Abstract
Background
Bisphenol A (BPA) is an endocrine disruptor that it is present in numerous products of daily use. The aim of this study was to assess the potential association of serum BPA concentrations and the risk of incident breast and prostate cancer in a sub-cohort of the Spanish European Prospective Investigation into Cancer and Nutrition (EPIC).
Methods
We designed a case-cohort study within the EPIC-Spain cohort. Study population consisted on 4812 participants from 4 EPIC-Spain centers (547 breast cancer cases, 575 prostate cancer cases and 3690 sub-cohort participants). BPA exposure was assessed by means of chemical analyses of serum samples collected at recruitment. Borgan II weighted Cox regression was used to estimate hazard ratios.
Results
Median follow-up time in our study was 16.9 years. BPA geometric mean serum values of cases and sub-cohort were 1.12 ng/ml vs 1.10 ng/ml respectively for breast cancer and 1.33 ng/ml vs 1.29 ng/ml respectively for prostate cancer. When categorizing BPA into tertiles, a 40% increase in risk of prostate cancer for tertile 1 (p = 0.022), 37% increase for tertile 2 (p = 0.034) and 31% increase for tertile 3 (p = 0.072) was observed with respect to values bellow the limit of detection. No significant association was observed between BPA levels and breast cancer risk.
Conclusions
We found a similar percentage of detection of BPA among cases and sub-cohort from our population, and no association with breast cancer risk was observed. However, we found a higher risk of prostate cancer for the increase in serum BPA levels. Further investigation is needed to understand the influence of BPA in prostate cancer risk.
Similar content being viewed by others
Background
Cancer incidence is increasing worldwide with 18.1 million new cancer cases and 9.6 million cancer deaths in 2018 [1]. In Europe, breast and prostate cancers lead cancer incidence as they account for 13.5 and 12.6% of the newly diagnosed cases in 2018 respectively [2]. The same is observed in Spain, with 32,536 incident breast cancer cases and 34,394 prostate cancer cases in 2019 [3]. Some risk factors of these hormone dependent cancers are related to lifestyle: diet, smoking habit, weight, alcohol consumption and physical activity [4, 5]. However, owing to the hormonal dependence of these tumors, some environmental pollutants have the potential to act as carcinogens. In this regard, Bisphenol A (BPA) is considered an endocrine disruptor (ED) first developed in the 1890s. BPA is widely produced for the manufacture of polysulfones and polycarbonate plastic, polymers and epoxy resin, and thermal paper and it is one of the highest volume chemicals produced worldwide with 372,000 t produced in 2012 [6]. Therefore its presence is considered to be ubiquitous in the environment and human exposure is continuous [7, 8]. BPA has been detected in the urine (> 0.4 ng/ml) [9,10,11,12] of nearly 90% of adults and children as well as in the serum of general population, pregnant women, placenta, breast milk and amniotic fluid [13,14,15,16,17,18]. Humans are exposed to BPA through several routes: food (oral), occupation (inhalation) and contact materials, plastic type and medical devices (dermal) [7, 19]. However, the main exposure route of BPA is through diet, as many food packaging like tins, cans, plastic boxing etc. have BPA in their composition and it migrates to the food [7, 20,21,22,23,24].
BPA is considered a non-persistent chemical, i.e., as it is degraded in the organism and there is evidence that BPA acts as an endocrine disruptor with estrogenic effects in the rodent mammary gland [25,26,27]. Moreover, prenatal BPA exposure in rats induces preneoplastic lesions in the mammary [28]. Thus, studies conducted in vitro have shown that the exposure of the human breast cancer cell line to BPA increased its proliferation and caused increased oxidative stress [29]. In this regard, in vitro and animal studies have shown that BPA induces the proliferation of the androgen-sensitive human prostate cancer cells and increases epididymis weight [14, 30]. However, although BPA has been linked to hormone dependent cancer risk in animals its evidence in human is scare [31,32,33]. However, the number of epidemiological studies addressing this issue is growing [34,35,36,37,38,39]. Tough some of them have showed certain suffers from limitations the samples were collected after breast cancer diagnosis or have the limitation characteristic of retrospective case–control studies. In this study we have sought to avoid these limitations in our sample design and sampling.
The present study aims to assess the potential association of serum BPA concentrations and the risk of incident breast and prostate cancer in a sub-cohort of the Spanish European Prospective Investigation into Cancer and Nutrition (EPIC).
Methods
Study design
We designed a case-cohort study within the EPIC-Spain cohort. EPIC is a prospective multi-centric cohort study planned to investigate the relationship between diet, lifestyles and cancer. It involves 23 research centers in 10 European countries, including five Spanish centers: Asturias, Granada, Murcia, Navarra and Gipuzkoa [40]. Study participants reported information about dietary, lifestyle, reproductive and anthropometric factors at baseline.
Study population
The EPIC-Spain included 41,446 participants (62% women) aged 29–69 years enrolled between 1992 and 1996 in five provinces of Spain. Participants were recruited mostly among blood donors (about 60%) and the study population covered a broad range of socioeconomic and educational levels. Furthermore, they signed an informed consent and the study was approved by Ethics Committee of the Bellvitge Hospital (Barcelona). EPIC study populations and data collection were explained elsewhere [41].
Study population in the present study consisted of 3690 sub-cohort participants, 547 breast cancer cases and 575 prostate cancer cases from four EPIC-Spain centers (Gipuzkoa, Granada, Murcia and Navarra) with available data on BPA exposure. Participants selected for the sub-cohort included, by design, an overlap of 57 breast cancer cases and 111 prostate cancer cases (Fig. 1).
The sub-cohort was selected among participants registered as alive in the EPIC cohort until 30/12/2013 using stratified random sampling by sex (50% men and 50% women) and age (quintiles), excluding persons with cancer at recruitment. In our sub-cohort, 79.6% of the participants provided a fasting blood sample at recruitment and 85.6% of them were extracted between 6 am and 11 am. However, we can generalize and assume most of our samples were taken during the mornings and in fasting conditions.
Follow-up time began at EPIC recruitment and cancer cases were defined as participants with a diagnosis of breast or prostate cancer (i.e. ICD10 codes C50 and C61 respectively) during the study period. Incident cancer cases are identified by linkage with the Population Cancer Registries. Incidence date was determined by the date of cancer diagnosis and prevalent cases were excluded (participants with a cancer diagnosis prior to recruitment). Dates of end of follow-up for cases identification were: 31/12/2012 for Granada, 31/12/2013 for Murcia, 31/12/2011 for Navarra and 30/12/2013 for Gipuzkoa. For sub-cohort participants, the end of follow-up date was the lowest among date of diagnosis, date of death, date of loss of follow-up or the center-specific end-of-follow-up, whatever happened first.
Vital status and date of death of participants in our sub-cohort was determined by linking EPIC data base with the National and regional Registries, IND (death national index), INE (statistical national institute) and regional mortality register until 30/12/2013 (maximum date of identification of incident cases).
