Abstract
Background
We investigate the correlation between programmed cell death-ligand 1 (PD-L1) and tumor-associated immune cell (TAIC) density in small-cell neuroendocrine carcinoma of the uterine cervix (SCNEC) and their correlation with clinicopathologic features.
Methods
PD-L1 and mismatch repair protein (MMR) expression in cancer cells and the density of TAIC were evaluated by immunohistochemistry in 89 SCNEC patients. The combined positive score (CPS), tumor proportion score (TPS), and immune cell score (ICS) of PD-L1 were measured, along with their correlation with clinicopathologic features in SCNEC patients using statistical analyses.
Results
CPS of PD-L1 ≥ 1 was seen in 68.5% of patients, positive TPS and ICS of PD-L1 were detected in 59.6% and 33.7% of patients, respectively. PD-L1CPS was higher in tumor-infiltrating immune cells (r = 0.387, p = 0.001) and positively correlated with programmed cell death-1 and forkhead box P3 + regulatory T cell (FOXP3 + Treg) infiltration (r = 0.443, p < 0.001; r = 0.532, p < 0.001). There was no statistical correlation between PD-L1 and MMR status. PD-L1CPS and PD-L1ICS positivity were independent prognostic factors, correlating with a favorable survival (HR (95%CI) = 0.363(0.139–0.950), p = 0.039 and HR (95% CI) = 0.199(0.050–0.802), p = 0.023, respectively). PD-L1ICS positivity was an independent indicator of recurrence in SCNEC patients and associated with better disease-free survival (HR (95% CI) = 0.124(0.036–0425), p = 0.001). TAIC and MMR levels had no statistical impact on survival results.
Conclusions
PD-L1 positivity was seen in over half of SCNEC tumors. It may work synergistically with FOXP3 + Treg and other infiltrating immune cells to support an adaptive immune response. PD-L1 positivity may be a favorable prognostic factor in SCNEC.
Similar content being viewed by others
Introduction
Small-cell neuroendocrine carcinoma of the cervix (SCNEC) is a rare but lethal cervical malignancy, constituting 0.9–1.5% of invasive cervical cancers and an annual incidence rate of 0.06 per 100,000 women[1, 2]. SCNEC has highly aggressive biological characteristics with high incidence rates of hematogenous (80%) and lymphogenous (45–57%) metastases [3, 4]. Even with advancements in treatment, SCNEC prognosis is poor (including patients diagnosed at early stages of disease) with survival rates for SCNEC patients at all stages ranging between 11–54% [5]. Thus, identifying prognostic factors and novel therapeutic options are strongly warranted for SCNEC patients.
Several studies suggest that tumor-infiltrating immune cells (TILs) with different cell types and densities play a significant role in the prognoses of many tumors, such as lung, breast, and cervical cancer [6,7,8]. Programmed cell death-1 (PD-1) regulates effector T cell activity by interacting with one of its ligands, programmed cell death protein 1 ligand 1 (PD-L1), which is expressed on various types of tumor cells including cervical cancer [9], and PD-L1 influences the functional maintenance of regulatory T cells (Tregs), a subset of CD4 + cells [10]. Tregs regulated by forkhead box P3 + (FOXP3 +), a forkhead helix transcription factor, are found in various tumors and are considered as a prognostic factor in human cancers [11,12,13]. Deficient mismatch repair (dMMR) and PD-L1 positivity have been shown to predict the benefit of anti-PD-1/PD-L1 immunotherapy in several cancers [14,15,16]. Recently, a case study found that PD-L1 expression, mainly focal, occurred in 70% of SCNEC tumors, and loss of MMR occurred in 33% of SCNEC tumors [17].
However, few studies have explored the expression, infiltration, relationship, and prognostic role of immune and anti-immune factors in SCNEC. In this study, we evaluated and explored the correlation between PD-L1 and tumor-associated immune cell (TAIC) levels in SCNEC tumors and investigated their relationship with SCNEC clinicopathological features and prognosis.
Materials and methods
Patients
This study enrolled 89 SCNEC patients who had undergone radical hysterectomy at the Sun Yat-sen University Cancer Center from 2005 to 2019. The last follow-up was in January 2020. The patients were followed up for 1.0–125.7 months. Clinical characteristics were collected including age, the International Federation of Gynecology and Obstetrics (FIGO) stage, tumor size, cervical human papillomavirus (HPV) DNA level, neuron-specific enolase (NSE) serum level, operative reports, histopathology, adjuvant therapy, tumor recurrence, and current status. Staging is based on the FIGO 2018 cervical cancer staging system. This trial was approved by the Sun Yat-sen University Cancer Center Institutional Review Board (YB2019-182–01), where all samples were handled in line with ethical and legal standards.
