Abstract
Background
Cobalt (Co) is a metal which is widely used in the industrial production. The previous studies found the toxic effects of environmental Co exposure on multiple organs. However, the correlation of blood Co concentration with lung function was inconsistent in patients with chronic obstructive pulmonary disease (COPD).
Methods
All 771 stable COPD patients were recruited. Peripheral blood and clinical information were collected. The levels of blood Co and serum CC16 were measured.
Results
Cross-sectional study suggested that the level of blood Co was inversely and dose-dependently related to lung function parameters. Each 1 ppm elevation of blood Co was related to 0.598 L decline in FVC, 0.465 L decline in FEV1, 6.540% decline in FEV1/FVC%, and 14.013% decline in FEV1%, respectively. Moreover, higher age, enrolled in winter, current-smoking, higher smoking amount, and inhaled corticosteroids prominently exacerbated the negative correlation between blood Co and lung function. Besides, serum CC16 content was gradually reduced with blood Co elevation in COPD patients. Besides, serum CC16 was positively correlated with lung function, and inversely related to blood Co. Additionally, decreased CC16 substantially mediated 11.45% and 6.37% Co-triggered downregulations in FEV1 and FEV1%, respectively.
Conclusion
Blood Co elevation is closely related to the reductions of pulmonary function and serum CC16. CC16 exerts a significantly mediating role of Co-related to pulmonary function decrease among COPD patients.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is the third prominent disease for mortality all over the world. Due to obstructive bronchiolitis, emphysema, and chronic inflammation in lungs, COPD is mainly characterized by irreversible airflow limitation and persistent respiratory symptoms [1, 2]. Shortness of breath or breathing difficulties restrict daily physical activity of COPD patients. Moreover, COPD patients often accompany with anxiety, depression, cardiovascular diseases, as well as affect overall health and the quality of life perpetually [3]. COPD has become an importantly healthy burden affecting nearly 200 million populations, and evoked millions of deaths globally every year [4]. Cigarette smoking is still the central risk factor in the pathogenesis of COPD [5]. Additionally, environmental exposure to biofuel emissions, inhaled toxic gases, particles and air pollution also leads to the initiation and development for COPD [6,7,8]. However, the associations between heavy metals exposure and COPD are not fully expounded.
Although COPD is a chronically respiratory disease, reducing environmental hazards exposure can decrease the risk of COPD. Previous studies have suggested that COPD is linked with heavy metals exposure [9, 10]. Cobalt (Co) and several of its compounds are widely used for industrial applications, mainly included the manufacture of batteries and alloys, medicinal products, wear-resistant cobalt alloys, and hard metal industries [11]. Not only that, Co also exerts important role in the normal biological function, such as vitamin B12 synthesis, hematopoiesis, nervous system, and bone marrow erythropoiesis [12]. A longitudinal study indicated that pulmonary function is continuously declined in workers exposed to Co compounds [13]. The former investigation hinted that the concentration of toenail Co is inversely related to the level of pulmonary function in children with asthma in Chicago [14]. However, a longitudinal study indicated no obvious correlation of urinary Co with COPD in the American adult population [15]. Though previous surveys have explored the influence of environmental Co on COPD, the conclusions are inconsistent. Therefore, we think that it is necessary for us to clarify whether environmental Co affect the progression of COPD.
Over the past decade, an increasing body of evidence has revealed that the cellular and molecular mechanisms of COPD including oxidative stress response, inflammatory cells, inflammatory cytokines, the imbalance of proteases and elastases, senescence, and aging, as well as epigenetic modifications [16,17,18,19]. The Club cell secretory protein (CC16) is a highly conserved and circulating homodimeric protein, which is primarily secreted by airway club cells into epithelial airway and spread everywhere in the body [20, 21]. The former investigations have demonstrated that CC16 play the anti-inflammatory and anti-oxidant roles [22, 23]. Moreover, increasing data have confirmed that CC16 is involved in many respiratory diseases, such as COPD, asthma, lung cancer, pulmonary infectious diseases [24,25,26,27]. As we all known, Co nanoparticles can cause oxidative stress and DNA damage in hematopoietic stem cells [28]. Additionally, there is an exposure-response relationship between blood Co and CC16 in the workers from Swedish hard metal industry [29]. Therefore, we thought that environmental Co exposure is a risk for COPD progression through evoking CC16 decrease.
