Abstract
Introduction
Evidence to date indicates that patients from ethnic minority backgrounds may experience disparity in the quality and safety of health care they receive due to a range of socio-cultural factors. Although heightened risk of patient safety events is of key concern, there is a dearth of evidence regarding the nature and rate of patient safety events occurring amongst ethnic minority consumers, which is critical for the development of relevant intervention approaches to enhance the safety of their care.
Objectives
To establish how ethnic minority populations are conceptualised in the international literature, and the implications of this in shaping of our findings; the evidence of patient safety events arising among ethnic minority healthcare consumers internationally; and the individual, service and system factors that contribute to unsafe care.
Method
A systematic review of five databases (MEDLINE, PUBMED, PsycINFO, EMBASE and CINAHL) were undertaken using subject headings (MeSH) and keywords to identify studies relevant to our objectives. Inclusion criteria were applied independently by two researchers. A narrative synthesis was undertaken due to heterogeneity of the study designs of included studies followed by a study appraisal process.
Results
Forty-five studies were included in this review. Findings indicate that: (1) those from ethnic minority backgrounds were conceptualised variably; (2) people from ethnic minority backgrounds had higher rates of hospital acquired infections, complications, adverse drug events and dosing errors when compared to the wider population; and (3) factors including language proficiency, beliefs about illness and treatment, formal and informal interpreter use, consumer engagement, and interactions with health professionals contributed to increased risk of safety events amongst these populations.
Conclusion
Ethnic minority consumers may experience inequity in the safety of care and be at higher risk of patient safety events. Health services and systems must consider the individual, inter- and intra-ethnic variations in the nature of safety events to understand the where and how to invest resource to enhance equity in the safety of care.
Review registration
This systematic review is registered with Research Registry: reviewregistry761.
Similar content being viewed by others
Introduction
A multitude of factors contribute to health inequity amongst ethnic minority populations including limited social support, lower health literacy, lower socio-economic status, greater incidence of ill health and a sense of disempowerment [1,2,3,4]. Access to care and language barriers have been the predominant focus of research, with evidence of failure to provide qualified interpreting services to people with limited English proficiency (LEP) as a key contributor to poor care outcomes [5,6,7,8,9,10,11,12].
Whilst health inequities amongst ethnic minorities internationally are well-established, patients’ ethnicity, language and culture are increasingly recognised as significant predictors of the quality of health care delivery in addition to health outcomes [13,14,15,16]. An emerging body of research indicates that patients from minority groups are at higher risk of patient safety events,which are events that could have or did result in harm to the patient, compared to the mainstream population [17,18,19].
Internationally, there has been significant investment in enhancing patient safety mechanisms across health systems [20] through funded international and national bodies responsible for patient safety in health, including dedicated units within the World Health Organisation (WHO) and organisations such as the Australian Commission on Safety and Quality in Health Care (ACSQHC) in Australia, the National Safety Investigation Branch in the UK and the Agency for Healthcare Research and Quality (AHRQ) in the US. Widespread implementation of clinical governance frameworks by these bodies and human capital and system-level resourcing to improve safety in care such as incident reporting and analysis among others has been notable over the past 30 years [20,21,22,23].
Despite international efforts to enhance patient safety and care quality, there has been limited focus on improving safety for ethnic minority populations, which remains an under-researched area [13, 24]. Patients from ethnic minorities continue to report feeling unsafe when receiving health care, with experiences of discrimination, not having appropriate interpreting services and having inadequate knowledge of healthcare settings [25]. Current policy guidelines in Australia and many countries internationally require use of trained interpreters, yet research to date highlights patients reliance on informal translating mediums to support their healthcare interactions [25]. Lack of sufficient systems support comprising inadequate policies and resource for mandatory use of trained interpreters may lead to poor quality interactions between patients, carers and professionals and exacerbate the risk of safety events [17].
In the context of established disparities in the rate of safety events experienced by ethnic minority and majority populations, the nature and rate of patient safety events and the underpinning factors associated with safe care involving ethnic minorities are not well understood [17]. Systematic reviews of patient safety events for ethnic minorities have been limited to only one type of patient safety event, e.g. medication errors or country [26]. To address the knowledge gap, we conducted a systematic review with the following objectives:1) how ethnic minority populations are conceptualised across the international literature and the implications for this conceptualisation in shaping our findings; 2) to establish the evidence for patient safety events involving ethnic minority healthcare consumers internationally; and 3) the individual, service and system factors that contribute to safety among ethnic minority healthcare consumers.
Methods
The Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement was used to guide the reporting of this systematic review [27].
Inclusion criteria
We included available publications in English that reported original, primary empirical, conceptual or theoretical work published from January 2000 to October 2019. Conceptual, theoretical, quantitative or qualitative studies of any research design were eligible including systematic reviews. Studies had to include a sub- or full sample of ethnic minority patients/consumers or data related to ethnic minority patients/consumers. Ethnic minority patients/consumers were defined broadly to include any group who did not speak one of the national languages of the study country, were born in another country, or those who belonged to an ethnic minority group. Outcomes relating to any patient safety events were included except for the specific exclusion applied below. We defined patient safety event as an event that could have or did result in unnecessary harm to the patient.
Exclusion criteria
Publications were excluded if they were not from countries within the Organisation for Economic Co-operation and Development (OECD). Case reports, letters, editorials, and comments were excluded. Studies discussing the following were also excluded: 1) disparity in clinical outcomes or health outcomes in ethnic minorities; 2) diagnostic disparities in ethnic minorities in mental health settings; 3) disparities in access to health care, health prevention and health promotion activities; 4) disparity in quality of healthcare delivery; and 5) safety issues or incidents relating to multicultural healthcare staff. Though these studies are important in understanding the health disparities between ethnic minorities and the mainstream population, they present their own line of inquiry and were considered too broad for this systematic review.
Study identification
An initial range of text words, synonyms and subject headings for the two concepts of this study, patient safety events and ethnic minority, were compiled using several documents as a guide [18, 28, 29]. A lack of consistent terminology used across studies meant that a broad range MeSH (Medical Subject Headings) terms and text words were needed to cover each concept. For example, the concept of patient safety events can be encompassed by subject headings and text words such as adverse events, medication errors, diagnostic errors, as well as patient safety, among others. The concept of an ethnic minority is encompassed by an even wider range of subject headings and text words including cultural diversity, ethnic groups, minority groups and Non-English Speaking. We searched five databases (MEDLINE, PUBMED, PsycINFO, EMBASE and CINAHL). We also hand searched the reference list of the included studies to ensure that we included all relevant studies.
