Abstract
Background
The influence of diabetes on the mortality and risk of implantable cardioverter defibrillator (ICD) therapies is still controversial, and a comprehensive assessment is lacking. We performed this systematic review and meta-analysis to address this controversy.
Methods
We systematically searched the PubMed, Embase, Web of Science and Cochrane Library databases to collect relevant literature. Fixed and random effects models were used to estimate the hazard ratio (HR) with 95% CIs.
Results
Thirty-six articles reporting on 162,780 ICD recipients were included in this analysis. Compared with nondiabetic ICD recipients, diabetic ICD recipients had higher all-cause mortality (HR = 1.45, 95% CI 1.36–1.55). The subgroup analysis showed that secondary prevention patients with diabetes may suffer a higher risk of all-cause mortality (HR = 1.89, 95% CI 1.56–2.28) (for subgroup analysis, P = 0.03). Cardiac mortality was also higher in ICD recipients with diabetes (HR = 1.68, 95% CI 1.35–2.08). However, diabetes had no significant effect on the risks of ICD therapies, including appropriate or inappropriate therapy, appropriate or inappropriate shock and appropriate anti-tachycardia pacing (ATP). Diabetes was associated with a decreased risk of inappropriate ATP (HR = 0.56, 95% CI 0.39–0.79).
Conclusion
Diabetes is associated with an increased risk of mortality in ICD recipients, especially in the secondary prevention patients, but does not significantly influence the risks of ICD therapies, indicating that the increased mortality of ICD recipients with diabetes may not be caused by arrhythmias. The survival benefits of ICD treatment in diabetes patients are limited.
Similar content being viewed by others
Introduction
According to the latest data released by the International Diabetes Federation, the number of adult diabetic patients worldwide reached 537 million in 2021, and approximately 6.7 million people died of diabetes or diabetic complications, accounting for 12.2% of all-cause mortality [1]. Patients with diabetes have a higher risk of cardiovascular disease and mortality [2]. Heart failure (HF) is an end-stage clinical manifestation of organic heart disease and has become a major public health problem worldwide.
The prevalence of diabetes is 24% in chronic HF patients and up to 40% in hospitalized HF patients. Studies have shown that diabetes is an independent predictor of sudden cardiac death (SCD) in patients with HF and is associated with an increased risk of mortality [3, 4]. For example, in postinfarction patients, the mortality in the diabetic group was higher than that in the nondiabetic group [5]. It has been proven that implantable cardioverter defibrillator (ICD) can effectively prevent SCD and terminate malignant arrhythmias such as persistent ventricular tachycardia and ventricular fibrillation. Because of this unique property, ICD has been recommended as a class I recommendation to prevent SCD in patients with ischemic and nonischemic HF in current guideline [6]. Since diabetes generates a higher risk of SCD in HF patients, ICD implantation would be expected to have additional survival benefits.
To date, the influence of diabetes on the mortality and risk of ICD therapy is still controversial, and a comprehensive assessment is lacking. We performed this systematic review and meta-analysis to address this controversy.
Methods
This article was prepared according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [7].
Search strategy
The meta-analysis was conducted according to the PRISMA guidelines. Two authors (H.-L.L and W.Z.) systematically searched the PubMed, Embase and Cochrane Library from through February 28, 2022 for relevant articles published in English. The search strategy was as follows: [(Diabetes Mellitus) OR (Diabetes)] AND (“Defibrillators, Implantable” OR “Implantable Defibrillators” OR “Implantable Defibrillator” OR “Cardioverter-Defibrillators, Implantable” OR “Implantable Cardioverter-Defibrillator” OR “Implantable Cardioverter Defibrillators” OR “Defibrillator, Implantable”). Endnote X8 was used to manage the articles. The articles were independently selected by two authors (H.-L.L and J.-Z.H). After the title and abstract were reviewed and the off-topic articles were excluded, the full text of the remaining articles was screened against the inclusion criteria. Disagreements were resolved by discussion.
