Abstract
Kalimantan is a part of Indonesia, which occupies the southern three-quarters of the island of Borneo, sharing a border with the Malaysian states of Sabah and Sarawak. Although most areas of Kalimantan have low and stable transmission of Plasmodium falciparum and Plasmodium vivax, there are relatively high case numbers in the province of East Kalimantan. Two aspects of malaria endemicity in Kalimantan differentiate it from the rest of Indonesia, namely recent deforestation and potential exposure to the zoonotic malaria caused by Plasmodium knowlesi that occurs in relatively large numbers in adjacent Malaysian Borneo. In the present review, the history of malaria and its current epidemiology in Kalimantan are examined, including control and eradication efforts over the past two centuries, mosquito vector prevalence, anti-malarial use and parasite resistance, and the available data from case reports of knowlesi malaria and the presence of conditions which would support transmission of this zoonotic infection.
Similar content being viewed by others
Background
Indonesia, the fourth most populated country and occupying most of the largest archipelago in the world, had an estimated 800,000 malaria cases in 2021 according to the latest World Health Organization (WHO) report, the second highest number in South-east Asia after India [1]. Although the Indonesian government has targeted malaria elimination by 2030 [2], case numbers have remained relatively stable over the past 5 years [3]. Approximately 130 million Indonesians live in high risk regions [3,4,5], but the geographical distribution of transmission is highly heterogeneous [4]. Of the 514 districts and municipalities of Indonesia, 351 (68.3%) were certified free of malaria in 2022 [6]. In the remainder, and based on the most complete estimates, the prevalence varies from 0.02 to 12.07% [7]. Even though the majority of provinces have hypoendemic to mesoendemic malaria [3, 8], there is relatively intense transmission in eastern Indonesia [7, 9] including parts of Indonesian Borneo (Kalimantan) [7, 10].
Kalimantan occupies the southern three-quarters of the island of Borneo (Fig. 1). In the north, it shares a border with the Malaysian Borneo states of Sabah and Sarawak. Most areas of Kalimantan have low and stable transmission of the dominant Plasmodium species, Plasmodium falciparum and Plasmodium vivax [11]. The average Annual Parasite Index (API; number of positive cases per 1000 individuals in a year) is below 0.15 except for relatively high transmission areas in East Kalimantan [2, 11]. There are two aspects of malaria endemicity in Kalimantan that differentiate it from the rest of Indonesia. First, although the island of Borneo has one of the largest remaining forested areas in South-east Asia, about a third of Borneo has been deforested in the last 50 years [12] which, with increasing urbanization and climate change [13], has the potential to impact malaria transmission. Second, the zoonotic malaria caused by Plasmodium knowlesi is widespread in South-east Asia [14] and there are relatively large numbers of cases in both Sarawak [15,16,17,18] and Sabah [19,20,21]. Although P. knowlesi is the predominant cause of human malaria in Malaysian Borneo [22, 23], very few cases have been reported from Kalimantan despite its geographical proximity and shared ecologies.
Given this background, the aim of the present narrative review was to detail the recent history of malaria in Kalimantan including cases of P. knowlesi, and to examine geo-epidemiological trends that are likely to influence future malaria transmission in this large Indonesian territory.
Methods
The present systematic review was conducted according to PRISMA 2020 guidelines [24]. A publication search was performed in PubMed (MEDLINE) and the Indonesian repository site www.neliti.com using the keywords “malaria + Kalimantan + Indonesia” and “plasmodium + Kalimantan”. The references cited in all eligible publications were reviewed to identify relevant articles that had been missed in the initial search. Supplementary malaria data were obtained from reports of Provincial Health Department compiled from monthly reports of Health Centres at village to sub-district and from sub-district to district level. Information on Anopheles vectors was collected from identified publications, and government and Global Fund reports. Information regarding malaria control measures in Kalimantan was collected from the provincial Health Department and personal communication with malaria officers.
Geographical situation and population
Kalimantan is located at 1S 114°E, has a total area of 539,238 square km [25], and is crossed by the equator [25] (Fig. 1). It is connected to Malaysian Borneo by roads from West, East and North Kalimantan. About 77% of Kalimantan is state forest land, including a million hectares of peat land where a large portion of primary rainforest has been converted to palm-oil plantations and timber logging areas [26]. The total population in 2021 was 16.8 million (representing approximately 6% of the total Indonesian population) with most inhabitants aged between 15 and 50 years [27]. The average annual population growth rate was 2.12% in 2020 [27].
Kalimantan consists of five provinces (propinsi) (Fig. 1): Central Kalimantan (Kalimantan Tengah, capital city Palangkaraya, area 154,000 km2, population 2.65 million), East Kalimantan (Kalimantan Timur, capital city Samarinda, area 127,300 km2, population 3.72 million), North Kalimantan (Kalimantan Utara, capital city Tanjung Selor, area 154,000 km2, population 0.072 million), South Kalimantan (Kalimantan Selatan, capital city Banjarbaru, area 38,700 km2, population 4.31 million), and West Kalimantan (Kalimantan Barat, capital city Pontianak, area 147.300 km2, population 5.07 million) [25, 27, 28]. Most of the population engages in agricultural and forest-related industries, but other economic activities include mining, fisheries, government agencies and trade [27].
History of malaria in Kalimantan
Early reports of malaria
Dutch traders arrived in Indonesia in the late 16th Century and the Dutch colonized the archipelago over the next two centuries. Early letters and reports from Dutch traders indicated that a certain type fever, very likely malaria, was a significant health problem affecting military activity and trade [29]. As the Indonesian central government and the administration of the Dutch East Indies Company (Vereenigde Oost-Indische Company; VOC) were located on the island of Java, most early Indonesian malaria-related publications were from Java. These included a cross-sectional comparison of malaria prevalence and parasite density in two major cities [30] and a subsequent study in the 18th Century in Batavia (now Jakarta, the country’s capital) that showed high morbidity from tertian or continual fevers that claimed thousands of VOC employees’ lives each year [31]. In a report to the German Colonial Office in 1899, Robert Koch investigated aspects of malaria in adults, (including military hospitals) and children in Java [30, 32]. Subsequently, the Netherland East Indies ‘ethical policy’ (ethische politiek) that was meant to improve the welfare of indigenous Indonesians through irrigation, transmigration and education inadvertently ignited malaria outbreaks in Java in the first 30 years of the 20th Century by increasing transmission [33, 34].
Indonesian Borneo has been occupied by Dayak tribes since 242 BC and was colonized by Hindu, Buddhist and Muslim kingdoms over the following centuries before the arrival of European settlers [35]. Although it is likely that malaria was present in Kalimantan since the beginning of human settlement, documentation is sparse. Chinese merchants trading in South Kalimantan in 1660 declined the Sultan of Banjarmasin’s demand to work in the non-tidal zone of Martapura rather than in their usual location at Old Banjar due the possibility of contracting fatal ‘hot fevers’ [36, 37]. In 1786, many Dutch soldiers developed ‘febris intermittens’ during the first military intervention inland from Banjarmasin, and this malady was encountered repeatedly in subsequent military missions [37]. Dutch military health service reports from Kalimantan in 1860 indicated that approximately 20% of the patients in coastal city hospitals were suspected to suffer from malaria compared to almost 50% in inland hospitals [36, 37], highlighting the lower case load in tidal coastal zones compared to forested areas. However, during early European settlement, Kalimantan was considered as a relatively healthy place according to the first European explorer Schwaner in 1853 [38], presumably because intense malaria transmission was limited in the small, dispersed agricultural communities [36].
The first formal report of malaria in Kalimantan in the published medical literature was written by the Dutch physician Nieuwenhuis [36, 39]. While working in Sambas, West Kalimantan, between 1894 and 1898, he argued that malaria was more prevalent at higher altitudes and in sandy areas. He found only 6 malaria cases out of 2,103 children living on the alluvial plain compared to almost all (403 out of 420) children from the hilly inland area. This difference was suggested subsequently to be due to fluctuating tides and salinity adversely affected breeding of Anopheles sundaicus and Anopheles beazai mosquito vectors in low lying areas [40]. There were exceptions to Nieuwenhuis’ observations, however, in that the Apo-Kayan villages in hilly areas had a low incidence of malaria [41] while the nomadic tribes remained virtually malaria free [42]. For this latter group, their mobility was thought to inhibit the development of foci of local transmission [42]. In the case of the Apo-Kayan, it was suggested that habitation at high altitude and at a relatively low temperature, as well as the cultivation of dry rice, did not favour mosquito breeding [39, 43]. Nevertheless, population movement from coastal areas to the interior resulted in an increased incidence of malaria in the early 19th Century, a situation that is still relevant for malaria epidemiology in Kalimantan two centuries later.
