Abstract
Background
The safety and immunogenicity of PfAMA1, adjuvanted with Alhydrogel® was assessed in malaria–experienced Malian adults. The malaria vaccine, PfAMA1-FVO [25-545] is a recombinant protein Pichia pastoris-expressed AMA-1 from Plasmodium falciparum FVO clone adsorbed to Alhydrogel®, the control vaccine was tetanus toxoid produced from formaldehyde detoxified and purified tetanus toxin.
Methods
A double blind randomized controlled phase 1 study enrolled and followed 40 healthy adults aged 18–55 years in Bandiagara, Mali, West Africa, a rural setting with intense seasonal transmission of P. falciparum malaria. Volunteers were randomized to receive either 50 µg of malaria vaccine or the control vaccine. Three doses of vaccine were given on Days 0, 28 and 56, and participants were followed for 1 year. Solicited symptoms were assessed for seven days and unsolicited symptoms for 28 days after each vaccination. Serious adverse events were assessed throughout the study. The titres of anti-AMA-1 antibodies were measured by ELISA and P. falciparum growth inhibition assays were performed.
Results
Commonest local solicited adverse events were the injection site pain and swelling more frequent in the PfAMA1 group. No vaccine related serious adverse events were reported. A significant 3.5-fold increase of anti-AMA-1 IgG antibodies was observed in malaria vaccine recipients four weeks after the third immunization compared to the control group.
Conclusion
The PfAMA1 showed a good safety profile. Most adverse events reported were of mild to moderate intensity. In addition, the vaccine induced a significant though short-lived increase in the anti-AMA1 IgG titres.
Registered on www.clinicaltrials.gov with the number NCT00431808
Similar content being viewed by others

Background
Despite recent renewed malaria control efforts, the disease still caused in 2013, 438,000 deaths (uncertainty range 236,000–635,000), 90 % of which occurred in Africa south of the Sahara [1]. An effective malaria vaccine would be a valuable additional tool particularly if one considers the new impetus towards malaria elimination [2]. Apical membrane antigen-1 (AMA1) is a surface protein expressed during the asexual blood stage of Plasmodium falciparum, and a leading blood stage vaccine candidate, with different formulations assessed and being tested in malaria endemic areas in Africa [3–5]. Three AMA-1-based vaccines have been evaluated in clinical trials in Mali, including two different monovalent vaccines based on AMA-1 derived from the 3D7 and FVO clones of P. falciparum, respectively, [5] and a bivalent vaccine that includes both of these versions of AMA-1 [6]. Preclinical studies [7, 8] of AMA1-based vaccines as well as clinical trials in people not naturally exposed to malaria [9, 10] have shown promise.
The trial reported here used PfAMA1-FVO [25-545], a lyophilized preparation of the ectodomain of the FVO clone of P. falciparum AMA1 [11]. This first phase 1 trial in malaria-exposed adults was the logical sequence of the clinical development of PfAMA1-FVO [25-545], and took place after a phase 1a trial done in Nijmegen [9]. The aim was to assess the malaria vaccine candidate immunogenicity and reactogenicity in adults naturally exposed to malaria in Mali.
Methods
This was a double blind conducted, randomized, controlled clinical trial designed to assess the safety and immunogenicity of the blood stage malaria vaccine candidate PfAMA1 [25-545] of P. falciparum FVO strain, adjuvanted with Alhydrogel®.
Study setting
The study was conducted at the Bandiagara Malaria Project (BMP) research clinic located close to the district hospital in Bandiagara, a rural setting with 13,634 inhabitants in the Dogon country in northeast Mali. Mean annual rainfall is 600 mm and Anopheles gambiae is the principal malaria vector. Malaria transmission is highly seasonal and overlaps with the rainy season [12]. Plasmodium falciparum is the most frequent parasite species causing 97 % of malaria infections. Malaria burden is heavy, children aged less than 10 years have an average of two clinical malaria episodes every transmission season [12, 13] and severe malaria afflicts one in 50 children aged less than 6 years each year [14]. Older children and adults are relatively protected against malaria disease but remain susceptible to malaria infection.
Participants
Participants were healthy adult men and women residing in Bandiagara aged 18–55 years old. After a screening for eligibility they were included if they planned to remain in Bandiagara for at least 12 months, showed good general health based on history, clinical and laboratory examinations and gave written informed consent. Female volunteers had in addition to declare willingness not to become pregnant during the first 5 months of the study, and they were referred to existing birth control programme at the district health care centre. Exclusion criteria were significant current illness as indicated by history, examination and/or laboratory testing including complete blood counts, alanine aminotransferase (ALT) and serum creatinine; previous immunization with any experimental vaccine; chronic use of immunosuppressants; receipt of blood products during the previous 6 months; and allergy to substances present in the vaccines.
