Abstract
Background
A reversal of chloroquine (CQ) resistance following a period of withdrawal has raised the possibility of its re-introduction. This study evaluated the current prevalence of Pfcrt and Pfmdr1 alleles in Plasmodium falciparum isolates, 11 years after CQ withdrawal in Southeast Nigeria.
Methods
Filter-paper blood samples were collected from 725 non-febrile individuals, comprising 250 children (≤ 12 years), 250 pregnant women and 225 other adults, between October 2014 and February 2015 in Nnewi town, Southeast Nigeria. Nested PCR followed by direct sequencing was employed for the genotyping of Pfcrt and Pfmdr1 genes.
Results
A total of 103 parasites-positive samples were recovered, comprising of 48 (19.20%) among children, 20 (20.00%) among pregnant women and 35 (15.50%) among other adults cohort. The frequency of the mutant genotype of Pfcrt 76T, 75E and 74I was 94.50% each. Parasite isolates from children had a frequency of 100% for mutant alleles in all Pfcrt codons while isolates from pregnant women and other adults had a frequency of 91% each in all codons. Haplotype distribution of pfcrt gene were 5.45, 0.00 and 76.37% for CVMNK, SVMNT and CVIET, respectively. For Pfmdr1 gene, the frequency of 86Y, 184F and 1246Y mutant alleles were 8.54, 29.27 and 3.66%, respectively. Amongst the Pfmdr1 haplotypes analysed, NFD had the highest frequency of 24.4%, followed by YFD at 6.10%. NYF and NYY occurred the least (1.20%).
Conclusion
The high level of Pfcrt mutations is suggestive of a sustained CQ pressure on P. falciparum isolates in the study area, despite the change of first line treatment from CQ to artemisinin combination therapy for 11 years. A new strategy to ensure the complete withdrawal of CQ from the country is recommended.
Similar content being viewed by others
Background
Drug resistance in Plasmodium falciparum has led to a major setback in the control and eradication of malaria across the globe, including Nigeria [1, 2]. Chloroquine (CQ), a safe and cheap anti-malarial was once the drug of choice for treating uncomplicated falciparum malaria for several decades [3]. However, the emergence of CQ-resistant malaria parasites, first reported in Southeast Asia along the Thai-Cambodian border during the late 1950s, and now spread across the globe, has greatly hampered the usefulness of this drug [4]. In Nigeria, the first emergence of CQ-resistant malaria parasites was reported in the southern region in 1987 and later spread across the country [1, 5]. Following high level resistance of P. falciparum to CQ, Nigeria changed the first-line option for the treatment of malaria from CQ to artemisinin combination therapy (ACT), with artemether-lumefantrine (AL) in 2005 [1, 6]. Published reports have shown that the switch from CQ to ACT in areas where CQ-resistant P. falciparum is prevalent has resulted in the re-emergence of CQ-sensitive strains, a few years after the cessation of CQ use [7], although some other studies have reported otherwise [8, 9].
Surveillance of CQ-resistant P. falciparum has relied on molecular methods that have allowed for better understanding of the emergence and spread of drug resistance genes. Plasmodium falciparum CQ resistance transporter (Pfcrt) gene, located on chromosome 7 with 13 exons encoding 424 amino acid transmembrane protein of 48.6 kDa molecular mass, was identified as CQ resistance marker [10]. It is believed that K76T mutation is the principal determinant of CQ resistance and susceptibility [10]. Other common mutations, C72S, M74I, N75E, A220S, Q271E, I356T, R371I, have also been shown to confer resistance in association with K76 mutation [10, 11]. In addition, point mutation in P. falciparum multidrug resistance protein 1 (Pfmdr1) gene located on chromosome 5, with one exon which codes for P-glycoprotein homologue 1 with 1419 amino acids and 162.25 kDa [12, 13] has been reported to modulate sensitivity and resistance to multiple anti-malarials. It is known that polymorphism, amplification and variation in mRNA expression level of Pfmdr1 gene are responsible for resistance to various anti-malarials and sudden uptick of multidrug parasites [12]. Mutations at positions N86Y, Y184F, S1034, N1042D, and D1246Y of Pfmdr1 have been shown to be responsible for either susceptibility or resistance to CQ, quinine, mefloquine, halofantrine, lumefantrine, and artemisinin [14,15,16,17].