Prevention and treatment timelines
The first drug used widely for both malaria treatment and prophylaxis was quinine, a short-acting alkaloid extracted from the bark of the cinchona tree that is native to South America [44, 45]. It was introduced in the 19th Century and Dutch cinchona plantations in Java became the most successful globally [46]. Indeed, the Dutch had a near monopoly on the supply of quinine and the Bandoengsche Kininefabriek company was the biggest quinine producer in the world in 1924 [47]. The drug had a significant role during the Second World War as the loss of soldiers due to malaria was greater than war-related injuries [48]. Worldwide quinine production diminished substantially after the Japanese Imperial Army invaded and occupied Indonesia in 1942. Chloroquine was synthesized in Germany in the 1930s as resochin and a wartime American effort saw it registered in 1946 as a less expensive, safer, and better tolerated therapy of acute malaria. Plantation-dependent quinine subsequently declined significantly because of a lack of demand [49].
In the mid-19th Century, a restricted amount of quinine was brought by the Dutch to coastal towns in Kalimantan at a time when native Bornean people employed various non-pharmacological ways of preventing and remedying the disease [36, 50]. The indigenous Dayaks built their longhouses on stilts above the maximum vertical flight range of mosquitoes, separated their villages by distances exceeding the horizontal flight range, and produced smoke around the house that deterred mosquito bites [36, 51, 52]. Domesticated animals such as pigs, cows and goats provided a degree of zooprophylaxis [42, 53]. Moreover, the animals also disturbed local water sources which inhibited mosquito breeding [54]. When Dayaks contracted fever, they applied cold bath rituals and took traditional medicines that had some anti-malarial activity [55,56,57]. Nevertheless, the estimated malaria-associated death rate did not change after the introduction of quinine [31, 36], suggesting that its distribution did not reach the interior of Kalimantan.
In the pre-Independence era (before 1945), a specific vector control strategy was implemented in Indonesia with beneficial results [58]. This was called ‘species sanitation’ by Swellengrebel [59], a Dutch physician, and consisted of ‘a naturalistic approach of vector control, directed against the main vectors, through modification of the habitat in such a way that the vectors avoid these areas’ [40, 60]. In North Sumatra, for example, drainage of fish ponds, the main breeding site for An. sundaicus, reduced local spleen rates from > 90 to 10% [61]. Another example was from West Java, where synchronized rice planting and harvesting attenuated Anopheles aconitus breeding in rice paddies and drainage ditches, and decreased malaria transmission to the point where it was no longer a significant health problem in contrast to other parts of the country. Species sanitation was facilitated by documentation of region-specific vector prevalence, starting with Swellengrebel in 1919 [62] and updated by Soesilo in 1936 [40, 63]. In areas of Kalimantan where the main malaria vectors were known (Table 1), malaria outbreaks were successfully managed using this approach.
After Independence, the newly established Indonesian Ministry of Health recognized the social and economic impact of malaria which was a threat to over a third of the population [64]. New control efforts were implemented based on widespread use of insecticides (including dichloro-diphenyl-trichlorethane (DDT) and dieldrin) and chloroquine. In parts of Indonesia other than Kalimantan such as Java, South Sumatra, Northern Central Sulawesi and Maluku [65,66,67], DDT spraying was introduced along with mass chloroquine treatment [68]. DDT control of An. aconitus, Anopheles subpictus and An. sundaicus [69] led to a marked reduction in malaria hospitalizations in Java, Sumatra and Sulawesi [70]. Unfortunately, the targeted effect of the species sanitation approach on mosquito vectors contrasted with the potentially devastating impact of DDT spraying on local insect populations. Kalimantan did not have the same degree of wet agriculture as other areas of Indonesia and so was not initially included in the new control programme.
Supported by the WHO and United States Agency for International Development, the Indonesian Government next launched a malaria eradication programme between 1959 and 1968 which was still based on the use of DDT and chloroquine [71]. This strategy became increasingly ineffective because malaria parasites developed resistance to chloroquine monotherapy and mosquitoes became tolerant or resistant to DDT and dieldrin, against a background of financial restraints as well as political unrest in the mid-1960s [40]. The WHO effectively abandoned eradication as a goal in 1969 [72]. From 1969 to 1999, the eradication programme in Indonesia was replaced by a malaria control programme under the Indonesian Directorate General of Communicable Disease Control. Due to population density and economic considerations, the programme focused heavily on Java and Bali. Malaria control in Kalimantan consisted solely of passive case detection at village level Public Health Centres (PHCs) and malariometric surveys in provinces where there was high rates of migration and new economic development projects. Chemoprophylaxis was reserved only for visitors and migrants to Kalimantan, and primaquine was not available to reduce the burden of P. vivax infection [7, 11].
The malaria control programme of 1969–1999 reduced the incidence of malaria significantly in western Indonesia but challenges remained in the outer islands including Kalimantan due to poor infrastructure, limited human resources and logistic difficulties in accessing at-risk populations. In 2000, the strategy changed to a Roll Back Malaria campaign with case mapping, identification of foci of transmission, and tailoring of interventions to local needs [2, 7]. A particular aim was to minimize the gap between western and eastern Indonesia and to achieve staged elimination for the whole country [9]. For Kalimantan, elimination by 2020 was planned [8]. In recent years, the numbers of malaria cases in Kalimantan, apart from East Kalimantan, have been generally low [11], but the emergence of P. knowlesi in neighbouring Sabah and Sarawak demonstrate a potential new threat to Indonesia’s aspirations for malaria elimination [73].
Prevalence of malaria in Kalimantan
After the landmark epidemiological studies of Nieuwenhuis in the late 1800s [74], subsequent reports of malaria prevalence in Kalimantan were from West Kalimantan in the 1970s at a time when the logging industry was flourishing [75]. The first formal scientific assessment of malaria in Kalimantan was published at this time as a part of wider parasitological survey of the Indonesian archipelago [76]. Of 5773 samples taken in 15 villages, slide positivity rates (SPRs) were between 4.4% [76] and 5.6% [77]. Most cases were in children and young adults, and the infecting species were P. vivax (predominant), P. falciparum, or both. In Central Kalimantan in the 1980s, malaria was found in forest workers in two logging companies with SPRs of 7.9% and 14.5% [78]. In East Kalimantan, the SPR in Atap village was 59.7% (P. falciparum in all 94 cases including one mixed infection with P. vivax) in 2008, and the SPR in Lubakan village at around the same time was 97.3% (by contrast, all but one of 183 cases were P. vivax) [79]. In South Kalimantan, data from PHCs at Muara Uya and Santuun showed the predominant species to be P. falciparum (79% at Muara Uya and 44% at Santuun) followed by P. vivax (10% and 23% respectively) with mixed P. falciparum/P. vivax infections accounting for the remainder [80]. In South Kalimantan, a survey of people living near cattle sheds showed 12% P. falciparum and 88% P. vivax amongst a total of 235 cases [81]. In four villages in Nunukan, East Borneo, an area bordering Malaysian Borneo, SPRs varied from 0.9 to 5.60%, all P. falciparum [82], although mixed infections with P. vivax have also been found in this area [79]. A mass blood survey and passive case detection in forested areas of Central and South Kalimantan revealed SPRs between 1.4% and 3.0%, with Plasmodium malariae identified in addition to P. falciparum and P. vivax [83]. In Kotabaru [84] and Tanah Bumbu districts [85], South Kalimantan, active mass blood surveys found SPRs of 23.0% and 1.4%, respectively, with P. falciparum, P. vivax and some mixed P. falciparum/P. vivax infections.
These data, from a variety of sources published between 1975 and 2005, and utilizing a range of epidemiological survey methods at 17 locations generating 7,367 blood film examinations, show that (i) the SPR is heterogeneous between and within the provinces of Kalimantan, ranging from low level transmission (< 6.0%) in parts of South, East, West and Central Kalimantan to very high (> 50%) in areas of East Kalimantan (there are no published data from North Kalimantan), (ii) although overall P. falciparum is the predominant infecting species (5.4% of all blood film examinations [7, 76, 86,87,88]), P. vivax is also regularly encountered (3.4%) alone and in a small minority of mixed infections with P. falciparum, and a few (0.3%) P. malariae infections have been reported, and (iii) although no cases of P. knowlesi have been detected in the publications reviewed (which does not include case reports, as detailed below), it is possible that this parasite has been misdiagnosed by microscopy not only as P. malariae since the blood stages of these two species have similar morphology but also as P. falciparum or P. vivax, as observed previously in Malaysian Borneo [18, 89, 90].
