Abstract
Background
Although mycobacterial glycolipids are among the first-line molecules involved in host–pathogen interactions, their contribution in virulence remains incomplete. Mycobacterium marinum is a waterborne pathogen of fish and other ectotherms, closely related to Mycobacterium tuberculosis. Since it causes tuberculosis-like systemic infection it is widely used as a model organism for studying the pathogenesis of tuberculosis. It is also an occasional opportunistic human pathogen. The M. marinum surface-exposed lipooligosaccharides (LOS) are immunogenic molecules that participate in the early interactions with macrophages and modulate the host immune system. Four major LOS species, designated LOS-I to LOS-IV, have been identified and characterized in M. marinum. Herein, we investigated the interactions between a panel of defined M. marinum LOS mutants that exhibited various degrees of truncation in the LOS structure, and human-derived THP-1 macrophages to address the potential of LOSs to act as pro- or avirulence factors.
Results
A moderately truncated LOS structure did not interfere with M. marinum invasion. However, a deeper shortening of the LOS structure was associated with increased entry of M. marinum into host cells and increased elimination of the bacilli by the macrophages. These effects were dependent on Toll-like receptor 2.
Conclusion
We provide the first evidence that LOSs inhibit the interaction between mycobacterial cell wall ligands and appropriate macrophage pattern recognition receptors, affecting uptake and elimination of the bacteria by host phagocytes.
Similar content being viewed by others
Background
Mycobacterium marinum is a waterborne pathogen that is phylogenetically related to M. tuberculosis and causes tuberculosis-like systemic infection in fish and in other ectotherms [1,2,3]. It can also induce granulomatous infection in humans called “fish tank disease” [2] and, as other nontuberculous mycobacteria, is responsible for opportunistic infections in immune-deficient patients [4]. Similar to M. tuberculosis, M. marinum is able to replicate and survive within infected host cells. As both species share a conserved skeleton of host–pathogen interactions, M. marinum is also widely used as a surrogate to decipher many aspects of the immunopathogenesis of tuberculosis [5]. Therefore it is vital to gain insight into the structure and biological significance of cell-envelope associated molecules that may be important for M. marinum immunopathology.
The uptake of mycobacteria by professional phagocytes, such as macrophages, is dependent upon the early recognition of the pathogen-associated molecular patterns (PAMPs) by specific pathogen recognition receptors (PRRs) that are crucial in initiating and driving the host immune response. Among the PRRs, Toll-like receptor 2 (TLR2) and complement receptor 3 (CR3) have been demonstrated to play key roles in macrophage-Mycobacterium interactions [6]. Among the PAMPs, phosphatidyl-myo-inositol mannosides (PIM), lipomannan (LM), lipoarabinomannan (LAM), lipoproteins or proteins, such as the Ag85 complex, have been documented to act as TLR2 and/or CR3 ligands in the early events that precede phagocytosis by macrophages [7,8,9].
A major hallmark of mycobacteria is the very thick and highly impermeable cell envelope, which plays a critical role in innate resistance to many antimicrobial agents and in directing host–pathogen interactions [10]. Although the structure, biosynthesis and physiological roles of the cell wall-associated mycolyl-arabinogalactan-peptidoglycan (mAGP) core complex have been well described [11,12,13], our knowledge regarding the (glyco)lipids interspersed within the mAGP remains incomplete in many aspects. These extractable lipids largely contribute to the modulation of the host immune system and in conditioning infection outcomes [14, 15]. They comprise the highly polar, surface-exposed lipooligosaccharides (LOSs) that have been reported in more than 10 mycobacterial species, such as Mycobacterium marinum, Mycobacterium kansasii, Mycobacterium gastri, Mycobacterium szulgai and the Mycobacterium canettii variant of Mycobacterium tuberculosis [16,17,18,19,20,21,22]. Among the different species, these glycolipids exhibit considerable structural variations in the glycan core as well as in the lipid moiety.
LOSs are of great interest, as it has been inferred that they are structurally and functionally similar to other trehalose-containing glycolipids, such as diacyltrehalose (DAT) and polyacyltrehalose (PAT) in M. tuberculosis [23]. In M. marinum, four major LOS species, designated LOS-I to LOS-IV, have been identified and characterized [24]. The structure of LOS-I comprises a glycan core consisting of trehalose, glucose and one methylated rhamnose (3-O-Me-Rhap-(1-3)-Glcp-(1-3)-Glcp-(1-4)-Glcp-(1-1)-Glcp). This oligosaccharide moiety is subsequently glycosylated by additional monosaccharides, giving rise to more polar LOS species. In addition to the glycan core, LOS-II, LOS-III and LOS-IV are substituted by α-d-Xylp. LOS-II also possesses a terminal α-caryophyllose residue (α-3,6-dideoxy-4-C-[d-altro-1,3,4,5-tetra-hydroxyhexyl]-d-xylo-hexopyranose), whereas LOS-III and LOS-IV contain two α-caryophyllose units [25]. The second caryophyllose of LOS-IV is decorated by an atypical N-acetylated dideoxy galactose [26]. Similar to other trehalose-based glycolipids, all LOS species are acylated by polymethyled fatty acids [27]. Depending on growth medium, various LOS subspecies exist in a different amount and proportion [24], indicating that M. marinum has the ability to modulate its LOS content.
LOSs are known as highly antigenic glycoconjugates exposed to the cell surface [15]. In M. marinum, they have clearly been associated with colony morphology, sliding motility and biofilm formation [28]. Although early studies suggested their involvement in macrophage uptake [25, 28], their contribution to the virulence and pathogenesis of M. marinum remains obscure. Initial work on M. kansasii indicated that rough variants devoid of LOSs induce chronic infections, whereas smooth variants producing LOSs are rapidly eliminated [29, 30], leading to the hypothesis that LOSs may be considered as avirulence determinants. The work of Alibaud et al. [31], based on a large panel of selected/generated LOS mutants led to the observation that phagocytosis of M. marinum was conditioned by the LOS pattern and pointed to an inverse correlation between LOS production and uptake by J774 murine macrophages or amoeba, which contrasted with another study in which LOS-deficient mutants were associated with impaired cell entry [28].
