Abstract
Background
The triglyceride glucose (TyG) index, as a reliable marker of insulin resistance, is associated with the incidence and poor prognosis of various cardiovascular diseases. However, the relationship between the TyG index and clinical outcomes in patients with severe aortic stenosis (AS) who underwent transcatheter aortic valve replacement (TAVR) remains unclear.
Methods
This study consecutively enrolled 1569 patients with AS underwent TAVR at West China Hospital of Sichuan University between April 2014 and August 2023. The outcomes of interest included all-cause mortality, cardiovascular mortality, and major adverse cardiovascular events (MACE). Multivariate adjusted Cox regression and restricted cubic splines (RCS) regression analyses were used to assess the associations between the TyG index and the clinical outcomes. The incremental prognostic value of the TyG index was further assessed by the time-dependent Harrell’s C-index, integrated discrimination improvement (IDI) and the net reclassification improvement (NRI).
Results
During a median follow-up of 1.09 years, there were 146, 70, and 196 patients experienced all-cause death, cardiovascular death, and MACE, respectively. After fully adjusting for confounders, a per-unit increase of TyG index was associated with a 441% (adjusted HR: 5.41, 95% CI: 4.01–7.32), 385% (adjusted HR: 4.85, 95% CI: 3.16–7.43), and 347% (adjusted HR: 4.47, 95% CI: 3.42–5.85) higher risk of all-cause mortality, cardiovascular mortality and MACE, respectively. The RCS regression analyses revealed a linear association between TyG index and endpoints (all P for non-linearity > 0.05) with 8.40 as the optimal binary cutoff point. Furthermore, adding TyG index to the basic risk model provided a significant incremental value in predicting poor prognosis (Time-dependent Harrell’s C-index increased for all the endpoints; All-cause mortality, IDI: 0.11, P < 0.001; NRI: 0.32, P < 0.001; Cardiovascular mortality, IDI: 0.043, P < 0.001; NRI: 0.37, P < 0.001; MACE, IDI: 0.092, P < 0.001; NRI: 0.32, P < 0.001).
Conclusions
In patients with severe AS receiving TAVR, there was a positive linear relationship between TyG index and poor prognosis, with 8.4 as the optimal bivariate cutoff value. Our findings suggest TyG index holds potential value for risk stratification and guiding therapeutic decisions in patients after TAVR.
Similar content being viewed by others
Background
Aortic stenosis (AS) is the most common valvular disease worldwide that significantly worsens with age and is associated with a grim prognosis [1]. Transcatheter aortic valve replacement (TAVR) is now being considered a valid alternative to surgery for patients with symptomatic severe AS, regardless of the Society of Thoracic Surgeons Predicted Risk of Mortality (STS-PROM) level [2,3,4]. As more and more low risk as well as younger patients become the candidates for TAVR, it is crucial to strengthen preoperative prognostic assessment [5]. While the factors that influence the prognosis of TAVR are still largely unknown till now, especially in terms of metabolism-related indicators [6, 7].
Previous studies have shown that metabolic abnormalities, primarily in metabolic syndrome and diabetes, are associated with an increased prevalence of aortic valve calcification, faster disease progression of AS, and worse outcome in patients with AS [8,9,10,11]. Insulin resistance (IR), as a central feature of metabolic syndrome, type 2 diabetes and its associated metabolic abnormalities [9, 12], could be a key mediator of these associations. Patients with severe AS who need to receive TAVR may exhibit higher IR [13]. After solving the structural problems of aortic valve by TAVR, these metabolic abnormalities may still continue and have severe adverse effects [14]. IR has been proved to be strongly associated with the incidence of various cardiovascular diseases [15,16,17] and poor prognosis [13, 18, 19]. However, to date, there have been no studies investigating the relationship between IR and prognosis in patients with severe AS underwent TAVR.
