Abstract
Background
Dietary diversity has been suggested as a potential preventive measure against frailty in older adults, but the effect of changes in dietary diversity on frailty is unclear. This study was conducted to examine the association between the dietary diversity score (DDS) and frailty among older Chinese adults.
Methods
A total of 12,457 adults aged 65 years or older were enrolled from three consecutive and nonoverlapping cohorts from the Chinese Longitudinal Healthy Longevity Survey (the 2002 cohort, the 2005 cohort, and the 2008 cohort). DDS was calculated based on nine predefined food groups, and DDS changes were assessed by comparing scores at baseline and the first follow-up survey. We used 39 self-reported health items to assess frailty. Cox proportional hazard models were performed to examine the association between DDS change patterns and frailty.
Results
Participants with low-to-low DDS had the highest frailty incidence (111.1/1000 person-years), while high-to-high DDS had the lowest (41.1/1000 person-years). Compared to the high-to-high group of overall DDS pattern, participants in other DDS change patterns had a higher risk of frailty (HRs ranged from 1.25 to 2.15). Similar associations were observed for plant-based and animal-based DDS. Compared to stable DDS changes, participants with an extreme decline in DDS had an increased risk of frailty, with HRs of 1.38 (1.24, 1.53), 1.31 (1.19, 1.44), and 1.29 (1.16, 1.43) for overall, plant-based, and animal-based DDS, respectively.
Conclusions
Maintaining a lower DDS or having a large reduction in DDS was associated with a higher risk of frailty among Chinese older adults. These findings highlight the importance of improving a diverse diet across old age for preventing frailty in later life.
Similar content being viewed by others
Introduction
With the noted increase in the average age of global populations, frailty in older people is gaining international attention [1]. Frailty is associated with an increased risk of adverse outcomes, such as falls, hospitalization, and mortality [2, 3], and effective treatments are currently lacking. Therefore, identifying possible modifiable protective and risk factors has become increasingly crucial for preventing and delaying the progression of frailty.
Diet has been identified as a key factor in preventing the development of frailty [4, 5]. Previous studies have highlighted the association between frailty and individual food groups, such as proteins, fruits and vegetables, and dairy products, as well as energy intake [6,7,8]. Recently, dietary patterns, such as the Healthy Eating Index (HEI), Diet Quality Index (DQI), Mediterranean Diet Score (MDS), and Dietary Approach to Stop Hypertension (DASH) diet score, have aroused particular interest worldwide. Increasing evidence showing that a high-quality diet may be associated with a lower risk of frailty [9,10,11,12].
Dietary diversity, which ensures an adequate intake of essential nutrients [13, 14], has been acknowledged as a critical component of high-quality diets and is advocated by dietary guidelines in numerous countries [15,16,17]. It is quantified by counting the consumption of different foods or food groups within a specified period [13]. Several cross-sectional [18,19,20,21] and prospective studies [22, 23] have shown the relationship between dietary variety and frailty. Moreover, our previous large-scale prospective cohort study of Chinese older adults demonstrated that higher dietary diversity scores (DDS) were associated with lower frailty risk [24]. However, considering potential fluctuations in the diet of participants during the follow-up, baseline dietary diversity as the relevant exposure may introduce some measurement errors [24]. Moreover, it is unclear how the DDS changes during follow-up affected the development of frailty.
Therefore, the aim of this study was to examine the association between DDS changes and frailty among Chinese older adults by using the Chinese Longitudinal Healthy Longevity Survey (CLHLS). We hope that these real data can reflect dynamic changes in the diet of Chinese older adults and provide reliable evidence for the formulation of dietary plans.
Materials and methods
Study setting and participants
The data were derived from the Chinese Longitudinal Healthy Longevity Survey (CLHLS), a large prospective cohort study of the Chinese population aged 65 years or over. For a more detailed description of the study design and data quality assessment can be referred to the published literature [25]. In brief, this survey began in 1998, follow-up surveys and recruitment of new participants in 2000, 2002, 2005, 2008/2009, 2011/2012, 2014, and 2017/2018. Using a multi-stage cluster sampling method, the CLHLS randomly recruit participants from 22 of 34 provinces in China, and the study covered 85% of the total population of China. The questionnaire information was collected by trained interviewers through face-to-face surveys, including family structure, living arrangement, self-rated health, self-rated life satisfaction, chronic diseases, diet, smoking status and alcohol consumption, physical activity, psychological characteristics, education, preretirement occupation, economic status, activities of daily living (ADL), instrumental activities of daily living (IADL), and cognitive function [24]. The CLHLS study was approved by the Biomedical Ethics Committee of Peking University (IRB00001052-13074) and written informed consent was provided by all participants or their proxy respondents.
