Abstract
Background
An “obesity paradox” for mortality has been shown in chronic disorders such as diabetes, and attributed to methodological bias, including the use of body mass index (BMI) for obesity definition. This analysis investigated the independent association of BMI versus surrogate measures of central adiposity with all-cause mortality in individuals with type 2 diabetes.
Methods
The Renal Insufficiency And Cardiovascular Events Italian Multicentre Study is a prospective cohort study that enrolled 15,773 patients in 19 Italian centres in 2006–2008. Exposures were BMI and the surrogate measures of central adiposity waist circumference (WC), waist-to-height ratio (WHtR), and A Body Shape Index (ABSI). Vital status was retrieved on 31 October 2015 for 15,656 patients (99.3%),
Results
Age- and sex-adjusted hazard ratios and 95% confidence intervals were significantly higher in BMI-based underweight (1.729 [1.193–2.505), P = 0.004), moderately obese (1.214 [1.058–1.392), P = 0.006) and severely obese (1.703 [1.402–2.068), P < 0.0001), lower in overweight (0.842 [0.775–0.915), P < 0.0001) and similar in mildly obese (0.950 [0.864–1.045), P = 0.292), compared to normal-weight individuals. When further adjusting for smoking, physical activity (PA), and comorbidities, risk was lower also in mildly obese versus normal-weight patients. The BMI-mortality relationship did not change after sequentially excluding ever smokers, individuals with comorbidities, and those died within two years from enrollment and when analyzing separately participants below and above the median age. Conversely, a paradox relationship was observed among inactive/moderately inactive, but not moderately/highly active patients. Mortality risk adjusted for age, gender, smoking, PA and comorbidities was significantly higher in the highest tertile of WC (1.279 [1.089–1.501], P = 0.003), WHtR (1.372 [1.165–1.615], P < 0.0001), and ABSI (1.263 [1.067–1.495], P = 0.007) versus the lowest tertile. However, risk was lower in the intermediate versus lowest tertile for WC (0.823 [0.693–0.979], P = 0.028), similar for WHtR, and higher, though not significantly, for ABSI.
Conclusions
An “overweight paradox” remained after controlling for age, smoking, and comorbidities, arguing against a collider bias or reverse causation. However, it could be partly explained by confounding from PA level, possibly through its impact on lean mass and cardiorespiratory fitness. No obesity paradox was observed with WHtR and especially ABSI, which predicted mortality risk associated with central adiposity better than WC.
Trial registration ClinicalTrials.gov, NCT00715481, 15 July, 2008
Similar content being viewed by others
Background
In the general population, higher body mass index (BMI) is associated with increased all-cause mortality [1], with the nadir of the curve generally found in the upper normal-weight range [2], though the relationship is J-shaped [3], as also underweight carries an increased risk of death. However, numerous epidemiological surveys have reported an association of increased BMI with decreased mortality in older individuals as well as in patients in acute clinical settings or suffering from several chronic disorders, suggesting that a mild-to-moderate excess of fat might be protective under these conditions [4].
Indeed, this so-called “obesity paradox” has been attributed to misclassification bias caused by methodological problems. Potential sources of bias include residual or unmeasured confounding, if relevant variables are not taken into account. An example is physical fitness, including cardiorespiratory and muscle fitness, which are both associated with better survival irrespective of BMI [5]. An inverse relationship between exposure (obesity) and outcome (death) has also been related to reverse causation, as unintentional weight loss may be a consequence of several, potentially fatal illnesses, thereby increasing mortality among previously overweight or obese individuals who had become non-obese because of the disease [6]. Another reason can be selection bias, including survivor bias and collider bias. A survivor bias may occur if the most obese and sickest individuals have already died at the time of enrolment, though obese patients might also have better outcomes because they are treated more aggressively than non-obese individuals [7]. A collider bias may be due to smoking, which is inversely related to BMI and is a stronger risk factor for mortality than obesity itself, thus potentially reversing the direction of the association between the two [8].
However, the main source of bias might be the use of BMI as a measure of obesity, as weight reflects not only fat mass but also lean (muscle) mass and does not provide information about the central (visceral) versus peripheral (subcutaneous) distribution of fat accumulation [9]. Hence, differences in the relative contributions to BMI of “harmful” fat mass and central fat versus “protective” lean mass and peripheral fat have been claimed for explaining the obesity paradox [9]. The reported weakening of the BMI-mortality relationship with increasing age [10] may in fact be related to the combination of decreased muscle mass and increased central fat in the context of an overall reduction of body weight (and BMI) characterizing older individuals [7]. Consistently, surrogate measures of visceral adiposity, such as waist circumference (WC) and waist-to-hip ratio (WHR), were reported to be linearly related to death in subjects with coronary artery disease [11] and recent evidence indicates that two WC-derived measures, waist-to-height ratio (WHtR) [12] and A Body Shape Index (ABSI) [13] predict mortality even better than WC and WHR.
An obesity paradox has been almost consistently shown in people with type 2 diabetes [14, 15], with the lowest mortality in those with a BMI in the overweight [16,17,18,19] or even the obesity [20,21,22,23,24] range. However, in these individuals, the BMI-mortality relationship may be strongly influenced by confounding due to reverse causation from associated comorbidities or low fitness and related changes in body composition [25, 26]. Two studies using a multiple obesity index approach have in fact shown that either WHtR [27] or ABSI [28] are superior to both BMI and WC as predictors of mortality also in patients with type 2 diabetes. In order to confirm and extend these observations, the present analysis aimed at assessing the independent association of BMI versus surrogate measures of central adiposity (including both WHtR and ABSI) with death from any cause in the large cohort of well-characterized individuals with type 2 diabetes from the Renal Insufficiency And Cardiovascular Events (RIACE) Italian Multicentre Study, which allows accounting for several potential sources of bias.
