Abstract
Background
Trimethylamine-N-oxide (TMAO) is linked with obesity, while limited evidence on its relationship with body fat distribution. Herein, we investigated the associations between serum TMAO and longitudinal change of fat distribution in this prospective cohort study.
Methods
Data of 1964 participants (40–75y old) from Guangzhou Nutrition and Health Study (GNHS) during 2008–2014 was analyzed. Serum TMAO concentration was quantified by HPLC–MS/MS at baseline. The body composition was assessed by dual-energy X-ray absorptiometry at each 3-y follow-up. Fat distribution parameters were fat-to-lean mass ratio (FLR) and trunk-to-leg fat ratio (TLR). Fat distribution changes were derived from the coefficient of linear regression between their parameters and follow-up duration.
Results
After an average of 6.2-y follow-up, analysis of covariance (ANCOVA) and linear regression displayed women with higher serum TMAO level had greater increments in trunk FLR (mean ± SD: 1.47 ± 4.39, P-trend = 0.006) and TLR (mean ± SD: 0.06 ± 0.24, P-trend = 0.011). Meanwhile, for women in the highest TMAO tertile, linear mixed-effects model (LMEM) analysis demonstrated the annual estimated increments (95% CI) were 0.03 (95% CI: 0.003 – 0.06, P = 0.032) in trunk FLR and 1.28 (95% CI: -0.17 – 2.73, P = 0.083) in TLR, respectively. In men, there were no similar significant observations. Sensitivity analysis yielded consistent results.
Conclusion
Serum TMAO displayed a more profound correlation with increment of FLR and TLR in middle-aged and older community-dwelling women in current study. More and further studies are still warranted in the future.
Trial registration
NCT 03179657.
Similar content being viewed by others
Background
Obesity, characterized by a high body mass index (BMI), is linked to various health issues like metabolic syndrome (MetS) [1], and cardiovascular diseases (CVDs) [2]. However, the paradox that older adults with higher BMI tend to live longer, and that the aging population faces equal risks of chronic diseases regardless of BMI, has shifted focus to body fat distribution [3]. Specifically, the buildup of visceral adipose tissue (VAT) is strongly connected to problems like dyslipidemia, insulin resistance, and higher mortality risk, regardless of overall body weight or fat mass [4,5,6]. Additionally, the trunk-to-leg fat ratio (TLR), a marker of unfavorable fat distribution, is a valuable predictor of CVD mortality [7]. These changes in body composition are important aspects of aging and can harm overall health as individuals age [8].
Although sex hormones, aging, and genetic variations have been suggested as factors influencing body fat redistribution, studies on serum metabolites that could act as potential biomarkers for body fat distribution are limited. Trimethylamine-N-oxide (TMAO), a gut-derived metabolite produced following ingestion of dietary choline or carnitine, is regulated by these aforementioned factors [9]. Meanwhile, TMAO is reported to promote dyslipidemia, atherosclerosis, and clotting, making it an independent risk factor for CVD [10]. Researches also shown strong links between TMAO and obesity or obesity-related diseases [11,12,13]. Notably, a case–control study showed a significant positive correlation between serum TMAO and visceral fat in hemodialysis patients [14]. Meanwhile, participants with obesity in two different intervention programs demonstrated positive associations between serum TMAO levels and visceral fat mass or trunk fat at baseline [15, 16]. However, previous studies have often focused on individuals with hemodialysis or obesity, neglecting the general population, and primarily considered body weight or absolute fat quantity. What is more, whether serum TMAO levels relate to long-term unfavorable fat accumulation in the broader population remains uncertain. Therefore, further prospective studies are necessary to explore the link between serum TMAO levels and fat distribution, especially the adverse kind, which could inform strategies for preventing obesity and related metabolic conditions.
In this prospective cohort study, we enrolled community-dwelling Chinese adults aged 40 to 75 from the "Guangzhou Nutrition and Health Study (GNHS)" with a median follow-up of 6.2 years. Our goal was to investigate how serum TMAO levels relate to changes in fat distribution over time, focusing particularly on unfavorable fat distribution.