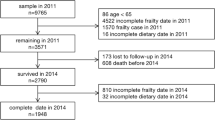
Given that all items used to construct the frailty index (FI) were only included from the 2002 survey onwards, data from the 1998 and 2000 waves were excluded [24]. We assessed data from three consecutive and nonoverlapping cohorts from CLHLS cohorts: the 2002 cohort (waves from 2002, 2005, 2008 and 2011), the 2005 cohort (waves from 2005, 2008, 2011 and 2014) and the 2008 cohort (waves from 2008, 2011, 2014 and 2017). In each time period, the first wave was considered the baseline survey, the three subsequent waves were considered follow-up surveys. Out of a total of 33,009 participants, we excluded those who were below 65 years of age (n = 460), with frailty at baseline (n = 11,542), without follow-up measurements of frailty (n = 8474), and had missing dietary data at baseline survey (n = 12) or the first follow-up survey (n = 64). Ultimately, 12,457 participants were included in the study. The flowchart of the participant enrollment process is shown in Figure S1.
Definitions of dietary diversity score change patterns
Dietary intake information was collected through a face-to-face interview, using a food frequency questionnaire that included several food items traditionally consumed in the Chinese diet, such as fresh fruits, fresh vegetables, beans, salted vegetables, garlic, tea, meat, fish, and eggs. Notably, garlic and salted vegetables, as traditional and prevalently consumed foods [26, 27], along with tea [28], a cornerstone of Chinese cultural expression, are considered independent food groups in the formulation of the DDS. The reproducibility and validity of the questionnaire have been confirmed in the Chinese population [29, 30]. Participants were asked about their current consumption frequency of the nine food groups, which were categorized into three categories: “almost every day” (coded as 2 point), “sometimes or occasionally” (coded as 1 point), or “rarely or never” (coded as 0 point) without consideration for minimum intake levels [31,32,33]. DDS is calculated by summing the scores of the above nine food groups, and previous studies have shown that this DDS is associated with various health outcomes in the Chinese elderly population [22, 24, 31, 34,35,36,37].
The DDS was calculated at baseline and the first follow-up survey. The overall DDS, plant-based DDS (including fresh fruits, fresh vegetables, beans, salted vegetables, garlic, and tea), and animal-based DDS (including meat, fish, and eggs) were scored from 0 to 18, 0 to 12, and 0 to 6, respectively [34]. We divided the overall DDS into three groups: high (13–18 points), middle (7–12 points), and low (0–6 points). Similarly, the plant-based DDS was divided into high (9–12 points), medium (5–8 points), and low (0–4 points) groups; and the animal-based DDS was divided into high (5–6 points), medium (3–4 points), and low (0–2 points) groups.
Nine patterns of relative changes in DDS were identified, including high-to-high, high-to-medium, high-to-low, medium-to-high, medium-to-medium, medium-to-low, low-to-high, low-to-medium, and low-to-low. Additionally, five patterns of absolute changes in DDS were defined using the DDS score changes from baseline to the first follow-up: stable (score of 0), extreme decline (score from “minimum” to “median between minimum and − 1”), moderate decline (score from “median between minimum and − 1” to -1), moderate improvement (score from 1 to “median between 1 and maximum”), and extreme improvement (score from “median between 1 and maximum” to “maximum”) [31]. The specific score ranges of absolute change patterns for overall DDS, plant-based DDS, and animal-based DDS were provided in Table S1.
Ascertainment of frailty
The FI was constructed to evaluate the frailty status. Following the previous CLHLS study, we incorporated 39 health deficits, including self-reported health status, cognitive function, ADL, IADL, functional limitations, hearing and vision, mental health, chronic diseases, and interviewer-rated health status [24, 38, 39] (Table S2). Each item was dichotomous or ordinal variable, mapped to the interval 0 to 1 to indicate the severity of the health deficit. Participants were assigned a score of 2 if they had reported two or more serious illnesses in the previous 2 years. The FI was calculated as the number of health deficiencies present divided by the total number of measured included deficits, with the range from 0 to 1. For participants with missing data, we calculated the FI after removing these variables in the denominator and numerator. A higher FI indicated the worse the health status of the participants. We defined individuals with an FI ≥ 0.25 as frail [1, 38, 40]. The duration of the survival analysis was defined as the time from the baseline survey date to the first time that a participant developed frailty or the last assessment.
