Abstract
Background
Liver disease is an important contributor to the mortality gap between First Nations Peoples and non-Indigenous Australian adults. Despite a high burden of metabolic comorbidities among First Nations Peoples, data about the epidemiology of metabolic dysfunction-associated steatotic liver disease (MASLD) in this population is scarce.
Methods
A retrospective analysis of all adults hospitalized with MASLD or metabolic dysfunction-associated steatohepatitis (MASH) with/without cirrhosis during 2007–2019 in the state of Queensland was performed. Patients were followed from the first admission with MASLD/MASH (identified based on validated algorithms) to decompensated cirrhosis and overall mortality. We explored differences according to Indigenous status using Multivariable Cox regression.
Findings
439 First Nations Peoples and 7,547 non-Indigenous Australians were followed for a median of 4.6 years (interquartile range 2.7–7.2). Overall, women were overrepresented, but more so in the First Nations cohort (72.7% vs. 57.0%, p < 0.001). First Nations patients were younger, a higher proportion lived in remote and socioeconomic disadvantaged areas, and had higher comorbidity compared to non-Indigenous Australians (all p < 0.001). Diabetes, the most common comorbidity affecting both groups, was overrepresented in First Nations Peoples versus non-Indigenous Australians (43.5% vs. 30.8%, p < 0.001, respectively). Nineteen (4.3%) First Nations Peoples and 332 (4.4%) of non-Indigenous patients progressed to cirrhosis decompensation (9.0% [95%CI 4.5–17.7] vs. 7.7% [95%CI 6.6–8.9; p = 0.956] respectively within 10 years). In multivariable analysis, there was no association between Indigenous status and progression to decompensated cirrhosis (p = 0.759) and survival (p = 0.437).
Conclusions
This study provides the first population-based epidemiological data on MASLD in First Nations Australians. The high prevalence of diabetes (that is associated with advanced fibrosis and liver disease mortality) among young First Nations Peoples with MASLD raises concern about future risk of progressive liver disease in this patient population. These data highlight the importance of early identification of MASLD, and providing culturally appropriate intervention to reduce disease progression in parallel with the management of cardiometabolic comorbidities.
Similar content being viewed by others
Background
Liver disease is an important contributor to the mortality gap between Aboriginal and Torres Strait Islander peoples, the First Nations Peoples of Australia, and non-Indigenous Australian adults. Liver cancer is the third most common cancer-related death in First Nations men, and incidence rates are approximately double that of non-Indigenous Australians [1].
In Queensland (2007–2016), the third-most populous Australian state, the rate of cirrhosis hospitalisation was 3.4-times higher for First Nations Peoples compared to non-Indigenous Australians [2]. Moreover, unadjusted survival was poorer for First Nations Peoples hospitalised for cirrhosis [3] and for those diagnosed with hepatocellular carcinoma (HCC) [4], with part of the survival deficit explained by sociodemographic and clinical factors including comorbidity burden.
Alcohol misuse, chronic hepatitis B and C, and metabolic dysfunction-associated steatotic liver disease (MASLD) are important causes of cirrhosis among all Australians [2, 5]. First Nations Peoples experience a disproportionately higher burden of alcohol misuse, and chronic hepatitis B and C infection compared to non-Indigenous Australians [6,7,8]. However, data about the epidemiology of MASLD in First Nations Peoples is scarce. In a population-based linkage study of cirrhosis admissions which included 779 First Nations Peoples, 23 Indigenous patients (3.0%) had MASLD or metabolic dysfunction-associated steatohepatitis (MASH) compared to 5% of non-Indigenous Australians (p = 0.005) [3]. Among all patients with cirrhosis, the prevalence of alcohol-related cirrhosis and hepatitis C virus remained stable during 2007–2016, that of MASLD/MASH increased by 67% (p < 0.001), and the prevalence of diabetes mellitus nearly doubled (from 13.7 to 25.4%; p < 0.001) [5].
