Abstract
Background
In-hospital cardiac arrest (IHCA) is an acute disease with a high fatality rate that burdens individuals, society, and the economy. This study aimed to develop a machine learning (ML) model using routine laboratory parameters to predict the risk of IHCA in rescue-treated patients.
Methods
This retrospective cohort study examined all rescue-treated patients hospitalized at the First Medical Center of the PLA General Hospital in Beijing, China, from January 2016 to December 2020. Five machine learning algorithms, including support vector machine, random forest, extra trees classifier (ETC), decision tree, and logistic regression algorithms, were trained to develop models for predicting IHCA. We included blood counts, biochemical markers, and coagulation markers in the model development. We validated model performance using fivefold cross-validation and used the SHapley Additive exPlanation (SHAP) for model interpretation.
Results
A total of 11,308 participants were included in the study, of which 7779 patients remained. Among these patients, 1796 (23.09%) cases of IHCA occurred. Among five machine learning models for predicting IHCA, the ETC algorithm exhibited better performance, with an AUC of 0.920, compared with the other four machine learning models in the fivefold cross-validation. The SHAP showed that the top ten factors accounting for cardiac arrest in rescue-treated patients are prothrombin activity, platelets, hemoglobin, N-terminal pro-brain natriuretic peptide, neutrophils, prothrombin time, serum albumin, sodium, activated partial thromboplastin time, and potassium.
Conclusions
We developed a reliable machine learning-derived model that integrates readily available laboratory parameters to predict IHCA in patients treated with rescue therapy.
Similar content being viewed by others
Background
In-hospital cardiac arrest (IHCA) is an acute disease with a high fatality rate that burdens individuals, society, and the economy [1, 2]. There are approximately 290,000 cases of IHCA in the United States annually, with only 25% of such cases surviving and being discharged from the hospital [3]. A study [4] of IHCA in China observed that the incidence of IHCA was 17.5 per 1000 admissions, and the rates of return of spontaneous circulation and survival to hospital discharge were 35.5% and 9.1%, respectively. Thus, the current situation of IHCA in China is still concerning. Although technologies, such as mild hypothermia and extracorporeal membrane oxygenation, are increasingly used in cardiac arrest therapy [5, 6], patient prognosis remains poor. Therefore, identifying patients with high risk of IHCA is crucial for early intervention.
Machine learning has been demonstrated as a powerful tool that could detect unnoticed data trends and patterns in the use of conventional statistical models [7]. Recently, machine learning methods are increasingly applied to predict IHCA in hospitalized patients, emergency department patients, and intensive care unit patients [8,9,10,11]. However, to the best of our knowledge, a few studies explored approaches for predicting IHCA in patients treated with rescue therapy. Compared with previous study patients, patients treated with rescue therapy are in worse condition and need more efficient risk assessment. Furthermore, laboratory parameter are subject to strict quality control and have been identified as independent risk factors of poor patient outcomes [12, 13]. However, previous studies mainly focused on the performance of the model, with limited emphasis on the predictive factors [14,15,16]. Moreover, most previous studies only included blood cell counts and biochemical markers but overlooked the predictive value of coagulation markers [9, 11, 17, 18]. A study conducted by Deng et al. reported that D-dimer was associated with immediate mortality in patients with IHCA, while other markers related to coagulation were not analyzed [19]. Meanwhile, a number of former studies included subjective and unstructured variables in prediction modeling, which need manual discrimination or data conversion that might not be applicable to a rescue setting [8, 11, 20,21,22,23]. Laboratory results are objective and readily available; however, no previous studies have used machine learning to predict cardiac arrest solely based on routine laboratory parameters.
Therefore, we aimed to develop an appreciable model solely using routine laboratory data obtained from hospital information system (including blood counts, biochemical markers, and coagulation markers) to predict incident IHCA in patients requiring rescue therapy.
Results
Population characteristics
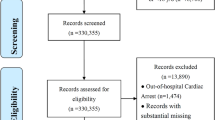
A total of 11,308 hospitalized patients receiving rescue therapy were included in this study, and 3529 patients were excluded according to the exclusion criteria. Among 7779 patients included in the present analysis, 1796 patients experienced IHCA (positive samples) and 5983 patients did not experience IHCA (negative samples) (Fig. 1). The incidence rate of IHCA did not differ by sex (63.73% vs 64.70%, P = 0.453). Patients with IHCA were older (80 years old vs 63 years old, P < 0.001) and had a higher proportion of comorbidities, such as hypertension (48.55% vs 38.84%, P < 0.001) and diabetes (25.84% vs 21.16%, P < 0.001), compared with those without IHCA (Table 1).
