Abstract
Background
Effectiveness of glucagon-like peptide-1 receptor agonists (GLP-1RAs) versus long-acting insulins (LAIs) on preventing progressive chronic kidney outcomes is uncertain for type 2 diabetes (T2D) patients requiring intensive glycemic control. This study aimed to evaluate comparative effectiveness of GLP-1RA versus LAI therapies on progressive chronic kidney outcomes among patients having poor glycemic control and requiring these injectable glucose-lowering agents (GLAs).
Methods
7279 propensity-score-matched pairs of newly stable GLP-1RA and LAI users in 2013–2018 were identified from Taiwan’s National Health Insurance Research Database and followed until death or 12/31/2019 (intention-to-treat). Subdistributional hazard model was utilized to assess the comparative effectiveness on a composite renal outcome (i.e., renal insufficiency [eGFR < 15 mL/min/1.73 m2], dialysis-dependent end-stage renal disease [ESRD], or renal death) and its individual components. Sensitivity analyses with the as-treated scenario, PS weighting, high-dimensional PS techniques, using cardiovascular diseases (CVDs) as positive control outcomes, and interaction testing were performed.
Results
In primary analyses, subdistribution hazard ratios (95% CIs) for initiating GLP-1RAs versus LAIs for the composite renal outcome, renal insufficiency, dialysis-dependent ESRD, and renal death were 0.39 (0.30–0.51), 0.43 (0.32–0.57), 0.29 (0.20–0.43), and 0.28 (0.15–0.51), respectively. Sensitivity analysis results were consistent with the primary findings. CVD history and the medication possession ratio of prior oral GLAs possessed modification effects on GLP-1RA-associated kidney outcomes.
Conclusion
Using GLP-1RAs versus LAIs was associated with kidney benefits in T2D patients requiring intensive glycemic control and potentially at high risk of kidney progression. GLP-1RAs should be prioritized to patients with CVDs or adherence to prior oral GLAs to maximize kidney benefits.
Similar content being viewed by others
Background
Persistent hyperglycemia despite the use of multiple glucose-lowering agents (GLAs) among patients with type 2 diabetes (T2D) could deteriorate renal functions and thereby increase the risk of renal diseases [1]. Hence, optimizing GLA therapies that can normalize glucose levels and improve glycemic control is essential for delaying the progression to renal failure in this population [2]. For such patients, long-acting insulins (LAIs) and glucagon-like peptide-1 receptor agonists (GLP-1RAs) are recommended as injectable GLAs to intensify glycemic control [3]. In particular, the use of GLP-1RAs and LAIs in Taiwan’s clinical practice setting is generally limited to T2D patients in the late treatment course (i.e., having persistent hyperglycemia under three types of oral GLAs or at the level of HbA1c ≥ 8.5% under oral GLA treatments [4]) requiring intensive glycemic control.
Possible renal benefits with the use of GLP-1RAs have been recognized in recent studies. Direct interactions of GLP-1RAs with human glomerulus and renal tubules have been shown to slow the progression to renal failure [5,6,7]. A decreased incidence of macroalbumiuria among GLP-1RA users compared to those with placebo was reported in both LEADER [8, 9] and REWIND trials [10]. Unfortunately, the generalizability of trial findings [8,9,10] to real-world settings, which comprise diverse patients and multiple competing treatments, is unclear. In addition, it is unclear whether short-term improvements in renal outcomes (e.g., macroalbuminuria) associated with GLP-1RA use obtained from limited follow-up trial periods can translate into the long-term benefits for clinically meaningful renal events (e.g., dialysis or renal death) in daily practice settings. Few real-world studies have assessed the chronic renal outcomes of GLP-1RA therapies versus other GLA therapies among general T2D populations [11,12,13], and there is a lack of data on the comparative renal effects of GLP-1RAs versus LAIs in patients who require intensive glycemic control and are at a high risk of the progression of renal diseases.
Against this background, we sought to generate real-world data on the comparative effectiveness of GLP-1RA versus LAI therapies on progressive chronic renal outcomes among patients with need for intensified injectable GLAs. In addition, exploratory analyses were performed to investigate the heterogeneity of treatment effects among real-world patient populations with diverse clinical characteristics to identify potential effect modifiers. Such information can facilitate clinical treatment decision-makings to enhance personalized medicine for patients.
Methods
Data source
This study was approved by the Institutional Review Board of National Cheng Kung University Hospital (B-ER-108-474). Taiwan’s National Health Insurance Research Database (NHIRD) was utilized in this study. Briefly, Taiwan’s NHIRD is a nationwide, population-based claims database that comprises de-identified, individual-level, and longitudinal health records (i.e., outpatient, emergency, and inpatient departments, and pharmacy refills) of each beneficiary enrolled in the National Health Insurance (NHI) program, which covers over 99% of the population in Taiwan [14]. Details of the NHIRD are available elsewhere [14].