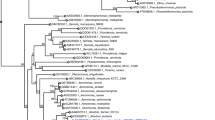
In this study, among a vast panoply of previously characterized M. marinum mutants [27, 31], producing different LOS variants due to mutations in the genes involved in the early or late stages of the LOS biosynthetic pathway, four were selected, each representing a particular step of LOS pathway inhibition (Fig. 1). Briefly, the ΔMMAR_2321 mutant that lacked the probable N-acyltransferase involved in the linkage of the pyrrolidone cycle on the α-4-amino-4,6-dideoxy-Galp residue of LOS-IV produced all LOS subspecies, except the most polar LOS-IV [31]. Disruption of MMAR_2331 leads to a mutant that is unable to produce LOS-II, LOS-III and LOS-IV; however, it accumulates LOS-II*—a LOS-II intermediate lacking the terminal caryophyllose, thus connecting MMAR_2331 to either the synthesis of caryophyllose or to its transfer on LOS-II* to produce LOS-II [31]. The ΔMMAR_2349 (wbbL2) mutant is affected at a very early step in the LOS pathway, leading to the accumulation of LOS-0—a LOS-I precursor devoid of the terminal methyl-Rha residue, which confirms the involvement of WbbL2 in rhamnose metabolism. Additionally, the accumulation of LOS-0 also leads to the synthesis of the so-called LOS-0*, most likely through the addition of another glucose residue onto the tetraglucosyl backbone of LOS-0 [31]. Disruption of MMAR_2343 (papA4) resulted in complete LOS breakdown, indicating that PapA4 fulfills the requirements for LOS acylation and assembly [27]. Described mutants were used to revisit the potential correlation between the LOS structure and mycobacterial macrophage infection.
Schematic representation of the different LOS subspecies and intermediates synthesized by the M. marinum mutants. The genes inactivated in the different mutants are indicated. Glc glucose, Me-Rha methylated rhamnose, Xyl xylopyranose, Car caryophyllose, NAcGal N-acylated dideoxygalactose, R1, R2, R3 the acyl chains
Results
Phagocytosis of M. marinum LOS mutants by THP-1 macrophages
Previous studies suggested that the presence of LOS facilitates the uptake of M. marinum by macrophages [28], whereas other studies suggested that the M. marinum strains producing shorter LOS versions, were more efficiently phagocytosed by J774 murine macrophages or by Acanthamoeba [31]. To examine the role of LOS in the uptake of M. marinum by THP-1 macrophages, the number of bacteria ingested by macrophages was determined by CFU plating after a 2-h incubation period (Fig. 2). The ability of the wild-type M. marinum strain to enter macrophages is very low (only 1 ± 0.2% of phagocytosis). However, in contrast to the wild-type strain, the mutants exhibiting truncated LOS variants were more efficiently phagocytosed by THP-1 macrophages, which is consistent with a previous study performed in J774 cells [31]. Accordingly, the phagocytosis percentage increased progressively and correlated to the decrease in the LOS structure size: 3% ± 0.4, 4% ± 0.5 and 7% ± 0.8 in the ΔMMAR_2321, ΔMMAR_2331 and ΔMMAR_2349 (wbbL2) strains, respectively. Remarkably, this phenomenon was further enhanced in the LOS-deficient MMAR_2343::Tn (papA4) mutant (12% ± 1.0). All complemented control strains were phagocytosed similarly to the wild-type strain (Fig. 2). Overall, these results show that the presence of LOS imparts the bacterial phagocytosis efficiency by macrophages.
Phagocytosis of the M. marinum mutants by macrophages. Macrophages were incubated with M. marinum strains for 2 h at an MOI of 10. Non-ingested bacteria were extensively washed and killed by gentamycin. Macrophages were lysed with Triton X-100, and then cell lysates were plated onto Middlebrook 7H10 agar supplemented with 10% OADC for CFU determination. The number of ingested bacteria are presented as the mean ± SEM from 6 to 7 separate experiments. Figure describes the difference in phagocytosis between mutants, their complemented counterparts and wild-type M. marinum. Statistical significance: *p ≤ 0.03 (Mann–Whitney U test)
Minimal LOS structure requirements for intramacrophage survival
We next addressed whether the mutants were affected in their intramacrophage survival rate. The CFU counts after 48 h of growth in THP-1 macrophages resulted in a sharp decrease in the survival of the ∆MMAR_2349 (wbbL2) and MMAR_2343::Tn (papA4) mutants compared with the wild-type strain (Fig. 3). However, the strains with less severe changes in their LOS profiles (ΔMMAR_2321, lacking LOS-IV or ΔMMAR_2331, lacking LOS-II to LOS-IV) grew similarly to the wild-type strain inside of the macrophages. These results suggest that near-complete LOS compounds are sufficient for optimal survival of M. marinum in their macrophage host.
Intracellular survival of the LOS mutants in macrophages. Macrophages were incubated with M. marinum strains for 2 h at an MOI of 10. Non-ingested bacteria were extensively washed and killed by gentamycin. Macrophages were either lysed with Triton X-100 or maintained in culture for 2 additional days prior to lysis. Cell lysates were plated onto Middlebrook 7H10 agar supplemented with 10% OADC for CFU determination. The data are presented as fold increase in CFU/ml (number of bacteria 2 days post-infection divided by the number of bacteria after 2-h of phagocytosis), expressed as the mean ± SEM from 6 to 7 separate experiments. Figure describes the difference in intracellular survival between mutants, their complemented counterparts and wild-type M. marinum. Statistical significance: *p ≤ 0.05 (Mann–Whitney U test)
Impact of M. marinum on macrophage TLR2 and CR3 surface receptor expression
TLR2 and CR3 are important cell surface recognition receptors for mycobacteria [6]; therefore, we next assessed the contribution of CR3 and TLR2 in the phagocytosis of the M. marinum strains. Macrophages were first infected with M. marinum and then stained with fluorochrome conjugated anti-TLR2 or anti-CR3 mAbs. Surface marker expression was then assessed by flow cytometry, and non-infected cells were included as controls. The median fluorescence intensity (MFI) of the non-infected macrophages amounted to 309 ± 24 and 112 ± 5 for CR3 and TLR2, respectively (Fig. 4). Infection of the cells for 2 h with either the wild-type or LOS mutant strains was accompanied by a significant increase in TLR2 expression—MFI = 195 ± 28 (wild-type), 178 ± 30 (ΔMMAR_2321), 198 ± 17 (ΔMMAR_2331), 184 ± 9 (∆MMAR_2349), 211 ± 21 (MMAR_2343::Tn). However, the CR3 expression level remained unaffected by the presence of M. marinum (Fig. 4). Together these results suggest that M. marinum induces the specific expression of TLR2, but not of CR3, in a LOS-independent manner.
