Abstract
Background
Brominated Flame Retardants (BFRs) have attracted widespread concern due to their environmental persistence and potential toxicity. This study aims to examine the association between BFRs exposure and hypertension.
Methods
We used data from the National Health and Nutrition Examination Survey (NHANES) spanning 2005 to 2016 for the cross-sectional analysis. To evaluate the individual and combined impacts of BFRs exposure on hypertension, we utilized multivariate models, including generalized additive models, weighted quantile sum (WQS) regression, and Bayesian kernel machine regression (BKMR) models.
Results
9882 individuals (48% male) aged ≥ 20 were included in the final analysis, of whom 4114 had hypertension. After controlling for potential covariates, higher serum concentrations of PBDE100 (OR: 1.26; 95% CI: 1.01, 1.57) and PBDE153 (OR: 1.50; 95% CI: 1.18, 1.88) were significantly associated with hypertension. A nonlinear relationship between PBDE28 and hypertension was observed (P = 0.03). Moreover, BFRs mixture were positively associated with the prevalence of hypertension in both the WQS (β:1.09; 95% CI: 1.02, 1.17; P = 0.02) and BKMR models.
Conclusion
Our study suggested that BFRs exposure is positively associated with hypertension in the general population. To confirm this association and elucidate the mechanisms, further research is required.
Similar content being viewed by others
Introduction
Brominated Flame Retardants (BFRs) are chemical compounds widely used in various products such as plastics, furniture, textiles, construction materials, and electrical and electronic devices to adhere to fire safety standards [1,2,3]. Due to the persistence, accumulation and environmental ubiquity, BFRs can be detected in wildlife around the world and in humans [4,5,6], even in newborns [7], which has raised considerable attention. Polybrominated diphenyl ethers (PBDEs) and polybrominated biphenyls (PBBs), as subgroups of BFRs, are considered more hazardous than other types [8]. PBDEs are classified into three principal varieties: penta-BDE, octa-BDE, and deca-BDE. Penta- and Octa-BDE were removed from the broad market in the United States in 2004, while the production and importation of deca-BDE ceased in 2013 [9]. The Stockholm Convention, an international treaty managed by the United Nations Environment Program, has categorized certain BFRs (such as PBDEs and PBBs) as persistent organic pollutants (POPs), leading to their restricted use and gradual phase-out [10]. Despite these restrictions, BFRs can still be consistently detected in consumer durables, foods and indoor dust. Prior research has revealed that BFRs can cause a range of harmful effects, including endocrine disruption, neurotoxicity, liver, and kidney damage, as well as negative impacts on reproduction and development, posing risks to the environment and human well-being [11,12,13,14,15,16]. Nevertheless, the cardiovascular implications of exposure to BFRs have not been thoroughly studied.
Hypertension, a prevalent cardiovascular disease (CVD) worldwide, impacts approximately 1.28 billion adults aged 30 to 79. In the United States, the age-adjusted prevalence of hypertension was 45.1% as of 2021 [17]. Elevated blood pressure is consistently associated with the development and progression of coronary artery disease, chronic renal disease, and stroke [18, 19]. Furthermore, hypertension frequently coexists with dyslipidemia, glucose intolerance, and type 2 diabetes, hence increasing the risk of CVD [20]. In addition to hereditary factors, hypertension is mainly affected by lifestyles, physical inactivity, psychological stress, and exposure to specific environmental contaminants [21,22,23]. There is increasing worry about environmental toxins, including heavy metals, air pollution, and POPs. Everett found that greater serum levels of polychlorinated biphenyl (PCB) 138 and PCB126 were associated with an elevated risk of hypertension, based on data from the National Health and Nutrition Examination Survey (NHANES) [24]. Valera discovered a direct correlation between PCB138 and hypertension risk among the Inuit population highly exposed to PCB138 [25]. While PBDEs and PCBs have comparable chemical structures and functional mechanisms, few studies have investigated the effect of BFRs exposure on hypertension in the general population.
Our study aims to delve the effect of BFRs exposure on hypertension by using the NHANES database. Additionally, we explore whether specific population subsets exhibit a more pronounced association between BFRs exposure and hypertension.
Methods
Study population
The data was obtained from NHANES, a nationwide cross-sectional survey conducted by the National Center for Health Statistics (NCHS) and the Centers for Disease Control and Prevention (CDC), to evaluate the health and nutritional conditions of the general U.S. population. The comprehensive survey design, methodologies, and data are available on the NHANES website (https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/BFRPOL_I.htm). The NHANES study protocol received approval from the NCHS research ethics review board, and participants gave written informed consent at enrollment. A total of 12,333 individuals from six consecutive cycles (NHANES 2005–2016), who underwent a series of serum BFRs measurements, were initially included. 45 subjects with missing data on blood pressure and 2406 subjects aged < 20 years were excluded. Finally, 9882 individuals were enrolled in the analyses (Fig. 1).
