Abstract
Background
Both genetic factors and air pollution are risk factors for coronary artery disease (CAD), but their combined effects on CAD are uncertain. The study aimed to comprehensively investigate their separate, combined and interaction effects on the onset of CAD.
Methods
We utilized data from the UK Biobank with a recruitment of 487,507 participants who were free of CAD at baseline from 2006 to 2010. We explored the separate, combined effect or interaction association among genetic factors, air pollution and CAD with the polygenic risk score (PRS) and Cox proportional hazard models.
Results
The hazard ratios (HRs) [95% confidence interval (CI)] of CAD for 10-µg/m3 increases in PM2.5, NO2 and NOx concentrations were 1.25 (1.09, 1.44), 1.03 (1.01, 1.05) and 1.01 (1.00, 1.02), respectively. Participants with high PRS and air pollution exposure had a higher risk of CAD than those with the low genetic risk and low air pollution exposure, and the HRs (95% CI) of CAD in the PM2.5, PM10, NO2 and NOx high joint exposure groups were 1.56 (1.48, 1.64), 1.55(1.48, 1.63), 1.57 (1.49, 1.65), and 1.57 (1.49, 1.65), respectively. Air pollution and genetic factors exerted significant additive effects on the development of CAD (relative excess risk due to the interaction [RERI]: 0.12 (0.05, 0.19) for PM2.5, 0.17 (0.10, 0.24) for PM10, 0.14 (0.07, 0.21) for NO2, and 0.17 (0.10, 0.24) for NOx; attributable proportion due to the interaction [AP]: 0.09 (0.04, 0.14) for PM2.5, 0.12 (0.07, 0.18) for PM10, 0.11 (0.06, 0.16) for NO2, and 0.13 (0.08, 0.18) for NOx).
Conclusion
Exposure to air pollution was significantly related to an increased CAD risk, which could be further strengthened by CAD gene susceptibility. Additionally, there were positive additive interactions between genetic factors and air pollution on the onset of CAD. This can provide a more comprehensive, precise and individualized scientific basis for the risk assessment, prevention and control of CAD.
Similar content being viewed by others
Background
Coronary artery disease (CAD), also called coronary heart disease (CHD), is the leading cause of multiple metabolic diseases and mortality [1,2,3]. To date, CAD is still incurable, and its pathogenesis is not clear [4]. Therefore, CAD prevention becomes particularly important, especially the identification and risk assessment of risk factors, which are the first steps in the prevention of CAD [1]. In addition to some common risk factors, such as age, sex and race, recent studies have more consistently shown that air pollution also leads to cardiovascular disease (CVD) [5,6,7,8].
Moreover, the limited previous studies involving the relationship between air pollution and CAD risk were mainly concentrated on certain subclinical or clinical disorders of CAD, such as coronary vasomotor abnormalities [9], coronary artery calcium [10, 11], acute myocardial infarction [12] and coronary plaques [13]. Other studies mainly considered the risk of near-roadway air pollution (NRAP) on CAD morbidity [14, 15]. However, national prospective population studies assessing the relationship between ambient air pollution exposure and CAD risk remain scarce.
Additionally, it is well accepted that both hereditary susceptibility and air pollution exposure contribute to the risk of CAD, but neglect of their combined or interaction effects made the results biased [1]. Recently, increasing evidence has reported that genetic susceptibility could interact with environmental factors to affect the onset of cardiometabolic diseases [16, 17], including CVDs [18, 19]. However, whether the air pollution exposure alters the association between genetic factors and CAD remains unknown.
Therefore, by means of the polygenic risk score (PRS) [20, 21], we applied data from the UK Biobank with comprehensive information on common baseline characteristics, exposure factors and outcomes to evaluate the separate, combined effect or interaction association between genetic factors and air pollutants, including particulate matter with diameters ranging from ≤ 2.5–≤10 μm (PM2.5, PM2.5−10 and PM10), nitrogen dioxide (NO2), and nitrogen oxides (NOx), and the risk of CAD.
Methods
Study cohort and data access
The current study utilized data from the UK Biobank, a national multicentre prospective cohort study [22]. Briefly, ~ 0.5 million residents aged 40–69 years between 2006 and 2010 were recruited from the UK National Health Service and living < 25 miles from 1 of the 22 study assessment centres across the UK (England, Wales and Scotland). The baseline summary characteristics can be viewed at the website of UK Biobank (https://biobank.ndph.ox.ac.uk/showcase/). The UKB was approved by the North West Multi-Center Research Ethics Committee, and all participants provided informed consent forms.
All eligible researchers could submit the application for data access. The detailed access procedure can be found at UK Biobank’s website (http://www.ukbiobank.ac.uk/register-apply/).