Methods
Design
The RIACE is an observational, prospective, cohort study on the impact of estimated glomerular filtration rate (eGFR) on morbidity and mortality in individuals with type 2 diabetes [29]. The study was conducted in accordance with the Declaration of Helsinki. The research protocol was approved by the locally appointed ethics committees and participants provided an informed consent.
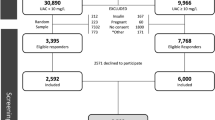
Patients
The study population included 15,773 Caucasian patients (after excluding 160 individuals with missing or implausible values), consecutively attending 19 hospital-based, tertiary referral Diabetes Clinics of the National Health Service throughout Italy in the years 2006–2008. Exclusion criteria were dialysis or renal transplantation.
All-cause mortality
The vital status of study participants on 31 October 2015 was verified by interrogating the Italian Health Card database (http://sistemats1.sanita.finanze.it/wps/portal/), which provides updated and reliable information on all current Italian residents [30].
Baseline measurements
Baseline data were collected using a standardized protocol across participating centres [29].
Participants underwent a structured interview in order to collect the following information: age at the time of the interview, smoking status, physical activity (PA) level; known diabetes duration, current glucose-, lipid-, and blood pressure (BP)-lowering treatments, and severe comorbidities. Patients were categorized by smoking status as never, former, or current smokers and by moderate-to-vigorous PA level as physically inactive or moderately inactive (< 60 min·week−1), moderately active (60–150 min·week−1), or highly active (> 150 min·week−1). Comorbidities included chronic obstructive pulmonary disease (COPD), chronic liver disease, and cancer.
The BMI was calculated from weight and height and BP was measured with a sphygmomanometer with the patients seated with the arm at the heart level. Moreover, WC was measured at the umbilicus and then divided by height to obtain WHtR [12, 27] and used together with BMI and height for calculating ABSI by the formula: WC/(BMI2/3 × height1/2) [13, 28].
Haemoglobin A1c (HbA1c) and fasting levels of triglycerides and total and HDL cholesterol were measured by standard methods. The triglyceride:HDL cholesterol ratio (TG:HDL) was then calculated by dividing triglyceride for HDL cholesterol levels (both in mg/dl) and LDL cholesterol was estimated by the Friedewald formula.
The presence of diabetic kidney disease (DKD) was assessed by measuring albuminuria and serum creatinine, as previously detailed [31]. Patients were then assigned to one of the following DKD phenotypes: no DKD, albuminuria alone (albuminuric DKD with preserved eGFR), reduced eGFR alone (non-albuminuric DKD), or both albuminuria and reduced eGFR (albuminuric DKD with reduced eGFR).
In each centre, the presence of diabetic retinopathy (DR) was assessed by an expert ophthalmologist by dilated fundoscopy. Patients with mild or moderate non-proliferative DR were classified as having non-advanced DR, whereas those with severe non-proliferative DR, proliferative DR, or maculopathy were grouped into the advanced DR category. DR grade was assigned based on the worse eye [32].
Previous major acute CVD events, including myocardial infarction; stroke; foot ulcer/gangrene/amputation; and coronary, carotid, and lower limb revascularization, were adjudicated based on hospital discharge records by an ad hoc committee in each centre [29].
The above data were obtained from all participants, except for WC, which was available only from 5 out 19 centres (4618 individuals), and LDL cholesterol, which was calculable only for 15,501 patients because of triglyceride levels exceeding 4.5 mmol l−1 in the remaining 272 individuals.
Statistical analysis
For the purpose of the current analysis, the RIACE cohort was divided into the following BMI categories (kg·m−2): underweight (< 18.5), normal-weight (18.5–24.9), overweight (25.0–29.9), grade I or mild obesity (30.0–34.9), grade II or moderate obesity (35.0–39.9), and grade III or severe obesity (≥ 40.0). In addition, the individuals with available WC measurements were divided into sex-specific tertiles of WC, WHtR, and ABSI, three surrogate measures of central adiposity.
Data are expressed as mean ± SD or median (interquartile range) for continuous variables, and number of cases and percentage for categorical variables. Comparisons among groups were performed by one-way ANOVA for continuous variables and by Pearson’s χ2 test for categorical variables.
Crude mortality rates were described as events per 1000 patient-years, with 95% exact Poisson confidence intervals (CIs) and adjusted for age and sex by a Poisson regression model. Kaplan–Meier survival probabilities for all-cause mortality were estimated according to BMI categories and WC or WHtR tertiles and differences were analysed using the log-rank statistic. The hazard ratios (HRs) and their 95% CIs were estimated by Cox proportional hazards regression, using the normal-weight category as reference. These analyses were adjusted for age and sex (model 1), plus smoking, PA level, and severe comorbidities (model 2), plus CVD risk factors, i.e., diabetes duration, HbA1c, triglycerides, total and HDL cholesterol, and systolic and diastolic BP, and treatment, i.e., anti-hyperglycaemic, lipid-lowering, and anti-hypertensive therapy (model 3), and plus presence of complications, i.e., DKD phenotypes, DR grade and any CVD (model 4). The analyses by WC and WHtR tertiles were adjusted also for BMI. All the analyses were repeated separately for men and women. In addition, the analyses by BMI categories were repeated (a) separately in participants below and above the median age (i.e., 67.25 years) and in physically inactive or moderately inactive versus moderately and highly active individuals; and (b) after sequentially excluding former or current smokers, patients with comorbidities, and those who died within two years since enrolment.