Exposure variables
To avoid additional variability and potential bias introduced by lipid adjustment, we used serum BFR concentrations to reflect individual exposure levels [26, 27]. The quantification of PBB-153 and 11 PBDEs in serum was performed using automated liquid-liquid extraction and dilution gas chromatography high-resolution mass spectrometry. Table S1 illustrates the rates of detection and distribution of BFRs. To ensure the reliability of our study, we chose PBB153 and eight PBDEs with a detection rate over 65% as exposure factors. The eight PBDEs include 2,4,4´-Tribromodiphenyl ether (PBDE28), 2,2´,4,4´-Tetrabromodiphenyl ether (PBDE47), 2,2´,3,4,4´-Tetrabromodiphenyl ether (PBDE85), 2,2´,4,4´,5-Pentabromodiphenyl ether (PBDE99), 2,2´,4,4´,6-Pentabromodiphenyl ether (PBDE100), 2,2´,4,4´,5,5´-Hexabromodiphenyl ether (PBDE153), 2,2´,4,4´,5,6´-Hexabromodiphenyl ether (PBDE154), Decabromodiphenyl ether (PBDE209). Concentrations of serum BFRs below the lower limit of detection (LOD) were determined with the LOD value divided by the square root of 2.
Outcome definition
In this study, the occurrence of hypertension is the primary outcome. During the personal interview addressing various health concerns, a standardized medical questionnaire was employed. Participants were queried, ‘Has a doctor or any medical professional ever informed you a diagnosis of high blood pressure or hypertension?’ Those who affirmed were categorized as hypertensive, while negative responses indicated an absence of hypertension. During each interview, the participants were also asked to report the medications that they have taken in the past 30 days. The blood pressures (BP) measurements of participants were taken by trained physicians in the mobile examination center (MEC). After five minutes of quiet sitting, participants take three consecutive BP readings to obtain the maximum inflation level (MIL). A fourth try is allowed in cases where the measurement is interrupted or incomplete. The average of the three or four BP recordings was calculated as systolic blood pressure (SBP) and diastolic blood pressure (DBP) for each participant. Hypertension was defined based on participants meeting at least one of the following criteria: (1) self-reported diagnosis of hypertension; (2) self-reported antihypertensive medication use; (3) SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg.
Covariates
Based on previous literature [28,29,30,31,32], we incorporated a number of potentially confounding variables, including age, gender, race, education level, the family income to poverty ratio (PIR), serum cotinine, alcohol consumption, sleep disorders, depression, physical activity, dietary sodium intake, dietary potassium intake, body mass index (BMI), eGFR, history of diabetes and NHANES cycles (Figure S1). Demographic data, lifestyle information, disease history and physical measurements as well as laboratory tests were collected and administered by trained staffs according to standardized questionnaires and MEC. Demographic characteristics, including age (years) (20 ≤ Age < 65, Age ≥ 65), gender (male, female), race (Non-Hispanic White, Non-Hispanic Black, Mexican American, Other Race), education level (below high school, high school, above high school) and PIR (< 1, 1–3, > 3). PIR was calculated by dividing the yearly household income by the poverty threshold for the family size in the state of residence for that year, according to federal criteria. In this study, PIR was recoded as a dichotomous variable. Lifestyle included serum cotinine (≤ 1 µg/L, > 1 µg/L), alcohol consumption (< 12 drinks, ≥ 12 drinks), sleep disorders (yes or no), depression (yes or no), physical activity (activity or inactivity), dietary sodium intake (milligrams) and dietary potassium intake (milligrams). Serum cotinine levels indicate both active and passive smoking and was categorized into two groups (≤ 1 µg/L, > 1 µg/L) to distinguish between smokers and non-smokers [33]. Alcohol consumption was assessed by the question: “In any one year, have you had at least 12 drinks of any type of alcoholic beverage?” (yes/no). Sleeping disorders was evaluated with the question: “Have you ever informed a doctor or other health professional that you have difficulty sleeping?” (yes/no). Depression was tested using the Patient Health Questionnaire (PHQ-9), with total scores ranging from 0 to 27 points. A cutoff score of 10 was used to identify clinically relevant depression. Physical activity and inactivity were defined as less than four hours of moderate to high physical activities per week, according to the WHO Global Physical Activity Questionnaire [34]. Dietary sodium and potassium intake was extracted from 24-h dietary recall interviews in the NHANES database. BMI was calculated as weight (kg) /height (m2). We categorized participants into three BMI groups: normal (< 25 kg/m2), overweight (25–29.9 kg/m2), and obese (≥ 30 kg/m2). The estimated glomerular filtration rate (eGFR) was determined for each participant based on the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation. Diabetes was defined as fasting plasma glucose (FPG) levels ≥ 7.0 mmol/L or/and glycosylated hemoglobin levels > 6.5%, self-reported diagnosis of diabetes or use of oral lowing glucose medications or insulin.