Considering the limitations of traditional IR measurements, the triglyceride-glucose (TyG) index has been suggested as a reliable surrogate marker, offering advantages of simplicity, rapidity, and cost-effectiveness. As an easily obtainable marker, the TyG index may provide valuable insights to better predict clinical outcomes in patients undergoing TAVR from a metabolic perspective. Therefore, we aimed to assess the prognostic value of IR using the TyG index in patients who undergoing TAVR for severe AS at a high-volume heart center for nearly 10 years.
Materials and methods
Study design and population
This is a single-center retrospective analysis of consecutive patients who underwent TAVR procedures for symptomatic severe AS at West China Hospital, Sichuan University from April 2012 to August 2023. Our multidisciplinary heart team discussed the indication for TAVR in all patients accounting for age, estimated life expectancy, comorbidities, anatomical and procedural characteristics, feasibility of vascular access, the risks of operation, bioprosthetic valve durability, and the long-term outcomes. TAVR procedures were performed according to standard clinical practice [2, 20]. Most of the patients in our study used the domestic Venus valve with strong radical force, to tackle the more calcified anatomy of the Chinese population [21].
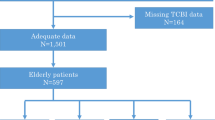
Of the 1825 patients, 256 were excluded for meeting the exclusion criteria, i.e., (1) lack follow-up data (n = 112); (2) without data for TyG index (n = 67); (3) missing other covariates (n = 77). A total of 1569 patients were included in our final analyses and were divided into three groups based on tertiles and set the first tertile as the reference: group 1 (TyG < 8.22, n = 523), group 2 (8.22 ≤ TyG ≤ 8.61, n = 523), and group 3 (TyG > 8.61, n = 523) (Additional file 1: Fig. 1). This retrospective study was performed in line with the Declaration of Helsinki, with the approval from the ethics committee of West China Hospital. Written informed consent was obtained from all patients.
Data collection and definitions
The demographic data, laboratory test data, medical history, echocardiogram data, and medication at discharge after TAVR of all patients were collected from our electronic data collection system and subjected to double verification. All comorbidities were defined based on ICD-10 codes according to medical diagnosis. STS-PROM scores were calculated by the professional cardiologists. All the baseline characteristics and clinical treatment data were prospectively collected before TAVR. All patients underwent an overnight fast (> 8 h) and venous blood samples were collected the following morning. Laboratory measurements of key hematological parameters, including total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), triglyceride (TG), and fasting plasma glucose (FPG), were uniformly detected by the department of laboratory medicine using the Roche Cobas c 702 analyzer (Roche Diagnostics GmbH, Mannheim, Germany). Body mass index (BMI) was calculated via weight (kilograms) divided by height (meters) squared. The TyG index was calculated as ln (TG [mg/dl] × FPG [mg/dl]/2).
Endpoint and follow-up
The primary endpoints were all-cause mortality and cardiovascular mortality. The secondary endpoint was Major Adverse Cardiovascular Events (MACE) including nonfatal stroke, nonfatal myocardial infarction, readmission for acute heart failure, and all-cause mortality during the follow-up. TAVR procedural complications in these patients were also collected. All patients were followed up at 1, 3, 6, and 12 months after TAVR and annually thereafter.
Statistical analyses
The patients were divided into three groups according to the tertiles of TyG index. Continuous and categorical baseline statistics were described as means (SD), median (interquartile range), or number and percentage when appropriate. Baseline data comparisons were conducted using analysis of variance (ANOVA) for normally distributed data, Kruskal-Wallis H test for skewed data, and chi-square test/Fisher’s exact test for categorical variables to assess the differences among TyG groups.
Chi-square tests and linear-by-linear association analyses were conducted to calculate P-values and P for trend per tertile increase of TyG index for TAVR procedural complications. The cumulative event rates of all the endpoints were calculated using the Kaplan-Meier method and compared using the log-rank test. Cox proportional hazards regression models were used to evaluate the independent relationships between the TyG index and outcomes in patients after TAVR. Hazard ratios (HR) and 95% confidence interval (CI) were also reported. Three models were established: Model 1, unadjusted; Model 2, adjusted for age and sex; Model 3, as the primary result, was the final multivariate adjustment model. Variables that demonstrated a P-value < 0.05 in the univariate Cox analysis and those clinically considered to be associated with the endpoints in TAVR patients (included sex, BMI, diabetes, and cerebral vascular disease) were included in the final multivariate Cox regression model.