Ethical clearance
The Institutional Review Board of the University of Bamako Faculty of Medicine approved the protocol and the informed consent forms, approval letter 07-35/FMPOS dated on May 15, 2007. The informed consent forms specified that the trial data will be published and that the participants confidentiality will be preserved by using only anonymous study numbers and no reference to particular individual identity. After obtaining community permission as described [15], the trial was publicized by local radio broadcast. The trial was conducted in compliance with the International Conference on Harmonisation Good Clinical Practices, the Declaration of Helsinki and applicable regulatory requirements of Mali. Separate written informed consent was obtained for screening and enrolment. Verbal consent of illiterate participants was administered and then documented using their fingerprints, a process verified by signatures of independent witnesses. Permission to import the investigational products in Mali was given by the Republic of Mali Ministry of Health. The trial sponsor was the African Malaria Network Trust (AMANET). A safety monitoring committee set by AMANET reviewed the safety data after the first and second vaccine dose and gave authorization to administer respectively the second and third vaccine doses.
Interventions and participant surveillance
PfAMA1 antigen comprises amino acids 25-545 corresponding to the ectodomain of AMA1 derived from the FVO clone of P. falciparum. Vaccine production and formulation are described elsewhere [11]. The vaccine was manufactured under GMP conditions by Eurogentec SA, Belgium, and supplied as lyophilized single dose vials containing 62.5 µg AMA1 protein, 23.3 µg EDTA, 25 mg saccharose, 187 µg NaH2PO4·2H2O, 226 µg Na2HPO4. The adjuvant used, Alhydrogel® is a crystalline aluminium oxyhydroxide AlOOH, also known as boehmite supplied as a 0.2 % suspension by Staten Serum Institute (SSI), Denmark. Vials were reconstituted by adding 625 µL 0.2 % Alhydrogel® suspension; the adsorption to Alhydrogel® was previously confirmed to be greater than 99 %. The reconstituted vaccine was then incubated for 60 min at room temperature to facilitate adsorption to the Alhydrogel® and a dose of 0.5 mL containing 50 µg AMA1 and approximately 0.5 mg aluminium was used for injection.
The control vaccine, tetanus toxoid was also manufactured at SSI. The tetanus toxoid was produced from a formaldehyde detoxified and purified tetanus toxin. The vaccine was supplied in pre-filled syringes of 0.5 mL containing more than 20 IU tetanus toxoid, aluminum hydroxyde as adjuvant and thiomersal as preservative. A buffer solution, water for injection, was added. All doses of all vaccines were administered by intramuscular injection in the left deltoid muscle.
The study vaccines were given on study days 0, 28 and 56, the first vaccine dose being injected in May 2007. Study day 84 clinic visit was done in August, at the peak of malaria transmission. Study day 140 clinic visit took place at the height of the dry season. The final study follow-up on day 365 coincided with the beginning of the 2008 malaria season. Interim safety reports were reviewed by an independent safety monitoring committee before the second and third vaccine doses. Active surveillance of participants for 28 days after each immunization was completed in August 2008 corresponding to study day 84. The database was locked for the primary unblinded analysis after study day 84, and the study continued in a single-blinded fashion, although individual study allocations were not disclosed to on-site study investigators or staff with the exception of the principal investigator. The extended surveillance phase included continuous access to free basic medical care at the research clinic, monthly home visits, and scheduled visits on study days 140 and 364. All participants completed the follow-up schedule and were included in the analysis.
Outcomes
The primary outcome was safety, measured through the occurrence of solicited symptoms during a 7-day follow-up period after immunization (day of immunization and days 1, 3 and 7 after immunization); the occurrence of unsolicited symptoms during a 28-day follow-up period after immunization (day of immunization and 28 subsequent days); the occurrence of laboratory toxicities; and the occurrence of serious adverse events during the entire study period. Secondary outcomes measured titres of anti-AMA1 antibody (IgG) by ELISA and activity of anti-AMA1 antibody by growth inhibition assay (GIA). These assays were performed at baseline and at specified times during and after immunization (Additional file 1).
Safety assessment
Following each immunization, participants were directly observed for 30 min, and then evaluated at the study clinic 1, 3, 7 and 14 days after each immunization and on study days 84, 140 and 364. Starting on day 140, monthly home visits were made to check the health status of participants and to encourage them to come to the research clinic if they felt ill. Clinical evaluations consisted of measurement of vital signs and assessment for local injection site and general solicited signs or symptoms. Local signs and solicited symptoms included pain, swelling, erythema at the injection site and limitation of arm abduction at the shoulder. General signs and solicited symptoms included fever (oral temperature ≥37.5 °C), chills, nausea, headache, malaise, myalgia and joint pain. Any other signs or symptoms were considered to be unsolicited, as were all signs or symptoms that occurred more than 7 days after immunization. All solicited local symptoms were considered related to the study vaccines. Pregnancies were monitored throughout the 12-month study period and until delivery, when this occurred after the study end. Blood was collected at screening, on immunization days and 7 days after each immunization and on study days 84, 140 and 364 to determine Complete blood count, biochemistry parameters (serum potassium, sodium, ASAT, ALAT, total bilirubin, alkaline phosphatase, γGT and creatinine). Adverse events were judged for relatedness to study vaccines and graded by severity as shown in Additional file 2: Table I. Laboratory parameters intensity was graded as indicated in Additional file 3: Table II.