Materials
Participants
The data of this prospective cohort study were obtained from the Guangdong Nutrition and Health Study (GNHS), a prospective cohort study designed to explore the effects of dietary and environmental factors on cardio metabolic outcomes and osteoporosis. Recruitment took place from July 2008 to June 2010. As previously described [17], the inclusion criteria encompassed individuals aged 40 to 75 years who had resided in Guangzhou for at least five years. Demographic characteristics and biological samples were obtained at baseline; body composition was assessed during the follow-up phase every 3 years thereafter. The current exclusion criteria comprised: (1) self-reported or diagnosed cognitive impairment, immobility, chronic renal dysfunction, or cancer (n = 72) at baseline or during the 6.2-year follow-up period; (2) missing data on key covariates (n = 29); (3) implausible dietary energy intake (men, < 800 kcal/d or > 4000 kcal/d; women, < 500 kcal/d or > 3500 kcal/d) (n = 17); (4) missing data on serum TMAO level or serum TMAO level being out of 95% CI (n = 736); (5) participants did not complete two follow-up body composition examinations (n = 351). Eventually, a total of 1964 participants with a median follow-up of 6.2 years were included for the data analysis (Fig. 1). All participants provided written informed consent. The study protocol was approved by the ethics committee (L2017-004).
Serum TMAO and its precursors measurement
After a 10-h fasting period, a 10-mL venous blood sample was collected at the beginning of the study and stayed undisturbed. S Serum was subsequently separated by centrifugation at 3000 × g for 15 min and stored at -80°C until analysis.
Serum TMAO and its precursors (choline, betaine) were quantified by high-performance liquid chromatography-tandem mass spectrometry (HPLC–MS/MS, Agilent 6400 Series Tridple Quad LC/MS, CA, USA), following previously established protocols [11]. In brief, 50 μL of serum was combined with a working solution containing internal standards (TMAO-d9, choline-d9, betaine-d9). Subsequently, 50 μL of acetonitrile spiked with 1% formic acid was added to the mixture and vortexed. After centrifugation at 15,100 × g at 4 °C for 10 min, approximately 120 μL of the supernatants were transferred into vials for HPLC–MS/MS analysis. The analytes and their corresponding isotopes were monitored using specific precursor-product ion transitions, with an iron spray voltage of 3500 V. The coefficients of variance (CVs) for between-run assays were 6.0% for TMAO, 4.91% for choline, and 6.21% for betaine.
Body composition assessment
During each follow-up visit, a trained physician conducted an examination of the body composition of every participant. This assessment utilized dual-energy X-ray absorptiometry (DXA, Discovery W, Hologic Inc, Waltham, USA), operating in the "whole-body scans" mode.
The software accompanying the Hologic Discovery system (version 3.2) facilitated the direct acquisition of fat mass (FM) and bone mineral content (BMC). Absolute lean mass (LM) was determined by subtracting BMC from the original fat-free lean mass, thereby isolating non-bone lean mass. Precise positioning of regions of interest, such as the arms, legs, and trunk areas, and subsequent DXA scan analyses, were carried out by a proficient physician (Additional Fig. S1). Subsequently, to account for variations in weight, FM and LM were adjusted at baseline using the residual method. This adjustment was made in preparation for subsequent analyses [18].
Covariates
The covariates were collected at baseline. Sociodemographic information (age and income), lifestyle (smoking, alcohol or tea drinking, and daily activity), and medical history were collected using a structured questionnaire administered in a face-to-face interview. Dietary intake was assessed by a validated 79-item food frequency questionnaire (FFQ) and adjusted by the energy residual method. Daily activities were assessed by a 19-item questionnaire, including daily occupation, leisure-time activity, and household chores [19]. Anthropometric data, including weight, height, and waist circumference (WC), were measured twice at baseline and each follow-up visit, and the averages were applied to later analyses. Fasting glucose levels were examined using fingertip blood sampling. Serum total cholesterol (TC), triglycerides (TG), and fasting glucose levels were quantified by colorimetric methods using a Roche Cobas 8000 C702 automated analyzer (Roche Diagnostics, Shanghai, China). The intra-assay coefficient of variation was 3.1% for TC, 5.8% for TG, and 2.5% for glucose, respectively [20]. For the concentration of serum TMAO would be affected by its precursors, the serum choline and betaine were also adjusted in the models.
Statistical analysis
Descriptive data were expressed as either mean and standard deviation (SD) for normally distributed variables or median and interquartile range for non-normally distributed variables. Categorical variables were presented as frequencies and percentages. Given the observed differences in body composition between females and males, we displayed all primary results separately for women and men. Baseline characteristics were assessed based on data distribution, utilizing independent t-tests, Kruskal–Wallis tests, or χ2 tests.