Impact of the M. marinum strains on TLR2 and CR3 expression. Macrophages were incubated with the various M. marinum strains for 2 h at an MOI of 10, after which the cells were stained with fluorochrome-conjugated antibodies for 30 min at 4 °C and analyzed by flow cytometry. The data are presented as the mean median fluorescence intensity (MFI) ± SEM from five separate experiments. For statistical significance *p ≤ 0.05 (Mann–Whitney U test) the following datasets were compared: uninfected macrophages versus macrophages infected with mutants or wild-type strain
Involvement of TLR2 and CR3 in M. marinum phagocytosis
The abovementioned results prompted us to assess the contribution of CR3 and TLR2 in the phagocytosis of the M. marinum strains. Macrophages were first pre-treated with blocking anti-TLR2 or anti-CR3 mAbs prior to infection. CFUs corresponding to the ingested bacilli were then determined by plating the cellular lysates. The results clearly demonstrated that blocking of either CR3 or TLR2 strongly reduced the entry of the MMAR_2343::Tn (papA4) strain into the cells (Fig. 5). The ∆MMAR_2349 (wbbL2) mutant ingestion was also dependent on TLR2 expression but not on CR3 expression. In contrast to the MMAR_2343::Tn and ∆MMAR_2349 strains, blocking of either TLR2 or CR3 had no significant effect on the uptake of the ΔMMAR_2321 and ΔMMAR_2331 mutant or wild-type strains (Fig. 5). In control experiments we tested the phagocytosis of M. marinum strains by macrophages pre-treated with appropriate isotype control and we did not notice any influence on bacteria entry. The mean numbers of CFU/ml after a 2-h phagocytosis of wild-type and ΔMMAR_2321, ΔMMAR_2331, ΔMMAR_2349 or MMAR_2343::Tn mutants were 18,790, 30,625, 43,125, 49,386, 119,913 in the presence of isotype control to anti-TLR2 mAbs and 12,356, 33,625, 42,863, 46,410, 93,040 in the presence of isotype control to anti-CR3 mAbs, respectively. Moreover we tested the influence of blocking antibodies on activity of non-infected macrophages. We found that PMA-induced ROS generation by macrophages in the presence or absence of anti-TLR2 or anti-CR3 mAbs was similar (RLU total = 1091; 1008; 915, respectively). Secondly, the nitric oxide production (measured as nitrite) was also similar (control macrophages = 0.4 µM; macrophages + anti-TLR2 mAbs = 0.39 µM; or + anti-CR3 mAbs = 0.33 µM). These results suggest that complete, but not near-complete, lack of LOS structures facilitates interaction of TLR2 with its cell wall agonists, which increases the entry of M. marinum into host cells.
Involvement of TLR2 and CR3 in phagocytosis of the M. marinum strains by macrophages. Comparison of the M. marinum strains phagocytosis rates after blocking of macrophage TLR2 or CR3. Macrophages were pretreated with blocking antibodies (anti-TLR2 or anti-CR3) for 1 h and incubated with the M. marinum strains for 2 h at an MOI of 10. Non-ingested bacteria were extensively washed and killed by gentamycin. Macrophages were then lysed with Triton X-100 and the cell lysates were plated onto Middlebrook 7H10 agar supplemented with 10% OADC for CFU determination. The data are presented as the mean number of ingested bacteria ± SEM from six separate experiments. For statistical significance: *p ≤ 0.03, (Mann–Whitney U test) the following datasets were compared: mutant/wild-type versus mutant/wild-type + blocking antibodies
Participation of TLR2 and CR3 in the intramacrophage survival of M. marinum
The potential contribution of TLR2 and CR3 expression on intramacrophage survival was next investigated following CFU determination of intracellular bacteria after pretreatment of the cells with the corresponding blocking mAbs. The growth comparisons of the wild-type strain and the LOS mutants indicate that blocking of TLR2, but not CR3, significantly increased the replication rate of both the ∆MMAR_2349 (wbbL2) and the MMAR_2343::Tn (papA4) mutants (Fig. 6). TLR2 or CR3 blocking did not influence the intracellular growth of the wild-type strain or the ΔMMAR_2321 and ΔMMAR_2331 mutant strains. Overall, this indicates that the lack of LOS severely increases M. marinum elimination in a TLR2-dependent manner.
Involvement of TLR2 and CR3 in intracellular M. marinum survival. Macrophages were pretreated with blocking antibodies (anti-TLR2 or anti-CR3) for 1 h and incubated with M. marinum mutants for 2 h at an MOI of 10. Non-ingested bacteria were extensively washed and killed by gentamycin. Macrophages were lysed with Triton X-100 or maintained in culture for another 2 days and then lysed, plated on Middlebrook 7H10 agar supplemented with 10% OADC and cultured for CFU determination. The data are presented as fold increase in CFU/ml (number of bacteria 2 days post-infection divided by the number of bacteria after 2-h of phagocytosis), expressed as the mean ± SEM from six separate experiments. For statistical significance: *p ≤ 0.03, (Mann–Whitney U test) the following datasets were compared: mutant/wild-type versus mutant/wild-type + blocking antibodies
Discussion
Although the LOS structures and their distribution have been well studied in various mycobacterial species, their roles in pathogenesis and virulence are still unclear [25, 28,29,30, 32]. By studying a large panel of defined M. marinum mutants with impaired LOS synthesis, in a previous paper Alibaud et al. [31] demonstrated in the J774 cell line that M. marinum phagocytosis is conditioned by the LOS pattern and pointed to a clear inverse correlation between LOS production and the efficient uptake into professional phagocytic cells. The mentioned results, together with other studies done with M. marinum [32] or M. kansasii [29, 30] seem to confirm the thesis of LOSs as factors masking the bacterial ligands that are recognized by host cells. However, neither the influence of LOS inhibition on M. marinum intramacrophage survival nor their “masking” potential in host–pathogen interactions has been clearly confirmed.