Cohort identification and follow-up
This comparative effectiveness research applied an active-comparator, new-user design [15]. Stable users of the study drugs (i.e., individuals with at least three prescriptions of GLP-1RAs or LAIs with any gaps between two consecutive drug refills of less than 30 days) were first identified from patients with T2D in the NHIRD in the period of 2013 to 2018. The initiation of the study drugs was defined as the index date. Patients younger than 18 years of age at the index date and those with undefined sex were excluded. Per the new-user design in this study, prevalent users of GLP-1RAs or LAIs in the year before the index date were excluded. Patients prescribed with both GLP-1RAs and LAIs at the index date were also excluded to avoid the misclassification of treatment exposure. We also excluded patients with concurrent use of a basal-bolus insulin regimen or premixed insulin at the index date because they were likely to have poor glycemic control or fluctuating blood glucose levels during mealtimes [3]. Next, to avoid prevalent cases with renal insufficiency in the present study, study subjects with one of the following characteristics at baseline were excluded: prior use of erythropoiesis stimulating agents (ESAs), end-stage renal disease (ESRD), or renal transplantation in the year before the index date. Moreover, to enhance the comparability of study cohorts, 5-to-1-digit greedy propensity score matching (PSM) procedures were implemented to obtain GLP-1RA- and LAI-matched pairs at a 1:1 ratio [16]. Briefly, each patient’s PS, which indicated the probability of receiving the treatment of interest (i.e., GLP-1RAs versus LAIs), was estimated using a logistic regression analysis, where a series of patient characteristics at baseline (i.e., demographics at the index date, diabetes-related complications, exposure to GLAs, medication possession ratio [MPR] of prior GLA use, which was calculated as the day supply of GLAs divided by 365 days [17], and exposure to cardiovascular [CV] and kidney-disease-associated medications in the year prior to the index date) were treated as explanatory variables for treatment status (i.e., GLP-1RAs or LAIs). Among these variables, the number of oral GLA prescriptions in the year before the index date and the status of prandial insulin use in the month before the index date were specified as proxies for the diabetes severity of individual patients, as recommended by the literature [4] and clinical experts. The details of cohort selection are available in Additional file 1: Fig. S1. Each patient was followed from the initiation of the study drugs until the occurrence of study outcomes, loss of follow-up, death, or the end of 2019, whichever came first (i.e., intention-to-treat [ITT] scenario).
Drug exposure and study outcome assessment
Drug exposure was measured according to the World Health Organization Anatomical Therapeutic Chemical Classification System. Of noted, only human-based GLP-1RAs (i.e., liraglutide and dulaglutide) available during study period in Taiwan were included in analysis. Study outcomes of interest were the composite progressive chronic renal outcome, including (1) renal insufficiency which referred to estimated glomerular filtration rate (eGFR) < 15 mL/min/1.73 m2 and was determined by the stable use of ESAs (i.e., at least two prescriptions of darbepoetin alfa or methoxy polyethylene glycol-epoetin beta, or four prescriptions of erythropoietin within 3 months) [18], given that the reimbursement policy of Taiwan’s NHI program restricts the use of ESAs only to patients with stage 5 chronic kidney disease (CKD), (2) dialysis-dependent ESRD, which was ascertained using the Registry of Catastrophic Illness Patients, and (3) renal death, which was determined according to the Cause of Death in the NHIRD, and individual components of the composite outcome. The operational definitions of the study outcomes are detailed in Additional file 1: Table S1.
Statistical analyses
The standardized mean difference (SMD) was employed to examine the between-group difference in baseline patient characteristics before and after the PSM, with an absolute SMD value greater than 0.1 indicating a statistically significant between-group difference. The event rates of study outcomes in each treatment group were calculated as the number of events per 100 person-years. Given the high mortality risk of our study subjects, who were likely to be severe cases requiring intensive glycemic control with injectable GLAs (i.e., GLP-1RAs or LAIs) in the late treatment course of diabetes [19], the primary analyses under the ITT scenario employed subdistribution hazard models instead of traditional Cox models [20], to account for the possibility of competing risk of death to study events in our study cohort. The results are presented as subdistribution hazard ratios (SDHRs) and associated 95% CIs.
A series of sensitivity analyses were performed to test the robustness of the study findings. First, an as-treated (AST) scenario analysis was performed, where each patient was followed from the index date until the discontinuation of the study drug, a switch to or addition of another study drug, the occurrence of study outcomes, loss of follow-up, death, or the end of 2019, whichever came first. Second, to retain the most GLP-1RA and LAI users during our study period and thereby all observed events in the analysis, three PS weighting approaches, namely inverse probability of treatment weighting (IPTW), stabilized IPTW, and standardized mortality ratio weighting (SMRW) [21], were utilized to obtain the SDHRs of the study outcomes. Third, to minimize the possibility of unmeasured confounding effects that may arise with the use of the NHIRD, we estimated the high-dimensional PS (hdPS) using baseline patient characteristics that were associated with the receipt of the treatment of interest (i.e., GLP-1RAs versus LAIs) and simultaneously generated from empirical variables in five data dimensions of the NHIRD (i.e., outpatient diagnoses, outpatient procedures, inpatient diagnoses, inpatient procedures, and medication use) [22]. We re-matched the study cohorts using hdPS and estimated the SDHR accordingly. Fourth, to investigate the heterogeneity of GLP-1RA-associated renal effects by baseline patient characteristics, the primary analyses were stratified by patients’ age, sex, history of diabetes-related complications, and MPR of previously used GLAs (MPR ≥ 0.8 versus < 0.8 [17]) and use of renin-angiotensin aldosterone system agents, where these characteristics were modeled with treatment status (i.e., GLP-1RAs versus LAIs) as interaction terms in the analysis. These characteristics have been recognized as potential effect modifiers for GLP-1RA-associated outcomes according to existing evidence [11, 23] and are recommended by clinical experts. Lastly, analyses of clinical outcomes that are well known to be positively associated with GLP1-RA therapy (i.e., positive control outcomes) were conducted to examine the validity of the study procedures [24]. That is, given the apparent GLP-1RA-associated CV benefits [4, 25], the three-point major adverse CV event (3P-MACE, including nonfatal myocardial infarction [MI], nonfatal stroke, and CV death) and individual components of 3P-MACE were selected as positive control outcomes for analysis. All of the above-mentioned analyses were performed using SAS software version 9.4.