The ratio of fat-to-lean mass (FLRs) or percentage of fat mass (FM%) for the entire body and specific regions were calculated. The trunk-to-leg fat ratio (TLR) was determined by the ratio of absolute trunk FM to leg FM. These FLR and TLR values served as indices for fat distribution (FD). Changes in FD (ΔFD) were derived from linear regression coefficients between these indices and follow-up duration, multiplied by the mean follow-up duration of 6.2 years [21].
Analysis of covariance (ANCOVA) was conducted to compare the mean 6.2-year changes across serum TMAO tertiles. This model was adjusted for baseline variables, including age, BMI, TG, TC, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), TMAO precursors (choline, betaine), dietary intake (energy, protein, and fat), lifestyle, and daily activity [5]. Preliminary results did not show significant differences in ΔFM across serum TMAO tertiles (all P > 0.05, Additional Tables S1 and S2); therefore, subsequent analyses focused on the association between serum TMAO and the 6.2-year ΔFD.
Multiple linear regressions (MLR) were employed to explore the adjusted association between ΔFD and each SD increment of serum TMAO. To validate these findings, linear mixed-effects models (LMEMs) were utilized to compare estimated changes in FD over time across serum TMAO tertiles. This analysis incorporated an interaction test between tertiles and time to account for repeated assessments of whole or regional FD over time.
Sensitivity analysis was performed on participants under 65 years of age who had complete covariate data. For participants with missing covariate values, multivariate imputation by chained equations (MICE) was employed to address these gaps. All statistical tests were two-sided, and statistical significance was determined at a P-value < 0.05. Statistical analyses were conducted using R software (version 4.1.2). LMEMs were analyzed using the "nlme" package (version 3.1–152), MICE was conducted using "mice" (version 3.13.0), and additional packages included "tidyverse" (version 1.3.1) and "VIM" (version 6.1.1) in R studio (version 1.3.1093). Data visualization was achieved using the "ggplot2" package (version 3.3.5) in R studio.
Results
Characteristics of the study participants
A total of 1964 eligible participants, consisting of 1423 women and 541 men, were enrolled in the study. The sex-specific baseline characteristics of the participants are detailed in Table 1. The median age of all participants at baseline was 57 years, and the average serum TMAO level was 2.33 μmol/L. In comparison to women, men were older and had higher monthly income levels (> 3000 yuan/month). Additionally, men exhibited a higher likelihood of developing CVDs, type 2 diabetes, or obesity. Furthermore, men engaged in less physical activity and had lower levels of TC, HDL-C, LDL-C, and TG (all P < 0.05).
Changes in fat distribution over 6.2 years among serum TMAO level tertiles
To investigate differences in 6.2-year ΔFD across serum TMAO tertiles, we employed ANCOVA analyses. As illustrated in Fig. 2, after adjusting for potential confounding factors, women exhibited a dose–response relationship in Δ total FLR, Δ trunk FLR, and Δ TLR across serum TMAO level tertiles (Ptrend = 0.037, 0.006, and 0.011, respectively). However, no significant differences in Δ FD were observed among men (Fig. 2).
Comparisons of Δ FD indices across serum TMAO tertiles are shown by violin plot. P1:ANCOVA were conducted to compare the difference in total and regional Δ FD indices across the tertiles of serum TMAO after adjusted co-variables of baseline age, BMI, dietary intake (energy, protein, and fat), daily activity, and lifestyles (smoking, alcohol drinking), TC, TG, HDL-C, LDL-C, serum choline, and betaine. P2: Median of each serum TMAO tertile was applied for p-trend test using linear regression model to investigate the dose-response relationship of total and regional Δ FD indices across the tertiles of serum TMAO. The value of P2 was obtained after adjusting covariates of baseline age, BMI, dietary intake (energy, protein, and fat), daily activity, and lifestyles (smoking, alcohol drinking), TC, TG, HDL-C, LDL-C, serum choline, and betaine
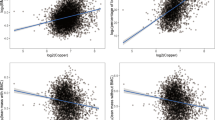
Subsequently, MLR analysis was conducted to explore associations between each SD increase of serum TMAO levels and ΔFD. In women, the results showed that each SD increase in serum TMAO level (0.44 μmol/L) was associated with a 0.260 increase in Δ trunk FLR (P = 0.030) and a 0.069 increase in in ΔTLR (P = 0.024) (Additional Table S3). Similar associations were observed when analyzing TMAO as a continuous variable (Additional Fig. S2). However, in men, no significant associations were observed between each SD increase in serum TMAO levels (0.42 μmol/L) and any of the 6.2-year Δ FD indices (all P > 0.05, Additional Table S3 and Fig. S3).
