Abstract
Background
Acute kidney injury (AKI) can be caused by multiple factors/events, including acute coronary syndrome (ACS). Ceramides are involved in atherosclerosis progression, cardiovascular events, and renal damage. Almost no studies have been conducted on the relationship between ceramide concentrations and AKI events. Therefore, we evaluated the association between plasma ceramide level at admission and AKI in patients with ACS undergoing percutaneous coronary intervention.
Methods
We enrolled 842 ACS patients from the Prospective Multicenter Study for Early Evaluation of Acute Chest Pain. AKI was defined using the criteria from the 2012 Kidney Disease: Improving Global Outcomes. Eleven C16–C26 ceramides were measured using the high-performance liquid chromatography interfaced to tandem mass spectrometer procedure. Logistic regression models were used to evaluate relationships between ceramides and AKI risk. The area under the receiver operating characteristic curves (AUC) was used to evaluate differences between ceramides.
Results
Overall, 139 (16.5%) patients developed AKI during hospitalisation. Patients who developed AKI had higher levels of Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/20:0), Cer(d18:1/21:0), Cer(d18:1/24:1), and Cer(d18:1/24:2) than patients who did not (P < 0.05). In risk-factor adjusted logistic regression models, these ceramides were independently associated with AKI risk (P < 0.05). Cer(d18:1/24:2) had the highest odds ratio of 3.503 (Q4 vs. Q1, 95% confidence interval: 1.743–7.040, P < 0.001). Ceramides had AUCs of 0.581–0.661 (P < 0.001) for AKI. Each ceramide combined with the Mehran risk score (AUC: 0.780) had AUCs of 0.802–0.808, greater than the Mehran risk score alone.
Conclusion
Long-chain and very-long-chain ceramide levels may help determine the high AKI risk beyond traditional assessments.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is a complex syndrome that is wildly considered a common and catastrophic complication of acute coronary syndrome (ACS) [1]. The presence of AKI is related to worsening prognosis at both short- and long-term follow-up, raising mortality two- to three-fold [2,3,4,5]. The incidence of ACS-related AKI is heterogeneous at 5–55% and varies with the AKI diagnostic criteria, clinical background, and patient population [1]. Given the high incidence of AKI in ACS and the lack of specific therapy, discovering novel biomarkers is of great significance for more effective clinical prediction and prevention.
Ceramide is a type of complex sphingolipid; it is at the centre of sphingolipid synthesis and degradation metabolism. Ceramide consists of two hydrocarbon chains: the long-chain base of sphingosine and the saturated, or unsaturated, fatty acid of the C16–C26 chain length, linked to the C-2 position of the long-chain base of sphingosine via N-acylation [6]. In the blood, ceramides constitute a part of the circulating lipoprotein particles and are also present in blood cells [6]. Multiple studies have repeatedly confirmed the strong predictive value of plasma ceramides for cardiovascular events and mortality in patients with stable and unstable coronary heart disease [7,8,9,10,11], owing to their biochemical role in atherosclerosis progression and rupture of plaque [12]. A potential detrimental impact of a higher ceramide ratio (C16:0/24:0) on cardiac remodelling has been reported [13]. Importantly, ceramides have strong biological activity, play a central role in inflammatory signalling, cellular stress response, cell membrane integrity, nephrotoxicity, and apoptosis, and are associated with worsening cardiac function [14,15,16]; these mechanisms are a key component of AKI pathogenesis [1, 17]. Ceramide synthases 5 and 6 are upregulated by stress stimuli and promote the synthesis of long-chain ceramides, which are involved in various metabolic dysfunctions [18,19,20,21,22,23,24]. On the other hand, very long-chain ceramides are considered benign or protective [25, 26]. Therefore, an increased ratio of Cer(d18:1/24:2) indicates an increase in long-chain ceramides and/or a decrease in benign/protective ceramides, suggesting a shift toward metabolic dysfunction. Long-chain ceramides are known to be involved in diabetic kidney disease [27]. It is why this study selected long-chain and very-long-chain ceramides.
Recent studies have shown that increased levels of plasma ceramides are associated with chronic kidney disease, independent of common cardiovascular risk factors [28, 29]. One study suggested that the increased accumulation of ceramides in plasma plays an important role in kidney injury [30]. To our knowledge, almost no studies have been conducted on the relationship between ceramide concentrations and AKI events. We hypothesised that an increased plasma ceramide concentration results in a higher risk of AKI, especially in vulnerable populations, such as patients with ACS. Therefore, this Prospective Multicenter Study for Early Evaluation of Acute Chest Pain (PEACP) aimed to investigate the relationship between plasma ceramide levels and the risk of AKI in patients with ACS undergoing percutaneous coronary intervention (PCI).