After undersampling, 1796 patients with IHCA and 1796 patients without IHCA were included in the model development. Basic characteristics are shown in Additional file 2: Table S1. After randomly grouping at a ratio of 8:2, the training set included 2873 patients and the testing set included 719 patients. The basic characteristics of the training set and testing set are listed in Table 2. There was no statistically significant difference between training set and testing set.
Model development and validation
We used a heatmap to present the correlation coefficient between all variables (Fig. 2), and the results showed that hemoglobin and red blood cell, direct bilirubin, and total bilirubin had high correlation coefficient (> 0.8), respectively. The variable importance ranked by extra trees classifier (ETC) algorithm showed that red blood cell and total bilirubin had lower variable importance compared with their counterparts. Therefore, we discarded red blood cell and total bilirubin in the model development.
Correlation between variables. WBC white blood cell, PT prothrombin time, PTA prothrombin activity, TT thrombin time, LDH lumbar disc herniation, ALT alanine aminotransferase, NT-proBNP N-terminal pro-BNP, RBC red blood cells, APTT activated partial thromboplastin time, TnT troponin T, AST aspartate aminotransferase, CRP C-reactive protein
ETC, logistic regression, random forest, support vector machine (SVM), and decision tree algorithms were used to develop the prediction models of IHCA in patients treated with rescue therapy. In the training group, we observed that ETC algorithm showed better performance compared with the other four algorithms (area under curve [AUC], 0.939 in ETC vs. 0.896 in logistic regression, 0.938 in random forest, 0.829 in SVM, and 0.871 in decision tree; P for comparison < 0.01) (Table 3 and Fig. 3). In the testing group, ETC algorithm also showed the best performance among five algorithms (AUC, 0.920 in ETC vs. 0.895 in logistic regression, 0.877 in random forest, 0.864 in SVM, and 0.843 in decision tree; P for comparison < 0.01) (Table 3 and Fig. 3). After fivefold cross-validation, the ETC algorithm generally provided the best overall performance regarding the AUC, accuracy, specificity, sensitivity, and F1-score compared with the other four algorithms (Table 3 and Fig. 4), indicating the consistency and robustness of our model. After considering these scores, especially the AUCs, we chose ETC model as the final prediction model. The hyperparameters for the ETC model as selected are summarized as follows: number of trees (n_estimators) = 100, supported criteria (criterion) = gini, maximum tree depth (max_depth) = 12, minimum number of samples leaf (min_samples_leaf) = 1, and minimum number of samples split (min_samples_split) = 2.
Model interpretation
As shown in Fig. 5a, the mean absolute SHapley Additive exPlanation (SHAP) value indicates individual feature importance in the ETC model, and the top ten variables were prothrombin activity (PTA), platelets (PLT), hemoglobin, N-terminal pro-BNP (NT-proBNP), neutrophils, prothrombin time (PT), serum albumin, sodium, activated partial thromboplastin time (APTT), and potassium. According to the summary plot (Fig. 5b), PTA, PLT, hemoglobin, and serum albumin were negatively correlated with IHCA occurrence. For example, a low PTA increases the importance of IHCA prediction, whereas a high PTA reduces the importance of IHCA prediction. In contrast, NT-proBNP, neutrophils, PT, sodium, APTT, and potassium were positively correlated with IHCA occurrence. The dependence plots of the SHAP value of top ten important variables are shown in Additional file 1: Fig. S1. The difference of abnormalities of top ten important variables between patients with and without IHCA is shown in Additional file 2: Table S2 [24,25,26,27,28,29,30]
SHapley Additive exPlanations (SHAP) results. a SHAP feature importance; b SHAP summary plot of the top 20 variables. PTA prothrombin activity, NT-proBNP N-terminal pro-BNP, PT prothrombin time, APTT activated partial thromboplastin time, CRP C-reactive protein, WBC white blood cell, LDH lumbar disc herniation, AST aspartate aminotransferase, TT thrombin time, ALT alanine aminotransferase, TnT troponin T
Discussion
In this study, we developed a machine learning-derived prediction model of IHCA in patients treated with rescue therapy. After fivefold cross-validation, the prediction model of IHCA based on the ETC algorithm showed the best performance among five algorithms used for model development. The SHAP interpreted the output of machine learning model and estimated the positive and negative contributions of each feature to the model prediction. The top ten important variables included PTA, PLT, hemoglobin, NT-proBNP, neutrophils, PT, serum albumin, sodium, APTT, and potassium, which are important predictors for IHCA in rescue-treated patients and provide valuable information for early intervention in rescue-treated patients to prevent IHCA.