Study selection and data extraction
The database search was uploaded to Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) with articles available online for initial title and abstract review. Based on the information available in the title and abstract, one reviewer (AC) completed the initial title and abstract review. The inclusion criteria were then independently applied for full text review by two reviewers (AC; RH). Disagreements were resolved by consultation. The following data were extracted from included studies: author, publication year, location & setting, research methodology & sample, population studied, objectives and key findings.
Assessment of study quality
Due to heterogeneity of the study types included, we used a revised version of the Quality Assessment Tool for Studies with Diverse Designs (QATSDD) with 13 items [30]. The revised version was checked for reliability with two reviewers independently scoring the included studies. The Kappa test was used for inter-rater reliability [31]. The score of 0.65 was obtained and is considered substantial for reliability [31, 32].
Narrative data synthesis
We used a narrative synthesis to analyse our findings due to the heterogeneity of the study types, as a pure quantitative or qualitative approach for synthesis was not suitable. In addition, the outcomes discussed in each study were not directly comparable. The data extraction provided us with key findings from each study. A textual approach was used to summarise and synthesise the findings from the included studies against the stated objectives.
Results
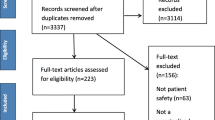
After removing duplicates, 1578 articles were identified. Initial title and abstract screening led to identification of 225 studies. Based on the inclusion and exclusion criteria, two reviewers then reviewed the full text which resulted in 40 studies for inclusion. The reference list searching of the included articles led of inclusion of additional 5 studies. See PRISMA diagram for full search strategy (Fig. 1).
Study characteristics
The included studies represented various countries, health settings and a range of study methods. The studies originated from the United States (US) (25), The Netherlands (5), The United Kingdom (UK) (2), Australia (5), Canada (1), Denmark (1), Switzerland (1), Sweden (1), and Israel (1). Three studies did not specify a geographic setting. A large number of studies were based in hospital settings (26) with others based in the community such as a pharmacy (7), and primary health setting (5). Two studies did not specify a setting. A majority of the included studies used large administrative datasets or retrospective chart review (14) followed by qualitative studies conducting explorative analysis of patient safety events (8) and systematic reviews (8). Summary of the study findings are presented in Table 1.
Study quality
Overall, the included studies varied against the quality assessment criteria. Most studies achieved the total possible score for criteria relating to: statement of aims, objectives or goals; study design being appropriate to address research aims; format of data collection tool to address research aims; method of data analysis; and discussing strengths and limitations. Most studies achieved a nil score against the quality criteria for the involvement of consumers or stakeholders in the research design and conduct. Only two studies described any involvement of consumers or stakeholders in the process of study design and conduct [46, 51]. Our findings highlights lack of reporting of engagement of stakeholders and ethnic minority consumers in research that concerns ethnic minority groups. The included studies provided evidence around the following key areas: I) link between patient safety events and the description of ethnic minorities in the given context; II) the disparity in iatrogenic infections, complications and medicine-related safety events relating to the process of health care; and III) various factors influencing safety events such as communication barriers, cultural factors.
Review Q 1: how ethnic minority populations are conceptualised across the international literature and what are the implications of this conceptualisation in shaping our findings?
Three studies defined or included a definition of ethnic minority [26, 33, 69]. Minority populations were generally conceptualised in the following ways (1): by race, such as African Americans, Caucasians, Asians (2); by language, such as Spanish speaking, Low English Proficiency (LEP); and/or (3) country of origin. Most studies used one or two of the methods to define their ethnic minority populations of study [41, 66, 68]. Large administrative dataset studies largely used race as the key determinant [62, 66]. The methods used reflect the data available in major databases or routinely collected.
Review Q 2: what is the evidence for patient safety events involving ethnic minority healthcare consumers internationally?
The nature and severity of adverse events and disparity in the occurrence of these events was examined in thirteen studies, primary emerging from the US. Differences between ethnic minority patients and others in safety events were predominantly examined using large administrative datasets, retrospective record reviews and systematic reviews focused on rates of (i) hospital acquired infections (HAIs), (ii) complications in care and (iii) adverse drug events (ADEs) [15, 35, 37, 39, 48, 56,57,58,59, 62, 66, 69, 71].
Five retrospective studies using large administrative datasets, three using the Patient Safety Indicators (PSIs) as outcome measures [39, 62, 66] and two using Medication Patient Safety Monitoring System (MPSMS) [15, 57] explored the rate of various HAIs and ADEs among patients from different ethnic backgrounds. These studies reported mixed results highlighting that some ethnic groups were at greater risk of some patient safety events. For example, in a review of administrative data from 16 states in the US, African Americans were reported to have 1.25 to over 1.5 times the rate of infections, postoperative sepsis, decubitus ulcers, postoperative respiratory failure, postoperative pulmonary embolism or deep vein thrombosis (PE/DVT) as Caucasians even when controlling for income level [39]. Findings also revealed that Hispanics had 1.25 to 1.50 times the rate of sepsis and physiologic and metabolic derangements as Caucasians; and Asian/ Pacific Islanders had 1.25 to 1.50 times the rate of sepsis, haemorrhage or hematoma, respiratory failure, and physiologic and metabolic derangement [39]. Further US studies reported disparities in a range of safety indicators for African American and Asian /Pacific Islander peoples [57, 66]. Yet in the Netherlands, a study of 763 Dutch patients and 576 ethnic minority patients revealed no difference in the rate of adverse events between the groups [71]. When compared to the US studies, the authors explained this as being due to the availability of equal access to care through a mandatory insurance scheme for patients [71].
The evidence relating to ADEs among ethnic minorities was mixed and was observed to depend on contextual features such as geographical, genetic and cultural features [35, 57, 59]. Metersky et al. in their retrospective review of 102,623 charts in US hospital settings found that the risk-adjusted odds of African American patients suffering an ADE compared with Caucasian patients was 1.29 (95% CI, 1.19–1.40) [57]. Baehr et al. in their systematic review observed that Asians were more prone to ADEs related to anticoagulants such as bleeding and African American to ADEs relating to diabetes agents such as hypoglycaemia [35]. The term Asian represented combined Asian/Pacific Islander group but authors did not specify any specific ethnic minority group from Asia. Baehr et al. and Okoroh et al. in their systematic reviews also noted increased risk of certain ADEs among certain ethnicities for some drugs and contributed these to genetic predisposition and overuse [35, 59].