Covariate assessment
Information on lifestyle and other health-related factors was obtained by an interviewer-administered questionnaire at baseline. All interviewers had received appropriate training for this task.
Measurements of height, weight, and hip and waist circumferences were taken at recruitment using standardised procedures [41]. The questionnaire included items on educational level, history of previous illnesses, history of tobacco use, alcohol consumption, physical activity, and reproductive history [41]. The participants were classified into three categories by body mass index (BMI): < 25 kg/m2, 25- < 30 kg/m2, ≥30 kg/m2. Educational level was classified according to five categories: none, primary school, secondary school, technical or vocational training and university degree. Smoking status was summarised in three categories: never smoked, former smoker and current smoker. Alcohol consumption at recruitment in grams per day was categorized as no drinker (0 g/day), drinker (≤30 g/d in men and ≤ 20 g/d in women) and heavy drinker (> 30 g/d in men and > 20 g/d in women). Information on the domains of physical activity was compiled taking seasonal variation into account. A simple four-level physical activity index (low, medium, high, very high) was derived and validated by combining recreational and household activity [42]. Reproductive history was additionally measured for women, including menopausal status at recruitment, number of pregnancies, breastfeeding (yes/no regardless of the duration), and use of oral contraceptive or hormone replacement therapy sometime in life.
Sample collection and chemical analyses
Blood samples were drawn from each participant at recruitment, which were subsequently centrifuged, and aliquots of plasma, serum, red blood cells and buffy coat in 0.5 mL straws were stored in liquid nitrogen (− 196 °C).
BPA levels were quantified in serum samples using two of 0.5 mL straws, in an adaptation of a previously-validated methodology [43]. In brief, BPA was analysed by dispersive liquid–liquid micro-extraction (DLLME) and ultra-high performance liquid chromatography with tandem mass spectrometry detection (UHPLC-MS/MS). Samples were thawed completely at room temperature, centrifuged at 2600 g for 10 min and 0.75 mL was extracted for analysis. In order to determine total BPA (free plus conjugated) in serum, each sample was spiked with 50 μL of enzyme solution (β-glucuronidase/sulphatase) and incubated at 37 °C for 24 h. The treated serum was placed in a 15 mL screw-cap glass tube and spiked with 30 μL of the surrogate standard solution (1.25 mg/L of BPA-d16). The serum was then diluted to 10.0 mL with 5% NaCl aqueous solution (w/v) and the pH was adjusted to 2.0. Next, 0.75 mL of acetone and 0.75 mL of trichloromethane were mixed and injected rapidly into the aqueous sample with a syringe. After manual shaking, centrifugation and evaporation of the extract, the residue was dissolved with 100 μL of a mixture consisting of water (0.1% ammonia)/acetonitrile (0.1% ammonia), 70:30 (v/v), and finally 10 μL was injected into the LC system. Limit of detection (LOD) was 0.2 ng/ml. Values below LOD were assigned the LOD divided by the square root of 2.
Chemical analyses were performed at Centro de Excelencia en Investigación de Medicamentos Innovadores en Andalucía MEDINA (https://www.medinadiscovery.com/, which has been assessed and certified for the standards of ISO 9001:2015, and routinely performs internal and external quality control analyses. In addition, the present analyses are encompassed in the activities of our research group within the The Human Biomonitoring Initiative (HBM4EU, https://www.hbm4eu.eu/).
Statistical analysis
Geometric means and 95% confidence intervals of the BPA levels (in ng/ml) were calculated for cases and sub-cohort and according to center, sex, age group, educational level, body mass index, physical activity and alcohol consumption and smoker status. Statistical differences were assessed through the Mann-Whitney or Kruskall-Wallis tests.
Time to cancer event were modelled by means of Borgan II weighted Cox proportional hazard models [44], stratified by center. Robust standard errors were used as recommended in such case-cohort design [45]. Hazard ratios and 95% confidence intervals were derived from these Cox models. BPA levels acted as principal independent variable, and were treated as continuous variable, transformed by base 2 logarithm to smooth their strong asymmetric distribution and categorized into tertiles to assess non-linear relationship. Multivariate Cox-regression models were always stratified by center and age group, and constructed using three strategies: A) linear BPA as independent variable; B) log2-transformed BPA as independent variable; C) categorized BPA as independent variable (considering a category with values <LOD as a reference and distributing the rest of the detectable values into terciles). The last two models allowed us to evaluate the non-linear relationship, which was also verified by the analysis of the martingale-based residuals in model A. All models were adjusted by age, education level, BMI, physical activity, smoking status, and alcohol consumption. For women, models were also adjusted by menopause, number of pregnancies, breastfeeding, oral contraceptives and hormone replacement therapy (HRT). An interaction term between BMI and menopause status was additionally included, since the join effect of these two factors can act as a modifier of breast cancer risk. The confounders were selected based on the evidence on factors potentially associated with the risk of the studied cancers among the variables available in the EPIC cohort. Statistical analysis was conducted with Stata v14 (Stata Statistical Software: Release 14. College Station, TX: StataCorp LP).
Results
In our study, median follow-up time was 17 years. We had 547 cases of breast cancer and 575 prostate cancer cases and 3690 sub-cohort participants (1918 women and 1772 men). Table 1 shows the main characteristics of cancer patients and sub-cohort participants of the study.
Breast cancer
Among breast cancer patients, there were more smokers (18.1% vs 10.3%) than in the sub-cohort. Regarding physical activity, the sub-cohort had more participants in the “very high” classification than the cases: 58.7% vs 50.3% respectively. Other significant differences were observed in education level, BMI, menopausal status, number of pregnancies, breastfeeding and oral contractive use comparing breast cancer cases and sub-cohort participants (Table 1).
Percentage of detection was similar between cases and sub-cohort, around 68% of the samples showed levels above LOD (Supplementary material, Table 1). BPA geometric mean was slightly higher in cases than in participants of the sub-cohort (1.12 ng/ml vs 1.10 ng/ml) (p = 0.754) (Supplementary material, Table 1). Breast cancer cases presented higher percentage of detection above LOD (75.7% vs 63.4%) and higher GM (1.51 ng/ml vs 0.90 ng/ml) than participants from the sub-cohort (p = 0.010) between smoker (Supplementary material, Table 1). We found significant differences in serum BPA concentrations in the participants with secondary school when comparing cancer cases and sub-cohort (p = 0.002). However, there were no significant differences when observing other variables, neither those concerning women reproducibility (Supplementary material, Table 1).
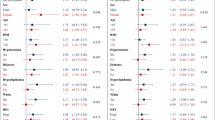
Cox regression analyses showed no statistically significant association between BPA levels and breast cancer incidence in our cohort in the developed models (Table 2). There were no significant association when analyzing linear BPA in model A (HR = 1.047; p = 0.200), neither in logarithmic model (Models B, Table 2). In the same way, no significant effect was observed when the exposure variable was categorized into tertiles (Models C, Table 2).