In this work, the interplay between M. marinum LOS mutants and human macrophage-derived THP-1 cells was explored to address the ability of these structures to mask other mycobacterial cell wall components which, in turn, may act as potential ligands for pathogen recognition receptors. The complete absence (MMAR_2343::Tn) or synthesis of only the early LOS subspecies (ΔMMAR_2349) resulted in highly enhanced uptake by macrophages. Analysis of the MMAR_2343::Tn and ΔMMAR_2349 mutant intracellular survival revealed that both strains were effectively eliminated by the phagocytes. Conversely, the replication of two mutants with moderately impaired LOS structure (ΔMMAR_2321, lacking LOS-IV or ΔMMAR_2331, lacking LOS-II to LOS-IV) remained unchanged compared with the wild-type strain, despite the significantly increased phagocytosis rate.
To address how the various LOS profiles influence their interactions with phagocytes, we first analyzed the expression level of two major macrophage PRR in response to M. marinum infection. This resulted in a significant increase in TLR2 but not CR3 expression. Additionally, TLR2 blocking significantly reduced the uptake of the MMAR_2343::Tn (papA4) and ΔMMAR_2349 (wbbL2) mutants and increased their survival within macrophages. Moreover, the blocking of CR3 receptor indicated that it could participate in another pathway of MMAR_2343::Tn uptake, despite the fact that its expression was not significantly increased upon infection. However, CR3 blocking did not affect the intracellular survival of MMAR_2343::Tn. This is consistent with the reported role of CR3 to act as a “silent receptor”, allowing pathogenic bacteria to enter into macrophages without inducing mycobacterial killing [33, 34]. Strikingly, the fates of ΔMMAR_2321 and ΔMMAR_2331 in the early infection events seem to be TLR2- and CR3-independent.
Our results add new insight into the role of LOS, which may mask other cell wall-associated PAMPs, thereby conditioning the outcome of the infection. Moderately impaired LOS structures failed to uncover antigenic determinants that may be recognized by their cognate macrophage receptors. The increased phagocytosis of ΔMMAR_2321 and ΔMMAR_2331 may therefore result from a modified cell surface composition/architecture. In example the lack of at least LOS-IV is sufficient to reduce the release of PE_PGRS proteins from the mycobacterial cell surface [32]. Moreover high number of other secretion mutants with disruption in LOS biosynthesis region ranging from LOS-IV to complete LOS deficiency show clear correlation between LOS content and PE_PGRS release [32]. Since the strongest secretion defect is observed in LOS deficient mutants, it seems like LOS may act as a detergent for capsular proteins. However, the absence of LOS-IV resulted in an altered surface attachment of PE_PGRS proteins, indicating that the terminal sugar moiety plays a role in this process [32]. PE_PGRS proteins are substrates for the ESX-5 secretion system and implicated in virulence [35,36,37,38,39]. Therefore, LOS may play a role in the modulation of mycobacterial virulence by regulation of surface protein attachment. Similar function was also attributed to diacyltrehalose (DAT) and polyacyltrehalose (PAT) of M. tuberculosis which are closely related to LOS. Phenotypic observations made on a mutant of M. tuberculosis deficient in the biosynthesis of DAT and PAT indicated a role for these lipids in the retention of the capsular material at the cell surface. Such modification of the mutant surface properties increased its binding and uptake by phagocytic and nonphagocytic cells, but did not influence its ability to replicate and persist in cultured macrophages and in mice [23].
In ΔMMAR_2331, not only LOS-IV but also LOS-III and LOS-II production is arrested [31]. Similar to ΔMMAR_2332 [28] and ΔMMAR_2333 [40], ΔMMAR_2331 accumulates the LOS-II biosynthetic precursor (LOS-II*). The intracellular growth of these three ΔMMAR_2331-ΔMMAR_2333 mutants was not attenuated; however, only in the case of ΔMMAR_2331, a concomitant increase in host cell entry was detected.
From our structural/functional relationship studies, it can be inferred that the minimal functional LOS structure is LOS-II. The results suggest that all mutants exhibiting an unchanged or improved ability to invade macrophages require at least the LOS-0 to LOS-II* structures. Deeper changes of the LOS structure, that goes beyond LOS-II, present in the ΔMMAR_2349 (wbbL2) and MMAR_2343::Tn (papA4) mutants, exerts additional effects on the host–pathogen interaction and increases clearance of the pathogen from the host cell. Interestingly, the suggested functional LOS structure distinction corresponds to the LOS synthesis and transport. Sarkar et al. [40] proposed a model for LOS biosynthesis, wherein early intermediates up to acylated hexasaccharide comprised LOS-II* are synthesized intracellularly and then transported across the membrane. Further elongation of LOS-II* occurs on the extracytoplasmic site. We cannot exclude that by the precise regulation of extracytoplasmic glycosyltransferases, the mycobacterial cell is able to modify the final LOS structure in response to different environmental factors.
It appears that a complete or at least a near-complete LOS structure is required for survival in the host cell, and LOS-deficient strains are eliminated in a TLR2 dependent manner. Signaling through TLR2 is important for macrophage activation and induction of a protective immune response to mycobacterial infection [41]. The mycobacterial cell envelope contains many diverse TLR2 ligands, such as lipoproteins, lipoglycans and glycolipids [42]. Among the various mycobacterial glycolipids that interact with TLR2, only a limited number of TLR2 agonists have been reported in M. marinum. These include the apolar, surface-exposed dimycolyl-diarabino-glycerol (DMAG) [43]. Due to structural similarities between DMAG and other mycobacterial glycolipids that interact with TLR2 (e.g. trehalose dimycolate or glucose monomycolate), one can assume that the spectrum of molecules exposed/uncovered in the LOS mutants that promote TLR2-dependent activation is relatively broad. The phagocytosis of the MMAR_2343::Tn (papA4) mutant, in which LOS synthesis is completely blocked, appeared to be not only TLR2 but also CR3 dependent. The essential role of the abundance and composition of polysaccharides, especially PIMs, was demonstrated for the non-opsonic binding of mycobacterium to CR3 [44]. As the LOSs may be present across the whole polysaccharide-protein matrix of the mycobacterial cell wall [45], we suspect that their absence results in the reorganization and better exposure of polysaccharides that directly interact with CR3, thus promoting this phagocytosis pathway.