Five systematic reviews concerning adverse events in surgical patients and ADEs were also included [35, 37, 56, 58, 59]. In their systematic review and meta-analyses of 26 studies relating to complications and mortality in surgical care, Bloo et al. found that ethnic minorities have a higher risk of complications in perioperative care as compared to the ethnic majority patients resulting in a higher incidence of pain and re-operation [37]. Some included studies in their review discussed the causative factors of the differences in the outcome and ranged from sociocultural, biological and presurgical risk factors but noted that these were mostly speculative highlighting the need for further analyses of the factors at patient, physician and system level [37].
Medicine-related problems were further discussed in eleven included studies [12, 26, 33, 34, 38, 44, 47, 51, 55, 61, 63]. with a range of multifactorial issues identified [12, 33, 47]. Dosing errors were highlighted as the most common error, especially in the context of children receiving the wrong dose by parents from ethnic minorities [47, 51, 55, 63]. Harris et al. in their cross sectional analysis of data from a randomised controlled experiment, identified that greater than 80% of the Hispanic parents made at least one dosing error related to liquid mediation dosage [47]. They observed that the rate of dosing errors was almost double for parents with LEP and low health literacy [47]. In their systematic review based in the UK, Alhomoud et al. demonstrated that most common medicine-related problems among ethnic minority group in the UK were not taking medicines as advised, non-adherence and limited knowledge of illness, its consequences and therapies [26].
Review Q 3: what individual, service and system factors contribute to safety among ethnic minority healthcare consumers?
Several factors contributed to the risk of patient safety events in health care for ethnic minority patients, although their independent and collective contribution was not clear from work to date. Our narrative thematic synthesis identified following factors: 1) language proficiency; 2) errors associated with formal and informal interpretation; 3) misinterpretation of instructions; 4) income and insurance; 5) beliefs about illness and treatment; 6) family and friends for safety vigilance; and 7) patient-professional interactions. We found that often these factors were integrated and not readily distinguished as uniquely individual or service or system level factors. For example, issues around language proficiency were an individual issue in terms of one’s own language proficiency, but it was also about readiness or feasibility of accessing a health system without strong proficiency in a national or native language.
-
a)
Language proficiency
In their prospective incident record review study, Divi et al. identified some degree of detectable physical harm occurred in almost 50% of the LEP identified patients as compared to 30% harm among English speaking patients [41]. They defined LEP status as inability or limited ability to read, write or understand English that impacts on their ability to interact with healthcare professionals [41]. Although communication failure was detected as a factor for more than half of the adverse events occurring in LEP patients, the authors also identified the giving of questionable advice, and incorrect/inadequate interpretation and assessment of the patient by the health professional as possible causes [41]. In a paediatric setting, Cohen et al. found that Spanish speaking families who needed language assistance had a significantly higher risk of experiencing a serious adverse event [40]. But authors also acknowledged that lower socioeconomic status, lower income level and lack of insurance status may impact on their findings [40]. Identifying patients with limited language proficiency is essential to provide relevant interpreting services; however, three studies identified that often there is either an overestimation or incorrect recording of the language data [45, 70, 73]. In one retrospective record review of adverse or sentinel events in the US, the authors identified that medical records data relating to language was only entered correctly 30% of the time [73]. In another record review study conducted in the Netherlands, 30% of patients identified as low Dutch proficient, had no mention of a language barrier or language proficiency documented in their medical record [70].
-
b)
Errors associated with formal and informal interpretation
The review revealed that use of professional interpreting services was free in most developed countries. However, their use by healthcare professionals was limited with many choosing to use ad hoc interpreters, such as carers, family members or people other than the qualified interpreters, or no interpreters [17, 54, 68, 70]. In their qualitative study exploring the role of relatives of ethnic minority patients for patient safety in hospital care, van Rosse et al. noted that use of relatives as interpreters can increase the patient safety risk by inadequately interpreting information to the patient but can also decrease the patient safety risk when the use of interpreter is not feasible [72]. Relying on patient/carer interpretation during the care process is sometimes required and this can reduce reliance on professional services, but is problematic due to the code of confidentiality thus limiting communication [46]. The key risks resulting were poor communication, inadequate patient assessment, poor patient understanding of prescribed treatment and inadequate warning about clinical risks associated with treatment [46, 72, 73]. Two studies examining use of various types of interpreters and their impact on errors of potential clinical consequences were also included [42, 43]. Flores et al. analysed 13 interview transcripts consisting of six trained medical interpreters and seven ad hoc interpreters [42]. They found 396 interpreting errors with an average of 31 errors per encounter. The most common error types were omission, false fluency, substitution, editorialisation and addition [42]. They found that errors with potential clinical consequence to be significantly higher when ad hoc interpreters were used compared to the use of trained medical interpreters (77% vs 53%) [42]. However, this study did not discuss if adverse events occurred. In another cross-sectional study involving two paediatric hospitals, audio taped interpreter encounters (n = 57) revealed that the use of ad hoc or no interpreters was related to double the errors of potential clinical consequence when compared to using trained medical interpreters [43]. They noted that recency of practice was linked with less errors than the years of experience for the trained interpreters [43].
-
c)
Misinterpretation of instructions
Patient safety events resulting from the misinterpretation of medication prescription labels and misunderstanding of discharge instructions were more commonly reported among ethnic minority patients in nine studies [17, 36, 47, 50, 51, 55, 60, 63, 65]. In their mixed-method study involving 308 patients (203 with LEP), Karliner et al. used principle discharge diagnosis, medication outcomes (category, purpose, combined category and purpose) and follow up appointment type as markers for understanding discharge instructions [50]. They observed that patients with LEP had lower odds of understanding medication category (0.63) and combined medication purpose and category after adjusted analysis reflecting some difficulty in understanding discharge instructions [50]. Masland et al. in their analysis of California’s 2007 Health Interview Survey (n = 48,968) found that LEP increased the odds of difficulty in understanding the prescription instructions three times for Central Americans, Mexicans and Koreans and four times for Chinese. They also found that low income (OR1.7), low education (OR1.6) and recent migration (OR1.5) increased the chances of difficulty in understanding prescription [55]. While having a bilingual doctor reduces the odds of difficulty in understanding of prescriptions for Mexicans, Koreans and Vietnamese, it does not for Chinese and Central Americans [55]. The authors explain that high level of linguistic diversity within the Central Americans and Chinese may have impact on truly finding a language concordant bilingual doctor [55]. Two studies also identified that health professionals’ self-identified capacity to provide instructions in patients language can also lead to increased risk of safety events though no quantitative data was available [53, 73].