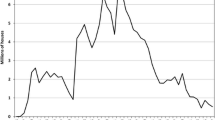
To obtain contemporary estimates of malaria prevalence, unpublished data from the Indonesian Health Department were obtained to complement limited published sources. These are summarized in Tables 2 and 3, and in Fig. 2, and confirm that the highest transmission is in East Kalimantan. The case numbers appear stable (allowing for partial data in 2021) over the last 4 years. There is a slight predominance of P. vivax over P. falciparum, a relatively small number of cases of P. malariae (which given the rarity of testing by PCR, as noted as above, may be P. knowlesi) and single cases of Plasmodium ovale and P. knowlesi (the latter presumably having been confirmed by PCR). Most cases are in adult males, consistent with occupational exposure through agriculture and forest-related activities [27, 91].
Mosquito vectors in Kalimantan
The first published literature on mosquito vectors in Kalimantan appeared during the implementation of the species sanitation control strategy in the early twentieth century. The Dutch physician Swellengrebel pioneered the identification of Indonesian anopheline mosquitoes in 1919 [62] and described Anopheles roperi and Anopheles letifer in Sanggau, West Kalimantan in 1921 and 1932 [40]. The recognition of Anopheles barbirostris as an important vector species in Sumatra, Java and Kalimantan, and the introduction of water vegetation-eating fish Puntius javanicus as an effective measure against water surface plant-loving mosquitoes by Walch followed in 1935 [58]. Indonesian physician Soesilo compiled an updated list of vectors in 1936 [63] which has proved a valuable tool in reducing the burden of malaria in endemic areas of Indonesia including Kalimantan [58] (Table 1).
A more recent 1987 study of Anopheles mosquitoes collected in South Kalimantan using human bait determined that Anopheles leucosphyrus and Anopheles balabacensis (97.7% of the 217 female specimens) were malaria vectors, with sporozoite infection rates of 1.0% and 1.3%, respectively [92]. A subsequent study used malaria case mapping and examined mosquito vector species and habitats in Sebatik Island in East Kalimantan in 2009. An. balabacensis, An. sundaicus and Anopheles maculatus were identified as vectors, while An. balabacensis and An. maculatus were found to be resistant to the insecticides permethrin and lambdacyhalothrin, and tolerant to malathion [82]. In 2012, in a study of the efficacy of vector control strategies in Nunukan, East Kalimantan [93], the habitat characteristics of Anopheles spp. larvae indicated that potential breeding places were dominated by fish ponds with stagnant water and muddy substrate, located around settlements and surrounded by grasses, shrubs and trees [94]. Another vector identification study in Sebatik Island, North Kalimantan, revealed that Anopheles vagus, An. sundaicus and An. subpictus were the most abundant species caught and that both Anopheles peditaeniatus and An. sundaicus were P. falciparum vectors [95]. A mosquito survey in Kotabaru using nested PCR assays found that P. vivax was present in Anopheles vagus, An. peditaeniatus and Anopheles tesselatus, indicating that they were new malaria vectors in South Kalimantan [96].
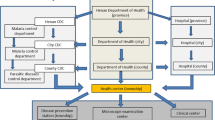
Data on malaria mosquito vectors and insecticide resistance of Anopheles spp. in Kalimantan from a few published sources but mainly from unpublished Indonesian Health Department (Balitbangkes) and Global Fund reports are summarized in Tables 4, 5 and Fig. 3. These indicate that the vectors of P. knowlesi and other simian malaria parasites in Malaysian Borneo such as An. balabacensis, Anopheles latens and Anopheles umbrosus are present in Kalimantan [97, 98].
Mapping of Anopheles spp. distribution in Indonesian Kalimantan (adapted from Elyazar et al. [69])
Non-human primate malaria
The first non-human primate malaria species in Borneo were identified by Halberstaedter and Prowazek in 1907 [99]. The blood of Macaca irus and Macaca nemestrina imported from Indonesian Borneo harboured a new species of parasite Plasmodium inui (after the old generic name of the primate host Inuus). This parasite was also found in cynomolgus monkeys (Macaca fascicularis). Plasmodium pitheci was discovered in the same year in the blood of an orang-utan (Pongo pygmaeus) and Plasmodium hylobati was detected in gibbon blood from a mature male Hylobates moloch, both from Borneo [100]. These two latter parasites are known to be host specific, but human infection with Plasmodium cynomolgi has been reported from Malaysian Borneo [101]. Plasmodium inui can also infect humans [102] and its sporozoites have been found in Anopheles mosquitoes in Sabah, Malaysian Borneo [103].
Three other species of malaria that can be harboured by macaques in Malaysian Borneo are Plasmodium fieldi [104], Plasmodium coatneyi [105] and Plasmodium simiovale [106]. Plasmodium fieldi and P. coatneyi have been found in An. balabacensis Baisa in Sabah [103], while P. simiovale was detected in long-tailed macaques in Sarawak [107]. Both P. fieldi and P. coatneyi human infections have been found outside Borneo in Peninsular Malaysia, and human P. simiovale infections have been detected in Peninsular Malaysia and Sarawak, Malaysian Borneo [102].
The predominant simian malaria species that infects humans in Malaysian Borneo is P. knowlesi [108]. Malaysia is the nation with the highest reported prevalence of P. knowlesi in South-east Asia [109, 110] and, in Sabah and Sarawak, nearly 80% of malaria cases are caused by P. knowlesi [111] which is also the predominant species responsible for malaria hospitalizations [112, 113]. Given that it shares borders with Sabah and Sarawak, it is important to determine whether knowlesi malaria is also found in Kalimantan. Reports of P. knowlesi in humans from Kalimantan are scant, in part because the species is not included as part of routine malaria diagnostic screening in PHCs. The diagnosis of P. knowlesi has not normally been considered, except in a few suspected cases where identification was performed in a laboratory outside Kalimantan. In the first such report, 4 out of 22 human blood samples from Kalimantan patients with malaria were identified by molecular methods as containing P. knowlesi (two of them mixed infections with P. falciparum or P. vivax) by a laboratory in Germany in 2009 [114]. A second report was of an Australian working in South Kalimantan with the diagnosis made by PCR in a Sydney laboratory [115]. A third report involved PCR analysis of 287 filter paper dried blood spots from malaria patients in Central and South Kalimantan, three of which (1.1%) were positive for P. knowlesi [116]. A fourth report in 2016 of P. knowlesi was the case of a 60-year-old man working at a coal mining site in Central Kalimantan [117].
The limited number of P. knowlesi cases both in the literature and recent Indonesian Health Department data contrast with the relatively large numbers seen in Sarawak [15,16,17,18] and Sabah [19,20,21]. Long-tailed and pig-tailed macaques are present in Kalimantan [118] and so are the vectors capable of transmitting knowlesi malaria [69, 118]. Kalimantan is within the geographic range of the species required for P. knowlesi zoonotic transmission and therefore estimated as a high-risk area in P. knowlesi risk-prediction mapping, indeed as high as in Malaysian Borneo (Fig. 4). This may mean that the distribution of vectors, environmental conditions facilitating transmission and/or methods of accurate detection of the parasite are different in Kalimantan compared with Malaysian Borneo. Unfortunately, data relating to the prevalence of malaria parasites in macaques in Kalimantan are lacking. There are non-human primates in Kalimantan other than Macaca, Pongo and Hylobates, from genus Nycticebus, Cephalopachus, Presbytis, Trachypithecus, Nasalis [119], but it is not known whether they can harbour malaria.
Map of Plasmodium knowlesi malaria risk on the island of Borneo as adapted from Shearer et al. [73]. The darker the shaded area, the higher the risk
Plasmodium parasite genetic diversity
A study in Ketapang district of West Kalimantan found that P. falciparum genetic diversity was low and its linkage patterns were consistent with unstable transmission and therefore amenable to targeted intervention; P. vivax diversity was higher and transmission seemed to be more stable [120]. Two studies of P. vivax genetic diversity in South and Central Kalimantan demonstrated that the Kalimantan parasite had distinct haplotypes due to mutation, recombination, and positive selection [121] and that there was differences in merozoite surface protein-1 gene (Pvmsp-1) between migrant and indigenous Dayak people [122].