Assessment of covariates
A range of potential confounders and effect modifying variables were assessed and defined according to prior literature [31, 34, 41], including: age (year), sex (male or female), residence (rural or urban), occupation (farmer or others), education background (literate or illiterate), marital status (married or others), living pattern (with family members or alone/at nursing home), source of income (pension or others), sufficient income (yes or no), smoking status (current smoker, former smoker, or never smoker), drinking status (current drinker, former drinker, or non-drinker), regular exercise (yes or no), and body mass index (BMI; < 18.5, 18.5–23.9, or ≥ 24.0 kg/m2). More detailed information on the covariates was shown in Method S1. Information on all covariates was collected using standardized and structured questionnaires during the baseline survey [42].
Statistical analysis
The characteristics of the study populations were presented as means (standard deviations [SD]) for continuous variables and numbers (percentages [%]) for categorical variables. The proportion of missing values for any individual covariates were less than 0.3% (Table S3). Multiple imputation were performed to reduce potential inference bias and increase statistical power [43].
Cox proportional hazards model was used to estimate hazard ratios (HRs) and 95% confidence intervals (95%CI) of DDS change patterns and frailty. We tested the proportional-hazards assumption by establishing a cross-product of the duration of follow-up and the pattern of change in DDS. Dose–response relationships of DDS change scores and frailty were analyzed using nonparametric restricted cubic spline regression with knots at the 25th, 50th, and 75th percentiles [44]. Two sets of models were used. Model 1 adjusted for baseline age and sex; model 2 further adjusted for residence, occupation, education background, marital status, living pattern, source of income, sufficient income, smoking status, drinking status, regular exercise, and BMI. Cox proportional hazard models were also performed to examine the relationship of frailty with nine major food groups, adjusted with referred covariates.
Subgroup analyses were conducted in participants with different baseline characteristics, including age (65–79, ≥ 80years), sex (male or female), residence (rural or urban), smoking status (current/former smoker or never smoker), drinking status (current/former drinker or non-drinker), and regular exercise (yes or no). Sensitivity analyses were also conducted to assess the robustness of the results:1) excluding participants who developed frailty in the first follow-up survey; 2) excluding those with missing covariates; 3) additionally adjusting for the number of teeth and the use of artificial dentures; 4) additionally adjusting for the year of recruitment.
All statistical analyses were performed with the use of R software, version 4.0.0 (R Development Core Team, Vienna, Austria). A two-sided P value of less than 0.05 was considered statistically significant.
Results
Baseline characteristics of the participants
Among 12,457 participants, 48.7% were male, and the mean age was 80.54 years (SD, 10.75). In the nine patterns of relative changes of DDS, the medium-to-medium group had the largest number of people (6,209, 49.84%), while the low-to-high group had the least number of people (75, 0.60%). Participants with high-to-high patterns tended to be male, live in urban areas, have non-farming occupations, be literate, married, live with family members, have a pension, have sufficient income, never smoke or drink, engage in regular exercise, and have normal BMI (Table 1).
Association between DDS change and frailty
Figure 1 presents the association between the DDS change patterns and the risk of frailty. Among the 12,457 participants, the high-to-high DDS change pattern had the lowest incidence of frailty at 41.1 per 1000 person-years, whereas the low-to-low DDS change pattern had the highest incidence of frailty at 111.1 per 1000 person-years. Compared to those with a high-to-high of overall DDS pattern, participants in the high-to-medium, high-to-low, medium-to-high, medium-to-medium, medium-to-low, low-to-medium, and low-to-low groups had a higher risk of frailty, with HRs (95%CI) of 1.44 (1.19, 1.75), 2.13 (1.62, 2.80), 1.25 (1.02, 1.54), 1.40 (1.18, 1.67), 1.90 (1.57, 2.29), 1.64 (1.34, 2.00), and 2.15 (1.73, 2.66), respectively. The relationships between plant-based DDS and animal-based DDS and frailty were similar to the overall DDS (Fig. 1). Compared with the high-to-high plant-based DDS pattern, the high-to-medium, high-to-low, medium-to- medium, medium-to-low, low-to-medium, and low-to-low patterns had a higher risk of frailty, with HRs (95%CI) of 1.33 (1.07, 1.65), 2.20 (1.71, 2.84), 1.39 (1.14, 1.69), 1.67 (1.37, 2.05), 1.46 (1.19, 1.81), and 1.70 (1.37, 2.11), respectively. For animal-based DDS, compared to the high-to-high pattern, the high-to-medium, high-to-low, medium-to-low, low-to-medium, and low-to-low patterns had a higher risk of frailty, with HRs (95%CI) of 1.17 (1.02, 1.36), 1.41 (1.16, 1.71), 1.40 (1.21, 1.62), 1.24 (1.07, 1.44), and 1.55 (1.33, 1.80), respectively.