Immunogenicity assessment
Antibody responses to AMA-1 were measured by an enzyme-linked immunosorbent assay (ELISA). Briefly, IgG ELISAs were performed using PfAMA-1 FVO [25-545] from the same clinical batch which production was described by Faber et al. [9] and that was used in a Phase 1a trial in Nijmegen [11], as the capture antigen, in serial twofold dilution, and one arbitrary unit (AU) was defined at an optical density of 1.0 over background. Thus the titre in AU represents the dilution of the serum required to obtain an OD of 1 over background. Antibody responses were measured on serum obtained from participants at the time of each immunization (study days 0 [baseline]), 28, 56, 84, 140 and 364.
Pre-immunization (day 0) sera and sera from 4 weeks after the third immunization (day 84, corresponding to peak antibody titres) were tested for growth inhibitory effects against homologous parasites expressing AMA1 (derived from FVO clone) P. falciparum line as described [16, 17]. Antibodies used for growth inhibition assays were purified on protein G columns (Sigma, St Louis, MO) using standard protocols, exchanged into RPMI 1640 using Amicon Ultra-15 concentrators (30 kDa cutoff, Millipore, Ireland), filter-sterilized and stored at −20 °C until use. IgG concentrations were determined using a Nanodrop ND-1000 spectrophotometer (Nanodrop Technologies, Wilmington, DE, USA).
Plasmodium falciparum strain FCR3 was cultured in vitro using standard P. falciparum culture techniques in an atmosphere of 5 % CO2, 5 % O2 and 90 % N2. FCR3 AMA1 (accession no. M34553) differs by 1 amino acid in the pro-sequence from FVO AMA1 (accession no. AJ277646).
The effect of 5 or 10 mg mL−1 purified IgG antibodies on parasite invasion was evaluated in triplicate using 96 well flat-bottomed plates (Greiner) with in vitro matured and synchronized P. falciparum schizonts at a starting parasitaemia of 0.2–0.4 %, a haematocrit of 2.0 % and a final volume of 50 µL containing 10 % normal human serum, 20 µg mL−1 gentamicin in RPMI 1640. After 40 to 42 h, cultures were resuspended, and 50 µL was transferred into 200 µL ice-cold PBS. The cultures were then centrifuged, the supernatant removed and the plates were frozen. Inhibition of parasite growth was estimated using the pLDH assay as previously described [16]. Parasite growth inhibition, reported as a percentage, was calculated as follows: 100 − ((Odexperimental − Od background)/(Odcontrol − Odbackground) × 100). Control IgG was isolated from malaria naïve donors. The AMA1 expressed was verified to be FCR3 by RFLP analysis and parasite cultures used for GIA tested negative for Mycoplasma by PCR.
Sample size
Determination of sample size was based on the primary safety endpoint, i.e. the occurrence of any solicited adverse events, unsolicited adverse events or change from baseline values of biological parameters during the study period. The primary analysis population was the intent-to-treat (ITT) population. Power calculations were based on the exact binomial distribution. With a sample size of 20 participants in each group, the study is powered to detect at least one adverse event or change from baseline values of biological parameters with a probability of at least 90 % if the incidence rate of adverse event or change from baseline values of biological parameters is 10.9 % or more. The study have a power of at least 80 % and 95 % to detect at least one adverse event or change from baseline values of biological parameters if their incidence rates are 7.7 % and 13.9 % or more, respectively. Incorporation of a comparator vaccine group of 20 permitted broad initial estimates of the incidence of local and general side effects and of immune responses among vaccine recipients.
Randomization and masking
Individual participants were randomized in a 1:1 ratio to receive either PfAMA1-FVO/Alhydrogel® or tetanus toxoid at the time of vaccination. Randomization to either of the two vaccines was done using a computer-generated randomization list. The randomization list contained sequential codes that linked a study number to a vaccine assignment. Study numbers were assigned to participants of each group in the order in which they were enrolled in the trial. The PfAMA1 vaccine and the comparator had different appearances. Therefore the vaccine preparation area was separated from the vaccine administration area. Vaccinations were carried out simultaneously in two separate consultation rooms, which were connected to a central pharmacy (the vaccine preparation room) by small windows with a sliding closure. On vaccination days, the prepared syringe was handed through the small window to a vaccinator for vaccine administration. In addition a study nurse not involved with assessment of study outcomes administered vaccines. And finally, the syringe containing vaccine was covered with opaque tape to mask its content and labelled with the participant study number and randomization code. At the study site, only the pharmacist, pharmacy assistant and the drug manager had access to the randomization list. Participants, investigators, lab personnel and all staff performing follow-up evaluations were blinded as to vaccine assignment. Following vaccine administration, participants were assessed and follow-up visits conducted by clinicians who had not been involved in the vaccinations.