Air pollution exposure assessment
Average exposure to air pollutants, including PM2.5, PM2.5−10, PM10, NO2 and NOx, was assessed in the UK Biobank study under strict measures and internationally recognized standards [23, 24]. Details can be viewed in the Supplementary Materials.
CAD ascertainment
The outcome of this study was CAD, which was defined with the 9th /10th Revision of International Classification of Diseases (ICD). In the UK Biobank, CAD was determined with the Office of Population Censuses and Surveys’ Classification of Interventions and Procedures, self-reported diagnoses and Hospital Episode Statistics data, as previously described [25], and the corresponding UK Biobank codes are provided in Table S1. This definition of CAD includes myocardial infarction and its related sequelae.
Calculation of covariates
We included multiple covariates including baseline characteristics such as age and sex, and health-related outcomes. The detailed contents about variable assessment and data access code are provided in the Supplementary Materials.
PRS contraction
We used the PRS to calculate the accumulative effects of multiple genetic variations, and the detailed definition and formula are presented in the Supplementary Materials. The present PRS utilized data from the largest available CAD genome-wide association meta-analysis without the UK Biobank population [26], with 44 single nucleotide polymorphisms (SNPs). Forty SNPs were finally available in the UK Biobank imputed dataset (see Table S2).
Analytical cohort
Participants were excluded if they met one of the following criteria: (i) preexisting CAD at enrolment, (ii) lack of air pollution exposure information, or (iii) lack of CAD genetic information (Fig. 1). After exclusion for the above reasons, 447,530 subjects were used to investigate the association of particulate matter (PM2.5, PM2.5−10, PM10) and CAD, and 480,298 subjects were used to investigate the association of nitrogen oxides (NO2, NOx) and CAD. Furthermore, when considering the genetic factors, there were 407,470 individuals to investigate the relationship of PM, genetic factors and CAD and 438,736 in the NO group.
Flow diagram for participant inclusion. PM2.5, fine particulate matter with a diameter ≤ 2.5 μm; PM10, particulate matter with diameter ≤ 10 μm; PM2.5−10, particulate matter with diameter between 2.5 and 10 μm; NO2, nitrogen dioxide; NOx, nitrogen oxides. CAD, coronary artery disease; PRS, polygenic risk score; GWAS, genome-wide association study
Statistical analyses
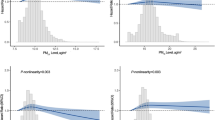
All analyses in the current study were conducted using R software (Version 4.1.1) and Stata (Version 15.1), and two-sided P values < 0.05 were defined as statistically significant. Cox regression models were constructed to investigate the relationship between air pollution and CAD and to calculate hazard ratios (HRs) and 95% confidence intervals (CIs) with adjustment for multiple covariates. We tested the proportional hazards assumption with Schoenfeld residuals methods. We performed a restricted cubic spline (RCS) transformation to explore possible linear/nonlinear correlations of air pollution and CAD and used the Akaike information criterion (AIC) to determine the optimal number of knots of RSC transformation [27].
Because more than 90% of participants are white and race is a common confounding factor, we limited subjects to the White race to explore the combined effects of air pollution exposure and genetic factors on CAD incidence. The additive interaction term was assessed with two indices: the relative excess risk due to the interaction (RERI) and the attributable proportion (AP) due to the interaction [28]. The 95% CIs of the RERI and AP were determined using Excel written by T. Andersson [29], and when 0 was within the CIs of the RERI and AP, it meant that there was no additive interaction. The multiplicative interaction term was assessed by setting variable cross-product terms of gene‒environmental factors in the models to observe whether the corresponding P value was < 0.05.
Multiple imputation was conducted to account for the missing covariate data. The missing categorical variables were imputed with multiple imputation based on latent class (MILC), and the missing continuous variables (e.g., physical activity) were imputed with multivariate imputation by chained equation (MICE) using predictive mean matching. To validate the robustness of our results, we perform several sensitivity analyses. Considering the characteristics of the cohort study, we excluded participants with less than 2 years of follow-up time to avoid false-positive associations.
Results
Table 1 presents the baseline characteristics of eligible participants by incident CAD. In the PM dataset, participants who suffered from CAD were mainly males, older, and had a higher BMI than controls (all P < 0.001). Moreover, previous or current smokers were more likely to develop CAD, while the opposite is true for current alcohol drinkers (all P < 0.001). Additionally, participants with diabetes or CVD at baseline were more likely to develop CAD (all P < 0.001). Participants in the NOx dataset had similar descriptions of baseline characteristics (all P < 0.001). In addition, PM2.5 was highly correlated with nitrogen oxides (r = 0.86 for NO2; r = 0.85 for NOx), while PM2.5−10 was related to PM10 (r = 0.82) (see Figure S1).