All p values were two-sided, and a p < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 13.0 (SPSS Inc., Chicago, IL, USA).
Results
Overall mortality in the study population
Valid information on vital status was retrieved for 99.3% of participants (15,656 out of 15,773) and 99.1% of those with available WC values (4,578 out of 4,618). At the time of the census, 3,602 (23.0%) individuals had died; death rate was 31.0 per 1000 person-years (95% CI 30.0, 32.0) over a mean follow-up of 7.4 ± 2.1 years, as previously reported [31].
Clinical features and mortality by BMI categories
The baseline clinical features of the RIACE participants stratified by BMI categories are shown in Additional file 2: Table S1. Age, proportion of current smokers, PA level, diabetes duration, and HDL cholesterol decreased, whereas HbA1c, triglycerides, triglycerides:HDL ratio, systolic and diastolic BP, and prevalence of anti-hypertensive treatment increased from the lowest to the highest BMI category. Moreover, a U-shaped trend was observed for proportion of females, albuminuria, eGFR, and prevalence of insulin and anti-coagulant treatment. Finally, underweight individuals showed the lowest prevalence of any CVD, whereas the highest prevalence of chronic liver disease and cancer and the lowest prevalence of COPD were observed in the underweight group and opposite figures were detected in the severely obese group.
Percent deaths (Additional file 2: Table S1), crude mortality rates (Table 1), Kaplan–Meier estimates (Fig. 1A), and unadjusted HRs (Fig. 1B) were higher in underweight and, to a lesser extent, normal-weight participants versus all other BMI categories. When adjusted for age and sex, mortality rates (Table 1) and HRs (Fig. 1C) remained significantly higher in underweight and significantly lower in overweight, as compared with normal-weight individuals; however, mortality became higher in severely obese and, to a lesser extent, moderately obese than in normal-weight participants, as age was much higher in the latter group. When adjusting also for smoking, PA level, and comorbidities, mortality risk was significantly lower also in mildly obese versus normal-weight individuals (Fig. 1D). When further adjusting for CVD risk factors and complications, mortality risk was not significantly different in mildly and moderately obese versus normal weight individuals (not shown). The HRs were similar in patients below (Additional file 3: Fig. S1A, B) and above (Additional file 3: Fig. S1C, D) the median age; conversely, the U-shaped relationship between BMI and mortality was maintained in inactive or moderately inactive participants (Fig. 2A, B), but not in moderately or highly active individuals (Fig. 2C, D). Moreover, when sequentially excluding former and current smokers, participants with comorbidities, and those who died within 2 years from enrolment, mortality risk in overweight and mildly obese patients remained lower and not significantly different, respectively, versus normal-weight individuals (Additional file 4: Fig. S2). Results were similar in males and females (Additional file 5: Table S2).
Survival analysis by BMI categories. Kaplan–Meier analysis (A) and Cox proportional hazards regression, unadjusted (B) and adjusted for age and sex (C), and age, sex, smoking status, PA level, and comorbidities (D), according to BMI categories. Numbers (percentages) of deaths and HRs (95% CI) for mortality are shown for each group. BMI: body mass index; PA: physical activity; HR: hazard ratio; CI: confidence interval; UW: underweight; NW: normal-weight; OW: overweight; Ob-I: grade I obesity; Ob-II: grade II obesity; Ob-III: grade III obesity
Survival analysis by PA level. Cox proportional hazards regression, adjusted for age and sex (A, C) and age, sex, smoking status, and comorbidities (B, D), according to BMI categories, in inactive or moderately inactive (A, B) and moderately or highly active (C, D) patients. HRs (95% CI) for mortality are shown for each group. PA: physical activity; BMI: body mass index; HR: hazard ratio; CI: confidence interval; UW: underweight; NW: normal-weight; OW: overweight; Ob-I: grade I obesity; Ob-II: grade II obesity; Ob-III: grade III obesity
Clinical features and mortality by surrogate measures of central adiposity
The clinical features of participants with WC measurements are shown in Additional file 6: Table S3. As compared with those without WC measurements, they were younger and had lower diabetes duration and HbA1c levels than those without. As a consequence, they had also lower prevalence of complications (except DR) and death (19.0 vs 24.7%, P < 0.0001) and lower unadjusted death rate (24.15 [22.60–25.81] vs 34.11 [32.86–35.42] per 1,000 patient-years, P < 0.0001) and mortality risk (0.704 [0.652–0.760], P < 0.0001) than participants without WC measurements. However, both death rate (12.56 [11.02–14.32] vs 12.76 [11.30–14.41] per 1,000 patient-years, P = 0.697) and mortality risk (0.977 [0.904–1.057], P = 0.563) became similar after adjusting for age and sex.
The three measures of central adiposity were significantly correlated between each other and with BMI. Correlations were stronger between WC and WHtR than between either one and ABSI; compared with WC and WHtR, correlation of ABSI with BMI was weaker and inverse (Additional file 7: Table S4).
