Abstract
The main causes of chronic kidney disease (CKD) globally are diabetes and hypertension but epidemics of chronic kidney disease of unknown etiology (CKDu) occur in Central America, Sri Lanka, India and beyond. Althoug also being observed in women, CKDu concentrates among men in agricultural sectors. Therefore, suspicions fell initially on pesticide exposure, but currently chronic heat stress and dehydration are considered key etiologic factors. Responding to persistent community and scientific concerns about the role of pesticides, we performed a systematic review of epidemiologic studies that addressed associations between any indicator of pesticide exposure and any outcome measure of CKD. Of the 21 analytical studies we identified, seven were categorized as with low, ten with medium and four with relatively high explanation value. Thirteen (62%) studies reported one or more positive associations, but four had a low explanation value and three presented equivocal results. The main limitations of both positive and negative studies were unspecific and unquantified exposure measurement (‘pesticides’), the cross-sectional nature of most studies, confounding and selection bias. The four studies with stronger designs and better exposure assessment (from Sri Lanka, India and USA) all showed exposure-responses or clear associations, but for different pesticides in each study, and three of these studies were conducted in areas without CKDu epidemics. No study investigated interactions between pesticides and other concommittant exposures in agricultural occupations, in particular heat stress and dehydration. In conclusion, existing studies provide scarce evidence for an association between pesticides and regional CKDu epidemics but, given the poor pesticide exposure assessment in the majority, a role of nephrotoxic agrochemicals cannot be conclusively discarded. Future research should procure assessment of lifetime exposures to relevant specific pesticides and enough power to look into interactions with other major risk factors, in particular heat stress.
Similar content being viewed by others
Background
The global epidemics of chronic kidney disease of unknown etiology (CKDu)
The primary causes of chronic kidney disease (CKD) are diabetes and hypertension, especially in developed countries [1]. However, for more than two decades, various regions of the world have experienced an excess of CKD unrelated to these traditional causes, hereafter referred to as “CKDu” (for CKD of unknown cause), in particular in Central America and Mexico (Mesoamerican nephropathy) [2], the North-Central Province of Sri Lanka (Sri Lanka nephropathy) [3] and in the state of Andhra Pradesh of India (Uddanam endemic nephropathy) [4, 5], and possibly in other countries like Egypt [6], Tunisia and Morocco [7], and Saudi Arabia [8].
These regional nephropathies occur mostly in poor adult workers in hot tropical agricultural areas, more frequently among men than women [2, 9]. The most heavily affected populations are sugarcane cutters in Mesoamerica, rice paddy farmers in Sri Lanka, and cashew nut, coconut and rice farmers in India [2, 9]. The nephropathy progresses silently to end-stage renal disease (ESRD) leading to the premature death of thousands of workers [10]. In Central America, national CKD mortality rates in El Salvador and Nicaragua in 2009 were about 12 times higher among men and and eight times higher among women as compared to the USA [11]. In Costa Rica, CKD mortality in the CKDu affected area of Guanacaste was almost five times higher than in the rest of the country during 2008-2012 [12]. Excess mortality is attributed to the CKDu epidemics [11,12,13]. In Sri Lanka, no mortality statistics have been published specifically for CKD or CKDu. However, in the North and North-Central Provinces of Sri Lanka diseases of the genitourinary system are the leading cause of inhospital deaths (as compared to the 9th cause for the entire country), which is attributed to the CKDu epidemic [14]. Also in India mortality due to the CKDu epidemics is known to be high in the affected areas [15]. From a clinical viewpoint, the regional nephropathies resemble an interstitial tubular pathology, with patients typically being diagnosed in advanced stages of CKD, without diabetes or hypertension, and with no or low-grade proteinuria [5, 16, 17]. The histology has been presented as predominantly interstitial fibrosis and tubular atrophy in studies from El Salvador [18], Sri Lanka [19,20,21] and India [5]. However, biopsy studies in El Salvador and Nicaragua show important glomerulosclerosis and ischemia with mild to moderate tubulointerstitial damage [22, 23].
Despite clinical, pathological and epidemiologic similarities, as of today it remains uncertain whether the epidemics in different regions of the world correspond to the same disease and whether the causes are the same [9, 24]. In any case, CKDu is now recognized as a serious public health problem to be addressed with renewed efforts in the coming years in Central America [2, 9, 25], Sri Lanka [24] and India [5].
Pesticides and the search for the etiology of CKDu epidemics
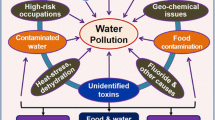
Most researchers believe that the etiology of the unusual CKDu occurrence is multi-factorial [26,27,28,29]. In Central America, both occupational and environmental causes have been suggested, including pesticides, heavy metals, nonsteroidal anti-inflammatory drugs (NSAIDs), infections, alcohol, recurrent dehydration due to occupational heat stress, intake of fructose-rich soft drinks, and hyperuricemia and hyperuricosuria [2, 9, 26, 29,30,31,32,33]. The search for the cause of the epidemic was initially focused on pesticides, because CKDu was observed mostly in men in agricultural areas with important pesticide use [30, 34], but the current leading hypothesis is chronic occupational heat stress and dehydration [2, 9, 35]. In Sri Lanka the focus has been almost exclusively on toxic exposures, both heavy metals and pesticides [36,37,38,39]. CKDu researchers in Andhra Pradesh, India, have postulated high silica levels in drinking water as a possible cause, either as a consequence of leaching from bedrocks or from pesticides containing silica [15], and recently the combination of silica, strontium and NSAIDs has been proposed [40].
In Central America pesticides have been extensively used for over half a century, yet compliance to regulations is poor [41,42,43]. Also in Sri Lanka, pesticide use has been high and largely uncontrolled since the green revolution [44], and also in Andhra Pradesh farmers are highly exposed to pesticides [15]. Nonetheless, in Chichigalpa, Nicaragua, where the highest prevalence of CKDu has been documented among men [45], there was no evidence of high levels of any of 57 pesticides analyzed in groundwater, but the study consisted of only one water sample from six locations [46]. A review of toxicological and epidemiologic data for 36 pesticides used historically by the sugarcane company in that specific area did not find a likely agent to explain the epidemic, but the authors indicated that for six pesticides used currently or in the past (2,4-D, paraquat dichloride, captan, cypermethrin, glyphosate and DBCP) there existed strong or good evidence of associations with acute kidney damage [47]. In cane cutters in El Salvador, urinary residues of several relevant pesticides or their metabolites (chlorpyrifos, 2,4-D, pyrethroids) were unremarkable and residues of chlorpyrifos were below the average levels encountered in the Swedish general population for this pesticide (Kristina Jakobsson, University of Gothenburg, personal communication). At the conclusion of the 1st International Mesoamerican Nephropathy (MeN) Workshop in November 2012, pesticides were considered by the participants as an unlikely cause of MeN [2, 48] and, during the last 5 years, recurrent heat stress and dehydration has emerged as a likely key etiologic factor of CKD [2, 9, 29, 35, 48]. However, community concerns about pesticides have persisted and pesticides as a potential cause of MeN continue being subject of debate also among scientists [11, 13, 28, 29, 49,50,51,52,53]. In addition, exposures to toxic agrochemicals (pesticides and fertilizers) remain a leading hypothesis in Sri Lanka [24, 38], and pesticides are considered as a likely cause of excess CKD in Egypt, where outbreaks of CKDu in rural areas have been reported [6]. The first CKDu review published from India recommends to investigate, besides silica and heat stress, also pesticides as a potential etiology [5].
