Abstract
Background
Infants under 6 months of age are often excluded from malaria surveillance and observational studies. The impact of malaria during early infancy on health later in childhood remains unknown.
Methods
Infants from two birth cohorts in Malawi were monitored at quarterly intervals and whenever they were ill from birth through 24 months for Plasmodium falciparum infections and clinical malaria. Poisson regression and linear mixed effects models measured the effect of exposure to malaria in infancy on subsequent malaria incidence, weight-for-age z-scores (WAZ), and haemoglobin concentrations after 6 months.
Results
Infants with at least one P. falciparum infection during their first 6 months had increased incidence ratio (IRR) of P. falciparum infection (IRR = 1.27, 95% CI, 1.06–1.52) and clinical malaria (IRR = 2.37, 95% CI, 2.02–2.80) compared to infants without infection. Infants with clinical malaria had increased risk of P. falciparum infection incidence between 6 and 24 months (IRR = 1.64, 95% CI, 1.38–1.94) and clinical malaria (IRR = 1.85, 95% CI, 1.48–2.32). Exposure to malaria was associated with lower WAZ over time (p = 0.02) and lower haemoglobin levels than unexposed infants at every time interval (p = 0.02).
Conclusions
Infants experiencing malaria infection or clinical malaria are at increased risk of subsequent infection and disease, have poorer growth, and lower haemoglobin concentrations.
Similar content being viewed by others
Background
The burden of Plasmodium falciparum infection and clinical malaria disease remains highest among under-five children in many regions of sub-Saharan Africa. In these settings, children aged 6 months to 2 years may have up to five episodes of clinical malaria per year [1, 2]. Infants under 6 months of age are typically excluded from observational studies because infants are not considered high risk for malaria due to presumed protective effects from maternal antibodies transferred through the placenta, lactoferrin from breastmilk, and fetal haemoglobin [3, 4]. However, recent facility-based surveys suggest that P. falciparum infection and clinical malaria is more common than expected in the under 6-months population in sub-Saharan Africa [5,6,7]. Associations between malaria and health outcomes, such as anaemia and growth have been studied in older children but the long-term, cumulative impact of early infections have not been well-characterized.
Malaria exposure in infancy may impact the health of young children, beyond the morbidity of acute infection. Infections of all varieties are known to impair nutritional status resulting in growth faltering, however the role of early P. falciparum infections in growth and development remains poorly defined and the literature is inconclusive [8,9,10]. Malaria infection is a leading cause of anaemia among young children in endemic regions of sub-Saharan Africa [11, 12]. Plasmodium falciparum infection causes both red blood cell destruction and reduced production), resulting in low haemoglobin levels. The association is strong enough that anaemia prevalence has been proposed as an indicator of acute malaria prevalence in malaria endemic regions, though less is understood about the impact on subsequent anaemia in early childhood [13,14,15]. Malaria infection is associated with low haemoglobin right after infection, but cumulative effects of repeated P. falciparum infections are not well documented in infants, although there is evidence of an association between Plasmodium vivax and anaemia in infants [16].
The study was designed to use longitudinal data collected from two birth cohorts in Malawi to measure malaria infection and disease in early infancy and the association this exposure has with subsequent malaria incidence in early childhood. Because malaria infection during early infancy may enhance or interfere with immunity and subsequent clinical response to malaria infection, the study tested the hypothesis that clinical malaria in the first 6 months of life would be associated with a statistically significant increase in incidence of P. falciparum infection and clinical malaria during early childhood. The study further evaluated the hypothesis that infants with P. falciparum infection or clinical malaria in the first 6 months may have lower weight-for-age z-scores and lower haemoglobin concentrations over time compared to unexposed infants.
Methods
Participants
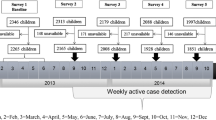
Study participants from two prospective cohorts conducted in southern Malawi were included in this study because they were conducted during the same timeframe and with similar follow-up procedures. The Liwonde cohort enrolled infants born to mothers who participated in a clinical trial that randomly allocated 602 pregnant women to receive monthly administration of either sulfadoxine-pyrimethamine or dihydroartemisinin-piperaquine as intermittent preventive treatment during pregnancy (NCT03009526). Women aged 16 years or older, with a viable singleton pregnancy at less than or equal to 28 gestational weeks were included in the clinical trial if they were HIV-negative and were not experiencing a high-risk pregnancy or experiencing severe anaemia. During pregnancy, women were offered the opportunity to enroll their babies in the infant cohort after completing the clinical trial. Inclusion criteria for mothers enrolling their babies in the infant cohort included intention to stay in the study area for at least one year following delivery and provision of informed consent. Participant enrollment in the infant cohort began in May 2017 and follow up was completed in May 2019. Details of this cohort were described previously [17].