ETC algorithm is an ensemble classifier that uses unpruned decision trees from the training datasets to construct an extremely randomized or extra tree classifier [31]. In this study, the ETC model showed excellent performance and better predictive power than the other four machine learning models. Notably, this model could predict the occurrence of IHCA in 24 h after testing laboratory parameters, and all variables were easy to obtain and under strict laboratory quality control. Therefore, this model is suitable for clinical practice in large tertiary hospitals.
Coagulopathy often occurs after resuscitation from cardiac arrest or during cardiac arrest [32]. Previous studies [33] have suggested that consumptive coagulopathy played a central role in the pathogenesis of cardiac arrest and the activation of the coagulation system was persistent during cardiac arrest. Among rescue-treated patients, sepsis-related coagulation dysfunction is one of the most common causes of death [34,35,36]. Because of the excessive production of plasminogen activator inhibitor-1, sepsis-related disseminated intravascular coagulation (DIC) causes excessive inhibition of fibrinolysis and may result in related prothrombotic effects, leading to reduced tissue perfusion, organ dysfunction, and poor outcomes [37, 38]. PT, APTT, and PLT are generally used to evaluate blood coagulation function, and have a high predictive value for DIC prediction [39]. Moreover, previous studies [40, 41] have indicated that PT prolongation and PLT decline are associated with increased mortality in patients with sepsis. Consistently, our study showed that coagulation markers are important predictors for IHCA. PT and APTT were positively correlated with the occurrence of IHCA, whereas PTA and PLT were negatively correlated with the occurrence of IHCA. 16.09% of patients with IHCA had abnormally prolonged PT by more than 3 s, and 42.20% of patients with IHCA had a PLT < 100 × 109/L. However, clinicians always ignored coagulation disorders at an early stage, because these coagulation parameters were easily affected by multiple diseases and the fluctuation range is large [39, 42]. The findings of our study indicated that more attention should be paid to the progressive deterioration of coagulation parameters. It is necessary to monitor coagulation parameters in patients treated with rescue therapy and intervene coagulation disorders as early as possible.
As a commonly used infection index in clinics, neutrophils have been proven as biomarkers of sepsis [43, 44], which explains the finding that higher neutrophils was positively correlated with the occurrence of IHCA. Consistently, patients with cardiac arrest were frequently accompanied with infection, as shown in Additional file 1: Fig. S1. Albumin is the one of the most important components in human plasma, which can reflect the nutritional status and maintain osmotic pressure. Hofer et al. [45] found that the plasma albumin level in septic patients was significantly lower than that in non-septic patients. Our study found that serum albumin was negatively correlated with incident IHCA, which supports the effort of early management on nutritional status to prevent the occurrence of IHCA.
Previous studies [3] suggested that cardiovascular problems are the most common cause of cardiac arrest (50–60%). Higher brain natriuretic peptide is significantly associated with more severe cardiac injury and poorer prognosis. Pfister et al. [46]showed that NT‐proBNP was associated with both death and cardiovascular composite outcomes in a clinical population of patients with cardiovascular disease or chronic kidney disease. Similar to these findings, the SHAP results in our study showed that NT-proBNP is a strong predictor of IHCA and those with high NT-proBNP were more likely to suffer IHCA. In addition, 64.25% of patients with IHCA had an NT-proBNP level > 450 pg/mL, as shown in Additional file 2: Table S2.
Electrolyte disorder is one of the potential cause of cardiac arrest, among which potassium disorder is closely related to life-threatening arrhythmia [47]. Potassium is the main intracellular cation in the human body, which regulates the cardiac function, bones’ metabolism, and acid–base balance. Abnormality in potassium concentration can lead to serious complications. Patients with hyperkalemia are in extremely high risk of life-threatening cardiac arrest. Meanwhile, our study found that the level of sodium is positively correlated with the occurrence of IHCA in rescue-treated patients. A former study suggested that hypernatremia (> 145 mmol/L) can increase the risk of mortality [25]. Coppini et al. [48] found that the change in intracellular calcium homeostasis and the increase of late sodium current promoted arrhythmia. Additionally, Wu et al. [11] found that low level of hemoglobin is related to incident cardiac arrest. Taken together, these findings explain the importance of electrolyte and hemoglobin in the prediction of IHCA and suggest that the blood concentration of electrolyte and hemoglobin should be monitored frequently in rescue-treated patients to better prevent the occurrence of IHCA.