Data analysis
Data quality assurance
The trial was conducted in compliance with BMP Clinical Trial Quality Assurance Procedures and the MRTC Clinical Laboratory Quality Assurance Plan. The study sponsor ensured the external monitoring of the trial. Following the pre study assessment, study initiation, three routine monitoring and closeout visits were performed during the trial. Standard Case Report Forms pages monitored and validated were sent to MRTC Data Management Unit for data entry into a GCP compliant database. Data was double entered by two independent data entry clerks and then reconciled by the study statistician. After resolution of all discrepancies, the database was frozen and used for analysis.
Statistical methods
For all safety endpoints, adverse events (AEs) were summarized by grade and vaccine doses for each vaccination group. Categorical data are summarized using counts and percentages. For immunogenicity analysis, ELISA titres of AMA1 antibodies are plotted by vaccine group and time points together with the 95 % CI bars.
Comparisons of proportions between vaccine groups were done using Fisher exact test and Wilcoxon-Mann–Whitney test was used for comparison of distributions of ordinal or continuous data. Comparisons between baseline level and post-vaccination level of biological parameters were done using McNemar change test (for categorical data) or Wilcoxon signed ranks test (for ordinal or continuous data). Analysis of Mean Fold Increase (MFI) was done using a Pearson’s product moment correlation (r) and the slope and intercept were estimated using linear regression. The significance of the correlation coefficient was assessed by a t test. All tests were 2-sided, and no correction of p-values was made for additional analyses.
Results
Participant flow and baseline data
Ninety participants were screened, 40 were enrolled (26 females and 14 males) and all received the first dose of the vaccine according to study allocation (Fig. 1). Common reasons for exclusion were concurrent illnesses, laboratory abnormalities during screening. The mean age was 30.1 years in the malaria vaccine group and 26.0 in the control group. In the PfAMA1 group two participants were excluded from vaccination after the second dose; one because of urticaria deemed to be possibly related to vaccine due to time relationship and the second because of pruritis of unknown cause. In the tetanus toxoid group, one participant was excluded from vaccination after having developed a swelling of the upper lip post dose 1 and a history known only after inclusion, of allergy to peanuts. The two groups were generally similar at enrolment with regard to gender, age or laboratory parameters (Table 1).
Safety and reactogenicity
Overall, the products showed a good safety profile similar to observations reported from previous trials. The 40 participants experienced a total of 257 adverse events, 136 were solicited AEs and 121 were unsolicited AEs. Additional vaccine doses did not globally increase the number of AEs.
Local solicited adverse events
In the PfAMA1 group the most frequent local solicited AE was injection site pain reported at least by 60 % of the participants after any dose (Table 2) as compared to 40 % in the control group. All cases of injection site pain were of mild to moderate intensity and resolved within three days post-vaccination. Second in frequency was swelling at the injection site observed at least in 45 % of the participants after any of the vaccine dose. Injection site swelling was the only solicited AEs with grade 3 intensity. The grade 3 swelling was defined as a diameter superior to 50 mm and was not associated with pain or with other functional impairments. The incidence of local solicited AEs did not increase with subsequent vaccine dose administration. In the tetanus toxoid group, frequency of injection site pain and swelling was more balanced between participants, with most of events having a mild to moderate intensity (Table 2). One participant had grade 3 swelling that resolved within the three days of follow up.
Systemic solicited adverse events
All solicited systemic AEs were of minor (93.5 %) or moderate (6.5 %) intensity and consisted mainly of headache and myalgia. There was no appreciable difference between the two groups though the control group experienced double the number of headaches after dose 1.
Unsolicited adverse events
Overall participants had a total of 123 unsolicited adverse events; 58 occurred in the malaria vaccine group and 65 in the control group. Unsolicited AEs classified by Body system and WHO preferred terms consisted mainly of respiratory disorders and infections, and were balanced by groups, being a representative picture of the morbidity usually observed in the study area.
One case of injection site induration of moderate intensity causally related to vaccine was reported in the malaria vaccine group after the second dose. The induration resolved within 4 weeks and the participant received the third vaccine dose. Three instances of pregnancy were reported, all after the study day 84. One case occurred in the control group and the participant decided to interrupt her pregnancy by abortion at the age of 4 weeks. Two others cases occurred in the malaria vaccine group; in both situations the pregnancy was diagnosed close to the last study clinic visit on study days 225 and 364. Both pregnancies resulted in healthy babies, one girl and one boy.
Serious adverse event
One serious adverse event occurred in one participant in the tetanus toxoid group on study day 94. The diagnosis was an acute episode of food poisoning that resolved without sequelae. The event was not related to vaccination.
Laboratory safety tests
Overall, the results showed a good biological safety profile. Only minor laboratory anomalies were reported and those consisted of grade 1 high Bilirubin levels in the malaria vaccine group after the first dose. These values returned to normal ranges before the second dose. There was no difference in mean haemoglobin levels between the two groups. No episode of anaemia defined as haemoglobin level ≤9.5 g/dL was observed among both vaccines recipients. The lowest haemoglobin level was 9.7 g/dL, recorded in a female participant on study days 35 and 84, in the malaria vaccine group.