-
d)
Income and Insurance
Six included studies discussed impact of income or insurance on patient safety with five studies emerging from the US [37, 39, 57, 66, 69, 71]. Coffey et al. and Shen et al. in their review using large administrative dataset and PSI as outcome measures noted that the rate of PSIs for low income group and the patients with Medicaid was higher than for high income group or those with private health insurance [39, 66]. These studies compared the impact of insurance or income independently. Mix results were obtained when they were studied together with ethnic status demonstrating increased risk for African Americans. Shen et al. observed that there was no racial disparities for pressure ulcer among patients with Medicaid, but African Americans with private insurance were more likely than Caucasians to incur pressure ulcer [66]. Coffey et al. studied the impact of income and racial group and noted that African Americans had higher rate for PSIs than Caucasians in all community income groups [39]. Authors noted a range of factors that may contribute to this relationship such as hospital resources [39, 66]. In settings with universal health insurance or access such as The Netherlands, there appeared to be fewer differences in safety events between ethnic minority and other patients but a lack of studies examined the role of income or private health care coverage on safety events outside of US settings [71].
-
e)
Beliefs about illness and treatment
Suurmond et al. and Masland et al. noted that consumers from ethnic minorities have different beliefs about illness and treatment to that of the health professionals depending on their cultural and religious beliefs [17, 55]. Six other studies discussed the differences in the beliefs about illness and treatment and its impact on safety events [12, 26, 33, 38, 52, 55]. These were discussed in the context of medication adherence, compliance to treatment recommendations, but no quantitative data was available to measure the impact on patient safety events. The impacts observed varied and depended on population and setting. A systematic review examining medicine-related problems among ethnic minority population in the UK identified that beliefs about illness and treatment based on religious practices may cause safety events such as not taking medication as prescribed [26]. A qualitative study expanding on this identified that religious practices such as patients fasting for religious purposes alter their medications by changing the time or completely stopping it without consulting their doctor [33]. In their mixed methods before-after study using focus groups and surveys, Cantarero-Arevalo et al. observed that ethnic minority consumers often feel isolated in a new country due to language and cultural differences resulting in mistrust with health professionals and non-compliance with medicine and treatment [38]. Two studies discussed interventions, using bilingual workers from same background to that of the consumers providing culturally appropriate education program to ethnic minorities, to improve medication adherence and improve knowledge of treatment [38, 52]. A pre- and post- intervention survey of the Korean adults (n = 68) receiving education about medication prescriptions by Korean speaking pharmacy students demonstrated the adults significantly increased their understanding of medication directions and had improved trust with pharmacists [52]. Another mixed method study evaluated culturally competent education provided by bilingual fieldworker from the same culture and concluded improved knowledge of medicine-related problems [38]. However, the sample size was small (n = 8) to demonstrate generalisability. Neither of these interventions demonstrated quantitative impact on patient safety events.
-
f)
Family and friends for safety vigilance
Families and friends were identified in having an important role for safety vigilance of their loved ones in two studies. Van Rosse et al. observed that patients from ethnic minorities were more often accompanied by families or friends compared to Dutch born patients during hospitalisation and voiced concerns to the health professionals which enhanced their safety [71]. Another qualitative study of 80 semi structured interviews with consumers from South Asian or Middle Eastern backgrounds in the UK reported that participant often stopped their medications on advice of family or friends, consumed non-prescription medication on advice of family or friends, and also shared their medicines with family members resulting in double dosing for some [33]. van Ross et al. in their study conclude that patient safety can be enhanced by optimising collaboration with the family and friends who are willing to take part in the care process [71]. Goenka, in her literature review, provided one such example of collaboration – Family centred round (FCR) - in a hospital setting to improve collaboration with families of LEP patients [45]. However, they did not evaluate the effectiveness of the program on patient safety.
-
g)
Patient-professional interactions
Ethnic minority patients’ interactions with health professionals and systems were discussed in seven studies with focus on bias and lack of communication resulting in inappropriate care with potential for a patient safety event [12, 17, 26, 33, 36, 63, 64]. Health professional’s presumption about the desire of ethnic minority consumers to engage in their care or their level of understanding may result in unsafe care. In their prospective observational study of 210 paediatric emergency department discharges, Samuels-Kalow et al. observed that when health professionals were providing information regarding pain killers (acetaminophen) to patients, they gave different information to English speaking and Spanish speaking parents [63]. In their systematic review of medicine-related problems in ethnic minority patients in the UK, Alhomoud et al. noted an underestimation of patients desire for information and engagement in decision making by health professionals [26]. In a mixed method study using interviews with consumers from four different ethnicities (n = 18), authors noted that the lack of communication between various departments within a hospital as well as with community practitioners such as general practitioners can impact on care such as ceasing a patient’s medicines prescribed by a GP during hospitalisation [36]. This frequent change applies to all populations but potentially this is a greater threat to patients from ethnic minorities due to various other compounding factors, such as greater investment of time required to build relationships and engagement with ethnic minority consumers [25].
Discussion
Our review findings provide substantial evidence to suggest that people from ethnic minorities are vulnerable to a higher rate of patient safety events in the hospital and community setting compared to the mainstream population. Specifically, included studies showed that ethnic minorities experienced higher incidences of healthcare associated infections, dosing errors, ADEs and complications resulting from their care [35, 37, 39, 57, 66]. Ethnic minority populations being more likely to experience unsafe health care may compound or contribute to already existing inequities in health outcomes. Importantly, this review also highlights the limited socio-cultural data available in health systems internationally and the implications of this for establishing healthcare inequalities.