Statistical analysis
Baseline characteristics were compared between participants with and without hypertension using the t and χ2 test for continuous and categorical variables, respectively. Mean (standard deviation) or median with interquartile range (IQR) are used to display continuous values, while percentages are used for categorical variables. PBDEs and PBB-153 levels were log10 transformed to normalize the distribution. We applied the MEC weights according to NCHS guidance to account for the complex, multistage sampling design of the NHANES [35]. Weighted models were used in the multiple regression analyses.
We performed multivariate logistic regression analysis to assess the association between individual BFR and hypertension. Three models were applied, Model 1 was a crude model, Model 2 was controlled for age, race, and gender, and Model 3 was further controlled for education level, PIR, serum cotinine, alcohol consumption, sleep disorders, depression, physical activity, dietary sodium intake, dietary potassium intake, BMI, eGFR, history of diabetes and NHANES cycles based on Model 2. A generalized additive model investigated the nonlinear association between exposure to BFRs and hypertension. Wald χ2 tests were used to test for nonlinearity in the associations. Stratified analyses were performed by age, gender, education level, PIR, serum cotinine, alcohol consumption, sleep disorders, physical activity, BMI and history of diabetes. Interaction tests were also carried out to assess the individualized effects of BFRs on hypertension across different subgroups in the multivariate logistic regression model.
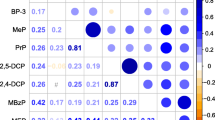
To investigate the effect of exposure to BFRs mixture on hypertension, we used the quantile weighted quantile sum (WQS) regression and Bayesian kernel machine regression (BKMR) analysis. Using a weighted index, in which the relative importance of each predictor variable establishes its total impact, the WQS regression assesses the combined impact of all predictor factors on the result. An estimation set comprising 40% of the training data and a validation set comprising 60% of the data were generated randomly. Bootstrap resampling, with 1000 iterations, facilitated the estimation of model parameters [36]. The BKMR provides succinct and versatile estimations of the multivariate exposure-response function [37, 38]. The integrative effect of the mixed BFRs on hypertension was determined by estimating the different risk of hypertension, when all 9 BFRs were maintained at the 10th to 90th percentiles (in increments of 10th percentile points) as compared to their 50th percentile. Moreover, we calculated the posterior inclusion probability (PIP) for each BRF in mixtures to determine the BRF that contributed most to the prevalence of hypertension. Following full covariate adjustment, this model underwent 10,000 iterations using Markov Chain Monte Carlo.
The statistical analyses were conducted using R software (version 3.6.0). A two-sided P value < 0.05 was considered statistically significant.
Results
Baseline characteristics
There were 4,114 cases of hypertension among the 9,882 participants in the study. The categories of hypertension diagnosis were listed in Table S2. Compared to those without hypertension, participants with hypertension were older, had a higher proportion of males, non-Hispanics, less educated, and prevalence of diabetes. PIR, sleep disorders, depression, physical activity, dietary sodium and potassium intake also differed between the two groups (P < 0.01). In addition, participants with hypertension have higher BMI and lower eGFR levels (Table 1). Participants with hypertension showed higher BFRs concentrations than those without hypertension (Table S3).
Associations between individual BFRs and hypertension
The multivariable logistic regression analysis revealed that all BFRs except PBDE209 were significantly positively associated with hypertension in model 1. After adjusting for demographic characteristics and all covariates, PBDE100 and PBDE153 were still significantly associated with hypertension, exhibiting 26% and 50% increase in odds (95% CI: 1.01, 1.57; P = 0.04; 95% CI: 1.18 1.88; P < 0.01; Table 2), respectively.
The generalized additive models revealed a non-linear relationship between PBDE28 and hypertension (P for nonlinear = 0.03). Non-linear relationships were not significantly observed for the remaining eight BFRs (P for non-linearity > 0.05) (Fig. 2).
Cubic splines for the associations of log-transformed serum BFRs with Hypertension. The horizontal dashed line represents the OR = 1.00. The red lines indicate multivariate-adjusted OR and the purple shaded area represents the 95%CI. All models were adjusted for age, gender, race, education level, PIR, serum cotinine, alcohol consumption, sleep disorders, depression, physical activity, dietary sodium intake, dietary potassium intake, BMI, eGFR, history of diabetes and NHANES cycles. lg, log-transformed; OR, odd ratio; CI, confidence interval
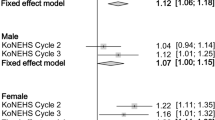
Stratified associations between BFRs and hypertension
As presented in Table 3, Interaction analyses demonstrated that PBB153 had obvious interaction with age and PBDE28 interacted with BMI. PBB153 was significantly associated with hypertension in participants with age < 65 (OR: 2.38; 95% CI: 2.05, 2.76; P < 0.001; P for interaction < 0.001), while PBDE28 (OR: 1.54; 95% CI: 1.04, 2.27; P = 0.03; P for interaction = 0.05) showed significantly association for hypertension in participants with BMI < 30. However, no significant differences were observed between subgroups stratified by gender, education level, PIR, serum cotinine, alcohol consumption, sleep disorders, physical activity and history of diabetes (Table S4).
