Abstract
Background
While many malaria-endemic countries have health management information systems that can measure and report malaria trends in a timely manner, these routine systems have limitations. Periodic community cross-sectional household surveys are used to estimate malaria prevalence and intervention coverage but lack geographic granularity and are resource intensive. Incorporating malaria testing for all women at their first antenatal care (ANC) visit (i.e., ANC1) could provide a more timely and granular source of data for monitoring trends in malaria burden and intervention coverage. This article describes a protocol designed to assess if ANC-based surveillance could be a pragmatic tool to monitor malaria.
Methods
This is an observational, cross-sectional study conducted in Benin, Burkina Faso, Mozambique, Nigeria, Tanzania, and Zambia. Pregnant women attending ANC1 in selected health facilities will be tested for malaria infection by rapid diagnostic test and administered a brief questionnaire to capture key indicators of malaria control intervention coverage and care-seeking behaviour. In each location, contemporaneous cross-sectional household surveys will be leveraged to assess correlations between estimates obtained using each method, and the use of ANC data as a tool to track trends in malaria burden and intervention coverage will be validated.
Results
This study will assess malaria prevalence at ANC1 aggregated at health facility and district levels, and by gravidity relative to current pregnancy (i.e., gravida 1, gravida 2, and gravida 3 +). ANC1 malaria prevalence will be presented as monthly trends. Additionally, correlation between ANC1 and household survey–derived estimates of malaria prevalence, bed net ownership and use, and care-seeking will be assessed.
Conclusion
ANC1-based surveillance has the potential to provide a cost-effective, localized measure of malaria prevalence that is representative of the general population and useful for tracking monthly changes in parasite prevalence, as well as providing population-representative estimates of intervention coverage and care-seeking behavior. This study will evaluate the representativeness of these measures and collect information on operational feasibility, usefulness for programmatic decision-making, and potential for scale-up of malaria ANC1 surveillance.
Similar content being viewed by others
Background
Malaria continues to be a significant cause of morbidity and mortality worldwide, and progress toward malaria control and elimination targets in many countries has now stalled due to a range of complex issues, including increased insecticide resistance, suboptimal control strategies, weak public health systems, reduced funding, and shifting global health priorities [1]. There were an estimated 247 million malaria cases in 2021, an increase from 227 million cases in 2019 [2, 3].
Health surveillance systems continuously monitor disease trends that inform the planning, implementation, and evaluation of prevention and control programs, as well as the allocation of health resources. The World Health Organization’s Global Technical Strategy for Malaria 2016–2030 describes surveillance as a key pillar of national and subnational strategies, necessary at all levels of malaria burden to achieve elimination [4]. However, current surveillance systems are costly and/or prone to error. Malaria-endemic countries have implemented standardized, electronic-based health management information systems (HMISs) on platforms such as the District Health Information Software 2 (DHIS2), which can provide real-time, monthly health facility data to measure trends in clinical malaria from outpatient department visits. However, timeliness and quality can be limited by the fact that the data are often collected on paper registers and must be tallied and uploaded to the DHIS2 system. Another key limitation is that these data are collected from public health systems and are subject to patient care-seeking behavior, and thus may not be representative of malaria transmission in the broader community [5]. Further, calculating accurate incidence measurements at the most granular level requires accompanying information about the population at the level of the health facility catchment area. In addition, although other country data platforms may exist, HMISs themselves do not currently collect information on intervention coverage or use and, despite recent improvements, data quality remains a limitation of these systems in many contexts [2]. In combination, these limitations mean that in the World Malaria Report 2021, the World Health Organization (WHO) deemed that the quality of surveillance data did not permit a robust estimate of disease burden from the number of reported cases for 30 malaria-endemic countries, all of which were in Africa [2]. Moreover, there are currently no routine indicators with which to assess trends in exposure to malaria in pregnancy, a key driver of many adverse pregnancy and birth outcomes, and a substantial contributor to overall malaria burden [6, 7], nor is there an indicator to assess the prevalence of asymptomatic malaria infections that contribute significantly to transmission.