Conclusions
Our data confirm the roles of different structural LOS variants in modulating M. marinum interaction with phagocytes. The absence of LOS results in an unmasking of cell wall surface epitopes that are recognized by macrophage receptors, which eventually lead to a greater elimination of the pathogen. We proposed that this effect might be mediated through the TLR2 pathway. The precise regulation of the lipooligosaccharide content in response to variable environmental conditions demands further study.
Methods
Reagents and antibodies
RPMI 1640 (Roswell Park Memorial Institute) medium, fetal bovine serum (FBS), Dulbecco’s phosphate buffered saline (D-PBS) and Hanks’ balanced salt solution (HBSS) were purchased from Life Technologies (Carlsbad, CA, USA). Middlebrook 7H10 agar, Middlebrook 7H9 broth and Middlebrook OADC enrichment were acquired from Becton–Dickinson (Franklin Lakes, NJ, USA). Phorbol-12-myristate-13-acetate (PMA), Triton X-100, gentamycin, β-mercaptoethanol, penicillin (10,000 U/ml)/streptomycin (10 mg/ml) solution (P/S), Tween 80 and 4% formaldehyde (FA) solution, horseradish peroxidase (HRP), luminol, sodium nitrite, were obtained from Sigma-Aldrich (St. Louis, MO, USA). Human type AB serum was purchased from PAN-Biotech GmbH (Aidenbach, Germany). Mouse IgG2a anti-human TLR2 (sodium/azide free) mouse IgG2a isotype control (azide free), phycoerythrin (PE)-conjugated mouse IgG2a anti-TLR2 and PE-conjugated mouse IgG2aκ isotype control antibodies were obtained from Novus Biologicals (Littleton, CO, USA). Mouse IgG1κ anti-human CR3 (CD11b/Mac-1; sodium/azide free) NA/LE mouse IgG1κ isotype control (sodium/azide free), PE-conjugated mouse IgG1κ anti-human CR3, PE-conjugated NA/LE mouse IgG1 isotype control antibodies were purchased from BD Biosciences (San Jose, CA, USA).
Bacterial strains and culture conditions
The Mycobacterium marinum strain M was isolated from a human patient [3], and the M. marinum mutants—ΔMMAR_2321, ΔMMAR_2331, ΔMMAR_2349 (wbbL2), MMAR_2343::Tn (papA4) and complemented strains - ΔMMAR_2321_C, ΔMMAR_2331_C, ΔMMAR_2349_C were reported previously [31] Cultures were grown/maintained at 30 °C in 7H9 liquid or 7H10 solid medium containing 10% oleic acid, albumin, dextrose and catalase (OADC) enrichment, supplemented with hygromycin (80 µg/ml) where necessary. The two-step homologous recombination protocol [46] was used to introduce unmarked deletions into the MMAR_2321, MMAR_2331 and MMAR_2349 (wbbL2) genes of M. marinum [31]. The MMAR_2343::Tn (papA4) strain was selected through a screen of a M. marinum transposon library to identify new cell wall-defective mutants [47]. The corresponding complemented strains, designated ΔMMAR_2321_C, ΔMMAR_2331_C and ΔMMAR_2349_C, were generated through the introduction a functional copy of the genes cloned either under the control of their own promoters (MMAR_2331 and MMAR_2349) or the constitutive hsp60 promoter (MMAR_2321) in the integrative pMV306 vector [31].
For use in infection tests, M. marinum wild-type, its mutants and complemented strains were grown in Middlebrook 7H9 broth enriched with 10% OADC and 0.05% Tween 80 for 7–10 days to reach an optical density of 1 (OD600). Then, the bacteria were divided into aliquots and stored at − 70 °C. After 7 days, one aliquot of each strain was thawed, and a colony forming unit (CFU) assay was used to determine the bacteria number.
On the day of the experiment, M. marinum strains were thawed, washed in RPMI 1640 medium, and then suspended in culture medium without P/S. Then, clumps of bacteria were disrupted by multiple passages through a 25-gauge needle, and serial dilutions of bacteria in culture medium without P/S were prepared.
THP-1 cell culture
The human monocyte-macrophage cell line, THP-1 cells (ACTC TIB-202; American Type Culture Collection, Manassas, VA, USA) were used. THP-1 cells were maintained in culture medium composed of RPMI 1640 medium supplemented with 1 mM sodium pyruvate, 10% FBS, 0.05 mM β-mercaptoethanol and antibiotics—100 U/ml of penicillin and 100 μg/ml of streptomycin. The cells were passaged every 3 days.
Phagocytosis and intracellular growth of bacteria
THP-1 cells (monocytes) suspended in culture medium (see above) were distributed to 24-well plates (Nunc, Roskilde, Denmark) at the density of 105 cells/well and differentiated into macrophages during 24 h of culture with 20 ng/ml of PMA (37 °C; 5% CO2). The ability of macrophages to attach to the plastic surface of the plates was confirmed by light microscopy [48]. After replacement of culture medium without antibiotics macrophages were pretreated with 35 μg/ml of anti-TLR2 blocking monoclonal antibodies (mAb) or with 55 μg/ml of anti-CR3 blocking mAb or appropriate isotype control for 1 h (37 °C, 5% CO2) or left untreated. The mAb at the utilized concentrations were sufficient to blocking surface expression of each receptor as was described previously [49]. Prior to infection, the macrophages were equilibrated at 33 °C, 5% CO2 for 1 h according to Subbian et al. [50]. Next, phagocytes were infected with wild-type M. marinum, its mutants (MMAR_2343::Tn, ΔMMAR_2349, ΔMMAR_2321 or ΔMMAR_2331) or complemented strains (ΔMMAR_2349_C, ΔMMAR_2321_C or ΔMMAR_2331_C) at a 1:10 multiplicity of infection (MOI) and incubated for 2 h (33 °C, 5% CO2). Next, in order to remove non-ingested bacilli, macrophages were extensively washed three times with HBSS and then, to kill extracellular bacteria, phagocytes were incubated in culture medium containing 1 mg/ml of gentamycin for 1 h (37 °C, 5% CO2). The gentamycin concentration used in the experiment was determined in preliminary study and confirmed to be bactericidal towards M. marinum. After incubation, macrophages were washed two times with HBSS, and then fresh culture medium without antibiotics as well as anti-TLR2 blocking mAb or anti-CR3 blocking mAb (where required) were added, and infected phagocytes were cultured for 2 days.