Methods
Study design
The PEACP study was conducted to investigate new markers of diagnosis and prognosis for patients with acute chest pain using multiomics data by mass spectrometry detection. The PEACP study enrolled patients with acute chest pain from the chest pain centres of seven tertiary hospitals in China; it is registered at https://clinicaltrials.gov/ct2/home (Identifier: NCT04122573). This study was designed to evaluate whether the level of ceramides could predict AKI in patients with ACS undergoing primary PCI.
Study population
From November 2019 to April 2020, 3 610 patients with chest pain onset time < 24 h visited the acute chest pain centre: 923 patients were diagnosed with ACS and underwent PCI according to the diagnostic standard for non-ST-elevation ACS (NSTE-ACS) and ST-elevation myocardial infarction (STEMI), according to the American College of Cardiology and American Heart Association guidelines [31, 32]. The inclusion criteria included: diagnosed as ACS; > 18 years old; onset time < 24 h; signed the informed consent. The exclusion criteria were received thrombolysis, unqualified data of ceramides, lack of dynamic assessment of creatinine, and requiring chronic haemodialysis treatment. Finally, 842 patients were included in this study. (Additional file 1: Figure 1).
Data collection and definition
Data were recorded prospectively by two independent researchers, including vital signs, chronic disease history, inpatient medications, imaging examination, and lab tests. Leukocytes, platelets, and hemoglobin was measured on a haematology analysis system (LH 750, Beckman Coulter, Brea, CA). Serum creatinine, estimated glomerular filtration rate (eGFR), blood lipid, and blood glucose were conducted using the Architect c16000 analyser (Abbott Diagnostics, Dallas, TX). Cardiac biomarkers were measured using an immunology analyser (Cobas E601, Roche Diagnostics). The Global Registry of Acute Coronary Events (GRACE) [33] score and Gensini score [34] were recorded as former reports [35, 36]. The Mehran risk score includes the following components: use of intra-aortic balloon pump, age, anaemia, diabetes mellitus, congestive heart failure, contrast media volume, hypotension, and eGFR [37]. If there was a difference between the two data checks, another researcher participated in the judgment.
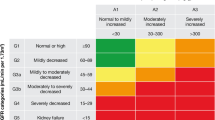
Diagnosis and staging of AKI were established using the Kidney Disease: Improving Global Outcomes (KDIGO) standard [38]. Meeting any of the following conditions is considered AKI stage 1: elevated serum creatinine level > 0.3 mg/dL (26.5 mmol/L) less than 2 days; serum creatinine increase to 1.5–1.9-fold from the baseline level; urine output < 0.5 mL/kg/h for 6–12 h. Meeting any of the following conditions is considered AKI stage 2: serum creatinine increase to 2.0–2.9-fold from the baseline level; urine output < 0.5 mL/kg/h for 12 h; Meeting any of the following conditions is considered AKI stage 3: serum creatinine concentration > 4.0 mg/dL (353.6 mmol/L); serum creatinine increased to > 3.0-fold from the baseline level; urine output < 0.3 mL/kg/h for 24 h; anuria for 12 h. The baseline level was regarded as the admission serum creatinine value tested at the emergency department. The primary endpoint of this study was AKI development.
Blood sample collection and quantification of ceramides
Blood samples (5 ml) were collected in EDTA tubes and stored at 4 °C for 30 min. To obtain plasma, blood samples were centrifuged at 1500 rpm for 10 min at 4 °C and then stored at −80 °C until further testing. Quality control (QC) was ensured by taking a mixture of 2 μL from each study sample. Ten microlitres of plasma were spiked before extraction with deuterated internal standards. The extraction of ceramide was performed as described previously [39]. Briefly, samples (150 µL) were deproteinated with 450 µL of cold isopropanol, vortexed for 30 s, centrifuged at 12,000 × g at 4 °C for 5 min, and 180 µL of the supernatant was transferred to an EP tube. The high-performance liquid chromatography interfaced with a tandem mass spectrometer (LC–MS/MS) procedure for ceramides testing has been showed in Supplementary materials in detail as reported previously [40]. The individual ceramides were quantified on the TSQ Quantiva Triple Quadrupole mass spectrometer equipped with the Dionex Ultimate 3000 UHPLC system (Thermo Fisher, San Jose, CA) and working in the MRM mode. Quantification was assessed using calibration line samples prepared with known amounts of synthetic Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/20:0), Cer(d18:1/21:0), Cer(d18:1/22:0), Cer(d18:1/23:0), Cer(d18:1/24:0), Cer(d18:1/24:1), Cer(d18:1/24:2), Cer(d18:1/25:0), and Cer(d18:1/26:0) and corresponding deuterated (D7) standards. The peak area ratios of ceramides and their deuterated forms were read. The value of ceramide added was plotted, and then linear regression analysis was carried out.
The endogenous plasma ceramide concentrations were derived from the obtained individual regression equations by calculating corresponding concentrations from the measured peak area ratios in samples. The precision (coefficient variance) and accuracy (relative error) for intra and inter for all 11 ceramides were within 10%; these were determined as previously described [40]. The final ceramide concentrations in plasma are presented as µmol/L.