Household cross-sectional surveys such as demographic health surveys and malaria indicator surveys are used to measure infection prevalence among both asymptomatic and symptomatic persons combined (and specifically, among children under 5 years of age in most surveys), coverage of malaria control interventions, and care-seeking behaviours in the general population to help provide accurate estimates of these indicators. They are also the basis for many geostatistical models of malaria burden, particularly in countries lacking sufficiently robust routine data, and often serve as a cornerstone of subnational stratification and tailoring exercises, which inform strategic plan and funding application development [8]. However, household surveys are rarely powered sufficiently to detect sub-provincial differences in these outcomes and are typically implemented every 2 to 5 years, making clear longitudinal trends difficult to assess. Additionally, in comparison to routine HMIS data, cross-sectional surveys are less granular, are unable to monitor short-term changes in malaria burden, and have limited use for real-time decision-making or subnational stratification.
Integrating malaria surveillance into routine antenatal care (ANC) visits has been proposed as a strategy to obtain representative data able to monitor population trends in malaria burden and intervention coverage in real time [9]. Continuous sentinel surveillance of pregnant women by testing them at their first scheduled antenatal care visit (ANC1) before they have received intermittent preventive treatment (IPTp) could be used to measure symptomatic and asymptomatic infections, provide data on spatial and temporal trends, add robustness to subnational geostatistical models, identify geographical areas with higher-than-average transmission intensity (“hot spots”), evaluate sustained changes in transmission following new interventions, and provide an early warning of increasing transmission. Women at ANC clinics could also participate in surveys about coverage, access, and use of malaria preventive tools, potentially allowing rapid assessments of intervention coverage, use, and progress in programme implementation, all with a higher degree of granularity and temporal resolution than household surveys.
Studies indicate that pregnant women attending ANC1 would be highly representative of the overall population of pregnant women where ANC attendance is high, and potentially representative of malaria prevalence in the broader population [9,10,11,12]. ANC coverage is high in sub-Saharan Africa, with an average of 72% of pregnant women attending at least one ANC visit in countries with moderate-to-high malaria transmission [3]. Monthly ANC attendance remains consistent over time, with less seasonal variation in attendance as compared to febrile visits to the outpatient department. Additionally, there is less correlation between the reason for attendance (ANC) and the outcome of interest (malaria) as compared to outpatient department attendance, where a large proportion of people present for evaluation of fever. Prevalence estimates using ANC1-based surveillance of all women regardless of symptoms would not be affected by rates of non-malarial febrile illness [13], which are likely to influence malaria test positivity rates obtained only from individuals with fever [14].
It has also been demonstrated that malaria prevalence among pregnant women correlates with the prevalence among children under 5 years of age and other populations [10,11,12, 15]. A systematic review and meta-analysis comparing prevalence of malaria infection in pregnant women to prevalence in children under five in the same region and during the same period showed a strong correlation between groups, with the strongest correlation between children under five and primigravid women [9]. In Tanzania, several studies have demonstrated a correlation between malaria prevalence in pregnant women attending ANC visits and other sources of prevalence estimates. In one study, data from 8 million pregnant women attending routine nationwide malaria screening at ANC1 before their first dose of IPTp were compared to data from 15,000 children under five, the latter being the total data from population-based household surveys in Tanzania in the equivalent time period. A strong positive correlation was found between the two indicators, with ANC data able to identify temporal and district-level trends well beyond the power of the survey data [12]. This suggests that ANC-based surveillance could be a highly cost-effective way to interpolate between survey data in both time and space toward the resolution needed for timely and tailored strategic action and allocation of resources [15].
While women attending ANC1 could be a pragmatic sentinel population for deriving granular and timely information on malaria burden, this measurement platform has not been thoroughly evaluated in multiple countries against current gold standard cross-sectional household surveys. This study leverages ongoing cross-sectional household surveys and contemporaneous ANC1 data collection to assess correlations and validate the use of ANC1 data to track monthly trends in malaria burden and intervention coverage, such as coverage and use of insecticide-treated nets and care seeking for febrile illness. In addition, where population denominator data are available, a secondary analysis will be conducted to look at the relationship between ANC1 malaria prevalence and malaria case incidence data derived from DHIS2.
This protocol provides a methodology and questionnaire for other national malaria control programs that may be interested in utilizing ANC1 surveillance to understand the pros and cons of using these data.
Objectives
The overall study objective is to assess the correlation between monthly malaria prevalence estimates obtained from ANC1-based surveillance and from cross-sectional household surveys assessing malaria prevalence among children under 5 years of age to validate the ANC1 surveillance approach as (a) representative of the metric of malaria prevalence reported by common household surveys and (b) useful for monitoring general trends in malaria burden and coverage of malaria control interventions over time.
Study outcomes
Primary outcome
-
1.
Monthly prevalence of rapid diagnostic test (RDT)-confirmed malaria infections among women at ANC1 (asymptomatic and symptomatic).