Multivariate adjusted restricted cubic splines (RCS) based on Cox regression models were used to explore the dose-response relationships between TyG index and the incidence of all endpoints, with four knots at the 5th, 35th, 65th, and 95th percentiles of the distribution. TyG values for which HRs equaled 1 in the RCS curves were selected as the optimal binary cutoff points for the three endpoints. In addition, time-dependent Harrell’s C-index, integrated discrimination improvement (IDI), and category-free net reclassification index (NRI) were used to assess the incremental prognostic value of the TyG index in the final fitted Cox regression models. IDI quantified the difference in the integrated sensitivity minus that of specificity over all possible cut-off values between two predictive models; and the category-free NRI reflected the improvement in classification rates by one model over the other based upon a continuous risk scale.
Subgroup analyses based on sex, age (< / ≥ 75 years), STS-PROM levels, and left ventricular ejection fraction (LVEF) (< / ≥ 50%) were performed to investigate the consistency of the prognostic impact of TyG index on outcomes. Likelihood ratio tests were executed to examine modifications and interactions between subgroups. Given the obvious differences in the 30-day endpoint rates among the different TyG groups after TAVR, patients with short-term deaths may have multiple serious illnesses or experienced TAVR-related mortality, which potentially have confounding high TyG values and high mortality or MACE. Therefore, we additionally conducted a 30-day landmark analysis. Finally, multivariate adjusted Cox regression analyses were repeated after excluding patients with cancer or severe renal insufficiency (eGFR < 30 ml/min/1.73 m2).
All data analyses were performed using R version 4.1.3 (R Foundation for Statistical Computing, Vienna, Austria) and the Statistical Package for Social Sciences IBM (SPSS-IBM), version 24 (SPSS Inc., Chicago, Illinois, USA). A two-sided P value < 0.05 was considered statistically significant.
Results
Baseline characteristics
The comparisons of baseline characteristics based on TyG index tertiles were presented in Table 1. The mean age of this cohort was 72.86 ± 7.63 years, and 901 (57.43%) were male. Compared with group 1 and group 2, group 3 with the higher TyG index generally had a higher proportion of diabetes and other complications. The STS-PROM score of the overall cohort was 4.50% ± 4.27%, and the highest STS-PROM score being in the group 3, at 4.90% ± 5.32%. The majority of patients were performed intervention via a femoral artery approach (99.04%), and were implanted with a self-expanding valve (81.90%).
Associations between the TyG index and endpoints
As presented in Table 1 in the additional file 1, there was no significant difference in the incidence of TAVR procedural complications across the three groups. During a median follow-up period of 1.09 years (IQR: 0.51–2.69), there were 146 (9.31%), 70 (4.46%), and 196 (12.49%) cases experienced all-cause mortality, cardiovascular mortality and MACE, respectively. As shown in Fig. 1, Kaplan-Meier curve analyses revealed the marked differences among three TyG groups for three endpoints (all P-values for log-rank test < 0.0001). The variables included in the fully Cox regression analyses were shown in Table 2 in the additional file 1.