Diabetes mellitus is associated with an increased risk of advanced fibrosis, cirrhosis-related complications, and liver disease mortality [9]. Obesity, lipid abnormalities, and hypertension are also important risk factors for severe liver disease [9]. In a population-based linkage study of people hospitalized with MASLD or MASH with or without cirrhosis in the state of Queensland, 37.1% of the patients with MASLD-related cirrhosis and diabetes mellitus progressed to decompensated cirrhosis within a decade [10]. These risk factors, in particular including diabetes and obesity, are overrepresented in First Nations Peoples versus non-Indigenous Australians [6]. The primary aim of this study was to compare the sociodemographic and clinical characteristics (in particular the prevalence of comorbidity) in First Nations Peoples and non-Indigenous Australians with MASLD/MASH admitted to a Queensland hospital during 2009–2018. The secondary aim included exploratory analyses to examine differences in patient outcomes (cumulative incidence of decompensated cirrhosis and overall mortality) according to indigenous status.
Methods
We conducted a population-based retrospective cohort study of people hospitalized with MASLD/MASH with or without cirrhosis in the state of Queensland, Australia. The details of the study have been previously described [10]. Briefly, the primary data source for this study included the Queensland Hospital Admitted Patient Data Collection that comprises information on all hospital episodes of care for patients admitted to Queensland public and private hospitals, and the Death Registry Data. The source population included all adult patients (≥ 20 years) with at least one hospital admission in Queensland during July-2007 to Dec-2019 with a recorded diagnosis of MASLD/MASH. We excluded patients whose age was < 20 years, residential location was unknown, and those who did not reside in Queensland. Following the global expert consensus statement that recommended the use of currently available ICD codes for NAFLD/NASH to define MASLD and MASH [11], a case of MASLD/MASH was defined by at least one hospitalization with any of the following ICD-10-AM codes: NAFLD (K76.0), NASH (K75.8) or other and unspecified cirrhosis of liver (K74.6). As in other NAFLD/MASLD linkage studies [12], patients who ever had other liver diseases recorded in a hospitalization (e.g. alcohol-related liver disease, viral hepatitis, autoimmune liver disease, hemochromatosis, Wilson’s disease), or ICD-10-AM codes associated with alcohol use disorder or somatic consequences of alcohol use were excluded [12].
A case of metabolic dysfunction-associated fatty liver disease (MASLD) or metabolic dysfunction-associated steatohepatitis (MASH) was defined by at least one hospitalization with an ICD-10-AM code for NAFLD (K76.0), NASH (K75.8) or other and unspecified cirrhosis of liver (K74.6). As described by Hagstrom et al. [12] and Petta et al. [13] patients who ever had other liver diseases recorded in a hospitalization were excluded. The complete list of exclusions comprised: alcoholic liver disease, viral hepatitis, autoimmune liver disease, hemochromatosis, Wilson’s disease, Alpha-1-antitrypsin deficiency, Budd-Chiari syndrome, chronic hepatitis, unspecified, secondary/unspecified biliary cirrhosis, or ICD-10-AM codes associated with alcohol use disorder or somatic consequences of alcohol use (e.g. F10 Mental and behavioural disorders due to use of alcohol, K70 Alcoholic liver disease, T51 Toxic effect of alcohol, K86.0 Alcohol-induced chronic pancreatitis) [12]. We selected the first hospital admission with MASLD/MASH during Jul-2009 to Dec-2018 (referred to as index admission), discharged alive and survived for at least 30 days. We excluded patients who had a code for liver decompensation, a history of liver transplant or HCC prior to the index admission. All patients had a minimum look-back period of 2 years and follow-up period of 1 year. As median survival of patients with decompensated cirrhosis is approximately 2 years, a two-year look-back period will likely identify the first admission for decompensation for most cases. The follow up period of 1 year is adequate to capture sufficient outcome events (death, hospital admissions) [14].
Measurements
Sociodemographic data obtained from the Queensland Hospital Admitted Patient Data Collection (QHAPDC) included: age group at admission (e.g. 20–24 years, 25–29 years,… to 75 + years), gender, marital status, country of birth, place of residence, and Indigenous status (patients were coded as First Nations Peoples if identified in at least one of their records within the study period). Area-based measures of remoteness of residence [15] and socioeconomic status [16] were based on place of residence. Comorbidity at the time of hospital admission was measured using the Charlson Comorbidity Index (CCI) [17]. All diseases listed in the CCI as primary or other diagnosis were analysed (excluding liver disease) using validated coding algorithms [18].
The data includes all admitted patient separations from public hospitals and private hospitals in the state of Queensland. When patients were transferred within the same hospital (e.g. from the emergency department to a ward) or to another hospital, we considered these episodes of care as one ‘hospital stay’. Hospital sector for each ‘hospital stay’ was categorized as ‘public hospital only’ or ‘private only or mix’.