To confirm the association between FD and serum TMAO levels over time, LMEMs were employed (Table 2). After adjusting for covariates, the interaction analysis indicated that in women, within the highest tertile of serum TMAO level, there were estimated mean changes (95% CI) per year of 1.28 (-0.17, 2.73)/year in trunk FLR and 0.03 (0.003, 0.06)/year in TLR (P-interaction = 0.083 and 0.032, respectively). Conversely, no significant associations were observed in men (Table 2).
Sensitivity analyses
To account for the impact of age on body fat mass, we conducted sensitivity analyses on participants under the age of 65 who had complete covariate data. In women, those in the highest tertile of serum TMAO still exhibited a greater increase in trunk FLR (Ptrend = 0.019) and ΔTLR (Ptrend = 0.087) compared to those in the lowest tertile (Additional Table S4). LMEMs further demonstrated an annual increment of 0.02 in trunk FLR (P = 0.041) and and 2.91 in TLR (P = 0.012) among women (Additional Table S5). However, similar to previous analyses, no significant associations between TMAO and changes in Δ FD were found in the sensitivity analysis.
For women, we further investigated whether menopausal status influences the distribution of body fat. Our findings show that the correlations between serum TMAO levels and trunk FLR and the change in ΔTLR were only significant in postmenopausal women (Additional Fig. S4).
Discussion
In this study, we examined the correlation between serum TMAO and long-term fat distribution in community-dwelling adults aged 40–75. In the follow-up period with a median of 6.2 years, we discovered that higher serum TMAO levels were significantly associated with increased FLR and TLR, especially in middle-aged and older women.
As individuals age, changes occur in their body weight and composition. Previous studies have mainly emphasized the strong correlation between higher body weight, often measured using BMI, and the risk of obesity-related diseases and CVDs [22,23,24]. However, recent research has drawn attention to the role of body fat distribution in these conditions. For example, a 12-year follow-up study found that body fat distribution was independently associated with cardiovascular disease risk in participants from the UK biobank [25]. Another cross-sectional study found that the ratio of trunk fat to peripheral fat, as determined by DXA examination, was positively associated with CVDs, independent of total body fat mass [26]. These findings indicate that BMI alone is insufficient as a predictor of these diseases, emphasizing the importance of monitoring changes in both body fat mass and distribution as individual age.
TMAO, a potentially harmful metabolite originating in the gut, is produced when dietary choline or carnitine is oxidized by the liver enzyme flavin monooxygenase 3 (FMO3) [27]. Previous research has identified TMAO as an independent risk factor for the CVD [10], and it is associated with insulin resistance and obesity [28, 29] However, a recent meta-analysis revealed a nonlinear correlation between TMAO levels and BMI in healthy individuals [13]. The existence of the obesity paradox during the natural aging process further highlights complexity of the relationship between TMAO levels and body weight (BMI) as well as body fat distribution in assessing chronic disease risk [30].
In the current study, we observed that changes in trunk FLR and TLR (Fig. 2, Table 2) increased with higher serum TMAO levels, particularly among women. Notably, the absolute body fat mass did not show significant changes (Additional Tables S1 and S2). Both FLR and TLR are well-established predictors of CVDs [5, 31]. Fat distribution in the trunk and legs can be influenced by factors such as inflammation and insulin resistance [32, 33]. In a study involving healthy Mexican adolescents, a positive association was found between trunk FLR and hyperinsulinemia [34]. Furthermore, the Korea National Health and Nutrition Examination Survey revealed a significant association between higher trunk FLR and increased prevalence of MetS [35]. While there is limited direct epidemiological evidence linking metabolically unhealthy fat distribution to TMAO, there are indications that TMAO could potentially impact body composition, specifically influencing fat distribution in the trunk and legs. A recent study demonstrated that TMAO exacerbated sarcopenic obesity development through ROS-AKT/mTOR signaling in aged mice fed a high-fat diet [36]. Additionally, previous reports have shown that elevated circulating TMAO could induce low-grade chronic systemic inflammation through various inflammatory proteins (IL-6, ICAM1, COX2, LPS etc.) and contribute to metabolic dysfunction [37, 38]. Moreover, a meta-analysis concluded that TMAO may serve as a novel biomarker for diabetes mellitus, CVDs, and kidney function [39]. These findings suggest that serum TMAO levels may impact fat distribution in the trunk and legs during the aging process, emphasizing the need for further research to fully comprehend the underlying mechanisms.