The Mfera cohort enrolled 100 infants at delivery. Infant’s mothers were recruited for the study at the antenatal clinic or the well-child clinic. Enrollment criteria included: provision of informed consent by the parent or guardian, infant born to a mother with documented HIV-negative status, intention to reside in the study region for two years, and willingness to comply with study procedures and attend the health center for regular medical care. Enrollment for the Mfera cohort ended in January 2016 and the final participant completed follow-up in November 2018.
Both studies were reviewed and approved by the University of Maryland Institutional Review Board and the Kamuzu University of Health Sciences College of Medicine Research Ethics Committee. Parents/guardians provided written informed consent for participation of the infant.
Study procedures
All women in the Liwonde clinical trial delivered in the maternity wards at Machinga District Hospital in Liwonde, while infants in the Mfera cohort were born at the Mfera Health Centre in Chikwawa, both in southern Malawi. Data collected at enrollment included demographic characteristics and pregnancy history, including infant sex, maternal age, gravidity, and parity.
Follow-up procedures were the same in both cohorts. Infants visited their respective study clinics for scheduled visits at 3-month intervals for up to 24 months. Growth measurements including weight, length, and head circumference were taken at each scheduled visit. Haemoglobin concentration was only measured in infants enrolled in the Mfera cohort. Mothers were encouraged to bring infants to the clinic in the event of illness. If an infant presented with signs and symptoms consistent with malaria at any visit (axillary fever of > 37.5 °C, report of fever in the previous 48 h, vomiting, irritability or weakness), a Paracheck-Pf (Orchid Biomedical Systems, Goa, India) rapid diagnostic test (RDT) for malaria was performed. All cases of malaria detected by RDT were treated with artemether-lumefantrine according to the national treatment policy in Malawi. Dried blood spots on 3M Whatman filter paper were collected at every scheduled and unscheduled visit from a finger prick.
Laboratory procedures
Asymptomatic and submicroscopic infections were detected from the dried blood spots collected at every visit. Dried blood spots underwent DNA extraction and real time quantitative polymerase chain reaction (qPCR) at the University of Maryland malaria laboratory for detection of the 18S ribosomal RNA gene of P. falciparum [18, 19]. The qPCR results were delayed and thus not available to participants.
Definitions
Exposure to malaria in the first 6 months of life was assessed and defined three ways:
-
A)
Asymptomatic P. falciparum infection includes infants with a positive qPCR but excludes infants with signs and symptoms of malaria accompanied by a positive RDT
-
B)
Clinical malaria was defined as signs or symptoms of malaria recorded at the clinic visit and a positive RDT, and
-
C)
All P. falciparum infections include all infants with clinical malaria or a positive qPCR.
Three outcomes were measured. Incidence of any malaria, including both asymptomatic P. falciparum infection and clinical malaria cases, and incidence of clinical malaria between 6 months of age and the end of follow-up (up to 2 years of age) were measured by the total number of malaria cases divided by the number of person-years at risk. Mean weight-for-age Z-score (WAZ) was assessed at three-month intervals during follow-up (6–24 months) classified according to WHO child growth standards. Mean haemoglobin concentration was assessed at three-month intervals during follow-up (6–24 months) in the Mfera cohort only.
Season of birth was classified as rainy (December–March) or dry (April–November) using historical definitions of rainy and dry seasons in the region. Length of follow-up times varied for participants, so an additional measure of seasonal exposure was included that measured the percent of study time each infant spent in the rainy season. A covariate measured malaria exposure during the follow-up period in the longitudinal analyses as a cumulative count of all malaria infections per individual.
Statistical analysis
Infants with follow up that ended prior to 9 months of age were excluded from these analyses due to inadequate follow up time. Covariates assessed include infant sex, study site, season of birth, percent of follow-up time in the rainy season, low birth weight (< 2.5 kg), maternal age at delivery, and maternal gravidity. Although data from the two studies were combined, study site was included because of varying environmental factors between the two sites. Maternal age at delivery and gravidity were assessed continuously. Bivariate analysis using Chi-square tests and Student’s t-tests were conducted to describe participant characteristics.