-
2.
Correlation at health facility and district level between malaria prevalence at the ANC1 (monthly or quarterly) and among children tested during cross-sectional household surveys.
Secondary outcomes
-
1.
Comparison of ANC1 data to cross-sectional household survey data to ascertain whether pregnant women attending ANC1 can be a sentinel population for estimating, both overall and by gravidity:
-
a.
Bed net ownership and use the previous night.
-
b.
Population access to bed nets (proportion of households achieving one net for every two people).
-
c.
Care-seeking behaviour for malaria.
-
a.
-
2.
Reported acceptability and feasibility of ANC1 malaria surveillance to women and providers.
-
3.
Relationship between ANC1 malaria prevalence and malaria case incidence derived from DHIS2 (where population denominator data are available).
Methods
Study design
This is a multi-country, observational, serial cross-sectional study with data from pregnant women attending ANC1 aggregated monthly. These data will be compared to similar survey questions (adapted from standard demographic health survey and malaria indicator survey questions) administered to households as part of cross-sectional surveys being conducted for evaluation of a number of different interventions (ClinicalTrials.gov Identifier: NCT04716387, NCT04157894, NCT04148690). Malaria prevalence by RDT among children under 5 years of age collected during the household surveys will also be compared to the prevalence among pregnant women at ANC1 in the same or a similar time period.
Study population
All pregnant women of legal age and emancipated minors attending ANC1 at selected health facilities in Benin, Burkina Faso, Mozambique, Nigeria, Tanzania, and Zambia are approached for enrollment (Table 1). In Mozambique and Nigeria only, pregnant women below the legal age are considered eligible with the consent of a legal guardian. Pregnant women with symptoms of severe disease as determined by the clinician at the ANC clinic are excluded and referred for urgent case management. Children under 5 years of age whose parents respond to the cross-sectional household survey and provide consent for malaria testing of their children are also included.
Study settings and location
This study is leveraging several planned intervention studies, including cross-sectional household surveys (modified malaria indicator surveys) at the district or village level that collect parasite prevalence data among children under 5 years (and other age groups as well, depending on country-specific epidemiology and national malaria control programme priorities). In Burkina Faso, Mozambique, and Nigeria, study activities are aligned with surveys from the New Nets Project, an observational quasi-experimental study that is evaluating the cost-effectiveness of various types of insecticide-treated nets [16]. During the New Nets Project, annual cross-sectional surveys are conducted from 2019 to 2022, including assessments of malaria prevalence, and corresponding ANC1-based surveillance occurs in a subset of health facilities in corresponding districts. Additionally, studies assessing the impact of group ANC are planned in the catchment areas of 40 health facilities each in Geita Region, Tanzania, and Atlantique Department, Benin, with corresponding cross-sectional surveys occurring as the primary method of evaluating the impact of the group ANC intervention. Due to the COVID-19 pandemic, the group intervention was stopped early in Tanzania, but the ANC1-based surveillance assessment and cross-sectional surveys continue. Cross-sectional surveys are conducted at study baseline and endline (November 2019 and June 2021 in Tanzania, February/March 2021 and September/October 2022 in Benin). In Chadiza, Zambia, this ANC1-based surveillance pilot leverages a study assessing the impact of proactive community case management in 21 health facility catchments, with surveys conducted in May 2021 and May 2023.
Health facility selection
Health facilities and their catchment areas are selected for participation in the parent studies according to the needs of each study; of these, health facilities with a minimum of 20 ANC1 per month are selected for co-inclusion in this ANC surveillance pilot. In some studies, all eligible health facilities are included, while in others a subset of eligible facilities are randomly selected for inclusion. Two activities are integrated into routine ANC1 consultations: malaria testing of eligible participants regardless of symptoms using an RDT, and administration of a questionnaire to collect data on participant demographics, gravidity, insecticide-treated net ownership and use, and care-seeking behaviour. For each facility, the corresponding catchment villages were identified in collaboration with the health facility workers. From among all the villages in the health facility catchment area, 1–2 villages or enumeration areas were selected for household sampling for the cross-sectional survey proportional to population size. The selected areas were mapped and respondents randomly selected as indicated by the parent study conducting the cross sectional survey.