Results
There were 99,889 of T2D patients with stable use of GLP-1RAs or LAIs identified from the NHIRD in 2013 ~ 2018. After applying study exclusion criteria (e.g., the use of basal-bolus insulin regimens or premixed insulins at index date [i.e., 12,593 subjects] shown in Additional file 1: Fig. S1), 7643 and 49,570 of incident new-users of GLP-1RAs and LAIs, respectively, were obtained for further PSM. A total of 7279 PS-matched pairs of GLP-1RA and LAI users were identified (Additional file 1: Fig. S1), and they had a satisfactory between-group comparability at baseline supported by all absolute SMD statistics less than 0.1 (Fig. 1). Kernel density plots of the PS distribution before and after the matching are shown in Additional file 1: Fig. S2, and the proportions of individual GLP-1RAs and LAIs are detailed in Additional file 1: Table S2. As shown in Additional file 1: Table S3, study subjects after PSM had a mean age of 49 years, and 49% of them were female, and 19%, 25.6%, 8.1% and 11.3% of the subjects had a history of cardiovascular diseases (CVDs), nephropathy, neuropathy, and retinopathy, respectively. On average, each patient was prescribed nearly three types of GLA in the year before the index date.
Absolute standardized mean differences of baseline characteristics between GLP-RA and LAI groups before and after propensity score matching. Black vertical line indicates standardized mean difference of 0.1. Values (i.e., black dots or crosses) greater than 0.1 indicate statistically significant between-group difference in patient baseline characteristics
Primary and sensitivity analyses of chronic renal outcomes and positive control outcome analyses
The results of primary analyses with the ITT scenario show that over a mean follow-up period of 2.64 years, the SDHRs (95% CIs) of composite chronic renal outcome, renal insufficiency (i.e., eGFR < 15 mL/min/1.73 m2), dialysis-dependent ESRD, and renal death for GLP-1RA versus LAI therapies were 0.39 (0.30–0.51), 0.43 (0.32–0.57), 0.29 (0.20–0.43), and 0.28 (0.15–0.51), respectively (Table 1). Similarly, the SDHRs (95% CIs) of these outcomes obtained from the AST scenario analyses were 0.36 (0.25–0.53), 0.40 (0.27–0.60), 0.20 (0.11–0.38), and 0.47 (0.11–1.68), respectively (Additional file 1: Table S4).
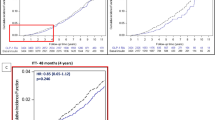
Sensitivity analyses based on PS-weighted cohorts (using IPTW, stabilized ITPW, and SMRW approaches) and hdPS-matched cohorts give results that are consistent with the primary findings (Fig. 2). That is, the SDHR estimates of these four sensitivity analyses fell within the 95% CIs of the estimates from primary analyses using the PSM approach for all study outcomes including composite chronic renal outcome, renal insufficiency, dialysis-dependent ESRD, and renal death. SDHRs and associated 95% CIs in these sensitivity analyses are detailed in Additional file 1: Table S5.
Results of subdistribution hazard model analyses for GLP-1RA versus LAI therapies on study outcomes (primary and sensitivity analyses). Black vertical dotted lines are 95% CIs of study outcomes obtained from primary analyses in propensity-score-matched cohorts. SDHRs subdistribution hazard ratios, PSM propensity score matching, IPTW inverse probability of treatment weighting, SMRW Standardized mortality ratio weighting, hdPS high-dimensional propensity score, ESRD end-stage renal disease. *Composite renal outcome includes stable use of ESA, dialysis-dependent ESRD, and renal death. †Renal insufficiency referred to estimated glomerular filtration rate < 15 mL/min/1.73 m2 and was determined by the stable use of erythropoiesis stimulating agents (ESAs) (i.e., at least two prescriptions of darbepoetin alfa or methoxy polyethylene glycol-epoetin beta, or four prescriptions of erythropoietin within three months), given that the reimbursement policy of Taiwan’s National Health Insurance program restricts the use of ESAs only to patients with stage 5 chronic kidney disease. This operational definition was also confirmed with clinical nephrologists. ‡We removed patients whose propensity scores were either more than 0.95 or less than 0.05; the weights were then estimated based on the trimmed populations. Weights in the IPTW approach were estimated as follows: WeightGLP1RAs = 1/PS and WeightLAIs = 1/(1-PS). Weights in the stabilized IPTW approach were estimated as follows: WeightGLP1RAs = Prevalence of GLP1RA users (%)/PS and WeightLAIs = Prevalence of LAI users (%)/(1-PS). Weights in the SMRW approach were estimated as follows: WeightGLP1RAs = 1 and WeightLAIs = PS/(1-PS)
Positive control outcome analyses show GLP-1RA-therapy-associated CV benefits; i.e., the SDHRs (95% CIs) of 3P-MACE, non-fatal MI, non-fatal stroke, and CV death for GLP-1RAs versus LAIs were 0.71 (0.60–0.84), 0.73 (0.54–0.99), 0.76 (0.60–0.95), and 0.49 (0.34–0.69), respectively (Additional file 1: Table S6).
Subgroup analyses to explore potential effect modifiers of GLP-1RA-associated chronic renal outcomes
Overall, the use of GLP-1RAs versus LAIs led to a reduced risk of renal outcomes across different subgroups, except those aged ≥ 65 years old for dialysis-dependent ESRD and four subgroups for renal death (Fig. 3). Except for renal death, marginally significant effects of the interactions between CVD history (i.e., with versus without established CVDs) and treatment status (i.e., GLP-1RAs versus LAIs) on the risk of the composite chronic renal outcome (p = 0.093), renal insufficiency (i.e., eGFR < 15 mL/min/1.73 m2) (p = 0.064), and dialysis-dependent ESRD (p = 0.054) were found. Furthermore, marginally significant or significant effects of the interactions between the use of prior oral GLAs (i.e., MPR ≥ 0.8 versus < 0.8) and treatment status (i.e., GLP-1RAs versus LAIs) on the risk of the composite chronic renal outcome (p = 0.071), renal insufficiency (p = 0.048), and dialysis-dependent ESRD (p = 0.045) were found.