Based on experimental and sometimes clinical evidence, a number of pesticides in common use in many parts of the world are known human nephrotoxins, albeit causes of acute kidney injury (AKI) rather than CKD, in particular glyphosate [54, 55], 2,4-D [56], paraquat [57,58,59], carbofuran [60], deltamethrin [61], as well as some organophosphates (OP) [62,63,64,65] and organochlorine (OC) insecticides [66,67,68]. Glyphosate has also been shown to trigger epigenetic effects and resulting kidney damage in rats following chronic exposure to ultra-low water concentration of 0.1 ppb of RoundUp [69]. In addition, contamination of commercial formulations of pesticides and fertilizers with heavy metals has been demonstrated in Sri Lanka [37, 44, 70]. Jayasinghe [39] from Sri Lanka went as far as to claim that there is mounting evidence pointing at chemical products used in agriculture, suggesting that CKDu should be renamed “chronic agrochemical nephropathy”.
Our aim was to review all available epidemiologic studies that assessed chronic renal effects from agrochemicals to better understand the current evidence for chronic nephrotoxic effects from pesticides in human populations and how such nephrotoxic effects could or could not underlie the regional epidemics of CKDu that are appearing globally.
Approach for evaluating evidence
Review process
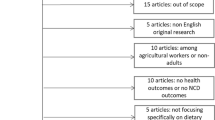
We performed a preliminary inspection to define the start of the review process. It appeared that before 2000 studies only referred to general (acute) nephrotoxicity of pesticides and never to CKD or CKDu. Therefore, we conducted a systematic literature review covering the period of January 1st, 2000 to April 30th 2014 (the date the review started) using PubMed, Lilacs, and, through OvidSP, Embase, Medline, Total access collection, EBMR and Global Health databases using a comprehensive list of key terms such as “chronic renal disease”, “agrochemical”, “kidney disease risk factor”, “pesticide”, “fertilizer”, “end-stage renal disease”, “chronic kidney disorder”. The Additional file 1 contain the complete search strategy. Epidemiological studies providing information on the association between occupational or environmental exposure to agrochemicals and the etiology of CKD or ESRD were included, irrespective of what the primary objective of the study was. A first screening identified potentially relevant publications on the basis of their titles. Further analysis of the publications’ abstracts allowed retaining 25 articles. During the review process we kept a scientific watch for the appearance of new publications and, in a second step, this list was manually complemented with 11 other studies published during this time period, nine peer reviewed articles, a thesis and a scientific university report (see Fig. 1). Despite being unpublished, the latter two studies from Nicaragua were included because they were being discussed as evidence among investigators and policy makers in the region. The 36 publications retrieved were organized per chronological order of publication and country or region in which they were conducted, and study characteristics were extracted along with results for associations between pesticide exposures and CKD or CKDu. We also annotated the authors’ conclusions, and commented on the strengths and limitations of the studies. Because the studies were highly heterogeneous and many had important methodological weaknesses, in particular related to exposure assessment, we did not use a scoring system but, based on design and potential bias (regarding pesticides only), we qualitatively concluded on the relative value of the study to contribute to elucidating the role of pesticides in the etiology of CKD or CKDu, as none, low, medium or high. Specific evaluation criteria were strength of study design, adequacy of outcome or case definition, quality of the exposure assessment, clearness and adequacy of statistical analyses; and potential for selection bias, recall bias and confounding. The details of all 36 reviewed documents are in Additional file 2: Table S1.
Results
Overview of the reviewed studies
Of the 36 documents, two pairs contained data referring to different aspects of a same study, specifically Orantes-Navarro et al. [71], Orantes et al. [72] and Laws et al. [73, 74]. In addition, Siddharth et al. 2012 [75] was an interim report concerning a subset of a larger population included in an article from 2014 [76]. Of the 33 distinct reviewed studies, three were excluded from further analysis since they did not specifically address agrochemicals (Fig. 1) [77,78,79].
The remaining 30 studies were analyzed in view of their potential to provide evidence regarding a potential causal relationship between pesticide exposure and the CKDu epidemics or just CKD. Nine were deemed inadequate in this regard and after assignation of an explanation value ‘none’, they were excluded from further analysis. Of these, one was a case series from El Salvador [17] and four were descriptive studies without hypothesis testing, three from El Salvador [80,81,82] and one from Sri Lanka [37]. In four studies, the results regarding associations of pesticides with kidney disease were not interpretable, either because the methodology underlying the results was not described or because the factual results related to pesticides were not presented: one study each from Mexico [83] and El Salvador [71, 72], and two from Sri Lanka [38, 84] (for details on studies with explanation value ‘none’, see Additional file 2: Table S1). This left 21 studies (23 articles) that analyzed associations between varying pesticide exposures and varying CKD outcomes [6, 19, 36, 45, 73,74,75,76, 85,86,87,88,89,90,91,92,93,94,95,96,97,98,99], 11 from Mesoamerica (Table 1) and 10 from other parts of the world (5 from Sri Lanka, 2 from the USA, and 1 each from Egypt, India and Thailand) (Table 2).
Methodological aspects of the reviewed studies
Tables 1 and 2 summarize basic epidemiologic characteristics of the 21 studies. With regard to study design, 13 studies were cross-sectional in nature [19, 45, 86,87,88,89,90,91,92,93,94, 98, 99], including five studies, − four population-based surveys [19, 45, 90, 92] and a screening program [89] -, that also performed nested case-control analyses. Five studies had a case-control design, all hospital-based and with prevalent cases [6, 36, 75, 76, 85, 95]. Only three studies had a longitudinal design, a prospective cohort during one harvest season among Nicaraguan sugarcane workers [73, 74] and two prospective cohorts of the USA Agricultural Health Study (AHS) among licensed pesticide applicators in Iowa and North Carolina and their wives, respectively, with a follow-up of more than 15 years [96, 97].
Depending on the design, the study populations comprised entire communities or a subset, volunteers, or groups of farmers or agricultural workers, in Mesoamerica especially sugarcane workers. Cases were often hospital CKD or CKDu patients, and controls most often patients with other diagnoses. The studies under scrutiny used many different markers and definitions of CKD, most often proteins in urine, serum creatinine (SCr) and CKD stages based on estimated glomerular filtration rate (eGFR), and a single study also early markers of tubular injury. All studies in Sri Lanka, India and Egypt were restricted to CKDu cases whereas in Mesoamerica and other countries, all cases of CKD were included in the studies independently of their cause.
With regard to exposure assessment, practically all studies focused on pesticide exposures in occupational settings and in the majority the exposure assessment was extremely crude. Eleven studies only had a dichotomous yes/no exposure variable of pesticide use without any specification of pesticidal agents or any quantification of duration and/or intensity of exposure over the lifetime [6, 19, 36, 85,86,87, 89, 91,92,93, 98]. Several studies used a proxy of high exposures, specifically the job title of pesticide applicator [73, 74, 96, 97], a history of self-reported pesticide poisoning [45, 88, 97], and an index of life-time days of mixing-spraying pesticides without specification of pesticidal agents [45, 96, 97], whereas three studies assessed the effects of a number of specific pesticidal agents but without quantification of their use [94, 95, 99]. One of these latter studies, a case-control from Sri Lanka, combined questionnaire data about source of drinking water with levels of glyphosate residues and hardness of the water to evaluate a gradient of exposure levels [95]. Only the two cohorts of the AHS in the USA computed intensity weighted lifetime use for specific pesticidal agents or groups of chemicals, defined as the product of frequency and duration of use, modified by an intensity factor to account for differences in application practices [96, 97]. A single study used biomarkers, i.e. blood concentrations of OC pesticides or their metabolites [75, 76], focusing on non-occupational exposures in Delhi, India. Lebov et al. [96] also examined several indicators of non-occupational exposures among wives of licensed applicators in the USA.
Many of the reviewed studies had no or inadequate control of potential confounding; selection bias related to volunteer participation, high non-participation, or the use of inadequate case or control groups; possible recall bias; and deficient description of statistical analyses (see Additional file 2: Table S1). We classified the explanation value of seven of the studies as relatively low, ten as medium, and four as relatively high (Table 3).