Statistical analysis
Based on our pilot study, the incidence of AKI is approximately 15%. It is assumed that the area under the receiver operating characteristic curve (AUC) of ceramides for AKI is > 0.6, and to satisfy this difference with 80% power at 5% significance (2-tailed), a sample size of 546 is required. The sample size was calculated using MedCalc Statistical Software version 19.0.2 (MedCalc Software, Belgium).
Categorical variables are reported as frequency (%) and were compared by the χ2 test. Nonparametric continuous variables are expressed as medians (25th–75th) and compared using the Mann–Whitney U test. Parametric continuous variables are performed as means ± standard deviations and were compared using analysis of variance.
The correlation between all 11 ceramides and common prognostic factors of ACS was determined using Pearson’s correlation analysis. Logistic regression models were used to evaluate whether the levels of ceramides were associated with the risk of AKI after adjustment for confounding factors, including age, sex, systolic blood pressure, heart rate, body mass index, statin use, hypertension, diabetes, hyperlipidemia, Killip class, white blood cell count, low-density lipoprotein cholesterol, total cholesterol, triglyceride, estimated glomerular filtration rate, high sensitive cardiac troponin T, N-terminal pro-brain natriuretic peptide, and Mehran risk score. The odds ratio was calculated per the standard deviation (SD) and interquartile range of ceramides. AUC was determined to assess the predictive power of the Mehran risk score, all ceramides, and the ratio of all ceramides to Cer(d18:1–24:0) for AKI and to investigate the incremental predictive value of ceramides over the Mehran risk score. A two-tailed p < 0.05 indicated statistical significance. Data were analysed by SPSS Statistics (version 26.0, Chicago, IL) and R (version 3.5.1, Vienna, Austria).
Results
Baseline characteristics
Among the 842 ACS patients undergoing PCI, 620 (73.6%) were men, and the average age was 66.9 ± 13.0 years. During the hospitalisation period, there were 75 (8.9%), 31 (3.7%), and 33 (3.9%) patients who developed AKI stages 1, 2, and 3, respectively. Table 1 shows the baseline characteristics of patients classified as having non-AKI, AKI stages 1 to 3. Generally, patients with AKI were older and more likely to have hypertension and diabetes; higher Killip class, heart rate, white blood cell count, neutrophil cell count, fibrinogen, blood glucose, creatinine, eGFR; NT-proBNP, hs-CTNT, contrast dose, GRACE score, Gensini score, Mehran risk score; and lower haemoglobin (p < 0.05) than patients without AKI (Fig. 1).
Correlation of all ceramides and common risk factors for ACS
According to Spearman’s correlation analysis (Fig. 2), all ceramides had a significant positive correlation with blood lipids (cholesterol and triglycerides) (P < 0.0001), while Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/20:0), Cer(d18:1/21:0), Cer(d18:1/24:1), and Cer(d18:1/24:2) had a significant positive correlation with ACS risk score (GRACE score and Mehran risk score), cardiac markers (NT-proBNP and hs-CTNT), baseline renal function (creatinine, eGFR, and blood urea nitrogen), stress marker (blood glucose), and inflammatory markers (white blood cell count and neutrophil to lymphocyte ratio). Moreover, all 11 ceramides had a positive correlation with each other (P < 0.0001, Additional file 1: Figure S1A). We calculated the average mass fraction of these ceramides in ACS patients; Cer(d18:1/24:0) and Cer(d18:1/24:1) accounted for the smallest (5%) and largest (20%) mass fractions, respectively (Additional file 1: Figure S1B).
Correlation between all eleven ceramides and common prognostic factors in patients with acute coronary syndrome. The value in the heat map is the correlation coefficient. * < 0.05; ** < 0.001; *** < 0.0001. GRACE Global Registry of Acute Coronary Events, WBC white blood cell count, BUN Blood urea nitrogen, HDL-C high-density lipoprotein, LDL-C low-density lipoprotein, eGFR estimated glomerular filtration rate, hs-CTnT high sensitive cardiac troponin T, NT-proBNP N-terminal pro-brain natriuretic peptide, NLR neutrophil to lymphocyte ratio
Relationship between all ceramides and AKI
Medians and interquartile ranges of levels of ceramides in patients with and without AKI are shown in Table 2. Patients with AKI had higher levels of Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/20:0), Cer(d18:1/21:0), Cer(d18:1/24:1), and Cer(d18:1/24:2) and a lower level of Cer(d18:1/24:0) than patients without AKI (P < 0.05).