Prostate cancer
There were no significant differences between prostate cancer patients and the sub-cohort concerning lifestyle variables (Table 1).
Serum BPA levels showed no significant differences in prostate cancer participants compared with the sub-cohort (1.33 ng/ml vs 1.29 ng/ml; p = 0.809) (Supplementary material, Table 2). Non-significant differences in BPA levels were observed between cases and sub-cohort according to sociodemographic and life style characteristics (Supplementary material, Table 2).
Cox regression models showed no significant association of BPA serum levels and prostate cancer risk in linear model (Table 2). However, the result of the adjusted logarithmic model showed a positive association between an increase in BPA levels with the risk of prostate cancer (HR = 1.035; p = 0.093). Moreover, when categorizing BPA in tertiles we observed an increased risk of prostate cancer in model C: a 40% increase in risk of prostate cancer for tertile 1 (HR = 1.40; p = 0.022), 37% increase for tertile 2 (HR = 1.37; p = 0.034) and 31% increase for tertile 3 (HR = 1.31; p = 0.072) was observed with respect to values bellow the limit of detection (p-trend = 0.069) (Table 2).
Discussion
This study longitudinally explores the potential contribution of participants’ exposure to BPA at recruitment in the development of breast and prostate cancer, over a relatively large follow-up time in Spain.
In our study, 70% of the population had detectable BPA values and its concentrations were similar among cancer cases and sub-cohort participants which is comparable to an epidemiological study in Korea (n = 167) were no significant differences in blood BPA levels between breast cases and controls were found (p = 0.42) [46].
Our results show no association for BPA serum concentrations and risk of incident breast cancer despite BPA is considered an ED with carcinogenic potential [31,32,33]. These results are in consonance with the study of Aschengrau et al., which found no association between adult occupational exposure to BPA and breast cancer diagnosis, although the exposure measure was through questionnaires (n = 1000 participants) [36]. In the same way, a population-based case–control study also showed no association between the urinary BPA levels and risk of breast cancer in postmenopausal Polish women (n = 575) [37]. However, recent reviews conclude that the evidence of the potential impact of BPA on human development of chronic diseases is sufficiently robust to raise concerns about BPA being an important health problem [32, 47,48,49]. These reviews are mostly based on animal and in vitro studies, due to the limited epidemiological studies. Experimental modelling suggests that BPA increases breast cancer susceptibility [47]. Still, few epidemiological studies have linked BPA to breast cancer. In this regard, high concentrations of serum BPA correlated with elevated mammographic breast density, a marker of breast cancer risk, in a study of postmenopausal women from Wisconsin (n = 264) [50]. Mammographic breast density increased from 12 to 17% when serum BPA levels increased to 0.55 ng/ml). However, case-control studies present a controversial validity when the possible risk factor is a biomarker, since this is measured in cases when the disease is already present and therefore the time sequence necessary to impute causality is not absent.
Regarding prostate cancer, we found a significant non-linear association with risk of prostate cancer when we categorized serum BPA in tertiles, as individuals with serum BPA levels in the 1st and 2nd tertile showed a 40 and 37% increased risk of prostate cancer respectively. In this regard, a case control study conducted in men with prostate cancer (n = 60) showed a much higher concentration of BPA in the urine of those patients in comparison with the control group [51]. In another case-control study in Hong-Kong [52] showed a positive exposure-response relationship between a cumulative BPA exposure index and prostate cancer, with the greatest and significant risk in the high versus reference category (OR = 1.57, 95% CI: 1.01–2.44). This study, however, did not had any biological measurement of BPA, as the cumulative BPA exposure index was based on self-reported information of the habitual use of specific type of food or beverage container including what the container is made of, the frequency of use, the handling practice, the heating and years of usage.
On the other hand, the biological matrix used for biomonitoring plays an important role. Serum BPA concentrations can be relatively unstable, representing recent exposures [53, 54]. In this regard, the biological matrix most commonly used to determine BPA is urine [55]. Indeed, some authors acknowledge urine concentrations as the best biomarker of BPA exposure, since metabolites in blood can be several orders of magnitude lower than in urine and it can be indicative of a relatively longer exposure period in comparison to other matrices [53]. Some studies point out that, among the biomonitoring matrices, urine contains the highest BPA concentrations, followed by serum [56] which implies a greater capacity to detect levels of exposure and also an improved estimator of medium-term exposure. However, there is still scarce studies about the correlation between matrices [56, 57]. The different biological matrices for measuring BPA have had many interrogations and discussion. Serum BPA specifically measures unconjugated BPA, and studies measuring BPA in blood are scarce, due to more complex logistics than urine. Therefore, our matrix selection could be interpreted as well as a contribution of the study to the scarce evidence of BPA in serum.
There is ample evidence about BPA exposure and risk of hormone dependent cancer in animal and in vitro studies both for breast cancer [58,59,60,61,62,63,64,65,66,67,68,69,70] and prostate cancer [71,72,73,74,75,76]. Conversely, the scarce epidemiological evidence on BPA exposure and risk of breast or prostate cancer studies have overall yielded to differing results, most likely due to different experimental designs, timing of exposure, and uncontrolled or residual confounding factors, such as the route of the administration of BPA, its degradation time or low exposure doses. The low range of BPA concentrations (ng/ml) is a consequence of its fast metabolism and short half-life in human body [77]. Moreover, human exposure to many potential EDs can be confounded because most existing cohorts and epidemiological studies (as our study) were designed to measure the impact of a single chemical without accounting for the effects of mixtures [78]. The heterogeneity of the populations of the studies, the different ways of assessing the exposure and, and the biological matrix can have a big influence in the exposure level as well as the different ways of evaluating the disease. In this regard, our method may have advantages, such as accessibility to practically the entire study population, taking advantage of the great coverage of public clinical records. However, we could have perhaps a possible underestimation of cases, or at least that usually happens when we rely on clinical records. Thus, different methodologies can result in inconsistent outcomes. Additional larger epidemiological studies are needed to obtain sufficient evidence and to identify the degree to which there is an association between low-dose BPA exposure and breast and prostate cancer risk.
On the other hand, some possible mechanisms of action of BPA carcinogenicity could be genetic damages, epigenetic effects, endocrine disruption, oxidative stress and mitochondrial dysfunction and cell signaling [31, 32]. It has been shown that BPA can interact with estrogen receptors, behaving as agonist or antagonist through endocrine receptor dependent signaling pathways [79]. These actions can lead to diverse changes in estrogen-target organs including mammary gland [9]. BPA can also regulate the proliferation and migration of prostate cancer cells and induce DNA adducts in prostate cancer cells [80,81,82]. Consequently, BPA plays a role in the pathogenesis of several endocrine disorders including female and male infertility, precocious puberty and hormone dependent tumors such as breast and prostate cancer [83]. Studies conducted in vitro have shown that the exposure of the human breast cancer cell line to BPA increased its proliferation and caused increased oxidative stress [84, 85]. Growing evidence suggests that BPA-induced damage is associated with oxidative stress [32, 86, 87] as BPA can disturb oxidative homeostasis through direct or indirect pathways, including cancer, infertility, and neurodegenerative diseases [88, 89]. In the epidemiological study of Yang et el., authors reported that BPA exposure apparently promotes oxidative stress and inflammation in women [90]. Regarding evidence for epigenetic alterations, several animal studies have identified plausible mechanisms of action of BPA on prostate cancer risk as early life BPA exposure provides a potential mechanism of action for low dose BPA [91, 92]. These mechanisms could induce the tumors of interest, which are hormone dependent as the constant induction of estrogen / androgen receptors, even at low doses, compared to endogenous hormones, could activate cell proliferation or inhibit protective mechanisms [93].