Findings and validity of the reviewed studies
Thirteen studies (62%) reported one or more positive associations between a pesticide exposure indicator and an indicator of CKD: four studies with a relatively low, five with a medium, and all four with a relatively high explanation value. Of the eight negative studies, three had a low explanation value and five were considered to have a medium explanation value (Table 3).
Studies considered with relatively low explanation value
Regarding the four studies with lower explanation value that reported a positive association between pesticides and CKD [6, 85, 87, 88], control of potential confounding was absent in three and inadequate in one study (no adjustment for age despite controls being 10 years older), and in three of these studies the exposure assessment was based on one single dichotomous ‘pesticide’ exposure variable. One could argue that the studies with ‘pesticide’ as the exposure variable could have given rise to a bias of non-differential exposure misclassification and that the true risk was higher than the observed. However, without control of potential confounding, an alternative explanation could also be that ‘pesticides’ correlate with other agricultural exposures, in particular heat stress. The fourth study [87] compared red blood cell acetylcholinesterase (AChE) levels among four groups, with and without OP exposure and with and without chronic renal failure (CRF). An important limitation of this study was that the unexposed groups were participants of other studies in other regions. The three negative studies with low explanation value had, besides non-specific and non-quantified exposure assessment, multiple other sources of potential bias (see Additional file 2: Table S1). The negative study from Thailand compared a group of farm workers highly exposed to pesticides on a daily basis (not all, 88%) with an undefined group of non-farmers from the same region without consideration of potential confounding [98]. The negative studies from El Salvador and Sri Lanka used proteinuria as a marker for CKDu, although CKDu is basically a non-proteinuric disease, leading to incomplete case detection and possible selection bias [86, 92].
Studies considered with medium explanation value
Of the 10 studies with a medium explanation value, five did not observe any association and five reported some positive association, albeit with equivocal or ambiguous results in three studies. All studies in this category had a cross-sectional design, except one negative cohort in Nicaragua.
Of the studies with a positive finding, three were community-based surveys conducted in the municipalities of León and Chinandega in Nicaragua [45, 89, 90], the region with the highest CKDu occurrence of Mesoamerica, especially among men [45]; one was an occupational cross-sectional survey among cane cutters in a CKDu epidemic area in El Salvador [94] and one a population-based survey in CKDu endemic and non-CKDu regions in Sri Lanka [19]. One of the studies in the Nicaraguan hotspot observed a weak association between ‘pesticide’ exposure both in data obtained through screening of volunteers (odds ratio (OR) =1.4, 95% confidence interval (CI) 0.9-2.1) and in a nested case-control analysis restricted to male participants (OR 1.6, 95% CI 1.0-2.6) [89]. This study controlled for confounding factors, and besides its crude exposure assessment, its main limitation was that study participants were volunteers and the authors did not address how a possible selection bias could have affected their results. The study in the hotspot in El Salvador found that ‘ever use of carbamate insecticides’ was more common among cane cutters with reduced eGFR than among cutters with normal eGFR (74% vs 29%) and carbamate use was a significant predictor for reduced eGFR in multivariate analyses [94]. This study was negative for all other specific pesticides or groups of pesticides that were examined qualitatively, including the herbicides glyphosate and paraquat. With regard to the three studies with equivocal or ambiguous results [19, 45, 90], in Nicaragua a non-significant increased risk of CKD stage ≥3 (OR 1.9, 95% CI 0.8-4.1) was found for ‘any pesticide exposure’, whereas no association was found for ‘applying and mixing pesticides’, the latter indicator likely reflecting higher exposures than the former [90]. In the hotspot of Chinandega, Raines et al. [45] reported a significant association of reduced kidney function with a vague exposure indicator ‘ever accidentally inhaling pesticides’ (OR 3.3, 95% 1.3-8.3) among agricultural workers, but did not find a relationship of CKD with a semi-quantitative exposure measure of life-time days of pesticide applications. The fifth study with a positive result, from Sri Lanka, reported an association between non specific and unquantified pesticide use and proteinuric CKD after adjusting for confounding (OR 2.3, 95% CI 1.4 – 3.9) but when stratifying by region the association was restricted to Hambantota, an area with low prevalence of CKDu (OR 5.6, 95% CI 2.3 – 13.2), whereas no association was observed in Medawachchiya, an area in the North Central province with high prevalence of CKDu (OR 1.1, 95% CI 0.7-1.9) [19].
Concerning the five negative studies with medium explanation value, their main limitation was the crude exposure assessment, three with a dichotomous pesticide exposure variable [91,92,93], one with jobtitle of pesticide applicator indicative only of current exposure [73, 74], and one with unquantified exposure of specific pesticides [99]. One negative study from Sri Lanka used proteinuria as a marker for CKD although CKDu is basically a non-proteinuric disease, possibly causing selection bias [86, 92]. One Nicaraguan study was conducted in a high-altitude non-CKDu area, not finding CKDu cases [93]. Another negative Nicaraguan study, a cohort of sugarcane workers, was conducted in the same hotspot of MeN as studies mentioned above [73, 74]. It compared change in SCr or eGFR and in markers of early tubular injury over the course of a 6-month harvest season beween workers performing different tasks. Pesticide applicators did not present any changes, in contrast with cutters and seeders exposed to extreme heat, whose eGFR did significantly decrease together with an increase of markers of early kidney damage. However, the limitation of using job title for current exposure without further specifications of exposure and its modifying factors was not addressed.
Studies considered with relatively high explanation value
The four studies (five articles) with a relatively high explanation value all reported a positive association between one or more pesticide exposure indicators and different markers of CKD [75, 76, 95,96,97]. One case-control study in a CKDu endemic area in Sri Lanka found a significant association with overall pesticide application (OR 2.3, 95% CI 1.0-5.6) and use of glyphosate (OR 5.1, 95% CI 2.3-11.3), adjusted for age, sex, education, family CKD and exposure modifiers [95]. Although this study did not quantify the use of specific pesticides, it was the only one among all those conducted in CKDu endemic areas that investigated a potential exposure-response relationship by combining questions on water intake from different sources in relation to water hardness and levels of the herbicide glyphosate detected in water. With drinking pipe water or reservoir water with soft water and with traces or no detection of glyphosate as the reference, drinking from serving wells with hard water and intermediate concentrations of glyphosate (median 0.6 μg/L) yielded an adjusted OR of 2.5 (95% CI 1.1-5.7), and drinking from abandoned wells with very hard water and highest concentrations of glyphosate (median 3.2 μg/L) yielded an adjusted OR of 5.5 (95% CI 2.9-10.3).
The three remaining studies with a higher explanation value were conducted in non-CKDu regions. The study in Delhi, India, found an association between blood concentrations of OCs and their metabolites with CKDu, in particular for alpha- and gamma-hexachlorocyclohexane, aldrin, and alpha- and beta-endosulfan [75, 76]. This study was conducted in an urban setting and, in addition, all subjects occupationally exposed to pesticides were excluded. Therefore, the observed relationships between OCs and CKDu can only derive from dietary and environmental exposures. The cohort of the AHS among licensed applicators in the USA observed significant exposure-response relationships of ESRD with all pesticides combined and specific pesticides (alachlor, atrazine, metalochlor, paraquat, pendimethalin, and permethrin) as well as increased risks in relation to more than one medical visit and hospitalization due to any pesticide use [97]. The cohort among the wives of licensed applicators showed an exposure-response relationship between ESRD and all pesticides combined among the subset of women who ever sprayed pesticides, and a significant exposure-response association between ESRD and the husband’s cumulative uses of paraquat and butylate among the women who had never worked with pesticides [96].