Forest plot for subgroup analysis results on (a) composite renal outcomes, (b) renal insufficiency (i.e., eGFR < 15 mL/min/1.73 m2), (c) dialysis-dependent end-stage renal disease, and (d) renal death. eGFR estimated glomerular filtration rate, ESRD end-stage renal disease, SDHRs subdistribution hazard ratios, MPR medication possession ratio, GLAs glucose-lowering agents, RAAS renin-angiotensin aldosterone system, GLP-1RAs glucagon-like peptide-1 receptor agonists, LAIs long-acting insulins. *Bold p values for interaction tests indicate that treatment effect of GLP-1RAs versus LAIs on study outcome was significantly modified by given baseline characteristics. †Renal insufficiency referred to eGFR < 15 mL/min/1.73 m2 and was determined by the stable use of erythropoiesis stimulating agents (ESAs) (i.e., at least two prescriptions of darbepoetin alfa or methoxy polyethylene glycol-epoetin beta, or four prescriptions of erythropoietin within three months), given that the reimbursement policy of Taiwan’s National Health Insurance program restricts the use of ESAs only to patients with stage 5 chronic kidney disease. This operational definition was also confirmed with clinical nephrologists
Discussion
To our best knowledge, this study was the first to determine the progressive chronic renal outcomes of human-based GLP-1RA therapy (i.e., liraglutide and dulaglutide) among T2D patients who required intensive glycemic control and were potentially at risk of poor kidney functions. Our findings show that among T2D patients with poor glycemic control and initiating injectable GLAs, the use of GLP-1RAs versus LAIs was associated with lower risks of chronic renal disease progression (i.e., renal insufficiency as defined by eGFR < 15 mL/min/1.73 m2, dialysis-dependent ESRD, or renal death). A series of sensitivity analyses not only corroborated the primary analysis findings but also revealed the possibility of heterogenous treatment effects following GLP-1RA versus LAI therapies by patients’ clinical characteristics (e.g., disease history, medication adherence). Hence, this study adds supporting evidence to optimize clinical treatment decisions and promote precision medicine for averting substantial renal deterioration among clinically vulnerable T2D patients with poor glycemic control and at high risk of poor kidney prognosis.
Existing evidence regarding GLP-1RA versus oral GLA therapies for chronic renal outcome
Considering the absence of trial results regarding the long-term renal effect of GLP-1RA therapy, real-world studies with the aim to assess the chronic renal outcomes of GLP-1RA versus oral GLA use have been conducted; however, the findings depend on the comparator drugs [11,12,13]. The HRs of GLP-1RAs versus dipeptidyl peptidase-4 inhibitors (DPP-4is) were in the range of 0.72 (95% CI: 0.53–0.98) [13] to 0.76 (0.68–0.85) [11] for the composite renal outcome, 0.73 (0.62–0.87) for renal dialysis or transplantation [11], and 0.72 (0.48–1.10) for renal death [11]. In contrast, those of sodium-glucose cotransporter-2 inhibitors versus GLP-1RAs were 0.77 (0.62–0.96) for the composite renal outcome and 0.53 (0.33–0.86) for ESRD [12]. Nevertheless, the findings obtained from comparative studies of GLP-1RAs and oral GLAs might not be generalizable to patients requiring injectable GLAs, who are likely to have poor glycemic control and are potentially at high risk of poor kidney outcomes compared to oral GLA users. Hence, an evaluation of the renal effects of GLA-1RA therapy among patients who require intensive glycemic control with injectable GLAs is urgently needed.
Comparative effectiveness of GLP-1RA versus LAI therapies for chronic renal outcome
Among trials investigating the short-term renal benefits of GLP-1RA therapies [8,9,10, 26, 27], only the SURPASS-4 [27] and AWARD-7 [26] trials employed an active comparator design. They showed that the use of tirzepatide [27], a dual glucose-dependent insulinotropic polypeptide and GLP-1RA, or dulaglutide [26] versus insulin glargine had a comparable glucose-lowering effect but a better eGFR at 52 weeks of follow-up [26, 27]. In particular, the use of tirzepatide versus insulin glargine had a significantly lower risk on composite kidney endpoint which comprised time to first occurrence of eGFR decline of at least 40% from baseline, ESRD, death owing to kidney failure, or new-onset macroalbuminuria (HR: 0.58; 95% CI: 0.43–0.80) [27]. However, such renal benefits may not be generalized to patients only using GLP1-RA therapy. Furthermore, comparative kidney outcomes associated with exenatide versus LAI use have been examined in a previous study [28], which however may not be generalizable to patients using human-based GLP-1RAs (i.e., liraglutide and dulaglutide). Recently, the FLOW trial, an ongoing trial, prospectively evaluates the effect of semaglutide versus insulin glargine on renal outcomes (including time to first kidney failure, persistent ≥ 50% reduction in eGFR or death from kidney or CV causes) in patients with T2D and CKD [29]. This trial is expected to complete in late 2024.