Tissue microarray (TMA) construction
TMAs were constructed from SCNEC patient samples that were embedded in paraffin, where representative tumor tissue areas were confirmed by two gynecologic pathologists based on hematoxylin–eosin (H&E) staining. Triplicate cores (1 mm2) were randomly punched in the marked tumor areas and placed into recipient paraffin blocks using a tissue microarrayer (Beecher instruments). Then, paraffin blocks were incubated at 37℃ for 15 min (so sample tissues attached to the wax) and cut into 4 mm-thick sections.
Immunohistochemistry (IHC)
All of the IHC markers were executed on the SCNEC tissue microarray slides following the manufacturer’s instructions (as described in our previous publication [18]). We assessed the expression of the following markers in SCNEC tumor samples: PD-L1 (clone SP263, Ventana, 1:150 dilution), PD-1 (clone NAT105, Abcam, 1:100 dilution), FOXP3 (clone 236A/E7, Abcam, 1:300 dilution), PMS1 homolog 2 (PMS2, clone EP51, Agilent, 1:100 dilution), mutS homolog 2 (MSH2, clone FE11, Agilent, 1:150 dilution), mutL homolog 1 (MLH1,clone ES05, Agilent, 1:50 dilution), mutS homolog 6 (MSH6, clone EP49, Agilent, 1:150 dilution), CD3 molecule (CD3, clone 2GV3, Ventana, 1:150 dilution), membrane spanning 4-domains A1(CD20, clone L26, Ventana, 1:100 dilution), CD4 molecule (CD4, clone SP35, Abcam, 1:50 dilution), CD8a molecule (CD8, clone 144B, Dako, 1:100 dilution), CD68 molecule (CD68, clone MRQ-42, Ventana, 1:100 dilution), marker of proliferation Ki-67 (Ki67, clone MIB-1, DAKO, 1:100 dilution), cyclin dependent kinase inhibitor 2A (P16, clone CINecP16,Ventana, 1:100 dilution).
Immunostaining was reviewed and evaluated by two independent pathologists who were blinded to the patients. The percentage of PD-L1 membrane staining in tumor and immune cells and combined positive score (CPS) were evaluated (minimum of 100 cells were evaluated) [19]. The tumor proportion score (TPS) was defined as the percentage of PD-L1-positive tumor cells. When TPS was ≥ 1% (the median value), tumors were considered as “PD-L1TPS positive”. The immune cell score (ICS) was defined by the percentage of PD-L1-positive immune cells. When ICS was ≥ 5% (the median value), tumors were considered as “PD-L1ICS positive”. The CPS was defined as the total number of all PD-L1-positive cells (including tumor cells, lymphocytes, and macrophages) divided by the number of viable tumor cells and multiplied by 100. When CPS was ≥ 1 (the median value), tumors were considered as “PD-L1CPS positive” [20, 21].
PD-1 staining in immune cells was assessed as present (positive) or absent (negative). And the percentage of CD3, CD20, CD4, CD8, CD68 and FOXP3 positive immune cells was obtained by dividing the total number of CD3, CD20, CD4, CD8, CD68 or FOXP3 positive immune cells by the total number of immune cells present in the tissue section. If the infiltration by percent of immune cells was less than the median value, the tumors were classed as having low immune cell infiltration. In addition, P16 was interpreted as positive if diffuse and block-like staining was found in all cores and negative if there was no or patchy staining in the cores. The loss of MMR proteins was defined as complete absence of nuclear staining. Ki67 index was defined by the percentage of positive-stained tumor cells out of a total number of tumor cells (at least 200 cells were evaluated), where “low proliferation” refers to samples that had positive-stained tumor cell percentages that were below the median value.
Statistical analyses
The Statistical Product and Service Solutions (SPSS) 25.0 statistical software package was used to perform all statistical analyses. The association between two variables was assessed by the chi-square test and Fisher’s exact test. Spearman’s rank correlation coefficients were used to calculate the bivariate correlations between the studied variables. Survival curves were plotted using the Kaplan–Meier method, and the log-rank test was used to determine the statistical differences. Multivariate analysis was analyzed using the Cox proportional hazards regression model on all significant characteristics determined using univariate analysis. Values were considered statistically significant when p < 0.05.
Results
Clinical characteristics
The clinicopathological information of the 89 SCNEC patients included in this study is summarized in Table 1. The median age was 44.5 years and the percentages of patients with tumor stages between I–II and III–IV were 59.6% and 40.4%, respectively. The tumor size range was 0.5–9 cm, where almost half of the tumors were of a size that was greater than 4 cm. There were 33 patients (37.1%) receiving neoadjuvant chemotherapy (NACT). Adjuvant chemotherapy was given in 84 (94.4%) patients, which included 55 patients who had also received adjuvant radiotherapy. The cisplatin and etoposide (EP) chemotherapy regimen was the therapy that was used the most in the patients. The total mortality rate was 33.7%, which involved much lower levels in early-stage cancer patients (26.4%) than in advanced-stage cancer patients (44.4%). The rate of tumor recurrence was 46.1%, where patients in early and advanced stages had similar levels.