The major strength of our study is that we developed a reliable machine learning model to predict IHCA in rescue-treated patients solely using readily available laboratory parameters, which minimums the potential subjective bias that is common in self-reported data and medical texts, and enables our model to be more robust and applicable. This model promotes accurate prediction for IHCA in rescue-treated patients, which may further reduce the burden in frontline healthcare and improve the rescue success rate. However, several limitations should be considered. First, the major limitation of our study is that we only included patients from a single hospital, lacking external validation, and due to issues like missing data, we were unable to compare our results with the existing models. This may limit the generalizability of our model to other hospitals or regions. However, we only used objective laboratory test data in model development. The homogeneous nature of laboratory test data could help to reduce potential confounding due to region and health care disparities. Second, our study was based on a retrospective design, which may cause selection bias. Future prospective study and external validation are still warranted to further validate the model of our study.
Conclusion
We developed an appreciable ETC model to predict IHCA in rescue-treated patients solely using routine laboratory parameters. The model showed that the major risk factors for IHCA in rescue-treated patients were PTA, PLT, hemoglobin, NT-proBNP, neutrophils, PT, serum albumin, sodium, APTT, and potassium. During the hospitalization of rescue-treated patients, physicians should attach great importance to frequently monitoring these parameters to prevent the occurrence of IHCA as possible.
Methods
Study population
This study was reviewed and approved by the ethics committee of the First Medical Center of Chinese PLA General Hospital (Ethics approval number: S2023-282-01). Rescue-treated patients were retrospectively identified from the hospital information system at the First Medical Center of the PLA General Hospital in Beijing, China, from January 2016 to December 2020. The inclusion criteria [11, 49, 50] were: (1) age ≥ 18 years and (2) length of hospital stay > 24 h; the exclusion criteria [11, 49, 50] were: (1) patients who had IHCA before rescue treatment, (2) patients who had history of out-of-hospital cardiac arrest (OHCA), (3) patients who had IHCA during surgery, and (4) patients with missing data on laboratory test.
Prediction outcome
The primary outcome measure was the incidence of IHCA. This study defined IHCA as hospitalized patients whose pulse disappeared and required chest compression or defibrillation because of electrical defibrillation/cardioversion events. Only the first cardiac arrest that occurred in the hospital was analyzed [3, 49, 51].
Candidate features
We abstracted data of the rescue-treated patients from the hospital information system. The following variables were collected: (1) demographic data: sex, age, body mass index (BMI), drinking, and smoking history; (2) basic diseases: hypertension and diabetes; (3) laboratory results: blood counts, biochemical markers, and coagulation markers, and C-reactive protein (CRP). For patients who experienced IHCA (positive samples), we collected laboratory data that were tested within the 24 h before incident IHCA. For patients who did not experienced IHCA (negative samples), we collected laboratory data that were tested within the 24 h after admission.
Data processing
Candidate variables with missing values greater than 40% were excluded [52]. We calculated correlation coefficient between all variables and identified those pairs with high correlation coefficient (> 0.8). In the pair of variables with high correlation coefficient, the one with lower variable importance would be excluded. We discarded outliers of each variable, which were defined as values whose difference with mean was greater than threefold standard deviation. Missing values were handled using means substitution method [53, 54]. Finally, given that the negative samples are several times of positive samples in our study, we conducted undersampling using k-means clustering algorithm to balance the imbalanced data sets. The k-means algorithm recognizes each negative sample as an eigenvector and divides all negative samples into n eigenvector datasets with similar features, where n is the same with the number of positive samples. For each dataset, the k-means algorithm selects 1 eigenvector, which is the closest to the mean of the eigenvectors in the dataset, as a negative sample, and ultimately forms a dataset with n negative samples to create sample balance [55].
Model development and validation
The dataset used for model development was randomly partitioned into two samples: 80% of the participants for model training and parameter learning and 20% of the participants for model performance evaluation and comparison. We used the ETC, logistic regression, random forest, SVM, and decision tree algorithms to develop a model for early prediction of IHCA. The performance metrics of the five models were evaluated by calculating the AUC of the receiver-operating characteristic curve, accuracy, specificity, sensitivity, and F1-score. Furthermore, we performed fivefold cross-validation to test the consistency and robustness of the model. To interpret the final predictive model, we used SHAP to explain the output of the model by evaluating the variable importance and the impact direction of variables [56]. Model development and validation were conducted using Python Version 3.8 (Python Software Foundation, Wilmington, DE, USA).