In fully multivariate Cox analysis, when the TyG index was regarded as a tripartite variable in Table 2, group 3 and 2 showed a significantly higher risk of all-cause mortality [group 3 vs. group 1, adjusted HR (aHR) = 9.48, 95% CI: 5.41–16.61; group 2 vs. group 1, aHR = 3.03, 95% CI: 1.66–5.51], cardiovascular mortality (group 3 vs. group 1, aHR = 11.61, 95% CI: 4.75–28.40; group 2 vs. group 1, aHR = 3.81, 95% CI: 1.48–9.77), and MACE (group 3 vs. group 1, aHR = 7.26, 95% CI: 4.59–11.49; group 2 vs. group 1, aHR = 2.84, 95% CI: 1.76–4.59). When the TyG index was evaluated on a continuous scale, the positive correlations between TyG index and endpoints still existed. Specifically, for a per-unit increase of TyG index, the risk of all-cause mortality, cardiovascular mortality, and MACE increased by 441% (aHR: 5.41, 95% CI: 4.01–7.32), 385% (aHR: 4.85, 95% CI: 3.16–7.43), and 347% (aHR: 4.47, 95% CI: 3.42–5.85), respectively (Table 2). Both unadjusted and multivariate adjusted RCS regression analyses revealed a linear association between the TyG index and the risk of all-cause mortality, cardiovascular mortality, and MACE (all P-values for non-linearity > 0.05, Fig. 2). For all the endpoints, a TyG index of 8.40, at which the HR equaled 1, was identified as the optimal bivariate cut-off value (Fig. 2).
Restricted spline curves of the TyG index hazard ratios for the endpoints. A All-cause mortalityunadjusted. B Cardiovascular mortalityunadjusted. C MACEunadjusted. D All-cause mortalityadjusted. E Cardiovascular mortalityadjusted. F MACEadjusted. TyG, Triglyceride glucose; MACE, Major adverse cardiovascular event; HR Hazard ratio; CI Confidence interval; Ref, Reference
Incremental predictive value of TyG index
Previous TAVR mortality prediction models usually did not include metabolic indicators as components. The incremental predictive values of the TyG index for endpoints were assessed using the final fitted multivariable Cox regression model components (basic model). After the TyG index was added, the time-dependent Harrell’s C-index of the basic models for all endpoints showed an increase (Fig. 3). In addition, the TyG index had significant incremental value in predicting poor prognosis for basic model (Table 3; All-cause mortality, IDI: 0.11, P < 0.001; NRI: 0.32, P < 0.001; Cardiovascular mortality, IDI: 0.043, P < 0.001; NRI: 0.37, P < 0.001; MACE, IDI: 0.092, P < 0.001; NRI: 0.32, P < 0.001).
Subgroup analyses
The subgroup analysis showed that the associations of the TyG index tertiles with the risk of the three endpoints were consistent with the main findings in most subgroups (Additional file 1: Fig. 2). Effect modifications were observed between TyG index and sex regarding the all-cause mortality (P for interaction: 0.033). Therefore, we further repeated the analysis for male and female separately, and multivariate adjusted RCS analysis found that female had a higher TyG index binary cutoff value than male (8.48 for female in Additional file 1: Fig. 3 vs. 8.35 for male in Additional file 1: Fig. 4), while male had a higher risk per unit TyG index increase compared to female in the multivariable adjusted Cox model in Table 3. in the additional file 1.
Sensitivity analyses
Sensitivity analysis further confirmed the robustness of the results. After excluding patients who died within 30 days after TAVR, the significant differences among three TyG groups still existed (all P-values < 0.001, Additional file 1: Fig. 5). Furthermore, the associations between TyG tripartite groups and different endpoints were still consistent with the main results after excluding patients with cancer or severe renal dysfunction (Additional file 1: Fig. 6).
Discussion
To our knowledge, this is the first study to identify the association between the TyG index and outcomes of AS patients who underwent TAVR. The primary findings of our research are as follows: (1) The TyG index, whether analyzed as a continuous or a categorical variable, was independently associated with all-cause mortality, cardiovascular mortality, and MACE after adjusting for the confounding factors; (2) the associations between the TyG index and all the endpoints were positively linear, with the optimal binary cutoff point of 8.40 for distinguishing poor prognosis; and (3) the TyG index enhanced the predictive ability for poor prognosis when added to the basic traditional risk model in TAVR patients (Additional file 1: Graphical Abstract Image).