On the day of infection (day 0) and 2 days post-infection, the macrophages were lysed with 1 ml of 0.2% Triton X-100 for 30 min, on ice. Appropriate dilutions of cell lysates were prepared and plated onto Middlebrook 7H10 agar supplemented with 10% of OADC. After 14 days of incubation (30 °C), the colony number was counted. For phagocytosis, the data are presented as CFUs/ml from day 0. For intracellular growth of bacteria, the data are presented as fold-increase in CFUs/ml, calculated as (CFUs/ml on day 2)/(CFUs/ml on day 0).
TLR2 and CR3 expression on macrophages infected with M. marinum strains
THP-1 cells in culture medium were distributed into 6-well plate (Nunc) at the density of 3 × 106 cells/well and differentiated into macrophages with PMA as described above and then fresh culture medium without antibiotics was added. Prior to infection, macrophages were equilibrated at 33 °C, 5% CO2 for 1 h. Next, phagocytes were infected with wild-type M. marinum or its mutants, MMAR_2343::Tn, ΔMMAR_2349, ΔMMAR_2321 and ΔMMAR_2331, at a 1:10 MOI for 2 h (33 °C, 5% CO2). Then, the non-ingested bacteria were removed by extensive washing of the macrophages with HBSS. Subsequently, phagocytes with engulfed bacteria were harvested, centrifuged (130g, 8 min) and incubated in 4% FA for 30 min at 4 °C. Thereafter, the macrophages were washed once in D-PBS supplemented with 1% FBS. Before staining with the mAbs, crystallizable fragment receptors (FcRs) were blocked using D-PBS with 10% human AB serum for 15 min at room temperature to prevent non-specific antibody binding. Afterwards, the cells were washed twice in D-PBS with 1% FBS and stained with 5 μl PE-conjugated anti-TLR2 mAb, 20 μl PE-conjugated anti-CR3 mAb or 10 μl of the appropriate isotype control for 30 min at 4 °C. Then, the cells were washed twice in D-PBS with 1% FBS, suspended in D-PBS and analyzed at once with an FACS LSR II BD flow cytometer (Becton–Dickinson, USA) that was equipped with the BD FACS Diva Software. The results are presented as median fluorescence intensity (MFI), which correlates with the surface expression of the target molecule.
Production of ROS and NO by macrophages treated with blocking antibodies
ROS production was measured using a luminol-enhanced chemiluminescence method. THP-1 cells in culture medium were distributed into 96-well black plate (Nunc) at the density of 1 × 105 cells/well and differentiated into macrophages (see above). Then, culture medium was removed and macrophages were pretreated with anti-TLR2 or anti-CR3 blocking monoclonal antibodies in HBSS as described above or cells left untreated. Thereafter, 1 μg/ml PMA (to initiate the oxygen burst) and 1 mM luminol and 40 U horseradish peroxidase (to enhance chemiluminescence were added to macrophages. Chemiluminescence was measured during 4 h at 5-min intervals using a Fluoroscan Ascent FL instrument (Labsystems, Helsinki, Finland). Data were acquired as relative light units (RLU), and the area under the curve of chemiluminescence versus assay time (total RLU) was calculated.
Production of NO by macrophages was determined using the Griess reagent (1:1 mix of 0.1% N-(1-naphthyl)ethylenediamine dihydrochloride and 1% sulfanilic acid in 5% phosphoric acid) which detect a nitrite, a stable metabolite of NO. Briefly, obtained macrophages (1 × 105 cells/well in a 96-well plate, NUNC) were treated with blocking monoclonal antibodies in culture medium for 48 h (36 °C, 5% CO2). The absorbance of culture supernatants was measured on a Multiscan RC ELISA reader (Labsystems) at wavelength of 550 nm. Nitrite concentration was calculated from a standard curve using sodium nitrite as a reference. The data were presented as nitrite concentration (μM).
Statistical analysis
The statistical evaluation of the results, which is presented as the mean ± SEM, was performed using data from 5 to 6 independent experiments. Statistical significance was verified using the Wilcoxon’s singed rank and Mann–Whitney U tests. Statistica 10.0 software was used for statistical calculations, and the statistical significance was defined as p ≤ 0.05.
References
Ramakrishnan L. Using Mycobacterium marinum and its hosts to study tuberculosis. Infect Immun. 1994;62:3222–9.
Petrini B. Mycobacterium marinum. Ubiquitous agent of waterborne granulomatous skin infections. Eur J Clin Microbiol Infect Dis. 2009;25:609–13.
Stinear TP, Seemann T, Harrison PF, Jenkin GA, Davies JK, Johnson PD, Abdellah Z, Arrowsmith C, Chillingworth T, Churcher C, Clarke K, Cronin A, Davi P, Goodhead I, Holroyd N, Jagels K, Lord A, Moule S, Mungall K, Norbertczak H, Quail MA, Rabbinowitsch E, Walker D, White B, Whitehead S, Small PL, Brosch R, Ramakrishnan L, Fischbach MA, Parkhill J, Cole ST. Insights from the complete genome sequence of Mycobacterium marinum on the evolution of Mycobacterium tuberculosis. Genome Res. 2008;18:729–41.
Ekerot L, Jacobsson L, Forsgren A. Mycobacterium marinum wrist arthritis: local and systemic dissemination caused by concomitant immunosuppressive therapy. Scand J Infect Dis. 1998;30:84–7.
Tobin DM, Ramakrishnan L. Comparative pathogenesis of Mycobacterium marinum and Mycobacterium tuberculosis. Cell Microbiol. 2008;10:1027–39.
Kleinnijenhuis J, Oosting M, Joosten LA, Netea MG, Van Crevel R. Innate immune recognition of Mycobacterium tuberculosis. Clin Dev Immunol. 2011. https://doi.org/10.1155/2011/405310.
Houben EN, Nguyen L, Pieters J. Interaction of pathogenic mycobacteria with the host immune system. Curr Opin Microbiol. 2006;9:76–85.