Selection criteria
The studies were included if (1) the articles were published in English with available full texts; (2) the studies reported the mortality or risk of ICD therapy and (3) the studies provided the hazard ratio (HR), odds ratio (OR) or risk ratio (RR) as well as their corresponding 95% confidence intervals (CIs).
We excluded studies if (1) the articles were of certain types, such as reviews, meta-analyses, notes, and case reports; (2) the studies contained overlapping study populations or (3) the full text could not be found.
Data extraction and quality assessment
Two reviewers (H.-L.L and W.Z.) independently extracted data from the included studies using a standard data extraction process. The following information was extracted from the articles: author’s name, publication year, study design, region of study, time frame, sample size, follow-up duration, age, sex ratio, region, time frame, left ventricular ejection fraction (LVEF), QRS duration, primary disease, prevention types, device implantation and outcomes.
The quality of the included studies was assessed independently by two reviewers (H.-L.L and J.-Z.H) using the Newcastle–Ottawa Scale (NOS). Each study was scored independently based on selection, comparability and outcome. We considered the article to be of high quality if it had a NOS score greater than 6. Disagreements were resolved by consensus.
Outcomes and subgroups
The primary outcome was mortality in diabetic and nondiabetic ICD recipients, which was divided into all-cause mortality and cardiac mortality. A subgroup analysis of all-cause mortality was further performed by separating patients into ICD recipients for primary prevention, ICD recipients for secondary prevention and ICD recipients for primary or secondary prevention. The secondary outcome was the risk of ICD therapies in diabetic and nondiabetic ICD recipients, which was divided into appropriate therapy, inappropriate therapy, appropriate shock, inappropriate shock, appropriate anti-tachycardia pacing (ATP) and inappropriate ATP.
Statistical analysis
Review Manager 5.3 (Cochrane Collaboration, Copenhagen, Denmark) was used to perform the meta-analysis. A sensitivity analysis was conducted to test the effect of individual studies using STATA version 12 (Stata Corporation, College Station, TX, USA). The natural logarithm of the hazard ratios (HRs) and its standard error (SElog HRs) were calculated. Heterogeneity was evaluated using chi-squared and I-squared tests. We considered there was substantial heterogeneity when I2 > 50%, and the random-effects model was used, otherwise, the fixed-effects model was used. Funnel plots as well as Begg and Egger test were drawn to evaluate the publication bias risk.
Results
Study selection and study characteristics
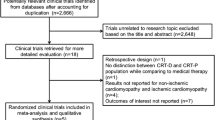
We identified 1100 articles through electronic retrieval strategies. Of these, 255 were duplicates, and 703 were excluded because the articles did not meet the inclusion criteria. Of 142 articles screened for eligibility, 57 studies were unwanted publication types, 41 articles were off-topic, 6 studies had overlapping study populations, and 2 studies were not published in English. Finally, 36 studies [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43] of 162,780 ICD recipients were included in the meta-analysis. The flow diagram of the literature inclusion process is shown in Fig. 1. Table 1 provides the main characteristics of the included studies, in addition to the regular index, including sample size, follow-up duration, region, time frame, age, sex ratio, LVEF, QRS duration, primary disease, device implantation, prevention types and outcomes. The quality of the included studies was assessed using the NOS, with an average NOS score of 7.55; the details of the quality assessment are shown in Table 2.
Increased mortality in ICD recipients with diabetes
In the included studies, 33 studies of 159,290 ICD recipients reported data for the association between diabetes and risk of all-cause mortality. A random effects model was used due to the existence of heterogeneity (I2 = 72%, P = 0.001), and the results showed that diabetes was associated with an increased risk of all-cause mortality in ICD recipients (HR = 1.45, 95% CI 1.36–1.55) (Fig. 2A). Data in 4 studies [10, 14, 29, 31] were available for cardiac mortality. The pooled data found an increased risk of cardiac mortality in ICD recipients with diabetes (HR = 1.68, 95% CI 1.35–2.08, I2 = 0%), shown in Fig. 2B. For the all-cause mortality outcome, funnel plots showed no significant publication bias (Additional file 1: Fig. S1). Furthermore, Begg and Egger tests also suggested no publication bias (all P > 0.1). Sensitivity analysis confirmed that the results did not change after removing individual studies (Additional file 1: Fig. S2).