Immunohistochemical assessment
The immunohistochemical outcomes are summarized in Table 2 and Additional file 1: Fig. S1. PD-L1CPS positivity was seen in 68.5% of SCNEC patients, PD-L1TPS and PD-L1ICS positivity was detected in 59.6% and 33.7% of patients, respectively (Fig. 1). The median PD-L1CPS value was 1 (range = 0–60), while the median PD-L1TPS was 1% (range = 0–15%). The median percentage of PD-L1ICS was 5% (range = 0–60%). There were 19.1% of samples that exhibited dMMR (MLH1/PMS2 loss), 70.6% of which had ≥ 1% PD-L1-positive tumor cells, compared to the proficient mismatch repair (pMMR) group, 56.9% of which showed ≥ 1% PD-L1-positive tumor cells (Spearman’s correlation coefficient(r) = 0.109, p = 0.412). The median percentage of Ki-67 index values was 70% (range = 50–95%, interquartile range = 22.5). 87.6% of the SCNEC showed that ≥ 60% of the tumor cells were Ki-67 positive. More than 85.0% of tumor samples showed positive expression for P16 protein. IHC studies revealed that PD1 protein positivity was identified in the immune cells and was found in 50.6% of samples, 10.0% exhibited PD-1 levels above 10%. FOXP3 positive TILs were observed in 62.9% of specimens. The percentage of specimens who had high level of CD3 + , CD20 + , CD4 + , CD8 + , and CD68 + TILs density were 49.4% (median = 6.0%), 56.2% (median = 0.0%), 51.7% (median 3.0%), 50.6% (median 5.0%), and 70.8% (median 2.0%), respectively.
Correlation of PD-L1 with clinicopathological features
PD-L1TPS, PD-L1ICS, and PD-L1CPS were associated with many clinicopathological parameters of SCNEC (Table 1). PD-L1CPS positivity was positively associated with HPV infection (r = 0.336, p = 0.028). We also showed that PD-L1CPS and PD-L1TPS positivity was associated with a favorable prognosis (r = − 0.336, p = 0.003 and r = − 0.236, p = 0.039, respectively). Moreover, PD-L1ICS positivity was negatively associated with Ki67 proliferation (r = − 0.214, p = 0.048) and tumor recurrence (r = − 0.278, p = 0.013).
PD-L1ICS value increased in the patients who received NACT (r = 0.258, p = 0.02). However, there was no statistical correlation between PD-L1 levels from TPS, ICS, and CPS levels and MMR status (Additional file 1: Fig. S2), PD-L1CPS levels also had no statistical correlation with P16 expression (Additional file 1: Fig. S3) and the proliferation of Ki67 (Additional file 1: Fig. S3).
Correlation of PD-L1 with TAICs
PD-L1 and TAIC levels were found to be significantly positively correlated, especially PL-D1CPS (Table 2; Fig. 2). PD-L1CPS value was positively correlated with PD-1 (r = 0.443, p < 0.001), FOXP3 + (r = 0.532, p < 0.001), TILs (r = 0.387, p = 0.001) and other specific TILs, including CD20 + (r = 0.377, p = 0.001), CD4 + (r = 0.507, p < 0.001), CD8 + (r = 0.492, p < 0.001), CD3 + (r = 0.540, p < 0.001), and CD68 + (r = 0.310, p = 0.006) immune cells. In addition, PD-L1TPS value was higher in TILs (r = 0.429, p < 0.001), such as CD20 + (r = 0.307, p = 0.005), CD4 + (r = 0.394, p < 0.001), CD8 + (r = 0.421, p < 0.001), and CD3 + (r = 0.467, p < 0.001) immune cells, and was positively correlated with PD-1 (r = 0.284, p = 0.01) and FOXP3 + (r = 0.457, p < 0.001) Treg infiltration. Moreover, PD-L1ICS value was also significantly positively correlated with PD-1 (r = 0.372, p = 0.001) and FOXP3 + (r = 0.301, p = 0.005), as well as CD20 + (r = 0.390, p < 0.001), CD3 + (r = 0.372, p = 0.001), and CD8 + (r = 0.515, p < 0.001) immune cells. Taken together, these results suggest that PD-L1 and immune cell markers such as PD-1, FOXP3 + , CD20 + , CD4 + , CD8 + , CD3 + , and CD68 + interact.