Patients were followed from the first hospital admission with MASLD/MASH with or without cirrhosis. The primary outcomes were progression to decompensated cirrhosis identified by the first decompensation event (having an ICD-10-AM code for ascites, hepatic encephalopathy, or oesophageal variceal bleeding) and overall mortality.
Data analysis
All statistical analyses were performed in Stata 18.0 (StataCorp). Descriptive analyses are presented as frequency (percentages, %) or median (interquartile range, IQR) value depending on data distribution. All p-values are 2-sided. The cumulative incidence of decompensated cirrhosis and mortality (death of any cause) were explored using the Kaplan–Meier method (log-rank statistic). For the former, patients were followed from the index admission to date of decompensation event or were censored at date of death (any cause), liver transplant, HCC diagnosis, or 31 December 2019. For the latter, all cases were followed until date of death (of any cause) or were censored at date of liver transplant, HCC diagnosis, or Dec-2019. Multivariable Cox regression analysis was used to assess the differences in cumulative incidence of decompensated cirrhosis and mortality according to selected sociodemographic and clinical characteristics. Hazard ratios (HRs) with associated 95% confidence intervals (CIs) were reported. The final multivariable models were based on the results of the bivariable analysis considering our understanding of the relationships and dependencies among variables as well as their clinical relevance. A Least Absolute Shrinkage and Selection Operators (LASSO) penalised regression cox proportional hazards model was used to identify a parsimonious model including variables that had the strongest association with the outcomes (decompensated cirrhosis and mortality) [19]. Variables included in the models were checked to ensure that they adhered to the assumption of proportional hazards over time (Schoenfeld residuals). The vce(robust) option was used to obtain robust standard errors for the parameter estimates to control for mild violation of underlying assumptions. Multivariable logistic regression analysis with extrahepatic cancers as dependent variable (presence vs. not) was used to examine the difference in prevalence of extrahepatic cancers at index admission according to Indigenous status adjusting for age group.
The study was approved by the Metro South Health Services and QIMR Berghofer Human Research Ethics Committees (HREC/17/QPAH/23; P2209).
Results
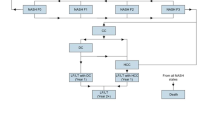
During Jul-2007 and Dec-2019, there were 42,057 hospitalizations with a recorded ICD-10-AM code for NAFLD/NASH. After exclusions described in Fig. 1, a total of 7,986 individual patients were included in the analysis: 439 (5.5%) were identified as First Nations Peoples, and 7,547 (94.5%) as non-Indigenous Australians. The proportion of First Nations Peoples in the study cohort did not vary during Jul-2009 and Dec-2018 (p = 0.31). Patients were followed for a median of 4.6 years (interquartile range (IQR) 2.7–7.2) with no significant difference according to Indigenous status (4.2 years (IQR 2.6–6.8) for First Nations Peoples vs. 4.6 years (IQR 2.7–7.2) for non-Indigenous Australians, p = 0.14).
Flowchart for case ascertainment. Note Metabolic dysfunction-associated steatotic liver disease (MASLD); Metabolic dysfunction-associated steatohepatitis (MASH); International Classification of Diseases 10th edition– Australian Modification (ICD-10‐AM). *Patients may have more than one exclusion criteria
The characteristics of the cohort of patients categorized according to Indigenous status is described in Table 1. Women were overrepresented in both groups, but more so in the First Nations cohort (72.7% vs. 57% of non-Indigenous patients, p < 0.001). About half of the First Nations patients were younger than 50 years (51.5% vs. 33.6% of non-Indigenous patients, p < 0.001) and had no partner (51.3% vs. 39.0%, p < 0.001), and about two-thirds lived outside major city areas (64.0% vs. 39.5%, p < 0.001) and in most disadvantaged areas (66.5% in quintiles Q4 and Q5 vs. 44.1%, p < 0.001). First Nations and non-Indigenous patients were similar with regard to the prevalence of cirrhosis at index admission (13.2% vs. 13.9%, respectively, p = 0.70).