The present study demonstrated a sex-related difference in the association between changes in body fat distribution and serum TMAO levels. One plausible explanation for this sex-related difference lies in the regulation of FMO3 expression by sex hormones. FMO3, responsible for the majority of hepatic TMA conversion to TMAO, exhibits higher expression in the female liver compared to the male liver [40]. Notably, the majority of women in our study were postmenopausal with an average age of 57, and it has been reported that declining estrogen levels might down-regulate FMO3 activation [40]. In our stratified analysis (Additional Fig. S4), we observed that only postmenopausal women showed increased trunk FLR (P = 0.009) and ΔTLR (P < 0.001) with elevated serum TMAO levels. However, the proportion of premenopausal women in the analysis was merely 22.9%, which could explain the lack of significance in the interaction effects between serum TMAO and menopausal status. Furthermore, as women age, the composition of their gut microbiome tends to shift towards a profile abundant in Firmicutes, leading to elevated levels of secondary bile acids and activation of the farnesoid X receptor (FXR) [41]. FXR, a crucial regulator of FMO3, may counterbalance the effects of reduced estrogen levels, partially elucidating the sex-related distinctions. Additionally, FMO3 contributes to metabolic dysfunction through TMAO, which triggers PERK signaling [38]. Studies in humans and rodents have consistently shown that estrogens promote fat accumulation in subcutaneous adipose tissue in women rather than visceral adipose tissue (VAT). The decrease in estrogen levels post-menopause contributes to increased visceral fat mass and metabolic obesity [42]. In contrast, adult men typically have a lower average total body fat percentage compared to adult women due to testosterone, despite a tendency for greater fat accumulation in VAT. These findings imply that women may be more vulnerable to the effects of serum TMAO concerning fat distribution.
The study has several strengths. Firstly, it is the first to investigate the link between serum TMAO levels and unhealthy fat accumulation in middle-aged and older Chinese adults using a prospective study design. Secondly, the study had a relatively large sample size and considered potential socioeconomic and behavioral factors that could affect the association between serum TMAO levels and body composition. Thirdly, a comparison between participants included and excluded from the study (Additional Table S6) showed that those included had healthier lifestyles, with fewer smokers, less alcohol consumption, and lower incomes. Despite the potential underestimation of results, the associations between serum TMAO levels and central fat deposition remained robust after adjusting for these factors. Additionally, accurate body composition measurements were obtained from participants using DEXA [43]. The quantification of Serum TMAO levels was precise, rapid, and stable using HPLC–MS.
However, this study had some limitations. The findings may not be directly applicable to other populations because this was a single-center study. A single assessment of TMAO levels did not account for changes in TMAO levels over time, so the LMEM analysis was performed to minimize the impact of covariates on TMAO and body fat over time. The smaller sample size of men in the study may have contributed to the lack of significant findings in this group, emphasizing the need for larger studies involving men in the future. Moreover, future research should consider measuring sex hormones to better assess post-menopausal status. Finally, it's important to note that since the study was observational in nature, establishing causality is not possible.
Conclusion
In conclusion, the study found a positive association between serum TMAO levels and long-term increases in trunk fat-to-lean ratio (FLR) and trunk-to-limb fat ratio (TLR) in Chinese women aged 40 to 75 years living in the community. This discovery suggests a potential strategy for preventing obesity or sarcopenia during aging. However, further research is needed to explore the underlying mechanisms of this association.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- TMAO:
-
Trimethylamine N-oxide
- GNHS:
-
Guangdong Nutrition and Health Study
- HPLC–MS/MS:
-
High-performance liquid chromatography-tandem mass spectrometry
- DXA:
-
Dual energy X-ray absorptiometer
- FM:
-
Fat mass
- LM:
-
Lean mass
- FLR:
-
Fat-mass to lean-mass ratio
- TLR:
-
Trunk-to-leg fat ratio
- VAT:
-
Visceral adipose tissue
- BMI:
-
Body mass index
- WHR:
-
Waist-to-hip ratio
- MetS:
-
Metabolic syndrome
- CVDs:
-
Cardiovascular diseases
- TMA:
-
Trimethylamine
- FMO3:
-
Flavin-containing monooxygenase 3
- BMC:
-
Bone mineral content
- FFQ:
-
Food frequency questionnaire
- WC:
-
Waist circumference
- HDL-C:
-
High density leptin cholesterol
- LDL-C:
-
Low density leptin cholesterol
- TC:
-
Total cholesterols
- TG:
-
Triglycerides
- ANOVA:
-
Analysis of variance
- LMEMs:
-
Linear mixed-effects models
- MICE:
-
Multivariate imputation by chained equations
- MET:
-
Metabolic equivalent
- SCAT:
-
Subcutaneous adipose tissue
References:
Caleyachetty R, Barber TM, Mohammed NI, Cappuccio FP, Hardy R, Mathur R, Banerjee A, Gill P. Ethnicity-specific BMI cutoffs for obesity based on type 2 diabetes risk in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2021;9:419–26.