IR, which is closely associated with cardiovascular diseases [22], involves the disruption of various molecular pathways in response to insulin stimulation in target tissues [23]. The hyperinsulinemic-euglycemic clamp was considered the gold standard method for assessing insulin sensitivity in vivo [23]. However, its application was limited by complex clinical procedures and high costs [24]. As a convenient, economical and reliable indicator to evaluate IR, the TyG index was not only closely associated with the incidence of various cardiovascular diseases, such as atrial fibrillation [25], coronary artery disease [26], arterial stiffness [27], and heart failure [28], but also highly correlated to the mortality in patients with cardiovascular diseases [13, 18]. TAVR, as a new interventional technology, with the gradual expansion of indications, more and more patients are being treated with this procedure. Nonetheless, many risk factors affecting outcomes after TAVR remain largely unidentified, especially in terms of serological markers [7]. Innovative, easily accessible clinical predictors to better determine prognostic outcomes in patients receiving TAVR are urgently needed [29]. Our study provides robust evidence of a significant correlation between the convenient serological marker TyG index and the intermediate-term outcomes of AS patients who underwent TAVR. In addition, we have established a prognostic TyG cutoff that helped identify high-risk patients post-TAVR, thus promoting enhanced comprehensive discharge management, which can be practical and informative.
Our study demonstrated that a higher IR was associated with a worse medium-term prognosis for severe AS patients, even after TAVR treatment. These results aligned with the outcomes previously observed in patients with coronary artery disease undergoing coronary artery bypass grafting or percutaneous coronary intervention [30, 31]. It underscores that the TyG index can predict not only the risk and natural prognosis of cardiovascular diseases but also the outcomes following interventional therapies. The results of subgroup analysis were basically consistent with the main findings, affirming the robustness of this study. Interestingly, there was a significant interaction between sex and TyG index, with a higher cutoff value for endpoints in female (8.48 vs. 8.35) and a greater impact on the outcomes per unit of TyG index change in male. Increased IR in menopausal women with reduced estrogen levels may be the reason for the higher binary cutoff value of TyG index in the female population [32]. In our study, female also had significantly higher TyG values than male (P < 0.001). A post-hoc analysis from the Specimen and Data Repository Information Coordinating Center identified a higher TyG index was correlated with greater risks of MACE in male, but not in female [33]. Similarly, a large sample study from the National Health and Nutrition Examination Survey also reported that the elevated TyG index meant a higher risk of mortality in male than female [34].
Our study identified several potential clinical implications. Firstly, the TyG index cutoff value of 8.4 identified by the RCS analysis in TAVR patients was similar to the results in moderate and severe AS patients from Huang et al. [13], indicating potential for future risk stratification in AS patients undergoing TAVR based on this threshold. Several clinical trials aimed at reducing IR have already shown positive effects on the prognosis of other cardiovascular diseases [35, 36]. Combined with the findings of this study, managing IR in TAVR patients with high TyG index may potentially improve the prognosis. Doctors should emphasize known strategies that improve insulin resistance, such as weight reduction, adherence to medication as well as a healthy diet, and engagement in regular physical exercise [37]. Secondly, the IDI and NRI metrics showed the TyG index could be a crucial component in constructing prognostic models for TAVR patients. However, metabolism-related indicators were not included in the traditional mortality prediction models for patients post-TAVR [38], which might significantly limit the predictive power of the model. Future studies are needed to validate these findings in larger and more diverse populations across different centers. Additional prospective studies are also needed to determine whether pre-TAVR interventions for IR can improve clinical outcomes.
Although the mechanisms by which IR affects the prognosis of TAVR patients remain unclear, the following are potential mechanisms: (1) Metabolism disturbances. A study by Perry et al. indicated that different metabolic profiles in TAVR patients could influence the outcomes after the procedure [39]. (2) Fibrinolysis and thrombosis. IR can disrupt fibrinolysis and coagulation, leading to fibrinolysis and thrombosis, which may be associated with thrombosis and lead to adverse outcomes [37, 40]. (3) Impaired endothelial cell function. IR can damage endothelial cell function through various ways, thereby triggering cardiovascular disease and aggravating poor prognosis [41, 42]. However, these associations require further confirmation.