In this project, we explored the associations of blood Co concentration with lung function decrease, and the potential mediating role of CC16 reduction in COPD patients. All 771 stable COPD cases were recruited. Pulmonary function test was carried out, the concentrations of Co and CC16 were detected. The role of CC16 decrease in the association of blood Co elevation with lung function reduction was explored among the 711 COPD patients.
Materials and methods
Study population
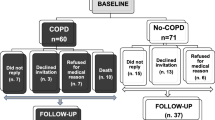
These participants were from the Anhui COPD cohort (AHCC). The whole of participator was recruited from Second Affiliated Hospital of Anhui Medical University and Bozhou People’s Hospital. All participants were resided in the current residence for five or more years, with the same environmental exposure condition from 2017 to 2020, which has been described previously [30, 31]. COPD was diagnosed and confirmed in the basis of GOLD criteria [32]. The first follow-up work was performed after enrollment at the end of two years. Peripheral blood specimens and clinical data were collected. Questionnaire investigation was conducted, the information of daily habits, exercise, occupational exposure, smoking status, and living environment were obtained. All cases were selected in the stable stage, without lung cancers, autoimmune diseases or accompanied with other pulmonary diseases. Ultimately, 771 eligible COPD patients were enrolled.
Determination of serum CC16 via enzyme linked immunosorbent assay (ELISA)
The content of serum CC16 was measured using ELISA. Human CC16 commercial ELISA kits (CSB-E08680h) were purchased from Cusabio, Wuhan, China (https://www.cusabio.com/). Experimental procedures were referred to the previous experiments with minor adjustments [33, 34].
Determination of blood co by inductively coupled-mass spectrometer (ICP-MS)
The concentration of Co in the blood was detected through ICP-MS in accord with the other research [35]. Shortly, blood samples, calibration standards, and quality control samples were added metal-free plastic tube prewashed using acid. Then, the internal standard working solution and 0.1% HNO3 were added. All samples were mixed and centrifuged. The supernatant was transferred into the new prewashed tubes. Ultimately, all tubes were placed in the autosampler and detected based on pre-set procedure. Lastly, the standard curve was established with the standard template and the concentration of blood Co was calculated.
Statistical analysis
All statistical analyses were conducted by SPSS 19.0 and R studio 3.6.1 software. All data were shown as mean, median or frequency. The difference of continuous data was compared with one-way ANOVA test or Student t test. The difference of categorical data was compared by chi-square test. According to the tertiles of blood Co concentration, COPD patients were divided into three groups. The value of serum CC16 was log-transformed. The correlations among blood Co, serum CC16, and lung function indicators were assessed by univariate linear and logistic regression models. To exclude the effect of covariates, confounding factors, mainly including age, gender, BMI, season, smoking status and amount, cooking methods, diabetes mellitus, and inhaled drugs usage, were adjusted and multivariate regression models were conducted to further estimate the correlations among blood Co, serum CC16, and lung function indicators among COPD patients. Stratified analyses were carried out by age, smoking status, smoking amount, enrolled season, and the usage of inhaled corticosteroids (ICS) among COPD patients. Additionally, for the sake of observing the dose-response correlations between blood Co and lung function indicators through a visualization method, restricted cubic splines (RCS) were conducted. Lastly, the mediating influence of CC16 reduction on the correlation between blood Co and lung function decline was estimated by mediation analyses. P value <0.05 was regarded as statistically significances. The P values were 2-side.
Results
Baseline characteristics
All participants were divided into three groups in the accordance with the tertiles of blood Co concentration. Among all COPD patients, the average age was 74.0 years, with 73.54% men. Additionally, 22.83% patients were enrolled from spring, 15.43% cases were from summer, 29.57% subjects were from winter, and 32.04% participants were from winter (Table 1). In addition, there were 26.37% current smokers, 78.04% self-cooking, and 31.78% drinkers (Table 1). The numbers of COPD patients enrolled from winter, current smokers, self-cooking, and smoking amount were obviously increased with the elevated blood Co concentration. Moreover, no difference of hypertension, coronary disease, and cerebrovascular diseases was found in COPD subgroups. However, the number of diabetes mellitus was most in the COPD patients with the highest blood Co (Table 1). Across the whole participants, the size of SABA usage was gradually elevated in parallel with the increasing blood Co concentration (Table 1). Moreover, serum CC16 and pulmonary function levels were prominently downregulated with the increasing blood Co concentration among COPD patients (Table 1).