Our study has some limitations since the exposure to BPA was estimated by using serum concentrations at recruitment, and we do not have information on changes in BPA concentrations and covariates during the follow-up time as BPA may vary over time in our longitudinal design. In addition, the use of one BPA point measurement might not take into account intra-person and intra-day fluctuations, which might be relevant in certain populations [94, 95]. However, The use of one-spot samples, have been shown to be a reflection of BPA exposure in the population in some studies [96]. Though, BPA levels in the organism are not stable, as levels are higher the moment the person has been exposed and until BPA is metabolized and excreted 7 or 8 h after its incorporation into the body. BPA is rapidly conjugated and excreted by humans due to the efficient glucuronidation of BPA [77]. Moreover, we have to take into account that our population have been exposed to other pollutants. Therefore, possible associations from one single contaminant may be due to other highly correlated (and unmeasured) co-exposures, potentially including both persistent and non-persistent pollutants, or even a result of interactions among different co-exposures [97, 98]. Finally, although we adjusted for n° of pregnancies, breastfeeding, oral contraceptives, HRT and the interaction between BMI and menopause for women, we cannot exclude a potential residual confounding. Therefore, more research considering subclinical disease markers would shed light on the causality of the observed associations.
This study also has a number of strengths. The population considered is large and well representative of exposure to BPA in the 1990s. This characteristic is valuable, enabling us to study possible associations between BPA exposure at recruitment and certain chronic illnesses currently present in the participants. In this respect, it is of notable importance that 70% of the study population had detectable levels of BPA. We used previously-validated questionnaires which allow to have a precise characterization of the covariates. Besides, BPA was screened using validated analytical methodologies [43].
Conclusions
We evidenced a similar percentage of detection of BPA among breast cancer cases and sub-cohort from our population, and slightly higher percentage of detection in prostate cancer participants than in the sub-cohort. We observed an increased risk of prostate cancer in the 1st and 2nd tertile of serum BPA. However, we found no associations between serum BPA concentrations and risk of breast cancer. Further investigation is needed to elucidate the potential influence BPA exposure on breast and prostate cancer risk.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin Wiley. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
ECIS European Cancer Information System [Internet]. [cited 2018 Nov 22]. Available from: https://ecis.jrc.ec.europa.eu/
Red española de registros de cancer. Estimaciones de la incidencia del cáncer en España, 2019. Redecan. 2019;19:1–14.
World Cancer Research Foundation; American Institute for Cancer Research. Diet, nutrition, physical activity and breast cancer [Internet]. 2017. Available from: http://www.wcrf.org/sites/default/files/CUP_BREAST_REPORT_2017_WEB.pdf
WCRF. Diet, nutrition, physical activity and prostate cancer. 2018.
Mcgroup. World BPA Production Grew by Over 372,000 Tonnes in 2012 [Internet]. 2013. p. 1–3. Available from: http://mcgroup.co.uk/news/20131108/bpa-production-grew-372000-tonnes.html
Geens T, Aerts D, Berthot C, Bourguignon J-P, Goeyens L, Lecomte P, et al. A review of dietary and non-dietary exposure to bisphenol-A. Food Chem Toxicol [Internet]. Pergamon; 2012 [cited 2019 Apr 9];50:3725–40. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22889897.
vom Saal FS, Hughes C. An extensive new literature concerning low-dose effects of bisphenol A shows the need for a new risk assessment. Environ Health Perspect [Internet]. 2005;113:926–33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16079060
Vandenberg LN, Maffini M V., Sonnenschein C, Rubin BS, Soto AM. Bisphenol-a and the great divide: A review of controversies in the field of endocrine disruption. Endocr Rev [Internet]. 2009 [cited 2019 Aug 22];30:75–95. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19074586.
Hormann AM, Vom Saal FS, Nagel SC, Stahlhut RW, Moyer CL, Ellersieck MR, et al. Holding thermal receipt paper and eating food after using hand sanitizer results in high serum bioactive and urine total levels of bisphenol a (BPA). PLoS one [Internet]. 2014;9:e110509. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25337790.
Liao C, Kannan K. Determination of free and conjugated forms of bisphenol a in human urine and serum by liquid chromatography-tandem mass spectrometry. Environ Sci Technol [Internet]. 2012;46:5003–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22489688.
Vandenberg LN, Chahoud I, Heindel JJ, Padmanabhan V, Paumgartten FJR, Schoenfelder G. Urinary, circulating, and tissue biomonitoring studies indicate widespread exposure to bisphenol a. Environ Health Perspect [Internet]. 2010;118:1055–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20338858.
Bloom MS, vom Saal FS, Kim D, Taylor JA, Lamb JD, Fujimoto VY. Serum unconjugated bisphenol A concentrations in men may influence embryo quality indicators during in vitro fertilization. Environ Toxicol Pharmacol [Internet]. 2011;32:319–23. Available from: http://www.sciencedirect.com/science/article/pii/S1382668911001062
Prins GS, Ye SH, Birch L, Ho S Mei, Kannan K. Serum bisphenol A pharmacokinetics and prostate neoplastic responses following oral and subcutaneous exposures in neonatal Sprague-Dawley rats. Reprod Toxicol [Internet]. 2011;31:1–9. Available from: http://www.sciencedirect.com/science/article/pii/S0890623810003060
Fujimoto VY, Kim D, Vom Saal FS, Lamb JD, Taylor JA, Bloom MS. Serum unconjugated bisphenol A concentrations in women may adversely influence oocyte quality during in vitro fertilization. Fertil Steril [Internet]. 2011;95:1816–9. Available from: http://www.sciencedirect.com/science/article/pii/S0015028210027949
Ye X, Zhou X, Hennings R, Kramer J, Calafat AM. Potential external contamination with bisphenol a and other ubiquitous organic environmental chemicals during biomonitoring analysis: an elusive laboratory challenge. Environ Health Perspect [Internet]. 2013;121:283–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23458838.