During a median of 8.8 years (4,187,431 person-years) of follow-up, 22,897 incident CAD cases were recorded. Kaplan‒Meier (K‒M) plots for CAD in the PM2.5, PM10, PM2.5−10, NO2 and NOx, concentration quartiles are presented in Figures S2-S6, respectively. The results showed that the differences in Kaplan‒Meier curves were significant among PM2.5 (P = 4.0 × 10−13), PM10 (P = 0.010), NO2 (P = 9.0 × 10−11) and NOx (P = 6.0 × 10−14) concentration quartiles but not PM2.5−10 (P = 0.200).
Table 2 presents the relationships between air pollution exposure and CAD risk after adjustment for multiple possible confounders. The results showed that PM2.5, PM10, NO2 and NOx each was still related to an elevated risk of CAD in the multivariate-adjusted models (all P < 0.05). In the model 1, the HRs (95% CI) of CAD for 10-µg/m3 increases in PM2.5, PM10, NO2 and NOx concentrations were 2.56 (2.27, 2.90), 1.22 (1.14, 1.31), 1.11 (1.09, 1.13) and 1.05 (1.04, 1.06), respectively. After further adjusting for race, drinking, smoking status, education level, BMI, UK Biobank assessment centre, physical activity, diabetes and CVD at baseline, the HRs (95% CI) of CAD for 10-µg/m3 increases in PM2.5, NO2 and NOx concentrations were 1.25 (1.09, 1.44), 1.03 (1.01, 1.05) and 1.01 (1.00, 1.02), respectively. The relationship between PM2.5−10 and PM10 exposure and CAD risk were not statistically significant (P = 0.865 for PM2.5−10; P = 0.146 for PM10). Certainly, the third quartiles of PM10 concentration presented more significant effect on CAD risk than first quartiles (HRs [95% CI]: 1.05 [1.01, 1.09], P = 0.027). Interestingly, the association between air pollutants and CAD were not statistically significant after further adjusting TDI (All P > 0.05, Table S3). Furthermore, the RCS results also verified the significant association of air pollutants, including PM2.5 (P < 0.0001), PM10 (P = 0.0001), NO2 (P < 0.0001) and NOx (P < 0.0001), and CAD risk (Figures S7). In addition, subgroup analysis showed that PM2.5, NO2 and NOx had more significant effects on CAD risk in female group, overweight/obesity group and previous or current smokers (see Table S4). And NOx and sex have an interaction effect on CAD risk.
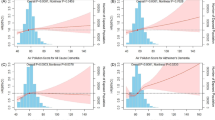
Then, we explored the combined effects of genetic factors and air pollution on the risk of CAD and found the statistically significant results (see Fig. 2). Although the multiplicative interactions of the genetic variation and air pollution on CAD risk were not statistically significant (all P-interaction > 0.05), we observed that individuals with high PRS and air pollution exposure simultaneously showed the highest risk of CAD compared with any other group. The HRs (95% CI) of CAD in the PM2.5, PM10, NO2 and NOx high joint exposure groups were 1.56 (1.48, 1.64), 1.55 (1.48, 1.63), 1.57 (1.49, 1.65), and 1.57 (1.49, 1.65), respectively.
The joint association of the included air pollutant exposure and genetic categories with the risk of incident CAD in the UK Biobank. A Joint effects of PM2.5 and genetic variations; (B) Joint effects of PM10 and genetic variations; (C) Joint effects of NO2 and genetic variations; (D) Joint effects of NOx and genetic variations. Adjusted for age (continuous), sex (male/female), alcohol consumption (never, previous, current, missing), smoking status (never, previous, current, missing), body mass index (< 25 kg/m2, 25 to 29.9 kg/m2, ≥ 30 kg/m2, missing), education level (College or University degree, A/AS-level, O-level/GCSE, CSE, NVQ/HND/HNC, other qualifications, none), UK Biobank assessment center, physical activity (continuous, MET-min/week), diabetes at baseline (yes/no), cardiovascular disease at baseline (yes/no), genotyping batch, and the first 4 genetic principal components
In addition, the RERI and AP were statistically significant, which demonstrated the positive additive interactions of genetic factors and air pollutants on CAD risk (see Table 3). Compared with the low genetic risk and low air pollution exposure group, the RERIs (95% CI) of CAD in the PM2.5, PM10, NO2 and NOx high joint exposure groups were 0.12 (0.05, 0.19), 0.17(0.10, 0.24), 0.14 (0.07, 0.21), and 0.17 (0.10, 0.24), respectively, and the APs (95% CI) of CAD in the PM2.5, PM10, NO2 and NOx high joint exposure groups were 0.09 (0.04, 0.14), 0.12(0.07, 0.18), 0.11 (0.06, 0.16), and 0.13 (0.08, 0.18), respectively. Specifically, in the high PM2.5 exposure and high PRS group, participants had an additional 13% risk of CAD compared with those with low PM2.5 exposure and a low PRS due to the synergistic effect of PM2.5 exposure and genetic risk; the gene-PM2.5 interaction was responsible for 10% of the CAD cases in the participants with high PM2.5 exposure and high genetic risk.