Discussion
The epidemiologic evidence for pesticides as a causal factor in CKDu
In this review we included to the best of our knowledge all epidemiologic studies conducted this century that examined an association between pesticide exposures and any of a variety of outcomes indicating CKD. However, few of the 21 analytical studies had a robust design and, although 13 (62%) of the studies reported one or more positive associations, 4 of these studies were of low quality [6, 85, 87, 88], 3 had equivocal results [19, 45, 90] and 3 were not conducted in a CKDu-endemic region [75, 76, 96, 97]. In general, the heterogeneity in study designs, exposure assessment and outcomes or case definitions, together with important bias in most studies, severely limit the interpretation of both positive and negative results and the comparisons between these studies. In particular the unquantified and/or unspecific pesticide exposure assessment contributed to low quality of the studies. ‘Pesticides’ is a questionable exposure measure, because pesticides are a group composed of hundreds of toxins with distinct toxicological actions. In addition, the use of pesticidal agents varies enormously between crops, regions and over time, as well as exposure determinants such as mixing and application methods, use of personal protective equipment, and storage and disposal practices. None of the studies conducted in CKDu endemic or epidemic areas examined all such factors in depth and most of these studies, either positive or negative, add only marginally to the evidence in pro or con of a causal association between pesticides and CKD or CKDu, due to their methodological limitations. Even if toxicological data demonstrate the nephrotoxicity of specific pesticides, deficient exposure assessment may result in false negative studies [100].
Positive associations between pesticides and CKD or CKDu became more apparent with stronger designs and better exposure assessments but, of the four studies classified as with higher explanation value, three were conducted in non-CKDu regions limiting the generalization of these results to areas with high prevalence of CKDu. Of the three remaining positive studies, one reported in Nicaragua a weak relationship between eGFR <60 and any nonspecific and unquantified pesticide exposure [90], one reported in El Salvador an association of reduced eGFR with carbamate insecticides [94], and the strongest study by Jayasumana et al. [95] implicated glyphosate as a causal agent in the CKDu epidemic in Sri Lanka.
Conversely, none of the negative studies was classified as with a higher explanation value. The strongest evidence against a pesticide association with CKDu epidemics has been provided by the cohort of Nicaraguan sugarcane workers, which did not show kidney effects during the 6-month follow-up of pesticide applicators [73, 74]. Whether or not such a short period of exposure could have triggered kidney damage was not discussed, and the study did not include individual exposure measures. Two cross-sectional studies, conducted in the same area, did not observe associations between reduced eGFR and days of pesticide use over a lifetime [45] and use of several specific pesticides including glyphosate and paraquat [99], respectively. However, not one of the negative studies had a comprehensive exposure assessment.
When taking a closer look at the four studies classified as with higher explanation value, all four reported positive findings for specific pesticides. In Sri Lanka, glyphosate applications associated with a highly increased risk for CKDu among male farmworkers, and an exposure-response for water intake from glyphosate polluted wells was observed in the only high explanation value study conducted in a CKDu epidemic area [95]. The herbicide glyphosate is a ubiquitously used nephrotoxic pesticide, including on rice in Sri Lanka and on sugarcane in Mesoamerica. The findings of this study are in accordance with a previously launched hypothesis that glyphosate, a metal-chelating agent, forms glyphosate-metal complexes in the presence of hard water and that the intake of such water could produce kidney damage [44, 101]. A very small study also examined urinary levels of many different metals and glyphosate in endemic CKDu cases (n = 10) and endemic (n = 10) and non-endemic (n = 10) healthy controls [101]. Levels were higher in both cases and controls in the CKDu area as compared to the area without CKDu, but the higher levels in cases in the endemic area were compatible with leakage into urine due to renal damage (Gerd Sällsten, University of Gothenburg, personal communication). In addition, glyphosate was not identified as a risk factor in studies in the USA [97], El Salvador [94] and Nicaragua [99]. According to Jayasumana et al. [101], the time of appearance of the epidemic in Sri Lanka coincides with the introduction and subsequent widespread use of this herbicide in Sri Lanka. However, in Central America there are differences in timing between the use of glyphosate and the surge of the CKDu epidemic. Precisely, although glyphosate is aerially sprayed since the 1990s as a maturation agent in sugarcane fields situated in areas where most CKDu cases occur, increased CKD mortality in the MeN-endemic area of Guanacaste in Costa Rica was observed as early as in the 1970s, at least a decade before the introduction of glyphosate on the market [12]. Thus, as of today, glyphosate can be considered as a potential risk factor for CKDu in Sri Lanka, but not in Mesoamerica.
Although the findings of the other three studies with high explanation value contribute to evidence of associations between various types of pesticides and CKD, they cannot be generalized to explain the CKDu epidemics in other regions [75, 76, 96, 97]. Regarding the study in urban Delhi, the associations between CKDu stage ≥3 and dietary or environmental exposures to OC insecticides [75, 76] do not exhibit differences in CKDu occurrence beween men and women. Exposure to OC alone would neither explain the CKDu epidemics in Central America and Sri Lanka, mainly because the clear male predominance is not in line with overall environmental OC pesticide exposures. OCs have been widely used worldwide against vector born diseases and, in Central America, also intensively in cotton cultivation during the 1970s [102], including in several of the regions of El Salvador and Nicaragua with current CKDu epidemics. OCs were banned or severely restricted since the 1980s [103], but there are stockpiles of obsolete pesticides in controlled and uncontrolled sites that may contaminate water and soil and eventually lead to human exposures. However, the only Central American location with co-occurrence of identified environmental pesticide contamination and excess CKDu cases in both male and female inhabitants is Las Brisas in El Salvador [71, 72].
The US cohort study of licensed applicators observed causal associations between ESRD and a considerable number of specific pesticidal agents as well as to repeated medical visits and hospitalization due to unspecified pesticide use [97]. Most interesting is the association with paraquat, also implicated in ESRD among the wives of the applicators [96]. Paraquat is a widely used herbicide, including in the CKDu epidemic regions around the world, and its acute nephrotoxicy is well-known. The positive results from the USA cohorts [96, 97] raise questions about much overlooked nephrotoxic effects of different pesticides, not surprisingly since the kidney is an excretory organ of toxins, and this should be further explored in other settings. It seems feasible that the increased risk of ESRD related to paraquat use and medical conditions from pesticide exposures is a consequence of episodes of clinical or subclinical AKI caused by nephrotoxic pesticides. Noteworthy, clinical AKI is associated with development of CKD later in life [104].
Of note is that only six studies (7 articles), in five countries, specified pesticidal agents [75, 76, 94,95,96,97, 99]. Each study reported different associations or no-associations, except for paraquat which was associated with ESRD both among the licensed applicators and their wives. One possible interpretation of the incongruent pattern in different regions could be that different sets of contributing causes, including different pesticides, trigger the occurrence of the same disease in different regions. However, currently there is no reasonable evidence to sustain this hypothesis.
The clear predominance of CKDu among males in agricultural sectors of both Mesoamerica, Sri Lanka and India allows commenting about the occupational versus environmental nature of the epidemics. Male predominance may be a consequence of occupational exposures that are related to gender differences, such as pesticide mixing and spraying or strenuous work done mostly by men, or there may be a biological difference between sexes responding to a toxic or physical insult, or both. Relatively few studies have explored occupational differences more in depth through stratified analyses by sex. In El Salvador, CKD was much more prevalent among males on the community level, but women who had worked in sugarcane and cotton plantations were also at increased risk for CKD just as their male colleagues, which suggests that the gender differences are in fact attributable to occupational exposures and not to sex differences [78].