ANC1 screening and enrollment
All pregnant women attending ANC1 are tested for malaria infection. During group counselling sessions at initial ANC1 intake, women are informed of this pilot surveillance activity. Women are consented for this pilot surveillance activity individually prior to testing. The number of women refusing malaria testing is noted on a screening form. For consenting women, a malaria RDT is administered concurrently with other routine ANC testing, using blood from the same finger prick. While awaiting the results from these tests, the short ANC surveillance questionnaire (Additional file 1) is administered by a trained study team or staff member, and the RDT result recorded when available. Women have the option of responding to the questionnaire even if they declined the RDT. During a regular ANC visit, the nurse asks questions to determine a woman’s age, gravidity, and gestational age. These data are recorded in the ANC registers and copied into the corresponding study questionnaires to avoid asking women the same questions twice. In Burkina Faso, Mozambique, and Zambia, a paid trained field worker assists with recruitment and administering the questionnaire while in the other countries, this task is completed by clinic staff.
Blood sample collection
As stated above, finger-prick capillary blood samples are collected for malaria diagnosis using malaria RDTs. The RDT used for both ANC1 surveillance and the cross-sectional household surveys is determined by national procurement protocols. For ANC1 surveillance, the blood used for malaria testing is taken from the same finger prick that is used to collect blood for standard ANC testing. If positive, treatment is given to the women according to the national guidelines for malaria treatment.
Sample size
A sample size of 88 people from a population of 1,000 people produces a two-sided 95% confidence interval with a precision (half-width) of 0.10 when the actual proportion is near 0.50. The sample size needed for a given confidence interval around a proportion is greatest for a proportion of 0.50. This is used to provide the most conservative assumption of sample size. The health facility sampling scheme is implemented across the different countries to provide a minimum of 88 women enrolled per month per sampling unit (i.e., health facility, district, or country), for a yearly total of 1,056 women per sampling unit. In cases where this sample size is not achieved in a single month at a given health facility, the data will be aggregated across facilities to provide a district/country estimate or across months to provide quarterly estimates to have sufficient sample size to provide an accurate estimate.
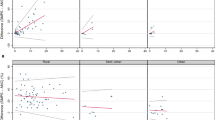
To calculate the correlation between the facility-level data and community-level data, an estimated minimum of 20 facilities is needed to provide an accurate estimate of the correlation coefficient (R), using a two-tailed alpha test (alpha 0.05) and with 80% power, assuming an expected correlation coefficient of 0.6 or greater (Fig. 1). This is not feasible across all individual countries, thus using the combined data from multiple countries aimed to ensure sufficient sample sizes to assess the correlation.
Data analysis and modelling
This study will summarize ANC1 participant demographic characteristics using descriptive statistics for age and gravidity by health facility and district. Key indicators will include:
-
Total women attending ANC1, and proportion enrolled in ANC1 surveillance.
-
Mean age of enrolled women (years; mean, 95% CI).
-
Number enrolled by gravidity (n, %) by gravida 1, gravida 2, and gravida 3 + .
Prevalence is calculated as the number of women with positive RDT results divided by the total number of women tested [11]. Within each health facility and district, prevalence will be disaggregated by gravidity relative to the current pregnancy (i.e., first pregnancy [gravida 1], second pregnancy [gravida 2], and third or more pregnancy [gravida 3 +]). The monthly malaria prevalence data will be used to produce time series graphs, quarterly and/or annually, for correlation with cross-sectional survey estimates. In addition, where available, the proportion of RDT-positive women who are asymptomatic and symptomatic will be calculated.
To compare ANC1 malaria prevalence to prevalence from cross-sectional surveys within the same district, ANC1 malaria prevalence are obtained for the three months surrounding the community cross-sectional surveys (i.e., the month before the cross-sectional survey, the month of the survey, and the month directly following the cross-sectional survey). The relationship between malaria prevalence at ANC1 and in the community will be quantified using mixed-effects logistic regression, accounting for likely modifiers such as age, gravidity, transmission intensity, and transmission season, and adjusting for sampling effort in time and space. To quantify the incremental value of the ANC1 data, the ability of the ANC1 data to predict population prevalence using these models will be tested using leave-one-out cross-validation for each district and compared to alternative predictive models in the absence of any ANC1 data (e.g., extrapolating district-level trends from other districts sampled within the region). With support of national malaria control programmes and operational partners, district-level data on the temporal distribution of interventions within each region will be leveraged to assess the utility of ANC1 data to capture plausible trends in intervention impact. Similar analyses will be conducted to quantify the relationship between the cross-sectional surveys, the ANC1 data, reported case incidence, and the malaria test-positivity rate (obtained by dividing the number of positive malaria tests by the number of tests performed). In addition, the use of more heuristic measures such as the Kendall correlation coefficient, which provides a summary of the extent to which prevalence ranking of each district remains constant over time [12], will be used to assess the extent to which the choice of malaria metric influences operational decision-making.