Collaborators GBDO, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27.
Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;24094(53):1925–32 IF.
Stefan N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 2020;8:616–27.
Chen GC, Arthur R, Iyengar NM, Kamensky V, Xue X, Wassertheil-Smoller S, Allison MA, Shadyab AH, Wild RA, Sun Y, et al. Association between regional body fat and cardiovascular disease risk among postmenopausal women with normal body mass index. Eur Heart J IF. 2019;29983(40):2849–55 IF.
Murai J, Nishizawa H, Otsuka A, Fukuda S, Tanaka Y, Nagao H, Sakai Y, Suzuki M, Yokota S, Tada H, et al. Low muscle quality in Japanese type 2 diabetic patients with visceral fat accumulation. Cardiovasc Diabetol. 2018;17:112 IF 9951.
Han E, Lee YH, Lee BW, Kang ES, Lee IK, Cha BS. Anatomic fat depots and cardiovascular risk: a focus on the leg fat using nationwide surveys (KNHANES 2008–2011). Cardiovasc Diabetol. 2017;16:54 IF 9951.
Al-Sofiani ME, Ganji SS, Kalyani RR. Body composition changes in diabetes and aging. J Diabetes Complications. 2019;33:451–9.
Witkowski M, Weeks TL, Hazen SL. Gut microbiota and cardiovascular disease. Circ Res. 2020;127:553–70.
Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, Wu Y, Hazen SL. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368:1575–84.
Chen YM, Liu Y, Zhou RF, Chen XL, Wang C, Tan XY, Wang LJ, Zheng RD, Zhang HW, Ling WH, Zhu HL. Associations of gut-flora-dependent metabolite trimethylamine-N-oxide, betaine and choline with non-alcoholic fatty liver disease in adults. Sci Rep. 2016;6:19076.
Al-Obaide MAI, Singh R, Datta P, Rewers-Felkins KA, Salguero MV, Al-Obaidi I, Kottapalli KR, Vasylyeva TL. Gut microbiota-dependent trimethylamine-N-oxide and serum biomarkers in patients with T2DM and advanced CKD. J Clin Med. 2017;6:86.
Dehghan P, Farhangi MA, Nikniaz L, Nikniaz Z, Asghari-Jafarabadi M. Gut microbiota-derived metabolite trimethylamine N-oxide (TMAO) potentially increases the risk of obesity in adults: an exploratory systematic review and dose-response meta- analysis. Obes Rev. 2020;21:e12993.
Bi SH, Su C, Yang P, Zhang X, Wang Y, Tang W, Yang W, He L. Higher serum trimethylamine N-oxide (TMAO) levels are associated with increased visceral fat in hemodialysis patients. Clin Nephrol. 2023;100:275–83.
Heianza Y, Sun D, Smith SR, Bray GA, Sacks FM, Qi L. Changes in gut microbiota-related metabolites and long-term successful weight loss in response to weight-loss diets: the POUNDS lost trial. Diabetes Care. 2018;41:413–9.
Randrianarisoa E, Lehn-Stefan A, Wang X, Hoene M, Peter A, Heinzmann SS, Zhao X, Konigsrainer I, Konigsrainer A, Balletshofer B, et al. Relationship of serum Trimethylamine N-Oxide (TMAO) levels with early atherosclerosis in humans. Sci Rep. 2016;6:26745.
Chen YM, Liu Y, Liu YH, Wang X, Guan K, Zhu HL. Higher serum concentrations of betaine rather than choline is associated with better profiles of DXA-derived body fat and fat distribution in Chinese adults. Int J Obes (Lond). 2015;39:465–71 IF 5095.