Data examined at the time of the First and Second International Workshops on Mesoamerican Nephropathy in 2012 and 2015, respectively, led to insights that MeN is an occupational disease [2, 9]. The Consortium on the Epidemic of Nephropathy in Central America and Mexico (CENCAM) issued a statement that occupational heat stress is a likely key factor in the MeN epidemic and that pesticides is one of the risk factors that need to be investigated further, both a potential etiologic role and a possible role in disease progression [105]. It has been pointed out that heat exposure alone likely does not explain the disease pattern, and a ‘heat-plus’ hypothesis has been proposed [106]. On the other hand, Jayasumana et al. [28] questioned why in other regions with similar climatic conditions, there are no CKDu epidemics or, conversely, why CKDu occurs among people assumedly not exposed to extreme working conditions. Occupational pesticide and heat exposures co-occur in agricultural settings but no studies have looked yet into potential interactions between pesticides and heat stress, although a combined impact of these two separate factors seems plausible, as primary causal factors as well as in disease progression. Additional to its own adverse effects on the kidney, heavy physical workload in intense heat may result in increased exposure to putative nephrotoxic agrochemicals, because of greater pulmonary ventilation leading to greater inhaled intake, as well as of increased doses absorbed through the skin due to dilatation of skin’s capillaries and pores. Further in-depth exploration of the various identified or hypothesized risk factors and their interactions could improve the understanding of a possible multi-causality in CKDu epidemics.
Concluding remarks
This review found some evidence of associations between pesticides exposure and CKD or CKDu, more clearly in studies with stronger design and better exposure assessment. Although these findings add to the recognition that certain pesticides produce acute and chronic kidney damage in humans, there is no strong epidemiologic evidence that pesticides are the culprit of the CKDu epidemics in Mesoamerica, Sri Lanka and beyond. Glyphosate in Sri Lanka could be an exception, but no associations have been seen for this herbicide in other CKDu regions. For a specific pesticide to be a key cause of an epidemic of the magnitude seen in Mesoamerica, Sri Lanka and India, it must be present during prolonged time periods in a diversity of agricultural settings in multiple countries, while generating elevated and widespread occupational or environmental exposures. Such a pesticide has not been identified.
Yet, up to today, no research has been conducted in CKDu endemic areas with a strong design and examining the role of lifetime exposures to specific pesticides or chemical groups with similar toxicological actions, especially not in combination with heat exposure or other major risk factors. Therefore, a role of nephrotoxic agrochemicals in the etiology of CKDu and the extent of their contribution to the CKDu epidemic, if any, cannot be adequately evaluated based on currently available data. Given the diversity of pesticide use, such research is difficult and costly, but necessary to elucidate the role, if any, of agrochemicals in this epidemic. We recommend that any future pesticide research should be conducted with the best possible assessment of lifetime exposures to relevant specific pesticides and enough power to look at interactions with other risk factors, in particular heat stress.
Abbreviations
- AChE:
-
Acetylcholinesterase
- ACR:
-
Albumin creatinine ratio
- AHS:
-
Agricultural Health Study
- AKI:
-
Acute kidney injury
- ANOVA:
-
Analysis of variance
- BUN:
-
Blood urea nitrogen
- CENCAM:
-
Consortium on the Epidemic of Nephropathy in Central America and Mexico
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CKDu:
-
Chronic Kidney Disease of unknown etiology
- CRF:
-
Chronic renal failure
- DB:
-
Diabetes
- DDE:
-
Dichlorodiphenyldichloroethylene
- DW:
-
Drinking water
- eGFR:
-
Estimated glomerular filtration rate
- ESRD:
-
End-stage renal disease
- F:
-
Female
- GST:
-
Glutathione-S-transferase
- HCH:
-
Hexachlorocyclohexane
- HT:
-
Hypertension
- IL-18:
-
Interleukin-18
- M:
-
Male
- MeN:
-
Mesoamerican nephropathy
- MVLR:
-
Multivariate logistic regression
- NAG:
-
N-acetyl-β-o-glucosaminidase
- NGAL:
-
Neutrophil gelatinase-associated lipocalin
- NSAID:
-
Nonsteroidal anti-inflammatory drugs
- OC:
-
Organochlorine
- OP:
-
Organophosphate
- OR:
-
Odds ratio
- PAHO:
-
Pan American Health Organization
- SCr:
-
Serum creatinine
- USA:
-
United States of America
References
Levey AS, Coresh J. Chronic kidney disease. Lancet. 2012;379:165–80.
Wesseling C, Crowe J, Hogstedt C, Jakobsson K, Lucas R, Wegman D. Mesoamerican nephropathy: report from the first international research workshop on MeN. Heredia: SALTRA, IRET-UNA; 2013. http://www.regionalnephropathy.org/wp-content/uploads/2013/04/Technical-Report-for-Website-Final.pdf. Accessed 15 May 2016.
Chandrajith R, Nanayakkara S, Itai K, Aturaliya TNC, Dissanayake CB, Abeysekera T, et al. Chronic kidney diseases of uncertain etiology (CKDue) in Sri Lanka: geographic distribution and environmental implications. Environ Geochem Health. 2011;33:267–78.
Singh AK, Farag YMK, Mittal BV, Subramanian KK, Reddy SRK, Acharya VN, et al. Epidemiology and risk factors of chronic kidney disease in India - results from the SEEK (screening and early evaluation of kidney disease) study. BMC Nephrol. 2013;14:114.
Ganguli A. Uddanam nephropathy/regional nephropathy in India: preliminary findings and a plea for further research. Am J Kidney Dis. 2016;68:344–8.
Kamel EG, El-Minshawy O. Environmental factors incriminated in the development of end stage renal disease in el-Minia governorate, Upper Egypt. Int J Nephrol Urol. 2010;2:431–7.
Barsoum RS. Burden of chronic kidney disease: North Africa. Kidney Int Suppl. 2011;2013(3):164–6.
El Minshawy O, Ghabrah T, El Bassuoni E. End-stage renal disease in Tabuk area, Saudi Arabia: an epidemiological study. Saudi J Kidney Dis Transpl. 2014;25:192–5.
Wegman D, Crowe J, Hogstedt C, Jakobsson K, Wesseling C. Mesoamerican nephropathy: report from the second international research workshop on MeN. Heredia: SALTRA, IRET-UNA; 2016. http://www.regionalnephropathy.org/wp-content/uploads/2016/08/MeN-2015-Scientific-Report-high-resolution_final.pdf. Accessed 30 Nov 2016.
Ramirez-Rubio O, McClean MD, Amador JJ, Brooks DR. An epidemic of chronic kidney disease in central America: an overview. Postgrad Med J. 2013;89:123–5.
Ordunez P, Martinez R, Reveiz L, Chapman E, Saenz C, Soares da Silva A, et al. Chronic kidney disease epidemic in central America: urgent public health action is needed amid causal uncertainty. PLoS Negl Trop Dis. 2014;8:e3019.
Wesseling C, van Wendel de Joode B, Crowe J, Rittner R, Sanati NA, Hogstedt C, et al. Mesoamerican nephropathy: geographical distribution and time trends of chronic kidney disease mortality between 1970 and 2012 in Costa Rica. Occup Environ Med. 2015;72:714–21.
Ordunez P, Saenz C, Martinez R, Chapman E, Reveiz L, Becerra F. The epidemic of chronic kidney disease in central America. Lancet Glob Health. 2014;2:e440–1.
Wijewickrama ES, Weerasinghe D, Sumathipala PS, Horadagoda C, Lanarolle RD, Sheriff RMH. Epidemiology of chronic kidney disease in a Sri Lankan population: experience of a tertiary care center. Saudi J Kidney Dis Transpl. 2011;22:1289–93.
Chatterjee R. Mysterious kidney disease goes global. Science. 2016; http://www.sciencemag.org/news/2016/03/mysterious-kidney-disease-goes-global. Accessed 15 May 2016.
Wernerson A, Wijkström J, Elinder C-G. Update on endemic nephropathies. Curr Opin Nephrol Hypertens. 2014;23:232–8.
Herrera R, Orantes CM, Almaguer M, Alfonso P, Bayarre HD, Leiva IM, et al. Clinical characteristics of chronic kidney disease of nontraditional causes in Salvadoran farming communities. MEDICC Rev. 2014;16:39–48.
López-Marín L, Chávez Y, García XA, Flores WM, García YM, Herrera R, et al. Histopathology of chronic kidney disease of unknown etiology in Salvadoran agricultural communities. MEDICC Rev. 2014;16:49–54.