Association between all BFRs and hypertension in WQS model
The multiple exposure effects of BFRs on hypertension were investigated using the WQS model. After accounting for all potential covariates, the WQS model identified a positive association between exposure to BFRs mixture and the prevalence of hypertension (β: 1.09; 95% CI: 1.02, 1.17; P = 0.02) (Fig. 3A; Table 4). Figure 3B presented that PBDE209 contributed the most to the WQS index, followed by PBDE100, PBDE153, PBDE28 and PBB153 were relatively important for hypertension due to their higher calculated weights. The WQS regression in the negative direction showed no significant association of the BFRs mixture with hypertension (β: 1.09; 95% CI: 0.99, 1.19; P = 0.07) (Table 4).
Association between BFRs exposure and hypertension by WQS model. (A) The combined effects of mixed exposure to BFRs. (B) The weights of each BFR for hypertension in positive direction. The dashed red line represents the cutoff value (by default equal to the inverse of the number of elements in the mixture). The model was adjusted for age, gender, race, education level, PIR, serum cotinine, alcohol consumption, sleep disorders, depression, physical activity, dietary sodium intake, dietary potassium intake, BMI, eGFR, history of diabetes and NHANES cycles. WQS, weighted quantile sum; lg, log-transformed
WQS, weighted quantile sum; lg, log-transformed.
Association between all BFRs and hypertension in BKMR model
In the BKMR model, Fig. S2 summarizes the results of the univariate exposure–response functions with other concentrations fixed at the median. A significant positive trend was observed between PBDE100 and hypertension. As shown in Fig. 4A, a significant overall association between exposure to BFRs mixture and increased risk of hypertension was observed when the mixture was at the 55th percentile or above, compared to their 50th percentile. Among BFRs mixtures, the highest PIPs for hypertension were estimated for PBBDE100 (PIP = 0.78) and PBDE154 (PIP = 0.40) (Fig. 4B). Meanwhile, the interaction between BFRs were not significant (Fig. S3).
Association between combined BFRs exposure and hypertension analyzed by BKMR model. (A) Overall effects of BFRs mixture on hypertension at all concentrations ranged from the first quantile (10%) to the third quantile (90%) relative to the median (50%) level. (B) Posterior inclusion probabilities (PIPs) of each BFR for hypertension. Adjusted for age, gender, race, education level, PIR, serum cotinine, alcohol consumption, sleep disorders, depression, physical activity, dietary sodium intake, dietary potassium intake, BMI, eGFR, history of diabetes and NHANES cycles
Discussion
In this study, various statistical approaches were employed to thoroughly evaluate the effects of both individual and mixed BFRs exposures on hypertension. Our research demonstrated that PBDE100 and PBDE153 were independently associated with the prevalence of hypertension after accounting for potential covariates. A nonlinear relationship between PBDE28 and hypertension was observed. Positive overall trends between BFRs mixture and hypertension were found in both the WQS and BKMR models.