The association between the dietary diversity score change patterns and frailty. HR, hazard ratio; CI, confidence interval. The model Adjusted for age, sex, residence, occupation, education background, marital status, living pattern, source of income, sufficient income, smoking status, drinking status, regular exercise, and BMI
In addition, we examined the associations between special food consumption and the risk of frailty (Table 2). Compared to those who always-to-always consumed specific foods, participants who never-to-never consumed fresh fruit, fresh vegetables, garlic, tea, meat, and fish had a higher risk of frailty, with HRs (95% CI) of 1.31 (1.07, 1.59), 2.53 (1.43, 4.48), 1.38 (1.19, 1.60), 1.30 (1.18, 1.43), 1.86 (1.62, 2.14), and 1.32 (1.13, 1.54), respectively (Table 2).
Figure S2 illustrates the dose-response relationship between DDS change scores and frailty risk. In general, the degree of DDS decline was positively associated with the risk of frailty compared to stable (score change of 0) in overall DDS, plant-based DDS, and animal-based DDS. An increase in plant-based DDS was not significantly associated with the risk of frailty, whereas an increase in overall DDS exceeding 7 points or an increase in animal-based DDS exceeding 2 points was gradually associated with an increased risk of frailty (Figure S2). Moreover, we assessed the association of absolute patterns of DDS change with frailty (Fig. 2). Compared to participants with stable DDS changes, those with an extreme decline in DDS had an increased risk of frailty, with HRs of 1.38 (1.24, 1.53), 1.31 (1.19, 1.44), and 1.29 (1.16, 1.43) for overall, plant-based, and animal-based DDS, respectively. The extreme increase in animal-based DDS was also associated with an increased risk of frailty, with an HR of 1.12 (1.03, 1.23) (Fig. 2).
The association between the absolute patterns of dietary diversity score change and frailty. HR, hazard ratio; CI, confidence interval. Absolute DDS change patterns: stable (score of 0), extreme decline (score from “minimum” to “median between minimum and − 1”), moderate decline (score from “median between minimum and − 1” to -1), moderate improvement (score from 1 to “median between 1 and maximum”), and extreme improvement (score from “median between 1 and maximum” to “maximum”). The model Adjusted for age, sex, residence, occupation, education background, marital status, living pattern, source of income, sufficient income, smoking status, drinking status, regular exercise, and BMI
Subgroup and sensitivity analyses
The associations between DDS change patterns and frailty remained consistent when stratified by age group, sex, residence, smoking status, drinking status, and regular exercise, with no significant interaction (all P for interactions > 0.00625; Table 3). Sensitivity analyses were robust, showing no significant changes after excluding participants who developed frailty in the first follow-up survey (Figure S3) or those with missing covariates (Figure S4). Additionally, adjusting for the number of teeth and the use of artificial dentures (Figure S5), as well as adjusting for the year of recruitment (Figure S6) did not substantially alter the results.
Discussion
In this large cohort study of Chinese older adults, maintaining a low level of overall DDS was significantly associated with an increased risk of frailty. This association also existed in both plant-based and animal-based DDS. Furthermore, an extreme decline in overall DDS was associated with a 38% increased risk of frailty. We adjusted for a range of confounding factors and conducted subgroup and sensitivity analyses, which increased the reliability of our results.
Over recent years, more attention has been devoted to the relationship between dietary patterns and frailty, rather than focusing on single food groups such as protein, fruits, vegetables, dairy products. Previous studies examining the relationship between dietary patterns (including HEI, DQI, MDS, and DASH dietary scores) and frailty found that higher diet quality scores were associated with a lower risk of frailty [9,10,11,12]. However, measuring the above diet quality scores may be difficult, and DDS may be a more feasible option without requiring quantitative measurement. Moreover, evidence regarding the links between DDS change and frailty in older adults is rather sparse. Therefore, focused on the population of Chinese older adult, the present study expands on our earlier research, examined the association between baseline DDS and frailty [24], and found that maintaining a low level DDS was associated with an increased risk of frailty in subsequent years among older adults.
Previous studies have found that lowering or maintaining a lower DDS increases the risk of cognitive impairment and all-cause mortality [31, 34]. Our study is the first to demonstrate a relationship between changes in DDS and frailty in the older population. This finding may be explained by the fact that a higher DDS might indicate a high-quality diet, which is a proxy and rapid indicator of nutrient adequacy. Increasing the variety of foods in the diet is strongly associated with adequate nutritional intake [45, 46]. Lowering or maintaining a lower DDS can increases the odds of nutrient deficiencies, especially in older adults, and malnutrition and multiple nutrient deficiencies or a single diet may be associated with frailty [47,48,49]. Our study suggested that maintaining a higher dietary diversity, even after older age can still reduce the risk of frailty, which has important public health implications for older Chinese adults.