Poisson regression was employed to estimate the incidence rate of exposure to malaria in the first 6 months of life and the incidence rate ratio (IRR) for malaria up to 24 months of age comparing those with and without malaria exposure in the first 6 months of life. To adjust for the effect of covariates on the association between the predictors and outcomes, multivariable Poisson regression models were developed with offset of follow up time to control for varying infection and disease rates.
Unadjusted mean WAZ and haemoglobin were plotted over time and adjusted linear mixed effects models, with participant as the random effect, were built and graphed. An interaction term of exposure and infant age was included in every model, regardless of statistical significance, to visualize the difference in slope between the exposed and unexposed infants.
All analyses were conducted using SAS software, Version 9.4 of the SAS System for Microsoft Windows.
Results
Baseline characteristics
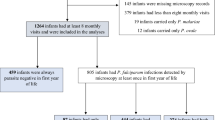
A total of 437 infants with complete data and sufficient follow-up time were included in the final analyses (Table 1). Infant sex, maternal gravidity, and maternal age were not differentially distributed in any of the exposure categories. The proportion of infants with clinical malaria in the first 6 months of life was significantly higher in the Mfera cohort (p = < 0.0001) compared to participants in the Liwonde cohort, but the proportion of infants with asymptomatic P. falciparum infection was not different. While infants in the Mfera cohort comprised 21% of the total study population, they made up 47% of the infants with clinical malaria.
Malaria incidence in infants
Among 127 (27%) infants in the first 6 months of life, there were 241 episodes of any malaria, with an incidence rate of 1.1 episodes per person-year and 69 episodes of clinical malaria with an incidence rate of 0.3 cases per person-year, all in the first 6 months of life. Among 99 (26%) infants with asymptomatic P. falciparum infections in the first 6 months of life, the incidence of any P. falciparum infections after 6 months of life was 2 cases per person-year and incidence of clinical malaria after 6 months of life was 0.9 cases per person-year. Among the 49 (11%) infants with clinical malaria in the first 6 months of life, incidence of asymptomatic P. falciparum infections was 3.8 cases per person-year and incidence of clinical malaria was 2.3 cases per person-year after the first 6 months of life. Results are summarized in Table 2.
In multivariable analysis controlling for study site, season of birth, maternal age, and gravidity, incidence of any malaria up to 24 months of age among infants with any P. falciparum infection during their first 6 months was 27% higher than unexposed infants (IRR = 1.27, 95% CI, 1.06–1.52, Table 3) and clinical malaria incidence was 76% higher in exposed infants (IRR = 1.76, 95% CI, 1.42–2.19). Any malaria incidence among infants who experience clinical malaria during the first 6 months was 64% higher than unexposed infants (IRR = 1.64, 95% CI, 1.38–1.94) and clinical malaria incidence was 85% higher in exposed infants (IRR = 1.85, 95% CI, 1.48–2.32).
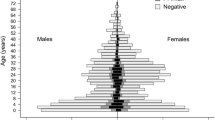
Effect of malaria exposure on growth
The unadjusted mean WAZ for exposed and unexposed infants in all three analyses were between -0.2 and -1.2 (Fig. 1). After including an interaction term comprising infant age and exposure status (to assess the slope of WAZ over the course of follow-up) and adjusting for infant age, malaria during follow-up, infant sex, and low birthweight, the difference in WAZ between infants exposed to any malaria before 6 months and unexposed infants was -0.21 for the duration of follow-up (p = 0.06, Table 4). The difference in WAZ between infants exposed to asymptomatic P. falciparum infection before 6 months and unexposed infants was -0.29 for the duration of follow-up (p = 0.02). Across all 3 analyses, mean WAZ decreased over time in both the exposed and unexposed infants, but never fell to more than two standard deviations below the mean (Fig. 1)
A WAZ over follow-up time by any malaria exposure adjusted for infant age, infant sex, low birthweight, and an interaction term of infants age and malaria exposure (p = 0.21); B WAZ over follow-up time by asymptomatic P. falciparum infection exposure adjusted for infant age, infant sex, low birthweight, and an interaction term of infants age and malaria exposure (p = 0.34); C WAZ over follow-up time by clinical malaria exposure adjusted for infant age, infant sex, low birthweight, and an interaction term of infants age and malaria exposure (p = 0.08). The shaded area indicated 95% confidence intervals
.