The infiltration by different proportion of TILs in PD-L1CPS negative and PD-L1CPS positive groups. A–E The IHC of the infiltration by a low (left side) or high (right part) proportion of CD3/CD4/CD8/CD20/FOXP3 positive immune cells in each group. F The IHC of PD-L1CPS negative and PD-L1CPS positive. G The infiltration by a higher proportion of CD3 positive immune cells in PD-L1CPS positive groups compared with PD-L1CPS negative groups. H The infiltration by a higher proportion of CD4 positive immune cells in PD-L1CPS positive groups compared with PD-L1CPS negative groups. I The infiltration by a higher proportion of CD8 positive immune cells in PD-L1CPS positive groups compared with PD-L1CPS negative groups. G The infiltration by a higher proportion of CD20 positive immune cells in PD-L1CPS positive groups compared with PD-L1CPS negative groups. K The infiltration by a higher proportion of FOXP3 positive immune cells in PD-L1CPS positive groups compared with PD-L1CPS negative groups (The scale bar is 200 μm, *** means p < 0.001)
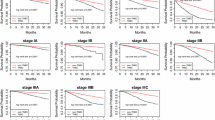
Prognostic significance of PD-L1
To investigate the prognostic significance of PD-L1, we analyzed overall survival (OS) rates and disease-free survival (DFS) rates among SCNEC patients (Tables 3; 4). Univariate and multivariate analyses indicated that PD-L1CPS and PD-L1ICS positivity were independent prognostic factors that were associated with a favorable survival (HR (95%CI) = 0.363(0.139–0.950), p = 0.039 and HR (95% CI) = 0.199(0.050–0.802), p = 0.023, respectively) and that PD-L1ICS positivity was an independent indicator of recurrence in SCNEC patients that was associated with a better DFS (HR (95% CI) = 0.124(0.036–0.425), p = 0.001). Univariate analysis revealed that PD-L1TPS was associated with a favorable OS and DFS, but there was no statistical significance when assessed with multivariate analyses (Fig. 3). TAIC and MMR status had no statistical impact on survival results.
Considering the clinicopathological characteristics, factors including FIGO stage (HR (95% CI) = 2.033(0.991–4.170), p = 0.048), NSE serum level (HR (95% CI) = 2.275(1.046–4.947), p = 0.038), parametrium invasion (HR (95% CI) = 3.251(1.384–7.633), p = 0.004), and perineural invasion (PNI, HR (95% CI) = 4.479(1.834–10.938), p = 0.001) were significantly associated with the survival of SCNEC patients. Moreover, multivariate analysis revealed that PNI was also an independent prognostic factor in SCNEC patients (HR (95% CI) = 3.617(1.361–9.616), p = 0.010).
Additionally, there was a negative association between DFS and stromal invasion (HR (95% CI) = 2.152(1.073–4.315), p = 0.031), parametrium invasion (HR (95% CI) = 2.849(1.253–6.476), p = 0.012), PNI (HR (95% CI) = 3.065(1.520–6.182), p = 0.002), lymphovascular invasion (LVSI, HR (95% CI) = 3.750(1.142–12.311), p = 0.029), and a positive correlation between DFS and postoperative therapy (HR (95% CI) = 0.292(0.102–0.831), p = 0.021). Among them, multivariate analysis showed that postoperative therapy (HR (95% CI) = 0.148(0.040–0.538), p = 0.004) was an independent recurrence factor in SCNEC patients (Additional file 1: Fig. S4).
Discussion
The tumor microenvironment, including TILs and tumor associated macrophages (TAMs), has a significant effect on therapy response and clinical results [6, 7, 22, 23]. PD-L1 plays a major role in the induction of tumor cell immune evasion by interacting with its receptor PD-1. Recently, immune checkpoint inhibitor therapy has been at the forefront of anti-tumor treatment showing great efficacy [24]. However, the clinical value of the immune microenvironment in SCNEC tumors has not been sufficiently researched.
This study used the largest cohort of SCNEC cases that has been published to date, investigating the association between PD-L1 and clinicopathological features. PD-L1CPS positivity was seen in 68.5% of SCNEC patients, and PD-L1TPS and PD-L1ICS positivity was detected in 59.6% and 33.7% of patients, respectively. Though without statistical significance, PD-L1 expressed higher in tumor cells in SCNEC patients with dMMR than in those with pMMR. The result was in accordance with a 10-case study in SCNEC patients, which found that PD-L1TPS positivity is seen in 70% of SCNEC and is associated with dMMR [17]. Consequently, dMMR may be able to identify those SCNEC patients who may benefit from PD-L1 inhibitors but needs further investigation.
PD-L1 was found to be significantly positively correlated with levels of TAICs, especially PD-L1CPS. PD-L1CPS value was higher in TILs, such as CD3 + , CD4 + , CD8 + , CD20 + , CD68 + immune cells, and was positively correlated with PD-1 and FOXP3 + Treg infiltration with statistical significance. These findings revealed a relationship between the PD-L1/PD-1 pathway and TILs. Much evidence has indicated that the PD-L1/PD-1 pathway is correlated with the maintenance of the immune microenvironment. PD-L1 positivity was correlated with TILs in many tumors, such as osteosarcoma, soft tissue sarcoma, and cervical cancer [17, 25,26,27]. Several studies showed that PD-L1 has an important effect on sustaining Tregs function in some autoimmune diseases, such as FOXP3 positive TILs and regulating signaling molecules that play a critical role in transforming naive T cells into Tregs [28, 29]. There are two mechanisms for the regulation of PD-L1 TPS including innate and adaptive immune regulation [30]. One is the tumoral constitutive PD-L1 and the other is an adaptive immune response to local inflammatory signals. In our study, PD-L1 may have an effect on the TIL-mediated anti-tumor inflammatory response in SCNEC.