Factors contributing to the increased threat to ethnic minority populations include socioeconomic factors such as income, insurance and education; language proficiency; health literacy; length of stay in the host country; feeling of alienation and distrust for the health professional, services and systems; and, engagement [38, 39, 41, 55, 64, 66]. Included studies mostly studied these factors independently of each other with little discussion of any relationship between them. In the limited evidence available of this relationship, it was apparent that LEP and health literacy had implications for understanding prescriptions for medication [55]. Health literacy has been explored extensively in relation to poor health outcomes for ethnic minority patients, but there is limited evidence regarding its role in, and interactions with, factors linked to patient safety events [74]. A conceptual model (Fig. 2) has emerged from our review that identifies the major factors that heighten the vulnerability of ethnic minority patients to patient safety events. Further knowledge regarding the cumulative impact of these factors on patient safety events is required as well as better understanding of their relationship with each other and the level of impact each factor may have on potential patient safety events.
Health systems change towards providing culturally competent care by hiring more interpreters or using bilingual health professionals were commonly cited in the reviewed articles [51, 55, 64]. Yet studies to date have mainly explored organisational and staff cultural competence in the context of improving access to care and communication rather than preventing unsafe care specifically [75, 76]. The role of bilingual healthcare staff in positively addressing language and culture was identified in a number of studies [51, 58, 64]. Bilingual staff may improve communication and are highly valued by organisations and patients alike as they speak the patients’ language and understand their culture context [25, 77]. The evidence from the present review suggests that use of interpretation through a range of means is valuable in addressing some patient safety issues but may also leads to others.
Mobile technologies that can translate for interpretation are recognised as a potential solution to overcome language barriers; research indicates ethnic minority consumers use this technology [25]. Google Translate, a web-based tool, is available but low translation accuracy of medical terminologies has the potential for distress and harm [78]. Current applications such as CALD- Assist (an Australian application) that uses pre-recorded text words and phrases along with pictures and videos for allied health and nursing staff to facilitate communication when interpreters are not available or not practical [79] notwithstanding the applications have shown improved satisfaction for communication between consumers and health professionals. More research is needed to understand the patient safety implications of them.
The importance of the active participation and engagement of healthcare consumers both in care and study design is recognised through this review as contributing to safety outcomes and research quality. The relationship between consumer involvement in healthcare and enhanced health outcomes including patient safety is well-established and reinforced through this review [80]. The Australian Commission of Safety and Quality in Health Care (ACSQHC) identifies consumer engagement strategies as central to improved health and healthcare safety outcomes for consumers [21, 81]. Recent studies has also highlighted the role of patient and carer engagement among ethnic minority populations as critical for enhanced healthcare [25, 77]. Consumers can act as safety buffer by identifying when the care is not adequate or unsafe [82]. Included studies in the present review reflect this demonstrating that family members and carers can contribute to safety by voicing their concerns to health professionals and advocating for the patient [71].
Implications
Policy organisations focused to improve health care quality internationally identify ethnic minorities as a priority group but specific guidance about reducing patient safety events is limited [83, 84]. Key implications from this review relate to the vital role of family and carers in supporting safe care. Despite recognition of the need for enhanced consumer engagement among ethnic minority consumers, few service and system level support structures exist to support engagement with patients or their family members [14, 26]. Strategies utilised by the wider patient population, such as checklists or consumer toolkits designed to assist in asking health professionals questions and raising concerns during their care, are under-utilised in ethnic minority populations [81]. Engagement strategies that take into account the nuance differences between ethnic minority consumers are lacking and involving ethnic minority consumers can help develop relevant engagement strategies [25]. Co-design approaches to adapt and develop suitable engagement strategies may be of value to address this gap. A key consideration is how to ensure that approaches to enhance family and carer engagement are explored.
We also found deficiencies in routinely collected healthcare data. Our synthesis of the included studies showed insufficient data regarding factors, that collectively create an individual’s ethnic profile, with most data sets relying on information about country of birth, language spoken and in some instances race to classify ethnic minority individuals. Classifications such as ‘Asian’ or ‘Caucasian’ can be deemed to be homogenous and fails to capture the range of different ethnic minorities included under either of the terms [85]. Given the evidence of multiple patient safety threats for ethnic minority groups, establishing an individual’s ethnic profile in greater detail is essential so as to fully understand if particular patient safety issues are in play and to develop focused interventions.
Several authors commented on the superficial identification of ethnic minority patients and recommended systems be strengthened to allow complete identification of ethnic minorities [45, 70]. There is a need to register more specific socio-cultural data. It is recognised that nuanced differences exist between various ethnic minority groups [86] and collection of superficial indicators to identify ethnic minority population may not provide a full picture of cultural and social factors shaping practices and understanding of health of a particular ethnic minority group. The Australian Bureau of Statistics (ABS) recommends that diverse variables be used to identify consumers from different ethnic minorities [87]. Health services often only collect data relating to language, country and interpreter use [87, 88]. In the US context, Wilson-Stronks et al. recommended level of health literacy, cultural needs, dietary needs and socioeconomic variables be collected along with language and religion [85]. Similarly, Lopez et al. recommended an automated standard system -designed in consultation with ethnic minority consumers - for collecting data concerning ethnic minority and language proficiency [89]. They saw this as a way to reduce the disparity in quality and safety of health care [89].
Limitations
This review has some limitations. The diversity of the definitions used to determine the ethnic minority population shaped the findings. For example, in United States, ethnic minorities were primarily defined based on the race or the first language, with many studies focused to differentials between African Americans, Hispanic and Caucasian populations [57, 66]. This differentiation resulted in most studies from the US using large data to examine the impact of insurance or income to the disparity in safety events [39, 66]. This also led to focus on language, especially in context of Hispanic population, as a factor for the disparity [40]. In addition, use of terms such as ‘Asian’ appeared to refer to two different population groups; in US and Australia this primarily referred to people from China or far eastern Asian countries, but in the UK this was often used in the context of people from India/Pakistan [90]. We limited our search to Organisation for Economic Co-operation and Development (OECD) countries as the ethnic minority groups are considered more comparable and thus our findings are not generalisable beyond the OECD countries. The review sought only published works which may have led to the omission of other relevant works that were not published. Grey literature including government reports were not included and this may have led to the omission of relevant information. The inclusion of five databases along with the reference lists of included articles provided a broad and varied range of data sources to identify relevant literature. Publication bias may also had impact on included studies with non-published negative findings omitted [91].