The prevalence of asymptomatic malaria in Nigeria has been reported to range from 25% [18] to 59% [19, 20] in some regions of the country. Asymptomatic infection is an important obstacle in malaria control since such asymptomatic carriers do not seek treatment and thereby remain reservoirs for the life cycle of the infection to continue. The systematic identification and characterization of P. falciparum drug-resistant genes in asymptomatic individuals as part of surveillance intervention strategy is, therefore, very important for reducing the parasite reservoir and transmission of the disease. The current study investigated the prevalence of Pfcrt and Pfmdr1 alleles that have been recognized as CQ markers in P. falciparum isolates collected from asymptomatic individuals eleven years after withdrawal of CQ.
Methods
Study area, study population and ethics
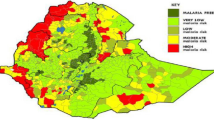
The study was conducted in Nnewi town, Anambra State, Southeastern Nigeria, with a population of 194,002 people, annual rainfall of about 1.4 m, and lies mainly in the deciduous forest area, spreading towards the grassland belt (National Census, 2006). Malaria is present throughout the year, with a marked increase during the rainy season, which normally runs from April to September.
Filter-paper blood samples were collected from 725 individuals, comprising 250 children under 12 years old and 225 adults during a community survey. Additional 250 filter-paper blood samples were collected from pregnant women attending Nnewi district hospital. All the samples were collected between October 2014 and February 2015. All participants were without malaria symptoms, as defined inclusion criteria accommodated only participants without obvious symptoms of malaria (axillary temperature ≥ 37.5 °C or history of fever 72 h preceeding presentation). Other enrolment criteria included absence of severe illness, a written consent from participants or guardians, and assent in cases where participants were children. Ethical approval for the study was obtained from the Ethics Review Board, University of Nigeria Teaching Hospital (approval number: NHREC/05/01/2008B-FWA00002458-IRB00002323).
Sample collection, processing and parasite detection
Blood was collected by finger prick and approximately 4 drops of blood were spotted on filter paper, air dried, individually sealed and stored at room temperature until DNA extraction. Genomic DNA was extracted from the dried blood spots using DNeasy Blood & Tissue kit (QIAGEN, Hilden, Germany), according to the manufacturer’s instructions and kept at − 20 °C until use. For the detection and identification of P. falciparum, the nested polymerase chain reaction (PCR) method described for all human malaria parasites molecular detection was used [21]. A first-step PCR was performed with specific primers rPLU1 and rPLU5 followed by genus specific (rFAL1/rFAL2—P. falciparum)-nested PCR. All PCR reactions were performed in a 25 μl total volume, containing 1X buffer, 2.5 mM MgCl2, 200 μM dNTPs, 200 nM primers, and 1U Taq DNA-polymerase (Qiagen, Hilden, Germany).
Genotyping of Pfcrt and Pfmdr1 polymorphisms
DNA was amplified using nested PCR in a 20 µl reaction volume containing 1× buffer, 2.5 mM MgCl2, 200 µM dNTPs, 2.0 mM, Q-solutions (PCR additive), 200 nM primers, 1 U Taq Polymerase and 10 ng of DNA template on a PTC-200 Thermal cycler (MJ Research, USA). The primers, cycling parameters and the amplified codons are listed in Table 1. Amplified PCR products were prepared for sequencing using Exo-SAP-IT (USB, Affymetrix, USA) and directly used as templates for DNA sequencing with the BigDye terminator v. 1.1 cycle sequencing kit (Applied Biosystems, Foster City, USA) on an ABI 3130XL DNA sequencer. Single nucleotide polymorphisms (SNPs) were identified by assembling the sequences with each reference sequence utilizing Sequencher 4.7 software and were reconfirmed visually from their respective electropherograms.