Sensitivity analyses showed that the additive interactions and combined effects of genetic factors and air pollution remained statistically significant after excluding the individuals with a follow-up time of less than two years (see Tables S5, Tables S6-S9).
Discussion
In this prospective cohort study with a median of 8.8 years of follow-up, we observed that air pollution exposure was significantly related to an increased CAD risk, and the risk could be further strengthened by CAD gene susceptibility. Additionally, there were positive gene‒environmental additive interactions on the onset of CAD.
Air pollutants are complex mixtures containing various different gases, liquids and particulates, whose complexities and biological responses make it difficult to demonstrate the relationship between different pollutants and diseases [30, 31]. Previous population-based studies have reported that PM2.5 exposure was relevant to both cardiovascular diseases and all-cause mortality [32, 33], and our results further verified this finding. Moreover, we found that PM10 exposure was also linked to an increased risk of CAD, but the association of PM2.5−10 and CAD risk was not statistically significant. The possible reason was that the effect of PM10 might rely on PM2.5 and PM10 comprising PM2.5−10 and PM2.5 [34]. To our knowledge, PM2.5 has the lowest particulate matter compared to PM2.5−10 and PM10, subsequently having the strongest potential toxicity, which is also responsible for an extensive proportion of the effects of PM10 [31]. Moreover, we also found significantly positive associations between NO2 and NOx and CAD risk, even though the effects were lower than those of PM. Nitrogen oxides, other components of air pollutant mixtures, were also reported to be significantly related to the risk of CVD, but the results remained inconsistent due to short-term air pollution exposure [35, 36]. In addition, it is well known that older age and male sex are risk factors for CAD [1]. Our results further verified these findings. We also found that PM2.5, NO2 and NOx had interactions with sex on CAD risk. NOx and age have an interaction effect on CAD risk.
Previous animal studies have shown that particulate components may promote the growth of atherosclerotic plaques and add markers of plaque rupture vulnerability [37, 38]. Subsequently, some potential mechanisms linking air pollution and CVD have been demonstrated. Of those mechanisms, oxidative stress and inflammation are the most acceptable mechanisms accounting for the observed associations of air pollution and CAD [31, 39, 40]. Prolonged or repeated oxidative stress and inflammation may cause endothelial dysfunction, asymptomatic atherosclerosis, coronary vasomotor abnormalities, coronary artery calcium, acute myocardial infarction and coronary plaques, which could eventually develop into CAD [41,42,43].
In addition to environmental effects, genetic factors are also an important influencing factor of CAD risk [1, 44]. Previous studies and genome-wide association studies (GWAS) have demonstrated that CVD has a strong genetic component, with heritability estimates ranging between 40 and 60% [26, 45, 46]. Of course, the genetic effects are composed of multiple common single genomes. Indeed, GWAS have shown that most cardio-metabolic diseases, including diabetes, hypertension and CAD, are influenced by many risk alleles [47]. In this study, we found that participants with high genetic risk and high air pollution levels were prone to developing CAD compared to subjects with low genetic risk and low air pollution based on the PRS. Furthermore, air pollution and genetic factors presented clear additive interactions on CAD risk. To the best of our knowledge, this is the first large-scale prospective study to evaluate the combined and interaction effects of air pollution and genetic factors on the incidence of CAD. Until now, limited previous studies only assessed the combination and interactions of the gene‒environment in some common CVDs, such as hypertension [16, 18, 19]. Certainly, a large study [48] with approximately 60 919 CAD cases and 80 243 controls revealed that the protective effect of ADAMTS7 gene polymorphism (rs7178051) on CAD was weakened by environmental factors (5% lower CAD risk in smokers; 12% lower CAD risk in nonsmokers) compared to nonsmokers (12% lower risk), which showed the gene‒environmental interaction effects on CAD risk from another aspect. Considering the reverse causality and confounding bias, when excluding the participants with a follow-up time of less than two years or with baseline CVD, we repeated the analysis procedure, and the results did not change appreciably.