Fénichel P, Déchaux H, Harthe C, Gal J, Ferrari P, Pacini P, et al. Unconjugated bisphenol A cord blood levels in boys with descended or undescended testes. Hum Reprod [Internet]. 2012;27:983–90. Available from: http://humrep.oxfordjournals.org/content/27/4/983
Salamanca-Fernández E, Rodríguez-Barranco M, Arrebola JP, Vela F, Díaz C, Chirlaque MD, et al. Bisphenol-A in the European Prospective Investigation into Cancer and Nutrition cohort in Spain: Levels at recruitment and associated dietary factors. Environ Res [Internet]. 2020 [cited 2019 Dec 11];182:109012. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0013935119308096
Vandenberg LN, Hunt PA, Myers JP, Vom Saal FS. Human exposures to bisphenol a: mismatches between data and assumptions. Rev Environ Health [Internet]. 2013;28:37–58. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23612528.
Hahladakis JN, Velis CA, Weber R, Iacovidou E, Purnell P. An overview of chemical additives present in plastics: Migration, release, fate and environmental impact during their use, disposal and recycling. J Hazard Mater [Internet]. 2018 [cited 2019 Apr 11];344:179–99. Available from: https://linkinghub.elsevier.com/retrieve/pii/S030438941730763X
López-Cervantes J, Paseiro-Losada P. Determination of bisphenol A in, and its migration from, PVC stretch film used for food packaging. Food Addit Contam [Internet]. 2003 [cited 2019 Apr 9];20:596–606. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12881134.
Grumetto L, Montesano D, Seccia S, Albrizio S, Barbato F. Determination of Bisphenol A and Bisphenol B Residues in Canned Peeled Tomatoes by Reversed-Phase Liquid Chromatography. J Agric Food Chem [Internet]. American Chemical Society; 2008 [cited 2019 Feb 16];56:10633–7. Available from: http://pubs.acs.org/doi/abs/10.1021/jf802297z, 56, 22, 10633, 10637
Ćwiek-Ludwicka K. Bisphenol A (BPA) in food contact materials - new scientific opinion from EFSA regarding public health risk. Rocz Państwowego Zakładu Hig [Internet]. 2015;66:299–307. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26656411.
Huang R-P, Liu Z-H, Yuan S-F, Yin H, Dang Z, Wu P-X. Worldwide human daily intakes of bisphenol A (BPA) estimated from global urinary concentration data (2000–2016) and its risk analysis. Environ Pollut [Internet]. 2017 [cited 2019 May 8];230:143–52. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0269749117311703
Mandrup K, Boberg J, Isling LK, Christiansen S, Hass U. Low-dose effects of bisphenol a on mammary gland development in rats. Andrology [Internet]. 2016;4:673–83. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27088260.
Betancourt AM, Wang J, Jenkins S, Mobley J, Russo J, Lamartiniere CA. Altered carcinogenesis and proteome in mammary glands of rats after prepubertal exposures to the hormonally active chemicals bisphenol a and genistein. J Nutr [Internet]. 2012;142:1382S–8S. Available from: http://jn.nutrition.org.ezproxy.ulb.ac.be/content/142/7/1382S.long
Acevedo N, Davis B, Schaeberle CM, Sonnenschein C, Soto AM. Perinatally administered bisphenol A as a potential mammary gland carcinogen in rats. Environ Health Perspect [Internet]. 2013;121:1040–6. Available from: http://files/974/display.html
Durando M, Kass L, Piva J, Sonnenschein C, Soto AM, Luque EH, et al. Prenatal bisphenol a exposure induces preneoplastic lesions in the mammary gland in wistar rats. Environ Health Perspect. Public Health Services, US Dept of Health and Human Services. 2006;115:80–6.
Wetherill YB, Akingbemi BT, Kanno J, McLachlan JA, Nadal A, Sonnenschein C, et al. In vitro molecular mechanisms of bisphenol A action [Internet]. Reprod. Toxicol. Reprod Toxicol; 2007 [cited 2020 Nov 16]. p. 178–98. Available from: https://pubmed.ncbi.nlm.nih.gov/17628395/
Prins GS, Tang WY, Belmonte J, Ho SM. Perinatal exposure to oestradiol and bisphenol a alters the prostate epigenome and increases susceptibility to carcinogenesis. Basic Clin Pharmacol Toxicol [Internet] 2008;102:134–138. Available from: http://onlinelibrary.wiley.com/doi/10.1111/j.1742-7843.2007.00166.x/abstract, 2
Wang Z, Liu H, Liu S. Low-Dose Bisphenol A Exposure: A Seemingly Instigating Carcinogenic Effect on Breast Cancer. Adv Sci (Weinheim, Baden-Wurttemberg, Ger [Internet]. Wiley-Blackwell; 2017 [cited 2019 may 8];4:1600248. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28251049.
Rezg R, El-Fazaa S, Gharbi N, Mornagui B. Bisphenol A and human chronic diseases: current evidences, possible mechanisms, and future perspectives. Environ Int [Internet]. 2014;64:83–90. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24382480.
Keri RA, Ho SM, Hunt PA, Knudsen KE, Soto AM, Prins GS. An evaluation of evidence for the carcinogenic activity of bisphenol a. Reprod Toxicol [Internet]. 2007;24:240–52. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17706921.
Vandenberg LN, Hauser R, Marcus M, Olea N, Welshons WV. Human exposure to bisphenol A (BPA). Reprod Toxicol [Internet]. Pergamon; 2007 [cited 2018 Sep 7];24:139–77. Available from: https://www.sciencedirect.com/science/article/pii/S0890623807002377
Morgan M, Deoraj A, Felty Q, Roy D. Environmental estrogen-like endocrine disrupting chemicals and breast cancer. Mol Cell Endocrinol Elsevier Ireland Ltd. 2017;457:89–102. https://doi.org/10.1016/j.mce.2016.10.003.
Aschengrau A, Coogan PF, Quinn MM, Cashins LJ. Occupational exposure to estrogenic chemicals and the occurrence of breast cancer: an exploratory analysis. Am J Ind med [Internet]. 1998;34:6–14. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9617382.
Trabert B, Falk RT, Figueroa JD, Graubard BI, Garcia-Closas M, Lissowska J, et al. Urinary bisphenol A-glucuronide and postmenopausal breast cancer in Poland. Cancer causes control [Internet]. 2014;25:1587–93. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25189422.
Parada H, Gammon MD, Ettore HL, Chen J, Calafat AM, Neugut AI, et al. Urinary concentrations of environmental phenols and their associations with breast cancer incidence and mortality following breast cancer. Environ Int Elsevier Ltd. 2019;130:104890.
Reeves KW, Schneider S, Xue J, Kannan K, Mason H, Johnson M, et al. Bisphenol-A in breast adipose tissue of breast cancer cases and controls. Environ Res [Internet]. Academic Press Inc.; 2018 [cited 2020 mar 2];167:735–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30236518.
González CA, Navarro C, Martínez C, Quirós JR, Dorronsoro M, Barricarte A, et al. El estudio prospectivo Europeo sobre cáncer y nutrición (EPIC). Rev Esp Salud Publica [Internet]. Ministerio de Sanidad y Consumo; 2004 [cited 2018 Jan 26];78:167–76. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15199795.