Subgroup analysis of prevention types
We performed a subgroup analysis of prevention type by separating the ICD recipients into 3 groups: ICD recipients with primary prevention, with secondary prevention and with primary or secondary prevention. Figure 3 shows that diabetes was associated with an increased risk of all-cause mortality in all 3 groups. The increase of all-cause mortality varied between the above groups (for subgroup analysis, P = 0.03), and that secondary prevention patients with diabetes may suffer a higher risk of all-cause mortality (HR = 1.89, 95% CI 1.56–2.28).
No significant effect on ICD therapy, shock and appropriate ATP, but a decreased risk of inappropriate ATP
In the 36 included articles, 5 studies [31,32,33,34, 39] reported appropriate therapy, 3 studies [31, 33, 39] reported inappropriate therapy, 5 studies [15, 24, 33, 36, 39] reported appropriate shock, 2 studies [33, 39] reported inappropriate shock, ATP and inappropriate ATP. Forest plots showed that diabetes had nonsignificant relationship with the risk of appropriate therapy (HR = 1.10, 95% CI 0.93–1.31, I2 = 53%) (Fig. 4A), inappropriate therapy (HR = 0.79, 95% CI 0.45—1.39, I2 = 67%) (Fig. 4B), appropriate shock (HR = 0.95, 95% CI 0.70–1.29, I2 = 69%) (Fig. 4C) and inappropriate shock (HR = 1.04, 95% CI 0.69–1.56, I2 = 0%) (Fig. 4D) in ICD recipients. Meanwhile, no statistically significant difference was found between diabetes and the risk of ATP (HR = 1.36, 95% CI 0.97–1.91, I2 = 51%) (Fig. 4E) in ICD recipients. However, Fig. 4F shows that diabetes was associated with a decreased risk of inappropriate ATP (HR = 0.56, 95% CI 0.39–0.79, I2 = 0%).
Discussion
The present study systematically and comprehensively reviewed the current available literature, including 36 publications with 162,780 ICD recipients, to assess the potential influence of diabetes on the mortality and risk of ICD therapy. Not as we expected, the meta-analysis indicated that in ICD recipients, diabetes was associated with an increased risk of both all-cause mortality and cardiac mortality, and secondary prevention patients with diabetes may suffer a higher risk of all-cause mortality. Another important discovery was that there were no nonsignificant differences in the proportion of ICD therapies (appropriate therapy, inappropriate therapy, appropriate shock, inappropriate shock and appropriate ATP) between diabetes patients and non-diabetes patients. However, diabetes was associated with a reduced risk of inappropriate ATP. To the best of our knowledge, this study is the first systematic review and meta-analysis to comprehensively assess the cumulative evidence of diabetes associated with mortality and the risk of ICD therapy in ICD recipients. Although there were no randomized controlled trials due to the particularity of the study design, according to the quality evaluation of the NOS, all of the included studies were of high quality. Sensitivity analysis also showed that the results were not affected by any individual studies. The above factors show the robustness of the results.
There is a high proportion of diabetes in HF patients, especially in hospitalized HF patients, and diabetes has been found to be an independent predictor of SCD in HF patients [3, 4]. On the other hand, ICD is an effective method of SCD prevention in patients with HF [6]. Based on the above theory, it can be deduced that diabetes ICD recipients with HF should receive more survival benefits than nondiabetic recipients. However, our pooled results showed that in ICD recipients, diabetes also significantly increased the risk of all-cause mortality and cardiac mortality, especially for patients with ICD implantation for secondary prevention. This result indicates that even with ICD implantation, diabetic patients still have a higher mortality than nondiabetic patients of all-cause or the cardiac mortality, which is consistent with other studies [8, 38, 39]. How to explain the increased mortality of diabetic ICD recipients is a key question. Our following work regarding whether diabetic patients have the higher risk of ICD therapies is very important to address this question, because both inappropriate and appropriate ICD therapies are associated with an increased risk of subsequent death [44,45,46].