Jo EK. Mycobacterial interaction with innate receptors: TLRs, C-type lectins, and NLRs. Curr Opin Infect Dis. 2008;21:279–86.
Schäfer G, Jacobs M, Wilkinson RJ, Brown GD. Non-opsonic recognition of Mycobacterium tuberculosis by phagocytes. J Innate Immun. 2009;1:231–43.
Karakousis PC, Bishai WR, Dorman SE. Mycobacterium tuberculosis cell envelope lipids and the host immune response. Cell Microbiol. 2004;6:105–16.
Pavelka MS Jr, Mahapatra S, Crick DC. Genetics of peptidoglycan biosynthesis. Microbiol Spectr. 2014. https://doi.org/10.1128/microbiolspec.MGM2-0034-2013.
Jankute M, Grover S, Birch HL, Besra GS. Genetics of mycobacterial arabinogalactan and lipoarabinomannan assembly. Microbiol Spectr. 2014. https://doi.org/10.1128/microbiolspec.MGM2-0013-2013.
Pawełczyk J, Kremer L. The molecular genetics of mycolic acid biosynthesis. Microbiol Spectr. 2014. https://doi.org/10.1128/microbiolspec.MGM2-0003-2013.
Neyrolles O, Guilhot C. Recent advances in deciphering the contribution of Mycobacterium tuberculosis lipids to pathogenesis. Tuberculosis. 2001;91:187–95.
Daffe M, Crick DC, Jackson M. Genetics of capsular polysaccharides and cell envelope (glyco)lipids. Microbiol Spectr. 2014. https://doi.org/10.1128/microbiolspec.MGM2-0021-2013.
Hunter SW, Barr VL, McNeil M, Jardine I, Brennan PJ. Trehalose-containing lipooligosaccharide antigens of Mycobacterium sp. presence of a mono-O-methyltri-O-acyltrehalose ‘core’. Biochemistry. 1988;27:1549–56.
Hunter SW, Murphy RC, Clay K, Goren MB, Brennan PJ. Trehalose-containing lipooligosaccharides. A new class of species-specific antigens from Mycobacterium. J Biol Chem. 1983;258:10481–7.
Daffe M, McNeil M, Brennan PJ. Novel type-specific lipooligosaccharides from Mycobacterium tuberculosis. Biochemistry. 1991;30:378–88.
Besra GS, McNeil MR, Khoo KH, Dell A, Morris HR, Brennan PJ. Trehalose-containing lipooligosaccharides of Mycobacterium gordonae: presence of a mono-O-methyltetra-O-acyltrehalose ‘core’ and branching in the oligosaccharide backbone. Biochemistry. 1993;32:12705–14.
Gilleron M, Vercauteren J, Puzo G. Lipooligosaccharidic antigen containing a novel C4-branched 3,6-dideoxy-alpha-hexopyranose typifies Mycobacterium gastri. J Biol Chem. 1993;268:3168–79.
van Soolingen D, Hoogenboezem T, de Haas PE, Hermans PW, Koedam MA, Teppema KS, Brennan PJ, Besra GS, Portaels F, Top J, Schouls LM, van Embden JD. A novel pathogenic taxon of the Mycobacterium tuberculosis complex, Canetti: characterization of an exceptional isolate from Africa. Int J Syst Bacteriol. 1997;47:1236–45.
Boritsch EC, Frigui W, Cascioferro A, Malaga W, Etienne G, Laval F, Pawlik A, Le Chevalier F, Orgeur M, Ma L, Bouchier C, Stinear TP, Supply P, Majlessi L, Daffé M, Guilhot C, Brosch R. pks5-recombination-mediated surface remodelling in Mycobacterium tuberculosis emergence. Nat Microbiol. 2016;1:15019.
Rousseau C, Neyrolles O, Bordat Y, Giroux S, Sirakova TD, Prevost MC, Kolattukudy PE, Gicquel B, Jackson M. Deficiency in mycolipenate- and mycosanoate-derived acyltrehaloses enhances early interactions of Mycobacterium tuberculosis with host cells. Cell Microbiol. 2003;5:405–15.
Burguière A, Hitchen PG, Dover LG, Kremer L, Ridell M, Alexander DC, Liu J, Morris HR, Minnikin DE, Del A, Besra GS. LosA, a key glycosyltransferase involved in the biosynthesis of a novel family of glycosylated acyltrehalose lipooligosaccharides from Mycobacterium marinum. J Biol Chem. 2005;280:42124–33.
Rombouts Y, Burguière A, Maes E, Coddeville B, Elass E, Guérardel Y, Kremer L. Mycobacterium marinum lipooligosaccharides are unique caryophyllose-containing cell wall glycolipids that inhibit tumor necrosis factor-alpha secretion in macrophages. J Biol Chem. 2009;284:20975–88.
Rombouts Y, Elass E, Biot C, Maes E, Coddeville B, Burguière A, Tokarski C, Buisine E, Trivelli X, Kremer L, Guérardel Y. Structural analysis of an unusual bioactive N-acylated lipooligosaccharide LOS-IV in Mycobacterium marinum. J Am Chem Soc. 2010;132:16073–84.
Rombouts Y, Alibaud L, Carrère-Kremer S, Maes E, Tokarski C, Elass E, Kremer L, Guérardel Y. Fatty acyl chains of Mycobacterium marinum lipooligosaccharides: structure, localization and acylation by PapA4 (MMAR_2343) protein. J Biol Chem. 2011;286:33678–88.
Ren H, Dover LG, Islam ST, Alexander DC, Chen JM, Besra GS, Liu J. Identification of the lipooligosaccharide biosynthetic gene cluster from Mycobacterium marinum. Mol Microbiol. 2007;63:1345–59.
Collins FM, Cunningham DS. Systemic Mycobacterium kansasii infection and regulation of the alloantigenic response. Infect Immun. 1981;32:614–24.
Belisle JT, Brennan PJ. Chemical basis of rough and smooth variation in mycobacteria. J Bacteriol. 1989;171:3465–70.