Comorbidities
First Nations Peoples had a significantly higher burden of comorbidity; 51.3% had at least one comorbidity listed in the Charlson index compared to 40.7% for non-Indigenous Australians (p < 0.001), 43.5% had diabetes (vs. 30.8%, p < 0.001), 33.0% had obesity (vs. 27.5%, p = 0.011), and 6.8% had chronic renal disease (vs. 4.2%, p = 0.009). While fewer First Nations Peoples had extrahepatic cancers at index admission (1.8% vs. 4.2%, p = 0.014) vs. non-Indigenous Australians, in multivariable analysis adjusting for age group this difference was not statistically significant (p = 0.114).
Incidence of decompensated cirrhosis
At the end of the follow-up period 19 (4.3%) First Nations Peoples progressed to cirrhosis decompensation compared to 332 (4.4%) of non-Indigenous patients. Among those who progressed to cirrhosis decompensation, the median time from index admission to the first episode of decompensation was 1.4 years for First Nations Peoples (IQR 0.8–3.9) vs. 1.5 years (IQR 0.4–3.3) for non-Indigenous Australians. The average proportion of First Nations Peoples progressing to decompensated cirrhosis was 1.0% per year (95%CI 0.6–1.5), and 9.0% (95%CI 4.5–17.7) had at least one admission with cirrhosis complications within 10 years compared to 1.0% per year (95%CI 0.9–1.1) and 7.7% (95%CI 6.6–8.9), respectively, for non-Indigenous Australians (p = 0.956). See Kaplan Meier curves for the overall cohort (Fig. 2), and according to sex and age group (Supplementary Fig. 1). These similarities were reflected in the unadjusted hazard rates comparing First Nations Peoples with non-Indigenous Australians (HR = 0.99, 95%CI 0.62–1.57). In multivariable analysis, when adjusting for age group only, First Nations Peoples were 34% more likely to progress to decompensated cirrhosis (adj-HR = 1.34, 95%CI 0.84–2.13), but chance could not be ruled out. Adding cirrhosis and portal hypertension (adj-HR = 1.03, 95%CI 0.65–1.63), and comorbidities (diabetes, cancer, and hypertension - adj-HR = 0.91, 95%CI 0.58–1.44), one at a time, did not alter the hazard ratio substantially. In the final adjusted model including all the abovementioned variables, there was no association between Indigenous status and progression to decompensated cirrhosis (adjusted HR = 1.08, 95%CI 0.68–1.71).
Survival
At the end of the follow-up period 35 (8.0%) First Nations Peoples had died compared to 990 (13.1%) of non-Indigenous patients. During the follow-up period, 50 (0.6%) non-Indigenous patients were diagnosed with HCC and eight had a liver transplant (0.1%), and no First Nations Peoples had either HCC or liver transplant.
The probability of 10-year survival for First Nations Peoples was 86.7% (95%CI 80.5–91.1) versus 77.2% (95%CI 75.4–78.9; p = 0.005), as demonstrated in Kaplan Meier curves for the overall cohort (Fig. 3), and according to sex and age group (Supplementary Fig. 2). In univariable analysis, First Nations Peoples were 39% less likely to die within the follow-up period compared to non-Indigenous Australian (HR = 0.61, 95%CI 0.44–0.86; p = 0.005) (Table 2). In multivariable analysis, the disparity in survival according to Indigenous status was mostly explained by differences in age. When adjusting for age group only, the association was no longer significant (adjusted HR = 0.99, 95%CI 0.69–1.49; p = 0.950). Adding the other sociodemographic variables (sex, socioeconomic status and hospital sector - adj-HR = 0.57, 95%CI 0.40–0.80), cirrhosis and portal hypertension (adj-HR = 0.63, 95%CI 0.45–0.88), and comorbidities (diabetes, obesity, major cardiovascular events, renal disease, chronic pulmonary disease, cancer, disorders of lipoprotein metabolism, and mood disorders - adj-HR = 0.61, 95%CI 0.43–0.86), one at a time, did not alter the hazard ratio substantially. In the final adjusted model including all the abovementioned variables, there was no significant difference in survival between First Nations and non-Indigenous patients (adj-HR = 0.87, 95%CI 0.60–1.24, p = 0.437).
Discussion
This study provides the first population-based epidemiological data concerning MASLD/MASH in a large cohort of an indigenous population in a developed country. In comparison to non-Indigenous Australians with MASLD/MASH, the most striking differences were that First Nations Peoples were predominantly female, substantially younger, and had a higher burden of concurrent conditions.