ICD therapies mainly include shock and ATP. Several previous studies showed different results regarding whether diabetes increases the risk of ICD therapies. Steiner et al. showed that diabetes was not associated with an increased risk of appropriate or inappropriate ICD therapies [31, 32, 39]. However, Ruwald et al. found that patients with diabetes had a 58% increased risk of appropriate therapy and a 46% decreased risk of inappropriate therapy [33] For ICD shock and ATP, the conclusions are also not consistent [15, 24, 33, 39]. Our cumulative meta-analysis showed that diabetes ICD recipients do not have a higher risk of ICD therapies, including appropriate therapy, inappropriate therapy, appropriate shock, inappropriate shock and appropriate ATP, than nondiabetic ICD recipients. This means that the higher mortality in diabetic ICD recipients is not caused by ventricular arrhythmias or ICD therapies. Therefore, a possible reason for the increased mortality in diabetes recipients may be the comorbidities related to diabetes, independent of the effects of ICD therapy [24]. Our study found that diabetes was associated with a reduced risk of inappropriate ATP. The underlying mechanism for this phenomenon is not clear, and the possible reasons are that diabetic patients are less likely to experience exercise-induced sinus tachycardia due to reduced activity, and their cardiovascular reflexes are reduced due to autonomic nervous dysfunction and neuropathy [33].
Our results show that diabetes is significantly associated with an increased risk of mortality in ICD recipients. On the other hand, diabetes has no effect on the risk of ICD therapies. This suggests that the increased risk of mortality caused by diabetes in ICD recipients may be due to adverse pathophysiological changes and related complications caused by diabetes itself rather than arrhythmias.
Our results showed that the all-cause mortality of secondary prevention patients with diabetes was higher than diabetic primary prevention patients. A study suggested that secondary prevention patients have a higher risk of death than primary prevention patients [47], which is consistent with our finding. The results indicated that secondary prevention patients may have a vulnerable myocardium resulting from more risk factors, therefore, the vulnerable myocardium may be more likely to be damaged by diabetic complications, resulting in a higher risk of mortality. In addition, the survival benefits of ICD treatment for diabetes recipients are limited. ICD is effective in treating ventricular tachyarrhythmias; however, HF patients with diabetes may be at increased risk of mortality through mechanisms other than arrhythmias that can be treated by ICD. Our results also suggest that for these diabetes ICD recipients, more aggressive treatment should be applied to treat the adverse pathophysiological changes and complications caused by diabetes, rather than just focusing on the treatment of arrhythmias. For example, many anti-diabetic medications have been shown to improve the prognosis of diabetic patients with HF. For example, dapagliflozin, a sodium–glucose cotransporter 2 inhibitor, can significantly reduce cardiac and all-cause mortality in diabetic patients with HF [48]. Real-world studies have shown that metformin also significantly reduces mortality in diabetic patients with HF [49].
Our research has several advantages. First, to the best of our knowledge, this is the first systematic review and meta-analysis to comprehensively assess the cumulative evidence of diabetes associated with mortality and the risk of ICD therapy in ICD recipients. Second, we strictly followed the PRISMA guidelines to carry out this study. Third, all of the included studies were of high quality, and sensitivity analysis also showed the robustness of the results. Finally, such a large sample (36 studies containing 162,780 patients) can ensure the reliability of the study results. However, several limitations should be considered. First, due to the particularity of the study design, no randomized controlled trials were included. Second, there was relatively high heterogeneity among the included articles, such as in the outcomes of all-cause mortality, appropriate and inappropriate therapy, appropriate shock and ATP, which may mainly due to the individual characteristics of each included studies. Hence, we tried several ways to reduce the impact of heterogeneity on the results, including using random effects models, performing sensitivity analysis and subgroup analysis. Third, although most of the included studies adjusted for a range of confounding variables, we could not rule out an effect of residual confounding variables on the results, which may also account for the heterogeneity existence in the outcomes above.