Figure 3 shows non-adjusted and adjusted ORs for all 11 ceramides. Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/20:0), Cer(d18:1/21:0), Cer(d18:1/24:1), and Cer(d18:1/24:2) were independently associated with the risk of AKI (P < 0.05). Among them, Cer(d18:1/16:0) had the highest adjusted OR (2.046, 95% confidence interval [CI] 1.215–3.445, P = 0.007) for per SD increase, and Cer(d18:1/24:2) had the highest adjusted OR (3.503, 95% CI 1.743–7.040, P < 0.001) when Q4 was compared with Q1. The multivariable logistic regression analysis results were consistent for patients with NSTE-ACS and STEMI (Additional file 2: Table S1). We also analyzed the ratios of all 10 ceramides to Cer(d18:1/24:0). As shown in Additional file 2: Table S2, all 10 ratios were independently associated with AKI.
Unadjusted and adjusted OR of eleven ceramides for AKI. Models were adjusted by age, sex (male vs. female), systolic blood pressure, heart rate, body mass index, statin (yes vs. no), hypertension (yes vs. no), diabetes (yes vs. no), hyperlipidemia (yes vs. no), Killip class (I vs. II vs. III vs. IV), white blood cell count, low-density lipoprotein cholesterol, total cholesterol, triglyceride, estimated glomerular filtration rate, high sensitive cardiac troponin T, N-terminal pro-brain natriuretic peptide, and Mehran risk score. OR odds, ratio, CI confidence interval, AKI acute kidney injury
Predictive value of ceramides
ROC curve analysis was conducted to evaluate the discrimination of Mehran risk score and ceramides for AKI (Table 3). These ceramides achieved an AUC of 0.581–0.661 (P < 0.001) for AKI, and the AUC of the Mehran risk score was 0.780 (95% CI 0.738–0.821, P < 0.001). In order to evaluate the additional prognostic value of ceramides with respect to AKI risk beyond the Mehran risk score, models of each ceramide combined with the Mehran risk score were calculated and achieved an AUC of 0.802–0.808, which was significantly greater than that of the Mehran risk score alone (P < 0.05, Table 3). Moreover, the AUC of the ratio of the 10 ceramides to Cer(d18:1–24:0) for patients with ACS was 0.550–0.738, significantly larger than that of the 10 ceramides alone (Additional file 2: Table S3). Notably, the ratio of Cer(d18:1–24:2) to Cer(d18:1–24:0) had the highest AUCs among the ceramides.
Discussion
In this study, the incidence of AKI in patients with ACS was 16.5%, similar to those in previous meta-analysis reports (15.8%) and our previous retrospective study [41, 42]. We tested 11 ceramides using targeted LC–MS/MS; the chain lengths ranged from 16 to 26. Patients with AKI had higher levels of long-chain ceramides (C16:0, C18:0, C20:0, and C21:0) and very long-chain ceramides (C24:1 and C24:2). Furthermore, in risk-factor adjusted logistic models, these ceramides were independently associated with AKI events in patients with both STEMI and NSTE-ACS. Per Spearman’s correlation analysis, these ceramides positively correlated with the ACS risk score, contrast-induced nephropathy risk score, cardiac marker, baseline renal function, stress marker, and inflammatory markers, all of which may be potential contributing factors to AKI.
Previous studies have confirmed the relationship between ceramides, cardiovascular disease progression, and adverse events [7,8,9,10]. However, most studies only focused on Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/24:0), and Cer(d18:1/24:1) [5, 9, 43]. To our knowledge, we provided a wider spectrum of ceramides in cardiovascular research; we identified six ceramides related to AKI. Moreover, incremental predictive power was shown when ceramides were standardised to Cer(d18:1/24:0) [7,8,9,10, 44], which is highly abundant and stable in plasma and unaffected by the disease. Consistent with previous reports, ceramides standardised to Cer(d18:1/24:0) had a higher OR and AUC, especially Cer(d18:1/24:2).
Given that ACS patients are often exposed to contrast agents during treatment, the Mehran risk score for the prediction of contrast-induced nephropathy after PCI was established in 2004 [37]. Similar to previous studies, the AUC of the Mehran risk score was 0.78 in this study [45, 46]. Although ceramides alone demonstrated a poor discrimination power for AKI, when combined with the Mehran risk score, the AUC could significantly improve over 0.80. These results suggested that ceramides significantly increase the predictive effect of AKI beyond traditional scoring. It may be because they are involved in other mechanisms of AKI. According to a review by Ueda, ceramides are synthesised under stimulation and lead to apoptosis in renal tubular cells through mitogen-activated protein kinases signal [16]. Furthermore, a major precondition of AKI is producing reactive oxygen species [47]. In vivo and in vitro studies have explored the role of ceramide triggers in generating reactive oxygen species and the increase in oxidative stress that leads to endothelial dysfunction and renal function injury [14, 48]. More importantly, one study showed that plasma ceramide from other tissues and organs might also cause kidney damage [30]; upregulated ceramide levels in ACS patients may have derived from the cardiovascular system and led to AKI. Additionally, some studies found that patients with chronic kidney disease had elevated plasma ceramide levels [28, 29]. Previous studies found that long-chain (C16, C22) and very long-chain (C24) ceramides accounted for 20%, 10%, and 70%, respectively, of the amount of ceramides in the renal cortex [49]. In plasma, very long chain ceramides (C24) also have the highest mass fraction (approximately 30%), and Cer(d18:1/24:2) normalised to Cer(d18:1/24:0) had the best performance for AKI prediction. These results suggested that very long-chain ceramides (C24) may be key bioactive substances in the pathophysiology of AKI.