Australia is a highly developed country, and First Nations Peoples, like indigenous populations in comparable countries, are over-represented in low socioeconomic strata and have poorer access to health services [20]. However, comparing our findings with that of indigenous groups in similar countries is not possible, as comparable data about MASLD/NAFLD in these groups are also lacking. Nevertheless, there are reports that the prevalence of clinical findings suggestive of MASLD in many indigenous populations may be similar to the global prevalence (e.g. indigenous Arctic populations [21], Maori and Pacific peoples in New Zealand) [22], and that MASLD-related mortality is comparable to their non-indigenous counterparts (e.g. American Indians and Alaska Natives in the US experienced similar rising trend in NAFLD-related mortality during 1999–2022 compared to white individuals) [23].
In this study, diabetes was the most common comorbidity recorded at admission and was present at a disproportionately higher rate in First Nations Peoples with MASLD/MASH than in non-Indigenous patients. This finding is consistent with previous reports showing a higher burden of disease secondary to diabetes in all Indigenous populations around the globe. Australian First Nations People appear to have the greatest burden of this complication and are 2.9 times more likely to develop diabetes than their non-Indigenous counterparts, and at a significantly premature age of onset [20, 24]. Additionally they tend to have worse glycaemic control and higher rates of diabetes-related complications, contributing to higher rates of potentially preventable hospitalisations [4, 5]. Females are disproportionately affected with a higher prevalence of both impaired glucose tolerance and diabetes than Indigenous Australian males [1]. The reasons driving the prevalence of diabetes in Indigenous Australians are complex. Higher rates of cigarette smoking and obesity in this group certainly contribute, as well as lower socioeconomic status and the social determinants of health [6, 7], factors that also contribute to development of MASLD. There is growing evidence for intrauterine exposures on the later development of chronic diseases, with maternal pre-gestational and gestational diabetes becoming increasingly prevalent among Indigenous women, contributing to the transgenerational nature of metabolic disease [8,9,10].
Despite the significantly higher burden of metabolic comorbidities such as diabetes mellitus, obesity, dyslipidaemia and cardiovascular disease among First Nations Peoples with MASLD/MASH, this patient population appears to have a similar pattern of progression to decompensated cirrhosis when compared to non-Indigenous Australians. Similarly, after adjusting for sociodemographic and clinical factors, mortality did not vary according to Indigenous status. This finding should be interpreted with caution however, as it is likely that the significantly younger age of the First Nations cohort, and the median of 4.6 years of follow-up accruing a relatively small number of study end points affects these results. In fact previous studies of all-cause cirrhosis and hepatocellular carcinoma showed that First Nations Peoples were younger, had higher burden of comorbidities, higher rates of hospitalisation for cirrhosis, and poorer survival compared to non-Indigenous Australians [3, 4]. Moreover, as age is a key marker for duration of metabolic dysfunction and liver disease, and older age is an independent predictor of poorer survival, the significantly younger age of First Nations Peoples may be a key explanation for the findings. While we adjusted for age group in multivariable analysis, the data available for analysis were categorized and since the age cut-offs are arbitrary, incomplete adjustment for age is possible as the variation of a risk within a category may be wide. Importantly, the influence of ancestry and prevalence of genetic variants that may impact on the severity of MASLD has not been examined in First Nations Peoples. Racial disparity in the prevalence of MASLD has been reported, with the highest frequency among Hispanics and Caucasians and the lowest among African Americans [25]. Genetic factors play a role in the pathophysiology of MASLD, and the prevalence of genetic variations is influenced by ethnicity, affecting the susceptibility of different races to MASLD [26]. There is a paucity of genomic data for Aboriginal Australians, however the few genome-wide studies to date suggest there is a genetic predisposition towards obesity and diabetes in this population group, with similar archaic haplotypes being identified in Indigenous Australians as in other currently marginalised Indigenous groups [11, 12]. Over the years, observations have been made regarding the contribution of colonisation on the metabolic health of Indigenous Australians, resulting in a shift away from their traditional diets to more Westernised lifestyles [12,13,14].
Not unexpectedly, the strongest factors associated with progression to decompensated cirrhosis were the presence of portal hypertension and compensated cirrhosis at index admission, and their prevalence was similar according to Indigenous status. Extrahepatic cancer was also independently associated with liver disease progression and mortality, although fewer First Nations Peoples had cancer. Previous studies have reported comparable [27] or slightly higher incidence [28] of cancers and younger age [4, 29] at diagnosis in First Nations Peoples compared to the general Australian population. The fewer number of extrahepatic cancers in First Nations Peoples included in the current study was explained by the younger age of this cohort when compared to non-Indigenous Australians with MASLD/MASH.