Statistical analysis
Continuous variables with a normal distribution were presented as the mean ± standard deviation, and t tests were used for comparison between groups. Furthermore, non-normally distributed continuous variables were presented as median (interquartile range). Moreover, the Mann–Whitney U test was used for comparisons between groups. Categorical variables were presented as percentages (%), and the Chi-square test was used for comparisons between groups. To enhance the interpretability of our model, we provided the difference of abnormalities of parameters with high feature importance between patients with and without IHCA. All statistical analyses were conducted using SPSS statistical software (version 26.0; IBM Corp., Armonk, NY, USA). P value < 0.05 was considered statistically significant.
Availability of data and materials
The data sets are available from the corresponding author.
Abbreviations
- IHCA:
-
In-hospital cardiac arrest
- CA:
-
Cardiac arrest
- OHCA:
-
Out-of-hospital cardiac arrest
- BMI:
-
Body mass index
- CRP:
-
C-reactive protein
- SVM:
-
Support vector machine
- ETC:
-
Extra trees classifier
- AUC:
-
Area under the receiver operator curve
- SHAP:
-
SHapley Additive Explanations
- PTA:
-
Prothrombin activity
- PLT:
-
Platelet
- NT-proBNP:
-
N-terminal pro-BNP
- PT:
-
Prothrombin time
- APTT:
-
Activated partial thromboplastin time
- DIC:
-
Disseminated intravascular coagulation
References
DiLibero J, Misto K. Outcomes of in-hospital cardiac arrest. Crit Care Nurs Clin North Am. 2021;33(3):343–56.
Holmberg MJ, Ross CE, Fitzmaurice GM, Chan PS, Duval-Arnould J, Grossestreuer AV, Yankama T, Donnino MW, Andersen LW. Annual incidence of adult and pediatric in-hospital cardiac arrest in the United States. Circ Cardiovasc Qual Outcomes. 2019;12(7): e005580.
Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. In-hospital cardiac arrest: a review. JAMA. 2019;321(12):1200–10.
Shao F, Li CS, Liang LR, Qin J, Ding N, Fu Y, Yang K, Zhang GQ, Zhao L, Zhao B, et al. Incidence and outcome of adult in-hospital cardiac arrest in Beijing, China. Resuscitation. 2016;102:51–6.
Maekawa K, Tanno K, Hase M, Mori K, Asai Y. Extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest of cardiac origin: a propensity-matched study and predictor analysis. Crit Care Med. 2013;41(5):1186–96.
Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, Leary M, Meurer WJ, Peberdy MA, Thompson TM, Zimmerman JL. Part 8: post-cardiac arrest care: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S465-482.
Cho SM, Austin PC, Ross HJ, Abdel-Qadir H, Chicco D, Tomlinson G, Taheri C, Foroutan F, Lawler PR, Billia F, et al. Machine learning compared with conventional statistical models for predicting myocardial infarction readmission and mortality: a systematic review. Can J Cardiol. 2021;37(8):1207–14.
Tsai CL, Lu TC, Fang CC, Wang CH, Lin JY, Chen WJ, Huang CH. Development and validation of a novel triage tool for predicting cardiac arrest in the emergency department. West J Emerg Med. 2022;23(2):258–67.
Wu TT, Yang DL, Li H, Guo YS. Development and validation of a nomogram to predict in-hospital cardiac arrest among patients admitted with acute coronary syndrome. Am J Emerg Med. 2021;49:240–8.
Kenet AL, Pemmaraju R, Ghate S, Raghunath S, Zhang Y, Yuan M, Wei TY, Desman JM, Greenstein JL, Taylor CO, et al. A pilot study to predict cardiac arrest in the pediatric intensive care unit. Resuscitation. 2023;185: 109740.
Wu TT, Lin XQ, Mu Y, Li H, Guo YS. Machine learning for early prediction of in-hospital cardiac arrest in patients with acute coronary syndromes. Clin Cardiol. 2021;44(3):349–56.
Asadollahi K, Hastings IM, Gill GV, Beeching NJ. Prediction of hospital mortality from admission laboratory data and patient age: a simple model. Emerg Med Aust EMA. 2011;23(3):354–63.