Conclusion
Our findings indicate substantial disparity in safety events occurring between ethnic minority and mainstream populations. The nature of patient safety events to which ethnic minority populations are exposed to is dependent on the setting and minority population. Patient safety appears to be linked with the availability and use of interpreters, degree of engagement with family and carers, and the availability of systemic processes to overcome language and socio-economic barriers. Enhanced socio-cultural data across health systems is critical. Knowledge of the factors that contribute and compound to create safety for ethnic minority groups, and of the individual differences between various ethnic minority groups in terms of their healthcare safety is limited. Engaging ethnic minority consumers in the design of interventions to enhance safety is key.
Abbreviations
- ABS:
-
Australian Bureau of Statistics
- ACSQHC:
-
Australian Commission of Safety and Quality in Health Care
- ADE:
-
Adverse drug events
- CALD:
-
Culturally and linguistically diverse
- FCR:
-
Family centred round
- LEP:
-
Low English proficiency
- MPSMS:
-
Medication Patient Safety Monitoring System
- OECD:
-
Organisation for Economic Co-operation and Development
- PSI:
-
Patient Safety Incident
- UK:
-
United Kingdom
- US:
-
United States
References
Sze M, Butow P, Bell M, Vaccaro L, Dong S, Eisenbruch M, et al. Migrant health in cancer: outcome disparities and the determinant role of migrant-specific variables. Oncologist. 2015;20(5):523–31.
Bach PB. Unequal treatment: Confronting racial and ethnic disparities in health care. New England J Med. 2003;349(13):1296.
Manna DR, Bruijnzeels MA, Mokkink HG, Berg M. Ethnic specific recommendations in clinical practice guidelines: a first exploratory comparison between guidelines from the USA, Canada, the UK, and the Netherlands. Quality Safety Health Care. 2003;12(5):353–8..
Harun A, Harrison JD, Young JM. Interventions to improve patient participation in the treatment process for culturally and linguistically diverse people with cancer: a systematic review. Asia-Pacific J Clin Oncol. 2013;9(2):99–109.
Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255–99.
Alegria M, Nakash O, NeMoyer A. Increasing equity in access to mental health care: a critical first step in improving service quality. World Psychiatry. 2018;17(1):43–4.
Sentell T, Shumway M, Snowden L. Access to Mental Health Treatment by English Language Proficiency and Race/Ethnicity. J Gen Intern Med. 2007;22(Supplement 2):289–93.
Diamond L, Izquierdo K, Canfield D, Matsoukas K, Gany F. A systematic review of the impact of Patient-physician non-English language concordance on quality of care and outcomes. J Gen Intern Med. 2019;34(8):1591–606.
Shi L, Lebrun LA, Tsai J. The influence of English proficiency on access to care. Ethnicity Health. 2009;14(6):625–42.
Shepherd SM, Willis-Esqueda C, Paradies Y, Sivasubramaniam D, Sherwood J, Brockie T. Racial and cultural minority experiences and perceptions of health care provision in a mid-western region. Int J Equity Health. 2018;17(1):33.
Riley WJ. Health disparities: gaps in access, quality and affordability of medical care. Trans Am Clin Climatol Assoc. 2012;123:167–72 discussion 72-4.
White L, Klinner C. Medicine use of elderly Chinese and Vietnamese immigrants and attitudes to home medicines review. Aust J Primary Health. 2012;18(1):50–5.
Johnstone MJ, Kanitsaki O. Culture, language, and patient safety: making the link. Int J Qual Health Care. 2006;18(5):383–8.
Johnstone MJ, Kanitsaki O. Engaging patients as safety partners: some considerations for ensuring a culturally and linguistically appropriate approach. Health Policy (Amsterdam, Netherlands). 2009;90(1):1–7.
Bakullari A, Metersky ML, Wang Y, Eldridge N, Eckenrode S, Pandolfi MM, et al. Racial and ethnic disparities in healthcare-associated infections in the United States, 2009-2011. Infect Control Hosp Epidemiol. 2014;35(Suppl 3):S10–6.
Belihu FB, Davey MA, Small R. Perinatal health outcomes of east African immigrant populations in Victoria, Australia: a population based study. BMC Pregnancy Childbirth. 2016;16:86.
Suurmond J, Uiters E, de Bruijne MC, Stronks K, Essink-Bot ML. Explaining ethnic disparities in patient safety: a qualitative analysis. Am J Public Health. 2010;100(Suppl 1):S113–7.
Runciman W, Hibbert P, Thomson R, Van Der Schaaf T, Sherman H, Lewalle P. Towards an international classification for Patient safety: key concepts and terms. Int J Qual Health Care. 2009;21(1):18–26.
World Alliance for Patient Safety. WHO Draft Guidelines for Adverse Event Reporting and Learning Systems. Geneva: World Health Organisation; 2005.
World Health Organization. Patinet Safety: Policies and Strategies WHO; 2020 [Available from: https://www.who.int/patientsafety/policies/en/.
Australian Commission on Safety and Quality in Health Care. The NSQHS Standards.: Australian Commission on Safety and Quality in Health Care (ACSQHC); 2019.
Agency for Healthcare Research and Quality. About AHRQ's Quality & Patient Safety Work: AHRQ; 2019 [Available from: https://www.ahrq.gov/patient-safety/about/index.html.
Health Safety Investigatoin Branch. Healthcare Safety Investigation Branch: HSIB; 2020 [Available from: https://www.hsib.org.uk/.
Federation of Ethnic Communities' Council of Australia. Review of Australian Research on Older People from Culturally and Linguistically Diverse Backgrounds. FECCA; 2015.
Harrison R, Walton M, Chitkara U, Manias E, Chauhan A, Latanik M, et al. Beyond translation: engaging with culturally and linguistically diverse consumers. Health Expectations. 2020;23(1):159–68.
Alhomoud F, Dhillon S, Aslanpour Z, Smith F. Medicine use and medicine-related problems experienced by ethnic minority patients in the United Kingdom: a review. Int J Pharm Pract. 2013;21(5):277–87.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9 w64.
Queensland Government. Working with people from culturally and linguistically diverse backgrounds. 2010.
World Health Organization. World Alliance for Patient Safety. Conceptual framework for the international classification for patient safety version 1.1: final technical report January 2009. Available from https://www.who.int/patientsafety/taxonomy/icps_full_report.pdf.
Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract. 2012;18(4):746–52.
Gisev N, Bell JS, Chen TF. Interrater agreement and interrater reliability: key concepts, approaches, and applications. Res Soc Administrative Pharmacy. 2013;9(3):330–8.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276–82.