Correlations between blood co and pulmonary function parameters
RCS analyses found that there were inverse and non-linear relationships between blood Co and FVC, FEV1, FEV1/FVC%, and FEV1% among COPD patients (Fig. 1A-D). Univariate logistic regression analyses suggested the odd ratios of the reductions in FVC, FEV1, and FEV1% were obviously elevated in COPD patients with highest tertile of blood Co (Fig. 2A-D). Moreover, to further confirm this correlation, multivariate linear regression analyses were conducted. Age, gender, enrolled season, smoking status and amount, cooking methods, hypertension, coronary disease, and ICS usage were simultaneously controlled. As represented in Table 2, each 1 ppm elevation of blood Co was related to 0.598 L decline in FVC, 0.465 L decline in FEV1, 6.540% decline in FEV1/FVC%, and 14.013% decline in FEV1%, respectively. Moreover, COPD patients were divided into three groups. Multivariate logistic regression models indicated that blood Co elevation increased the risks of declines in FVC, FEV1, and FEV1% (Table 2). In addition, stratified analyses were carried out. As represented in Supplemental Table 1, age, enrolled season, smoking status, smoking amount, hypertension, coronary disease, and ICS usage prominently affected the correlation of Co concentration with pulmonary function. However, no dramatically influence of gender, cooking methods, diabetes mellitus, cerebrovascular diseases, the usages of SABA, SAMA, LABA, and LAMA on this correlation among all participants (Supplemental Table 1).
Estimated percent changes (mean and 95% confidence intervals) by tertiles of blood Co in COPD patients. The correlations between blood tertile of blood Co and lung function indicators were assessed via logistic regression analyses. (A) Tertiles of blood Co and FVC. (B) Tertiles of blood Co and FEV1. (C) Tertiles of blood Co and FEV1/FVC%. (D) Tertiles of blood Co and FEV1%.
Correlation between blood co and serum CC16
The correlation between blood Co and serum CC16 was estimated. As represented in Table 3, each 1-unit upregulation of blood Co was linked to 0.340 ng/mL decrease in serum CC16. Furthermore, blood Co was significantly associated with serum CC16 content in tertile 2 (β=-0.177) and tertile 3 (β=-0.277) (Table 3). In addition, the correlation of blood Co with serum CC16 was estimated in the whole participators with potential confounding factors. Stratified analyses revealed that self-cooking, diabetes mellitus, and the usage of ICS didn’t affect the correlation between blood Co and serum CC16. Interestingly, smoking status, smoking amount, and enrolled season affected the relationship of blood Co level with serum CC16 content in all subjects (Table 3). Current smoking obviously aggravated the inverse association between blood Co and serum CC16 in COPD patients (Table 3).
Correlations between serum CC16 and pulmonary function parameters
Linear regression analyses were used to determine the positive dose-response correlations between serum CC16 and pulmonary function parameters (Table 4). Further, logistic regression analyses demonstrated that pulmonary function levels were substantially upregulated with elevated serum CC16 content (Table 4). Besides, the correlations between serum CC16 and pulmonary function parameters were also estimated in patients with different clinical characteristics. As represented in Table 4, smoking status, smoking amount, and the usage of ICS sensibly modified these correlations.
Mediation effects of CC16 on the correlation between Co exposure and pulmonary function decline
The combined effects of blood Co increase and serum CC16 decrease on pulmonary function decline were further explored in COPD patients. COPD cases were divided into three subgroups according to the tertiles of serum CC16 concentration, and then stratified by enrolled season, smoking status, and smoking amount. As shown in Supplemental Table 2, multivariate linear regression analyses revealed that blood Co was inversely associated with pulmonary function indicators. And, with the decreasing serum CC16 concentration, the negative relationships between blood Co and pulmonary function parameters were gradually elevated, and were strongest in the subgroup with the lowest serum CC16 (Supplemental Table 2). These results suggested that blood Co elevation was an independent risk factor for pulmonary function damage among COPD patients. Then, mediating influence of CC16 downregulation was analyzed on this correlation of blood Co elevation with pulmonary function decline. As shown in Table 5, CC16 decline dramatically mediated 11.45% and 6.37% of Co-triggered the downregulations in FEV1 and FEV1%, respectively. There was no obviously mediating effect of the relationships between Co exposure and the decreases of FVC and FEV1/FVC% among COPD patients (Table 5).