Immunogenicity
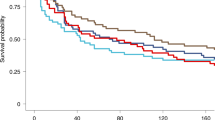
IgG antibody levels to the FVO-AMA1 antigen are depicted in Figs. 2 and 3, and summary statistics are tabulated in Table 3. Baseline levels of anti-AMA1 antibodies were high in both groups and were higher in the tetanus toxoid group as compared to the PfAMA1 group; 5164, 95 % CI (2494 to 10,691) versus 9938, 95 % CI (4484 to 22,025), respectively. The PfAMA1 vaccine induced a significant increase in AMA1-specific IgG (i.e., ratio day x/baseline >1) at all time points following vaccination (p < 0.05) (Table 3); after vaccination, titres increased gradually in the PfAMA1 recipients until day 84 when a maximum level was observed with a geometric mean of 17,584 arbitrary units 95 % CI (9889 to 31,267). The PfAMA1 group showed a 3.5, 95 % CI (2.3–5.4) fold rise in the IgG titres by day 84 as compared to baseline levels, while in the control group the day 84 fold rise compared to baseline was 1.07, 95 % CI (0.7–1.6). Thereafter, IgG titres decreased gradually during the study. This group assessment covers a wide range of individual variability. In the PfAMA1 group the highest increase in antibody titres was 60-fold increase reported after second vaccination. Those with the highest increase had the lowest baseline levels. In the PfAMA-1 group, MFI was significantly and negatively correlated with day 0 IgG titre (p = 0.002). The correlation coefficient was −0.67 with 95 % CI (−0.86 to −0.31). In the malaria vaccine group antibody responses were not sustained and returned to baseline levels after 12 months.
Growth inhibition assays
GIA titres are summarized in Table 4. Baseline levels of GIA were high in both groups: PfAMA1 and control vaccines recipients had baseline GIA levels of 56 (25–44) and 59 (19–50), respectively. Vaccination did not change GIA titres resulting in day 84 GIA titres of 68 (7–64) and 62 (19–53) for the PfAMA1 and control group, respectively. GIA titres decreased slightly by day 365, with GIA titres of 43 (26–31) and 49 (25–36) for PfAMA1 and controls, respectively.
Discussion
This study is the first evaluation of the AMA1-based malaria vaccine PfAMA1-FVO [25-545] adjuvanted with alum in malaria-experienced adults. The vaccine showed acceptable tolerability. Local reactions were more frequent in malaria vaccine groups than in the comparator group. Most recipients of the malaria vaccine experienced pain at the injection site. The incidence of injection site pain did not increase with subsequent administration of doses of the vaccine. Although swelling was often classified and graded based on the size of the reaction, these episodes of swelling were short-lived and were not associated with pain or with other functional impairments. There was a slight, non-statistical significant tendency to more adverse events in the control group than in the PfAMA1 group.
The safety and tolerability profile of the PfAMA1-FVO [25-545]/Alhydrogel® vaccine was similar to that seen in a previous trial of this vaccine in malaria-naïve volunteers [9]. Others formulations of AMA1 using different adjuvant system also showed acceptable tolerance profile in malaria-naïve [18–20] and Malian adults [3, 4, 21]. Biological parameters assessed have remained within area normal ranges. Anaemia was a concern in AMA1-based malaria vaccines tested in children [5, 22]. In this adult population, no anaemia cases were observed. A female participant recipient of the malaria vaccine had decreased levels of haemoglobin measured at two time points. However, these decreased levels were above the threshold that defined anaemia in the study population.
Antibody titres peaked 1 month after the third dose reaching a 3.5 fold rise. A comparable dynamic in antibody titres was reported in naive volunteers [9]. There is a very clear relation between pre-immunization titre and fold rise. The highest pre-titre have resulted in the lowest fold rise. In this trial, immunization started with the rainy season when most malaria transmission occurs in the study area. However high antibody titres were not sustained and returned to baseline levels after 12 months. This could witness an absence of natural boosting. Previous trials of AMA1 using AS02, a more potent adjuvant system, have generated much higher antibody titres [4], that persisted in children more than 12 months [23].
No significant change in GIA activities were observed, despite the rise in IgG titres. In previous trials, serum from naive adults immunized with AMA-1 3D7 did not show good grow inhibition on heterologous (FVO) parasites as compared to homologous (3D7) parasites [24]. Interestingly the immune response elicited by AMA1 from P. falciparum 3D7 in semi-immune adults showed a higher grow inhibitory activity on FVO clone than 3D7 clone of P. falciparum [4].
The functionality of immune response induced by AMA-1 may not be function of the system of expression of recombinant protein used, since the AMA-1 FVO expressed in Pichia pastoris and Escherichia coli has shown similar functionality in growth inhibitory experiments [25]. The adjuvant system might play a more prominent role in inducing functional antibodies.