To our best knowledge, the present study is the first to assess the comparative effectiveness of GLP-1RAs (i.e., liraglutide and dulaglutide) versus LAIs for a series of progressive chronic renal outcomes. The results of primary and sensitivity analyses suggest that in a mean 2.64-year follow-up, the use of GLP-1RAs versus LAIs significantly decreased the risk of the composite chronic renal outcome by 51–63%, renal insufficiency (i.e., eGFR < 15 mL/min/1.73 m2) by 50–63%, dialysis-dependent ESRD by 54–71%, and renal death by 47–72% (Fig. 2). Of note, injectable GLAs, including GLP-1RAs, are commonly initiated at a later treatment course among real-world T2D populations, especially for patients with persistent hyperglycemia despite the use of multiple oral GLAs [30, 31]. Our study patients had multiple oral GLA therapies prior to the initiation of GLP-1RAs or LAIs, which could be attributable to the reimbursement policy of Taiwan’s NHI program where the use of GLP-1RAs was restricted to T2D patients with glycated hemoglobin (HbA1c) greater than 8.5% for at least 6 months. Previous real-world studies in Taiwan showed that the HbA1c level of patients at the beginning of GLP-1RAs generally ranged between 9.2 and 9.4% [32,33,34]. Such high HbA1c levels (i.e., 9% and above) have been correlated with undesired kidney outcomes, including ESRD [35, 36], leading to high mortality, poor quality of life [37], and considerable healthcare spending [38]. Hence, given the remarkable renal outcomes of GLA-1RA therapies shown in this study, timely initiation of GLP-1RAs among T2D patients who require intensive glycemic control with injectable GLAs is suggested to avert the progression to renal failure/dialysis or death, leading to better patient quality of life and better economic outcomes.
Effect modifiers for GLP-1RA-associated kidney outcomes
Our exploratory analyses identified CVD history and the MPR of prior oral GLAs as potential effect modifiers (Fig. 3). That is, CVD history had marginally significant modification effects on the GLP-1RA-associated composite renal outcome, renal insufficiency (i.e., eGFR < 15 mL/min/1.73 m2), and dialysis-dependent ESRD, while the MPR of prior oral GLAs had significant modification effects on the renal insufficiency and dialysis-dependent ESRD. Our findings may be explained by existing non-clinical and clinical studies. Specifically, CV impairment could worsen renal functions [39]. Owing to drug action on cardiomyocytes, GLP-1RAs could enhance nitric oxide production, glucose uptake, and coronary flow, thereby averting myocardial ischemia and ventricular dysfunction [40]. Such CV improvement could also benefit kidney systems. Together with our results, one may expect that compared to those without CVD history, patients with established CVDs will gain more kidney benefits (i.e., slowed or preserved renal function) from timely intervention with GLP-1RAs.
Non-adherence to GLAs is a well-known risk factor for treatment failure (i.e., uncontrolled HbA1c), and is associated with increased comorbidities and diabetes-related complications [41, 42]. We found that patients who previously achieved greater adherence to oral GLAs (i.e., MPR ≥ 0.8) had a lower risk of poor progressive chronic renal outcomes (i.e., renal insufficiency as defined by eGFR < 15 mL/min/1.73 m2, and dialysis-dependent ESRD; Fig. 3) compared to those with less adherence (i.e., MPR < 0.8). Therefore, greater glycemic control and renal benefits following GLP-1RA therapy among patients with good medication adherence are expected. In contrast, for those with poor adherence to prior oral GLAs, education or close monitoring to enhance medication adherence is important for optimizing the treatment effects of GLP-1RAs.
Study limitations
Several limitations of this study should be acknowledged. First, due to the lack of laboratory (e.g., HbA1c, blood pressure, and albuminuria) and behavioral data in claims-based data, residual unmeasured confounding might exist in our study. Several methodology efforts therefore were carried out to minimize the possibility of unmeasured confounding effect to study results, including (1) the adjustment of well-known proxies (e.g., prior use of GLAs for the level of glycemic control, past history of diabetic nephropathy, neuropathy and retinopathy for the severity of diabetes, prior exposure of anti-hypertensive medications for the status of blood pressure control) in the PS estimation in primary analysis, (2) using the hdPS and considering baseline patient characteristics from empirical data in the NHIRD in a sensitivity analysis, and 3) applying 3P-MACE as positive control outcomes to support the validity of our study procedures. Of noted, our finding in positive control outcome analysis (i.e., the magnitude of CV effect: 29% of reduction in 3P-MACE risk associated with GLP-1RA versus LAI use) falls in the range of 19–41% of risk reduction shown in previous studies [4, 25], suggesting that the issue of unmeasured confounding effect in this study might be negligible. Second, the treatment pattern (e.g., adherence) in real-world patient populations may be suboptimal and could consequently affect treatment outcomes. Therefore, in additional to the ITT scenario in the primary analyses, AST scenario analyses were performed with consideration of the discontinuation or switching of study drugs in this real-world study. Third, the primary analyses might be limited to PSM-derived GLP-1RA and LAI users with similar baseline characteristics because these patients might not be representative of drug users with diverse clinical characteristics in real-world settings. Therefore, sensitivity analyses using various PS weighting techniques (i.e., IPTW, stabilized PTW, and SMRW) were further performed, where the original users of study drugs were retained to ensure the diversity of study cohorts to reflect real-world patients. Fourth, the subgroup analyses stratified by baseline patient characteristics are considered as exploratory in nature. Hence, future research is warranted to corroborate our findings. Lastly, the generalizability of study results on renal insufficiency might be limited. Since the stable use of ESAs (i.e., only for patients with eGFR level < 15 ml/min/1.73m2 under Taiwan’s NHI reimbursement policy) was applied as a surrogate indicator for renal insufficiency [18], our study patients having renal insufficiency were likely to be severe cases.
Conclusions
Compared to LAIs, using GLP-1RAs was associated with lower risk of progressive chronic renal outcomes among a real-world T2D patient population that required intensive GLA therapy and was at risk of poor renal progression. GLP-1RA therapy for these vulnerable patients should thus be timely administered. Prioritization of GLP-1RAs for the patients with established CVDs or optimal adherence to prior oral GLAs should be considered to maximize the renal benefits of using GLP-1RA therapy.
Availability of data and materials
Raw data were generated at Taiwan’s National Health Insurance Research Database. Derived data supporting the findings of this study are available from the corresponding author Dr. Huang-Tz Ou on request.