Results
Total of 103 (n = 103) parasite-positive samples were recovered from children (n = 48), pregnant women (n = 20) and other adult cohort (n = 35). The general characteristics of the study population are presented in Table 2. For the children cohort, the mean age of the population was 3.17 ± 0.17 (age range 2 months to 10 years). Gender ratio was 159 male versus 92 females. The overall prevalence of P. falciparum in the children cohort was 19.20%. For pregnant women, the mean age was 31.10 ± 0.35 (age range: 19 to 59 years) and the prevalence of P. falciparum was 8%. In the other adult population, the mean age of the population was 36.83 ± 0.85 (age range: 13 years to 82 years, gender ratio: 0.98 [155:157]). The overall percentage prevalence of P. falciparum in this group was 15.60%.
Frequency of the Pfmdr1 mutations
Of the 103 parasite-positive samples, the Pfmdr1 gene was successfully sequenced in 82 samples. The results for Pfmdr1 polymorphisms are shown in Table 3. Twenty-one single nucleotide polymorphisms were observed in the Pfmdr1 gene, with the highest number among pregnant women (15), followed by children cohort (12). The highest frequency of point mutation was observed in the position Y184F (29.3%) with the children cohort recording the highest frequency (38.9%). The frequency of the N86Y mutation was 8.54%, with the children also recording the highest frequency (16.7%). The highest frequency of heterozygote (3.7%) was observed at position Y184F. All the mutations observed were as shown in the Table 3. At codon 1157, 1 (1.22%) sample had synonymous mutation. All the other mutations observed were non-synonymous.
Frequency of the Pfcrt gene mutations with possible haplotypes
A total of 55 P. falciparum samples were successfully sequenced for the Pfcrt gene mutation with Table 4 showing the frequency of the mutations at different codons. All the samples had 100% wild type at codon 72. At codons 74, 75 and 76, the frequency of the mutation observed was 94.5% each, with the pregnant women recording 91% each followed by the adult group with 90.5% each. The resultant amino acid changes were all non-synonymous. For the haplotypes analysis, 52 (94.54%) had CVIET, 3 (5.45%) had CVMNK while none of the samples had SVMNT.
Frequency of Pfcrt and Pfmdr1 combined mutations
The frequency of Pfcrt and Pfmdr1 combined mutations are shown in Table 5. Combined point mutations of the two most important positions 86Y/76T (8.70%) was observed only in parasites collected from children, while 184F/76T occurred across the three cohorts with frequencies of 39.10%, 27.30% and 23.80% for the children, pregnant women and other adults, respectively. None of the isolates had 1246Y/76T mutations. In total, 30.90% of the parasites analysed harboured 184F/76T combined mutation.
Discussion
This report provides insight into the Pfcrt and Pfmdr1 genetic profile of P. falciparum isolates in asymptomatic individuals in Nnewi, Nigeria, and represent a unique place in the Southeast Nigeria on the prevalence of anti-malarial resistance genes among asymptomatic individuals. Most of the isolates in this study had mutations on Pfcrt gene at codons 74I, 75E and 76T, while no mutation was detected at codon 72S. The overall prevalence of Pfcrt 76T was 94.56%, which is similar to the prevalence previously reported for isolates in other parts of the country [1, 22, 23]. The present high prevalence of the 76T in Pfcrt gene clearly demonstrated that CQ-sensitive strain of P. falciparum has not yet re-emerged, 11 years after changing the malaria treatment policy to ACT. This could be attributed to the sustained CQ pressure, possibly facilitated by the availability of CQ in most pharmacies in this location and in many parts of the country [6, 24]. There is also the possibility that there may be persistent circulation of the marker due to drug selection pressure from amodiaquine, and not necessarily from CQ [25]. The persistence of the mutant allele in the present study is in contrast to the report from other African countries such as Malawi [3, 26], Tanzania [27,28,29,30], Kenya [30, 31], Mozambique [32], and Ethiopia [7] following CQ withdrawal. In agreement with the current report however, isolates of P. falciparum from South America have been reported to harbour mutant alleles, despite the withdrawal of CQ [8]. There has been no study in Nigeria that suggests re-emergence of CQ-sensitive strains after CQ withdrawal, implying that this may require several more years for reversal to be observed or the need to revamp treatment policy in rural areas, or the availability of CQ in local pharmacies. Also, a very similar study conducted in Ethiopia showed continual circulation of Pfcrt 76T mutations after withdrawal of CQ for more than 12 years [33].