Conclusions
In summary, our study shows that diabetes is associated with an increased risk of mortality in ICD recipients, especially in the secondary prevention patients, but diabetes has no significant effect on the risks of ICD therapies. These results indicate that the increased mortality of ICD recipients with diabetes may not be caused by arrhythmias. The survival benefits of ICD treatment for diabetic ICD recipients are limited, and more aggressive treatment should be sought to reduce mortality.
Availability of data and materials
None.
Abbreviations
- ICD:
-
Implantable cardioverter-defibrillator
- HRs:
-
Hazard ratios
- CIs:
-
Confidence intervals
- HF:
-
Heart failure
- SCD:
-
Sudden cardiac death
- ATP:
-
Anti-tachycardia pacing
- LVEF:
-
Left ventricular ejection fractions
- NOS:
-
Newcastle–Ottawa Scale
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- NYHA:
-
New York Heart Association
- RevMan:
-
Review Manager
References
International Diabetes Federation. IDF diabetes atlas. 10th ed. Brussels: International Diabetes Federation; 2021.
Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Emerging Risk Factors C, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215–22.
Dei Cas A, Khan SS, Butler J, Mentz RJ, Bonow RO, Avogaro A, Tschoepe D, Doehner W, Greene SJ, Senni M, et al. Impact of diabetes on epidemiology, treatment, and outcomes of patients with heart failure. JACC Heart Failure. 2015;3(2):136–45.
MacDonald MR, Petrie MC, Varyani F, Ostergren J, Michelson EL, Young JB, Solomon SD, Granger CB, Swedberg K, Yusuf S, et al. Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: an analysis of the candesartan in heart failure: assessment of reduction in mortality and morbidity (CHARM) programme. Eur Heart J. 2008;29(11):1377–85.
Junttila MJ, Barthel P, Myerburg RJ, Makikallio TH, Bauer A, Ulm K, Kiviniemi A, Tulppo M, Perkiomaki JS, Schmidt G, et al. Sudden cardiac death after myocardial infarction in patients with type 2 diabetes. Heart Rhythm. 2010;7(10):1396–403.
Kusumoto FM, Bailey KR, Chaouki AS, Deshmukh AJ, Gautam S, Kim RJ, Kramer DB, Lambrakos LK, Nasser NH, Sorajja D. Systematic review for the 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2018;138(13):e392–414.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7): e1000097.
Bilchick KC, Stukenborg GJ, Kamath S, Cheng A. Prediction of mortality in clinical practice for medicare patients undergoing defibrillator implantation for primary prevention of sudden cardiac death. J Am Coll Cardiol. 2012;60(17):1647–55.
Borleffs CJ, van Erven L, Schotman M, Boersma E, Kies P, van der Burg AE, Zeppenfeld K, Bootsma M, van der Wall EE, Bax JJ, et al. Recurrence of ventricular arrhythmias in ischaemic secondary prevention implantable cardioverter defibrillator recipients: long-term follow-up of the Leiden out-of-hospital cardiac arrest study (LOHCAT). Eur Heart J. 2009;30(13):1621–6.
Briongos-Figuero S, Estevez A, Perez ML, Martinez-Ferrer JB, Garcia E, Vinolas X, Arenal A, Alzueta J, Munoz-Aguilera R. Prognostic role of NYHA class in heart failure patients undergoing primary prevention ICD therapy. ESC Heart Failure. 2020;7(1):279–83.
Chao TF, Lai CH, Tuan TC, Wu TJ, Huang JL, Chiou CW, Hsiao HC, Lin YJ, Liao JN, Kong CW, et al. Long-term prognosis in recipients of implantable cardioverter-defibrillators for secondary preventions in Taiwan—a multicenter registry study. Acta Cardiol Sin. 2014;30(1):22–8.
Coleman CI, Kluger J, Bhavnani S, Clyne C, Yarlagadda R, Guertin D, White CM. Association between statin use and mortality in patients with implantable cardioverter-defibrillators and left ventricular systolic dysfunction. Heart Rhythm. 2008;5(4):507–10.
Cygankiewicz I, Gillespie J, Zareba W, Brown MW, Goldenberg I, Klein H, McNitt S, Polonsky S, Andrews M, Dwyer EM, et al. Predictors of long-term mortality in multicenter automatic defibrillator implantation trial II (MADIT II) patients with implantable cardioverter-defibrillators. Heart Rhythm. 2009;6(4):468–73.