The application prospect of ceramides as biomarkers of AKI is that it may measure risk and guide interventions. Although randomised controlled trials regarding ceramides have not been reported, some studies have found that plasma ceramide levels could be reduced following aerobic exercise and statin therapy [12, 50]. While exercise and lipid-lowering treatment can also prevent the occurrence of AKI [51, 52], it means that the lowering of ceramide levels can be achieved through efficient lifestyle counselling and optimal administration of statin doses, ezetimibe combinations, and novel therapies such as PCSK9 inhibitors and may be an effective protective measure against AKI. Additionally, many clinical laboratories in modern medical institutions have automatic sample processing systems and mass spectrometry equipment. Therefore, in high-throughput QC environments, the measurement of plasma ceramides could be direct and cost-effective. Nevertheless, a sample run with the method used in the present study takes 5 min, allowing only about 20 samples to be run in an hour, making it unsuitable for large-scale clinical screening of AKI, but it could be kept for selected patients. In addition, it could be possible to optimize the technique. The present study provides data for the involvement of long-chain and very-long-chain ceramides in the development of AKI after ACS. Whether these ceramides are markers of AKI development or factors involved in AKI development remains to be investigated. More research is needed to explore the relationship between ceramides in cardiovascular disease and kidney disease, as well as the interaction between them. Additionally, there are many kinds of ceramides, and their biological activities in diseases are different, which may be related to different synthetic pathways. In a word, the implications of having a deep understanding of ceramide subtypes are significant.
Limitations
First, although this was a multicentre, prospective study, owing to the relatively small sample size, additional studies are required to confirm these findings. Second, the first creatinine measure on admission was used as the baseline creatinine value, which may have been higher than the actual baseline creatinine for patients with ACS, even though only patients with onset time < 24 h were included; thus, the incidence of AKI may be underestimated, and the causality between ceramides and AKI remains inconclusive. Third, a control group of patients with CKD who did not develop AKI would have been useful, but the available data did not allow such analyses. Fourth, data for subgrouping AKI were not available. Fifth, although statins were administered to almost all patients with acute chest pain, this study did not collect data on the history of statin use, which may have impacted ceramide levels and the risk of AKI. Sixth, C12:0, C14:0, and > C26:0 ceramides were not examined in the present study, and whether they could be used for diagnosing AKI remains unknown. Seventh, ceramides have been associated with heart remodelling [11, 13], but no heart remodelling parameters were available. Finally, the role of metabolites, such as sphingosine, in ceramide synthetic pathways and carriers of ceramide, such as lipoprotein, and their relation to AKI were not studied.
Conclusion
Long-chain ceramides (C16:0, C18:0, C20:0, and C21:0) and very long-chain ceramides (C24:1 and C24:2) were independently associated with the risk of AKI. These ceramides have a significant additional predictive value for AKI beyond traditional risk assessment tools. The ratio of Cer(d18:1/24:2) to Cer(d18:1/24:0) may be an indicator to identify AKI risk and guide effective clinical prediction, prevention, and intervention. The function of ceramide subtypes in cardiorenal diseases should be further researched.
Disclosure
The authors report no disclosures relevant to the manuscript.
Availability of data and materials
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Marenzi G, Cosentino N, Bartorelli AL. Acute kidney injury in patients with acute coronary syndromes. Heart. 2015;101(22):1778–85.
Marenzi G, Cabiati A, Bertoli SV, Assanelli E, Marana I, De Metrio M, Rubino M, Moltrasio M, Grazi M, Campodonico J, et al. Incidence and relevance of acute kidney injury in patients hospitalized with acute coronary syndromes. Am J Cardiol. 2013;111(6):816–22.
Goldberg A, Hammerman H, Petcherski S, Zdorovyak A, Yalonetsky S, Kapeliovich M, Agmon Y, Markiewicz W, Aronson D. Inhospital and 1-year mortality of patients who develop worsening renal function following acute ST-elevation myocardial infarction. Am Heart J. 2005;150(2):330–7.
Kaltsas E, Chalikias G, Tziakas D. The incidence and the prognostic impact of acute kidney injury in acute myocardial infarction patients: current preventive strategies. Cardiovasc Drugs Ther. 2018;32(1):81–98.
Marenzi G, Assanelli E, Campodonico J, De Metrio M, Lauri G, Marana I, Moltrasio M, Rubino M, Veglia F, Montorsi P, et al. Acute kidney injury in ST-segment elevation acute myocardial infarction complicated by cardiogenic shock at admission. Crit Care Med. 2010;38(2):438–44.