The present study also showed that the CVIET haplotype was predominant (94.54%) among other haplotypes of Pfcrt gene in the study area, which is consistent with other findings in Nigeria [22, 23]. In addition, CVMNK (wild type) haplotypes was detected in only 5.45% of the isolates, mostly from pregnant women and other adult cohorts. Return of CQ-sensitive parasites (CVMNK haplotype) has been reported following cessation of CQ in some malaria-endemic countries, including Malawi [26], Gabon [34] and Brazil [35]. The absence of SVMNT haplotype observed in this study is in line with reports that confirm the absence of this haplotype in West Africa [36].
This study observed that the frequency of Pfmdr1 gene mutations varied among the isolates from the three cohorts. Codon 184F (29.27%) mutation predominates all other mutations observed in the study area. Confirmed mutations observed had 8.54% and 3.66% for 86Y and 1246Y, respectively, and no mutation was detected for the 1042 and 1246 codon positions. Oladipo et al. observed a higher prevalence in 86Y (62.20%) and 184F (69.00%) in their findings for the Pfmdr1 gene mutation among pregnant women in Lagos, Nigeria while no mutation was reported at codon 1246 [26]. Mutant Pfmdr1 N86Y has been linked to amodiaquine pressure in The Gambia [12], Kenya [37] and Nigeria [25]. Thus, the present data could suggest that the parasites in the study area might be resistant to amodiaquine. Studies have also shown that increased copy number of Pfmdr1 gene increases the risk of failure after treatment with mefloquine [38]. In Nigeria, some authors have reported high prevalence of 86Y allele of Pfmdr1 in children with acute uncomplicated malaria in some other regions [39, 40].
The present study also reveals double (86Y/76T, 184F/76T) and triple (86Y/184F/76T) mutations in some of the isolates, particularly among children, potentially indicating that CQ exerts a selective pressure in this area. It could also reflect the extensive use of the drugs among children in the area, demonstrating that children are the major reservoirs for these combined resistance markers. Before now, double mutation at positions 184 and 1042 of Pfmdr1 had been reported to reduce sensitivity to quinine, while mutations at positions 86 and 1042 increases the parasite’s susceptibility to quinine [41, 42]. If this present observation persists, the biggest challenge would be how to treat severe malaria among children, especially those with cerebral malaria, for which quinine is the medication of last resort.
Conclusion
This study reveals a high prevalence of Pfcrt mutant genotypes and haplotypes and low frequency of Pfmdr1 mutant genotypes, 11 years after the switch in malaria treatment policy from CQ to ACT in Nnewi, Nigeria. This may suggest continual circulation and spread of CQ-resistant P. falciparum parasites in the study area. The continued use of unrecommended CQ for the treatment of malaria, and its possible availability in open market in Nigeria needs to be addressed urgently.
Availability of data and materials
The datasets during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ojurongbe O, Ogungbamigbe TO, Fagbenro-Beyioku AF, Fendel R, Kremsner PG, Kun JF. Rapid detection of Pfcrt and Pfmdr1 mutations in Plasmodium falciparum isolates by FRET and in vivo response to chloroquine among children from Osogbo, Nigeria. Malar J. 2007;6:41.
Yeung S, Pongtavornpinyo W, Hastings IM, Mills AJ, White NJ. Antimalarial drug resistance, artemisinin-based combination therapy, and the contribution of modeling to elucidating policy choices. Am J Trop Med Hyg. 2004;71:179–86.