Discussion
This investigation primarily explored the correlation of blood Co concentration with pulmonary function change, and the effect modification mechanism in COPD patients. Our results shown that there were substantially inverse dose-response correlations of blood Co with the levels of pulmonary function and serum CC16. CC16 reduction dramatically mediated environmental Co-trigged pulmonary function decline in COPD patients. These data hinted that CC16 reduction is implicated in the progress of environmental Co-caused pulmonary function decline in COPD patients.
Mounting evidence have implied that environmental heavy metals exposure is closely related to pulmonary function injury among COPD patients [30, 36]. Co is a metal which is widely used in the industrial production including the manufacturing of hard metals [12]. It is known that Co exposure has detrimental effect on the heart, lung, and skin. The previous studies have confirmed that environmental Co exposure is the hazard factor of occupational asthma and interstitial lung disease [37, 38]. In recent years, many researchers have concerned the implication of Co exposure on lung function in general population and COPD cases [13,14,15]. However, the conclusions are inconsistent in COPD patients. Consequently, the correlation was further analyzed via a multicenter and large sample cross-sectional study. We found that higher blood Co concentration was correlated with lower lung function. Not only that, age, enrolled season, smoking status, smoking amount, hypertension, coronary disease, and ICS usage prominently affected the correlations between blood Co and lung function. The stronger correlation of blood Co concentration with lung function level was observed in COPD patients with higher ager, enrolled in winter, current-smoking, higher smoking amount, combined with hypertension and coronary disease, and without ICS usage. Thus, blood Co concentration is negatively correlated with lung function among COPD cases.
The former research confirmed that inflammation and oxidative stress are the vital pathogenesis of COPD development process [16,17,18]. CC16 has multiple functions of anti-inflammation and anti-oxidation functions, aberrant inflammation and oxidation stress always induce CC16 reduction in the body [22, 23]. Additionally, recent research found that exposure to Co nanoparticles induce oxidative stress in hematopoietic stem cells [28]. In our study, we found that blood Co concentration was significantly and inversely related to serum CC16 level in COPD patients. Meanwhile, stratified analysis suggested that the correlation between blood Co concentration and serum CC16 content was stronger in the current-smoking patients than these in none- and former-smoking subjects. Therefore, these results indicated that environmental Co exposure induces CC16 reduction in COPD patients which could be exacerbated by current-smoking status.
CC16 is almost entirely secreted by Club cells and non-ciliated airway epithelial cells [20, 21]. CC16 transfers from the airway to the circulatory system when the epithelial cells are damaged by inhaled toxins such as environmental pollutants and cigarette smoke [39, 40]. Chronic exposure to polycyclic aromatic hydrocarbons and cigarette smoke obviously decreases the level of circulating CC16 level [39, 40]. Epidemiological study found that circulating CC16 level is reduced in COPD patients compared with smokers and nonsmokers [41]. Moreover, serum CC16 is decreased and negatively linked to the severity classification in COPD cases [42]. Animal experiment declared that CC16 deficiency aggravates lung inflammation and lung injury in mice model of inflamm-aging [20]. Therefore, we thought environmental Co exposure may evoke COPD progression through inducing Club cells and epithelial cells injury, and finally lead to CC16 reduction. In our study, there was an inverse correlation between serum CC16 and lung function. Besides, mediating analyses hinted that circulating CC16 conspicuously mediated the increase of blood Co-correlated with the declines in FEV1 and FEV1% among COPD patients, hinting that environmental Co exposure may evoke lung function reduction via the damaged Club cells and epithelial cells in COPD patients. Interestingly, serum CC16 decline just mediated partial lung function injury. Actually, multiple stressors, such as oxidative stress, nitrative stress, and endoplasmic reticulum stress, or cellular damage all can mediate the pathophysiological process of COPD [43,44,45]. Not only that, Co toxicity always activates oxidative stress, inflammation, and epithelial damage [29, 46, 47]. Co exposure promotes the initiation and development of COPD through not only evoking epithelial damage and CC16 decrease, but also causing inflammation and oxidative stress. Therefore, it was well explained why CC16 decrease just partially mediated Co-related to pulmonary function decline. So, we can’t exclude the other mechanisms in Co-incurred COPD progression via the current epidemiological research. To sum up, these results suggested that there are other pathophysiological mechanisms implicated in Co-evoked COPD progression at the same time.