Epidemiological studies on the relationship between BFRs exposure and hypertension are extremely sporadic. Smarr et al. reported an elevated odds of gestational hypertension associated with PBDE66, though this finding was not statistically significant [39]. Eslami et al. showed a significant correlation between total PBDEs and pre-eclampsia in first-time moms [40]. However, these studies focused on pregnant populations and did not investigate the correlation between PBDEs and hypertension in the general population. In contrast, our study indicated a positive association between BFRs and hypertension in general adults. Che et al. examined the association between BFRs and metabolic syndrome, including its components, using community-based data. Their research found no significant association between exposure to BFRs and hypertension [41]. The sample size of the study (4641 adults) was substantial for epidemiological research, but many cases were excluded for not meeting the inclusion criteria during the study period. Our study had a larger sample size, potentially increasing the statistical power and the ability to detect associations. The definition and determination of hypertension are consistent across both studies, as are the PBDEs and PBBs involved. However, variations in study periods may lead to differences in detection frequencies and levels of specific congeners. Additionally, our study included more covariates, whereas their study included fewer and different covariates, which may lead to residual confounding. Differences in population characteristics, covariate selection, and study periods may all contribute to the differing results. Our study included adults from six consecutive cycles from the NHANES database to evaluate the association between exposure to BFRs and hypertension. In the individual BFR analysis, PBDE100 and PBDE153 were significantly associated with hypertension. Meanwhile, we employed the WQS regression and BKMR models, two statistical tools, to examine the complexity of BFRs mixture exposure, avoiding the biases of traditional methods, which may simulate single chemical without considering the potential collinearity among similar compounds. To mitigate the effect of extreme concentrations and to evaluate the total risk of chemical exposure, WQS regression quantile-sorts continuous variables using bootstrap sample weights. In our study, the results from the WQS analysis indicate a significant positive association between mixed BFRs exposure and hypertension. Simultaneously, both the univariate exposure-response analysis and the combined exposure analysis using the BKMR model suggest that certain individual BFRs and mixed BFRs may exhibit a positive relationship with hypertension. In the WQS analysis, PBDE209 contributes the most to the WQS index, followed by PBDE100 and PBDE153, which have relatively greater impacts on hypertension. Meanwhile, in the BKMR model, PBDE100 has the highest PIPs. In the multivariable regression analysis, several PBDEs and PBB153 are significantly associated with hypertension in the crude model. Even after adjusting for all variables, PBDE100 and PBDE153 remain show significant association with hypertension. Across multiple statistical strategies applied in this study, PBDE100 consistently demonstrates a significant association with hypertension in both individual and mixed BFRs exposures.
Although the potential mechanisms by which BFRs exposure affects blood pressure are unclear, several hypotheses could be considered. First, evidence indicates that human exposure to certain POPs can disrupt lipid homeostasis, trigger diabetes, promote obesity, and related diseases [42,43,44], all of which are common conditions in hypertensive patients [45, 46]. Current biological evidence suggests that PBDEs may contribute to the development of gestational diabetes mellitus (GDM), with PBDE-154 being correlated with an increased risk of GDM [47]. GDM and type 2 diabetes are clinical manifestations of the same entity, both attributed to insulin resistance, which is a known precipitant of cardiovascular diseases including hypertension [48, 49]. Therefore, the link between POPs and hypertension may be due to the increases in dyslipidemia, diabetes, and/or obesity caused by POPs. Simultaneously, previous research has demonstrated that octa- and deca-BDEs can cause degenerative alterations and kidney histopathology in rats [50]. Perinatal exposure to PBDE mixtures (DE-71) in rats disrupts blood pressure homeostasis in later adulthood, which may partly result from toxic effects on the kidneys and renal pathology, leading to excessive sodium retention and hypertension [51]. Additionally, previous studies discovered that HepG2 cells, wild-type N2 worms, and adipocytes are susceptible to oxidative stress induced by PBDE-47 at different concentrations [15, 52]. The presence of reactive oxygen species, a hallmark of oxidative stress, was demonstrated in human umbilical vein endothelial cells exposed to PBDE-209 [53]. Another study based on NHANES data from 2007 to 2016 analyzed the relationship between BFR levels and oxidative stress markers in American adults, revealed a positive association of BFRs exposure with oxidative stress markers. According to clinical and experimental findings, hypertension is linked to inflammation and immune cell activation, which are mostly caused by oxidative stress [54]. Overall, we speculate that, BFRs, as a unique exogenous chemical, could influence blood pressure levels by affecting endocrine hormones, renal function, oxidative stress, and metabolic pathways. Prospective cohort studies and in vitro/vivo experimental research are needed to confirm and examine the precise relationship and underlying mechanisms between BFRs exposure and hypertension.
Our study possesses certain advantages: It is the first to examine the relationship between BFRs and hypertension in a nationally representative sample of US adults. This study employed generalized additive regression, WQS regression, and BKMR models to comprehensively investigate the impacts of exposure to individual and overall BFRs on hypertension. Nevertheless, this study has certain constraints. Firstly, the observational study methodology makes it impossible to establish any causal links based on this data. Secondly, there is currently no consensus on the optimal method for measuring lipophilic chemicals in serum. This study used serum BFR concentrations to indicate exposure levels, which may not fully represent individual exposure and could lead to measurement errors. Thirdly, despite frequently using covariates in regression models, it is important to acknowledge the potential influence of unmeasured confounding effects. Fourthly, the pathogenic properties and mechanisms of BFRs in animals and humans are unclear. Besides, since our study participants were American adults, the applicability of our findings to other populations remains uncertain. Future longitudinal studies are needed to establish a causal relationship between exposure to BFRs and hypertension and verify the findings in more extensive populations. Moreover, experimental exploration of the specific biological mechanisms of BFRs represents an important direction for future studies.