The clinical features of the RIACE participants stratified by WC, WHtR, and ABSI tertiles are shown in in Additional file 8: Table S5, respectively. Individuals in tertile III were slightly older, more frequently current smokers, with lower PA level (except for ABSI), LDL cholesterol, and eGFR and higher HbA1c, triglycerides, triglycerides:HDL ratio, systolic BP, albuminuria, and prevalence of hypertension, insulin, anti-hypertensive, anti-platelet, and anti-coagulant treatment, DKD, DR, CVD, and comorbidities, especially COPD, compared to those in tertile I of each measure. Moreover, BMI increased and HDL cholesterol decreased from tertile I to tertile III of WC and WHtR, whereas the opposite trend was observed for ABSI.
Percent deaths (Additional file 8: Table S5), crude and age- and sex-adjusted mortality rates (Table 1), Kaplan–Meier estimates (Figs. 3A, 4A, and 5A), and unadjusted HRs (Figs. 3B, 4B, and 5B) were higher in tertile III versus tertile I of each measure. Significant differences remained when adjusting for age and sex (Figs. 3C, 4C, and 5C) and when further adjusting for smoking, PA level, and comorbidities (Figs. 3D, 4D, and 5D) and, except for WC, for CVD risk factors and complications (not shown). Moreover, HRs were significantly lower in tertile II versus tertile I of WC when sequentially adjusting for age, sex, smoking, PA level, and comorbidities (Fig. 3C, D) and even after further adjustment for CVD risk factors and complications (not shown), whereas no significant differences were detected between tertile II and tertile I of WHtR (Fig. 4C, D) and an opposite, though non-significant trend was observed for ABSI (Fig. 5C, D). Further adjustment for BMI did not affect the association of WC and WHtR with mortality (not shown). Results of the analyses conducted separately in men and women yielded the same results as in the whole cohort for WC and WHtR tertiles, whereas the linear relationship between ABSI tertiles and death was evident only in males (Additional file 5: Table S2). Moreover, the associations between WC or WHtR and mortality were unaffected by further adjustment for BMI in males, whereas they disappeared in females (not shown).
Survival analysis by WC tertiles. Kaplan–Meier analysis (A) and Cox proportional hazards regression, unadjusted (B) and adjusted for age and sex (C), and age, sex, smoking status, PA level, and comorbidities (D), according to WC tertiles. Numbers (percentages) of deaths and HRs (95% CI) for mortality are shown for each group. WC: waist circumference; PA: physical activity; HR: hazard ratio; CI: confidence interval
Survival analysis by WHtR tertiles. Kaplan Meier analysis (A) and Cox proportional hazards regression, unadjusted (B) and adjusted for age and sex (C), and age, sex, smoking status, PA level, and comorbidities (D), according to WHtR tertiles. Numbers (percentages) of deaths and HRs (95% CI) for mortality are shown for each group. WHtR: waist-to-height ratio; PA: physical activity; HR: hazard ratio; CI: confidence interval
Survival analysis by ABSI tertiles. Kaplan–Meier analysis (A) and Cox proportional hazards regression, unadjusted (B) and adjusted for age and sex (C), and age, sex, smoking status, PA level, and comorbidities (D), according to ABSI tertiles. Numbers (percentages) of deaths and HRs (95% CI) for mortality are shown for each group. ABSI: A Body Shape Index; PA: physical activity; HR: hazard ratio; CI: confidence interval
Discussion
By comparing BMI and three surrogate indices of central adiposity as measure of obesity, this analysis provides important insights into the obesity paradox for mortality in patients with type 2 diabetes. On the one hand, the paradox relationship between BMI and death was limited to the overweight category, with the individuals with grade I obesity showing no survival advantage compared to those in the normal-weight range. On the other hand, an obesity paradox was also observed when adiposity was defined using WC, but not WHtR and especially ABSI, instead of BMI.
The nadir for mortality risk in the overweight range is consistent with previous studies in people with type 2 diabetes [16,17,18,19], though other surveys showed a nadir for mortality well above the obesity threshold [20,21,22,23,24]. Furthermore, a meta-analysis of 414,587 participants with type 2 diabetes reported that all-cause mortality was lowest in those with a BMI in the overweight and obesity range in women and men, respectively [15], and a pooled analysis of 5 longitudinal cohort studies showed a lower adjusted risk of death in overweight/obese than in normal-weight adults with incident diabetes [14]. However, a survival benefit for overweight individuals was also reported in a meta-analysis of 97 prospective studies of general populations of adults [33] and in both diabetic and non-diabetic individuals from the US National Health Interview Survey [16], pointing to the existence of a BMI paradox rather than an obesity/overweight paradox.
The unchanged relationship between BMI and mortality after controlling for age, smoking, and comorbidities argues against a confounding from collider bias or reverse causation. The same BMI-mortality curve as in the entire cohort was in fact obtained after sequentially excluding ever smokers, patients with comorbidities, and those who died within 2 years of follow-up and when analyzing separately participants below and above the median age. In addition, when further adjusting for smoking, PA level, and comorbidities, risk of death versus normal-weight individuals became significantly lower also in those in the mildly obese range. This is at variance with reports from the general population or people with type 2 diabetes showing no obesity paradox when considering factors potentially affecting this association. In fact, an inverse relationship between BMI and death was found in diabetic individuals aged ≥ 65 years and a direct one in those aged < 65 years [34]. Moreover, previous studies showed an obesity paradox among ever smokers, but not never smokers [35, 36], and an attenuated or no obesity paradox when restricting the analysis to never smokers without previous disease who survived at least 5 or 3 years, respectively [1, 16]. However, a study in patients with type 2 diabetes also reported that the association of BMI and central adiposity measures with mortality did not change when excluding individuals with cancer or surviving at least one year [28].