El Kinany K, Garcia-Larsen V, Khalis M, Deoula MMS, Benslimane A, Ibrahim A, Benjelloun MC, El Rhazi K. Adaptation and validation of a food frequency questionnaire (FFQ) to assess dietary intake in Moroccan adults. Nutr J. 2018;17:61.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, Leon AS. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–81.
Miao Z, Lin JS, Mao Y, Chen GD, Zeng FF, Dong HL, Jiang Z, Wang J, Xiao C, Shuai M, et al. Erythrocyte n-6 polyunsaturated fatty acids, gut microbiota, and incident type 2 diabetes: a prospective cohort study. Diabetes Care. 2020;43:2435–43.
Zuo LS, Tang XY, Xiong F, Liu YP, Liu M, Ling CW, Sun TY, Ling W, Zhang ZQ, Chen YM. Isoflavone biomarkers are inversely associated with atherosclerosis progression in adults: a prospective study. Am J Clin Nutr. 2021;114:203–13.
Gao M, Lv J, Yu C, Guo Y, Bian Z, Yang R, Du H, Yang L, Chen Y, Li Z, et al. Metabolically healthy obesity, transition to unhealthy metabolic status, and vascular disease in Chinese adults: a cohort study. PLoS Med. 2020;17:e1003351.
Spiegelman D, Israel RG, Bouchard C, Willett WC. Absolute fat mass, percent body fat, and body-fat distribution: which is the real determinant of blood pressure and serum glucose? Am J Clin Nutr. 1992;55:1033–44.
Eckel N, Li Y, Kuxhaus O, Stefan N, Hu FB, Schulze MB. Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90 257 women (the Nurses’ Health Study): 30 year follow-up from a prospective cohort study. Lancet Diabetes Endocrinol. 2018;6:714–24.
Zhong P, Tan S, Zhu Z, Zhu Z, Liang Y, Huang W, Wang W. Normal-weight central obesity and risk of cardiovascular and microvascular events in adults with prediabetes or diabetes: Chinese and British cohorts. Diabetes Metab Res Rev. 2023;39(8):e3707.
Kouda K, Fujita Y, Ohara K, Tachiki T, Tamaki J, Yura A, Moon JS, Kajita E, Uenishi K, Iki M. Associations between trunk-to-peripheral fat ratio and cardiometabolic risk factors in elderly Japanese men: baseline data from the Fujiwara-kyo osteoporosis risk in men (FORMEN) study. Environ Health Prev Med. 2021;26:35.
Lv S, Wang Y, Zhang W, Shang H. Trimethylamine oxide: a potential target for heart failure therapy. Heart. 2022;5994(108):917–22 IF.
Papandreou C, Bullo M, Zheng Y, Ruiz-Canela M, Yu E, Guasch-Ferre M, Toledo E, Clish C, Corella D, Estruch R, et al. Plasma trimethylamine-N-oxide and related metabolites are associated with type 2 diabetes risk in the Prevencion con Dieta Mediterranea (PREDIMED) trial. Am J Clin Nutr IF. 2018;7045(108):163–73.
Heianza Y, Zhou T, He H, DiDonato JA, Bray GA, Sacks FM, Qi L. Changes in gut-microbiota-related metabolites and long-term improvements in lipoprotein subspecies in overweight and obese adults: the POUNDS lost trial. Int J Obes (Lond). 2021;45:2600–7.
Bosello O, Vanzo A. Obesity paradox and aging. Eat Weight Disord. 2021;26:27–35.
Zhou R, Chen HW, Lin Y, Li FR, Zhong Q, Huang YN, Wu XB. Total and regional fat/muscle mass ratio and risks of incident cardiovascular disease and mortality. J Am Heart Assoc. 2023;12:e030101.
Wu H, Qi Q, Yu Z, Sun Q, Wang J, Franco OH, Sun L, Li H, Liu Y, Hu FB, Lin X. Independent and opposite associations of trunk and leg fat depots with adipokines, inflammatory markers, and metabolic syndrome in middle-aged and older Chinese men and women. J Clin Endocrinol Metab. 2010;95:4389–98.
Qiu Z, Lee DH, Lu Q, Li R, Zhu K, Li L, Li R, Pan A, Giovannucci EL, Liu G. Associations of regional body fat with risk of cardiovascular disease and mortality among individuals with type 2 diabetes. J Clin Endocrinol Metab . 2024:dgae192.2024.