Anti-malarial therapy and drug resistance
Choice of anti-malarial therapy in Kalimantan is as contained in national guidelines [123] which have been developed from studies in the eastern part of Indonesia [124,125,126]. First-line treatment for any malaria species is dihydroartemisinin-piperaquine (DHP) and primaquine. For complicated severe malaria, parenteral artesunate or quinine are recommended [123]. Before the WHO recommendation of artemisinin-based combination therapy (ACT) was widely implemented, chloroquine was used as monotherapy in Kalimantan. Some studies in Kalimantan between 1975 and 1991 found chloroquine-resistant malaria [88, 127,128,129,130] and many patients experienced relapse or recrudescence [88, 127]. In 1991, the first line treatment for malaria in Kalimantan was still chloroquine followed by primaquine, with sulfadoxine-pyrimethamine (SP) second line and quinine third line [7].
In 2004, artesunate plus amodiaquine (AS-AQ) was recommended as the first line therapy for P. falciparum infection only, followed by quinine and doxycycline as second line, and by quinine and tetracycline as the third line [7, 123]. Intramuscular artemether was also recommended for severe complicated falciparum malaria. Other malaria species were still to be treated with chloroquine and primaquine. These changing and complex treatment recommendations may have caused confusion amongst health professionals. In 2007, the government recommendation was that all malaria cases should be treated with an ACT, either AS-AQ or DHP, apart from P. malariae and P. ovale infections, and chemoprophylaxis, where chloroquine and doxycycline were used, respectively [2, 123]. The current recommendation from 2017 is, however, to use ACT for all malaria cases as a result of several drug safety and efficacy studies in Papua, Indonesia [124]. Chloroquine is no longer available as an anti-malarial. After the introduction of ACT, several studies took place in Kalimantan to assess the safety and efficacies of DHP and ASAQ in P. falciparum, P. vivax or both P. falciparum and P. vivax in malaria patients in Central and West Kalimantan with positive results [131,132,133].
Plasmodium falciparum resistance to chloroquine was identified in vitro in the early 90s in Nunukan and in vivo in Banjarmasin, both in East Kalimantan [87, 134]. Plasmodium vivax resistance to chloroquine has since been identified in the Ketapang district of West Kalimantan [86]. The chloroquine-resistant East Kalimantan P. falciparum strains were sensitive to other anti-malarial drugs such as halofantrine, mefloquine and artesunate [135,136,137,138]. A summary of studies of parasite resistance to standard anti-malarial medications before ACT was introduced In Indonesia is shown in Table 6. In 2012, molecular studies were performed in Kalimantan to determine the mutations in P. falciparum and P. vivax that cause resistance [139, 140]. Another study analysed mutations in P. falciparum dihydrofolate reductase and dihydropteroate synthase in South Kalimantan samples from pregnant women [141] and in adults [142]. In these studies, there was evidence of previously reported mutations in P. falciparum and P. vivax associated with resistance to chloroquine and SP.
A study of traditional falciparum malaria remedies performed in Kenyah indigenous people of the Apo Kayan region in East and North Kalimantan showed evidence of anti-malarial activity [55]. More recently, in 2021, two traditional treatments for P. falciparum, Cratoxylum sumatranum and Garcinia parvifolia, were analysed in Balikpapan Botanical Garden in East Kalimantan [143, 144] and the extracts also showed anti-malarial activity. The potential role of such therapies in the treatment of malaria needs further validation.
Current malaria control efforts in Kalimantan
Since the Roll Back Malaria programme was implemented in 2000, Kalimantan has been targeted for elimination by 2020 (Stage 3) [2, 9] with an increased emphasis on control measures such as enhanced case detection and improved diagnostic accuracy [145]. Even though elimination has not yet been achieved, there has been a substantial reduction in the burden of malaria in Kalimantan during the last two decades so that there are generally low rates of local transmission [9]. The API for South, West, North and Central Provinces was 0.13 in 2020 while it was 1.23 in East Kalimantan [11]. Some studies in Kalimantan assessing diagnostic accuracy have suggested the possibility of malaria being underdiagnosed. A qualitative study involving 10 PHCs in Sambas, West Kalimantan, found that inadequate laboratory facilities and human resources are associated with low compliance with malaria service delivery including blood film examination in suspected cases [146]. Nevertheless, the reliability of diagnosis by microscopy seemed high in differentiating positive from negative blood films, but less in determining Plasmodium species [147]. Quantifying parasite densities can, if available, provide useful prognostic information in P. falciparum (if not for P. vivax) infections, with a study from Kalimantan showing that this is particularly useful in children aged under 15 years [148].
Regarding malaria control efforts such as the usage of long-lasting insecticidal nets (LLINs), a study in Sungai Nyamuk village, Nunukan district, East Kalimantan, analysed the effectiveness of LLINs against Anopheles spp. [149]. The result was that the most effective LLIN was one that had been used for up to 6 months with those still in use at 12–24 months were much less effective, although it needs to be acknowledged that LLINs will have limited impact where local vectors feed in the early evening and outdoors. Identifying foci of malaria transmission is important in targeting malaria control strategies. In a spatial analysis study of recorded malaria cases in high-risk villages in the northern part of Kotabaru, South Kalimantan, two persistent and four re-emerging high-risk clusters were identified, confirming its potential role in informing the efficient deployment of limited malaria control resources [150].
Conclusions
Kalimantan is a large forested landmass with a substantial number of inhabitants living in heterogeneous environmental conditions ranging from densely populated coastal towns to sparsely populated logging regions, palm oil plantations and mining areas. There are water bodies where mosquitoes breed and dense forested areas where different species of primates thrive, including macaques (the hosts for P. knowlesi), Most people in Kalimantan are at risk of malaria despite the fact that parasite species distributions and prevalence rates vary substantially across the provinces in line with differences in population density and mobility, and the presence of mosquito vectors [4, 5, 69]. As a result, malaria control efforts need to be tailored to the local situation in order to be successful. Although the malaria situation has improved little over the last few years, there has been progress in Kalimantan since Roll Back Malaria was instituted in 2000.
The large number of human P. knowlesi infections seen in Malaysian Borneo has no parallel in Kalimantan. This is despite the presence of anopheline vectors known to transmit P. knowlesi [97] and long-tailed macaques [151]. Interestingly, P. knowlesi has not been detected in wild macaques in Indonesia [152] even though some human cases have been reported. This may reflect limited screening studies to date or sampling in areas of Indonesia with relatively low primate transmission. Indeed, the recent reduction in human malaria cases in Indonesia has resulted in more cases of simian malaria, especially due to P. knowlesi, in Sumatra [153]. It is possible that better diagnostic testing through more widely available PCR (including correctly identifying P. malariae as P. knowlesi) could unmask a more significant number of knowlesi malaria cases in Kalimantan. The role of deforestation and climate change may increase human contact with vectors carrying P. knowlesi in areas of Kalimantan in future. Given the potentially lethal nature of knowlesi malaria [154], efforts to ensure that it is diagnosed promptly and accurately should be a priority.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
WHO. World malaria report 2021. Geneva: World Health Organization; 2021.
Indonesia DKR. Malaria - pengendalian malaria di Indonesia. Jakarta: Kementrian Kesehatan Republik Indonesia; 2020.
GIDEON Informatics: Infectious diseases of Indonesia. 2021. p. 201–9.
Elyazar IR, Gething PW, Patil AP, Rogayah H, Kusriastuti R, Wismarini DM, et al. Plasmodium falciparum malaria endemicity in Indonesia in 2010. PLoS ONE. 2011;6: e21315.
Elyazar IR, Gething PW, Patil AP, Rogayah H, Sariwati E, Palupi NW, et al. Plasmodium vivax malaria endemicity in Indonesia in 2010. PLoS ONE. 2012;7: e37325.
Departemen Kesehatan Republik Indonesia. Ciptakan inovasi untuk eliminasi malaria 2022. http://p2p.kemkes.go.id/hms-2022/. Accessed Aug 2022.
Elyazar IR, Hay SI, Baird JK. Malaria distribution, prevalence, drug resistance and control in Indonesia. Adv Parasitol. 2011;74:41–175.
Sitohang V, Sariwati E, Fajariyani SB, Hwang D, Kurnia B, Hapsari RK, et al. Malaria elimination in Indonesia: halfway there. Lancet Glob Health. 2018;6:e604–6.