Riboli E, Hunt KJK, Slimani N, Ferrari P, Norat T, Fahey M, et al. European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr [Internet]. 2003 [cited 2017 Feb 6];5:1113–24. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12639222.
Cust AE, Smith BJ, Chau J, van der Ploeg HP, Friedenreich CM, Armstrong BK, et al. Validity and repeatability of the EPIC physical activity questionnaire: A validation study using accelerometers as an objective measure. Int J Behav Nutr Phys Act [Internet]. BioMed Central; 2008 [cited 2021 May 21];5:1–13. Available from: http://www.ijbnpa.org/content/5/1/33
Vela-Soria F, Ballesteros O, Zafra-Gómez A, Ballesteros L, Navalón A. A multiclass method for the analysis of endocrine disrupting chemicals in human urine samples. Sample treatment by dispersive liquid–liquid microextraction. Talanta [Internet]. 2014 [cited 2019 Apr 11];129:209–18. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25127586.
Borgan ØrnulfSven, Ove Samuelsen. A review of cohort sampling designs for Cox’s regression model: Potentials in epidemiology. Nor Epidemiol [Internet]. 2003 [cited 2020 Jan 15];13:239–48. Available from: https://www.researchgate.net/publication/41758192_A_review_of_cohort_sampling_designs_for_Cox%27s_regression_model_Potentials_in_epidemiology
Barlow WE. Robust Variance Estimation for the Case-Cohort Design. Biometrics JSTOR. 1994;50:1064.
Yang M, Ryu J-H, Jeon R, Kang D, Yoo K-Y. Effects of bisphenol a on breast cancer and its risk factors. Arch Toxicol [Internet]. 2009;83:281–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18843480.
Seachrist DD, Bonk KW, Ho S-MM, Prins GS, Soto AM, Keri RA. A review of the carcinogenic potential of bisphenol A. Reprod Toxicol [Internet]. 2016 [cited 2018 Sep 18];59:167–82. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26493093.
Gao H, Yang BJ, Li N, Feng LM, Shi XY, Zhao WH, et al. Bisphenol A and hormone-associated cancers: Current progress and perspectives. Med (United States). Lippincott Williams and Wilkins. 2015;94:e211.
Rodgers KM, Udesky JO, Rudel RA, Brody JG. Environmental chemicals and breast cancer: An updated review of epidemiological literature informed by biological mechanisms. Environ. Res. Academic Press Inc.; 2018. p. 152–82.
Sprague BL, Trentham-Dietz A, Hedman CJ, Wang J, Hemming JD, Hampton JM, et al. Circulating serum xenoestrogens and mammographic breast density. Breast Cancer Res [Internet]. 2013;15:R45. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23710608%5Cn, http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4053153&tool=pmcentrez&rendertype=abstract
Tarapore P, Ying J, Ouyang B, Burke B, Bracken B, Ho SM. Exposure to bisphenol a correlates with early-onset prostate cancer and promotes centrosome amplification and anchorage-independent growth in vitro. PLoS one [Internet]. 2014;9:e90332. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24594937.
Tse LA, Lee PMY, Ho WM, Lam AT, Lee MK, Ng SSM, et al. Bisphenol A and other environmental risk factors for prostate cancer in Hong Kong. Environ Int [Internet]. Elsevier Ltd; 2017 [cited 2020 mar 2];107:1–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28644961.
Calafat AM, Koch HM, Swan SH, Hauser R, Goldman LR, Lanphear BP, et al. Misuse of blood serum to assess exposure to bisphenol A and phthalates. Breast Cancer Res [Internet]. 2013 [cited 2019 Jul 16];15:403. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3978629&tool=pmcentrez&rendertype=abstract
LaKind JS, Sobus JR, Goodman M, Barr DB, Fürst P, Albertini RJ, et al. A proposal for assessing study quality: Biomonitoring, Environmental Epidemiology, and Short-lived Chemicals (BEES-C) instrument. Environ Int [Internet]. Pergamon; 2014 [cited 2019 Jul 11];73:195–207. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0160412014002232
Sowlat MH, Lotfi S, Yunesian M, Ahmadkhaniha R, Rastkari N. The association between bisphenol A exposure and type-2 diabetes: a world systematic review. Environ Sci Pollut Res [Internet]. 2016 [cited 2018 Sep 18];23:21125–40. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27650850.
Lee JJJ, Choi K, Park J, Moon H-B, Choi G, Lee JJJ, et al. Bisphenol A distribution in serum, urine, placenta, breast milk, and umbilical cord serum in a birth panel of mother–neonate pairs. Sci Total Environ [Internet]. 2018 [cited 2018 mar 16];626:1494–501. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29146078.
Artacho-Cordón F, Arrebola JP, Nielsen O, Hernández P, Skakkebaek NE, Fernández MF, et al. Assumed non-persistent environmental chemicals in human adipose tissue; matrix stability and correlation with levels measured in urine and serum. Environ Res [Internet]. Academic Press Inc.; 2017 [cited 2021 May 24];156:120–7. Available from: https://pubmed.ncbi.nlm.nih.gov/28342347/
Soto AM, Vandenberg LN, Maffini MV, Sonnenschein C. Does breast cancer start in the womb? Basic Clin Pharmacol Toxicol. 2008:125–33.
Ayyanan A, Laribi O, Schuepbach-Mallepell S, Schrick C, Gutierrez M, Tanos T, Lefebvre G, Rougemont J, Yalcin-Ozuysal Ö, Brisken C Perinatal exposure to bisphenol a increases adult mammary gland progesterone response and cell number. Mol Endocrinol [Internet] 2011;25:1915–23. Available from: http://press.endocrine.org.ezproxy.ulb.ac.be/doi/10.1210/me.2011-1129?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub=pubmed, 11
Durando M, Kass L, Piva J, Sonnenschein C, Soto AM, Luque EH, et al. Prenatal bisphenol a exposure induces preneoplastic lesions in the mammary gland in wistar rats. Environ Health Perspect [Internet]. 2006;115:80–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17366824.
Heindel JJ, Blumberg B, Cave M, Machtinger R, Mantovani A, Mendez MA, et al. Metabolism disrupting chemicals and metabolic disorders. Reprod Toxicol [Internet]. 2017 [cited 2019 Jul 10];68:3–33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27760374.
Markey CM, Coombs MA, Sonnenschein C, Soto AM. Mammalian development in a changing environment: exposure to endocrine disruptors reveals the developmental plasticity of steroid-hormone target organs. Evol Dev. 2003;5(1):67–75. https://doi.org/10.1046/j.1525-142X.2003.03011.x.
