related infections. Atlanta: Centers for Disease Control; 2001.
Carlson RP, Taffs R, Davison WM, Stewart PS. Anti-biofilm properties of chitosan-coated surfaces. J Biomater Sci Polym Ed. 2008;19(8):1035–46.
Alalwan H, Rajendran R, Lappin DF, Combet E, Shahzad M, Robertson D, Nile CJ, Williams C, Ramage G. The anti-adhesive effect of curcumin on Candida albicans biofilms on denture materials. Front Microbiol. 2017;8:659.
Kucharikova S, Gerits E, De Brucker K, Braem A, Ceh K, Majdic G, Spanic T, Pogorevc E, Verstraeten N, Tournu H, et al. Covalent immobilization of antimicrobial agents on titanium prevents Staphylococcus aureus and Candida albicans colonization and biofilm formation. J Antimicrob Chemother. 2016;71(4):936–45.
Gillum AM, Tsay EY, Kirsch DR. Isolation of the Candida albicans gene for orotidine-5′-phosphate decarboxylase by complementation of S. cerevisiae ura3 and E. coli pyrF mutations. Mol General Genet MGG. 1984;198(2):179–82.
Brothers KM, Newman ZR, Wheeler RT. Live imaging of disseminated candidiasis in zebrafish reveals role of phagocyte oxidase in limiting filamentous growth. Eukaryot Cell. 2011;10(7):932–44.
Wheeler RT, Kombe D, Agarwala SD, Fink GR. Dynamic, morphotype-specific Candida albicans beta-glucan exposure during infection and drug treatment. PLoS Pathog. 2008;4(12):e1000227.
Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, Preibisch S, Rueden C, Saalfeld S, Schmid B, et al. Fiji: an open-source platform for biological-image analysis. Nat Methods. 2012;9(7):676–82.
Asami K, Hanai T, Koizumi N. Dielectric properties of yeast cells. J Membr Biol. 1976;28(2–3):169–80.
Benson K, Cramer S, Galla HJ. Impedance-based cell monitoring: barrier properties and beyond. Fluids Barriers CNS. 2013;10(1):5.
Bruchmann J, Sachsenheimer K, Rapp BE, Schwartz T. Multi-channel microfluidic biosensor platform applied for online monitoring and screening of biofilm formation and activity. PLoS ONE. 2015;10(2):e0117300.
Stone SD, Hollins BC. Modeling shear stress in microfluidic channels for cellular applications. In: Biomedical engineering conference (SBEC), 2013 29th Southern: 3–5 May 2013; 2013. p. 117–8.
Lu H, Koo LY, Wang WM, Lauffenburger DA, Griffith LG, Jensen KF. Microfluidic shear devices for quantitative analysis of cell adhesion. Anal Chem. 2004;76(18):5257–64.
De Oliveira R, Albuquerque D, Leite F, Yamaji F, Cruz T. Measurement of the nanoscale roughness by atomic force microscopy: basic principles and applications. Croatia: INTECH Open Access Publisher; 2012.
K’Owino IO, Sadik OA. Impedance spectroscopy: a powerful tool for rapid biomolecular screening and cell culture monitoring. Electroanalysis. 2005;17(23):2101–13.
Fidel PL Jr, Sobel JD. Immunopathogenesis of recurrent vulvovaginal candidiasis. Clin Microbiol Rev. 1996;9(3):335–48.
Gudlaugsson O, Gillespie S, Lee K, Vande Berg J, Hu J, Messer S, Herwaldt L, Pfaller M, Diekema D. Attributable mortality of nosocomial candidemia, revisited. Clin Infect Dis. 2003;37(9):1172–7.
Rangel-Frausto MS, Wiblin T, Blumberg HM, Saiman L, Patterson J, Rinaldi M, Pfaller M, Edwards JE Jr, Jarvis W, Dawson J, et al. National epidemiology of mycoses survey (NEMIS): variations in rates of bloodstream infections due to Candida species in seven surgical intensive care units and six neonatal intensive care units. Clin Infect Dis. 1999;29(2):253–8.
Centres for Disease Control and Prevention (CDC) Prevention: Antibiotic resistance threats in the United States, 2013. US Department of Health and Human Services; 2013.
Laxminarayan R, Duse A, Wattal C, Zaidi AK, Wertheim HF, Sumpradit N, Vlieghe E, Hara GL, Gould IM, Goossens H. Antibiotic resistance—the need for global solutions. Lancet Infect Dis. 2013;13(12):1057–98.
Finkel JS, Mitchell AP. Genetic control of Candida albicans biofilm development. Nat Rev Microbiol. 2011;9(2):109–18.
Pierce CG, Chaturvedi AK, Lazzell AL, Powell AT, Saville SP, McHardy SF, Lopez-Ribot JL. A novel small molecule inhibitor of Candida albicans biofilm formation, filamentation and virulence with low potential for the development of resistance. NPJ Biofilms Microb. 2015;1:15012.
Product information sheet for DMSO. https://www.sigmaaldrich.com/content/dam/sigma-aldrich/docs/Sigma/Product_Information_Sheet/d2650pis.pdf.
Chaffin WL. Candida albicans cell wall proteins. Microbiol Mol Biol Rev MMBR. 2008;72(3):495–544.
Dranginis AM, Rauceo JM, Coronado JE, Lipke PN. A biochemical guide to yeast adhesins: glycoproteins for social and antisocial occasions. Microbiol Mol Biol Rev MMBR. 2007;71(2):282–94.
Lo HJ, Kohler JR, DiDomenico B, Loebenberg D, Cacciapuoti A, Fink GR. Nonfilamentous C. albicans mutants are avirulent. Cell. 1997;90(5):939–49.
d’Enfert C. Hidden killers: persistence of opportunistic fungal pathogens in the human host. Curr Opin Microbiol. 2009;12(4):358–64.
Blankenship JR, Mitchell AP. How to build a biofilm: a fungal perspective. Curr Opin Microbiol. 2006;9(6):588–94.
Authors’ contributions
DVB, RPR, CL and AL contributed to the intellectual content, experimental design of the study. DVB and RPR drafted the manuscript. DVB and AL carried out the laboratory studies, JR and RN performed the AFM studies, AS designed and prepared the microfluidics device used in this study. CL was involved with critically evaluation and constructive discussions during all stages of this study. All authors read and approved the final manuscript.
Acknowledgements
The authors thank Dr. Mairi Noverr (LSU Health Science Center) for generously providing the dental resins used in this study. We would like to acknowledge, T. Gawain for his help in the acquisition of the AFM data.
Competing interests
The authors declare that they have no competing interests.
Funding
This work was partially supported by a WPI, Pilot Project Initiative Grant to RPR. DVB was partially supported by the LASPAU, Fulbright Foreign Student Program.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Vargas-Blanco, D., Lynn, A., Rosch, J. et al. A pre-therapeutic coating for medical devices that prevents the attachment of Candida albicans . Ann Clin Microbiol Antimicrob 16, 41 (2017). https://doi.org/10.1186/s12941-017-0215-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-017-0215-z