Malaria S, Pencegahan D. Direktorat Pencegahan dan Pengendalian Penyakit Tular Vektor dan Zoonotik Kementerian Kesehatan Republik Indonesia. Informasi malaria Indonesia: Peta situs. Last updated 2022 edition. Jakarta: Kementrian Kesehatan Republik Indonesia; 2022. p. 2022.
Surjadjaja C, Surya A, Baird JK. Epidemiology of Plasmodium vivax in Indonesia. Am J Trop Med Hyg. 2016;95:121–32.
Indonesia Departemen Kesehatan Republik Indonesia. Laporan kasus malaria. Departmen Kesehatan Kalimantan, 2021.
Margono BA, Potapov PV, Turubanova S, Stolle F, Hansen MC. Primary forest cover loss in Indonesia over 2000–2012. Nat Clim Chang. 2014;4:730–5.
Van de Vuurst P, Escobar LE. Perspective: climate change and the relocation of Indonesia’s capital to Borneo. Front Earth Sci. 2020;8:5.
Cox-Singh J, Singh B. Knowlesi malaria: newly emergent and of public health importance? Trends Parasitol. 2008;24:406–10.
Ooi CH, Bujang MA, Tg A, Sidik TMI, Ngui R, Lim YA. Over two decades of Plasmodium knowlesi infections in Sarawak: trend and forecast. Acta Trop. 2017;176:83–90.
Ooi CH, Phang WK, Kent Liew JW, Lau YL. Spatial and temporal patterns of Plasmodium knowlesi malaria in Sarawak from 2008 to 2017. Am J Trop Med Hyg. 2021;104:1814–9.
Lee KS, Cox-Singh J, Brooke G, Matusop A, Singh B. Plasmodium knowlesi from archival blood films: further evidence that human infections are widely distributed and not newly emergent in Malaysian Borneo. Int J Parasitol. 2009;39:1125–8.
Singh B, Kim Sung L, Matusop A, Radhakrishnan A, Shamsul SS, Cox-Singh J, et al. A large focus of naturally acquired Plasmodium knowlesi infections in human beings. Lancet. 2004;363:1017–24.
William T, Rahman HA, Jelip J, Ibrahim MY, Menon J, Grigg MJ, et al. Increasing incidence of Plasmodium knowlesi malaria following control of P. falciparum and P. vivax malaria in Sabah. Malaysia PLoS Negl Trop Dis. 2013;7:e2026.
Cooper DJ, Rajahram GS, William T, Jelip J, Mohammad R, Benedict J, et al. Plasmodium knowlesi malaria in Sabah, Malaysia, 2015–2017: ongoing increase in incidence despite near-elimination of the human-only Plasmodium species. Clin Infect Dis. 2020;70:361–7.
Ramdzan AR, Ismail A, Mohd Zanib ZS. Prevalence of malaria and its risk factors in Sabah. Malaysia Int J Infect Dis. 2020;91:68–72.
Cuenca PR, Key S, Jumail A, Surendra H, Ferguson HM, Drakeley CJ, Fornace K. Epidemiology of the zoonotic malaria Plasmodium knowlesi in changing landscapes. Adv Parasitol. 2021;113:225–86.
Amir A, Cheong FW, de Silva JR, Liew JWK, Lau YL. Plasmodium knowlesi malaria: current research perspectives. Infect Drug Resist. 2018;11:1145–55.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178–89.
Departement Dalam Negeri. Info teritori yang terdaftar dalam wilayah kepulauan Indonesia. https://kemendagri.go.id. Accessed Mar 2022.
Austin KG, Kasibhatla PS, Urban DL, Stolle F, Vincent J. Reconciling oil palm expansion and climate change mitigation in Kalimantan, Indonesia. PLoS ONE. 2015;10: e0127963.
Badan Pusat Statistik (BPS). Informasi statistik Indonesia. https://www.bps.go.id/. Accessed Mar 2022.
Knoema. Data insight: population. https://knoema.com/insights?tag=Population. Accessed Mar 2022.
Snapper L. Medical contributions from the Netherlands Indies. In: Honig P, Verdoom F (eds.) Science and scientists in the Netherlands Indies. Board for the Netherlands Indies, 1945. p. 309–20.
Koch R. Dritter bericht über die Tätigkeit der Malaria-Expedition. Dtsch Med Wochenschr. 1900;26:281–4.
van der Brug PH. Malaria in Batavia in the 18th century. Trop Med Int Health. 1997;2:892–902.
Koch R. Professor Koch’s investigations on malaria: second report to the German Colonial Office. Br Med J. 1900;1:325–7.
Marbun DS, Zein U. Malaria in the Dutch East Indies: a study on indigenous health during colonial times. In: Proceedings of the 7th International Conference on Multidisciplinary Research (ICMR 2018). 2020. p. 123–7.
Departemen Kesehatan Republik Indonesia. Sejarah Kesehatan Nasional Indonesia: Health report. Jakarta, 1978.
Sunarningsih H. Jangkung site and Maayan community. Naditira Widya. 2016;10:113–28.
Knapen H. Lethal diseases in the history of Borneo (1700–1900): mortality and the interplay between disease environment and human geography. In: Royal Institute of Linguistics and Anthropology Proceedings of the First Conference of the European Association for South-East Asian Studies, 1995.
Knapen H. Epidemics, droughts, and other uncertainties on Southeast Borneo during the eighteenth and nineteenth centuries. In: Paper landscapes. Brill, Leiden; 1998: 121–152
Schwaner CALM. Borneo: Beschrijving van het stroomgebied van den Barito en reizen langs eenige voorname rivieren van het zuid-oostelijk gedeelte van dat eiland. New York: Nabu Press; 2013.
Sellato B. A. W. Nieuwenhuis across Borneo (1894–1994). French National Centre for Scientific Research, 1993.
Takken W, Snellen W, Verhave J, Knols B, Atmosoedjono S. Environmental measures for malaria control in Indonesia - an historical review on species sanitation. Wageningen Agricultural University Papers. 1990;90:1–67.
Elshout JM. Over de geneeskunde der Kĕnja-Dajak in Centraal-Borneo in verband met hunnen godsdienst. Amsterdam, 1923.
de Zulueta J, LaChance F. A malaria-control experiment in the interior of Borneo. Bull World Health Organ. 1956;15:673–93.
Nieuwenhuis AW. Ten years of hygiene and ethnography in primitive Borneo (1891–1901). Batavia: Kolff and Company; 1929.
Shanks GD. Historical review: problematic malaria prophylaxis with quinine. Am J Trop Med Hyg. 2016;95:269–72.
Christensen SB. Natural products that changed society. Biomedicines. 2021;9:472.
Taylor N. Cinchona in Java: the story of quinine. New York: Greenberg; 1945.
Dawson RF. Quinine and quinidine production in the Americas: a brief history. Hort Technol. 1991;1:7–21.
Smocovitis VB. Desperately seeking quinine. Mod Drug Discov. 2003;6:57–8.
Krafts K, Hempelmann E, Skórska-Stania A. From methylene blue to chloroquine: a brief review of the development of an antimalarial therapy. Parasitol Res. 2012;111:1–6.
Roth HL. The natives of Sarawak and British North Borneo. London: Truslove & Hanson Publ; 1896.
Gomes EH. Seventeen years among the Sea Dyaks of Borneo: a record of intimate association with the natives of the Bornean jungles. Norderstedt: Hansebooks; 2018.
Clarke MC. Some impressions of the muruts of north Borneo. Trans R Soc Trop Med Hyg. 1951;44:453–64.
May JM. Medical geography: its methods and objectives. Geograph Rev. 1950;40:9–41.
Grijpstra BG. Common efforts in the development of rural Sarawak. Malaysia: Centre for Agricultural Publishing and Documentation; 1976.
Leaman DJ, Arnason JT, Yusuf R, Sangat-Roemantyo H, Soedjito H, Angerhofer CK, et al. Malaria remedies of the Kenyah of the Apo Kayan, East Kalimantan, Indonesian Borneo: a quantitative assessment of local consensus as an indicator of biological efficacy. J Ethnopharmacol. 1995;49:1–16.
Kimball LA. The concept of malaria in Brunei Malay indigenous medicine. Borneo Res Bull. 1975;7:5–11.
Ahmad FB. Medicinal plants used by Kadayan community in Sarawak. Sarawak Museum J. 1993;44:45–57.
Walch E, Soesilo R. Malaria control in the Netherlands Indies. Mededelingen van den Dienst der Volksgezondheid in Nederlandsch-Indie. 1935:24.
Bradley DJ. Watson, Swellengrebel and species sanitation: environmental and ecological aspects. Parassitologia. 1994;36:137–47.