The combined survival rates of SCNEC range from 11 to 54% for all stages [5]. The OS for early-stage SCNEC patients is 30% to 60%, while the 5-year OS for advanced stages is 0% to 17% [31]. Similarly, in our study, the total mortality rate of SCNEC patients was 33.7%, where patient mortality in early stages was 26.4%, which was lower than that of advanced patients (44.4%). Considering the prognosis of SCNEC patients, PNI was an independent prognostic factor and postoperative therapy was an independent recurrence factor in SCNEC patients. PNI may prove to be another metastatic route in cervical cancer [32]. In small cell lung cancer (SCLC), ASCL1 and NEUROD1 could regulate various genes such as SOX2, MYCL1, that contribute to neuronal function and promote perineural invasion [33, 34]. Since PNI is associated with poor survival of SENEC patients, selecting an appropriate surgical method without nerve-sparing methods is significantly important. And postoperative therapy is necessary for some SCNEC patients to reduce the risk of tumor recurrence.
In addition, we identified that PD-L1CPS and PD-L1ICS positivity were independent favorable prognostic indicators and that PD-L1ICS positivity was an independent favorable recurrence factor in SCNEC patients. This study identified a relationship between improved survival of SCNEC patients and PD-L1, indicating that local immunity plays a critical role in limiting tumor progression. Recently, PD-L1 has been classed as an adverse prognostic factor for many types of malignancies [35,36,37,38], FOXP3 as the same [27]. One study suggested that PD-L1 is a poor prognostic factor and TILs are favorable prognostic factors in cervical squamous cell carcinoma [39]. The role of PD-L1/PD-1 and TILs in tumors is controversial. A study about SCLC indicated that about 39.3% of patients had PD-L1 protein positivity, and PD-L1 and CD8 + TILs density were associated with better prognoses in patients with SCLC [40].In other studies, PD-L1/PD-1 is also associated with favorable prognoses in various tumors, such as triple negative breast cancer, melanoma, and colorectal cancer [15, 41, 42]. It is difficult to rationalize two diametrically opposed results of PD-L1. With our consideration, one of the reasons that caused this opposed prognostic results of PD-L1 might be related with the different type of cancer and specimens, the different definition of “PD-L1 positive”, and the complex mechanism of PD-L1/PD-1 and TILs.
A next-generation sequencing study of 10 SCNEC patients revealed that genetic alterations involved pathways such as PI3K/AKT/mTOR, MAPK, and TP53/BRCA pathways [43]. In addition, a review of 126 published papers demonstrated that PD-L1, which is regulated by many signaling pathways including PI3K/AKT and MAPK (which can be activated by HPV E6/E7 oncogenes), is associated with HPV-caused cervical cancer carcinogenesis [44]. High-risk HPV infection, especially HPV 18 and HPV 16, participates in the development of SCNEC [45]. In our study, PD-L1CPS positivity was positively correlated with HPV infection, indicating PD-L1 and HPV infection may have some interacting functions which need further research. Another comprehensive sequencing analysis found that PD-L1 and CD8 + TILs are much higher in cervical cancer patients with complete response to chemoradiotherapy than those who did not respond to chemoradiotherapy, indicating an inflammatory tumor microenvironment exists in cervical cancer patients that will respond to chemoradiotherapy [46]. TILs may be a basic predictor of tumor treatment response [47]. All of these studies demonstrate complex mechanisms of PD-L1 and TILs, which may be possible predictors of response to chemoradiotherapy and favorable prognostic indicators in SCNEC patients.
Due to the histopathological similarity to SCLC, the treatment of SCNEC is predominantly based on SCLC, including surgery, radiotherapy, and chemotherapy, which has improved SCNEC patient prognoses to some extent [17]. Researches have suggested that SCLC patients with neuroendocrine (NE)-low subtype are correlated with increased TILs compared to NE-high tumors, providing potential biomarkers for SCLC immunotherapies [48, 49]. Pembrolizumab was approved by the Food and Drug Administration (FDA) for therapy of patients with metastatic or recurrent cervical cancer with PD-L1positivity (as determined by an FDA-approved test in cervical cancer) and patients with metastatic SCLC. More pembrolizumab related clinical research should be carried out in SCNEC.
In conclusion, our study demonstrated that PD-L1 and PD-1 positivity in more than half of SCNEC tumors and may work synergistically with FOXP3 + Treg and other TAICs in support of an adaptive immune response to local inflammatory signals. PD-L1 may be a favorable prognostic factor in SCNEC. Conventional therapies that are in combination with immune modulation treatments, such as a combined strategy to block PD-L1/PD-1 with depletion of FOXP3 + Tregs, may show as a promising treatment for SCNEC patients and may change the course of the disease.