Apical Membrane Antigen 1 is an extremely polymorphic protein, with more than 100 polymorphic amino acid sites, and in vitro experiments and studies in both animals and humans have indicated some degree of allele-specificity in the antibody responses to genetically different forms of AMA-1 [26, 27]. The PfAMA1 vaccine is based on AMA-1 sequence from the FVO clone of P. falciparum and other AMA-1-based vaccines developed from both 3D7 and FVO [4, 10, 19, 21, 24] have given good immune responses and acceptable reactogenicity. A phase 2b trial conducted in the same site assessed the efficacy of the 3D7 derived AMA-1 associated with AS02A did not have significant efficacy against clinical malaria episodes but showed high allele-specific efficacy against clinical malaria [28]. Vaccine allele-specific efficacy depended on the degree of homology at key amino acid residues between the vaccine antigen and AMA-1 in parasites circulating at the vaccine trial site [29, 30].
The PfAMA1-FVO [25-545] malaria vaccine candidate clinical development was stopped after the present trial was completed, partly because of the potential limits imposed by strain specificity of protection to polymorphic AMA1 confirmed in human [28]. However efforts were pursued to overcome strain-specificity of protection. The diversity covering approach developed a couple of years before by the same team at the Biomedical Primate Research Centre [31–33] that developed the PfAMA1-FVO [25-545], is promising and have now gone into clinical trials in malaria endemic settings [34].
Conclusion
The PfAMA1-FVO [25-545] malaria vaccine candidate was safe and well tolerated in adult exposed to intense and seasonal malaria transmission in Mali. The vaccine induced high antibody response that was not however sustained over the malaria transmission season.
Abbreviations
- ALT (ALAT):
-
Alanine transaminase (Alanine amino transferase)
- AST (ASAT):
-
Aspartate transaminase (Aspartate amino transferase)
- BMP:
-
Bandiagara Malaria Project
- °C:
-
Degree Celsius or centigrade
- CI:
-
Confidence interval
- CO2 :
-
Carbon dioxide
- dL:
-
Decilitre
- EDTA:
-
Ethylene diamine tetraacetic acid
- ELISA:
-
Enzyme-linked immunosorbent assay
- FMPOS:
-
Faculty of Medicine, Pharmacy and Odonto-Stomatology of Bamako, Mali
- FVO, FCR3:
-
Plasmodium falciparum parasites clones
- GCP:
-
Good clinical practice
- GIA:
-
Growth inhibition assay
- GMP:
-
Good manufacturing practice
- γGT:
-
Gamma-glutamyl transferase
- IgG:
-
Immunoglobulin G
- kDa:
-
KiloDaltons
- mg:
-
Milligramme
- mL:
-
Millilitre
- MRTC:
-
Malaria Research and Training Center
- OD:
-
Optical density
- O2 :
-
Oxygen
- PBS:
-
Phosphate-buffered saline
- PCR:
-
Polymerase chain reaction
- PfAMA1[25-545]:
-
Plasmodium falciparum Apical membrane Antigen 1, amino acids 25–545
- pLDH:
-
Plasmodium falciparum lactate dehydrogenase
- RFLP:
-
Restriction fragment length polymorphism
- RPMI 1640:
-
Roswell Park Memorial Institute culture medium
- SA:
-
Société Anonyme
- µg:
-
Microgramme
- WHO:
-
World Health Organization
References
WHO. World Malaria Report 2015. Geneva: World Health Organization; 2015.
Breman JG, Plowe CV. A malaria vaccine for control: more progress. J Infect Dis. 2009;200:317–20.
Dicko A, Diemert DJ, Sagara I, Sogoba M, Niambele MB, Assadou MH, et al. Impact of a Plasmodium falciparum AMA1 vaccine on antibody responses in adult Malians. PLoS ONE. 2007;2:e1045.
Thera MA, Doumbo OK, Coulibaly D, Diallo DA, Kone AK, Guindo AB, et al. Safety and immunogenicity of an AMA-1 malaria vaccine in Malian adults: results of a phase 1 randomized controlled trial. PLoS ONE. 2008;3:e1465.
Sagara I, Dicko A, Ellis RD, Fay MP, Diawara SI, Assadou MH, et al. A randomized controlled phase 2 trial of the blood stage AMA1-C1/Alhydrogel malaria vaccine in children in Mali. Vaccine. 2009;27:3090–8.
Dicko A, Sagara I, Ellis RD, Miura K, Guindo O, Kamate B, et al. Phase 1 study of a combination AMA1 blood stage malaria vaccine in Malian children. PLoS ONE. 2008;3:e1563.
Anders RF, Crewther PE, Edwards S, Margetts M, Matthew ML, Pollock B, et al. Immunisation with recombinant AMA-1 protects mice against infection with Plasmodium chabaudi. Vaccine. 1998;16:240–7.
Stowers AW, Kennedy MC, Keegan BP, Saul A, Long CA, Miller LH. Vaccination of monkeys with recombinant Plasmodium falciparum apical membrane antigen 1 confers protection against blood-stage malaria. Infect Immun. 2002;70:6961–7.
Roestenberg M, Remarque E, de Jonge E, Hermsen R, Blythman H, Leroy O, et al. Safety and immunogenicity of a recombinant Plasmodium falciparum AMA1 malaria vaccine adjuvanted with Alhydrogel, Montanide ISA 720 or AS02. PLoS ONE. 2008;3:e3960.