Markey CM, Luque EH, De Toro MM, Sonnenschein C, Soto AM. In utero exposure to bisphenol A alters the development and tissue organization of the mouse mammary gland. Biol Reprod [Internet]. 2001 [cited 2020 Mar 4];65:1215–23. Available from: https://academic.oup.com/biolreprod/article-abstract/65/4/1215/2723779
Munoz-de-Toro M, Markey C, Wadia PR, Luque EH, Rubin BS, Sonnenschein C, et al. Perinatal exposure to Bisphenol A alters peripubertal mammary gland development in mice. Endocrinology [Internet]. 2005 [cited 2020 Mar 4];146:4138–47. Available from: https://academic.oup.com/endo/article-abstract/146/9/4138/2500852
Murray TJ, Maffini M V., Ucci AA, Sonnenschein C, Soto AM. Induction of mammary gland ductal hyperplasias and carcinoma in situ following fetal bisphenol a exposure. Reprod Toxicol [Internet] 2007;23:383–90. Available from: http://www.sciencedirect.com/science/article/pii/S0890623806002632, 3, DOI: 10.1016/j.reprotox.2006.10.002
Betancourt AM, Eltoum IA, Desmond RA, Russo J, Lamartiniere CA. In utero exposure to bisphenol a shifts the window of susceptibility for mammary carcinogenesis in the rat. Environ Health Perspect [Internet]. 2011;119:1614–9 Available from: http://ehp.niehs.nih.gov/1002148.
Vandenberg LN, Maffini M V., Schaeberle CM, Ucci AA, Sonnenschein C, Rubin BS, et al. Perinatal exposure to the xenoestrogen bisphenol-A induces mammary intraductal hyperplasias in adult CD-1 mice. Reprod Toxicol [Internet]. 2008 [cited 2020 Mar 4];26:210–9. Available from: https://www.sciencedirect.com/science/article/pii/S0890623808002451
Moral R, Wang R, Russo IH, Lamartiniere C, Pereira J, Russo J. Effect of prenatal exposure to the endocrine disruptor bisphenol A on mammary gland morphology and gene expression signature. J Endocrinol [Internet]. 2008;196:101–12. Available from: http://joe.endocrinology-journals.org/content/196/1/101
Jenkins S, Raghuraman N, Eltoum I, Carpenter M, Russo J, Lamartiniere CA. Oral exposure to Bisphenol a increases dimethylbenzanthraceneo-induced mammary cancer in rats. Environ Health Perspect. 2009;117(6):910–5. https://doi.org/10.1289/ehp.11751.
Tharp AP, Maffini M V., Hunt P, Vande Voort C, Sonnenschein C, Soto AM. Bisphenol A alters the development of the rhesus monkey mammary gland. Proc Natl Acad Sci [Internet]. 2012;109:8190–5. Available from: http://www.pnas.org/content/109/21/8190
Castro B, Sánchez P, Torres JM, Preda O, del Moral RG, Ortega E. Bisphenol A Exposure during Adulthood Alters Expression of Aromatase and 5α-Reductase Isozymes in Rat Prostate. PLoS One [Internet]. 2013;8:e55905. Available from: http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0055905
Prins GS, Tang WY, Belmonte J, Ho SM. Developmental exposure to bisphenol A increases prostate cancer susceptibility in adult rats: epigenetic mode of action is implicated. Fertil Steril [Internet]. 2008 [cited 2020 Mar 4];89. Available from: https://www.fertstert.org/article/S0015-0282(07)04305-1/abstract
Wetherill YB, Hess-Wilson JK, Comstock CES, Shah SA, Ralph Buncher C, Sallans L, et al. Bisphenol A facilitates bypass of androgen ablation therapy in prostate cancer. AACR [Internet]. 2006 [cited 2020 Mar 4]; Available from: https://mct.aacrjournals.org/content/5/12/3181.short
Hess-Wilson JK, Webb SL, Daly HK, Leung YK, Boldison J, Comstock CES, et al. Unique bisphenol A transcriptome in prostate cancer: Novel effects on ERβ expression that correspond to androgen receptor mutation status. Environ Health Perspect [Internet]. 2007 [cited 2020 Mar 4];115:1646–53. Available from: http://www.bioconductor.org
Wetherill YB, Petre CE, Monk KR, Puga A, Knudsen KE. The xenoestrogen bisphenol a induces inappropriate androgen receptor activation and mitogenesis in prostatic adenocarcinoma cells. Mol Cancer Ther [Internet]. 2002;1:515–24. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12479269.
Ho S-M, Tang W-Y, Belmonte De Frausto J, Prins GS. Developmental Exposure to Estradiol and Bisphenol A Increases Susceptibility to Prostate Carcinogenesis and Epigenetically Regulates Phosphodiesterase Type 4 Variant 4. Cancer Res [Internet]. 2006 [cited 2020 Mar 4];66:5624–56. Available from: http://cancerres.aacrjournals.org/
Völkel W, Colnot T, Csanády GA, Filser JG, Dekant W. Metabolism and kinetics of bisphenol a in humans at low doses following oral administration. Chem Res Toxicol [Internet]. 2002 [cited 2019 Feb 18];15:1281–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12387626.
Braun JM, Gennings C, Hauser R, Webster TF. What can epidemiological studies tell us about the impact of chemical mixtures on human health? Environ Health Perspect. Public Health Services, US Dept of Health and Human Services. 2016;124:A6–9.
Delfosse V, Grimaldi M, Pons JL, Boulahtouf A, Le Maire A, Cavailles V, et al. Structural and mechanistic insights into bisphenols action provide guidelines for risk assessment and discovery of bisphenol a substitutes. Proc Natl Acad Sci U S A National Academy of Sciences. 2012;109(37):14930–5. https://doi.org/10.1073/pnas.1203574109.
Derouiche S, Warnier M, Mariot P, Gosset P, Mauroy B, Bonnal JL, et al. Bisphenol A stimulates human prostate cancer cell migration via remodelling of calcium signalling. Springerplus [Internet]. SpringerOpen; 2013 [cited 2020 mar 4];2:1–16. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23450760.
De Flora S, Micale RT, La Maestra S, Izzotti A, D’Agostini F, Camoirano A, et al. Upregulation of clusterin in prostate and DNA damage in spermatozoa from bisphenol A-treated rats and formation of DNA adducts in cultured human prostatic cells. Toxicol Sci [Internet]. 2011 [cited 2020 mar 4];122:45–51. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21536718.
Hess-Wilson JK. Bisphenol A May reduce the efficacy of androgen deprivation therapy in prostate cancer [Internet]. Cancer causes control. 2009 [cited 2020 mar 4]. p. 1029–37. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19370395.
Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, Hauser R, Prins GS, Soto AM, et al. Endocrine-disrupting chemicals: An Endocrine Society scientific statement. Endocr Rev. 2009:293–342.
Wetherill YB, Akingbemi BT, Kanno J, McLachlan JA, Nadal A, Sonnenschein C, et al. In vitro molecular mechanisms of bisphenol A action. Reprod Toxicol Pergamon. 2007:178–98.
Lenaz G. Mitochondria and reactive oxygen species. Which role in physiology and pathology? Adv Exp Med Biol. 2012;942:93–136. https://doi.org/10.1007/978-94-007-2869-1_5.