Gamboa-Gomez CI, Guerrero-Romero F, Aradillas-Garcia C, Rodriguez-Moran M, Simental-Mendia LE. The fat-to-lean mass ratio is associated with hyperinsulinemia in healthy mexican adolescents. J Am Coll Nutr. 2021;3169(40):219–23 IF.
Seo YG, Song HJ, Song YR. Fat-to-muscle ratio as a predictor of insulin resistance and metabolic syndrome in Korean adults. J Cachexia Sarcopenia Muscle. 2020;11:710–25.
Mo X, Cheng R, Shen L, Sun Y, Wang P, Jiang G, Wen L, Li X, Peng X, Liao Y, et al. High-fat diet induces sarcopenic obesity in natural aging rats through the gut-trimethylamine N-oxide-muscle axis. J Adv Res. 2024.
Komaroff AL. The microbiome and risk for atherosclerosis. JAMA. 2018;319:2381–2.
Chen S, Henderson A, Petriello MC, Romano KA, Gearing M, Miao J, Schell M, Sandoval-Espinola WJ, Tao J, Sha B, et al. Trimethylamine N-oxide binds and activates PERK to promote metabolic dysfunction. Cell Metab. 2019;30:1141-1151 e1145.
Li D, Lu Y, Yuan S, Cai X, He Y, Chen J, Wu Q, He D, Fang A, Bo Y, et al. Gut microbiota-derived metabolite trimethylamine-N-oxide and multiple health outcomes: an umbrella review and updated meta-analysis. Am J Clin Nutr. 2022;116:230–43.
Bennett BJ, de Aguiar Vallim TQ, Wang Z, Shih DM, Meng Y, Gregory J, Allayee H, Lee R, Graham M, Crooke R, et al. Trimethylamine-N-oxide, a metabolite associated with atherosclerosis, exhibits complex genetic and dietary regulation. Cell Metab. 2013;27287(17):49–60 IF.
Razavi AC, Potts KS, Kelly TN, Bazzano LA. Sex, gut microbiome, and cardiovascular disease risk. Biol Sex Differ. 2019;10:29 IF 5027.
Frank AP, de Souza SR, Palmer BF, Clegg DJ. Determinants of body fat distribution in humans may provide insight about obesity-related health risks. J Lipid Res. 2019;5922(60):1710–9 IF.
Wang H, Hai S, Cao L, Zhou J, Liu P, Dong BR. Estimation of prevalence of sarcopenia by using a new bioelectrical impedance analysis in Chinese community-dwelling elderly people. BMC Geriatr. 2016;16:216.
Acknowledgements
The authors thanks to the participants, and would like to especially thank Luo-Shi-Yuan Zuo, Zhuo-zhi Liang and Heng-Gui Chen for their technical suggestion of data analysis and manuscript revision. The raw data supporting the conclusions of this manuscript will be made available by the authors, upon request, to any qualified researcher.
Funding
This work was supported by the Basic and Applied Basic Research Foundation of Guangdong Province, China (Youth Fund, Grant: 2021A1515110848), National Natural Science Youth Foundation of China (82204020), and National Natural Science Foundation of China (Grant: 81773415).
Author information
Authors and Affiliations
Contributions
S.C. and H.-L.Z. were responsible for the conception and designed the research; Y.-M.C. and H.-L.Z. were administrated the project; X.-Y.C. and Z.-H.H. contributed to HPLC–MS/MS analysis; X.-Y.C., R.-Z.H. and S.-Y.L. assisted with the collection of data; S.C. and A.P.-F involved in statistical analysis and graphing; S.C. and B.-X.H. involved in data interpretation and manuscript writing; H.-L.Z. finally approved the manuscript. No conflict of interest exits in the submission of this manuscript, and manuscript is approved by all authors for publication after reading it.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All participants provided written informed consent. The study protocol was approved by the ethics committee (L2017-004).
Consent for publication
No conflict of interest exits in the submission of this manuscript, and manuscript is approved by all authors for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, S., Chen, Xy., Huang, Zh. et al. Correlation between serum trimethylamine-N-oxide and body fat distribution in middle-aged and older adults: a prospective cohort study. Nutr J 23, 70 (2024). https://doi.org/10.1186/s12937-024-00974-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12937-024-00974-w