Conclusion
In summary, our investigation showed a significant positive association between BFRs exposure and hypertension in the general adults. This would help enhance public awareness about preventing exposure to BFRs. Further research would be required to confirm our findings and elucidate the potential mechanisms.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- BFRs:
-
Brominated flame retardants
- PBDEs:
-
Polybrominated diphenyl ethers
- PBBs:
-
Polybrominated biphenyls
- POPs:
-
Persistent organic pollutants
- CVD:
-
Cardiovascular disease
- PCB:
-
Polychlorinated biphenyl
- NHANES:
-
National health and nutrition examination survey
- MEC:
-
Mobile examination center
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- PIR:
-
The family income to poverty ratio
- WQS:
-
Weighted quantile sum
- BKMR:
-
Bayesian kernel machine regression
- BMI:
-
Body mass index
- eGFR:
-
Estimated glomerular filtration rate
- GDM:
-
Gestational diabetes mellitus
References
Siddiqi MA, Laessig RH, Reed KD. Polybrominated diphenyl ethers (PBDEs): new pollutants-old diseases. Clin Med Res. 2003;1(4):281–90.
Zota AR, Mitro SD, Robinson JF, Hamilton EG, Park JS, Parry E, et al. Polybrominated diphenyl ethers (PBDEs) and hydroxylated PBDE metabolites (OH-PBDEs) in maternal and fetal tissues, and associations with fetal cytochrome P450 gene expression. Environ Int. 2018;112:269–78.
Kim UJ, Oh JE. Tetrabromobisphenol A and hexabromocyclododecane flame retardants in infant-mother paired serum samples, and their relationships with thyroid hormones and environmental factors. Environ Pollut. 2014;184:193–200.
Vanden BM, Weijs L, Habran S, Das K, Bugli C, Pillet S, et al. Effects of polychlorobiphenyls, polybromodiphenylethers, organochlorine pesticides and their metabolites on vitamin A status in lactating grey seals. Environ Res. 2013;120:18–26.
Shaw SD, Kannan K. Polybrominated diphenyl ethers in marine ecosystems of the American continents: foresight from current knowledge. Rev Environ Health. 2009;24(3):157–229.
Hohenblum P, Steinbichl P, Raffesberg W, Weiss S, Moche W, Vallant B, et al. Pollution gets personal! A first population-based human biomonitoring study in Austria. Int J Hyg Environ Health. 2012;215(2):176–9.
Terry P, Towers CV, Liu LY, Peverly AA, Chen J, Salamova A. Polybrominated diphenyl ethers (flame retardants) in motherinfant pairs in the Southeastern U.S. Int J Environ Health Res. 2017;27(3):205–14.
Rani M, Keshu, Meenu, Sillanp¨a¨a M, Shanker U. An updated review on environmental occurrence, scientific assessment and removal of brominated flame retardants by engineered nanomaterials. J Environ Manage. 2022;1:321115998.
Sharkey M, Harrad S, Abou-Elwafa AM, Drage DS, Berresheim H. Phasing-out of legacy brominated flame retardants: the UNEP Stockholm Convention and other legislative action worldwide. Environ Int. 2020;144:106041.
Wu Z, He C, Han W, Song J, Li HJ, Zhang YD, et al. Exposure pathways, levels and toxicity of polybrominated diphenyl ethers in humans: a review. Environ Res. 2020;187:109531.
Chen L, Yu K, Huang C, Yu L, Zhu B, Lam PK, et al. Prenatal transfer of polybrominated diphenyl ethers (PBDEs) results in developmental neurotoxicity in zebrafish larvae. Environ Sci Technol. 2012;46(17):9727–34.
Kuriyama SN, Wanner A, Fidalgo-Neto AA, Talsness CE, Koerner W, Chahoud I. Developmental exposure to low-dose PBDE-99: tissue distribution and thyroid hormone levels. Toxicology. 2007;242:80–90.
Yang LZ, Sun PX, Tao L, Zhao XM. An in silico study on human carcinogenicity mechanism of polybrominated biphenyls exposure. Chem Biol Interact. 2024;28:397.
Macaulay LJ, Chernick M, Chen A, Hinton DE, Bailey JM, Kullman SW, et al. Exposure to a PBDE/OH-BDE mixture alters juvenile zebrafish (Danio rerio) development. Environ Toxicol Chem. 2017;36(1):36–48.
Yang J, Zhao H, Chan KM. Toxic effects of polybrominated diphenyl ethers (BDE 47 and 99) and localization of BDE-99-induced cyp1a mRNA in zebrafish larvae. Toxicol Rep. 2017;4:614–24.
Emond C, Raymer JH, Studabaker WB, Garner CE, Birnbaum LS. A physiologically based pharmacokinetic model for developmental exposure to BDE-47 in rats. Toxicol Appl Pharmacol. 2010;242(3):290–8.