Abbreviations
- 3P-MACE:
-
Three-point major adverse cardiovascular event
- AST:
-
As-treated
- CV:
-
Cardiovascular
- CVDs:
-
Cardiovascular diseases
- CKD:
-
Chronic kidney disease
- DPP-4is:
-
Dipeptidyl peptidase-4 inhibitors
- eGFR:
-
Estimated Glomerular filtration rate
- ESAs:
-
Erythropoiesis stimulating agents
- ESRD:
-
End-stage renal disease
- GLAs:
-
Glucose-lowering agents
- GLP-1RAs:
-
Glucagon-like peptide-1 receptor agonists
- hdPS:
-
High-dimensional propensity score
- HbA1c :
-
Glycated hemoglobin
- IPTW:
-
Inverse probability of treatment weighting
- ITT:
-
Intention-to-treat
- LAIs:
-
Long-acting insulins
- MPR:
-
Medication possession ratio
- NHIRD:
-
National Health Insurance Research Database
- NHI:
-
National Health Insurance
- PSM:
-
Propensity score matching
- SMD:
-
Standardized mean difference
- SDHR:
-
Subdistribution hazard ratio
- SMRW:
-
Standardized mortality ratio weighting
- T2D:
-
Type 2 diabetes
References
Thomas MC, Brownlee M, Susztak K, Sharma K, Jandeleit-Dahm KA, Zoungas S, Rossing P, Groop PH, Cooper ME. Diabetic kidney disease. Nat Rev Dis Primers. 2015;30(1):15018. https://doi.org/10.1038/nrdp.2015.18.
Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, Cuddihy R, Cushman WC, Genuth S, Grimm RH Jr, Hamilton BP, Hoogwerf B, Karl D, Katz L, Krikorian A, O'Connor P, Pop-Busui R, Schubart U, Simmons D, Taylor H, Thomas A, Weiss D, Hramiak I, ACCORD trial group. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010 Aug 7;376(9739):419–30. doi: https://doi.org/10.1016/S0140-6736(10)60576-4. Epub 2010 Jun 30. Erratum in: Lancet. 2010;376(9751):1466.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Leon J, Lyons SK, Perry ML, Prahalad P, Pratley RE, Seley JJ, Stanton RC, Gabbay RA, on behalf of the American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S140–57. https://doi.org/10.2337/dc23-S009.
Yang CT, Yang CY, Ou HT, Kuo S. Comparative cardiovascular safety of GLP-1 receptor agonists versus other glucose-lowering agents in real-world patients with type 2 diabetes: a nationwide population-based cohort study. Cardiovasc Diabetol. 2020;19(1):83. https://doi.org/10.1186/s12933-020-01053-0.
Crajoinas RO, Oricchio FT, Pessoa TD, Pacheco BP, Lessa LM, Malnic G, Girardi AC. Mechanisms mediating the diuretic and natriuretic actions of the incretin hormone glucagon-like peptide-1. Am J Physiol Renal Physiol. 2011;301(2):F355–63. https://doi.org/10.1152/ajprenal.00729.2010.
Kim M, Platt MJ, Shibasaki T, Quaggin SE, Backx PH, Seino S, Simpson JA, Drucker DJ. GLP-1 receptor activation and Epac2 link atrial natriuretic peptide secretion to control of blood pressure. Nat Med. 2013;19(5):567–75. https://doi.org/10.1038/nm.3128.
Kawanami D, Takashi Y. GLP-1 receptor agonists in diabetic kidney disease: from clinical outcomes to mechanisms. Front Pharmacol. 2020;30(11):967. https://doi.org/10.3389/fphar.2020.00967.
Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, Nissen SE, Pocock S, Poulter NR, Ravn LS, Steinberg WM, Stockner M, Zinman B, Bergenstal RM, Buse JB, LEADER Steering Committee; LEADER Trial Investigators. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22. https://doi.org/10.1056/NEJMoa1603827.
Mann JFE, Ørsted DD, Brown-Frandsen K, Marso SP, Poulter NR, Rasmussen S, Tornøe K, Zinman B, Buse JB, LEADER Steering Committee and Investigators. Liraglutide and renal outcomes in type 2 diabetes. N Engl J Med. 2017;377(9):839–48. https://doi.org/10.1056/NEJMoa1616011.
Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, Probstfield J, Riesmeyer JS, Riddle MC, Rydén L, Xavier D, Atisso CM, Dyal L, Hall S, Rao-Melacini P, Wong G, Avezum A, Basile J, Chung N, Conget I, Cushman WC, Franek E, Hancu N, Hanefeld M, Holt S, Jansky P, Keltai M, Lanas F, Leiter LA, Lopez-Jaramillo P, Cardona Munoz EG, Pirags V, Pogosova N, Raubenheimer PJ, Shaw JE, Sheu WH, Temelkova-Kurktschiev T, REWIND Investigators. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394(10193):121–30. https://doi.org/10.1016/S0140-6736(19)31149-3.
Pasternak B, Wintzell V, Eliasson B, Svensson AM, Franzén S, Gudbjörnsdottir S, Hveem K, Jonasson C, Melbye M, Svanström H, Ueda P. Use of glucagon-like peptide 1 receptor agonists and risk of serious renal events: Scandinavian cohort study. Diabetes Care. 2020;43(6):1326–35. https://doi.org/10.2337/dc19-2088.
Lui DTW, Au ICH, Tang EHM, Cheung CL, Lee CH, Woo YC, Wu T, Tan KCB, Wong CKH. Kidney outcomes associated with sodium-glucose cotransporter 2 inhibitors versus glucagon-like peptide 1 receptor agonists: a real-world population-based analysis. EClinicalMedicine. 2022;50: 101510. https://doi.org/10.1016/j.eclinm.2022.101510.