Estimates of care-seeking behaviors and indicators for bed net ownership, use, and access will be determined for ANC1 data and compared to the corresponding indicators from the cross-sectional surveys. Net use and ownership (proportion of households that own at least one bed net and proportion of households with one net for every two people) will be aggregated monthly for each sampling unit/district and correlated with monthly ANC1 malaria prevalence to compare trends.
Once an optimal predictive model of community prevalence using ANC1 data has been obtained, this relationship will be incorporated within an existing, well-established mechanistic model of malaria transmission [17,18,19] in an attempt to provide a framework that can convert estimates of ANC1 malaria prevalence into continuous measures of community malaria transmission and burden with which to explore future intervention scenarios (analogous to a current framework that involves calibrating to cross-sectional data [20]).
Data management
Data will be obtained from separately generated electronic or paper registers in each country. At each health facility, teams will be trained to conduct data quality assessments to monitor and improve data quality and completeness. Health facility–level ANC1 data from the DHIS2 system will include the monthly number of ANC attendees, the number tested for malaria at ANC1, and the number positive for malaria. Additional data will be collected on maternal age, gravidity, and insecticide-treated net ownership and utilization. Data on malaria prevalence among children will be obtained from representative, cross-sectional, household surveys as specified in the parent studies. Participants will be assigned a unique identifier number by the study, and will be identified only by this number in the dataset. No participant names or other information that would make the participant identifiable will be included.
Consent
Individual written consent is obtained from women of legal age prior to testing and questionnaire administration during ANC1. In Mozambique and Nigeria, women under legal age are able to participate with the consent of their parent or legal guardian. Participants are told the general purpose, possible risks, and benefits of the ANC1 pilot surveillance activity in the local language. Participation is voluntary.
Ethical clearance
Ethical clearance for the study was sought and obtained from the following institutional review boards:
-
Comité d’Ethique de La Recherche de l’ISBA, Institut des Sciences Biomédicales Appliquées (Benin).
-
PATH Research Ethics Committee (Burkina Faso, Mozambique, Zambia).
-
Centre National de Recherche et de Formation sur le Paludisme (Burkina Faso).
-
Comité d’Ethique pour la Recherche en Santé (Burkina Faso).
-
Comité Institucional de Bioética para Saúde (Mozambique).
-
National Health Research Ethics Committee of Nigeria (Nigeria).
-
World Health Organization Research Ethics Review Committee (Nigeria).
-
Medical Research Coordination Committee of the National Institute for Medical Research (Tanzania).
-
National Health Research Ethics Committee (Zambia).
In addition, this activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.
Discussion
This work builds on previous work assessing the validity of using pregnant women attending ANC1 as a sentinel population for monitoring malaria prevalence over time [10, 12]. In the present expanded observational study, ANC1-based surveillance collects additional data on indicators of bed net access and use and care-seeking behavior, information that is not collected in routine HMIS settings. The results generated from this study will be used to validate how reliably data collected during routine ANC visits can be used for malaria surveillance in malaria-endemic regions of sub-Saharan Africa.
Public health importance of ANC-based malaria surveillance
In sub-Saharan Africa, approximately 72% of pregnant women attend ANC at least once during pregnancy [3], even in many rural areas where health care is not easily obtained. Malaria prevalence estimates from ANC1 attendees (before administration of IPTp) could, therefore, prove useful for monitoring changes in malaria transmission over time. ANC1-based surveillance could provide real-time, weekly or monthly data on malaria trends as well as information on access to control interventions such as ownership and use of insecticide-treated bed nets at the district and health facility level, which is sometimes missed in routine HMISs. Subtle changes in trends like early epidemics may be detectible, allowing more timely responses from malaria control programmes.
ANC1-based surveillance offers a basis for targeting malaria control interventions and resource allocation depending on local transmission levels [11]. As malaria transmission continues to decline and infections become more heterogeneous [21] in some settings, ANC1-based surveillance can be used as an adjunct for malaria elimination activities by identifying foci of residual transmission not captured by case-based passive surveillance or cross-sectional surveys. Where funding is available, molecular analysis of Plasmodium isolates from pregnant women may characterize genetic signatures of malaria transmission intensity, anti-malarial resistance, and detection of deletions of antigens targeted by RDTs [22, 23] in a way that is easily obtained yet representative of the general population.