Stierman B, Afful J, Carroll MD, Chen TC, Davy O, Fink S et al. National Health and Nutrition Examination Survey 2017-March 2020 prepandemic data files—development of files and prevalence estimates for selected health outcomes. Natl Health Stat Rep. 2021; 158.
Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18(11):785–802.
Nguyen TN, Chow CK. Global and national high blood pressure burden and control. Lancet. 2021;398:932–3.
Sehestedt T, Hansen TW, Li Y, Richart T, Boggia J, Kikuya M, et al. Are blood pressure and diabetes additive or synergistic risk factors? Outcome in 8494 subjects randomly recruited from 10 populations. Hypertens Res. 2011;34(6):714–21.
Valenzuela PL, Carrera BP, Gálvez BG, Ruiz HG, Ordovas JM, Ruilope LM, et al. Lifestyle interventions for the prevention and treatment of hypertension. Nat Rev Cardiol. 2021;18(4):251–75.
Salamanca FE, Vela SF, Rodríguez BM, Arrebola MA, Iribarne LM, Olea N, et al. Serum levels of non-persistent environmental pollutants and risk of incident hypertension in a subcohort from the EPIC study. Environ Res. 2021;193:110491.
Xu J, Niehoff NM, White AJ, Werder EJ, Sandler DP. Fossil-fuel and combustion-related air pollution and hypertension in the Sister Study. Environ Pollut. 2022;15:315.
Everett CJ, Mainous AG 3rd, Frithsen IL, Player MS, Matheson EM. Association of polychlorinated biphenyls with hypertension in the 1999–2002 National Health and Nutrition Examination Survey. Environ Res. 2008;108(1):94–7.
Valera B, Jorgensen ME, Jeppesen C, Bjerregaard P. Exposure to persistent organic pollutants and risk of hypertension among Inuit from Greenland. Environ Res. 2013;122:65–73.
Schisterman EF, Whitcomb BW, Louis GM, Louis TA. Lipid adjustment in the analysis of environmental contaminants and human health risks. Environ Health Perspect. 2005;113:853–7.
Donat-Vargas C, Åkesson A, Tornevi A, Wennberg M, Sommar J, Kiviranta H, et al. Persistent organochlorine pollutants in plasma, blood pressure, and hypertension in a longitudinal study. Hypertension. 2018;71:1258–68.
Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018ESC/ESH guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953–2041.
Cai YJ, Chen MS, Zhai WX, Wang CH. Interaction between trouble sleeping and depression on hypertension in the NHANES 2005–2018. BMC Public Health. 2022;22:481.
Kou CK, Zhao X, Fan X, Lin X, Wang QY, Yu J. Dietary sodium/potassium intake and cognitive impairment in older patients with hypertension: data from NHANES 2011–2014. J Clin Hypertens. 2023;25:534–44.
Börjesson M, Onerup A, Lundqvist S, Dahlöf B. Physical activity and exercise lower blood pressure in individuals with hypertension: narrative review of 27 RCTs. Br J Sports Med. 2016;50:356–61.
Landsberg L. Insulin-mediated sympathetic stimulation: role in the pathogenesis of obesity-related hypertension (or, how insulin affects blood pressure, and why). J Hypertens. 2001;19:523–8.
Hudson-Hanley B, Smit E, Branscum A, Hystad P, Kile ML. Trends in urinary metabolites of polycyclic aromatic hydrocarbons (PAHs) in the non-smoking U.S. population, NHANES 2001–2014. Chemosphere. 2021;276:130211.
Akpa OM, Okekunle AP, Ovbiagele B, Sarfo FS, Akinyemi RO, Akpalu A, et al. Factors associated with hypertension among stroke-free indigenous africans: findings from the SIREN study. J Clin Hypertens. 2021;23(4):773–84.
Akinbam L, Chen TC, Davy O, Ogden C, Fink S, Clark J, et al. National Health and Nutrition Examination Survey, 2017-March 2020 Prepandemic file: Sample Design, Estimation, and Analytic guidelines. Vital Health Stat1. 2022;190:1–36.
Carrico C, Gennings C, Wheeler DC, Factor-Litvak P. Characterization of weighted quantile sum regression for highly correlated data in a risk analysis setting. J Agric Biol Environ Stat. 2015;20(1):100–20.
Bobb JF, Claus Henn B, Valeri L, Coull BA. Statistical software for analyzing the health effects of multiple concurrent exposures via bayesian kernel machine regression. Environ Health. 2018;17(1):67.
Bobb JF, Valeri L, Claus Henn B, Christiani DC, Wright RO, Mazumdar M, et al. Bayesian kernel machine regression for estimating the health effects of multipollutant mixtures. Biostatistics. 2015;16(3):493–508.
Smarr MM, Grantz KL, Zhang C, Sundaram R, Maisog JM, Barr DB, et al. Persistent organic pollutants and pregnancy complications. Sci Total Enviro. 2016;1:551–2.