Xu Y, Fu EL, Clase CM, Mazhar F, Jardine MJ, Carrero JJ. GLP-1 receptor agonist versus DPP-4 inhibitor and kidney and cardiovascular outcomes in clinical practice in type-2 diabetes. Kidney Int. 2022;101(2):360–8. https://doi.org/10.1016/j.kint.2021.10.033.
Hsieh CY, Su CC, Shao SC, Sung SF, Lin SJ, Kao Yang YH, Lai EC. Taiwan’s National Health Insurance Research Database: past and future. Clin Epidemiol. 2019;3(11):349–58. https://doi.org/10.2147/CLEP.S196293.
Lund JL, Richardson DB, Stürmer T. The active comparator, new user study design in pharmacoepidemiology: historical foundations and contemporary application. Curr Epidemiol Rep. 2015;2(4):221–8. https://doi.org/10.1007/s40471-015-0053-5.
Parsons L. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. Available from https://support.sas.com/resources/papers/proceedings/proceedings/sugi26/p214-26.pdf. Accessed 10 Jun 2021.
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC. Good and poor adherence: optimal cut-point for adherence measures using administrative claims data. Curr Med Res Opin. 2009;25(9):2303–10. https://doi.org/10.1185/03007990903126833.
Peng ZY, Yang CT, Kuo S, Wu CH, Lin WH, Ou HT. Restricted mean survival time analysis to estimate SGLT2i-associated heterogeneous treatment effects on primary and secondary prevention of cardiorenal outcomes in patients with type 2 diabetes in Taiwan. JAMA Netw Open. 2022;5(12):e2246928. doi: https://doi.org/10.1001/jamanetworkopen.2022.46928. Erratum in: JAMA Netw Open. 2023;6(1):e2254512.
Landman GW, van Hateren KJ, Kleefstra N, Groenier KH, Gans RO, Bilo HJ. The relationship between glycaemic control and mortality in patients with type 2 diabetes in general practice (ZODIAC-11). Br J Gen Pract. 2010;60(572):172–5. https://doi.org/10.3399/bjgp10X483517.
Lau B, Cole SR, Gange SJ. Competing risk regression models for epidemiologic data. Am J Epidemiol. 2009;170(2):244–56. https://doi.org/10.1093/aje/kwp107.
Desai RJ, Franklin JM. Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: a primer for practitioners. BMJ. 2019;367: l5657. https://doi.org/10.1136/bmj.l5657.
Schneeweiss S, Rassen JA, Glynn RJ, Avorn J, Mogun H, Brookhart MA. High-dimensional propensity score adjustment in studies of treatment effects using health care claims data (Erratum. In: Epidemiology. 2018;29(6):e63–e64). Epidemiology. 2009;20(4):512–22. https://doi.org/10.1097/EDE.0b013e3181a663cc.
Yang YS, Chen HH, Huang CN, Hsu CY, Hu KC, Kao CH. GLP-1RAs for ischemic stroke prevention in patients with type 2 diabetes without established atherosclerotic cardiovascular disease. Diabetes Care. 2022;45(5):1184–92. https://doi.org/10.2337/dc21-1993.
Desai JR, Hyde CL, Kabadi S, St Louis M, Bonato V, Katrina Loomis A, Galaznik A, Berger ML. Utilization of positive and negative controls to examine comorbid associations in observational database studies. Med Care. 2017;55(3):244–51. https://doi.org/10.1097/MLR.0000000000000640.
Longato E, Di Camillo B, Sparacino G, Tramontan L, Avogaro A, Fadini GP. Cardiovascular outcomes after initiating GLP-1 receptor agonist or basal insulin for the routine treatment of type 2 diabetes: a region-wide retrospective study. Cardiovasc Diabetol. 2021;20(1):222. https://doi.org/10.1186/s12933-021-01414-3.
Tuttle KR, Lakshmanan MC, Rayner B, Busch RS, Zimmermann AG, Woodward DB, Botros FT. Dulaglutide versus insulin glargine in patients with type 2 diabetes and moderate-to-severe chronic kidney disease (AWARD-7): a multicentre, open-label, randomised trial. Lancet Diabetes Endocrinol. 2018;6(8):605–17. https://doi.org/10.1016/S2213-8587(18)30104-9.
Heerspink HJL, Sattar N, Pavo I, Haupt A, Duffin KL, Yang Z, Wiese RJ, Tuttle KR, Cherney DZI. Effects of tirzepatide versus insulin glargine on kidney outcomes in type 2 diabetes in the SURPASS-4 trial: post-hoc analysis of an open-label, randomised, phase 3 trial. Lancet Diabetes Endocrinol. 2022;10(11):774–85. https://doi.org/10.1016/S2213-8587(22)00243-1.
Pawaskar M, Tuttle KR, Li Q, Best JH, Anderson PW. Observational study of kidney function and albuminuria in patients with type 2 diabetes treated with exenatide BID versus insulin glargine. Ann Pharmacother. 2014;48(5):571–6. https://doi.org/10.1177/1060028013520597.
Rossing P, Baeres FMM, Bakris G, Bosch-Traberg H, Gislum M, Gough SCL, Idorn T, Lawson J, Mahaffey KW, Mann JFE, Mersebach H, Perkovic V, Tuttle K, Pratley R. The rationale, design and baseline data of FLOW, a kidney outcomes trial with once-weekly semaglutide in people with type 2 diabetes and chronic kidney disease. Nephrol Dial Transplant. 2023. https://doi.org/10.1093/ndt/gfad009.
Federici MO, McQuillan J, Biricolti G, Losi S, Lebrec J, Richards C, Miglio C, Norrbacka K. Utilization patterns of glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes mellitus in italy: a retrospective cohort study. Diabetes Ther. 2018;9(2):789–801. https://doi.org/10.1007/s13300-018-0396-2.