There are some strengths in our study. Our study was the first prospective comprehensive study to evaluate the separate, combined and interaction effects of air pollution and genetic factors on the risk of CAD. This new viewpoint provides clues to the aetiology of CAD and provides a reference for the prevention and treatment of susceptible people. Moreover, our article has strict quality control, including strict assessment of air pollution exposure and outcomes, proper statistical methods (PRS), further guaranteeing the robustness and reliability of our findings.
However, we must acknowledge that our study also has some shortcomings. First, air pollutants are made up of many different components [30, 31], but we only explored the associations between some common pollutants, including PM2.5, PM2.5−10, PM10, NO2 and NOx and CAD risk, ignoring the specific parts of air pollutant chemical constituents. Further studies may concentrate on the associations of certain components or physical, chemical or biological properties of air pollutant components and CAD risk [49, 50]. Second, air pollution exposure may be misclassified because the exposure data for this study were only restricted to residential addresses. Although the coverage area of the monitoring system is up to 400 km, the specific real-time environmental exposure of the participants cannot be detected. Future research should consider adorning high-tech portable devices to detect the participants’ surrounding environment in real time. Third, the data were obtained from UK populations, most of which were white (94.0%). Therefore, the generalization of gene-associated findings should be interpreted with caution. Meanwhile, in the future, studies on the respective and combined effects of air pollution-genetic factors on CAD could be conducted in different ethnic groups. Fourth, air pollutant levels were a time-varying factor, but the air pollution information in the UK Biobank was available for several years (2010 for PM2.5, PM2.5−10, and NOx; 2005–2007 and 2010 for NO2; 2007 and 2010 for PM10). If applicable, further study should dynamically detect the air pollutant concentration to avoid over- or underestimating air pollutant toxicity. Fifth, although education level and the Townsend deprivation index are possibly associated with CAD, we did not include them as covariables because they were not available for us in the UK Biobank dataset. However, we included as many variables as possible that were associated with CAD, such as common metabolic disease, physical activity, smoking and alcohol consumption status. Certainly, it is necessary to consider these influencing factors, including education level and the Townsend deprivation index, in future studies related to CAD.
Conclusions
In summary, air pollution exposure was significantly associated with an increased CAD risk, which could be further strengthened by CAD. Additionally, our findings showed positive additive gene‒environmental interactions on the onset of CAD and highlighted the importance of comprehensively evaluating air pollution and genetic factors in prevention efforts for people who are vulnerable to CAD.
Availability of data and materials
The data that support the findings of this study are available from UK Biobank project site, subject to registration and application process. Further details can be found at https://www.ukbiobank.ac.uk.
Abbreviations
- AP:
-
Attributable proportion due to the interaction
- AIC:
-
Akaike information criterion
- CAD:
-
Coronary artery disease
- CHD:
-
Coronary heart disease
- CVD:
-
Cardiovascular disease
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- ICD:
-
International Classification of Diseases
- NRAP:
-
Near-roadway air pollution
- NO2:
-
Nitrogen dioxide
- NOx:
-
Nitrogen oxides
- PRS:
-
Polygenic risk score
- PM:
-
Particulate matter
- RERI:
-
Relative excess risk due to the interaction
- RCS:
-
Restricted cubic spline
- SNP:
-
Single nucleotide polymorphisms
References
Regmi M, Siccardi MA. Coronary artery Disease Prevention. StatPearls Treasure Island (FL): StatPearls Publishing Copyright © 2022. StatPearls Publishing LLC.; 2022.
Global R. National age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet (London England). 2017;390(10100):1151–210.
Kessler T, Schunkert H. Coronary artery Disease Genetics enlightened by Genome-Wide Association Studies. JACC Basic to Translational Science. 2021;6(7):610–23.
Sucato V, Coppola G, Manno G, Vadalà G, Novo G, Corrado E, Galassi AR. Coronary artery Disease in south Asian patients: Cardiovascular Risk factors, Pathogenesis and treatments. Curr Probl Cardiol. 2022;29:101228.
Miller MR. The cardiovascular effects of air pollution: Prevention and reversal by pharmacological agents. Pharmacol Ther. 2022;232: 107996.
Rajagopalan S, Al-Kindi SG, Brook RD. Air Pollution and Cardiovascular Disease: JACC State-of-the-art review. J Am Coll Cardiol. 2018;72(17):2054–70.
Combes A, Franchineau G. Fine particle environmental pollution and cardiovascular diseases. Metabolism: clinical and experimental. Metabolism. 2019;100s:153944.
Konduracka E, Rostoff P. Links between chronic exposure to outdoor air pollution and Cardiovascular Diseases: a review. Environ Chem Lett. 2022; 20(5):2971–88.
Camilli M, Russo M, Rinaldi R, Caffè A, La Vecchia G, Bonanni A, Iannaccone G, Basile M, Vergallo R, Aurigemma C, et al. Air Pollution and Coronary Vasomotor disorders in patients with myocardial ischemia and non-obstructive coronary arteries. J Am Coll Cardiol. 2022;80:1818.