The current research mainly analyzed the effect of Co exposure on lung function, and the potentially mediating mechanism among COPD patients. Our study provided important clue about this association and explored the possible pathological mechanisms. However, it also had many deficiencies. First, this investigation was only a cross-sectional study, the specific mechanism by Co-evoked lung function reduction was unclear among COPD patients. Co exposure can evoke inflammation and oxidative stress. However, other mechanisms, such as oxidative stress and inflammation, can’t be eliminated in the current cross-sectional study. Whether the relationship between oxidative stress and Co exposure is synergistic, causal, or others can’t be determined. More animal and cellular experiments would be conducted in the laboratory and are helpful for elucidating the associations. Second, the source of Co exposure was not analyzed and explored in this project. More information about occupational exposure and living environment should be investigated during the epidemiological analysis. Third, the concentration of Co was detected in the blood samples at same point in time among the whole COPD cases. Nevertheless, the concentration of blood Co at one time point may noy fully reflect the true level of Co exposure in body. Therefore, more biological samples, such as urine sample and bronchoalveolar lavage fluid from different time points should be collected in the future. Fourth, the exact time and dosage of ICS were unknown. The influence of ICS dosage on the relationship between blood Co and pulmonary function can’t be explored in the current research. A prospective cohort study will help to resolve this puzzle.
Conclusions
In total, this investigation primarily reveals that blood Co concentration is dose-dependently and negatively related to lung function parameters and serum CC16 level in COPD patients. The current investigation first provides evidence that Co exposure incurs lung function reduction partially through CC16 decline in COPD patients. Moreover, higher age, winter, current-smoking, higher smoking amount, and ICS usage prominently exacerbate the negative correlation of blood Co content with lung function. This investigation has vital public healthy significance and is helpful for implementing new policies in daily protection and clinical therapy for COPD patients. Our findings highlight the importance to guard against lung function decline of COPD patients by environmental Co exposure.
Data availability
No datasets were generated or analysed during the current study.
References
Rabe KF, Watz H. Chronic obstructive pulmonary disease. Lancet. 2017;389(10082):1931–40.
Sin DD, Doiron D, Agusti A, Anzueto A, Barnes PJ, Celli BR, Criner GJ, Halpin D, Han MK, Martinez FJ, et al. Air pollution and COPD: GOLD 2023 committee report. Eur Respir J. 2023;61(5):2202469.
Ford ES, Murphy LB, Khavjou O, Giles WH, Holt JB, Croft JB. Total and state-specific medical and absenteeism costs of COPD among adults aged ≥ 18 years in the United States for 2010 and projections through 2020. Chest. 2015;147(1):31–45.
Mannino DM. COPD: epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest. 2002;121:s121–6.
Brusselle GG, Joos GF, Bracke KR. New insights into the immunology of chronic obstructive pulmonary disease. Lancet. 2011;378(9795):1015–26.
Berg K, Wright JL. The Pathology of Chronic Obstructive Pulmonary Disease: Progress in the 20th and 21st centuries. Arch Pathol Lab Med. 2016;140(12):1423–8.
Bagdonas E, Raudoniute J, Bruzauskaite I, Aldonyte R. Novel aspects of pathogenesis and regeneration mechanisms in COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:995–1013.
Po JY, FitzGerald JM, Carlsten C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax. 2011;66(3):232–9.
Hassan F, Xu X, Nuovo G, Killilea DW, Tyrrell J, Da, Tan C, Tarran R, Diaz P, Jee J, et al. Accumulation of metals in GOLD4 COPD lungs is associated with decreased CFTR levels. Respir Res. 2014;15(1):69.