Dave CV, Schneeweiss S, Wexler DJ, Brill G, Patorno E. Trends in clinical characteristics and prescribing preferences for SGLT2 inhibitors and GLP-1 receptor agonists, 2013–2018. Diabetes Care. 2020;43(4):921–4. https://doi.org/10.2337/dc19-1943.
Su YC, Hung JH, Chang KC, Sun CC, Huang YH, Lee CN, Hung MJ, Lai CC, Shao SC, Lai EC. Comparison of sodium-glucose cotransporter 2 inhibitors vs glucagonlike peptide-1 receptor agonists and incidence of dry eye disease in patients with type 2 diabetes in Taiwan. JAMA Netw Open. 2022;5(9): e2232584. https://doi.org/10.1001/jamanetworkopen.2022.32584.
Hsiao FC, Yen KC, Chao TF, Chen SW, Chan YH, Chu PH. New-onset atrial fibrillation in patients with type 2 diabetes treated with novel glucose-lowering therapies. J Clin Endocrinol Metab. 2022;107(9):2493–9. https://doi.org/10.1210/clinem/dgac402.
Tsai CJ, Tsao CF. Comparison of glucose lowering efficacy of human GLP-1 agonist in Taiwan type 2 diabetes patients after switching from DPP-4 inhibitor use or non-use. J Pers Med. 2022;12(11):1915. https://doi.org/10.3390/jpm12111915.
Kuo IC, Lin HY, Niu SW, Hwang DY, Lee JJ, Tsai JC, Hung CC, Hwang SJ, Chen HC. Glycated hemoglobin and outcomes in patients with advanced diabetic chronic kidney disease. Sci Rep. 2016;28(6):20028. https://doi.org/10.1038/srep20028.
Bash LD, Selvin E, Steffes M, Coresh J, Astor BC. Poor glycemic control in diabetes and the risk of incident chronic kidney disease even in the absence of albuminuria and retinopathy: Atherosclerosis Risk in Communities (ARIC) Study. Arch Intern Med. 2008;168(22):2440–7. https://doi.org/10.1001/archinte.168.22.2440.
Kuo S, Yang CT, Chen HY, Ou HT. Valuing health states of people with type 2 diabetes: analyses of the nationwide representative linked databases. J Diabetes Investig. 2021;12(9):1749–58. https://doi.org/10.1111/jdi.13520.
Chen HY, Kuo S, Su PF, Wu JS, Ou HT. Health care costs associated with macrovascular, microvascular, and metabolic complications of type 2 diabetes across time: estimates from a population-based cohort of more than 0.8 million individuals with up to 15 years of follow-up. Diabetes Care. 2020;43(8):1732–40. https://doi.org/10.2337/dc20-0072.
Jankowski J, Floege J, Fliser D, Böhm M, Marx N. Cardiovascular disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation. 2021;143(11):1157–72. https://doi.org/10.1161/CIRCULATIONAHA.120.050686.
Nauck MA, Meier JJ, Cavender MA, Abd El Aziz M, Drucker DJ. Cardiovascular actions and clinical outcomes with glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors. Circulation. 2017;136(9):849–70. https://doi.org/10.1161/CIRCULATIONAHA.117.028136.
Chang PY, Chien LN, Lin YF, Chiou HY, Chiu WT. Nonadherence of oral antihyperglycemic medication will increase risk of end-stage renal disease. Medicine (Baltimore). 2015;94(47): e2051. https://doi.org/10.1097/MD.0000000000002051.
Denicolò S, Perco P, Thöni S, Mayer G. Non-adherence to antidiabetic and cardiovascular drugs in type 2 diabetes mellitus and its association with renal and cardiovascular outcomes: a narrative review. J Diabetes Complications. 2021;35(7): 107931. https://doi.org/10.1016/j.jdiacomp.2021.107931.
Acknowledgements
We are grateful to the Health Data Science Center, National Cheng Kung University Hospital, for providing administrative and technical support.
Funding
This study was supported by grants from the Ministry of Science and Technology in Taiwan (grant MOST 109-2320-B-006-047-MY3) (recipient: Huang-Tz Ou). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Z.Y.P. designed the study, analyzed and interpreted the data, and wrote the manuscript. C.T.Y. designed the study, interpreted the data, and reviewed/edited the manuscript. W.H.L. designed the study, interpreted the data, and reviewed/edited the manuscript. W.Y.Y. designed the study, and analyzed and interpreted the data. H.T.O. provided study materials, designed the study, interpreted the data, and wrote the manuscript. S.K. designed the study, interpreted the data, and reviewed/edited the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of National Cheng Kung University Hospital (B-ER-108-474).
Consent for publication
Not applicable.
Competing interests
Authors have nothings to be disclosed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Operational definitions of study outcomes. Table S2. Proportions of individual GLP-1RAs and LAIs before and after propensity-score matching. Table S3. Baseline characteristics of study cohorts before and after propensity score matching. Table S4. Event rates and hazard ratios of renal outcomes associated with use of GLP-1RAs versus LAIs (as-treated scenario analyses). Table S5. Sensitivity analysis results of renal outcomes associated with use of GLP-1RAs versus LAIs. Table S6. Event rates and hazard ratios of cardiovascular outcomes associated with use of GLP-1RAs versus LAIs (positive control outcome analyses). Figure S1. Flow chart of cohort selection. Figure S2. Kernel density plots of propensity score distributions for study cohorts (a) before and (b) after matching.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Peng, ZY., Yang, CT., Lin, WH. et al. Chronic kidney outcomes associated with GLP-1 receptor agonists versus long-acting insulins among type 2 diabetes patients requiring intensive glycemic control: a nationwide cohort study. Cardiovasc Diabetol 22, 272 (2023). https://doi.org/10.1186/s12933-023-01991-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-01991-5