Effect of malaria exposure on haemoglobin concentration
Unadjusted mean haemoglobin concentrations for exposed and unexposed infants were below 11 g/dL from 6 months of age until at least 12 months of age, indicating mild to moderate anaemia in the first year of life (Fig. 2). After including an interaction term comprising infant age and exposure status to look at the differences in slope, and adjusting for infant age and malaria during follow-up, the difference in haemoglobin concentration between infants exposed to any malaria before 6 months and unexposed infants was -0.38 g/dL for the duration of follow-up (p = 0.09, Table 4). Mean haemoglobin concentration in infants exposed to asymptomatic P. falciparum infections differed by -0.26 g/dL compared to unexposed infants at 6 months (p = 0.34) and the difference steadily increased over time so that while the mean haemoglobin levels of unexposed infants reached the normal range (> 11 g/dL) around 12 months, exposed infants only reached that threshold around 21 months. The difference in mean haemoglobin levels between infants exposed to clinical malaria during their first 6 months and unexposed infants was -0.57 g/dL (p = 0.03).
A Hemoglobin concentration over follow-up time by any malaria exposure adjusted for infant age, any malaria during follow-up, and an interaction term of infants age and malaria exposure (p = 0.41); B Hemoglobin concentration over follow-up time by asymptomatic P. falciparum infection exposure adjusted for infant age, any malaria during follow-up, and an interaction term of infants age and malaria exposure (p = 0.12); C Hemoglobin concentration over follow-up time by clinical malaria exposure adjusted for infant age, any malaria during follow-up, and an interaction term of infants age and malaria exposure (p = 0.33). The shaded area indicated 95% confidence intervals
Discussion
This study found that infection with P. falciparum 6 months of life, whether symptomatic or asymptomatic, was associated with higher incidence of both malaria infection and clinical malaria in early childhood. Additionally, any malaria infection during the first 6 months of life is associated with lower haemoglobin levels over time and lower weight-for-age z-scores compared to children uninfected during the first 6 months.
Infants under 6 months of age have historically been excluded from malaria studies and thus the results about the burden of infection and disease in this population is an important contribution to the literature. One-third of infants in our study had at least one episode of clinical malaria or P. falciparum infection before reaching 6 months, confirming that infants are susceptible to malaria during early infancy. Nearly twice as many infants had asymptomatic P. falciparum infections before 6 months as infants who experienced clinical malaria during that period, which is consistent with other studies demonstrating relatively high rates of parasitaemia and lower rates of symptomatic malaria illness before 6 months [20].
Several possible causes can explain our finding of higher rates of malaria infection and diseases among infants infected with malaria in the first 6 months of life. Acquired immunity to malaria develops after repeated infection with P. falciparum, however despite their early infection or even multiple infections, the exposed infants in this study did not experience reduced incidence during follow-up suggesting that acquired immunity does not develop this early in life, mirroring the poor immunogenicity of live viral and certain antibacterial vaccines which do not induce immunity in young children. Alternatively, these higher rates may be a marker of environmental exposure to malaria, as demonstrated by the difference in malaria incidence observed in the study sites, with higher infection and clinical malaria rates in observed in the Mfera cohort, or a result of differential exposure to P. falciparum in utero.
Mean WAZ scores in infants infected with clinical malaria in their first 6 months are higher than unexposed infants at 24 months, while these measures are lower in infants with asymptomatic P. falciparum infection at 24 months compared to without malaria in their first 6 months. This may have been observed because infants with asymptomatic P. falciparum infection were classified as unexposed in the clinical malaria model, thereby raising the risk of infants classified as unexposed when assessing the risk posed by clinical malaria in the first 6 months of life and confirmed this with a sensitivity analysis that excluded infants with asymptomatic P. falciparum infection in the first 6 months of life.
Infants with clinical malaria in their first 6 months were diagnosed and treated so that their infections were cleared, whereas infants with asymptomatic infections could have prolonged infections, resulting in chronic infection causing slower growth and lower haemoglobin. This is consistent with recent research showing that asymptomatic malaria infections are prevalent in anaemic children [21].
The analysis identified a trend of decreasing mean weight-for-age z-scores over time in all infants regardless of malaria exposure in their first 6 months. A systematic review of this topic surmised that most studies found no association between malaria exposure and malnutrition (WAZ ≤ − 2.0) among populations in P. falciparum endemic areas [22]. However, to our knowledge, there are no comparable studies that assesses the long-term risk of low WAZ following exposure to malaria in the first 6 months and the association between anthropometry and malaria warrants further exploration.