Watson M. Drainage and malaria. Nature. 1911;85:471–3.
Swellengrebel NH. How the Malaria Service in Indonesia came into being, 1898–1948. J Hyg (Lond). 1950;48:146–57.
Swellengrebel NH. Eenige voor Nederlandsch-Indië nieuwe Anophelinen. Geneeskundig Tijdschrift voor Nederlandsch-Indië. 1919;59:1–12.
Soesilo R. Malariabestrijding in den Oost-Indischen archipel. Feestbundel. 1936. p. 45–72.
Ketterer WA. Economic benefits of malaria control in the Republic of Indonesia. Public Health Rep. 1953;68:1056–8.
Swellengrebel N, Lodens J. Anopheles aconitus and DDT spraying. Doc Neerl Ind Morb Trop. 1949;1:245–54.
Bonne-Wepster J, Swellengrebel N. Anopheles sundaicus and DDT spraying. Doc Neerl Ind Morb Trop. 1950;2:154–60.
Van Thiel P, Winoto R. Control of hyperendemic malaria in Java, caused by An sundaicus, by DDT house spraying. Doc Neerl Ind Morb Trop. 1951;3:295–319.
Soeparmo H, Laird R. Anopheles sundaicus and its control by DDT residual house spraying in Indonesia. Geneva: World Health Organization; 1954.
Elyazar IR, Sinka ME, Gething PW, Tarmidzi SN, Surya A, Kusriastuti R, et al. The distribution and bionomics of anopheles malaria vector mosquitoes in Indonesia. Adv Parasitol. 2013;83:173–266.
Soeparmo H, Stoker W. Malaria control in Indonesia Reprinted from Madjalah Kedokteran Indonesia. J Indonesian Med Ass. 1952;2:253–61.
Soemarlan Gandahusada S. The fight against malaria in Indonesia: a historical review and future outlook. National Institute of Health Research and Development, Ministry of Health, 1990.
Najera JA. Malaria and the work of WHO. Bull World Health Organ. 1989;67:229.
Shearer FM, Huang Z, Weiss DJ, Wiebe A, Gibson HS, Battle KE, et al. Estimating geographical variation in the risk of zoonotic Plasmodium knowlesi infection in countries eliminating malaria. PLoS Negl Trop Dis. 2016;10: e0004915.
Nieuwenhuis AW. De Verspreiding van malaria in verband met de geologische ge-steldheid van de afdeeling sambas - Borneo. Geneeskundig Tijdschrift voor Nederlandsch-Indië. 1894;34:125–37.
Tacconi L, Obidzinski K, Agung F. Learning lessons to promote forest certification and control illegal logging in Indonesia. Center for International Forestry Research (CIFOR). 2004. p. 1–81.
Cross JH, Clarke MD, Durfee PT, Irving GS, Taylor J, Partono F, et al. Parasitology survey and seroepidemiology of amoebiasis in South Kalimantan (Borneo), Indonesia. Southeast Asian J Trop Med Public Health. 1975;6:52–60.
Cross JH, Clarke MD, Cole WC, Lien JC, Partono F, Djakaria V, et al. Parasitic infections in humans in West Kalimantan (Borneo). Indonesia Trop Geogr Med. 1976;28:121–30.
Soenarno Soenarno MMI. Penyakit pekerja dalam kegiatan eksploitasi hutan di Kalimantan Tengah. Jurnal Penelitian Hasil Hutan. 1988;5:425–9.
Waris L. Potret vektor malaria dan filariasis di kecamatan sembakung kabupaten nunukan propinsi Kalimantan Timur. Vektora. 2011;3:122–36.
Sunaryo S. Situasi malaria di desa Santuun. Kecamatan muara uya kabupaten tabalong provinsi Kalimantan Selatan tahun 2010 Jurnal Litbang Pengendalian Penyakit Bersumber Binatang Banjarnegara. 2012;8:1–4.
Windy Tri Yuana NR, Wulan Sari Rg Sembiring. Gambaran letak kandang ternak dan kejadian malaria di 6 daerah endemis provinsi Kalimantan Selatan. Jurnal Epidemiologi dan Penyakit Bersumber Binatang.. 2014;5:29–34.
Umi Widyastuti RR, Widiarti Widiarti , Damar Tri Boewono. Studi bio-epidemiologi dan analisis spasial kasus malaria daerah lintas batas Indonesia-Malaysia (Pulau Sebatik) Kabupaten Nunukan, Provinsi Kalimantan Timur. Indonesian Bull Health Res. 2012;40:171–80.
Ompusunggu S. Malaria hutan di provinsi Kalimantan tengah dan Kalimantan Selatan, Indonesia Tahun 2013. Indonesian J Health Ecol. 2015;14:145–56.
Liestiana AR, Juhairiyah J, Windy TY, Erly H. Habitat perkembangbiakan spesifik Anopheles spp di tambang emas Kura-Kura Banian (perubahan perilaku Anopheles spp). Jurnal Litbang Pengendalian Penyakit Bersumber Binatang Banjarnegara. 2016;12:121–34.
Rahayu N, Suryatinah Y, Kusumaningtyas H. Discovery of malaria cases in forest workers in public health center, Teluk Kepayang, Tanah Bumbu, South Kalimantan. In: BIO Web of Conferences EDP Sciences; 2020. p. 01008.
Fryauff DJ, Tuti S, Mardi A, Masbar S, Patipelohi R, Leksana B, et al. Chloroquine-resistant Plasmodium vivax in transmigration settlements of West Kalimantan. Indonesia Am J Trop Med Hyg. 1998;59:513–8.
Tjitra ESG, Laihad F, Marwoto H, Sulaksono S, Arjoso S, Richie TL, et al. Penelitian obat anti malaria Indonesian. Bull Health Res. 1991;19:15–23.
Verdrager J. Effect of single dose of minocycline on a chloroquine resistant falciparum infection from Balikpapan, Kalimantan Indonesian. Bull Health Res. 1975;3:41–6.
Barber BE, William T, Grigg MJ, Yeo TW, Anstey NM. Limitations of microscopy to differentiate Plasmodium species in a region co-endemic for Plasmodium falciparum, Plasmodium vivax and Plasmodium knowlesi. Malar J. 2013;12:8.
Lee KS, Cox-Singh J, Singh B. Morphological features and differential counts of Plasmodium knowlesi parasites in naturally acquired human infections. Malar J. 2009;8:73.
Fletcher A. Staying safe in the jungles of Borneo: five studies of fatigue and cultural issues in remote mining projects. Ind Health. 2010;48:406–15.
Harbach RE, Baimai V, Sukowati S. Some observations on sympatric populations of the malaria vectors Anopheles leucosphyrus and Anopheles balabacensis in a village-forest setting in South Kalimantan. Southeast Asian J Trop Med Public Health. 1987;18:241–7.
Mujiono BH, Umi W, Damar TB. Pengendalian Vektor Terpadu Pengaruhnya terhadap indikator entomologi daerah endemis malaria Pulau Sebatik, Kabupaten Nunukan. Media Penelitian dan Pengembangan Kesehatan. 2012;22:152–60.
Sugiarto UKH, Soviana S, Hakim L. Karakteristik habitat larva Anopheles spp. di desa Sungai Nyamuk, daerah endemik malaria di kabupaten Nunukan, Kalimantan Utara Jurnal Litbang Pengendalian Penyakit Bersumber Binatang Banjarnegara. 2016; 12:47–54.
Sugiarto UKH, Soviana S, Hakim L. Bionomics of Anopheles (Diptera: Culicidae) in a malaria endemic region of Sungai Nyamuk village, Sebatik Island - North Kalimantan. Indonesia Acta Trop. 2017;171:30–6.
Liestiana Indriyati DA, Hairani B. Vektor malaria baru di kabupaten Kotabaru. Provinsi Kalimantan Selatan, Indonesia Vektora: Jurnal Vektor dan Reservoir Penyakit. 2017;9:1–8.
De Ang JX, Yaman K, Kadir KA, Matusop A, Singh B. New vectors that are early feeders for Plasmodium knowlesi and other simian malaria parasites in Sarawak. Malaysian Borneo Sci Rep. 2021;11:7739.
Ang JXD, Kadir KA, Mohamad DSA, Matusop A, Divis PCS, Yaman K, et al. New vectors in northern Sarawak, Malaysian Borneo, for the zoonotic malaria parasite Plasmodium knowlesi. Parasit Vectors. 2020;13:472.