Availability of data and materials
The data that support the findings of this study are available from the RDD website: http://www.researchdata.org.cn/.
Abbreviations
- SCNEC:
-
Small-cell neuroendocrine carcinoma of the cervix
- TILs:
-
Tumor-infiltrating immune cells
- PD-1:
-
Programmed cell death-1
- PD-L1:
-
Programmed cell death protein 1 ligand 1
- Tregs:
-
Regulatory T cells
- FOXP3 + :
-
Tregs regulated by forkhead box P3 +
- dMMR:
-
Deficient mismatch repair
- TAIC:
-
Tumor-associated immune cell
- FIGO:
-
The International Federation of Gynecology and Obstetrics
- HPV:
-
Human papillomavirus
- NSE:
-
Neuron-specific enolase
- TMA:
-
Tissue microarray
- PMS2:
-
PMS1 homolog 2
- MSH2:
-
MutS homolog 2
- MLH1:
-
MutL homolog 1
- MSH6:
-
MutS homolog 6
- CD20:
-
Membrane spanning 4-domains A1
- Ki-67:
-
Marker of proliferation Ki-67
- P16:
-
Cyclin dependent kinase inhibitor 2A
- CPS:
-
Combined positive score
- TPS:
-
Tumor proportion score
- ICS:
-
Immune cell score
- SPSS:
-
The Statistical Product and Service Solutions
- NACT:
-
Neoadjuvant chemotherapy
- EP:
-
The cisplatin and etoposide
- DFS:
-
Disease-free survival
- OS:
-
Overall survival
- TAMs:
-
Tumor associated macrophages
- SCLC:
-
Small cell lung cancer
- FDA:
-
The Food and Drug Administration
References
Chen J, Macdonald OK, Gaffney DK. Incidence, mortality, and prognostic factors of small cell carcinoma of the cervix. Obstet Gynecol. 2008;111:1394–402.
Margolis B, et al. Natural history and outcome of neuroendocrine carcinoma of the cervix. Gynecol Oncol. 2016;141:247–54.
Kuji S, et al. Diagnosis, clinicopathologic features, treatment, and prognosis of small cell carcinoma of the uterine cervix; Kansai Clinical Oncology Group/Intergroup study in Japan. Gynecol Oncol. 2013;129:522–7.
Chan JK, Loizzi V, Burger RA, Rutgers J, Monk BJ. Prognostic factors in neuroendocrine small cell cervical carcinoma: a multivariate analysis. Cancer. 2003;97:568–74.
Tc C, et al. Primary surgery versus primary radiation therapy for FIGO stages I-II small cell carcinoma of the uterine cervix: a retrospective Taiwanese Gynecologic Oncology Group study. Gynecol Oncol. 2015;137:468–73.
Adams S, et al. Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol. 2014;32:2959–66.
Kadota K, et al. Prognostic impact of immune microenvironment in lung squamous cell carcinoma: tumor-infiltrating CD10+ neutrophil/CD20+ lymphocyte ratio as an independent prognostic factor. J Thorac Oncol. 2015;10:1301–10.
Shah W, et al. A reversed CD4/CD8 ratio of tumor-infiltrating lymphocytes and a high percentage of CD4(+)FOXP3(+) regulatory T cells are significantly associated with clinical outcome in squamous cell carcinoma of the cervix. Cell Mol Immunol. 2011;8:59–66.
Chen R, et al. Correlation between subsets of tumor-infiltrating immune cells and risk stratification in patients with cervical cancer. PeerJ. 2019;7: e7804.
Francisco LM, et al. PD-L1 regulates the development, maintenance, and function of induced regulatory T cells. J Exp Med. 2009;206:3015–29.
Jang TJ. Progressive increase of regulatory T cells and decrease of CD8+ T cells and CD8+ T cells/regulatory T cells ratio during colorectal cancer development. Korean J Pathol. 2013;47:443–51.
Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat Immunol. 2003;4:330–6.
Campbell DJ, Ziegler SF. FOXP3 modifies the phenotypic and functional properties of regulatory T cells. Nat Rev Immunol. 2007;7:305–10.
Xiao X, et al. Mismatch repair deficiency is associated with MSI phenotype, increased tumor-infiltrating lymphocytes and PD-L1 expression in immune cells in ovarian cancer. Gynecol Oncol. 2018;149:146–54.
Droeser RA, et al. Clinical impact of programmed cell death ligand 1 expression in colorectal cancer. Eur J Cancer. 2013;49:2233–42.
Chen YB, Mu CY, Huang JA. Clinical significance of programmed death-1 ligand-1 expression in patients with non-small cell lung cancer: a 5-year-follow-up study. Tumori. 2012;98:751–5.
Morgan S, Slodkowska E, Parra-Herran C, Mirkovic J. PD-L1, RB1 and mismatch repair protein immunohistochemical expression in neuroendocrine carcinoma, small cell type, of the uterine cervix. Histopathology. 2019;74:997–1004.