The study also had several limitations. Firstly, as a retrospective study, it confronted unavoidable confounders. For instance, we did not conduct a frailty assessment, which may be associated with adverse outcomes. Nevertheless, in the final multivariable Cox model, we adjusted for over 20 variables (including heart failure, NYHA class, serum albumin, BMI, and the presence of ten comorbidities, which may partially reflect frailty). And the robustness of our study findings was further validated by various sensitivity analyses conducted. Secondly, we did not monitor the dynamic changes of the TyG index post-discharge, nor did we document factors that could affect TG and glucose levels, such as dietary and physical activity variations. Thirdly, the majority of the cohort were treated with self-expanding valves. Further investigations are necessary to elucidate the impact of the TyG index on clinical outcomes in patients with balloon-expandable valves. Lastly, given that this study was conducted at a single center in China, its findings have limited applicability to populations in other countries.
Conclusion
In summary, our study is the first to demonstrate a positive linear relationship between IR assessed by the TyG index and all-cause mortality, cardiovascular mortality, and MACE in patients with severe AS undergoing TAVR. This study identified a TyG index of 8.4 as the optimal bivariate cutoff value for predicting poor outcomes. The findings suggest that the TyG index holds potential value for risk stratification and guiding therapeutic decisions in patients after TAVR.
Data availability
No datasets were generated or analysed during the current study.
References
Carabello BA. Introduction to aortic stenosis. Circ Res. 2013;113:179–85.
Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364:2187–98.
Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019;380:1695–705.
Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, et al. Transcatheter or Surgical aortic-valve replacement in Intermediate-Risk patients. N Engl J Med. 2016;374:1609–20.
Makkar RR, Kapadia S, Chakravarty T, Cubeddu RJ, Kaneko T, Mahoney P, et al. Outcomes of repeat transcatheter aortic valve replacement with balloon-expandable valves: a registry study. Lancet. 2023;402:1529–40.
Ludman PF, Moat N, de Belder MA, Blackman DJ, Duncan A, Banya W, et al. Transcatheter aortic valve implantation in the United Kingdom: temporal trends, predictors of outcome, and 6-year follow-up: a report from the UK Transcatheter aortic valve implantation (TAVI) Registry, 2007 to 2012. Circulation. 2015;131:1181–90.
Penso M, Pepi M, Fusini L, Muratori M, Cefalù C, Mantegazza V, et al. Predicting Long-Term Mortality in TAVI patients using machine learning techniques. J Cardiovasc Dev Dis. 2021;8:44.
Katz R, Wong ND, Kronmal R, Takasu J, Shavelle DM, Probstfield JL, et al. Features of the metabolic syndrome and diabetes mellitus as predictors of aortic valve calcification in the multi-ethnic study of atherosclerosis. Circulation. 2006;113:2113–9.
Capoulade R, Clavel M-A, Dumesnil JG, Chan KL, Teo KK, Tam JW, et al. Insulin Resistance and LVH progression in patients with calcific aortic stenosis: a Substudy of the ASTRONOMER trial. JACC: Cardiovasc Imaging. 2013;6:165–74.
Briand M, Lemieux I, Dumesnil JG, Mathieu P, Cartier A, Després J-P, et al. Metabolic syndrome negatively influences disease progression and prognosis in aortic stenosis. J Am Coll Cardiol. 2006;47:2229–36.
Ram E, Kogan A, Levin S, Fisman EZ, Tenenbaum A, Raanani E, et al. Type 2 diabetes mellitus increases long-term mortality risk after isolated surgical aortic valve replacement. Cardiovasc Diabetol. 2019;18:31.
Zangeneh F, Kudva YC, Basu A. Insulin sensitizers. Mayo Clin Proc. 2003;78:471–9.
Huang R, Xu X, Xu C, Zhang S, Xiong Z, Liu M, et al. Association between the insulin resistance and all-cause mortality in patients with moderate and severe aortic stenosis: a retrospective cohort study. Cardiovasc Diabetol. 2023;22:238.