Kublin JG, Cortese JF, Njunju EM, Mukadam RAG, Wirima JJ, Kazembe PN, et al. Reemergence of chloroquine-sensitive Plasmodium falciparum malaria after cessation of chloroquine use in Malawi. J Infect Dis. 2003;187:1870–5.
Young MD, Contacos PG, Stitcher JE, Willar JW. Drug resistance in Plasmodium falciparum from Thailand. Am J Trop Med Hyg. 1963;12:305–14.
Trape JF. The public health impact of chloroquine resistance in Africa. Am J Trop Med Hyg. 2001;64:12–7.
Gbotosho GO, Happi CT, Ganiyu A, Ogundahunsi OA, Sowunmi A, Oduola AM. Potential contribution of prescription practices to the emergence and spread of chloroquine resistance in south-west Nigeria: caution in the use of artemisinin combination therapy. Malar J. 2009;8:313.
Mekonnen SK, Aseffa A, Berhe N, Teklehaymanot T, Clouse RM, Gebru T, et al. Return of chloroquine-sensitive Plasmodium falciparum parasites and emergence of chloroquine-resistant Plasmodium vivax in Ethiopia. Malar J. 2014;13:244.
Adhin MR, Labadie-Bracho M, Bretas G. Molecular surveillance as monitoring tool for drug-resistant Plasmodium falciparum in Suriname. Am J Trop Med Hyg. 2013;89:311–6.
Olukosi YA, Oyebola MK, Ajibaye OO, Orok BA, Aina OO, Agomo CO, et al. Persistence of markers of chloroquine resistance among Plasmodium falciparum isolates recovered from two Nigerian communities. Malar World J. 2014;5:3.
Fidock DA, Nomura T, Talley AK, Cooper RA, Dzekunov SM, Ferdig MT, et al. Mutations in the Plasmodium falciparum digestive vacuole transmembrane protein PfCRT and evidence for their role in chloroquine resistance. Mol Cell. 2000;6:861–71.
Su X, Kirkman LA, Fujioka H, Wellems TE. Complex polymorphisms in an approximately 330 kDa protein are linked to chloroquine-resistant Plasmodium falciparum in Southeast Asia and Africa. Cell. 1997;91:593–603.
Duraisingh MT, Refour P. Multiple drug resistance genes in malaria—from epistasis to epidemiology. Mol Microbiol. 2005;57:874–7.
Foote SJ, Thompson JK, Cowman AF, Kemp DJ. Amplification of the multidrug resistance gene in some chloroquine-resistant isolates of Plasmodium falciparum. Cell. 1989;57:921–30.
Pickard AL, Wongsrichanalai C, Purfield A, Kamwendo D, Emery K, Zalewski C, et al. Resistance to antimalarials in Southeast Asia and genetic polymorphisms in pfmdr1. Antimicrob Agents Chemother. 2003;47:2418–23.
Reed MB, Saliba KJ, Caruana SR, Kirk K, Cowman AF. Pgh1 modulates sensitivity and resistance to multiple antimalarials in Plasmodium falciparum. Nature. 2000;403:906–9.
Sidhu ABS, Valderramos SG, Fidock DA. pfmdr1 mutations contribute to quinine resistance and enhance mefloquine and artemisinin sensitivity in Plasmodium falciparum. Mol Microbiol. 2005;57:913–26.
Sisowath C, Strömberg J, Mårtensson A, Msellem M, Obondo C, Björkman A, et al. In vivo selection of Plasmodium falciparum pfmdr1 86 N coding alleles by artemether-lumefantrine (Coartem). J Infect Dis. 2005;191:1014–7.
Ojurongbe O, Adegbayi AM, Bolaji OS, Akindele AA, Adefioye OA, Adeyeba OA. Asymptomatic falciparum malaria and intestinal helminths co-infection among school children in Osogbo, Nigeria. J Res Med Sci. 2011;16:680.
Singh S, Madaki AJK, Jiya NM, Singh R, Thacher TD. Predictors of malaria in febrile children in Sokoto, Nigeria. Niger Med J. 2014;55:480–5.