Denollet J, Tekle FB, Pedersen SS, van der Voort PH, Alings M, van den Broek KC. Prognostic importance of distressed (type D) personality and shocks in patients with an implantable cardioverter defibrillator. Int J Cardiol. 2013;167(6):2705–9.
Desai H, Aronow WS, Tsai FS, Ahn C, Lai HM, Amin H, Gandhi K, Frishman WH, Cohen M, Sorbera C. Statins reduce appropriate cardioverter-defibrillator shocks and mortality in patients with heart failure and combined cardiac resynchronization and implantable cardioverter-defibrillator therapy. J Cardiovasc Pharmacol Ther. 2009;14(3):176–9.
Echouffo-Tcheugui JB, Masoudi FA, Bao H, Spatz ES, Fonarow GC. Diabetes mellitus and outcomes of cardiac resynchronization with implantable cardioverter-defibrillator therapy in older patients with heart failure. Circ Arrhythm Electrophysiol. 2016;9(8): e004132.
Eckart RE, Gula LJ, Reynolds MR, Shry EA, Maisel WH. Mortality following defibrillator implantation in patients with renal insufficiency. J Cardiovasc Electrophysiol. 2006;17(9):940–3.
Exner DV, Pinski SL, Wyse DG, Renfroe EG, Follmann D, Gold M, Beckman KJ, Coromilas J, Lancaster S, Hallstrom AP, et al. Electrical storm presages nonsudden death: the antiarrhythmics versus implantable defibrillators (AVID) trial. Circulation. 2001;103(16):2066–71.
Fumagalli S, Gasparini M, Landolina M, Lunati M, Boriani G, Proclemer A, Santini M, Mangoni L, Padeletti M, Marchionni N, et al. Determinants of all-cause mortality in different age groups in patients with severe systolic left ventricular dysfunction receiving an implantable cardioverter defibrillator (from the Italian ClinicalService Multicenter Observational Project). Am J Cardiol. 2014;113(10):1691–6.
Hager CS, Jain S, Blackwell J, Culp B, Song J, Chiles CD. Effect of renal function on survival after implantable cardioverter defibrillator placement. Am J Cardiol. 2010;106(9):1297–300.
Hess PL, Hellkamp AS, Peterson ED, Sanders GD, Al-Khalidi HR, Curtis LH, Hammill BG, Pun PH, Curtis JP, Anstrom KJ, et al. Survival after primary prevention implantable cardioverter-defibrillator placement among patients with chronic kidney disease. Circ Arrhythm Electrophysiol. 2014;7(5):793–9.
Ho AT, Pai SM, Timothy P, Pai RG. Effect of concomitant antiarrhythmic therapy on survival in patients with implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2005;28(7):647–53.
Jahangir A, Mirza M, Shahreyar M, Mengesha T, Shearer R, Sultan S, Jahangir A, Choudhuri I, Nangia V, Dhala A, et al. Presence of obesity is associated with lower mortality in elderly patients with implantable cardioverter defibrillator. Int J Obes. 2018;42(2):169–74.
Junttila MJ, Pelli A, Kentta TV, Friede T, Willems R, Bergau L, Malik M, Vandenberk B, Vos MA, Schmidt G, et al. Appropriate shocks and mortality in patients with versus without diabetes with prophylactic implantable cardioverter defibrillators. Diabetes Care. 2020;43(1):196–200.
Lee DS, Tu JV, Austin PC, Dorian P, Yee R, Chong A, Alter DA, Laupacis A. Effect of cardiac and noncardiac conditions on survival after defibrillator implantation. J Am Coll Cardiol. 2007;49(25):2408–15.
Lee AY, Kutyifa V, Ruwald MH, McNitt S, Polonsky B, Zareba W, Moss AJ, Ruwald AC. Digoxin therapy and associated clinical outcomes in the MADIT-CRT trial. Heart Rhythm. 2015;12(9):2010–7.