Jarvis SW, Kovacs C, Badriyah T, Briggs J, Mohammed MA, Meredith P, Schmidt PE, Featherstone PI, Prytherch DR, Smith GB. Development and validation of a decision tree early warning score based on routine laboratory test results for the discrimination of hospital mortality in emergency medical admissions. Resuscitation. 2013;84(11):1494–9.
Chin KC, Cheng YC, Sun JT, Ou CY, Hu CH, Tsai MC, Ma MH, Chiang WC, Chen AY. Machine learning-based text analysis to predict severely injured patients in emergency medical dispatch: model development and validation. J Med Internet Res. 2022;24(6): e30210.
Jang DH, Kim J, Jo YH, Lee JH, Hwang JE, Park SM, Lee DK, Park I, Kim D, Chang H. Developing neural network models for early detection of cardiac arrest in emergency department. Am J Emerg Med. 2020;38(1):43–9.
Schnabel RB, Marinelli EA, Arbelo E, Boriani G, Boveda S, Buckley CM, Camm AJ, Casadei B, Chua W, Dagres N, et al. Early diagnosis and better rhythm management to improve outcomes in patients with atrial fibrillation: the 8th AFNET/EHRA consensus conference. Europace Eur Pacing Arrhythmias Cardiac Electrophysiol. 2023;25(1):6–27.
Chae M, Han S, Gil H, Cho N, Lee H. Prediction of in-hospital cardiac arrest using shallow and deep learning. Diagnostics (Basel). 2021;11(7):1255.
Choi A, Choi SY, Chung K, Chung HS, Song T, Choi B, Kim JH. Development of a machine learning-based clinical decision support system to predict clinical deterioration in patients visiting the emergency department. Sci Rep. 2023;13(1):8561.
Deng Y, He L, Yang J, Wang J. Serum D-dimer as an indicator of immediate mortality in patients with in-hospital cardiac arrest. Thromb Res. 2016;143:161–5.
Lu TC, Wang CH, Chou FY, Sun JT, Chou EH, Huang EP, Tsai CL, Ma MH, Fang CC, Huang CH. Machine learning to predict in-hospital cardiac arrest from patients presenting to the emergency department. Intern Emerg Med. 2023;18(2):595–605.
Kwon JM, Kim KH, Jeon KH, Lee SY, Park J, Oh BH. Artificial intelligence algorithm for predicting cardiac arrest using electrocardiography. Scand J Trauma Resusc Emerg Med. 2020;28(1):98.
Chi CY, Ao S, Winkler A, Fu KC, Xu J, Ho YL, Huang CH, Soltani R. Predicting the mortality and readmission of in-hospital cardiac arrest patients with electronic health records: a machine learning approach. J Med Internet Res. 2021;23(9): e27798.
Mayampurath A, Hagopian R, Venable L, Carey K, Edelson D, Churpek M. American Heart Association’s get with the guidelines-resuscitation i: comparison of machine learning methods for predicting outcomes after in-hospital cardiac arrest. Crit Care Med. 2022;50(2):e162–72.
Abdel-Azim H, Sun W, Wu L. Strategies to generate functionally normal neutrophils to reduce infection and infection-related mortality in cancer chemotherapy. Pharmacol Ther. 2019;204: 107403.
Bollaert PE, Monnier A, Schneider F, Argaud L, Badie J, Charpentier C, Meziani F, Bemer M, Quenot JP, Buzzi M, et al. Fluid balance control in critically ill patients: results from POINCARE-2 stepped wedge cluster-randomized trial. Critical care (London, England). 2023;27(1):66.
Jia CG, Gao JG, Liu FS, Li Z, Dong ZL, Yao LM, Wang LB, Yao XW. Efficacy, safety and prognosis of treating neurological deficits caused by spinal tuberculosis within 4 weeks’ standard anti-tuberculosis treatment: a single medical center’s experience. Exp Ther Med. 2020;19(1):519–26.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B. Worldwide prevalence of anaemia, WHO Vitamin and Mineral Nutrition Information System, 1993–2005. Public Health Nutr. 2009;12(4):444–54.
Sarin SK, Kedarisetty CK, Abbas Z, Amarapurkar D, Bihari C, Chan AC, Chawla YK, Dokmeci AK, Garg H, Ghazinyan H, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the Study of the Liver (APASL) 2014. Hep Intl. 2014;8(4):453–71.
Xu D, Zhou B, Zhang J, Li C, Guan C, Liu Y, Li L, Li H, Cui L, Xu L, et al. Prediction of hyperkalemia in ESRD patients by identification of multiple leads and multiple features on ECG. Ren Fail. 2023;45(1):2212800.