Alibaud L, Pawelczyk J, Gannoun-Zaki L, Singh VK, Rombouts Y, Drancourt M, Dziadek J, Guérardel Y, Kremer L. Increased phagocytosis of Mycobacterium marinum mutants defective in lipooligosaccharide production: a structure-activity relationship study. J Biol Chem. 2014;289:215–28.
van der Woude AD, Sarkar D, Bhat A, Sparrius M, Raadsen SA, Boon L, Geurtsen J, van der Sar AM, Luirink J, Houben EN, Besra GS, Bitter W. Unexpected link between lipooligosaccharide biosynthesis and surface protein release in Mycobacterium marinum. J Biol Chem. 2012;287:20417–29.
Rooyakkers AW, Stokes RW. Absence of complement receptor 3 results in reduced binding and ingestion of Mycobacterium tuberculosis but has no significant effect on the induction of reactive oxygen and nitrogen intermediates or on the survival of the bacteria in resident and interferon-gamma activated macrophages. Microb Pathog. 2005;39:57–67.
Korbel DS, Schneider BE, Schaible UE. Innate immunity in tuberculosis: myths and truth. Microbes Infect. 2008;10:995–1004.
Ramakrishnan L, Federspiel NA, Falkow S. Granuloma-specific expression of Mycobacterium virulence proteins from the glycine-rich PE-PGRS family. Science. 2000;288:1436–9.
Abdallah AM, Verboom T, Weerdenburg EM, Gey van Pittius NC, Mahasha PW, Jiménez C, Parra M, Cadieux N, Brennan MJ, Appelmelk BJ, Bitter W. PPE and PE_PGRS proteins of Mycobacterium marinum are transported via the type VII secretion system ESX-5. Mol Microbiol. 2009;73:329–40.
Dheenadhayalan V, Delogu G, Brennan MJ. Expression of the PE_PGRS 33 protein in Mycobacterium smegmatis triggers necrosis in macrophages and enhanced mycobacterial survival. Microbes Infect. 2006;8:262–72.
Koh KW, Lehming N, Seah GT. Degradation-resistant protein domains limit host cell processing and immune detection of mycobacteria. Mol Immunol. 2009;46:1312–8.
Singh VK, Berry L, Bernut A, Singh S, Carrère-Kremer S, Viljoen A, Alibaud L, Majlessi L, Brosch R, Chaturvedi V, Geurtsen J, Drancourt M, Kremer L. A unique PE_PGRS protein inhibiting host cell cytosolic defenses and sustaining full virulence of Mycobacterium marinum in multiple hosts. Cell Microbiol. 2016;18:1489–507.
Sarkar D, Sidhu M, Singh A, Chen J, Lammas DA, der Sar AM, Besra GS, Bhatt A. Identification of a glycosyltransferase from Mycobacterium marinum involved in addition of a caryophyllose moiety in lipooligosaccharides. J Bacteriol. 2011;193:2336–40.
Underhill DM, Ozinsky A, Smith KD, Aderem A. Toll-like receptor-2 mediates mycobacteria-induced proinflammatory signaling in macrophages. Proc Natl Acad Sci USA. 1999;96:14459–63.
Goldberg MF, Saini NK, Porcelli SA. Evasion of innate and adaptive immunity by Mycobacterium tuberculosis. Microbiol Spectr. 2014. https://doi.org/10.1128/microbiolspec.MGM2-0005-2013.
Elass-Rochard E, Rombouts Y, Coddeville B, Maes E, Blervaque R, Hot D, Kremer L, Guérardel Y. Structural determination and Toll-like receptor 2-dependent proinflammatory activity of dimycolyl-diarabino-glycerol from Mycobacterium marinum. J Biol Chem. 2012;287:34432–44.
Cywes C, Hoppe HC, Daffé M, Ehlers MR. Nonopsonic binding of Mycobacterium tuberculosis to complement receptor type 3 is mediated by capsular polysaccharides and is strain dependent. Infect Immun. 1997;65:4258–66.
Ortalo-Magné A, Lemassu A, Lanéelle MA, Bardou F, Silve G, Gounon P, Marchal G, Daffé M. Identification of the surface-exposed lipids on the cell envelopes of Mycobacterium tuberculosis and other mycobacterial species. J Bacteriol. 1996;178:456–61.
Parish T, Stoker NG. Use of a flexible cassette method to generate a double unmarked Mycobacterium tuberculosis tlyA plcABC mutant by gene replacement. Microbiology. 2000;146:1969–75.
Alibaud L, Rombouts Y, Trivelli X, Burguière A, Cirillo SL, Cirillo JD, Dubremetz JF, Guérardel Y, Lutfalla G, Kremer L. A Mycobacterium marinum TesA mutant defective for major cell wall-associated lipids is highly attenuated in Dictyostelium discoideum and zebrafish embryos. Mol Microbiol. 2011;80:919–34.
Brzezinska M, Szulc I, Brzostek A, Klink M, Kielbik M, Sulowska Z, Pawelczyk J, Dziadek J. The role of 3-ketosteroid 1(2)-dehydrogenase in the pathogenicity of Mycobacterium tuberculosis. BMC Microbiol. 2013;13:43.
Klink M, Brzezinska M, Szulc I, Brzostek A, Kielbik M, Sulowska Z, Dziadek J. Cholesterol oxidase is indispensable in the pathogenesis of Mycobacterium tuberculosis. PLoS ONE. 2013;8(9):e73333.
Subbian S, Mehta PK, Cirillo SL, Cirillo JD. The Mycobacterium marinum mel2 locus displays similarity to bacterial bioluminescence systems and plays a role in defense against reactive oxygen and nitrogen species. BMC Microbiol. 2007;7:4.
Authors’ contributions
MKl, IS-K, MK and JD conceived and designed the experiments; IS-K, MK, JP conducted the experiments; MKl, JP, IS-K, MK, LK and JD analyzed the data; MKl and JD contributed reagents/materials/analysis tools; IS-K, MKl, JP drafting manuscript; MKl, JP, LK and JD wrote and approved the paper. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Not applicable.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable. The manuscript does not report data from humans or animals.
Funding
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Szulc-Kielbik, I., Pawelczyk, J., Kielbik, M. et al. Severe inhibition of lipooligosaccharide synthesis induces TLR2-dependent elimination of Mycobacterium marinum from THP1-derived macrophages. Microb Cell Fact 16, 217 (2017). https://doi.org/10.1186/s12934-017-0829-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12934-017-0829-z