Wang M, Hou ZH, Xu H, Liu Y, Budoff MJ, Szpiro AA, Kaufman JD, Vedal S, Lu B. Association of Estimated Long-Term Exposure to Air Pollution and Traffic Proximity with a marker for coronary Atherosclerosis in a nationwide study in China. JAMA Netw open. 2019;2(6):e196553.
Huynh Q, Marwick TH, Venkataraman P, Knibbs LD, Johnston FH, Negishi K. Long-term exposure to ambient air pollution is associated with coronary artery calcification among asymptomatic adults. Eur Heart J Cardiovasc Imaging. 2021;22(8):922–9.
Ishii M, Seki T, Kaikita K, Sakamoto K, Nakai M, Sumita Y, Nishimura K, Miyamoto Y, Noguchi T, Yasuda S, et al. Short-term exposure to desert dust and the risk of acute Myocardial Infarction in Japan: a time-stratified case-crossover study. Eur J Epidemiol. 2020;35(5):455–64.
Yang S, Lee SP, Park JB, Lee H, Kang SH, Lee SE, Kim JB, Choi SY, Kim YJ, Chang HJ. PM2.5 concentration in the ambient air is a risk factor for the development of high-risk coronary plaques. Eur Heart J Cardiovasc Imaging. 2019;20(12):1355–64.
Ghosh R, Lurmann F, Perez L, Penfold B, Brandt S, Wilson J, Milet M, Künzli N, McConnell R. Near-Roadway Air Pollution and Coronary Heart Disease: Burden of Disease and potential impact of a Greenhouse Gas Reduction Strategy in Southern California. Environ Health Perspect. 2016;124(2):193–200.
Prochaska JH, Wild PS. Traffic-associated air pollution as a risk factor for cancer in individuals with coronary artery Disease. Eur J Prev Cardiol. 2018;25(10):1117–9.
Heianza Y, Qi L. Impact of genes and environment on obesity and Cardiovascular Disease. Endocrinology. 2019;160(1):81–100.
Wang T, Heianza Y, Sun D, Huang T, Ma W, Rimm EB, Manson JE, Hu FB, Willett WC, Qi L. Improving adherence to healthy dietary patterns, genetic risk, and long term weight gain: gene-diet interaction analysis in two prospective cohort studies. BMJ (Clinical Research ed). 2018;360:j5644.
Ward-Caviness CK. A review of gene-by-air pollution interactions for Cardiovascular Disease, risk factors, and biomarkers. Hum Genet. 2019;138(6):547–61.
Weng Z, Liu Q, Yan Q, Liang J, Zhang X, Xu J, Li W, Xu C, Gu A. Associations of genetic risk factors and air pollution with incident Hypertension among participants in the UK Biobank study. Chemosphere. 2022;299: 134398.
Lu X, Liu Z, Cui Q, Liu F, Li J, Niu X, Shen C, Hu D, Huang K, Chen J, et al. A polygenic risk score improves risk stratification of coronary artery Disease: a large-scale prospective Chinese cohort study. Eur Heart J. 2022;43(18):1702–11.
Emdin CA, Xia R, Agrawal S, Rana JS, Lloyd-Jones D, Fornage M, Khera AV. Polygenic score assessed in Young Adulthood and Onset of subclinical Atherosclerosis and Coronary Heart Disease. J Am Coll Cardiol. 2022;80(3):280–2.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P, Elliott P, Green J, Landray M, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex Diseases of middle and old age. PLoS Med. 2015;12(3): e1001779.
Beelen R, Hoek G, Vienneau D, Eeftens M, Dimakopoulou K, Pedeli X, Tsai M-Y, Künzli N, Schikowski T, Marcon A, et al. Development of NO2 and NOx land use regression models for estimating air pollution exposure in 36 study areas in Europe – The ESCAPE project. Atmos Environ. 2013;72:10–23.
Eeftens M, Beelen R, de Hoogh K, Bellander T, Cesaroni G, Cirach M, Declercq C, Dėdelė A, Dons E, de Nazelle A, et al. Development of Land Use Regression models for PM(2.5), PM(2.5) absorbance, PM(10) and PM(coarse) in 20 European study areas; results of the ESCAPE project. Environ Sci Technol. 2012;46(20):11195–205.
Said MA, Eppinga RN, Lipsic E, Verweij N, van der Harst P. Relationship of arterial stiffness index and pulse pressure with Cardiovascular Disease and Mortality. J Am Heart Assoc. 2018;7(2):e007621.