In addition, maintaining a lower intake of these foods, including fresh fruit, fresh vegetables, garlic, tea, meat, and fish, was associated with a higher risk of frailty. The possible mechanism is that fresh fruits, fresh vegetables, and teas contain high levels of antioxidants, which can prevent frailty by reducing reactive oxygen species, and garlic has been demonstrated to prevent osteoporosis and its active component allicin has various biological activities including antioxidant, anti-inflammatory, and anti-apoptotic effects [50, 51]. Moreover, meat and fish contain high-quality protein, which can help prevent or delay age-related muscle atrophy, and affect the development of frailty [52] 53. These findings emphasize the importance of maintaining a varied diet for the long-term health of older adults.
We also conducted analyses of plant-based and animal-based DDS changes and observed similar patterns to the main findings. Interestingly, we found that an extreme improvement in animal-based DDS was associated with an increased risk of frailty, a correlation not observed with plant-based DDS. A possible explanation includes that an extreme improvement in animal-based DDS primarily reports a transition from low-to-high and low-to-medium DDS within animal food groups, and it may also be associated with a lower intake of plant products rich in antioxidants, thereby contributing to the development of frailty [50, 51].
The strengths of this study include a prospective design, large sample size, long-term follow-up, repeated assessment of diet, and the robustness of results, supported by subgroup and sensitivity analyses. However, there were several limitations with regard to the study design and measurements in this study. Firstly, detailed quantitative dietary intake assessments were not performed, so we were unable to adjust for energy intake in our analyses. However, some key determinants of energy intake were considered, such as age, sex, BMI, economic situation, and lifestyle. Secondly, there is no direct evidence that this Chinese culture-based DDS reflects rich nutrient intake. However, previous studies have also shown that higher scores on this DDS are associated with a lower risk of adverse outcomes in the Chinese elderly population [22, 24, 31, 34,35,36,37]. Thirdly, despite carefully adjusting for a series of confounders, residual and unmeasured confounders may still be present. Fourthly, due to the observational design, a causal relationship cannot be established. Fifthly, although we conducted sensitivity analyses by excluding participants who developed frailty at the first follow-up, reverse causation may still exist. Finally, despite the findings might have important public health implications, the results may not be generalizable to other populations or countries given the unique characteristics of the study participants and the differences between Chinese and Western diets.
Conclusions
Among Chinese older adults, maintaining a lower DDS was associated with a higher risk of frailty, and a large reduction in DDS may significantly increase the risk of frailty. These findings highlight that maintaining a higher dietary diversity can still reduce frailty risk even after old age, which has important public health implications for older Chinese.
Data availability
No datasets were generated or analysed during the current study.
References
Hoogendijk EO, Afilalo J, Ensrud KE, et al. Frailty: implications for clinical practice and public health. Lancet (London England). 2019;394(10206):1365–75. https://doi.org/10.1016/s0140-6736(19)31786-6. [published Online First: 2019/10/15].
Clegg A, Young J, Iliffe S, et al. Frailty in elderly people. Lancet (London England). 2013;381(9868):752–62. https://doi.org/10.1016/s0140-6736(12)62167-9. [published Online First: 2013/02/12].
Fontana L, Addante F, Copetti M, et al. Identification of a metabolic signature for multidimensional impairment and mortality risk in hospitalized older patients. Aging Cell. 2013;12(3):459–66. https://doi.org/10.1111/acel.12068. [published Online First: 2013/03/19].
Bollwein J, Diekmann R, Kaiser MJ, et al. Dietary quality is related to frailty in community-dwelling older adults. Journals Gerontol Ser Biol Sci Med Sci. 2013;68(4):483–9. https://doi.org/10.1093/gerona/gls204. [published Online First: 2012/10/16].
Hernández Morante JJ, Gómez Martínez C, Morillas-Ruiz JM. Dietary factors Associated with Frailty in Old adults: a review of Nutritional interventions to prevent Frailty Development. Nutrients. 2019;11(1). https://doi.org/10.3390/nu11010102. [published Online First: 2019/01/10].
García-Esquinas E, Rahi B, Peres K, et al. Consumption of fruit and vegetables and risk of frailty: a dose-response analysis of 3 prospective cohorts of community-dwelling older adults. Am J Clin Nutr. 2016;104(1):132–42. https://doi.org/10.3945/ajcn.115.125781. [published Online First: 2016/05/20].
Cuesta-Triana F, Verdejo-Bravo C, Fernández-Pérez C, et al. Effect of milk and other dairy products on the risk of Frailty, Sarcopenia, and cognitive performance decline in the Elderly: a systematic review. Adv Nutr (Bethesda Md). 2019;10(suppl2):S105–19. https://doi.org/10.1093/advances/nmy105. [published Online First: 2019/05/16].