Sun X, et al. Stonin 2 overexpression is correlated with unfavorable prognosis and tumor invasion in epithelial ovarian cancer. Int J Mol Sci. 2017;18:1653.
Schildhaus H. Predictive value of PD-L1 diagnostics. Pathologe. 2018;39:498–519.
Santin AD, et al. Phase II evaluation of nivolumab in the treatment of persistent or recurrent cervical cancer (NCT02257528/NRG-GY002). Gynecol Oncol. 2020;157:161–6.
Fuchs CS, et al. Safety and efficacy of pembrolizumab monotherapy in patients with previously treated advanced gastric and gastroesophageal junction cancer: phase 2 clinical KEYNOTE-059 trial. JAMA Oncol. 2018;4: e180013.
Pages F, et al. International validation of the consensus Immunoscore for the classification of colon cancer: a prognostic and accuracy study. Lancet. 2018;391:2128–39.
Zhu M, et al. Evasion of innate immunity contributes to small cell lung cancer progression and metastasis. Can Res. 2021;81:1813–26.
Sharma P, Allison JP. The future of immune checkpoint therapy. Science. 2015;348:56–61.
Kawachi A, et al. Tumor-associated CD204(+) M2 macrophages are unfavorable prognostic indicators in uterine cervical adenocarcinoma. Cancer Sci. 2018;109:863–70.
Shen JK, et al. Programmed cell death ligand 1 expression in osteosarcoma. Cancer Immunol Res. 2014;2:690–8.
Que Y, et al. PD-L1 expression is associated with FOXP3+ regulatory T-cell infiltration of soft tissue sarcoma and poor patient prognosis. J Cancer. 2017;8:2018–25.
Jin HT, Ahmed R, Okazaki T. Role of PD-1 in regulating T-cell immunity. Curr Top Microbiol Immunol. 2011;350:17–37.
Burton OT, et al. Roles for TGF-beta and programmed cell death 1 ligand 1 in regulatory T cell expansion and diabetes suppression by zymosan in nonobese diabetic mice. J Immunol. 2010;185:2754–62.
Topalian SL, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–54.
Gadducci A, Carinelli S, Aletti G. Neuroendrocrine tumors of the uterine cervix: a therapeutic challenge for gynecologic oncologists. Gynecol Oncol. 2017;144:637–46.
Huang T, et al. Weighted gene co-expression network analysis identified cancer cell proliferation as a common phenomenon during perineural invasion. Onco Targets Ther. 2019;12:10361–74.
Borromeo MD, et al. ASCL1 and NEUROD1 reveal heterogeneity in pulmonary neuroendocrine tumors and regulate distinct genetic programs. Cell Rep. 2016;16:1259–72.
Rudin CM, et al. Molecular subtypes of small cell lung cancer: a synthesis of human and mouse model data. Nat Rev Cancer. 2019;19:289–97.
Hamanishi J, et al. Programmed cell death 1 ligand 1 and tumor-infiltrating CD8+ T lymphocytes are prognostic factors of human ovarian cancer. Proc Natl Acad Sci USA. 2007;104:3360–5.
Thompson RH, et al. Costimulatory B7–H1 in renal cell carcinoma patients: Indicator of tumor aggressiveness and potential therapeutic target. Proc Natl Acad Sci USA. 2004;101:17174–9.
Ohigashi Y, et al. Clinical significance of programmed death-1 ligand-1 and programmed death-1 ligand-2 expression in human esophageal cancer. Clin Cancer Res. 2005;11:2947–53.
Yamazaki T, et al. Expression of programmed death 1 ligands by murine T cells and APC. J Immunol. 2002;169:5538–45.
Feng YC, Ji WL, Yue N, Huang YC, Ma XM. The relationship between the PD-1/PD-L1 pathway and DNA mismatch repair in cervical cancer and its clinical significance. Cancer Manag Res. 2018;10:105–13.
Sun Y, et al. Characterization of PD-L1 protein expression and CD8 tumor-infiltrating lymphocyte density, and their associations with clinical outcome in small-cell lung cancer. Transl Lung Cancer Res. 2019;8:748–59.
AiErken N, et al. High PD-L1 expression is closely associated with tumor-infiltrating lymphocytes and leads to good clinical outcomes in chinese triple negative breast cancer patients. Int J Biol Sci. 2017;13:1172–9.
Taube JM, et al. Colocalization of inflammatory response with B7–h1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escape. Sci Transl Med. 2012;4:127ra137.
Xing D, et al. Next-generation sequencing reveals recurrent somatic mutations in small cell neuroendocrine carcinoma of the uterine cervix. Am J Surg Pathol. 2018;42:750–60.
Zhang L, et al. The role of programmed cell death ligand-1/ programmed cell death-1 (PD-L1/PD-1) in HPV-induced cervical cancer and potential for their use in blockade therapy. Curr Med Chem. 2020. https://doi.org/10.2174/0929867327666200128105459.