How results will be used
Routine malaria testing of all ANC1 attendees irrespective of symptoms potentially improves pregnancy outcomes by testing and treating women with asymptomatic but detectable parasitaemia. The results generated will add to existing knowledge and evidence that supports use of women attending ANC1 as a pragmatic sentinel (Additional file 1) population for malaria surveillance. The present study will continue to expand the evidence base generated by studies characterizing the relationship between malaria infection in pregnant women and in children in the same communities [9] across new locations and various transmission settings. Geospatial and temporal mapping of infection prevalence by village and/or health facility may also reveal specific hot spots [11].
Challenges
ANC1-based surveillance requires strengthening systems for routine data collection and changing data management and reporting procedures, as ANC registers would need to include additional fields such as questions on insecticide-treated net use and care-seeking, which are not typically recorded. Routinely aggregated data such as women’s age and gravidity would need to be included at an individual level to optimize analysis of prevalence trends. To be most useful, data would need to be collected and reviewed in near real-time, which can be a challenge. Scaling ANC1-based surveillance requires investment in the capacity of midwives, which would involve training on revised policy guidelines to test and treat all women, increasing the number of midwives to support malaria testing, and/or identification of other cadres of workers who can assist in collecting this information. While theoretically, universal malaria testing at ANC1 could increase the duration of the appointment or disrupt patient flow, studies assessing the feasibility have not found this to be the case [24,25,26,27]. Increased funding would be required to ensure that health facilities have sufficient RDTs for universal testing and to avoid stockouts of antimalarial treatments. Funding would also need to support modification of HMISs to distinguish between positive infections in women being tested routinely at ANC1 from symptomatic pregnant women tested during unscheduled visits or those later in pregnancy.
Study limitations
Using ANC1 for malaria surveillance depends on the extent to which pregnant women attend public ANC clinics, which is affected by nonattendance or attendance at private ANC clinics, among other factors. In countries where attendance at private ANC clinics is high, or if variations exist among rural and urban areas, underrepresentation of private clinics in the surveillance system could introduce selection bias if populations of pregnant women attending private and public ANC clinics differ with regard to malaria exposure [15]. Because private facilities are more commonly located in urban settings, where malaria risk is generally lower, ANC1 data may not be fully representative of the population. Similarly, areas with poor access to health facilities in general may be more likely to be rural and have higher malaria prevalence; this could induce bias if women who present for care are in the areas with lower prevalence. Additionally, bias may arise at screening, particularly if RDTs are limited, if symptomatic women are preferentially tested. Finally, while health facilities have defined catchment areas, people may, to varying extent, choose to seek care outside of their defined health facility. Defining catchment areas strictly is a complex task for many surveillance indicators [28], including malaria case metrics [29]. As data are aggregated upward to larger areas, i.e., districts rather than specific health facility catchments, the effect of people’s movement is likely diminished. To better account for movement of people outside of their designated catchment areas, one could collect data on where people reside; this was done in Zambia where it was recognized that many of the women seeking care in border facilities might have crossed over from Mozambique, allowing for exclusion of these women from the comparison with the household survey data.
Conclusions
ANC1-based surveillance offers the potential of a lower-cost, more granular, and potentially more representative measure of community malaria burden and other indicators typically sought through cross-sectional surveys. While there are numerous potential benefits of this method of malaria surveillance, it needs to be rigorously validated across a range of settings, particularly with respect to measuring coverage indicators for malaria control measures. As with many routine data collection efforts, post-validation challenges would remain, not the least of which would be ensuring adequate stock of commodities, expanded training requirements, register modifications, and policy changes.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANC:
-
Antenatal care
- ANC1:
-
First antenatal care visit
- DHIS2:
-
District Health Information Software 2
- HMIS:
-
Health management information system
- IPTp:
-
Intermittent preventive treatment in pregnancy
- RDT:
-
Rapid diagnostic test
References
Accrombessi M, Issifou S. Malaria control and elimination in sub-Saharan Africa: data from antenatal care centres. Lancet Glob Health. 2019;7:e1595–6.
WHO. World malaria report 2021. Geneva: World Health Organization; 2021.
WHO. World malaria report 2022. Geneva: World Health Organization; 2022.
WHO. Global technical strategy for malaria 2016–2030. Geneva: World Health Organization; 2015.