Alhomoud F, Dhillon S, Aslanpour Z, Smith F. South Asian and middle eastern patients' perspectives on medicine-related problems in the United Kingdom. Int J Clin Pharm. 2015;37(4):607–15.
Ajdukovic M, Crook M, Angley C, Stupans I, Soulsby N, Doecke C, et al. Pharmacist elicited medication histories in the emergency department: identifying patient groups at risk of medication misadventure. Pharm Practice. 2007;5(4):162–8.
Baehr A, Pena JC, Hu DJ. Racial and ethnic disparities in adverse drug events: a systematic review of the literature. J Racial Ethn Health Disparities. 2015;2(4):527–36.
Blennerhassett J, Hilbers J. Medicine Management in Older People from non-English speaking backgrounds. J Pharm Pract Res. 2011;41(1):33–6.
Bloo GJ, Hesselink GJ, Oron A, Emond EJ, Damen J, Dekkers WJ, et al. Meta-analysis of operative mortality and complications in patients from minority ethnic groups. Br J Surg. 2014;101(11):1341–9.
Cantarero-Arevalo L, Kassem D, Traulsen JM. A culturally competent education program to increase understanding about medicines among ethnic minorities. Int J Clin Pharm. 2014;36(5):922–32.
Coffey MR, Andrews MR, Moy ME. Racial, Ethnic, and Socioeconomic Disparities in Estimates of AHRQ Patient Safety Indicators. Medical care. 2005;43(3):I-48–57.
Cohen AL, Rivara F, Marcuse EK, McPhillips H, Davis R. Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics. 2005;116(3):575–9.
Divi C, Koss RG, Schmaltz SP, Loeb JM. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007;19(2):60–7..
Flores G, Laws MB, Mayo SJ, Zuckerman B, Abreu M, Medina L, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111(1):6–14.
Flores G, Abreu M, Barone CP, Bachur R, Lin H. Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Ann Emerg Med. 2012;60(5):545–53.
Fejzic JB, Tett SE. Medication management reviews for people from the former Yugoslavia now resident in Australia. Pharm World Sci. 2004;26(5):271–6.
Goenka PK. Lost in translation: impact of language barriers on children's healthcare. Curr Opin Pediatr. 2016;28(5):659–66.
Hadziabdic E, Heikkila K, Albin B, Hjelm K. Problems and consequences in the use of professional interpreters: qualitative analysis of incidents from primary healthcare. Nurs Inq. 2011;18(3):253–61.
Harris LM, Dreyer BP, Mendelsohn AL, Bailey SC, Sanders LM, Wolf MS, et al. Liquid medication dosing errors by Hispanic parents: role of health literacy and English proficiency. Acad Pediatr. 2017;17(4):403–10.
Hernandez-Suarez DF, Ranka S, Villablanca P, Yordan-Lopez N, González-Sepúlveda L, Wiley J, et al. Racial/ethnic disparities in patients undergoing Transcatheter aortic valve replacement: insights from the healthcare cost and utilization Project's National Inpatient Sample. Cardiovascular Revascularization Medicine. 2019;20(7):546–52.
Inagaki E, Farber A, Kalish J, et al. Role of language discordance in complication and readmission rate after infrainguinal bypass. J Vasc Surg. 2017;66(5):1473–8. https://doi.org/10.1016/j.jvs.2017.03.453.
Karliner SL, Auerbach JA, Nápoles JA, Schillinger JD, Nickleach JD, Pérez-Stable JE. Language barriers and understanding of hospital discharge instructions. Med Care. 2012;50(4):283–9.
Koster ES, Blom L, Winters NA, van Hulten RP, Bouvy ML. Interpretation of drug label instructions: a study among four immigrants groups in the Netherlands. Int J Clin Pharm. 2014;36(2):274–81.
Lee EJ, Riley AC. Understanding of medication directions: assessment of native Korean older adults. Consult Pharm. 2015;30(11):671–7 quiz 6-7.
Lion KC, Rafton SA, Shafii J, Brownstein D, Michel E, Tolman M, et al. Association between language, serious adverse events, and length of stay among hospitalized children. Hospital Pediatrics. 2013;3(3):219–25.
Lopez L, Rodriguez F, Huerta D, Soukup J, Hicks L. Use of interpreters by physicians for hospitalized limited English proficient patients and its impact on patient outcomes. J Gen Intern Med. 2015;30(6):783–9.
Masland MC, Kang SH, Ma Y. Association between limited English proficiency and understanding prescription labels among five ethnic groups in California. Ethnicity Health. 2011;16(2):125–44.
McDowell SE, Coleman JJ, Ferner RE. Systematic review and meta-analysis of ethnic differences in risks of adverse reactions to drugs used in cardiovascular medicine. BMJ (Clinical research ed). 2006;332(7551):1177–81.
Metersky LM, Hunt RD, Kliman HR, Wang HY, Curry HM, Verzier HN, et al. Racial disparities in the frequency of Patient safety events: results from the National Medicare Patient Safety Monitoring System. Med Care. 2011;49(5):504–10.
Nwachukwu BU, Kenny AD, Losina E, Chibnik LB, Katz JN. Complications for racial and ethnic minority groups after total hip and knee replacement: a review of the literature. J Bone Joint Surg. 2010;92(2):338–45.
Okoroh JS, Uribe EF, Weingart S. Racial and ethnic disparities in Patient safety. J Patient Safety. 2017;13(3):153–61.
Patel VL, Branch T, Arocha JF. Errors in interpreting quantities as procedures: the case of pharmaceutical labels. Int J Med Inform. 2002;65(3):193.
Raynor EM. Factors affecting Care in non-English-Speaking Patients and Families. Clin Pediatr. 2016;55(2):145–9.
Romano PS, Geppert JJ, Davies S, Miller MR, Elixhauser A, McDonald KM. A national profile of patient safety in U.S. hospitals. Health Affairs (Project Hope). 2003;22(2):154.
Samuels-Kalow ME, Stack AM, Porter SC. Parental language and dosing errors after discharge from the pediatric emergency department. Pediatr Emerg Care. 2013;29(9):982–7.
Schwappach D, Meyer Massetti C, Gehring K. Communication barriers in counselling foreign-language patients in public pharmacies: threats to patient safety? Int J Clin Pharmacy Pharmaceutical Care. 2012;34(5):765–72.