The U-shaped BMI-mortality curve observed in inactive or moderately inactive participants, but not in those accumulating moderate or high amounts of PA, suggests that the obesity (overweight) paradox might be explained, at least partly, by two unmeasured PA-related confounders that are rarely accounted for in studies assessing the relationship between obesity and mortality, i.e., physical fitness and body composition. In this view, underweight and even normal-weight individuals with a low PA level showed an increased risk of death compared to overweight patients because their lower body weight was also due to reduced muscle mass and was associated with poor cardiorespiratory fitness. Vice versa, overweight individuals with a high PA level showed a decreased risk of death compared to normal-weight patients because their higher body weight was also due to preserved muscle mass and was associated with good cardiorespiratory fitness. Our findings are consistent with previous studies investigating the relationship of cardiorespiratory fitness and lean (muscle) mass with death. The obesity paradox was in fact shown in patients with low but not in those with high cardiorespiratory fitness, regardless of using BMI, percent body fat or WC as a measure of adiposity [37]. Moreover, low fitness and obesity were independently and cumulatively associated with increased mortality [20] and fitness modified the effect of fatness to produce the obesity paradox [38], with individuals with good fitness and high BMI showing a lower risk for all-cause and CVD mortality than those with poor fitness and normal BMI [39]. Low lean mass, rather than low fat mass, was responsible for the increased mortality among individuals with low to normal BMI [40]. Furthermore, in older patients with heart failure, low BMI was a better indicator of reduction in lean mass than of reduction in fat mass [41], and, in patients with cancer, an obesity paradox emerged when using BMI, but was not confirmed by analyses based on body composition [42]. However, muscle mass (and its contribution to body weight/BMI and body composition) does not necessarily reflect muscle strength (i.e., muscular fitness), which is a better marker of muscle quality than mass and a major factor influencing mortality independently of cardiorespiratory fitness [37].
Although muscle mass and function and cardiorespiratory fitness may have contributed to the overweight paradox in the RIACE cohort, a potential role for moderate adiposity in providing a survival benefit cannot be ruled out. In patients with stable coronary heart disease, both lean and fat mass were in fact shown to predict death, with the highest mortality in those with low lean and fat mass and the lowest mortality in those with high lean and fat mass and one condition being protective independently of the other [43]. Moreover, subcutaneous adipose tissue may be protective in cancer due to better nutritional status, with moderate amounts enabling patients to survive longer weight losses that can occur with tumour progression and treatment [44].
The lower mortality risk in the intermediate versus the lowest WC tertile seems to suggest a protective effect of moderate adiposity even at the visceral level. This at variance with previous reports using WC and/or WHR. A systematic review of the literature and collaborative analysis with individual subject data did in fact show that central obesity, as defined on the basis of WC and WHR tertiles, was associated with higher mortality in individuals with either normal or elevated BMI, though the impact of each one alone was significant only for WHR [11]. Moreover, in the Melbourne Collaborative Cohort Study, WC and WHR were stronger predictors of mortality than BMI and fat mass [45], though other studies using measures of fat distribution failed to show a linear relationship between these measures and death [46]. Contrasting data were also found in previous studies in diabetic individuals, as WC and WHR were shown to be either associated [27] or not associated [47] with mortality. However, in our study, the difference between the lowest and intermediate tertile was not significant when using WHtR and tended to be inverted with ABSI. These data are consistent with previous reports showing that either WHtR [27] or ABSI [28] were superior to WC and WHR in predicting mortality. Moreover, the findings that the associations between WC or WHtR and mortality disappeared after adjusting for BMI in females and the relationship between ABSI and mortality was stronger in men than in women are also consistent with previous reports in people with type 2 diabetes [27, 28] and can be due to sex differences in body fat distribution [48].
Our findings have relevant implications for risk stratification and weight management strategies in individuals with type 2 diabetes. First, surrogate measures of central adiposity that normalize WC to height (and BMI) are superior to WC in integrating BMI for outcome prediction, as they separate the influence of the component of body shape measured by WC and reflecting visceral fat distribution from that of body size. Therefore, in routine clinical practice, the calculation of WHtR and especially ABSI from WC is highly recommended for prognostic purposes in people with type 2 diabetes in order to account for the detrimental impact of mild increases in (central) body fat. Second, though a moderate level of subcutaneous fat might confer a survival advantage to individuals getting older or developing potentially fat illnesses, this does not imply that weight loss programs are not indicated in overweight and mildly obese patients with type 2 diabetes, especially if they have excess central fat accumulation. Instead, our data support the need for combined diet and exercise intervention in order to minimize loss of muscle (and bone) mass associated with diet only [49], which may have a detrimental impact on mortality. However, further studies with concurrent assessment of body composition, fat distribution, and physical fitness are needed to dissect the relative contribution of these variables to survival in elderly individuals and patients suffering from chronic disorders and inform effective strategies for disease management.