Athuraliya NTC, Abeysekera TDJ, Amerasinghe PH, Kumarasiri R, Bandara P, Karunaratne U, et al. Uncertain etiologies of proteinuric-chronic kidney disease in rural Sri Lanka. Kidney Int. 2011;80:1212–21.
Wijetunge S, Ratnatunga NVI, Abeysekera DTDJ, Wazil AWM, Selvarajah M, Ratnatunga CN. Retrospective analysis of renal histology in asymptomatic patients with probable chronic kidney disease of unknown aetiology in Sri Lanka. Ceylon Med J. 2013;58:142–7.
Wijetunge S, Ratnatunga NVI, Abeysekera TDJ, Wazil AWM, Selvarajah M. Endemic chronic kidney disease of unknown etiology in Sri Lanka: correlation of pathology with clinical stages. Indian J Nephrol. 2015;25:274–80.
Wijkström J, Leiva R, Elinder C-G, Leiva S, Trujillo Z, Trujillo L, et al. Clinical and pathological characterization of Mesoamerican nephropathy: a new kidney disease in central America. Am J Kidney Dis. 2013;62:908–18.
Wijkström J, González-Quiroz M, Hernandez M, Trujillo Z, Hultenby K, Ring A, et al. Renal Morphology, Clinical Findings, and Progression Rate in Mesoamerican Nephropathy. Am J Kidney Dis. 2017. [Epub ahead of print].
WHO Country office for Sri Lanka. Report of the international expert consultation on chronic kidney disease of unknown etiology (CKDu) in Sri Lanka. 2016. http://www.searo.who.int/srilanka/documents/report_international_expert_consultation_on_ckdu.pdf?ua=1. Accessed 15 May 2016.
PAHO. Chronic kidney disease in agricultural communities in central America. 52nd directing council of PAHO, 65th session of the regional committee of WHO for the Americas; 2013 Sep 30-Oct 4. Washington (DC): Pan American Health Organization; 2013. http://www.paho.org/hq/index.php?option=com_docman&task=doc_download&gid=23347&Itemid=270&lang=en. Accessed 16 May 2016.
Soderland P, Lovekar S, Weiner DE, Brooks DR, Kaufman JS. Chronic kidney disease associated with environmental toxins and exposures. Adv Chronic Kidney Dis. 2010;17:254–64.
Wanigasuriya K. Update on uncertain etiology of chronic kidney disease in Sri Lanka’s north-central dry zone. MEDICC Rev. 2014;16:61–5.
Jayasumana C, Orantes C, Herrera R, Almaguer M, Lopez L, Silva LC, et al. Chronic interstitial nephritis in agricultural communities: a worldwide epidemic with social, occupational and environmental determinants. Nephrol Dial Transplant. 2016.
Correa-Rotter R, Wesseling C, Johnson RJ. CKD of unknown origin in central America: the case for a Mesoamerican nephropathy. Am J Kidney Dis. 2014;63:506–20.
Cuadra SN, Jakobsson K, Hogstedt C, Wesseling C. Chronic kidney disease: assessment of current knowledge and feasibility for regional research collaboration in central America. Heredia: SALTRA, IRET-UNA; 2006. Report No.: 2. http://www.iret.una.ac.cr/Publicaciones/01-0008.pdf. Accessed 2 July 2016.
Brooks DR, Ramirez-Rubio O, Amador JJ. CKD in central America: a hot issue. Am J Kidney Dis. 2012;59:481–4.
Weiner DE, McClean MD, Kaufman JS, Brooks DR. The central American epidemic of CKD. Clin J Am Soc Nephrol. 2013;8:504–11.
Roncal-Jiménez C, Lanaspa MA, Jensen T, Sanchez-Lozada LG, Johnson RJ. Mechanisms by which dehydration may lead to chronic kidney disease. Ann Nutr Metab. 2015;66(Suppl 3):10–3.
Flores Reyna R, Jenkins Molieri J, Vega Manzano R, Chicas Labor A, Leiva Merino R, Calderon G, et al. Enfermedad renal terminal: Hallazgos preliminares de un reciente estudio en el Salvador [End stage renal disease: Preliminary findings of a recent study in El Salvador]. Salud para un país de future [Health for a country of the future]. PAHO. 2004. p. 222–30.
Wesseling C, Crowe J, Hogstedt C, Jakobsson K, Lucas R, Wegman DH. The epidemic of chronic kidney disease of unknown etiology in Mesoamerica: a call for interdisciplinary research and action. Am J Public Health. 2013;103:1927–30.
Wanigasuriya KP, Peiris-John RJ, Wickremasinghe R, Hittarage A. Chronic renal failure in north Central Province of Sri Lanka: an environmentally induced disease. Trans R Soc Trop Med Hyg. 2007;101:1013–7.
Bandara JMRS, Senevirathna DM, Dasanayake DM, Herath V, JMRP B, Abeysekara T, et al. Chronic renal failure among farm families in cascade irrigation systems in Sri Lanka associated with elevated dietary cadmium levels in rice and freshwater fish (Tilapia). Environ Geochem Health. 2008;30:465–78.
Jayatilake N, Mendis S, Maheepala P, Mehta FR. Chronic kidney disease of uncertain aetiology: prevalence and causative factors in a developing country. BMC Nephrol. 2013;14:180.
Jayasinghe S. Chronic kidney disease of unknown etiology should be renamed chronic agrochemical nephropathy. MEDICC Rev. 2014;16:72–4.
Khandare AL, Reddy YS, Balakrishna N, Rao GS, Gangadhar T, Arlappa N. Role of drinking water with high silica and strontium in chronic kidney disease: an exploratory community-based study in an Indian Village. Indian J Comm Health. 2015;27:95–102.
Wesseling C, Corriols M, Bravo V. Acute pesticide poisoning and pesticide registration in central America. Toxicol Appl Pharmacol. 2005;207:697–705.
Wesseling C, Aragón A, Castillo L, Corriols M, Chaverri F, de la Cruz E, et al. Hazardous pesticides in Central America. Int J Occup Environ Health. 2001;7:287–94.
Bravo V, Rodríguez T, van Wendel de Joode B, Canto N, Calderón GR, Turcios M, et al. Monitoring pesticide use and associated health hazards in central America. Int J Occup Environ Health. 2011;17:258–69.
Jayasumana M, Paranagama P, Amarasinghe M, Fonseka S. Arsenic, lead and cadmium in technical organic pesticide compositions and in fertilizers available in the Sri Lankan market. Addendum on pesticides as a possible causal factor of MeN. Mesoamerican nephropathy: report from the first international research workshop on MeN. Heredia. SALTRA, IRET-UNA. 2013. 239–40.
Raines N, González M, Wyatt C, Kurzrok M, Pool C, Lemma T, et al. Risk factors for reduced glomerular filtration rate in a Nicaraguan community affected by Mesoamerican nephropathy. MEDICC Rev. 2014;16:16–22.
Atkins D, McClean M, Brooks D. Phase I Environmental Monitoring: April 2010 assessment of water samples. Boston University School of Public Health; 2010. http://www.cao-ombudsman.org/cases/document-links/documents/Water_sampling_report_August2010.pdf. Accessed 16 May 2016.
McClean M, Laws R, Ramirez Rubio O, Brooks D. Industrial hygiene/occupational health assessment: Evaluating potential hazards associated with chemicals and work practices at the Ingenio San Antonio (Chichigalpa, Nicaragua). Boston University School of Public Health; 2010. http://www.cao-ombudsman.org/cases/document-links/documents/FINALIHReport-AUG302010-ENGLISH.pdf. Accessed 16 May 2016.
Wesseling C, Crowe J, Hogstedt C, Jakobsson K, Lucas R, Wegman DH, et al. Resolving the enigma of the mesoamerican nephropathy: a research workshop summary. Am J Kidney Dis. 2014;63:396–404.
Orduñez P, Silva LC. Pesticides and the epidemic of CKD in central America. Am J Kidney Dis. 2014;64:477.