Singh R, Godson II, Singh S, Singh RB, Isyaku NT, Ebere UV. High prevalence of asymptomatic malaria in apparently healthy schoolchildren in Aliero, Kebbi state, Nigeria. J Vector Borne Dis. 2014;51:128–32.
Snounou G, Viriyakosol S, Zhu XP, Jarra W, Pinheiro L, do Rosario VE, et al. High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol Biochem Parasitol. 1993;61:315–20.
Agomo CO, Oyibo WA, Sutherland C, Hallet R, Oguike M. Assessment of markers of antimalarial drug resistance in Plasmodium falciparum isolates from pregnant women in Lagos, Nigeria. PLoS ONE. 2016;11:e0146908.
Oladipo OO, Wellington OA, Sutherland CJ. Persistence of chloroquine-resistant haplotypes of Plasmodium falciparum in children with uncomplicated malaria in Lagos, Nigeria, four years after change of chloroquine as first-line antimalarial medicine. Diagn Pathol. 2015;10:41.
Meremikwu M, Okomo U, Nwachukwu C, Oyo-Ita A, Eke-Njoku J, Okebe J, et al. Antimalarial drug prescribing practice in private and public health facilities in South-east Nigeria: a descriptive study. Malar J. 2007;6:55.
Happi CT, Gbotosho GO, Folarin OA, Bolaji OM, Sowunmi A, Kyle DE, et al. Association between mutations in Plasmodium falciparum chloroquine resistance transporter and Plasmodium falciparum multidrug resistance 1 genes and in vivo amodiaquine resistance in Plasmodium falciparum malaria-infected children in Nigeria. Am J Trop Med Hyg. 2006;75:155–61.
Laufer MK, Thesing PC, Eddington ND, Masonga R, Dzinjalamala FK, Takala SL, et al. Return of chloroquine antimalarial efficacy in Malawi. N Engl J Med. 2006;355:1959–66.
Alifrangis M, Lusingu JP, Mmbando B, Dalgaard MB, Vestergaard LS, Ishengoma D, et al. Five-year surveillance of molecular markers of Plasmodium falciparum antimalarial drug resistance in Korogwe District, Tanzania: accumulation of the 581G mutation in the Plasmodium falciparum dihydropteroate synthase gene. Am J Trop Med Hyg. 2009;80:523–7.
Kamugisha E, Bujila I, Lahdo M, Pello-Esso S, Minde M, Kongola G, et al. Large differences in prevalence of Pfcrt and Pfmdr1 mutations between Mwanza, Tanzania and Iganga, Uganda-a reflection of differences in policies regarding withdrawal of chloroquine? Acta Trop. 2012;121:148–51.
Malmberg M, Ngasala B, Ferreira PE, Larsson E, Jovel I, Hjalmarsson A, et al. Temporal trends of molecular markers associated with artemether-lumefantrine tolerance/resistance in Bagamoyo district, Tanzania. Malar J. 2013;12:103.
Mang’era CM, Mbai FN, Omedo IA, Mireji PO, Omar SA. Changes in genotypes of Plasmodium falciparum human malaria parasite following withdrawal of chloroquine in Tiwi, Kenya. Acta Trop. 2012;123:202–7.
Mwai L, Ochong E, Abdirahman A, Kiara SM, Ward S, Kokwaro G, et al. Chloroquine resistance before and after its withdrawal in Kenya. Malar J. 2009;8:106.
Thomsen TT, Madsen LB, Hansson HH, Tomás EVE, Charlwood D, Bygbjerg IC, et al. Rapid selection of Plasmodium falciparum chloroquine resistance transporter gene and multidrug resistance gene-1 haplotypes associated with past chloroquine and present artemether-lumefantrine use in Inhambane District, southern Mozambique. Am J Trop Med Hyg. 2013;88:536–41.
Golassa L, Enweji N, Erko B, Aseffa A, Swedberg G. High prevalence of pfcrt-CVIET haplotype in isolates from asymptomatic and symptomatic patients in south-central Oromia, Ethiopia. Malar J. 2014;13:120.