Gault CR, Obeid LM, Hannun YA. An overview of sphingolipid metabolism: from synthesis to breakdown. Adv Exp Med Biol. 2010;688:1–23.
Anroedh S, Hilvo M, Akkerhuis KM, Kauhanen D, Koistinen K, Oemrawsingh R, Serruys P, van Geuns RJ, Boersma E, Laaksonen R, et al. Plasma concentrations of molecular lipid species predict long-term clinical outcome in coronary artery disease patients. J Lipid Res. 2018;59(9):1729–37.
Cheng JM, Suoniemi M, Kardys I, Vihervaara T, de Boer SP, Akkerhuis KM, Sysi-Aho M, Ekroos K, Garcia-Garcia HM, Oemrawsingh RM, et al. Plasma concentrations of molecular lipid species in relation to coronary plaque characteristics and cardiovascular outcome: results of the ATHEROREMO-IVUS study. Atherosclerosis. 2015;243(2):560–6.
Laaksonen R, Ekroos K, Sysi-Aho M, Hilvo M, Vihervaara T, Kauhanen D, Suoniemi M, Hurme R, März W, Scharnagl H, et al. Plasma ceramides predict cardiovascular death in patients with stable coronary artery disease and acute coronary syndromes beyond LDL-cholesterol. Eur Heart J. 2016;37(25):1967–76.
Tu C, Xie L, Wang Z, Zhang L, Wu H, Ni W, Li C, Li L, Zeng Y. Association between ceramides and coronary artery stenosis in patients with coronary artery disease. Lipids Health Dis. 2020;19(1):151.
Peterson LR, Xanthakis V, Duncan MS, Gross S, Friedrich N, Volzke H, Felix SB, Jiang H, Sidhu R, Nauck M, et al. Ceramide remodeling and risk of cardiovascular events and mortality. J Am Heart Assoc. 2018. https://doi.org/10.1161/JAHA.117.007931.
Tarasov K, Ekroos K, Suoniemi M, Kauhanen D, Sylvänne T, Hurme R, Gouni-Berthold I, Berthold HK, Kleber ME, Laaksonen R, et al. Molecular lipids identify cardiovascular risk and are efficiently lowered by simvastatin and PCSK9 deficiency. J Clin Endocrinol Metab. 2014;99(1):E45-52.
Nwabuo CC, Duncan M, Xanthakis V, Peterson LR, Mitchell GF, McManus D, Cheng S, Vasan RS. Association of circulating ceramides with cardiac structure and function in the community: the framingham heart study. J Am Heart Assoc. 2019;8(19):e013050.
Li PL, Zhang Y. Cross talk between ceramide and redox signaling: implications for endothelial dysfunction and renal disease. Handb Exp Pharmacol. 2013;216:171–97.
Basnakian AG, Ueda N, Hong X, Galitovsky VE, Yin X, Shah SV. Ceramide synthase is essential for endonuclease-mediated death of renal tubular epithelial cells induced by hypoxia-reoxygenation. Am J Physiol Renal Physiol. 2005;288(2):F308-314.
Ueda N. Ceramide-induced apoptosis in renal tubular cells: a role of mitochondria and sphingosine-1-phoshate. Int J Mol Sci. 2015;16(3):5076–124.
Ostermann M, Liu K. Pathophysiology of AKI. Best Pract Res Clin Anaesthesiol. 2017;31(3):305–14.
Raichur S, Brunner B, Bielohuby M, Hansen G, Pfenninger A, Wang B, Bruning JC, Larsen PJ, Tennagels N. The role of C16:0 ceramide in the development of obesity and type 2 diabetes: CerS6 inhibition as a novel therapeutic approach. Mol Metab. 2019;21:36–50.
Turpin SM, Nicholls HT, Willmes DM, Mourier A, Brodesser S, Wunderlich CM, Mauer J, Xu E, Hammerschmidt P, Bronneke HS, et al. Obesity-induced CerS6-dependent C16:0 ceramide production promotes weight gain and glucose intolerance. Cell Metab. 2014;20(4):678–86.
Fekry B, Jeffries KA, Esmaeilniakooshkghazi A, Ogretmen B, Krupenko SA, Krupenko NI. CerS6 is a novel transcriptional target of p53 protein activated by non-genotoxic stress. J Biol Chem. 2016;291(32):16586–96.
Yacoub A, Hamed HA, Allegood J, Mitchell C, Spiegel S, Lesniak MS, Ogretmen B, Dash R, Sarkar D, Broaddus WC, et al. PERK-dependent regulation of ceramide synthase 6 and thioredoxin play a key role in mda-7/IL-24-induced killing of primary human glioblastoma multiforme cells. Cancer Res. 2010;70(3):1120–9.
Eberle M, Ebel P, Wegner MS, Mannich J, Tafferner N, Ferreiros N, Birod K, Schreiber Y, Krishnamoorthy G, Willecke K, et al. Regulation of ceramide synthase 6 in a spontaneous experimental autoimmune encephalomyelitis model is sex dependent. Biochem Pharmacol. 2014;92(2):326–35.