As over two-thirds of First Nations Peoples lived outside major city areas and in most disadvantaged areas, this study additionally highlights the importance of primary care management of MASLD in this patient population. Many challenges are faced in chronic disease management in the setting of limited resources and socioeconomic disadvantage that exist in this population. Indeed, lack of access to diagnostic care for First Nations Peoples residing in remote areas in the Northern Territory was associated with a low rate of HCC detection from ultrasound surveillance, with non-surveillance HCC diagnosed at an advanced stage and consequent poor prognosis [30]. The development of Aboriginal Community-Controlled Health Services (ACCHS) as early as 1971 led to the delivery of culturally appropriate, autonomous primary health care services that are governed and delivered by local Aboriginal Australian communities through a First Nations majority elected board of directors [15]. Non-invasive serum-based testing for liver fibrosis (e.g. FIB-4 test) complemented by point-of-care transient elastography, can be performed in remote communities and can accurately screen for advanced fibrosis/cirrhosis in populations at risk of disease, without the need for travel to a metropolitan liver centre [31]. To overcome the geographical barriers to best medical care, coupled with culturally appropriate health care services, First Nations Peoples residing in remote communities would benefit significantly from ready access to non-invasive serum-based testing for liver fibrosis.
There are several well-established evidence-based strategies that enable effective chronic disease management in Indigenous populations. These include a strong chronic disease workforce made up of Indigenous Health Workers (IHWs), who play a crucial role in facilitating culturally safe communication, as well as other chronic disease health professionals such as dedicated care coordinators. This workforce requires regular access to relevant training and upskilling in the management of MASLD and cardiometabolic risk factors. Facilitating equitable access to specialists with expertise in liver disease and metabolic health by incorporating outreach services and telemedicine into primary care is also essential [7, 16]. Beyond the health system, there is a need for interventions centred around addressing the social determinants of health including education, employment and availability of community support services.
This population-based study included all people who had at least one hospital admission with a recorded diagnosis of MASLD/MASH. Conducting this study in the state of Queensland, the third most populous state (20.8% of the Australian population), and the second largest population of First Nations Peoples (29.2% of First Nations Australians), allowed the inclusion of a large number of First Nations Peoples [32]. Variability in data capture in the hospital admissions dataset can potentially lead to misclassification of MASLD/MASH status, cofactors and comorbidities. A previous study has shown that identification of MASLD/MASH through ICD-10-AM codes in Queensland hospitals may underestimate its prevalence [33]. While Hagstrom et al. advocate the identification of metabolic syndrome components (diabetes, obesity, hypertension, or dyslipidemia) at or before a hospital admission with MASLD to improve sensitivity of capturing MASLD-related cirrhosis, the accuracy of ICD-10-AM codes for identification of these are varied (e.g. sensitivity 95.8% for diabetes, 54.7% for obesity) [33]. Importantly, we have no reason to believe that underestimation of MASLD prevalence in the study varied according to Indigenous status. Exclusion of patients with co-existing liver disease, in particular those that are more common in First Nations Peoples (e.g. chronic hepatitis B, alcohol related cirrhosis, alcohol use disorder) [12], together with a high specificity of ICD-10-AM codes for NAFLD/NASH [33] means that misclassification of MASLD/MASH diagnosis among those included is small. Lack of data on fibrosis stage (e.g. fibrosis scores) is an important limitation as liver fibrosis is a strong predictor of a patient’s prognosis [34, 35].
Conclusions
The high prevalence of diabetes and the younger age of First Nations Peoples with MASLD raises concern about future risk of progressive liver disease and highlights the importance of early identification of MASLD. Further studies with larger numbers of First Nations Peoples with MASLD (in particular MASLD without cirrhosis), and with longer follow-up are required to better examine the progression of MASLD to decompensated cirrhosis and mortality in this patient group. Provision of culturally appropriate intervention to reduce disease progression is crucial, in parallel with the management of cardiometabolic comorbidities. Our findings from an indigenous population in a high-income country emphasize the need for further MASLD research in indigenous populations.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- CCI:
-
Charlson Comorbidity Index
- CI:
-
Confidence interval
- HCC:
-
Hepatocellular cancer
- HR:
-
Hazard ratio
- ICD-10-AM:
-
International Classification of Diseases 10th edition– Australian Modification
- IQR:
-
Interquartile range
- LASSO:
-
Least absolute shrinkage and selection operators
- MASLD:
-
Metabolic dysfunction-associated steatotic liver disease
- MASH:
-
Metabolic dysfunction-associated steatohepatitis
- NAFLD:
-
Non-alcoholic fatty liver disease
References
Australian Institute of Health and Welfare (AIHW). Cancer in Australia 2021. Canberra: AIHW; 2021.