Eslami B, Malekafzali H, Rastkari N, Rashidi BH, Djazayeri A, Naddafi K. 870 Association of serum concentrations of persistent organic pollutants (POPs) and risk of 871 pre-eclampsia: a case-control study. J Environ Health Sci Eng. 2016;24:14: 17.
Che Z, Jia H, Chen R, Pan K, Fan Z, Su C, et al. Associations between exposure to brominated flame retardants and metabolic syndrome and its components in U.S. adults. Sci Total Environ. 2023;858(Pt 2):159935.
Arrebola JP, Gonzalez-Jimenez A, Fornieles-Gonzalez C, Artacho-Cordon F, Olea N, Escobar-Jimenez F, et al. Relationship between serum concentrations of persistent organic pollutants and markers of insulin resistance in a cohort of women with a history of gestational diabetes mellitus. Environ Res. 2014;136:435–40.
Lind PM, Penell J, Salihovic S, Bavel BV, Lind L. Circulating levels of p,p′-DDE are related to prevalent hypertension in the elderly. Environ Res. 2014;129:27–31.
Sharpe RM, Drake AJ. Obesogens and obesity – an alternative view? Obesity. 2013;21(6):1081–3.
de Simone G, Devereux RB, Chinali M, Roman MJ, Best LG, Welty TK, et al. Risk factors for arterial hypertension in adults with initial optimal blood pressure: the strong heart study. Hypertension. 2006;47(2):162–7.
de Winter CF, Bastiaanse LP, Hilgenkamp TI, Evenhuis HM, Echteld MA. Cardiovascular risk factors (diabetes, hypertension, hypercholesterolemia and metabolic syndrome) in older people with intellectual disability: results of the HA-ID study. Res Dev Disabil. 2012;33(6):1722–31.
Rahman ML, Zhang C, Smarr MM, Lee S, Honda M, Kannan K, et al. Persistent organic pollutants and gestational diabetes: a multi-center prospective cohort study of healthy US women. Environ Int. 2019;124:249–58.
Wang F, Han L, Hu D. Fasting insulin, insulin resistance and risk of hypertension in the general population: a meta-analysis. Clin Chim Acta. 2017;464:57–63.
Zhu B, Wang J, Chen K, Yan W, Wang A, Wang W, et al. A high triglyceride glucose index is more closely associated with hypertension than lipid or glycemic parameters in elderly individuals: a cross-sectional survey from the reaction study. Cardiovasc Diabetol. 2020;19(1):112.
Gill U, Chu I, Ryan JJ, Feeley M. Polybrominated diphenyl ethers: human tissue levels and toxicology. Rev Environ Contam Toxicol. 2004;183:55–97.
Strazzullo P, Galletti F, Barba G. Altered renal handling of sodium in human hypertension: short review of the evidence. Hypertension. 2003;41(5):1000–5.
Liu H, Tang S, Zheng XM, Zhu YT, Ma ZY, Liu CS, et al. Bioaccumulation, biotransformation, and toxicity of BDE-47, 6-OH-BDE-47, and 6-MeO-BDE-47 in early life-stages of zebrafish (Danio rerio). Environ Sci Technol. 2015;49(3):1823–33.
Hou Y, Fu J, Sun S, Jin Y, Wang X, Zhang L. BDE-209 induces autophagy and apoptosis via IRE1α/Akt/mTOR signaling pathway in human umbilical vein endothelial cells. Environ Pollut. 2019;253:429–38.
Griendling KK, Camargo LL, Rios FJ, Alves-Lopes R, Montezano AC, Touyz RM. Oxidative stress and hypertension. Circ Res. 2021;128(7):993–1020.
Acknowledgements
We extend our gratitude to all the workers who participated in this study.
Funding
This work was supported by Key Specialty Construction Project of Shanghai Pudong New Area Health Commission (Grant No. PWZzk2022-03) and Top-level Clinical Discipline Project of Shanghai Pudong District (Grant No. PWYgf 2021-01).
Author information
Authors and Affiliations
Contributions
Dian Cheng: Conceptualization, Methodology, Writing - Original Draft. Zijun Chen: Methodology, Software.Jian Zhou: Data curation, Visualization.Yue Cao: Methodology. Xin Xie: Investigation.Yizhang Wu: Investigation. Xiaorong Li: Investigation. Xuecheng Wang: Supervision, Writing-Review & Editing. Jinbo Yu: Investigation, Resources, Project administrationBing Yang: Funding acquisition.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cheng, D., Chen, Z., Zhou, J. et al. Association between brominated flame retardants (PBDEs and PBB153) exposure and hypertension in U.S. adults: results from NHANES 2005–2016. Environ Health 23, 64 (2024). https://doi.org/10.1186/s12940-024-01103-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-024-01103-0