Malaria is a known cause of low haemoglobin; however, this study suggests that infants exposed to P. falciparum infections during their first 6 months of life already have low haemoglobin levels at 6 months of age and continue to have lower haemoglobin levels compared to their unexposed peers through 2 years of age. The data analysis approach tried to control for the possibility that this trend may be due to repeated infections during follow-up by adjusting the models for cumulative malaria infections between 6 and 24 months. Malaria infections cause haemoglobin concentrations to drop rapidly after initial infection and it can take 4–6 weeks to completely normalize [11]. Infant haemoglobin levels drop off naturally after birth and only begin to recover around 6 months of age, it is possible that malaria infection and the accompanying slow recovery rate of haemoglobin concentrations during this period may be responsible for the prolonged haemoglobin recovery times observed in this population.
The primary limitation of this study is the inability to control for the confounding of environmental malaria exposure that is associated with both the exposure of interest and infection outcomes. If infants live in an environment with increased likelihood of acquiring malaria infection, they will have high rates of malaria throughout their childhood. This limits the ability to assess a causal relationship between early malaria infection and subsequent burden of infection and may confound our finding of decreased WAZ and haemoglobin after early malaria infection. An additional limitation in this analysis was missing data on socioeconomic status, nutrition, or breastfeeding. Socioeconomic status, in particular, may be a predictor of both malaria risk and food insecurity though the sample population belonged to the same socioeconomic group. Mothers in the Mfera cohort all reported breastfeeding until the end of follow-up, so dietary variation were unlikely to be different between exposed and unexposed infants in the haemoglobin analysis.
Conclusion
This study demonstrated that infants with malaria infection in the first 6 months of their lives have chronically lower haemoglobin levels than uninfected infants in the same cohort and higher incidence of malaria overall during early childhood. These early malaria episodes do not appear to elicit protective immunity. Rather, malaria infection before 6 months of age may be an indicator of increased environmental exposure risk suggesting a need to implement additional preventative measures targeting the household or neighbourhood, for example, focal indoor residual spraying or provision of chemoprophylaxis to these children. These results demonstrate the long-term impact of early malaria infection exposure on early childhood health and suggest a need for additional public health guidance for monitoring haemoglobin levels in young children with a history of malaria infection.
Availability of data and materials
The data will be available upon request made to the corresponding author.
References
Kamya MR, Kakuru A, Muhindo M, Arinaitwe E, Nankabirwa JI, Rek J, et al. The impact of control interventions on malaria burden in young children in a historically high-transmission district of Uganda: a pooled analysis of cohort studies from 2007 to 2018. Am J Trop Med Hyg. 2020;103:785–92.
WHO. World malaria report 2020. Geneva, World Health Organization, 2020. Available from: https://www.who.int/publications/i/item/9789240015791. Accessed 16 Mar 2021.
Mohan K, Omar BJ, Singh RD. Clinical presentation and management of neonatal malaria: a review. Malar Chemother Control Elimin. 2014;3:2.
Amaratunga C, Lopera-Mesa TM, Brittain NJ, Cholera R, Arie T, Fujioka H, et al. A role for fetal hemoglobin and maternal immune IgG in infant resistance to Plasmodium falciparum malaria. PLoS ONE. 2011;6: e14798.
D’Alessandro U, Ubben D, Hamed K, Ceesay SJ, Okebe J, Taal M, et al. Malaria in infants aged less than six months—is it an area of unmet medical need? Malar J. 2012;11:400.
Alao MJ, Gbadoé AD, Meremikwu M, Tshefu A, Tiono AB, Cousin M, et al. Plasmodium falciparum malaria in infants under 5 kg: retrospective surveillance of hospital records in five sub-saharan African countries. J Trop Pediatr. 2013;59:154–9.
Mbonye MK, Burnett SM, Naikoba S, Colebunders R, Wouters K, Weaver MR, et al. Malaria care in infants aged under six months in Uganda: an area of unmet needs! PLoS ONE. 2015;10: e0123283.
Scrimshaw NS. Historical concepts of interactions, synergism and antagonism between nutrition and infection. J Nutr. 2003;133:316S-321S.