Powell EE, Skoien R, Rahman T, et al. Increasing hospitalization rates for cirrhosis: overrepresentation of disadvantaged australians. EClinicalMedicine May-Jun. 2019;11:44–53.
Valery PC, Clark PJ, Pratt G, et al. Hospitalisation for cirrhosis in Australia: disparities in presentation and outcomes for indigenous australians. Int J Equity Health Feb. 2020;17(1):27.
Wigg AJ, Narayana SK, Hartel G, et al. Hepatocellular carcinoma amongst Aboriginal and Torres Strait Islander peoples of Australia. EClinicalMedicine Jun. 2021;36:100919.
Valery PC, McPhail S, Stuart KA, et al. Changing prevalence of aetiological factors and comorbidities among australians hospitalised for cirrhosis. Intern Med J May. 2021;51(5):691–8.
Australian Institute of Health and Welfare (AIHW). Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018. Canberra: AIHW; 2022. Catalogue number BOD 32.
Kirby Institute. National update on HIV, viral hepatitis and sexually transmissible infections in Australia: 2009–2018. Sydney, NSW: The Kirby Institute, University of New South Wales; 2020.
MacLachlan J, Romero N, Purcell I, Cowie B. Viral Hepatitis Mapping Project: Hepatitis B. National Report 2021. Darlinghurst, NSW: Australasian Society for HIV, Viral Hepatitis, and Sexual Health Medicine; 2023.
Jarvis H, Craig D, Barker R, et al. Metabolic risk factors and incident advanced liver disease in non-alcoholic fatty liver disease (NAFLD): a systematic review and meta-analysis of population-based observational studies. PLoS Med Apr. 2020;17(4):e1003100.
O’Beirne J, Skoien R, Leggett BA, et al. Diabetes mellitus and the progression of non-alcoholic fatty liver disease to decompensated cirrhosis: a retrospective cohort study. Med J Aust Oct. 2023;16(8):358–65.
Hagstrom H, Adams LA, Allen AM et al. The future of International classification of diseases coding in steatotic liver disease: an expert panel Delphi consensus statement. Hepatol Commun Feb 1 2024;8(2).
Hagstrom H, Adams LA, Allen AM, et al. Administrative Coding in Electronic Health Care Record-Based Research of NAFLD: an Expert Panel Consensus Statement. Hepatol Jul. 2021;74(1):474–82.
Petta S, Ting J, Saragoni S, et al. Healthcare resource utilization and costs of nonalcoholic steatohepatitis patients with advanced liver disease in Italy. Nutr Metab Cardiovasc Dis Jun. 2020;9(6):1014–22.
D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol Jan. 2006;44(1):217–31.
Australian Institute of Health and Welfare (AIHW). Rural, regional and remote health: A guide to remoteness classifications. Canberra, Australia: AIHW. 2004 https://www.aihw.gov.au/reports/rural-remote-australians/guide-to-remoteness-classifications/summary.
Australian Bureau of Statistics (ABS). Census of Population and Housing: Socio-economic Indexes for Areas (SEIFA), Australia, 2006. Canberra, Australia: ABS. 2008 https://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care Nov. 2005;43(11):1130–9.
Zou H, Hastie T. Regularization and variable selection via the elastic net. J R Stat Soc B Methodol. 2005;67:301–20.
Australian Institute of Health and Welfare (AIHW). Australian facts: Aboriginal and Torres Strait Islander people. Canberra: AIHW; 2015.
Gantzel RH, Villadsen GE, Rex KF, Pedersen ML, Gronbaek H. Signs of non-alcoholic fatty liver disease in indigenous Arctic populations - a systematic review. Dan Med J Apr 19 2023;70(5).
Coppell KJ, Miller JC, Gray AR, Schultz M, Mann JI, Parnell WR. Obesity and the extent of liver damage among adult new zealanders: findings from a national survey. Obes Sci Pract Dec. 2015;1(2):67–77.