Tiwari D, Kamble J, Chilgunde S, Patil P, Maru G, Kawle D, et al. Clastogenic and mutagenic effects of bisphenol a: an endocrine disruptor. Mutat Res Genet Toxicol Environ Mutagen. 2012;743(1-2):83–90. https://doi.org/10.1016/j.mrgentox.2011.12.023.
Anjum S, Rahman S, Kaur M, Ahmad F, Rashid H, Ansari RA, et al. Melatonin ameliorates bisphenol A-induced biochemical toxicity in testicular mitochondria of mouse. Food Chem Toxicol. 2011;49(11):2849–54. https://doi.org/10.1016/j.fct.2011.07.062.
Ooe H, Taira T, Iguchi-Ariga SMM, Ariga H. Induction of Reactive Oxygen Species by Bisphenol A and Abrogation of Bisphenol A-Induced Cell Injury by DJ-1. Toxicol Sci [Internet]. 2005 [cited 2019 Dec 17];88:114–26. Available from: http://academic.oup.com/toxsci/article/88/1/114/1662794/Induction-of-Reactive-Oxygen-Species-by-Bisphenol
Benhar M, Engelberg D, Reports AL-E, 2002 undefined. ROS, stress-activated kinases and stress signaling in cancer. embopress.org [Internet]. [cited 2020 Mar 3]; Available from: https://www.embopress.org/doi/full/10.1093/embo-reports/kvf094, 3, 5, 420, 425
Yang YJ, Hong Y-C, Oh S-Y, Park M-S, Kim H, Leem J-H, et al. Bisphenol A exposure is associated with oxidative stress and inflammation in postmenopausal women. Environ Res [Internet]. Academic Press; 2009 [cited 2019 Aug 22];109:797–801. Available from: https://www.sciencedirect.com/science/article/pii/S001393510900084X
Ho S-M, Johnson A, Tarapore P, Janakiram V, Zhang X, Leung Y-K. Environmental Epigenetics and Its Implication on Disease Risk and Health Outcomes. ILAR J [Internet]. Oxford University Press (OUP); 2012 [cited 2020 mar 3];53:289–305. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23744968.
Tang WY, Morey LM, Cheung YY, Birch L, Prins GS, Ho SM. Neonatal exposure to estradiol/bisphenol a alters promoter methylation and expression of Nsbp1 and Hpcal1 genes and transcriptional programs of Dnmt3a/b and Mbd2/4 in the ratprostate gland throughout life. Endocrinology [Internet] 2012;153:42–55. Available from: http://press.endocrine.org/doi/10.1210/en.2011-1308, 1
Arrebola JP, Fernández-Rodríguez M, Artacho-Cordón F, Garde C, Perez-Carrascosa F, Linares I, et al. Associations of persistent organic pollutants in serum and adipose tissue with breast cancer prognostic markers. Sci Total Environ Elsevier BV. 2016;566–567:41–9.
Jian L, Po ALW. Kinetic Evaluation of the Ciliotoxicity of Methyl- and Propyl-p-hydroxybenzoates Using Factorial Experiments. J Pharm Pharmacol [Internet]. 1993 [cited 2019 Dec 2];45:98–101. Available from: http://doi.wiley.com/10.1111/j.2042-7158.1993.tb03691.x, 45, 2, 98, 101
Martínez MA, Rovira J, Prasad Sharma R, Nadal M, Schuhmacher M, Kumar V. Comparing dietary and non-dietary source contribution of BPA and DEHP to prenatal exposure: A Catalonia (Spain) case study. Environ Res Academic Press Inc. 2018;166:25–34.
Ye X, Wong LY, Bishop AM, Calafat AM. Variability of urinary concentrations of bisphenol A in spot samples, first morning voids, and 24-hour collections. Environ Health Perspect [Internet]. Environ Health Perspect; 2011 [cited 2020 Jul 9];119:983–8. Available from: https://pubmed.ncbi.nlm.nih.gov/21406337/
Lenters V, Iszatt N, Forns J, Čechová E, Kočan A, Legler J, et al. Early-life exposure to persistent organic pollutants (OCPs, PBDEs, PCBs, PFASs) and attention-deficit/hyperactivity disorder: A multi-pollutant analysis of a Norwegian birth cohort. Environ Int [Internet]. 2019 [cited 2019 Oct 18];125:33–42. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30703609.
Lenters V, Portengen L, Rignell-Hydbom A, Jönsson BAG, Lindh CH, Piersma AH, et al. Prenatal Phthalate, Perfluoroalkyl Acid, and Organochlorine Exposures and Term Birth Weight in Three Birth Cohorts: Multi-Pollutant Models Based on Elastic Net Regression. Environ Health Perspect [Internet]. 2016 [cited 2019 Oct 18];124:365–72. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26115335.
Acknowledgements
Not applicable.
Funding
This work was supported by the Ministry of economy and competitiveness and the National Institute of Health: Instituto de Salud Carlos III (ISCIII). Exps: PI14/00067, PI14/01716, PI14/01880, PI14/00556. BA15/00093. FFIS-CC 2016–06 AECC “Junta provincial de Murcia”. FEDER and AECC 2015. Dr. J.P. Arrebola is under contract within Ramon y Cajal program (RYC-2016-20155, Ministerio de Economía, Industria y Competitividad, Spain). The EPIC-Spain cohort was supported by the Health Research Fund (FIS) - Instituto de Salud Carlos III (ISCIII), the Regional Governments of Andalucía, Asturias, Basque Country, Murcia and Navarra, and the Catalan Institute of Oncology - ICO (Spain).
Author information
Authors and Affiliations
Contributions
All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the manuscript. ESF: Writing- Original draft preparation, Data curation, Investigation. JPA, MJS: Supervision, Resources. MRB, FV: Methodology, Data curation, statistical analysis, Investigation. Chemical analysis. ESF, MRB, PA, JD, MDC, SC, MG, AJ, JPA, FV, NO, AA, MJS: Writing- Reviewing and Editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants were informed at recruitment and they signed an informed consent. This study was approved by Ethics Committee of Granada (Comité de Ética de la Investigación Biomédica de Granada).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Serum BPA levels (ng/ml) (percentage above the limit of detection (LOD) and geometric mean (GM) with 95% confidence interval) by sociodemographic and life style characteristics in breast cancer cases and sub-cohort. Table S2. Serum BPA levels (ng/ml) (percentage above the limit of detection (LOD) and geometric mean (GM) with 95% confidence interval) by sociodemographic and life style characteristics in prostate cancer cases and sub-cohort.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Salamanca-Fernández, E., Rodríguez-Barranco, M., Amiano, P. et al. Bisphenol-A exposure and risk of breast and prostate cancer in the Spanish European Prospective Investigation into Cancer and Nutrition study. Environ Health 20, 88 (2021). https://doi.org/10.1186/s12940-021-00779-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-021-00779-y