Bai X, He T, Liu M, Li L, Chen J, Cao M, Liu Y, Yang C, Jia W, Tao K, et al. Integrative analysis of MicroRNAs and mRNAs in LPS-induced macrophage inflammation based on adipose tissue stem cell therapy. Inflammation. 2021;44(1):407–20.
Hernandez-Corbacho MJ, Canals D, Adada MM, Liu M, Senkal CE, Yi JK, Mao C, Luberto C, Hannun YA, Obeid LM. Tumor Necrosis Factor-alpha (TNFalpha)-induced ceramide generation via ceramide synthases regulates loss of Focal Adhesion Kinase (FAK) and programmed cell death. J Biol Chem. 2015;290(42):25356–73.
Kim YR, Lee EJ, Shin KO, Kim MH, Pewzner-Jung Y, Lee YM, Park JW, Futerman AH, Park WJ. Hepatic triglyceride accumulation via endoplasmic reticulum stress-induced SREBP-1 activation is regulated by ceramide synthases. Exp Mol Med. 2019;51(11):1–16.
Stiban J, Perera M. Very long chain ceramides interfere with C16-ceramide-induced channel formation: a plausible mechanism for regulating the initiation of intrinsic apoptosis. Biochim Biophys Acta. 2015;1848(2):561–7.
Nicholson RJ, Pezzolesi MG, Summers SA. Rotten to the cortex: ceramide-mediated lipotoxicity in diabetic kidney disease. Front Endocrinol (Lausanne). 2020;11:622692.
Mantovani A, Lunardi G, Bonapace S, Dugo C, Altomari A, Molon G, Conti A, Bovo C, Laaksonen R, Byrne CD, et al. Association between increased plasma ceramides and chronic kidney disease in patients with and without ischemic heart disease. Diabetes Metab. 2021;47(1):101152.
Mitsnefes M, Scherer PE, Friedman LA, Gordillo R, Furth S, Warady BA. Ceramides and cardiac function in children with chronic kidney disease. Pediatric Nephrol (Berlin, Germany). 2014;29(3):415–22.
Ichi I, Kamikawa C, Nakagawa T, Kobayashi K, Kataoka R, Nagata E, Kitamura Y, Nakazaki C, Matsura T, Kojo S. Neutral sphingomyelinase-induced ceramide accumulation by oxidative stress during carbon tetrachloride intoxication. Toxicology. 2009;261(1–2):33–40.
Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, et al. 2014 AHA/ACC guideline for the management of patients with Non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014;64(24):e139–228.
O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78–140.
Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, Van De Werf F, Avezum A, Goodman SG, Flather MD, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163(19):2345–53.
Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51(3):606.
Jia Y, Gao Y, Li D, Cao Y, Cheng Y, Li F, Xiao L, Jiang Y, Wan Z, Zeng Z, et al. Geriatric nutritional risk index score predicts clinical outcome in patients with acute ST-segment elevation myocardial infarction. J Cardiovasc Nurs. 2020;35(6):E44-e52.
Jia Y, Li H, Li D, Li F, Li Q, Jiang Y, Gao Y, Wan Z, Cao Y, Zeng Z, et al. Prognostic value of Braden scale in patients with acute myocardial infarction: from the retrospective multicenter study for early evaluation of acute chest pain. J Cardiovasc Nurs. 2020;35(6):E53-e61.
Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, Mintz GS, Lansky AJ, Moses JW, Stone GW, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44(7):1393–9.
Section 2: AKI Definition. Kidney international supplements 2012;2(1):19–36. https://doi.org/10.1038/kisup.2011.32
Sarafian MH, Gaudin M, Lewis MR, Martin FP, Holmes E, Nicholson JK, Dumas ME. Objective set of criteria for optimization of sample preparation procedures for ultra-high throughput untargeted blood plasma lipid profiling by ultra performance liquid chromatography-mass spectrometry. Anal Chem. 2014;86(12):5766–74.
Huang Q, Hao S, Yao X, You J, Li X, Lai D, Han C, Schilling J, Hwa KY, Thyparambil S, et al. High-throughput quantitation of serological ceramides/dihydroceramides by LC/MS/MS: pregnancy baseline biomarkers and potential metabolic messengers. J Pharm Biomed Anal. 2021;192:113639.
Pickering JW, Blunt IRH, Than MP. Acute kidney injury and mortality prognosis in acute coronary syndrome patients: a meta-analysis. Nephrology (Carlton). 2018;23(3):237–46.
Yu J, Li D, Jia Y, Li F, Jiang Y, Zhang Q, Gao Y, Liao X, Zeng R, Wan Z. Nutritional risk screening 2002 was associated with acute kidney injury and mortality in patients with acute coronary syndrome: Insight from the REACP study. Nutr Metab Cardiovasc Dis. 2021;31(4):1121–8.