Nikpay M, Goel A, Won HH, Hall LM, Willenborg C, Kanoni S, Saleheen D, Kyriakou T, Nelson CP, Hopewell JC, et al. A comprehensive 1,000 genomes-based genome-wide association meta-analysis of coronary artery Disease. Nat Genet. 2015;47(10):1121–30.
Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6(12):944–53.
Li R, Chambless L. Test for additive interaction in proportional hazards models. Ann Epidemiol. 2007;17(3):227–36.
Hallqvist J, Ahlbom A, Diderichsen F, Reuterwall C. How to evaluate interaction between causes: a review of practices in cardiovascular epidemiology. J Intern Med. 1996;239(5):377–82.
Niemann B, Rohrbach S, Miller MR, Newby DE, Fuster V, Kovacic JC. Oxidative stress and Cardiovascular Risk: obesity, Diabetes, Smoking, and Pollution: part 3 of a 3-Part series. J Am Coll Cardiol. 2017;70(2):230–51.
Miller MR. Oxidative stress and the cardiovascular effects of air pollution. Free Radic Biol Med. 2020;151:69–87.
Wang B, Eum KD, Kazemiparkouhi F, Li C, Manjourides J, Pavlu V, Suh H. The impact of long-term PM(2.5) exposure on specific causes of death: exposure-response curves and effect modification among 53 million U.S. Medicare beneficiaries. Environ Health. 2020;19(1):20.
Pope CA 3, Lefler JS, Ezzati M, Higbee JD, Marshall JD, Kim SY, Bechle M, Gilliat KS, Vernon SE, Robinson AL, et al. Mortality risk and fine Particulate Air Pollution in a large, Representative Cohort of U.S. adults. Environ Health Perspect. 2019;127(7):77007.
Liu Q, Gu X, Deng F, Mu L, Baccarelli AA, Guo X, Wu S. Ambient particulate air pollution and circulating C-reactive protein level: a systematic review and meta-analysis. Int J Hyg Environ Health. 2019;222(5):756–64.
Langrish JP, Lundbäck M, Barath S, Söderberg S, Mills NL, Newby DE, Sandström T, Blomberg A. Exposure to nitrogen dioxide is not associated with vascular dysfunction in man. Inhalation Toxicol. 2010;22(3):192–8.
Atkinson RW, Carey IM, Kent AJ, van Staa TP, Anderson HR, Cook DG. Long-term exposure to outdoor air pollution and incidence of Cardiovascular Diseases. Epidemiol (Cambridge Mass). 2013;24(1):44–53.
Miller MR, McLean SG, Duffin R, Lawal AO, Araujo JA, Shaw CA, Mills NL, Donaldson K, Newby DE, Hadoke PW. Diesel exhaust particulate increases the size and complexity of lesions in atherosclerotic mice. Part Fibre Toxicol. 2013;10: 61.
Bai N, Kido T, Suzuki H, Yang G, Kavanagh TJ, Kaufman JD, Rosenfeld ME, van Breemen C. Eeden SFv: Changes in atherosclerotic plaques induced by inhalation of diesel exhaust. Atherosclerosis. 2011;216(2):299–306.
Kelly FJ, Fussell JC. Role of oxidative stress in Cardiovascular Disease outcomes following exposure to ambient air pollution. Free Radic Biol Med. 2017;110:345–67.
Rao X, Zhong J, Brook RD, Rajagopalan S. Effect of Particulate Matter Air Pollution on Cardiovascular oxidative stress pathways. Antioxid Redox Signal. 2018;28(9):797–818.
Brook RD, Rajagopalan S, Pope CA 3, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, et al. Particulate matter air pollution and Cardiovascular Disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–78.
Franchini M, Mannucci PM. Thrombogenicity and cardiovascular effects of ambient air pollution. Blood. 2011;118(9):2405–12.
Wold LE, Ying Z, Hutchinson KR, Velten M, Gorr MW, Velten C, Youtz DJ, Wang A, Lucchesi PA, Sun Q, et al. Cardiovascular remodeling in response to long-term exposure to fine particulate matter air pollution. Circ Heart Fail. 2012;5(4):452–61.
Gurdasani D, Barroso I, Zeggini E, Sandhu MS. Genomics of Disease risk in globally diverse populations. Nat Rev Genet. 2019;20(9):520–35.
Zdravkovic S, Wienke A, Pedersen NL, Marenberg ME, Yashin AI, De Faire U. Heritability of death from coronary Heart Disease: a 36-year follow-up of 20 966 Swedish twins. J Intern Med. 2002;252(3):247–54.
Vinkhuyzen AA, Wray NR, Yang J, Goddard ME, Visscher PM. Estimation and partition of heritability in human populations using whole-genome analysis methods. Annu Rev Genet. 2013;47:75–95.