Rowland MG, Cole TJ, Whitehead RG. A quantitative study into the role of infection in determining nutritional status in Gambian village children. Br J Nutr. 1977;37:441–50.
Alexandre MA, Benzecry SG, Siqueira AM, Vitor-Silva S, Melo GC, Monteiro WM, et al. The association between nutritional status and malaria in children from a rural community in the Amazonian region: a longitudinal study. PLoS Negl Trop Dis. 2015;9: e0003743.
White NJ. Anaemia and malaria. Malar J. 2018;17:371.
Yimgang DP, Buchwald AG, Coalson JE, Walldorf JA, Bauleni A, Kapito-Tembo A, et al. Population attributable fraction of anemia associated with Plasmodium falciparum infection in children in Southern Malawi. Am J Trop Med Hyg. 2021;104:1013–7.
Deribew A, Alemseged F, Tessema F, Sena L, Birhanu Z, Zeynudin A, et al. Malaria and under-nutrition: a community based study among under-five children at risk of malaria, South-West Ethiopia. PLoS ONE. 2010;5: e10775.
Kateera F, Ingabire CM, Hakizimana E, Kalinda P, Mens PF, Grobusch MP, et al. Malaria, anaemia and under-nutrition: three frequently co-existing conditions among preschool children in rural Rwanda. Malar J. 2015;14:440.
Kabaghe AN, Chipeta MG, Terlouw DJ, McCann RS, van Vugt M, Grobusch MP, et al. Short-term changes in anemia and malaria parasite prevalence in children under 5 years during one year of repeated cross-sectional surveys in rural Malawi. Am J Trop Med Hyg. 2017;97:1568–75.
Kenangalem E, Karyana M, Burdarm L, Yeung S, Simpson JA, Tjitra E, et al. Plasmodium vivax infection: a major determinant of severe anaemia in infancy. Malar J. 2016;15:321.
Andronescu LR, Sharma A, Peterson I, Kachingwe M, Kachepa W, Liang Y, et al. The effect of intermittent preventive treatment of malaria during pregnancy and placental malaria on infant risk of malaria. J Infect Dis. 2022;225:248–56.
Adams M, Joshi SN, Mbambo G, Mu AZ, Roemmich SM, Shrestha B, et al. An ultrasensitive reverse transcription polymerase chain reaction assay to detect asymptomatic low-density Plasmodium falciparum and Plasmodium vivax infections in small volume blood samples. Malar J. 2015;14:520.
Zainabadi K, Adams M, Han ZY, Lwin HW, Han KT, Ouattara A, et al. A novel method for extracting nucleic acids from dried blood spots for ultrasensitive detection of low-density Plasmodium falciparum and Plasmodium vivax infections. Malar J. 2017;16:377.
Botwe AK, Owusu-Agyei S, Asghar M, Hammar U, Oppong FB, Gyaase S, et al. Profiles of Plasmodium falciparum infections detected by microscopy through the first year of life in Kintampo a high transmission area of Ghana. PLoS ONE. 2020;15: e0240814.
Bahati YL, Delanghe J, Balaluka GB, Kishabongo AS, Philippé J. Asymptomatic submicroscopic Plasmodium infection is highly prevalent and is associated with anemia in children younger than 5 years in south Kivu/Democratic Republic of Congo. Am J Trop Med Hyg. 2020;102:1048–55.
Ferreira ED, Alexandre MA, Salinas JL, de Siqueira AM, Benzecry SG, de Lacerda MV, et al. Association between anthropometry-based nutritional status and malaria: a systematic review of observational studies. Malar J. 2015;14:440.
Funding
This work was supported by the National Institutes of Health [R21AI121990, K24AI114996 to MKL].
Author information
Authors and Affiliations
Contributions
DPM and MKL designed the study and obtain funding. AS, AB, PM, JC led the clinical study. LRA, AGB, AS, JRG, YL led the analysis of the results. LRA and MKL led the writing of the manuscript. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was reviewed and approved by the University of Malawi College of Medicine Research and Ethics Committee and the University of Maryland Institutional Review Board. Written informed consent was obtained from the mothers of the infants.
Consent for publication
All authors consent to publication of this manuscript.
Competing interests
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Andronescu, L.R., Buchwald, A.G., Sharma, A. et al. Plasmodium falciparum infection and disease in infancy associated with increased risk of malaria and anaemia in childhood. Malar J 22, 217 (2023). https://doi.org/10.1186/s12936-023-04646-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-023-04646-8