Gencer B, Morrow DA, Braunwald E, Goodrich EL, Hilvo M, Kauhanen D, Sabatine MS, Laaksonen R, O’Donoghue ML. Plasma ceramide and phospholipid-based risk score and the risk of cardiovascular death in patients after acute coronary syndrome. Eur J Prev Cardiol. 2020. https://doi.org/10.1093/eurjpc/zwaa143.
Yao K, Wang Y, Xu D, Liu X, Shen C, Hu W, Wang Z, Wu R, Tang X, Sun A, et al. Effect of combined testing of ceramides with high-sensitive troponin T on the detection of acute coronary syndrome in patients with chest pain in China: a prospective observational study. BMJ Open. 2019;9(7):e028211.
Abellás-Sequeiros RA, Raposeiras-Roubín S, Abu-Assi E, González-Salvado V, Iglesias-Álvarez D, Redondo-Diéguez A, González-Ferreiro R, Ocaranza-Sánchez R, Peña-Gil C, García-Acuña JM, et al. Mehran contrast nephropathy risk score: Is it still useful 10 years later? J Cardiol. 2016;67(3):262–7.
Koowattanatianchai S, Chantadansuwan T, Kaladee A, Phinyo P, Patumanond J. Practical risk stratification score for prediction of contrast-induced nephropathy after primary percutaneous coronary intervention in patients with acute ST-segment elevation myocardial infarction. Cardiol Res. 2019;10(6):350–7.
Rodriguez F, Bonacasa B, Fenoy FJ, Salom MG. Reactive oxygen and nitrogen species in the renal ischemia/reperfusion injury. Curr Pharm Des. 2013;19(15):2776–94.
Ueda N, Camargo SMR, Hong X, Basnakian AG, Walker PD, Shah SV. Role of ceramide synthase in oxidant injury to renal tubular epithelial cells. J Am Soc Nephrol. 2001;12(11):2384–91.
Kalhorn T, Zager RA. Renal cortical ceramide patterns during ischemic and toxic injury: assessments by HPLC-mass spectrometry. Am J Physiol. 1999;277(5):F723-733.
Bergman BC, Brozinick JT, Strauss A, Bacon S, Kerege A, Bui HH, Sanders P, Siddall P, Kuo MS, Perreault L. Serum sphingolipids: relationships to insulin sensitivity and changes with exercise in humans. Am J Physiol Endocrinol Metab. 2015;309(4):E398-408.
Couto SMF, Machado DI, Conde C, Silva VC, Souza AA, Peres KB, Brandi BA, Vattimo MFF. Physical training is a potential modifier of risk for contrast-induced acute kidney injury in diabetes mellitus. Biomed Res Int. 2020;2020:1830934.
Pistolesi V, Regolisti G, Morabito S, Gandolfini I, Corrado S, Piotti G, Fiaccadori E. Contrast medium induced acute kidney injury: a narrative review. J Nephrol. 2018;31(6):797–812.
Acknowledgements
We want to thank all the participants of this project and the investigators for collecting the data.
Funding
This work was supported financially by grants from the National Key Research and Development Program of China (No. 2020AAA0105000, 2020AAA0105005), Sichuan Science and Technology Program (No. 2022YFS0279, 2021YFQ0062), Sichuan Provincial Health Commission (Chuanganyan ZH2022-101), Sichuan University West China Nursing Discipline Development Special Fund Project (HXHL20017, HXHL20046, HXHL21016).
Author information
Authors and Affiliations
Contributions
Conceived the study design. DL and DL collected the epidemiological and clinical data. DL, WW, and LJ summarized data and performed the statistical analysis. DL and LJ interpreted the data and drafted the manuscript. DL, WW, and LJ participated in the design of the study, acquired the data, and helped to revise the manuscript. All the authors have accepted responsibility for the entire content of this submitted manuscript and approved the submission. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. The Human Ethical Committee of West China Hospital of Sichuan University approved the study protocol. All participants provided written informed consent before enrollment. This report was written in compliance with the STROBE statements for observational studies. Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
(A) Correlation analysis among all eleven ceramides. The value in the heat map is the correlation coefficient. * < 0.05; ** < 0.001; *** < 0.0001. (B) The average mass fraction of all eleven ceramides in ACS patients.
Additional file 2: Table S1.
Relationships between ceramides and acute kidney injury in patients with STEMI and NSTE-ACS according to multivariate Logistic regression analysis. Table S2. Relationships between ratio of ten ceramides to Cer(d18:1–24:0) and acute kidney injury in patients with acute coronary syndrome. Table S3. Predictive value of ratio of ten ceramides to Cer(d18:1–24:0) for patients with acute coronary syndrome.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liang, L., Li, D., Zeng, R. et al. Long- and very long-chain ceramides are predictors of acute kidney injury in patients with acute coronary syndrome: the PEACP study. Cardiovasc Diabetol 22, 92 (2023). https://doi.org/10.1186/s12933-023-01831-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-01831-6