Awan MJ, Mohd Rahim MS, Salim N, Rehman A, Nobanee H. Machine learning-based performance comparison to diagnose anterior cruciate ligament tears. J Healthcare Eng. 2022;2022:2550120.
Kim HJ, Michael K, Wee JH, Oh JS, Kim WY, Cho IS, Lee MJ, Lee DH, Kim YH, Youn CS. Coagulation measures after cardiac arrest (CMACA). PLoS ONE. 2023;18(1): e0279653.
Böttiger BW, Motsch J, Böhrer H, Böker T, Aulmann M, Nawroth PP, Martin E. Activation of blood coagulation after cardiac arrest is not balanced adequately by activation of endogenous fibrinolysis. Circulation. 1995;92(9):2572–8.
Font MD, Thyagarajan B, Khanna AK. Sepsis and Septic Shock—basics of diagnosis, pathophysiology and clinical decision making. Med Clin North Am. 2020;104(4):573–85.
Giustozzi M, Ehrlinder H, Bongiovanni D, Borovac JA, Guerreiro RA, Gąsecka A, Papakonstantinou PE, Parker WAE. Coagulopathy and sepsis: pathophysiology, clinical manifestations and treatment. Blood Rev. 2021;50: 100864.
Markwart R, Saito H, Harder T, Tomczyk S, Cassini A, Fleischmann-Struzek C, Reichert F, Eckmanns T, Allegranzi B. Epidemiology and burden of sepsis acquired in hospitals and intensive care units: a systematic review and meta-analysis. Intensive Care Med. 2020;46(8):1536–51.
Koyama K, Madoiwa S, Nunomiya S, Koinuma T, Wada M, Sakata A, Ohmori T, Mimuro J, Sakata Y. Combination of thrombin-antithrombin complex, plasminogen activator inhibitor-1, and protein C activity for early identification of severe coagulopathy in initial phase of sepsis: a prospective observational study. Critical care (London, England). 2014;18(1):R13.
Schmitt FCF, Manolov V, Morgenstern J, Fleming T, Heitmeier S, Uhle F, Al-Saeedi M, Hackert T, Bruckner T, Schöchl H, et al. Acute fibrinolysis shutdown occurs early in septic shock and is associated with increased morbidity and mortality: results of an observational pilot study. Ann Intensive Care. 2019;9(1):19.
Adelborg K, Larsen JB, Hvas AM. Disseminated intravascular coagulation: epidemiology, biomarkers, and management. Br J Haematol. 2021;192(5):803–18.
Cato LD, Wearn CM, Bishop JRB, Stone MJ, Harrison P, Moiemen N. Platelet count: a predictor of sepsis and mortality in severe burns. Burns. 2018;44(2):288–97.
Iba T, Di Nisio M, Thachil J, Wada H, Asakura H, Sato K, Saitoh D. A proposal of the modification of japanese society on thrombosis and hemostasis (JSTH) disseminated intravascular coagulation (DIC) Diagnostic criteria for sepsis-associated DIC. Clin Appl Thromb Hemost. 2018;24(3):439–45.
Levi M, Sivapalaratnam S. Disseminated intravascular coagulation: an update on pathogenesis and diagnosis. Expert Rev Hematol. 2018;11(8):663–72.
Meghraoui-Kheddar A, Chousterman BG, Guillou N, Barone SM, Granjeaud S, Vallet H, Corneau A, Guessous K, de Roquetaillade C, Boissonnas A, et al. Two new neutrophil subsets define a discriminating sepsis signature. Am J Respir Crit Care Med. 2022;205(1):46–59.
Pierrakos C, Velissaris D, Bisdorff M, Marshall JC, Vincent JL. Biomarkers of sepsis: time for a reappraisal. Critical care (London, England). 2020;24(1):287.
Omiya K, Sato H, Sato T, Wykes L, Hong M, Hatzakorzian R, Kristof AS, Schricker T. Albumin and fibrinogen kinetics in sepsis: a prospective observational study. Critical care (London, England). 2021;25(1):436.
Malachias MVB, Jhund PS, Claggett BL, Wijkman MO, Bentley-Lewis R, Chaturvedi N, Desai AS, Haffner SM, Parving HH, Prescott MF, et al. NT-proBNP by itself predicts death and cardiovascular events in high-risk patients with type 2 diabetes mellitus. J Am Heart Assoc. 2020;9(19): e017462.