Ilyas F, Ali H, Patel P et al. Increasing nonalcoholic fatty liver disease-related mortality rates in the United States from 1999 to 2022. Hepatol Commun Jul 1 2023;7(7).
Australian Institute of Health and Welfare (AIHW). 1.09 Diabetes. AIHW. Available at: https://www.indigenoushpf.gov.au/measures/1-09-diabetes. Accessed 7 Nov 2023.
Rich NE, Oji S, Mufti AR, et al. Racial and ethnic disparities in nonalcoholic fatty liver Disease Prevalence, Severity, and outcomes in the United States: a systematic review and Meta-analysis. Clin Gastroenterol Hepatol Feb. 2018;16(2):198–210. e192.
Samji NS, Snell PD, Singal AK, Satapathy SK. Racial disparities in diagnosis and prognosis of nonalcoholic fatty liver disease. Clin Liver Dis (Hoboken) Aug. 2020;16(2):66–72.
Australian Institute of Health and Welfare (AIHW). Cancer in Aboriginal & Torres Strait Islander people of Australia. AIHW; 2018.
Australian Institute of Health and Welfare (AIHW). Aboriginal and Torres Strait Islander Health Performance Framework: summary report July 2023. Canberra: AIHW; 2023.
Tervonen HE, Morrell S, Roder D, You H, Currow DC. Differences in cancer incidence by age at diagnosis between Aboriginal and non-aboriginal people for cancer types included in Australian national screening programs. Cancer Epidemiol Jun. 2019;60:102–5.
Parker C, Tong SY, Dempsey K, et al. Hepatocellular carcinoma in Australia’s Northern Territory: high incidence and poor outcome. Med J Aust Oct. 2014;20(8):470–4.
Loomba R, Huang DQ, Sanyal AJ, et al. Liver stiffness thresholds to predict disease progression and clinical outcomes in bridging fibrosis and cirrhosis. Gut Mar. 2023;72(3):581–9.
Australian Bureau of Statistics (ABS). Population: Census. Canberra: ABS; 2022.
Hayward KL, Johnson AL, Horsfall LU, Moser C, Valery PC, Powell EE. Detecting non-alcoholic fatty liver disease and risk factors in health databases: accuracy and limitations of the ICD-10-AM. BMJ Open Gastroenterol Feb. 2021;8(1):e000572.
Taylor RS, Taylor RJ, Bayliss S, et al. Association between Fibrosis Stage and outcomes of patients with nonalcoholic fatty liver disease: a systematic review and Meta-analysis. Gastroenterol May. 2020;158(6):1611–e16251612.
Allen AM, Therneau TM, Ahmed OT et al. Clinical course of non-alcoholic fatty liver disease and the implications for clinical trial design. J Hepatol Jul 14 2022.
Acknowledgements
The authors wish to thank the Registries of Births, Deaths and Marriages for enabling the death data to be used for this publication, and the Statistical Analysis and Linkage Unit of the Statistical Services Branch for linking the data sets used in this project.
Funding
This study was supported by the Sunshine Coast University Hospital and Health Service SERTF-Wishlist Collaborative Research Grants 2021.
Author information
Authors and Affiliations
Contributions
PCV and EEP contributed to the conception and design of the study. PCV performed the data analysis and takes responsibility for the integrity and the accuracy of the data. GH provided statistical advice, and directly accessed and verified the reported data. CB, a proud Quandamooka woman from Minjerribah, provided cultural guidance on the manuscript. PV drafted the manuscript. All authors (PCV, SR, CB, JO, GH, BL, RS, and EEP): (i) had full access to all the data in the study and accept responsibility to submit for publication, (ii) contributed to the interpretation of data, revising the draft critically for important intellectual content, and (iii) approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Human Research Ethics Committees of the QIMR Berghofer Medical Research Institute (P3506) and Queensland Health (HREC/17/QPAH/23; HREC/2018/QMS/43571).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests or financial disclosures. The funder had no role in study design, data collection, data analysis, interpretation, or writing of the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Valery, P.C., Roche, S., Brown, C. et al. High prevalence of diabetes among young First Nations Peoples with metabolic dysfunction-associated steatotic liver disease: a population-based study in Australia. Int J Equity Health 23, 84 (2024). https://doi.org/10.1186/s12939-024-02153-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12939-024-02153-z