Shadmi E. Quality of hospital to community care transitions: the experience of minority patients. Int J Qual Health Care. 2013;25(3):255–60.
Shen JJ, Cochran CR, Mazurenko O, Moseley CB, Shan G, Mukalian R, et al. Racial and insurance status disparities in Patient safety indicators among hospitalized patients. Ethnicity & Disease. 2016;26(3):443.
Stockwell DC, Landrigan CP, Toomey SL, Westfall MY, Liu S, Parry G, et al. Racial, ethnic, and socioeconomic disparities in Patient safety events for hospitalized children. Hosp Pediatr. 2019;9(1):1–5.
Thomas PE, Beckmann M, Gibbons K. The effect of cultural and linguistic diversity on pregnancy outcome. Aust N Z J Obstet Gynaecol. 2010;50(5):419–22.
Timmins CL. The impact of language barriers on the health care of latinos in the United States: a review of the literature and guidelines for practice. J Midwif Women's Health. 2002;47(2):80–96.
van Rosse F, de Bruijne M, Suurmond J, Essink-Bot ML, Wagner C. Language barriers and patient safety risks in hospital care. A mixed methods study. Int J Nurs Stud. 2016;54:45–53.
van Rosse F, Essink-Bot ML, Stronks K, de Bruijne M, Wagner C. Ethnic minority patients not at increased risk of adverse events during hospitalisation in urban hospitals in the Netherlands: results of a prospective observational study. BMJ Open. 2014;4(12):e005527.
van Rosse F, Suurmond J, Wagner C, de Bruijne M, Essink-Bot ML. Role of relatives of ethnic minority patients in patient safety in hospital care: a qualitative study. BMJ Open. 2016;6(4):e009052.
Wasserman M, Renfrew MR, Green AR, Lopez L, Tan-McGrory A, Brach C, et al. Identifying and preventing medical errors in patients with limited English proficiency: key findings and tools for the field. J Healthc Qual. 2014;36(3):5–16.
Sentell T, Braun KL. Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. J Health Commun. 2012;17(Suppl 3):82–99.
Karmali K, Grobovsky L, Levy J, Keatings M. Enhancing cultural competence for improved access to quality care. Healthcare Quarterly. 2011;14 Spec No 3:52–57.
Zeh P, Cannaby AM, Sandhu HK, Warwick J, Sturt JA. A cross-sectional survey of general practice health workers' perceptions of their provision of culturally competent services to ethnic minority people with diabetes. Primary Care Diabetes. 2018;12(6):501–9.
Harrison R, Walton M, Chauhan A, Manias E, Chitkara U, Latanik M, et al. What is the role of cultural competence in ethnic minority consumer engagement? An analysis in community healthcare. Int J Equity Health. 2019;18(1):191.
Freyne J, Bradford D, Pocock C, Silvera-Tawil D, Harrap K, Brinkmann S. Developing Digital Facilitation of Assessments in the Absence of an Interpreter: Participatory Design and Feasibility Evaluation With Allied Health Groups. JMIR Form Res. 2018;2(1):e1 e.
Silvera-Tawil D, Pocock C, Bradford D, Donnell A, Harrap K, Freyne J, et al. CALD assist-nursing: improving communication in the absence of interpreters. J Clin Nurs. 2018;27(21–22):4168–78.
Abid MH, Abid MM, Surani S, Ratnani I. Patient Engagement and Patient Safety: Are We Missing the Patient in the Center? Cureus. 2020;12(2):e7048 e.
Australian Commission on Safety and Quality in Health Care. Top Tips for Safe Health Care.: Australian Commission on Safety and Quality in Health Care (ACSQHC); 2017.
Davis RE, Jacklin R, Sevdalis N, Vincent CA. Patient involvement in patient safety: what factors influence patient participation and engagement? Health Expect. 2007;10(3):259–67.
Australian Commission on Safety and Quality in Health Care. The state of patient safety and quality in Australian hospitals 2019.: Australian Commission on Safety and Quality in Health Care (ACSQHC); 2019.
Agency for Healthcare Research and Quality. About AHRQ's Quality & Patient Safety Work.: Agency for Healthcare Research and Quality (AHRQ); 2019.
Wilson-Stronks A, Lee K, Cordero C, Kopp A, Galvez E. One Size Does Not Fit All: Meeting the Health Care Needs of Diverse Populations. Oakbrook Terrace, IL: The Joint Commission; 2008.
Dawson S, Campbell SM, Giles SJ, Morris RL, Cheraghi-Sohi S. Black and minority ethnic group involvement in health and social care research: a systematic review. Health Expect. 2018;21(1):3–22.
Australian Bureau of Statistics. Standards for Statistics on Cultural and Language Diversity. Canberra: Australian Bureau of Statistics; 1999.
Forrest S. Review of Cultural and Linguistic Diversity (CaLD) Data Collection Practices in the WA Health System 2018. Western Australia: Department of Health; 2018.
Lopez L, Green AR, Tan-McGrory A, King R, Betancourt JR. Bridging the digital divide in health care: the role of health information technology in addressing racial and ethnic disparities. Joint Commission J Qual Patient Safety. 2011;37(10):437–45.
Bhopal R. Glossary of terms relating to ethnicity and race: for reflection and debate. J Epidemiol Community Health. 2004;58(6):441–5.
Betrán AP, Say L, Gülmezoglu AM, Allen T, Hampson L. Effectiveness of different databases in identifying studies for systematic reviews: experience from the WHO systematic review of maternal morbidity and mortality. BMC Med Res Methodol. 2005;5(1):6.
Acknowledgements
Not applicable
Funding
This project is funded by NHMRC project grant 1049703 administered by the University of Sydney.
Author information
Authors and Affiliations
Contributions
AC and RH conceptualised the study. SM completed the database search. AC and RH completed the screening of the articles. AC completed writing the manuscript. RH, MW, EM. HS, RLW, DL, ML and SM provided feedback during analysis and reporting of the findings. All authors reviewed and agreed on the final version for submission. This review is also part of the AC’s doctoral thesis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Data available on request from the authors.
Competing interests
Authors declare no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Supplementary file 1
for search strategy.
Additional file 2: Supplementary file 2
for quality assessment criteria.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chauhan, A., Walton, M., Manias, E. et al. The safety of health care for ethnic minority patients: a systematic review. Int J Equity Health 19, 118 (2020). https://doi.org/10.1186/s12939-020-01223-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12939-020-01223-2