Strength of our study include the comparison of BMI and three surrogate measures of central adiposity (including both WHtR and ABSI), the large sample size, the assessment of a wide range of clinical parameters, the completeness of baseline and follow-up data. However, this study has several limitations. First, WC and WC-derived measures (WHtR and ABSI) were available only from 4618 individuals, though adjusted death rate and mortality risk were similar to those of participants without these measurements. Second, lack of information about the weight history of the RIACE participants both before and after enrolment may have influenced the results, though the potential impact of reverse causation from unintentional weight loss due to undiagnosed or diagnosed illnesses was reduced by excluding patients with comorbidities and deceased during the first two years of follow-up. Third, relevant confounders such as body composition and physical fitness were not assessed, and PA level, which might be considered a surrogate measure of these parameters, was self-reported. Fourth, the study findings may not be applicable to the general ambulatory diabetes population, as only part of the individuals with type 2 diabetes attend Diabetes Clinics in Italy; however, the RIACE cohort is representative of patients followed by diabetes specialists in these clinics [50]. Finally, the observational design makes causal interpretation impossible.
Conclusions
In patients with type 2 diabetes from the RIACE cohort, the lowest mortality risk was in the overweight BMI range. This overweight paradox could not be explained by confounders such as age, smoking, and comorbidities, but it could be attributed, at least partly, to confounding from PA level, likely through its impact on lean (muscle) mass and cardiorespiratory fitness, in addition to a possible survival advantage from a moderate excess of peripheral fat.
Intermediate values of WC were associated with a lower risk of death compared to low values, but a protective effect of moderate central fat accumulation was not confirmed by using WHtR and especially ABSI (at least in men) as surrogate measures of adiposity, which better reflected mortality risk associated with central adiposity and, therefore, should be routinely assessed in people with type 2 diabetes for prognostic purposes.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- DKD:
-
Diabetic kidney disease
- DR:
-
Diabetic retinopathy
- eGFR:
-
Estimated glomerular filtration rate
- HbA1c :
-
Haemoglobin A1c
- PA:
-
Physical activity
- RIACE:
-
Renal Insufficiency And Cardiovascular Events
- WHtR:
-
Waist-to-height ratio
- WC:
-
Waist circumference
- WHR:
-
Waist-to-hip ratio
References
Global BMI Mortality Collaboration, Di Angelantonio E, Bhupathiraju ShN, Wormser D, Gao P, Kaptoge S, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388:776–86.
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–105.
Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 146 million white adults. N Engl J Med. 2010;363:2211–9.
Hughes V. The big fat truth. Nature. 2013;497:428–30.
Lavie CJ, Carbone S, Kachur S, O’Keefe EL, Elagizi A. Effects of physical activity, exercise, and fitness on obesity-related morbidity and mortality. Curr Sports Med Rep. 2019;18:292–8.
Flegal KM, Graubard BI, Williamson DF, Cooper RS. Reverse causation and illness-related weight loss in observational studies of body weight and mortality. Am J Epidemiol. 2011;173:1–9.
Bosello O, Vanzo A. Obesity paradox and aging. Eat Weight Disord. 2021;26:27–35.
Stokes A, Preston SH. Smoking and reverse causation create an obesity paradox in cardiovascular disease. Obesity. 2015;23:2485–90.
Ahima RS, Lazar MA. Physiology. The health risk of obesity–better metrics imperative. Science. 2013;341:856–8.
Bender R, Jöckel KH, Trautner C, Spraul M, Berger M. Effect of age on excess mortality in obesity. JAMA. 1999;281:1498–504.
Coutinho T, Goel K, Corrêa de Sá D, Kragelund C, Kanaya AM, Zeller M, et al. Central obesity and survival in subjects with coronary artery disease: a systematic review of the literature and collaborative analysis with individual subject data. J Am Coll Cardiol. 2011;57:1877–86.
Schneider HJ, Friedrich N, Klotsche J, Pieper L, Nauck M, John U, et al. The predictive value of different measures of obesity for incident cardiovascular events and mortality. J Clin Endocrinol Metab. 2010;95:1777–85.
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE. 2012;7: e39504.
Carnethon MR, De Chavez PJ, Biggs ML, Lewis CE, Pankow JS, Bertoni AG, et al. Association of weight status with mortality in adults with incident diabetes. JAMA. 2012;308:581–90.
Zaccardi F, Dhalwani NN, Papamargaritis D, Webb DR, Murphy GJ, Davies MJ, et al. Nonlinear association of BMI with all-cause and cardiovascular mortality in type 2 diabetes mellitus: a systematic review and meta-analysis of 414,587 participants in prospective studies. Diabetologia. 2017;60:240–8.
Wang Z, Dong B, Hu J, Adegbija O, Arnold LW. Exploring the non-linear association between BMI and mortality in adults with and without diabetes: the US National Health Interview Survey. Diabet Med. 2016;33:1691–9.
Mulnier HE, Seaman HE, Raleigh VS, Soedamah-Muthu SS, Colhoun HM, et al. Mortality in people with type 2 diabetes in the UK. Diabet Med. 2006;23:516–21.
Logue J, Walker JJ, Leese G, Lindsay R, McKnight J, Morris A, et al. Association between BMI measured within a year after diagnosis of type 2 diabetes and mortality. Diabetes Care. 2013;36:887–93.