Schoufour JD, Franco OH, Kiefte-de Jong JC, et al. The association between dietary protein intake, energy intake and physical frailty: results from the Rotterdam Study. Br J Nutr. 2019;121(4):393–401. https://doi.org/10.1017/s0007114518003367. [published Online First: 2018/11/14].
Hengeveld LM, Wijnhoven HAH, Olthof MR, et al. Prospective associations of Diet Quality With Incident Frailty in older adults: the Health, Aging, and body composition study. J Am Geriatr Soc. 2019;67(9):1835–42. https://doi.org/10.1111/jgs.16011. [published Online First: 2019/07/04].
Chan R, Leung J, Woo J. Dietary patterns and risk of Frailty in Chinese Community-Dwelling Older people in Hong Kong: a prospective cohort study. Nutrients. 2015;7(8):7070–84. https://doi.org/10.3390/nu7085326. [published Online First: 2015/08/26].
Ward RE, Orkaby AR, Chen J, et al. Association between Diet Quality and Frailty Prevalence in the Physicians’ Health Study. J Am Geriatr Soc. 2020;68(4):770–76. https://doi.org/10.1111/jgs.16286. [published Online First: 2019/12/17].
Na W, Kim H, Sohn C. Association between frailty and dietary quality in community-dwelling elderly: data from the 6th Korea National Health and Nutrition Examination Survey (2014–2015). J Clin Biochem Nutr. 2021;68(3):268–74. https://doi.org/10.3164/jcbn.20-133. [published Online First: 2021/05/25].
Ruel MT. Operationalizing dietary diversity: a review of measurement issues and research priorities. J Nutr. 2003;133(11 Suppl 2):s3911–26. https://doi.org/10.1093/jn/133.11.3911S. [published Online First: 2003/12/16].
de Oliveira Otto MC, Anderson CAM, Dearborn JL et al. Dietary Diversity: Implications for Obesity Prevention in Adult Populations: A Science Advisory From the American Heart Association. Circulation 2018;138(11):e160-e68. https://doi.org/10.1161/cir.0000000000000595 [published Online First: 2018/10/26].
Society GN. 10 guidelines of the German Nutrition Society (DGE) for a wholesome diet. 2017.
Montagnese C, Santarpia L, Buonifacio M, et al. European food-based dietary guidelines: a comparison and update. Nutr (Burbank Los Angeles Cty Calif). 2015;31(7–8):908–15. https://doi.org/10.1016/j.nut.2015.01.002. [published Online First: 2015/05/28].
Mozaffarian D, Ludwig DS. Dietary guidelines in the 21st century–a time for food. JAMA. 2010;304(6):681–2. https://doi.org/10.1001/jama.2010.1116. [published Online First: 2010/08/12].
Kim J, Yang S, Kim H, et al. Association between Frailty and Dietary Diversity in Korean Elderly: based on the 2018 Korean National Health and Nutrition Examination Survey. Curr Developments Nutr. 2021;5(Supplement2):1050–50. https://doi.org/10.1093/cdn/nzab053_043.
Hayakawa M, Motokawa K, Mikami Y, et al. Low Dietary Variety and Diabetes Mellitus are Associated with Frailty among Community-Dwelling older Japanese adults: a cross-sectional study. Nutrients. 2021;13(2). https://doi.org/10.3390/nu13020641. [published Online First: 2021/03/07].
Motokawa K, Watanabe Y, Edahiro A, et al. Frailty Severity and Dietary Variety in Japanese older persons: a cross-sectional study. J Nutr Health Aging. 2018;22(3):451–56. https://doi.org/10.1007/s12603-018-1000-1. [published Online First: 2018/02/28].
Bernstein MA, Tucker KL, Ryan ND, et al. Higher dietary variety is associated with better nutritional status in frail elderly people. J Am Diet Assoc. 2002;102(8):1096–104. https://doi.org/10.1016/s0002-8223(02)90246-4. [published Online First: 2002/08/13].
Duan Y, Qi Q, Cui Y, et al. Effects of dietary diversity on frailty in Chinese older adults: a 3-year cohort study. BMC Geriatr. 2023;23(1):141. https://doi.org/10.1186/s12877-023-03875-5. [published Online First: 2023/03/16].
Huang WC, Huang YC, Lee MS et al. The Combined Effects of Dietary Diversity and Frailty on Mortality in Older Taiwanese People. Nutrients 2022;14(18) https://doi.org/10.3390/nu14183825 [published Online First: 2022/09/24].
Wang X-M, Zhong W-F, Li Z-H, et al. Dietary diversity and frailty among older Chinese people: evidence from the Chinese longitudinal healthy longevity study. Am J Clin Nutr. 2022. https://doi.org/10.1016/j.ajcnut.2022.11.017.