Tam V, Patel N, Turcotte M, Bossé Y, Paré G, Meyre D. Benefits and limitations of genome-wide association studies. Nat Rev Genet. 2019;20(8):467–84.
Saleheen D, Zhao W, Young R, Nelson CP, Ho W, Ferguson JF, Rasheed A, Ou K, Nurnberg ST, Bauer RC, et al. Loss of Cardioprotective effects at the ADAMTS7 locus as a result of gene-smoking interactions. Circulation. 2017;135(24):2336–53.
Huang Y, Wu S, Luo H, Yang Y, Xu J, Zhang Y, Wang Q, Shen H, Zhang Y, Yan D, et al. Association of Fine Particulate Matter and its components with Macrosomia: a Nationwide Birth Cohort Study of 336 Chinese cities. Environ Sci Technol. 2023;57(31):11465–75.
Jiao A, Sun Y, Avila C, Chiu V, Molitor J, Slezak J, Sacks DA, Chen JC, Benmarhnia T, Getahun D, et al. Maternal exposure to ambient air pollution mixture and premature rupture of membranes: evidence from a large cohort in Southern California (2008–2018). Environ Int. 2023;177: 108030.
Acknowledgements
This research was conducted using the UK Biobank study under application number 55858 and 44430. We thank all UK Biobank participants and investigators.
Funding
This work was supported by funding from the Joint Funds of the National Natural Science Foundation of China (U21A20340); the National key research and development program (2019YFA0802701); the National Science Foundation of China (81900281, 91839102, 91943301, 82121001), and the Key Project of Gusu School, Nanjing Medical University (GSKY202201012).
Author information
Authors and Affiliations
Contributions
C.X., Z.Q.F. and Y.Z. conceived the idea of the study; J.J.L. acquired the data; C.X. and Z.Q.F. carried out the statistical analysis; Q.L., S.J.Z. and X.C. interpreted the findings; Z.Q.F. and C.X. drafted the manuscript. C.X. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. T.H., J.X., Z.K.W., W.X.L. and C.J.Y provided input in the analysis; all authors critically reviewed the manuscript and A.H.G. revised the manuscript for final submission. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
UK Biobank study obtained informed consent from the study participants and approval from the North West Multicentric Research Ethics Committee (16/NW/0274).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Figure S1. Correlation heatmap of air pollutant exposures calculated using data from 447,530 samples. Figure S2. Kaplan‒Meier curve for the incidence of coronary artery disease in individuals exposed to PM2.5 with quartiles of concentrations. Figure S3. Kaplan‒Meier curve for the incidence of coronary artery disease in individuals exposed to PM2.5-10 with quartiles of concentrations. Figure S4. Kaplan‒Meier curve for the incidence of coronary artery disease in individuals exposed to PM10 with quartiles of concentrations. Figure S5. Kaplan‒Meier curve for the incidence of coronary artery disease in individuals exposed to NO2 at quartiles of concentrations. Figure S6. Kaplan‒Meier curve for the incidence of coronary artery disease in individuals exposed to NOx at quartiles of concentrations. Figure S7. Association between air pollution concentration and the risk of CAD. Table S1. Code list of coronary artery disease in the UK Biobank. Table S2. The main information on genetic variants associated with coronary artery disease in the UK Biobank. Table S3. Adjusted hazard ratio and 95% confidence interval of coronary artery disease by air pollution exposure. Table S4. Subgroup analysis for the association of coronary artery disease per 10 μg/m3 increase in air pollutants by specific characteristics. Table S5. Additive joint interaction for included air pollutant exposure and genetic categories on incident coronary artery disease after excluding participants with a follow-up time of less than 2 years in the UK Biobank. Table S6. The joint association of PM2.5 exposure and coronary artery disease PRS with the risk of incident coronary artery disease after excluding participants with a follow-up time of less than 2 years in the UK Biobank. Table S7.The joint association of PM10 exposure and coronary artery disease PRS with the risk of incident coronary artery disease after excluding participants with a follow-up time of less than 2 years in the UK Biobank. Table S8. The joint association of NO2 exposure and coronary artery disease PRS with the risk of incident coronary artery disease after excluding participants with a follow-up time of less than 2 years in the UK Biobank. Table S9. The joint association of NOx exposure and coronary artery disease PRS with the risk of incident coronary artery disease after excluding participants with a follow-up time of less than 2 years in the UK Biobank.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fu, Z., Ma, Y., Yang, C. et al. Association of air pollution exposure and increased coronary artery disease risk: the modifying effect of genetic susceptibility. Environ Health 22, 85 (2023). https://doi.org/10.1186/s12940-023-01038-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-023-01038-y