Lindblade KA, Steinhardt L, Samuels A, Kachur SP, Slutsker L. The silent threat: asymptomatic parasitemia and malaria transmission. Expert Rev Anti Infect. 2014;11:623–39.
Rogerson SJ, Desai M, Mayor A, Sicuri E, Taylor SM, van Eijk AM. Burden, pathology, and costs of malaria in pregnancy: new developments for an old problem. Lancet Infect Dis. 2018;18:e107–18.
Bousema T, Okell L, Felger I, Drakeley C. Asymptomatic malaria infections: detectability, transmissibility and public health relevance. Nat Rev Microbiol. 2014;12:833–40.
Weiss DJ, Lucas TCD, Nguyen M, Nandi AK, Bisanzio D, Battle KE, et al. Mapping the global prevalence, incidence, and mortality of Plasmodium falciparum, 2000–17: a spatial and temporal modelling study. Lancet. 2019;394:322–31.
van Eijk AM, Hill J, Noor AM, Snow RW, ter Kuile FO. Prevalence of malaria infection in pregnant women compared with children for tracking malaria transmission in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health. 2015;3:e617–28.
Brunner NC, Chacky F, Mandike R, Mohamed A, Runge M, Thawer SG, et al. The potential of pregnant women as a sentinel population for malaria surveillance. Malar J. 2019;18:370.
Willilo RA, Molteni F, Mandike R, Mugalura FE, Mutafungwa A, Thadeo A, et al. Pregnant women and infants as sentinel populations to monitor prevalence of malaria: results of pilot study in Lake Zone of Tanzania. Malar J. 2016;15:392.
Kitojo C, Gutman JR, Chacky F, Kigadye E, Mkude S, Mandike R, et al. Estimating malaria burden among pregnant women using data from antenatal care centres in Tanzania: a population-based study. Lancet Glob Health. 2019;7:e1695–705.
Dalrymple U, Cameron E, Bhatt S, Weiss DJ, Gupta S, Gething PW. Quantifying the contribution of Plasmodium falciparum malaria to febrile illness amongst African children. Elife. 2017;6: e29198.
Francis D, Gasasira A, Kigozi R, Kigozi S, Nasr S, Kamya MR, et al. Health facility-based malaria surveillance: the effects of age, area of residence and diagnostics on test positivity rates. Malar J. 2012;11:229.
Hellewell J, Walker P, Ghani A, Rao B, Churcher TS. Using ante-natal clinic prevalence data to monitor temporal changes in malaria incidence in a humanitarian setting in the Democratic Republic of Congo. Malar J. 2018;17:312.
Gansané A, Candrinho B, Mbituyumuremyi A, Uhomoibhi P, NFalé S, Mohammed AB, et al. Design and methods for a quasi-experimental pilot study to evaluate the impact of dual active ingredient insecticide-treated nets on malaria burden in five regions in sub-Saharan Africa. Malar J. 2022;21:19.
Griffin JT, Ferguson NM, Ghani AC. Estimates of the changing age-burden of Plasmodium falciparum malaria disease in sub-Saharan Africa. Nat Commun. 2014;5:3136.
Patouillard E, Griffin J, Bhatt S, Ghani A, Cibulskis R. Global investment targets for malaria control and elimination between 2016 and 2030. BMJ Glob Health. 2017;2: e000176.
Walker PGT, Cairns M, Slater H, Gutman J, Kayentao K, Williams JE, et al. Modelling the incremental benefit of introducing malaria screening strategies to antenatal care in Africa. Nat Commun. 2020;11:3799.
Charles G, Winskill P, Topazian H, Challenger J, Fitzjohn R. malariasimulation: an individual based model for malaria, R package version 1.4.1: matching PfPR2–10 to EIR. 2022. https://mrc-ide.github.io/malariasimulation/articles/EIRprevmatch.html. Accessed 15 Dec 2022.
WHO. Malaria surveillance, monitoring & evaluation: a reference manual. Geneva: World Health Organization; 2018.
Daniels RF, Schaffner SF, Wenger EA, Proctor JL, Chang H-H, Wong W, et al. Modeling malaria genomics reveals transmission decline and rebound in Senegal. Proc Natl Acad Sci USA. 2015;112:7067–72.
Cheng Q, Gatton ML, Barnwell J, Chiodini P, McCarthy J, Bell D, et al. Plasmodium falciparum parasites lacking histidine-rich protein 2 and 3: a review and recommendations for accurate reporting. Malar J. 2014;13:283.