Halberstadter L, Prowazek SV. Untersuchungen ueber die Malaria parasiten der Affen. Arb Klin Gesundheits (Berl). 1907;26:37–43.
Coatney RG, Collins WE, Warren MW, Contacos PG. The primate malarias. Atlanta: US Department of Health, Education and Welfare; 1971.
Kotepui M, Masangkay FR, Kotepui KU, Milanez GJ. Preliminary review on the prevalence, proportion, geographical distribution, and characteristics of naturally acquired Plasmodium cynomolgi infection in mosquitoes, macaques, and humans: a systematic review and meta-analysis. BMC Infect Dis. 2021;21:259.
Yap NJ, Hossain H, Nada-Raja T, Ngui R, Muslim A, Hoh BP, et al. Natural human infections with Plasmodium cynomolgi, P. inui, and 4 other simian malaria parasites, Malaysia. Emerg Infect Dis. 2021;27:2187–91.
Chua TH, Manin BO, Daim S, Vythilingam I, Drakeley C. Phylogenetic analysis of simian Plasmodium spp. infecting Anopheles balabacensis Baisas in Sabah, Malaysia. PLoS Negl Trop Dis. 2017;11:e0005991.
Eyles DE, Laing AB, Fong YL. Plasmodium fieldi sp. nov., a new species of malaria parasite from the pigtailed macaque in Malaya. Ann Trop Med Parasitol. 1962;56:242–7.
Eyles DE, Fong YL, Warren M, Guinn E, Sandosham AA, Wharton R. Plasmodium coatneyi, a new species of primate malaria from Malaya. Am J Trop Med Hyg. 1962;11:597–604.
Dissanaike AS, Nelson P, Garnham PCC, World Health Organization. Plasmodium simiovale sp. nov., a new simian malaria parasite from Ceylon. https://apps.who.int/iris/handle/10665/65290. Accessed Mar 2022.
Nada Raja T, Hu TH, Zainudin R, Lee KS, Perkins SL, Singh B. Malaria parasites of long-tailed macaques in Sarawak, Malaysian Borneo: a novel species and demographic and evolutionary histories. BMC Evol Biol. 2018;18:49.
Sinton JA, Mulligan HW. A critical review of the literature relating to the identification of the malaria parasites recorded from monkeys of the families Cercopithecidae and Colobidae. Records Malaria Survey India. 1932;3:357–80.
Zaw MT, Lin Z. Human Plasmodium knowlesi infections in South-East Asian countries. J Microbiol Immunol Infect. 2019;52:679–84.
Karunajeewa H, Berman J. Is the epidemiology of Plasmodium knowlesi changing, and what does this mean for malaria control in Southeast Asia? Clin Infect Dis. 2019;70:368–9.
Hussin N, Lim YA-L, Goh PP, William T, Jelip J, Mudin RN. Updates on malaria incidence and profile in Malaysia from 2013 to 2017. Malar J. 2020;19:55.
Lai MY, Rafieqin N, Lee PYL, Amir Rawa MS, Dzul S, Yahaya N, et al. High incidence of Plasmodium knowlesi malaria compared to other human malaria species in several hospitals in Malaysia. Trop Biomed. 2021;38:248–53.
William T, Menon J, Rajahram G, Chan L, Ma G, Donaldson S, et al. Severe Plasmodium knowlesi malaria in a tertiary care hospital, Sabah. Malaysia Emerg Infect Dis. 2011;17:1248–55.
Berens-Riha N, Sulistianingsih E, Fleischmann E, Loescher T. Plasmodium knowlesi found in several samples from Indonesia. ProMed. 2009. http://www.promedmail.org, archive no. 20090621.2278. Accessed March 2022.
Figtree MRL, Bain L, Kennedy T, Mackertich S, Urban M, Cheng Q, et al. Plasmodium knowlesi in Human, Indonesian Borneo. Emerging. Infect Dis. 2010;16:672–4.
Ompusunggu RMD, Yuliawaty R, Sihite BA, Ekowatiningsih RHS. Penemuan Baru Plasmodium knowlesi pada Manusia di Kalimantan Tengah Indonesian. Bull Health Res. 2015;43:63–76.
Setiadi W, Sudoyo H, Trimarsanto H, Sihite BA, Saragih RJ, Juliawaty R, et al. A zoonotic human infection with simian malaria, Plasmodium knowlesi, in Central Kalimantan. Indonesia Malar J. 2016;15:218.
Moyes CL, Shearer FM, Huang Z, Wiebe A, Gibson HS, Nijman V, Mohd-Azlan J, Brodie JF, Malaivijitnond S, Linkie M, et al. Predicting the geographical distributions of the macaque hosts and mosquito vectors of Plasmodium knowlesi malaria in forested and non-forested areas. Parasit Vectors. 2016;9:242.
Lempang MEP, Dewayanti FK, Syahrani L, Permana DH, Malaka R, Asih PBS, et al. Primate malaria: an emerging challenge of zoonotic malaria in Indonesia. One Health. 2022;14: 100389.
Noviyanti R, Coutrier F, Utami RA, Trimarsanto H, Tirta YK, Trianty L, et al. Contrasting transmission dynamics of co-endemic Plasmodium vivax and P falciparum: implications for malaria control and elimination. PLoS Negl Trop Dis. 2015;9:e0003739.
Murhandarwati EEH, Herningtyas EH, Puspawati P, Mau F, Chen SB, Shen HM, et al. Genetic diversity of merozoite surface protein 1–42 (MSP1-42) fragment of Plasmodium vivax from Indonesian isolates: rationale implementation of candidate MSP1 vaccine. Infect Genet Evol. 2020;85: 104573.
Lestarisa T, Arwati H, Dachlan YP, Keman S, Safruddin D. The use of archived Giemsa-stained blood smears and RDT for PCR-based genotyping of Plasmodium vivax merozoite surface protein-1 in central Kalimantan province. Indonesia Afr J Infect Dis. 2022;16:13–20.
Subdit Malaria Direktorat Penanggulangan dan Pengobatan Penyakit Tular Vektor dan Zoonosis. Buku saku tatalaksana kasus malaria. Departemen Kesehatan Republik Indonesia, Jakarta. 2017.
Sikora SA, Poespoprodjo JR, Kenangalem E, Lampah DA, Sugiarto P, Laksono IS, et al. Intravenous artesunate plus oral dihydroartemisinin-piperaquine or intravenous quinine plus oral quinine for optimum treatment of severe malaria: lesson learnt from a field hospital in Timika, Papua. Indonesia Malar J. 2019;18:448.
Ratcliff A, Siswantoro H, Kenangalem E, Maristela R, Wuwung RM, Laihad F, et al. Two fixed-dose artemisinin combinations for drug-resistant falciparum and vivax malaria in Papua, Indonesia: an open-label randomised comparison. Lancet. 2007;369:757–65.
Thriemer K, Poespoprodjo JR, Kenangalem E, Douglas NM, Sugiarto P, Anstey NM, et al. The risk of adverse clinical outcomes following treatment of Plasmodium vivax malaria with and without primaquine in Papua. Indonesia PLoS Negl Trop Dis. 2020;14:e0008838.
Ebisawa I, Fukuyama T. Chloroquine resistance of Plasmodium falciparum in West Irian and East Kalimantan. Ann Trop Med Parasitol. 1975;69:275–82.
Ebisawa I, Fukuyama T, Kawamura Y. Additional foci of chloroquine-resistant falciparum malaria in East Kalimantan and West Irian. Indonesia Trop Geogr Med. 1976;28:349–54.
Ebisawa I, Ohara H. A combination of sulfamonomethoxine and pyrimethamine versus other drugs for the treatment of malaria. Jpn J Exp Med. 1986;56:213–9.
Verdrager J, Simanjuntak CH, Saroso JS. Chloroquine-resistant falciparum malaria in East Kalimantan, Indonesia. J Trop Med Hyg. 1976;79:58–66.
Risniati YARH, Siswantoro H, Avrina R, Tjitra E, Delima D. Respon klinis dan parasitologis dihidroartemisinin-piperakuin pada subyek malaria falsiparum dan malaria vivaks pada hari ke-3 kunjungan ulang. Media Penelitian dan Pengembangan Kesehatan. 2011;21:157–65.
Raini MRG, Isnawati A, Tjitra E. Keluhan dan kepatuhan penderita malaria terhadap pengobatan malaria artesunat-amodiakuin di kalimantan dan Sulawesi. Media Penelitian dan Pengembangan Kesehatan. 2011;21:111–8.