Xiong T-Y, Liu C, Liao Y-B, Zheng W, Li Y-J, Li X, et al. Differences in metabolic profiles between bicuspid and tricuspid aortic stenosis in the setting of transcatheter aortic valve replacement. BMC Cardiovasc Disord. 2020;20:229.
Yang Y, Huang X, Wang Y, Leng L, Xu J, Feng L, et al. The impact of triglyceride-glucose index on ischemic stroke: a systematic review and meta-analysis. Cardiovasc Diabetol. 2023;22:2.
Huang R, Lin Y, Ye X, Zhong X, Xie P, Li M, et al. Triglyceride-glucose index in the development of heart failure and left ventricular dysfunction: analysis of the ARIC study. Eur J Prev Cardiol. 2022;29:1531–41.
Gao Q, Lin Y, Xu R, Luo F, Chen R, Li P, et al. Positive association of triglyceride-glucose index with new-onset hypertension among adults: a national cohort study in China. Cardiovasc Diabetol. 2023;22:58.
Zhang R, Shi S, Chen W, Wang Y, Lin X, Zhao Y, et al. Independent effects of the triglyceride-glucose index on all-cause mortality in critically ill patients with coronary heart disease: analysis of the MIMIC-III database. Cardiovasc Diabetol. 2023;22:10.
Miao M, Zhou G, Bao A, Sun Y, Du H, Song L, et al. Triglyceride-glucose index and common carotid artery intima-media thickness in patients with ischemic stroke. Cardiovasc Diabetol. 2022;21:43.
Popma JJ, Adams DH, Reardon MJ, Yakubov SJ, Kleiman NS, Heimansohn D, et al. Transcatheter aortic valve replacement using a self-expanding bioprosthesis in patients with severe aortic stenosis at extreme risk for surgery. J Am Coll Cardiol. 2014;63:1972–81.
He J-J, Xiong T-Y, Yao Y-J, Peng Y, Wei J-F, He S, et al. Sex difference in outcomes following transcatheter aortic valve replacement in bicuspid aortic stenosis. JACC Cardiovasc Interv. 2022;15:1652–60.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17:122.
Li M, Chi X, Wang Y, Setrerrahmane S, Xie W, Xu H. Trends in insulin resistance: insights into mechanisms and therapeutic strategy. Signal Transduct Target Ther. 2022;7:216.
Cersosimo E, Solis-Herrera C, Trautmann ME, Malloy J, Triplitt CL. Assessment of pancreatic β-cell function: review of methods and clinical applications. Curr Diabetes Rev. 2014;10:2–42.
Azarboo A, Behnoush AH, Vaziri Z, Daneshvar MS, Taghvaei A, Jalali A, et al. Assessing the association between triglyceride-glucose index and atrial fibrillation: a systematic review and meta-analysis. Eur J Med Res. 2024;29:118.
Liang S, Wang C, Zhang J, Liu Z, Bai Y, Chen Z, et al. Triglyceride-glucose index and coronary artery disease: a systematic review and meta-analysis of risk, severity, and prognosis. Cardiovasc Diabetol. 2023;22:170.
Wang S, Shi J, Peng Y, Fang Q, Mu Q, Gu W, et al. Stronger association of triglyceride glucose index than the HOMA-IR with arterial stiffness in patients with type 2 diabetes: a real-world single-centre study. Cardiovasc Diabetol. 2021;20:82.
Xu L, Wu M, Chen S, Yang Y, Wang Y, Wu S, et al. Triglyceride-glucose index associates with incident heart failure: a cohort study. Diabetes Metab. 2022;48:101365.
Hu X, Feng D, Zhang Y, Wang C, Chen Y, Niu G, et al. Prognostic effect of stress hyperglycemia ratio on patients with severe aortic stenosis receiving transcatheter aortic valve replacement: a prospective cohort study. Cardiovasc Diabetol. 2024;23:73.
Dong S, Zhao Z, Huang X, Ma M, Yang Z, Fan C, et al. Triglyceride-glucose index is associated with poor prognosis in acute coronary syndrome patients with prior coronary artery bypass grafting undergoing percutaneous coronary intervention. Cardiovasc Diabetol. 2023;22:286.