Morani G, Gasparini M, Zanon F, Casali E, Spotti A, Reggiani A, Bertaglia E, Solimene F, Molon G, Accogli M, et al. Cardiac resynchronization therapy-defibrillator improves long-term survival compared with cardiac resynchronization therapy-pacemaker in patients with a class IA indication for cardiac resynchronization therapy: data from the Contak Italian Registry. Europace. 2013;15(9):1273–9.
Morani G, Facchin D, Molon G, Zanotto G, Maines M, Zoppo F, Themistoclakis S, Allocca G, Dametto E, Bertaglia E, et al. Prediction of mortality in patients with implantable defibrillator using CHADS2 score: data from a prospective observational investigation. Am J Cardiovasc Dis. 2018;8(5):48–57.
Perkiomaki JS, Ruwald AC, Kutyifa V, Ruwald MH, McNitt S, Polonsky B, Goldstein RE, Haigney MC, Krone RJ, Zareba W, et al. Risk factors and the effect of cardiac resynchronization therapy on cardiac and non-cardiac mortality in MADIT-CRT. Europace. 2015;17(12):1816–22.
Rogstad TL, Powell AC, Song Y, Cordier T, Price SE, Long JW, Deshmukh UU, Simmons JD. Determinants of outcomes following outpatient placement of implantable cardioverter defibrillators in a medicare advantage population. Clin Cardiol. 2018;41(9):1130–5.
Rorth R, Thune JJ, Nielsen JC, Haarbo J, Videbaek L, Korup E, Signorovitch J, Bruun NE, Eiskjaer H, Hassager C, et al. The effect of implantable cardioverter-defibrillator in patients with diabetes and non-ischaemic systolic heart failure. Europace. 2019;21(8):1203–10.
Winkler A, Jagus-Jamiola A, Uzieblo-Zyczkowska B, Orski Z, Krzyzanowski K, Smalc-Stasiak M, Kiliszek M. Predictors of appropriate interventions and mortality in patients with implantable cardioverter-defibrillators. Pol Arch Intern Med. 2019;129(10):667–72.
Ruwald MH, Zareba W, Jons C, Zhang C, Ruwald AC, Olshansky B, McNitt S, Bloch Thomsen PE, Shoda M, Merkely B, et al. Influence of diabetes mellitus on inappropriate and appropriate implantable cardioverter-defibrillator therapy and mortality in the multicenter automatic defibrillator implantation trial-reduce inappropriate therapy (MADIT-RIT) trial. Circulation. 2013;128(7):694–701.
Ruwald AC, Vinther M, Gislason GH, Johansen JB, Nielsen JC, Petersen HH, Riahi S, Jons C. The impact of co-morbidity burden on appropriate implantable cardioverter defibrillator therapy and all-cause mortality: insight from Danish nationwide clinical registers. Eur J Heart Fail. 2017;19(3):377–86.
Santangelo G, Bursi F, Negroni MS, Gentile D, Provenzale G, Turriziani L, Zambelli DL, Fiorista L, Bacchioni G, Massironi L, et al. Arrhythmic event prediction in patients with heart failure and reduced ejection fraction. J Cardiovasc Med. 2021;22(2):110–7.
Seegers J, Conen D, Jung K, Bergau L, Dorenkamp M, Luthje L, Sohns C, Sossalla ST, Fischer TH, Hasenfuss G, et al. Sex difference in appropriate shocks but not mortality during long-term follow-up in patients with implantable cardioverter-defibrillators. Europace. 2016;18(8):1194–202.
Sjoblom J, Borgquist R, Gadler F, Kalm T, Ljung L, Rosenqvist M, Frykman V, Platonov PG. Clinical risk profile score predicts all cause mortality but not implantable cardioverter defibrillator intervention rate in a large unselected cohort of patients with congestive heart failure. Ann Noninvasive Electrocardiol. 2017;22(3): e12414.
Stein KM, Mittal S, Gilliam FR, Gilligan DM, Zhong Q, Kraus SM, Meyer TE. Predictors of early mortality in implantable cardioverter-defibrillator recipients. Europace. 2009;11(6):734–40.