Zeng Y, Feng Q, Hesketh T, et al. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet (London England). 2017;389(10079):1619–29. https://doi.org/10.1016/s0140-6736(17)30548-2. [published Online First: 2017/03/14].
Shi X, Lv Y, Mao C, et al. Garlic consumption and all-cause mortality among Chinese Oldest-Old individuals: a Population-based Cohort Study. Nutrients. 2019;11(7). https://doi.org/10.3390/nu11071504. [published Online First: 2019/07/03].
Zhuang P, Wu F, Liu X, et al. Preserved vegetable consumption and its association with mortality among 440,415 people in the China Kadoorie Biobank. BMC Med. 2023;21(1):135. https://doi.org/10.1186/s12916-023-02829-3. [published Online First: 2023/04/06].
Pan SY, Nie Q, Tai HC, et al. Tea and tea drinking: China’s outstanding contributions to the mankind. Chin Med. 2022;17(1):27. https://doi.org/10.1186/s13020-022-00571-1. [published Online First: 2022/02/24].
Liu D, Ju H, Yang ZY, et al. Food frequency questionnaire for Chinese children aged 12–17 years: validity and reliability. Biomed Environ Sci: BES. 2019;32(7):486–95. https://doi.org/10.3967/bes2019.066. [published Online First: 2019/07/25].
Zhao W, Hasegawa K, Chen J. The use of food-frequency questionnaires for various purposes in China. Public Health Nutr. 2002;5(6a):829–33. https://doi.org/10.1079/phn2002374. [published Online First: 2003/03/18].
Liu D, Zhang XR, Li ZH, et al. Association of dietary diversity changes and mortality among older people: a prospective cohort study. Clin Nutr. 2021;40(5):2620–29. https://doi.org/10.1016/j.clnu.2021.04.012. [published Online First: 2021/05/03].
Kant AK, Schatzkin A, Harris TB, et al. Dietary diversity and subsequent mortality in the First National Health and Nutrition Examination survey epidemiologic follow-up study. Am J Clin Nutr. 1993;57(3):434–40. https://doi.org/10.1093/ajcn/57.3.434. [published Online First: 1993/03/01].
Zhang Y, Jin X, Lutz MW, et al. Interaction between APOE ε4 and dietary protein intake on cognitive decline: a longitudinal cohort study. Clin Nutr. 2021;40(5):2716–25. https://doi.org/10.1016/j.clnu.2021.03.004. [published Online First: 2021/05/03].
Liu D, Zhang WT, Wang JH, et al. Association between Dietary Diversity Changes and cognitive impairment among older people: findings from a Nationwide Cohort Study. Nutrients. 2022;14(6). https://doi.org/10.3390/nu14061251. [published Online First: 2022/03/27].
Huang Q, Zhong W, Chen Z, et al. Associations between specific diets, Dietary Diversity, and cognitive Frailty in older adults - China, 2002–2018. China CDC Wkly. 2023;5(39):872–76. https://doi.org/10.46234/ccdcw2023.166. [published Online First: 2023/10/10].
Zhong WF, Song WQ, Wang XM, et al. Dietary diversity changes and cognitive Frailty in Chinese older adults: a prospective community-based Cohort Study. Nutrients. 2023;15(17). https://doi.org/10.3390/nu15173784. [published Online First: 2023/09/09].
Zheng J, Zhou R, Li F, et al. Association between dietary diversity and cognitive impairment among the oldest-old: findings from a nationwide cohort study. Clin Nutr. 2021;40(4):1452–62. https://doi.org/10.1016/j.clnu.2021.02.041. [published Online First: 2021/03/20].
Zhu A, Yan L, Wu C et al. Residential Greenness and Frailty Among Older Adults: A Longitudinal Cohort in China. Journal of the American Medical Directors Association 2020;21(6):759 – 65.e2. doi: 10.1016/j.jamda.2019.11.006 [published Online First: 2019/12/25].
Gu D, Dupre ME, Sautter J, et al. Frailty and mortality among Chinese at advanced ages. Journals Gerontol Ser B Psychol Sci Social Sci. 2009;64(2):279–89. https://doi.org/10.1093/geronb/gbn009. [published Online First: 2009/02/07].
Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. Journals Gerontol Ser Biol Sci Med Sci. 2007;62(7):722–7. https://doi.org/10.1093/gerona/62.7.722. [published Online First: 2007/07/20].
Zhang J, Zhao A, Wu W, et al. Beneficial effect of Dietary Diversity on the risk of disability in activities of Daily living in adults: a prospective cohort study. Nutrients. 2020;12(11). https://doi.org/10.3390/nu12113263. [published Online First: 2020/10/30].