Remarque EJ, Roestenberg M, Younis S, Walraven V, van der Werff N, Faber BW, et al. Humoral immune responses to a single allele PfAMA1 vaccine in healthy malaria-naïve adults. PLoS ONE. 2012;7:e388987.
Faber BW, Remarque EJ, Kocken CH, Cheront P, Cingolani D, Xhonneux F, et al. Production, quality control, stability and pharmacotoxicity of cGMP-produced Plasmodium falciparum AMA1 FVO strain ectodomain expressed in Pichia pastoris. Vaccine. 2008;26:6143–50.
Coulibaly D, Diallo DA, Thera MA, Dicko A, Guindo AB, Koné AK, et al. Impact of preseason treatment on incidence of falciparum malaria and parasite density at a site for testing malaria vaccines in Bandiagara, Mali. Am J Trop Med Hyg. 2002;67:604–10.
Coulibaly D, Travassos MA, Kone AK, Tolo Y, Laurens MB, Traore K, et al. Stable malaria incidence despite scaling up control strategies in a malaria vaccine-testing site in Mali. Malar J. 2014;13:374.
Lyke KE, Dicko A, Kone A, Coulibaly D, Guindo A, Cissoko Y, et al. Incidence of severe Plasmodium falciparum malaria as a primary endpoint for vaccine efficacy trials in Bandiagara, Mali. Vaccine. 2004;22:3169–74.
Diallo DA, Doumbo OK, Plowe CV, Wellems TE, Emanuel EJ, Hurst S. Community permission for medical research in developing countries. Clin Infect Dis. 2005;41:255–9.
Bergmann-Leitner E, Duncan E, Burge J, Spring M, Angov E. Miniaturization of a high throughput pLDH-based Plasmodium falciparum growth inhibition assay for small volume samples from preclinical and clinical vaccine trials. Am J Trop Med Hyg. 2008;78:468–71.
Kennedy MC, Wang J, Zhang Y, Miles AP, Chitsaz F, Saul A, et al. In vitro studies with recombinant Plasmodium falciparum apical membrane antigen 1 (AMA1): production and activity of an AMA1 vaccine and generation of a multiallelic response. Infect Immun. 2002;70:6948–60.
Polhemus ME, Magill AJ, Cummings JF, Kester KE, Ockenhouse CF, Lanar DE, et al. Phase I dose escalation safety and immunogenicity trial of Plasmodium falciparum apical membrane protein (AMA-1) FMP2.1, adjuvanted with AS02A, in malaria-naïve adults at the Walter Reed Army Institute of Research. Vaccine. 2007;25:4203–12.
Mullen GE, Ellis RD, Miura K, Malkin E, Nolan C, Hay M, et al. Phase 1 Trial of AMA1-C1/Alhydrogel plus CPG 7909: an asexual blood-stage vaccine for Plasmodium falciparum malaria. PLoS ONE. 2008;3:e2940.
Malkin EM, Diemert DJ, McArthur JH, Perreault JR, Miles AP, Giersing BK, et al. Phase 1 clinical trial of apical membrane antigen 1: an asexual blood-stage vaccine for Plasmodium falciparum malaria. Infect Immun. 2005;73:3677–85.
Sagara I, Ellis RD, Dicko A, Niambele MB, Kamate B, Guindo O, et al. A randomized and controlled Phase 1 study of the safety and immunogenicity of the AMA1-C1/Alhydrogel + CPG 7909 vaccine for Plasmodium falciparum malaria in semi-immune Malian adults. Vaccine. 2009;27:7292–8.
Ellis RD, Fay MP, Sagara I, Dicko A, Miura K, Guindo MA, et al. Anaemia in a phase 2 study of a blood stage falciparum malaria vaccine. Malar J. 2011;10:13.
Laurens MB, Thera MA, Coulibaly D, Ouattara A, Kone AK, Guindo AB, et al. Extended safety, immunogenicity and efficacy of a blood-stage malaria vaccine in malian children: 24-month follow-up of a randomized, double-blinded phase 2 trial. PLoS ONE. 2013;8:e79323.
Spring MD, Cummings JF, Ockenhouse CF, Dutta S, Reidler R, Angov E, et al. Phase 1/2a study of the malaria vaccine candidate apical membrane antigen-1 (AMA-1) administered in adjuvant system AS01B or AS02A. PLoS ONE. 2009;4:e5254.
Giersing B, Miura K, Shimp R, Wang J, Zhou H, Orcutt A, et al. Posttranslational modification of recombinant Plasmodium falciparum apical membrane antigen 1: impact on functional immune responses to a malaria vaccine candidate. Infect Immun. 2005;73:3963–70.
Cortés A, Mellombo M, Mueller I, Benet A, Reeder JC, Anders RF. Geographical structure of diversity and differences between symptomatic and asymptomatic infections for Plasmodium falciparum vaccine candidate AMA1. Infect Immun. 2003;71:1416–26.