Silva LC, Ordúñez P. Chronic kidney disease in central American agricultural communities: challenges for epidemiology and public health. MEDICC Rev. 2014;16:66–71.
Hanson L, Haynes LK, Turiano L. Chronic kidney disease in central America: the big picture. Am J Public Health. 2014;104:e9.
Wesseling C, Crowe J, Hogstedt C, Jakobsson K, Lucas R, Wegman D. Wesseling et al. respond. Am J Public Health. 2014;104:e9–10.
Orantes-Navarro CM, Herrera-Valdés R, Almaguer-López M, López-Marín L, Vela-Parada XF, Hernandez-Cuchillas M, et al. Toward a comprehensive hypothesis of chronic interstitial nephritis in agricultural communities. Adv Chronic Kidney Dis. 2017;24:101–6.
Mohamed F, Endre ZH, Pickering JW, Jayamanne S, Palangasinghe C, Shahmy S, et al. Mechanism-specific injury biomarkers predict nephrotoxicity early following glyphosate surfactant herbicide (GPSH) poisoning. Toxicol Lett. 2016;258:1–10.
Wunnapuk K, Gobe G, Endre Z, Peake P, Grice JE, Roberts MS, et al. Use of a glyphosate-based herbicide-induced nephrotoxicity model to investigate a panel of kidney injury biomarkers. Toxicol Lett. 2014;225:192–200.
Uyanikgil Y, Ateş U, Baka M, Biçer S, Oztaş E, Ergen G. Immunohistochemical and histopathological evaluation of 2,4-dichlorophenoxyacetic acid-induced changes in rat kidney cortex. Bull Environ Contam Toxicol. 2009;82:749–55.
Kim S-J, Gil H-W, Yang J-O, Lee E-Y, Hong S-Y. The clinical features of acute kidney injury in patients with acute paraquat intoxication. Nephrol Dial Transplant. 2009;24:1226–32.
Soloukides A, Moutzouris D-A, Kassimatis T, Metaxatos G, Hadjiconstantinou V. A fatal case of paraquat poisoning following minimal dermal exposure. Ren Fail. 2007;29:375–7.
Wesseling C, Hogstedt C, Picado A, Johansson L. Unintentional fatal paraquat poisonings among agricultural workers in Costa Rica: report of 15 cases. Am J Ind Med. 1997;32:433–41.
Kaur B, Khera A, Sandhir R. Attenuation of cellular antioxidant defense mechanisms in kidney of rats intoxicated with carbofuran. J Biochem Mol Toxicol. 2012;26:393–8.
Chargui I, Grissa I, Bensassi F, Hrira MY, Haouem S, Haouas Z, et al. Oxidative stress, biochemical and histopathological alterations in the liver and kidney of female rats exposed to low doses of deltamethrin (DM): a molecular assessment. Biomed Environ Sci. 2012;25:672–83.
Shah MD, Iqbal M. Diazinon-induced oxidative stress and renal dysfunction in rats. Food Chem Toxicol. 2010;48:3345–53.
Tripathi S, Srivastav AK. Nephrotoxicity induced by long-term oral administration of different doses of chlorpyrifos. Toxicol Ind Health. 2010;26:439–47.
Poovala VS, Kanji VK, Tachikawa H, Salahudeen AK. Role of oxidant stress and antioxidant protection in acephate-induced renal tubular cytotoxicity. Toxicol Sci. 1998;46:403–9.
Poovala VS, Huang H, Salahudeen AK. Role of reactive oxygen metabolites in organophosphate-bidrin-induced renal tubular cytotoxicity. J Am Soc Nephrol. 1999;10:1746–52.
Choudhary N, Sharma M, Verma P, Joshi SC. Hepato and nephrotoxicity in rat exposed to endosulfan. J Environ Biol. 2003;24:305–8.
Sonne C, Wolkers H, Leifsson PS, Jenssen BM, Fuglei E, Ahlstrøm O, et al. Organochlorine-induced histopathology in kidney and liver tissue from Arctic fox (Vulpes lagopus). Chemosphere. 2008;71:1214–24.
Sobel ES, Gianini J, Butfiloski EJ, Croker BP, Schiffenbauer J, Roberts SM. Acceleration of autoimmunity by organochlorine pesticides in (NZB x NZW)F1 mice. Environ Health Perspect. 2005;113:323–8.
Mesnage R, Arno M, Costanzo M, Malatesta M, Séralini G-E, Antoniou MN. Transcriptome profile analysis reflects rat liver and kidney damage following chronic ultra-low dose Roundup exposure. Environ Health. 2015;14:70.
Weeraratna C. Fertilizer use in Sri Lanka with special reference to Chronic Kidney Disease of unidentified etiology (CKDu). Symposium on “Chronic Kidney Disease of uncertain origin (CKDu): a scientific basis for future action”, 10 December 2013. Colombo: Galadari Hotel; 2013. http://nas-srilanka.org/wp-content/uploads/2013/01/Weeraratne-edited.pdf. Accessed 16 May 2016.
Orantes Navarro CM, Herrera Valdés R, López MA, Calero DJ, Fuentes de Morales J, Alvarado Ascencio NP, et al. Epidemiological characteristics of chronic kidney disease of non-traditional causes in women of agricultural communities of El Salvador. Clin Nephrol. 2015;83:24–31.
Orantes CM, Herrera R, Almaguer M, Brizuela EG, Núñez L, Alvarado NP, et al. Epidemiology of chronic kidney disease in adults of Salvadoran agricultural communities. MEDICC Rev. 2014;16:23–30.
Laws RL, Brooks DR, Amador JJ, Weiner DE, Kaufman JS, Ramírez-Rubio O, et al. Changes in kidney function among Nicaraguan sugarcane workers. Int J Occup Environ Health. 2015;21:241–50.
Laws RL, Brooks DR, Amador JJ, Weiner DE, Kaufman JS, Ramírez-Rubio O, et al. Biomarkers of kidney injury among Nicaraguan sugarcane workers. Am J Kidney Dis. 2016;67:209–17.
Siddharth M, Datta SK, Bansal S, Mustafa M, Banerjee BD, Kalra OP, et al. Study on organochlorine pesticide levels in chronic kidney disease patients: association with estimated glomerular filtration rate and oxidative stress. J Biochem Mol Toxicol. 2012;26:241–7.
Siddarth M, Datta SK, Mustafa M, Ahmed RS, Banerjee BD, Kalra OP, et al. Increased level of organochlorine pesticides in chronic kidney disease patients of unknown etiology: role of GSTM1/GSTT1 polymorphism. Chemosphere. 2014;96:174–9.
Torres C, Aragón A, González M, López I, Jakobsson K, Elinder C-G, et al. Decreased kidney function of unknown cause in Nicaragua: a community-based survey. Am J Kidney Dis. 2010;55:485–96.
Peraza S, Wesseling C, Aragon A, Leiva R, García-Trabanino RA, Torres C, et al. Decreased kidney function among agricultural workers in El Salvador. Am J Kidney Dis. 2012;59:531–40.
VanDervort DR, López DL, Orantes CM, Rodríguez DS. Spatial distribution of unspecified chronic kidney disease in El Salvador by crop area cultivated and ambient temperature. MEDICC Rev. 2014;16:31–8.
Trabanino RG, Aguilar R, Silva CR, Mercado MO, Merino RL. End-stage renal disease among patients in a referral hospital in El Salvador. Rev. Panam Salud Publica. 2002;12:202–6.
Mejía R, Quinteros E, López A, Ribó A, Cedillos H, Orantes CM, et al. Pesticide-handling practices in agriculture in El Salvador: an example from 42 patient farmers with chronic kidney disease in the Bajo Lempa region. Occ Dis Environ Med. 2014;2:56–70.