Costanzo P, Cleland JG, Pellicori P, Clark AL, Hepburn D, Kilpatrick ES, et al. The obesity paradox in type 2 diabetes mellitus: relationship of body mass index to prognosis: a cohort study. Ann Intern Med. 2015;162:610–8.
Kokkinos P, Myers J, Faselis C, Doumas M, Kheirbek R, Nylen E. BMI-mortality paradox and fitness in African American and Caucasian men with type 2 diabetes. Diabetes Care. 2012;35:1021–7.
Jackson CL, Yeh HC, Szklo M, Hu FB, Wang NY, Dray-Spira R, et al. Body-Mass Index and all-cause mortality in US adults with and without diabetes. J Gen Intern Med. 2014;29:25–33.
Thomas G, Khunti K, Curcin V, Molokhia M, Millett C, Majeed A, et al. Obesity paradox in people newly diagnosed with type 2 diabetes with and without prior cardiovascular disease. Diabetes Obes Metab. 2014;16:317–25.
Zhao W, Katzmarzyk PT, Horswell R, Wang Y, Li W, Johnson J, et al. Body mass index and the risk of all-cause mortality among patients with type 2 diabetes mellitus. Circulation. 2014;130:2143–51.
Liu XM, Liu YJ, Zhan J, He QQ. Overweight, obesity and risk of all-cause and cardiovascular mortality in patients with type 2 diabetes mellitus: a dose-response meta-analysis of prospective cohort studies. Eur J Epidemiol. 2015;30:35–45.
Carnethon MR, Rasmussen-Torvik LJ, Palaniappan L. The obesity paradox in diabetes. Curr Cardiol Rep. 2014;16:446.
Gravina G, Ferrari F, Nebbiai G. The obesity paradox and diabetes. Eat Weight Disord. 2021;26:1057–68.
Sluik D, Boeing H, Montonen J, Pischon T, Kaaks R, Teucher B, et al. Associations between general and abdominal adiposity and mortality in individuals with diabetes mellitus. Am J Epidemiol. 2011;174:22–34.
Tate J, Knuiman M, Davis WA, Davis TME, Bruce DG. A comparison of obesity indices in relation to mortality in type 2 diabetes: the Fremantle Diabetes Study. Diabetologia. 2020;63:528–36.
Penno G, Solini A, Bonora E, Fondelli C, Orsi E, Zerbini G, et al. Clinical significance of nonalbuminuric renal impairment in type 2 diabetes. J Hypertens. 2011;29:1802–9.
Orsi E, Solini A, Bonora E, Fondelli C, Trevisan R, Vedovato M, et al. Haemoglobin A1c variability is a strong, independent predictor of all-cause mortality in patients with type 2 diabetes. Diabetes Obes Metab. 2018;20:1885–93.
Penno G, Solini A, Orsi E, Bonora E, Fondelli C, Trevisan R, et al. Non-albuminuric renal impairment is a strong predictor of mortality in individuals with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicentre study. Diabetologia. 2018;61:2277–89.
Penno G, Solini A, Zoppini G, Orsi E, Zerbini G, Trevisan R, et al. Rate and determinants of association between advanced retinopathy and chronic kidney disease in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicenter study. Diabetes Care. 2012;35:2317–23.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82.
Zoppini G, Verlato G, Leuzinger C, Zamboni C, Brun E, Bonora E, et al. Body mass index and the risk of mortality in type II diabetic patients from Verona. Int J Obes Relat Metab Disord. 2003;27:281–5.
Badrick E, Sperrin M, Buchan IE, Renehan AG. Obesity paradox and mortality in adults with and without incident type 2 diabetes: a matched population-level cohort study. BMJ Open Diabetes Res Care. 2017;5(1): e000369. https://doi.org/10.1136/bmjdrc-2016-000369.
Tobias DK, Pan A, Jackson CL, O’Reilly EJ, Ding EL, Willett WC, Manson JE, Hu FB. Body-mass index and mortality among adults with incident type 2 diabetes. N Engl J Med. 2014;370(3):233–44. https://doi.org/10.1056/NEJMoa1304501 (Erratum in: N Engl J Med. 2014 Apr 3;370(14):1368).
McAuley PA, Artero EG, Sui X, Lee DC, Church TS, Lavie CJ, et al. The obesity paradox, cardiorespiratory fitness, and coronary heart disease. Mayo Clin Proc. 2012;87:443–51.
McAuley PA, Beavers KM. Contribution of cardiorespiratory fitness to the obesity paradox. Prog Cardiovasc Dis. 2014;56:434–40.
Fogelholm M. Physical activity, fitness and fatness: relations to mortality, morbidity and disease risk factors. A systematic review. Obes Rev. 2010;11:202–21.
Lee DH, Keum N, Hu FB, Orav EJ, Rimm EB, Willett WC, et al. Predicted lean body mass, fat mass, and all cause and cause specific mortality in men: prospective US cohort study. BMJ. 2018;362: k2575.
Oreopoulos A, Ezekowitz JA, McAlister FA, Kalantar-Zadeh K, Fonarow GC, Norris CM, et al. Association between direct measures of body composition and prognostic factors in chronic heart failure. Mayo Clin Proc. 2010;85:609–17.
Gonzalez MC, Pastore CA, Orlandi SP, Heymsfield SB. Obesity paradox in cancer: new insights provided by body composition. Am J Clin Nutr. 2014;99:999–1005.