Takala SL, Coulibaly D, Thera MA, Dicko A, Smith DL, Guindo AB, et al. Dynamics of polymorphism in a malaria vaccine antigen at a vaccine-testing site in Mali. PLoS Med. 2007;4:e93.
Thera MA, Doumbo OK, Coulibaly D, Laurens MB, Ouattara A, Kone AK, et al. A field trial to assess a blood-stage malaria vaccine. N Engl J Med. 2011;365:1004–13.
Ouattara A, Takala-Harrison S, Thera MA, Coulibaly D, Niangaly A, Saye R, et al. Molecular basis of allele-specific efficacy of a blood-stage malaria vaccine: vaccine development implications. J Infect Dis. 2013;207:511–9.
Takala SL, Coulibaly D, Thera MA, Batchelor AH, Cummings MP, Escalante AA, et al. Extreme polymorphism in a vaccine antigen and risk of clinical malaria: implications for vaccine development. Sci Transl Med. 2009;1:2ra5.
Remarque EJ, Faber BW, Kocken CH, Thomas AW. A diversity-covering approach to immunization with Plasmodium falciparum apical membrane antigen 1 induces broader allelic recognition and growth inhibition responses in rabbits. Infect Immun. 2008;76:2660–70.
Kusi KA, Faber BW, Riasat V, Thomas AW, Kocken CH, Remarque EJ. Generation of humoral immune responses to multi-allele PfAMA1 vaccines; effect of adjuvant and number of component alleles on the breadth of response. PLoS ONE. 2010;5:e15391.
Kusi KA, Remarque EJ, Riasat V, Walraven V, Thomas AW, Faber BW, et al. Safety and immunogenicity of multi-antigen AMA1-based vaccines formulated with CoVaccine HT™ and Montanide ISA 51 in rhesus macaques. Malar J. 2011;10:182.
http://www.pactr.org/ATMWeb/appmanager/atm/atmregistry?dar=true&tNo=PACTR201402000719423. Accessed 18 Dec 2015.
Authors’ contributions
MAT, CHMK, BWF, EBI, OL, DAD, ER, RC, OKD, conceived and designed the study. MAT, DC, AKK, ABG, KT, AHS, ID, MD, IMT, YT, MS, AN, CA, MB, BK, AD, AT, conducted the study and collected data, MSS, IS, OBT and ER analysed the data. RN, SS monitored the study. DC, AKK, ER, and MAT wrote the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Thanks to Prof Hamar A. Traore and Dr Boubakar Sidiki Kouyate for serving as Local Medical Monitors and with Dr Thomas Ritchie, Dr Christophe Rogier, Prof Robert Sauerwein, on the Safety Monitoring Committee; Dr Mohamed Keita, and Mr Hamidou Yalcouye for clinical assistance; Mr Danzele Coulibaly and Mr Moctar Traore for administrative support; laboratory technician Vanessa Walraven for expert technical assistance on GIA; Prof Wenceslaw Kilama, and AMANET for funding the trial; and the community of Bandiagara, Mali.
Competing interests
The authors declare they have no competing interests.
Availability of data and materials
Raw dataset for IgG and GIA responses are enclosed as additional file. Clinical dataset may be rendered available upon request directed to the corresponding author.
Consent for publication
No details, images, or videos relating to individual participants, are included in the manuscript. The approved informed consent forms specified that the trial data will be published and that the participants confidentiality will be preserved by using only anonymous study numbers and no reference to particular individual identity.
Ethics approval and consent to participate
The trial was conducted in compliance with the International Conference on Harmonization Good Clinical Practices, the Declaration of Helsinki and applicable regulatory requirements of Mali. The study protocol and informed consent forms were approved by the Institutional Review Board of the University of Bamako Faculty of Medicine, approval letter 07-35/FMPOS dated on May 15, 2007. Separate written informed consent was obtained for screening and enrolment. Verbal consent of illiterate participants was administered and then documented using their fingerprints, a process verified by signatures of independent witnesses. The trial sponsor was the African Malaria Network Trust (AMANET). A safety monitoring committee set by AMANET reviewed the safety data after the first and second vaccine dose and gave authorisation to administer respectively the second and third vaccine doses.
Funding
The trial was funded by AMANET under the contract 002/2007 CLIN signed by all parties on 12 March 2007.
Author information
Authors and Affiliations
Corresponding author
Additional files
12936_2016_1466_MOESM1_ESM.xlsx
Additional file 1. Raw data set of the IgG and GIA responses for the phase 1 trial of PfAMA1 FVO [25-545] in Malians adults in Bandiagara.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Thera, M.A., Coulibaly, D., Kone, A.K. et al. Phase 1 randomized controlled trial to evaluate the safety and immunogenicity of recombinant Pichia pastoris-expressed Plasmodium falciparum apical membrane antigen 1 (PfAMA1-FVO [25-545]) in healthy Malian adults in Bandiagara. Malar J 15, 442 (2016). https://doi.org/10.1186/s12936-016-1466-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-016-1466-4