Vela XF, Henríquez DO, Zelaya SM, Granados DV, Hernández MX, Orantes CM. Chronic kidney disease and associated risk factors in two Salvadoran farming communities, 2012. MEDICC Rev. 2014;16:55–60.
Payán-Rentería R, Garibay-Chávez G, Rangel-Ascencio R, Preciado-Martínez V, Muñoz-Islas L, Beltrán-Miranda C, et al. Effect of chronic pesticide exposure in farm workers of a Mexico community. Arch Environ Occup Health. 2012;67:22–30.
Rango T, Jeuland M, Manthrithilake H, McCornick P. Nephrotoxic contaminants in drinking water and urine, and chronic kidney disease in rural Sri Lanka. Sci Total Environ. 2015;518–519:574–85.
Rugama E. Risk factors that influence the occurence of chronic renal insufficiency in patients admitted at internal medicine service from hospital Oscar Danilo Rosales Arguello in Leon, January – December 2000. León: Universidad Nacional Autónoma de Nicaragua; 2001.
Gracia-Trabanino R, Domínguez J, Jansà JM, Oliver A. Proteinuria and chronic renal failure in the coast of El Salvador: detection with low cost methods and associated factors. Nefrologia. 2005;25:31–8.
Peiris-John RJ, Wanigasuriya JKP, Wickremasinghe AR, Dissanayake WP, Hittarage A. Exposure to acetylcholinesterase-inhibiting pesticides and chronic renal failure. Ceylon Med J. 2006;51:42–3.
Torres-Lacourt C, Gonzalez M, Vanegas R, Aragon A. Prevalence of chronic kidney insufficiency in the communities of “La Isla” and “Candelaria”, Chichigalpa. León: Universidad Nacional Autónoma de Nicaragua; 2008.
Sanoff SL, Callejas L, Alonso CD, Hu Y, Colindres RE, Chin H, et al. Positive association of renal insufficiency with agriculture employment and unregulated alcohol consumption in Nicaragua. Ren Fail. 2010;32:766–77.
O’Donnell JK, Tobey M, Weiner DE, Stevens LA, Johnson S, Stringham P, et al. Prevalence of and risk factors for chronic kidney disease in rural Nicaragua. Nephrol Dial Transplant. 2011;26:2798–805.
Orantes CM, Herrera R, Almaguer M, Brizuela EG, Hernández CE, Bayarre H, et al. Chronic kidney disease and associated risk factors in the Bajo Lempa region of El Salvador: Nefrolempa study, 2009. MEDICC Rev. 2011;13:14–22.
Wanigasuriya KP, Peiris-John RJ, Wickremasinghe R. Chronic kidney disease of unknown aetiology in Sri Lanka: is cadmium a likely cause? BMC Nephrol. 2011;12:32.
Laux TS, Bert PJ, Barreto Ruiz GM, González M, Unruh M, Aragon A, et al. Nicaragua revisited: evidence of lower prevalence of chronic kidney disease in a high-altitude, coffee-growing village. J Nephrol. 2012;25:533–40.
García-Trabanino R, Jarquín E, Wesseling C, Johnson RJ, González-Quiroz M, Weiss I, et al. Heat stress, dehydration, and kidney function in sugarcane cutters in El Salvador--a cross-shift study of workers at risk of Mesoamerican nephropathy. Environ Res. 2015;142:746–55.
Jayasumana C, Paranagama P, Agampodi S, Wijewardane C, Gunatilake S, Siribaddana S. Drinking well water and occupational exposure to herbicides is associated with chronic kidney disease, in Padavi-Sripura, Sri Lanka. Environ Health. 2015;14:6.
Lebov JF, Engel LS, Richardson D, Hogan SL, Sandler DP, Hoppin JA. Pesticide exposure and end-stage renal disease risk among wives of pesticide applicators in the agricultural health study. Environ Res. 2015;143:198–210.
Lebov JF, Engel LS, Richardson D, Hogan SL, Hoppin JA, Sandler DP. Pesticide use and risk of end-stage renal disease among licensed pesticide applicators in the agricultural health study. Occup Environ Med. 2016;73:3–12.
Aroonvilairat S, Kespichayawattana W, Sornprachum T, Chaisuriya P, Siwadune T, Ratanabanangkoon K. Effect of pesticide exposure on immunological, hematological and biochemical parameters in Thai orchid farmers—a cross-sectional study. Int J Environ Res Public Health. 2015;12:5846–61.
Wesseling C, Aragón A, González M, Weiss I, Glaser J, Rivard C, et al. Heat stress, hydration and uric acid: a cross-sectional study in workers of three occupations in a hotspot of Mesoamerican nephropathy in Nicaragua. BMJ Open. 2016;6:e011034.
Ritter L, Arbuckle TE. Can exposure characterization explain concurrence or discordance between toxicology and epidemiology? Toxicol Sci. 2007;97:241–52.
Jayasumana C, Gunatilake S, Siribaddana S. Simultaneous exposure to multiple heavy metals and glyphosate may contribute to Sri Lankan agricultural nephropathy. BMC Nephrol. 2015;16:103.
Murray D. Cultivating crisis, the human cost of pesticides in Latin America. Austin: University of Texas Press; 1994.
UNEP Chemicals. Regionally Based Assessment of Persistent Toxic Substances: Central America and the Caribbean Regional Report. United Nations Environment Programme; 2002.
Parr SK, Siew ED. Delayed consequences of acute kidney injury. Adv Chronic Kidney Dis. 2016;23:186–94.
CENCAM. Statement of the CENCAM Board and the Scientific Committee of the 2nd International Workshop on Mesoamerican Nephropathy regarding currently known facts about the epidemic. Consortium for the Epidemic of Nephropathy in Central America and Mexico; 2016. http://www.regionalnephropathy.org/wp-content/uploads/2014/07/Board-Statement-MeN-English.pdf. Accessed 16 May 2016.
Cohen J. Mesoamerica’s mystery killer. Science. 2014;344:143–7.
Acknowledgements
The authors thank Dr. Pierre Auger and Dr. Pierre Gosselin, from WHO-PAHO Collaborating Center INSPQ-CHUQ-DSPQ, for their insights. Dr. Ludovic Reveiz from the Pan American Health Organization participated in the conception, design, analysis and interpretation of data for the work and revised critically the content of the draft version, but did not approve the final version of the manuscript.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Authors’ contributions
Conception: AS, MV; study design: MV, AS; literature searches and other data collection: MEL; analysis and interpretation of studies: CW, MV; structure of first manuscript: MEL; writing of manuscript: CW and MV with input of AS and MEL; final approval of manuscript: all authors.
Competing interests
The authors declare that they have no competing interests. Agnes Soares is a staff member of the Pan American Health Organization. The author alone is responsible for the views expressed in this publication, and they do not necessarily represent the decisions or policies of the Pan American Health Organization.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Disclaimer
The author is a staff member of the Pan American Health Organization. The author alone is responsible for the views expressed in this publication, and they do not necessarily represent the decisions or policies of the Pan American Health Organization.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original version of this article was revised to correct copyright information.
An erratum to this article is available at http://dx.doi.org/10.1186/s12940-017-0274-9.
Additional files
Additional file 1:
Key terms used in the search strategy. (DOCX 29 kb)
Additional file 2: Table S1.
Details of studies from Mesoamerica, Sri Lanka and other countries assessing the role of pesticides in chronic kidney disease. (DOCX 75 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution IGO License (http://creativecommons.org/licenses/by/3.0/igo/legalcode), which permits unrestricted, use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. In any reproduction of this article there should not be any suggestion that PAHO or this article endorse any specific organization or products. The use of the PAHO logo is not permitted. This notice should be preserved along with the article's original URL.
About this article
Cite this article
Valcke, M., Levasseur, ME., Soares da Silva, A. et al. Pesticide exposures and chronic kidney disease of unknown etiology: an epidemiologic review. Environ Health 16, 49 (2017). https://doi.org/10.1186/s12940-017-0254-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-017-0254-0