Zeng YVJ, Xiao Z, Liu Y, Zhang C. Chinese longitudinal healthy longevity survey (CLHLS), 1998–2014. Inter-university Consortium Political Social Res 2017.
Van Buuren S G-OK. mice: Multivariate imputation by chained equations in R. Journal of statistical software 2011.
Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8(5):551–61. https://doi.org/10.1002/sim.4780080504. [published Online First: 1989/05/01].
Cano-Ibáñez N, Gea A, Martínez-González MA et al. Dietary Diversity and Nutritional Adequacy among an Older Spanish Population with Metabolic Syndrome in the PREDIMED-Plus Study: A Cross-Sectional Analysis. Nutrients 2019;11(5) https://doi.org/10.3390/nu11050958 [published Online First: 2019/05/01].
Azadbakht L, Akbari F, Esmaillzadeh A. Diet quality among Iranian adolescents needs improvement. Public Health Nutr. 2015;18(4):615–21. doi: 10.1017/s1368980014000767 [published Online First: 2014/05/14].
Khorsha F, Mirzababaei A, Togha M, et al. Association of dietary diversity score (DDS) and migraine headache severity among women. Neurol Sciences: Official J Italian Neurol Soc Italian Soc Clin Neurophysiol. 2021;42(8):3403–10. https://doi.org/10.1007/s10072-020-04982-6. [published Online First: 2021/01/12].
Huang WC, Huang YC, Lee MS, et al. Frailty Severity and Cognitive Impairment Associated with Dietary Diversity in older adults in Taiwan. Nutrients. 2021;13(2). https://doi.org/10.3390/nu13020418. [published Online First: 2021/02/03].
Chang SF. Frailty is a major related factor for at risk of Malnutrition in Community-Dwelling older adults. J Nurs Scholarship: Official Publication Sigma Theta Tau Int Honor Soc Nurs. 2017;49(1):63–72. https://doi.org/10.1111/jnu.12258. [published Online First: 2016/10/26].
Qian YQ, Feng ZH, Li XB, et al. Downregulating PI3K/Akt/NF-κB signaling with allicin for ameliorating the progression of osteoarthritis: in vitro and vivo studies. Food Funct. 2018;9(9):4865–75. https://doi.org/10.1039/c8fo01095a. [published Online First: 2018/08/31].
Liu Y, Qi H, Wang Y, et al. Allicin protects against myocardial apoptosis and fibrosis in streptozotocin-induced diabetic rats. Phytomedicine: Int J Phytotherapy Phytopharmacology. 2012;19(8–9):693–8. https://doi.org/10.1016/j.phymed.2012.04.007. [published Online First: 2012/05/29].
Houston DK, Nicklas BJ, Ding J, et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the Health, Aging, and body composition (Health ABC) Study. Am J Clin Nutr. 2008;87(1):150–5. https://doi.org/10.1093/ajcn/87.1.150. [published Online First: 2008/01/08].
Volpi E, Campbell WW, Dwyer JT et al. Is the optimal level of protein intake for older adults greater than the recommended dietary allowance? The journals of gerontology Series A, Biological sciences and medical sciences 2013;68(6):677 – 81. https://doi.org/10.1093/gerona/gls229 [published Online First: 2012/11/28].
Funding
This work was supported by the Guangdong Province Universities and Colleges Pearl River Scholar Funded Scheme (2019), the Guangdong Basic and Applied Basic Research Foundation (2023A1515110727), the China Postdoctoral Science Foundation (2023M741552), the Postdoctoral Fellowship Program of CPSF (GZC20231054), and the Construction of High-level University of Guangdong (G623330580 and G621331128). The funders played no role in the study design or implementation; manuscript preparation, review, or approval; or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
X-MW and W-FZ contributed to the statistical analyses, and had primary responsibility for writing the manuscript. CM and X-MS directed the study, revised the article critically for important intellectual content, and determined the final version to be submitted. X-MW, W-FZ, Y-TZ, J-XX, HC, Z-HL, Q-QS, DS, W-QS, QF, and JG contributed to the data cleaning. X-MW, W-FZ, Y-TZ, Z-TC, CL, J-HX, DL and Y-BL contributed to the analysis or interpretation of the data. All authors critically reviewed the manuscript for important intellectual content.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was conducted with the ethical approval of the Biomedical Ethics Committee of Peking University (IRB00001052-13074).
Competing interests
The authors declare no competing interests.
Consent for publication
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, XM., Zhong, WF., Zhang, YT. et al. Association between dietary diversity changes and frailty among Chinese older adults: findings from a nationwide cohort study. Nutr J 23, 91 (2024). https://doi.org/10.1186/s12937-024-00997-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12937-024-00997-3