Hoyt J, Hill J, Achieng F, Ouma P, Kariuki S, Desai M, et al. Healthcare provider and pregnant women’s perspectives on the implementation of intermittent screening and treatment with dihydroartemisinin-piperaquine for malaria in pregnancy in western Kenya: a qualitative study. Malar J. 2021;20:291.
Hoyt J, Landuwulang CUR, Ansariadi AR, Burdam FH, Bonsapia I, et al. Intermittent screening and treatment or intermittent preventive treatment compared to current policy of single screening and treatment for the prevention of malaria in pregnancy in eastern Indonesia: acceptability among health providers and pregnant women. Malaria J. 2018;17:341.
Young N, Achieng F, Desai M, Phillips-Howard P, Hill J, Aol G, et al. Integrated point-of-care testing (POCT) for HIV, syphilis, malaria and anaemia at antenatal facilities in western Kenya: a qualitative study exploring end-users’ perspectives of appropriateness, acceptability and feasibility. BMC Health Serv Res. 2019;19:74.
Hill J, Ouma P, Oluoch S, Bruce J, Kariuki S, Desai M, et al. Intermittent screening and treatment with dihydroartemisinin-piperaquine for the prevention of malaria in pregnancy: implementation feasibility in a routine healthcare system setting in western Kenya. Malar J. 2020;19:433.
Macharia PM, Ray N, Giorgi E, Okiro EA, Snow RW. Defining service catchment areas in low-resource settings. BMJ Glob Health. 2021;6: e006381.
Cameron E, Young AJ, Twohig KA, Pothin E, Bhavnani D, Dismer A, et al. Mapping the endemicity and seasonality of clinical malaria for intervention targeting in Haiti using routine case data. ELife. 2021;10: e62122.
Disclaimer
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the US Centers for Disease Control and Prevention or the US Agency for International Development.
Acknowledgements
All authors would like to acknowledge the contribution of many study team members of national malaria programs, Centre National de Recherche et de Formation sur le Paludisme (Burkina Faso), Ibolda Health International (Nigeria), and Tropical Health Consulting (Mozambique). In addition, we would like to thank funders and collaborators on the New Nets Project (The Global Fund to Fight AIDS, Tuberculosis and Malaria; Unitaid), and Program for the Advancement of Malaria Outcomes (US Agency for International Development).
Funding
Financial support for this study was provided in part by the US President's Malaria Initiative. Study activities in Burkina Faso and Mozambique were funded by the Bill & Melinda Gates Foundation (INV-003761). Study activities in Nigeria were partially supported by the Global Fund to Fight AIDS, Tuberculosis and Malaria through its grant to the National Malaria Elimination Programme.
Author information
Authors and Affiliations
Contributions
JG and MR conceived and developed the original study design with adaptations and inputs from JM, CK, RZ, KSG, PW, BC, AG, PU, OOO, and JW. JNM, JG, MR, and KA wrote the manuscript draft and all authors contributed to the revision and editing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance for this study was sought and obtained from Comite d'Ethique de La Recherche de l'ISBA, Institut des Sciences Biomédicales Appliquées (Benin); PATH Research Ethics Committee (Burkina Faso, Mozambique, Zambia); Centre National de Recherche et de Formation sur le Paludisme (Burkina Faso); Comité d’Ethique pour la Recherche en Santé (Burkina Faso); Comité Institucional de Bioética para Saúde (Mozambique); National Health Research Ethics Committee of Nigeria (Nigeria); World Health Organization Research Ethics Review Committee (Nigeria); Medical Research Coordination Committee of the National Institute for Medical Research (Tanzania); and National Health Research Ethics Committee (Zambia). This activity was reviewed by the US Centers for Disease Control and Prevention (CDC) and was conducted consistent with applicable US federal law and CDC policy. Data from this study will be compared to similar survey questions (adapted from standard demographic health surveys/malaria indicator surveys) administered to households as part of cross-sectional surveys being conducted for evaluation of a number of different interventions. These evaluations are registered at ClinicalTrials.gov (http://www.clinicaltrials.gov) under registration numbers NCT04716387, NCT04157894, NCT04148690.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
ANC1 Surveillance Questions.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gutman, J.R., Mwesigwa, J.N., Arnett, K. et al. Using antenatal care as a platform for malaria surveillance data collection: study protocol. Malar J 22, 99 (2023). https://doi.org/10.1186/s12936-023-04521-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-023-04521-6