Lavie CJ, De Schutter A, Patel DA, Romero-Corral A, Artham SM, Milani RV. Body composition and survival in stable coronary heart disease: impact of lean mass index and body fat in the “obesity paradox.” J Am Coll Cardiol. 2012;60:1374–80.
Caan BJ, Cespedes Feliciano EM, Kroenke CH. The importance of body composition in explaining the overweight paradox in cancer-counterpoint. Cancer Res. 2018;78:1906–12.
Simpson JA, MacInnis RJ, Peeters A, Hopper JL, Giles GG, English DR. A comparison of adiposity measures as predictors of all-cause mortality: the Melbourne Collaborative Cohort Study. Obesity. 2007;15:994–1003.
Prado CM, Gonzalez MC, Heymsfield SB. Body composition phenotypes and obesity paradox. Curr Opin Clin Nutr Metab Care. 2015;18:535–51.
Kahn HS, Bullard KM, Barker LE, Imperatore G. Differences between adiposity indicators for predicting all-cause mortality in a representative sample of United States non-elderly adults. PLoS ONE. 2012;7: e50428.
Stevens J, Katz EG, Huxley RR. Associations between gender, age and waist circumference. Eur J Clin Nutr. 2010;64:6–15.
Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364:1218–29.
De Cosmo S, Rossi MC, Pellegrini F, Lucisano G, Bacci S, Gentile S, et al. Kidney dysfunction and related cardiovascular risk factors among patients with type 2 diabetes. Nephrol Dial Transplant. 2014;29:657–62.
Acknowledgements
The Authors thank the RIACE Investigators for participating in this study (see the complete list in the Additional file 1: The RIACE Study Group).
Funding
This research was supported by the Research Foundation of the Italian Diabetes Society (Diabete Ricerca) and the Diabetes, Endocrinology and Metabolism (DEM) Foundation, and by unconditional grants from Eli-Lilly, Sigma-Tau, Takeda, Chiesi Farmaceutici, and Boehringer-Ingelheim. The funding sources had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
EO, AS, GPe, and GPu conceived and designed the study. All authors contributed to data acquisition, analysis, or interpretation. GPu drafted the article and had full access to all the data and took responsibility for the integrity of data and accuracy of the data analysis in this study. EO, AS, GPe, EB, CF, RT, MV, FC, OL, JH, and AN revised the manuscript critically for essential intellectual content. All authors approved the submitted version of the manuscript and agreed to be personally accountable for the individual’s own contributions and to ensure that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. The research protocol was approved by the ethics committee of the coordinating centre (Sant’Andrea Hospital, Rome, Italy) on 25 September 2006 (number 43/2006) and subsequently by the ethics committee of each participating centre. Participants provided an informed consent.
Consent for publication
Not applicable.
Competing interests
EO: consultant fees from Eli Lilly and Novo Nordisk, and lecture fees from Astellas. AS: consultant fees from Axxam, Bayer, and Novo Nordisk, and lecture fees from Eli Lilly, Novo Nordisk, and Sanofi-Aventis. Giuseppe Penno: consultant fees from Bayer and Eli Lilly, and lecture fees from AstraZeneca, Boerhinger Ingelheim, Eli-Lilly, Merck Sharp & Dohme, Mundipharma, Novo Nordisk, and Takeda. EB: consultant fees from Abbott, Bayer, Becton Dickinson, Boehringer Ingelheim, Daiichi-Sankyo, Eli Lilly, and Novo Nordisk. CF: lecture fees from Abbot, Boehringer Ingelheim, Daiichi Sankyo, Eli Lilly, Merck Sharp & Dohme, Mundipharma, and Theras Lifetech. RT: consultant fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Merck Sharp & Dohme, Novo Nordisk, and Sanofi-Aventis, and lecture fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, and Novo Nordisk. MV: lecture fees from Lifescan and Novo Nordisk. FC: consultant fees from Boehringer Ingelheim, and lecture fees from AstraZeneca. OL: lecture fees from Eli-Lilly, and grant support from Merck Serono and Merck Sharp & Dohme. JH: lecture fees from Boehringer Ingelheim. AN: consultant fees from AstraZeneca, lecture fees from Eli Lilly, Medtronic, and Novo Nordisk, and grant support from AlfaSigma, Novo Nordisk, Pikdare, Sanofi, Shionogi, SOBI, and Theras. GP: consultant fees from Abbot, Bayer, and Novo Nordisk, and lecture fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, and Novo Nordisk. No other disclosures were reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The RIACE Study Group.
Additional file 2: Table S1.
Baseline clinical features of study participants by BMI categories.
Additional file 3: Figure S1.
Survival analysis by age categories.
Additional file 4: Figure S2.
Survival analysis after sequential patients’ exclusion.
Additional file 5: Table S2.
Survival analysis by BMI categories according to sex.
Additional file 6: Table S3.
Baseline clinical features of study participants as a whole and by availability of WC measurements.
Additional file 7: Table S4.
Univariate correlations of surrogate measures of central adiposity between each other and with BMI by Pearson correlation coefficient.
Additional file 8: Table S5.
Baseline clinical features of study participants by WC, WHtR, and ABSI tertiles.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Orsi, E., Solini, A., Penno, G. et al. Body mass index versus surrogate measures of central adiposity as independent predictors of mortality in type 2 diabetes. Cardiovasc Diabetol 21, 266 (2022). https://doi.org/10.1186/s12933-022-01706-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-022-01706-2