Schwenke A, Brandts C, Philipps J, Winkler S, Wernsdorfer WH, Kremsner PG. Declining chloroquine resistance of Plasmodium falciparum in Lambaréné, Gabon from 1992 to 1998. Wien Klin Wochenschr. 2001;113:63–4.
Gama BE, de Oliveira NKA, Zalis MG, de Souza JM, Santos F, Daniel-Ribeiro CT, et al. Chloroquine and sulphadoxine-pyrimethamine sensitivity of Plasmodium falciparum parasites in a Brazilian endemic area. Malar J. 2009;8:156.
Mita T, Tanabe K, Kita K. Spread and evolution of Plasmodium falciparum drug resistance. Parasitol Int. 2009;58:201–9.
Holmgren G, Gil JP, Ferreira PM, Veiga MI, Obonyo CO, Björkman A. Amodiaquine resistant Plasmodium falciparum malaria in vivo is associated with selection of pfcrt 76T and pfmdr1 86Y. Infect Genet Evol. 2006;6:309–14.
Preechapornkul P, Imwong M, Chotivanich K, Pongtavornpinyo W, Dondorp AM, Day NPJ, et al. Plasmodium falciparum pfmdr1 amplification, mefloquine resistance, and parasite fitness. Antimicrob Agents Chemother. 2009;53:1509–15.
Happi TC, Thomas SM, Gbotosho GO, Falade CO, Akinboye DO, Gerena L, et al. Point mutations in the pfcrt and pfmdr-1 genes of Plasmodium falciparum and clinical response to chloroquine, among malaria patients from Nigeria. Am Trop Med Parasitol. 2003;97:439–51.
Ojurongbe O, Oyedeji SI, Oyibo WA, Fagbenro-Beyioku AF, Kun JF. Molecular surveillance of drug-resistant Plasmodium falciparum in two distinct geographical areas of Nigeria. Wien Klin Wochenschr. 2010;122:681–5.
Gadalla NB, Tavera G, Mu J, Kabyemela ER, Fried M, Duffy PE, et al. Prevalence of Plasmodium falciparum anti-malarial resistance-associated polymorphisms in pfcrt, pfmdr1 and pfnhe1 in Muheza, Tanzania, prior to introduction of artemisinin combination therapy. Malar J. 2015;14:129.
Wurtz N, Fall B, Pascual A, Fall M, Baret E, Camara C, et al. Role of Pfmdr1 in in vitro Plasmodium falciparum susceptibility to chloroquine, quinine, monodesethylamodiaquine, mefloquine, lumefantrine, and dihydroartemisinin. Antimicrob Agents Chemother. 2014;58:7032–40.
Acknowledgements
The authors are grateful to all parents/guardian and all individuals who volunteered to participate in the study. A special thanks to Albert Lalremruata and Christian Nguetse for sharing their expertise.
Funding
The study was supported by the Tertiary Education Trust Fund (TETFund) Benchwork Support Grant 2016/17 received by IMN.
Author information
Authors and Affiliations
Contributions
MNI performed the field study and experiments, data analysis with drafting first draft; CNN, BNT, and COE contributed to the study design and study samples and revisions of manuscript; TPV supervised the experiments and revision of the manuscript; OO designed the experiments and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
A written consent from participants or guardians, and assent in cases where participants were children were obtained. Ethical approval for the study was granted by the Ethics Review Board, University of Nigeria Teaching Hospital, Enugu, South Eastern Nigeria (Approval number: NHREC/05/01/2008B-FWA00002458-IRB00002323).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ikegbunam, M.N., Nkonganyi, C.N., Thomas, B.N. et al. Analysis of Plasmodium falciparum Pfcrt and Pfmdr1 genes in parasite isolates from asymptomatic individuals in Southeast Nigeria 11 years after withdrawal of chloroquine. Malar J 18, 343 (2019). https://doi.org/10.1186/s12936-019-2977-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-019-2977-6