Wang H, Lu D. Detection of human papillomavirus DNA and expression of p16, Rb, and p53 proteins in small cell carcinomas of the uterine cervix. Am J Surg Pathol. 2004;28:901–8.
Martins P, et al. Cervical cancer patients that respond to chemoradiation therapy display an intense tumor infiltrating immune profile before treatment. Exp Mol Pathol. 2019;111: 104314.
Tumeh PC, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515:568–71.
Dora D, et al. Neuroendocrine subtypes of small cell lung cancer differ in terms of immune microenvironment and checkpoint molecule distribution. Mol Oncol. 2020;14:1947–65.
Dora D, et al. Characterization of tumor-associated macrophages and the immune microenvironment in limited-stage neuroendocrine-high and -low small cell lung cancer. Biology. 2021;10:502.
Acknowledgements
We would like to thank the native English speaking scientists of Elixigen Company (Huntington Beach, California) for editing our manuscript.
Funding
No.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. XS and LL contributed equally to this work. XS contributed to the literature review, data curation, writing the original version of this manuscript. LL participated in the experiment and edited this draft. TW performed the literature search, data collection. QH performed the data analysis and revised the manuscript. JC performed the experiment. JL and RL participated in the protocol development, study-supervision and study design. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
the Institutional Review Board of Sun Yat-sen University Cancer Center (IRB No.: YB2019-182–01).
Consent for publication
The authors declare that they give their consent for publication.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Two SCNEC cases with distinct PD-L1 and immune cell immunohistochemical patterns. Case 1:(A) Hematoxylin and eosin-stained section of SCNEC with the distribution patterns of TILs (B) The IHC of PD-L1CPS negative; (C) The IHC of PD-1 negative; (D) The IHC of infiltration by a low proportion of FOXP3 positive immune cells; (E) The IHC of infiltration by a low proportion of CD3 positive immune cells; (F) The IHC of infiltration by a low proportion of CD4 positive immune cells; (G) The IHC of infiltration by a low proportion of CD8 positive immune cells; (H) The IHC of infiltration by a low proportion of CD20 positive immune cells; (I) The IHC of infiltration by a low proportion of CD68 positive immune cells. Case2:(J) Hematoxylin and eosin-stained section of SCNEC with the distribution patterns of TILs (K)The IHC of PD-L1CPS positive; (L) The IHC of PD-1 positive; (M) The IHC of infiltration by a high proportion of FOXP3 positive immune cells; (N) The IHC of infiltration by a high proportion of CD3 positive immune cells; (O) The IHC of infiltration by a high proportion of CD4 positive immune cells; (P) The IHC of infiltration by a high proportion of CD8 positive immune cells; (Q) The IHC of infiltration by a high proportion of CD20 positive immune cells; (R) The IHC of infiltration by a high proportion of CD68 positive immune cells(The scale bar is 200μm). Figure S2. The difference of PD-L1TPS, PD-L1ICS and PD-L1CPS in dMMR and pMMR groups. (A) PD-L1 negative in dMMR (MLH1/PMS2 loss) group;(B) PD-L1 positive in pMMR group;(C)The difference of PD-L1TPS in dMMR and pMMR groups(p>0.05).(D) The difference of PD-L1ICS in dMMR and pMMR groups (p>0.05).(E) The difference of PD-L1CPS in dMMR and pMMR groups. (p>0.05). (The scale bar is 200μm). Figure S3. The difference of PD-L1CPS in P16 positive and P16 negative groups and Ki67-Low proliferation and Ki67-High proliferation groups. (A) PD-L1CPS positive in P16 negative group (B) PD-L1CPS positive in P16 positive groups; (C) PD-L1CPS negative in Ki67-Low proliferation group; (D) PD-L1CPS positive in Ki67-High proliferation group;(E) PD-L1CPS levels had no statistical correlation with P16 expression (p>0.05); (F) PD-L1CPS levels had no statistical correlation with the proliferation of Ki67 (p>0.05) (The scale bar is 200μm). Figure S4. Kaplan-Meier plots of OS and DFS in SCNEC patients. (A) OS in patients with early-stage and advance-stage.(B)OS in patients with NSE level ≤15.2U/ml and >15.2 U/ml. (C)OS in patients with and without parametrium invasion.(D) OS in patients with and without PNI. (E) DFS in patients with and without PNI. (F)DFS in patients with and without parametrium invasion. (G)DFS in patients with and without LVSI. (H) DFS in patients with stromal invasion level more or less than 1/2. (I)DFS in patients accepting postoperative therapy or not. P values are based on the log-rank test.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, X., Liu, L., Wan, T. et al. The prognostic impact of the immune microenvironment in small-cell neuroendocrine carcinoma of the uterine cervix: PD-L1 and immune cell subtypes. Cancer Cell Int 22, 348 (2022). https://doi.org/10.1186/s12935-022-02716-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-022-02716-6