Steiner H, Geist M, Goldenberg I, Suleiman M, Glikson M, Tenenbaum A, Swissa M, Fisman EZ, Golovchiner G, Strasberg B, et al. Characteristics and outcomes of diabetic patients with an implantable cardioverter defibrillator in a real world setting: results from the Israeli ICD registry. Cardiovasc Diabetol. 2016;15(1):160.
Vandenberk B, Garweg C, Voros G, Flore V, Marynissen T, Sticherling C, Zabel M, Ector J, Willems R. Changes in implantation patterns and therapy rates of implantable cardioverter defibrillators over time in ischemic and dilated cardiomyopathy patients. Pacing Clin Electrophysiol. 2016;39(8):848–57.
Wasiak M, Tajstra M, Pyka L, Gasior M. Long-term clinical outcomes after placement of an implantable cardioverter-defibrillator: does the etiology of heart failure matter? Kardiol Pol. 2020;78(4):318–24.
Wilson DG, Zeljko HM, Leventopoulos G, Nauman A, Sylvester GE, Yue A, Roberts PR, Thomas G, Duncan ER, Roderick PJ, et al. Increasing age does not affect time to appropriate therapy in primary prevention ICD/CRT-D: a competing risks analysis. Europace. 2017;19(2):275–81.
Zhang Y, Guallar E, Blasco-Colmenares E, Dalal D, Butcher B, Norgard S, Tjong FV, Eldadah Z, Dickfeld T, Ellenbogen KA, et al. Clinical and serum-based markers are associated with death within 1 year of de novo implant in primary prevention ICD recipients. Heart Rhythm. 2015;12(2):360–6.
Saxon LA, Bristow MR, Boehmer J, Krueger S, Kass DA, De Marco T, Carson P, DiCarlo L, Feldman AM, Galle E, et al. Predictors of sudden cardiac death and appropriate shock in the comparison of medical therapy, pacing, and defibrillation in heart failure (COMPANION) trial. Circulation. 2006;114(25):2766–72.
Desai H, Aronow WS, Ahn C, Gandhi K, Hussain S, Lai HM, Sharma M, Frishman WH, Cohen M, Sorbera C. Risk factors for appropriate cardioverter-defibrillator shocks, inappropriate cardioverter-defibrillator shocks, and time to mortality in 549 patients with heart failure. Am J Cardiol. 2010;105(9):1336–8.
Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, Reddy RK, Marchlinski FE, Yee R, Guarnieri T, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008;359(10):1009–17.
Saxon LA, Hayes DL, Gilliam FR, Heidenreich PA, Day J, Seth M, Meyer TE, Jones PW, Boehmer JP. Long-term outcome after ICD and CRT implantation and influence of remote device follow-up: the ALTITUDE survival study. Circulation. 2010;122(23):2359–67.
Kato ET, Silverman MG, Mosenzon O, Zelniker TA, Cahn A, Furtado RHM, Kuder J, Murphy SA, Bhatt DL, Leiter LA, et al. Effect of dapagliflozin on heart failure and mortality in type 2 diabetes mellitus. Circulation. 2019;139(22):2528–36.
Eurich DT, Weir DL, Majumdar SR, Tsuyuki RT, Johnson JA, Tjosvold L, Vanderloo SE, McAlister FA. Comparative safety and effectiveness of metformin in patients with diabetes mellitus and heart failure: systematic review of observational studies involving 34,000 patients. Circ Heart Fail. 2013;6(3):395–402.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
HLL, JZH and WZ to the acquisition of data, analysis and interpretation of data, and drafting of the article. RW contributed to interpretation of data. KH contributed to the conception and design of the study, analysis and interpretation of data, and revising the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Funnel plot of the outcome (all-cause mortality). Figure S2. Sensitivity of the outcome (all-cause mortality).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, H., Hu, J., Zhuo, W. et al. Influence of diabetes on mortality and ICD therapies in ICD recipients: a systematic review and meta-analysis of 162,780 patients. Cardiovasc Diabetol 21, 143 (2022). https://doi.org/10.1186/s12933-022-01580-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-022-01580-y