Lott C, Truhlár A. Cardiac arrest in special circumstances. Curr Opin Crit Care. 2021;27(6):642–8.
Coppini R, Santini L, Olivotto I, Ackerman MJ, Cerbai E. Abnormalities in sodium current and calcium homoeostasis as drivers of arrhythmogenesis in hypertrophic cardiomyopathy. Cardiovasc Res. 2020;116(9):1585–99.
Kwon JM, Lee Y, Lee Y, Lee S, Park J. An algorithm based on deep learning for predicting in-hospital cardiac arrest. J Am Heart Assoc. 2018;7(13): e008678.
Lee YJ, Cho KJ, Kwon O, Park H, Lee Y, Kwon JM, Park J, Kim JS, Lee MJ, Kim AJ, et al. A multicentre validation study of the deep learning-based early warning score for predicting in-hospital cardiac arrest in patients admitted to general wards. Resuscitation. 2021;163:78–85.
Green M, Lander H, Snyder A, Hudson P, Churpek M, Edelson D. Comparison of the between the flags calling criteria to the MEWS, NEWS and the electronic Cardiac Arrest Risk Triage (eCART) score for the identification of deteriorating ward patients. Resuscitation. 2018;123:86–91.
Lang Q, Li L, Zhang Y, He X, Liu Y, Liu Z, Yan H. Development and validation of a diagnostic nomogram for Pneumocystis jirovecii pneumonia in non-HIV-infected pneumonia patients undergoing oral glucocorticoid treatment. Infection Drug Resist. 2023;16:755–67.
Khongrum J, Yingthongchai P, Boonyapranai K, Wongtanasarasin W, Aobchecy P, Tateing S, Prachansuwan A, Sitdhipol J, Niwasabutra K, Thaveethaptaikul P, et al. Safety and effects of Lactobacillus paracasei TISTR 2593 supplementation on improving cholesterol metabolism and atherosclerosis-related parameters in subjects with hypercholesterolemia: a randomized, double-blind, placebo-controlled clinical trial. Nutrients. 2023;15(3):661.
Veenis JF, Yalcin YC, Brugts JJ, Constantinescu AA, Manintveld OC, Bekkers JA, Bogers A, Caliskan K. Survival following a concomitant aortic valve procedure during left ventricular assist device surgery: an ISHLT Mechanically Assisted Circulatory Support (IMACS) Registry analysis. Eur J Heart Fail. 2020;22(10):1878–87.
Li J, Tao Y, Cong H, Zhu E, Cai T. Predicting liver cancers using skewed epidemiological data. Artif Intell Med. 2022;124: 102234.
Agius R, Brieghel C, Andersen MA, Pearson AT, Ledergerber B, Cozzi-Lepri A, Louzoun Y, Andersen CL, Bergstedt J, von Stemann JH, et al. Machine learning can identify newly diagnosed patients with CLL at high risk of infection. Nat Commun. 2020;11(1):363.
Funding
This study was supported by Major Science and Technology Program of Hainan Province (No. ZDKJ202004), National Key Research and Development Program of China (No. 2019YFC0119600), and Research on new concept of intelligent first aid for weapon injury (2022SYSZZKY17).
Author information
Authors and Affiliations
Contributions
XHD, YCW, and WYM are the major contributors to design the study and writing the manuscript. YJP, JJH, and MW collected the patient information and analyzed the date. XHD, YCW, and JJH supervised the manuscript critically for important intellectual content.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to Helsinki's statement and has been reviewed and approved by the ethics committee of The First Medical Center of Chinese PLA General Hospital (Ethics approval number: S2023-282-01).
This study is a retrospective electronic medical record study, so the ethics committee of The First Medical Center of Chinese PLA General Hospital exempted patients from informed consent.
Consent for publication
All authors consent to the publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Fig. S1. SHapley Additive exPlanations (SHAP) dependence plot for the top 10 variables. Fig. S2. Admission diagnoses of In-hospital cardiac arrest.
Additional file 2:
Table S1. Baseline characteristics of the undersampled dataset stratified by incident IHCA. Table S2. The difference of abnormalities of top 10 important parameters between patients with and without IHCA.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ding, X., Wang, Y., Ma, W. et al. Development of early prediction model of in-hospital cardiac arrest based on laboratory parameters. BioMed Eng OnLine 22, 116 (2023). https://doi.org/10.1186/s12938-023-01178-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12938-023-01178-9