Isnawati ARG, Tjitra E, Rooslamiati I, Raini M, Delima D. Rasionalisasi penggunaan obat simptomatik dan obat lain yang diberikan bersamaan dengan obat artesunate-amodiakuin pada subyek malaria di delapan puskesmas sentinel Kalimantan dan Sulawesi Media. Litbang Kesehatan (Media Penelitian dan Pengembangan Kesehatan). 2011;21:127–34.
Pribadi W. In vitro sensitivity of Plasmodium falciparum to chloroquine and other antimalarials in east Timor and east Kalimantan, Indonesia. Southeast Asian J Trop Med Public Health. 1992;23(Suppl 4):143–8.
Tjitra ESO, Pribadi W, Romzan A, Arbani PR, Reny M, Marwoto H. Pengobatan malaria falsiparum tanpa komplikasi dengan halofantrin di daerah resisten klorokuin. Indonesian Bull Health Res. 1992;20:1–8.
Tjitra ESO, Pribadi W, Reny M, Arbani PR, Romzan A, Marwoto H. Pengobatan penderita malaria falsiparum tanpa komplikasi dengan meflokuin di daerah resisten klorokuin. Indonesian Bull Health Res. 1992;20:25–33.
Tjitra ESO, Pribadi W, Arbadi PR, Renny M. Pengobatan artesunat pada penderita malaria falsiparum tanpa komplikasi di daerah resisten multidrug. Indonesian Bull Health Res. 1993;21:37–45.
Tjitra ESO, Pribadi W, Arbadi PR, Romzan A, Renny M, Marwoto H. Studi perbandingan pengobatan halofantrin antara penderita malaria falsiparum tanpa komplikasi yang in vitro sensitif dengan yang resisten klorokuin. Indonesian Bull Health Res. 1993;21:22–31.
Salwati ERH, Handayani S, Tjitra E. Deteksi Plasmodium vivax single nucleotide polymorphism (snp) y976f dari sampel monitoring pengobatan dihidroartemisinin-piperakuin di Kalimantan dan Sulawesi Media Penelitian dan Pengembangan Kesehatan. 2012;22:112–9.
Handayani SES, Tjitra E. Keragaman genetik petanda P. falciparum dari specimen subyek penelitian monitoring dihidroartemisinin-piperakuin di Kalimantan dan Sulawesi Media Penelitian dan Pengembangan Kesehatan. 2012;22:120–30.
Fitriah SS, Riyanto S, Budiono B, Basuki S, Dachlan YP, Uemura H. Polymorphism of Plasmodium falciparum dihydrofolate reductase and dihydropteroate synthase genes among pregnant women with falciparum malaria in Banjar District, South Kalimantan Province. Indonesia J Trop Life Sci. 2012;2:92–8.
Basuki S, Fitriah TY, Riyanto S, Budiono T, Dachlan YP, Uemura H. Two novel mutations of pfdhps K540T and I588F, affecting sulphadoxine-pyrimethamine-resistant response in uncomplicated falciparum malaria at Banjar district, South Kalimantan Province. Indonesia Malar J. 2014;13:135.
Tumewu L, Wardana FY, Ilmi H, Permanasari AA, Hafid AF, Widyawaruyanti A. Cratoxylum sumatranum stem bark exhibited antimalarial activity by lactate dehydrogenase (LDH) assay. J Basic Clin Physiol Pharmacol. 2021;32:817–22.
Kementrian Kesehatan Republik Indonesia. Profil kesehatan Indonesia tahun 2017. Indonesian Ministry of Health, Jakarta, 2017.
Wijayanti M, Ilmi H, Kemalahayati E, Tumewu L, Wardana FY, Suciati E, et al. In vitro antimalarial activity of Garcinia parvifolia Miq Stem extracts and fractions on Plasmodium falciparum lactate dehydrogenase (LDH) assay. J Basic Clin Physiol Pharmacol. 2021;32:839–44.
Kismed A. Analisis kepatuhan petugas puskesmas dalam melakukan pemeriksaan sediaan darah penderita malaria di wilayah Kabupaten Sambas tahun 2000. Fakultas Kesehatan Masyarakat: Universitas Indonesia; 2001.
Herman REA, Salwati E, Delima D, Tjitra E. Deteksi dan spesiasi parasit malaria sampel monitoring pengobatan dihydroartemisinin-piperaquine di Kalimantan dan Sulawesi. Mikroskopis vs polymerase chain reaction. Media Penelitian dan Pengembangan Kesehatan. 2011;21:104–10.
Avrina RYR, Siswantoro H, Hasugian AR, Tjitra E, Delima D. Hubungan kepadatan parasit dengan manifestasi klinis pada malaria Plasmodium falciparum dan Plasmodium vivax. Media Penelitian dan Pengembangan Kesehatan. 2011;21:119–26.
Sugiarto UKH, Susi S, Lukman H. Study of efficacy long-lasting insecticidal nets on An sundaicus (Diptera: Culicidae) and usage in Sungai Nyamuk village, Sebatik Island - North Kalimantan. Indonesian J Health Ecol. 2017;16:104–11.
Juhairiyah J, Andiarsa D, Indriyati L, Ridha MR, Prasodjo RS, Dhewantara PW. Spatial analysis of malaria in Kotabaru, South Kalimantan, Indonesia: an evaluation to guide elimination strategies. Trans R Soc Trop Med Hyg. 2021;115:500–11.
Jeyaprakasam NK, Liew JWK, Low VL, Wan-Sulaiman WY, Vythilingam I. Plasmodium knowlesi infecting humans in Southeast Asia: what’s next? PLoS Negl Trop Dis. 2020;14: e0008900.
Siregar JE, Faust CL, Murdiyarso LS, Rosmanah L, Saepuloh U, Dobson AP, et al. Non-invasive surveillance for Plasmodium in reservoir macaque species. Malar J. 2015;14:404.
Herdiana H, Cotter C, Coutrier FN, Zarlinda I, Zelman BW, Tirta YK, et al. Malaria risk factor assessment using active and passive surveillance data from Aceh Besar, Indonesia, a low endemic, malaria elimination setting with Plasmodium knowlesi, Plasmodium vivax, and Plasmodium falciparum. Malar J. 2016;15:468.
Cox-Singh J, Davis TM, Lee KS, Shamsul SS, Matusop A, Ratnam S, et al. Plasmodium knowlesi malaria in humans is widely distributed and potentially life threatening. Clin Infect Dis. 2008;46:165–71.
Acknowledgements
We would like to thank Health Department Republic of Indonesia in South, North, East, West and Central Kalimantan provinces and malaria officers at sub district level for providing malaria prevalence data in Kalimantan.
Funding
This review was supported by a Grant from the Australian Department of Foreign Affairs and Trade (DFAT) to SRS. TMED is supported by a Medical Research Future Fund Practitioner Fellowship.
Author information
Authors and Affiliations
Contributions
SRS identified relevant publications, extracted data, and produced the first draft of the manuscript. JKB facilitated identification of pertinent literature, contributed to data interpretation, and reviewed/edited the manuscript. BS and IE contributed to data interpretation, and reviewed/edited the manuscript. TMED conceived the study, verified identification and content of relevant publications, and produced the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Description of study sites and number of samples collected at each. Figure S1. Neighbour-Joining phylogenetic trees of Plasmodium-genus positive samples isolated from Kapuas Hulu, West Kalimantan, Indonesia based on the small subunit ribosomal RNA genes. Nucleotide sequences from the isolates are in bold, and were generated using (A) primers rPLU3 and rPLU4 with ~240 bp in length, and (B) primers Plasmo1 and Plasmo2 with ~252 bp in length. The bootstrap values at nodes were generated by 1,000 replicates, and only values above 70% are shown. In this result, the identity of the infecting Plasmodium species (samples in bold) could not be inferred through phylogenetic analyses since the DNA sequences generated were relatively short, resulting in phylogenetic trees with low bootstrap values. Samples KI 353 and KI 353 are from Participant no. 7, KI 809 is from Participant no. 8, KI 59 is from Participant no. 9, KI 334A and KI 334B are from Participant no. 10, KI 175A, KI 175B and KI 175 are from Participant no. 11, KI 978 is from Participant no. 15, and KI 676 is from Participant no. 16.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sugiarto, S.R., Baird, J.K., Singh, B. et al. The history and current epidemiology of malaria in Kalimantan, Indonesia. Malar J 21, 327 (2022). https://doi.org/10.1186/s12936-022-04366-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-022-04366-5