Luo E, Wang D, Yan G, Qiao Y, Liu B, Hou J, et al. High triglyceride-glucose index is associated with poor prognosis in patients with acute ST-elevation myocardial infarction after percutaneous coronary intervention. Cardiovasc Diabetol. 2019;18:150.
Lovejoy JC, Champagne CM, de Jonge L, Xie H, Smith SR. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes (Lond). 2008;32:949–58.
Yang K, Liu W. Triglyceride and glucose index and sex differences in relation to major adverse Cardiovascular events in hypertensive patients without diabetes. Front Endocrinol (Lausanne). 2021;12:761397.
Yu Y, Wang J, Ding L, Huang H, Cheng S, Deng Y, et al. Sex differences in the nonlinear association of triglyceride glucose index with all-cause and cardiovascular mortality in the general population. Diabetol Metab Syndr. 2023;15:136.
Andrikou E, Tsioufis C, Andrikou I, Leontsinis I, Tousoulis D, Papanas N. GLP-1 receptor agonists and cardiovascular outcome trials: an update. Hellenic J Cardiol. 2019;60:347–51.
Nissen SE, Nicholls SJ, Wolski K, Nesto R, Kupfer S, Perez A, et al. Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: the PERISCOPE randomized controlled trial. JAMA. 2008;299:1561–73.
Laakso M, Kuusisto J. Insulin resistance and hyperglycaemia in cardiovascular disease development. Nat Rev Endocrinol. 2014;10:293–302.
Gupta T, Joseph DT, Goel SS, Kleiman NS. Predicting and measuring mortality risk after transcatheter aortic valve replacement. Expert Rev Cardiovasc Ther. 2021;19:247–60.
Perry AS, Zhao S, Murthy V, Gupta DK, Fearon WF, Kim JB, et al. Metabolic signatures of Cardiac Dysfunction, Multimorbidity, and Post-transcatheter aortic valve implantation death. J Am Heart Assoc. 2023;12:e029542.
Cahill TJ, Kirtane AJ, Leon M, Kodali SK. Subclinical leaflet thrombosis and anticoagulation after transcatheter aortic valve replacement: a review. JAMA Cardiol. 2022;7:866–72.
Beverly JK, Budoff MJ, Atherosclerosis. Pathophysiology of insulin resistance, hyperglycemia, hyperlipidemia, and inflammation. J Diabetes. 2020;12:102–4.
Xu Y, Arora RC, Hiebert BM, Lerner B, Szwajcer A, McDonald K, et al. Non-invasive endothelial function testing and the risk of adverse outcomes: a systematic review and meta-analysis. Eur Heart J Cardiovasc Imaging. 2014;15:736–46.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (82170375, U23A20395 and 82300570), the Sichuan Science and Technology Program (2023NSFSC1657), the Key Research and Development Project of Science & Technology Department of Sichuan Province (2022ZDZX0020), the “1.3·5 project for disciplines of excellence-Clinical Research Fund, West China Hospital, Sichuan University” (23HXFH009), and the Post-Doctor Research Project, West China Hospital, Sichuan University (2023HXBH028).
Author information
Authors and Affiliations
Contributions
MC and WYL contributed to the conception and design of the study; WYL and HDL contributed to manuscript writing; SQP, JLL and YY contributed to data collection and management; WYL, FC and LB contributed to the statistics analysis; CXS, HRY and TYX participated in the patient follow-up; WYL, YP, JFW, ZGZ and MC contributed to manuscript revision and data review. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Sichuan University West China Hospital (No. 2020–470). All patients provided written informed consent.
Consent for publication
All the authors gave their consent to publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, W., Li, H., Peng, S. et al. Prognostic effect of the TyG index on patients with severe aortic stenosis following transcatheter aortic valve replacement: a retrospective cohort study. Cardiovasc Diabetol 23, 312 (2024). https://doi.org/10.1186/s12933-024-02414-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02414-9