Asker S, Asker M, Yeltekin AC, Aslan M, Ozbay B, Demir H, Turan H. Serum levels of trace minerals and heavy metals in severe COPD patients with and without pulmonary hypertension. Int J Chron Obstruct Pulmon Dis. 2018;13:1803–8.
Harper EM, Kavlak G, Graedel TE. Tracking the metal of the goblins: cobalt’s cycle of use. Environ Sci Technol. 2012;46(2):1079–86.
Barceloux DG, Cobalt. J Toxicol Clin Toxicol. 1999;37(2):201–6.
Verougstraete V, Mallants A, Buchet JP, Swennen B, Lison D. Lung function changes in workers exposed to cobalt compounds: a 13-year follow-up. Am J Respir Crit Care Med. 2004;170(2):162–6.
Madrigal JM, Persky V, Jackson BP, Bain A, Siemer M, Pappalardo AA, Argos M. Assessment of Metal concentrations and associations with pulmonary function among children with asthma in Chicago, Illinois. Int J Environ Res Public Health. 2021;18(14):7279.
Rahman HH, Niemann D, Munson-McGee SH. Association between environmental toxic metals, arsenic and polycyclic aromatic hydrocarbons and chronic obstructive pulmonary disease in the US adult population. Environ Sci Pollut Res Int. 2022;29(36):54507–17.
Fu L, Fei J, Tan ZX, Chen YH, Hu B, Xiang HX, Zhao H, Xu DX. Low vitamin D status is Associated with inflammation in patients with chronic obstructive Pulmonary Disease. J Immunol. 2021;206(3):515–23.
Guo P, Li R, Piao TH, Wang CL, Wu XL, Cai HY. Pathological mechanism and targeted drugs of COPD. Int J Chron Obstruct Pulmon Dis. 2022;17:1565–75.
Barnes PJ. Cellular and molecular mechanisms of asthma and COPD. Clin Sci. 2017;131(13):1541–58.
Fei J, Fu L, Cao W, Hu B, Zhao H, Li JB. Low vitamin D status is Associated with epithelial-mesenchymal transition in patients with chronic obstructive Pulmonary Disease. J Immunol. 2019;203(6):1428–35.
Laucho-Contreras ME, Polverino F, Tesfaigzi Y, Pilon A, Celli BR, Owen CA. Club cell protein 16 (CC16) deficiency increases inflamm-aging in the lungs of mice. Physiol Rep. 2018;6(15):e13797.
Bernard A, Marchandise FX, Depelchin S, Lauwerys R, Sibille Y. Clara cell protein in serum and bronchoalveolar lavage. Eur Respir J. 1992;5(10):1231–8.
Laucho-Contreras ME, Polverino F, Gupta K, Taylor KL, Kelly E, Pinto-Plata V, Divo M, Ashfaq N, Petersen H, Stripp B, et al. Protective role for club cell secretory protein-16 (CC16) in the development of COPD. Eur Respir J. 2015;45(6):1544–56.
Tufvesson E, Svensson H, Ankerst J, Bjermer L. Increase of club cell (Clara) protein (CC16) in plasma and urine after exercise challenge in asthmatics and healthy controls, and correlations to exhaled breath temperature and exhaled nitric oxide. Respir Med. 2013;107(11):1675–81.
Laucho-Contreras ME, Polverino F, Tesfaigzi Y, Pilon A, Celli BR, Owen CA. Club cell protein 16 (CC16) augmentation: a potential disease-modifying Approach for Chronic Obstructive Pulmonary Disease (COPD). Expert Opin Ther Targets. 2016;20(7):869–83.
Li X, Guerra S, Ledford JG, Kraft M, Li H, Hastie AT, Castro M, Denlinger LC, Erzurum SC, Fahy JV, et al. Low CC16 mRNA expression levels in bronchial epithelial cells are Associated with Asthma Severity. Am J Respir Crit Care Med. 2023;207(4):438–51.
Guerra S, Vasquez MM, Spangenberg A, Halonen M, Martinez FD. Serum concentrations of club cell secretory protein (Clara) and cancer mortality in adults: a population-based, prospective cohort study. Lancet Respir Med. 2013;1(10):779–85.
Rohmann N, Stürmer P, Geisler C, Schlicht K, Hartmann K, Türk K, Hollstein T, Tran F, Rosenstiel P, Franke A, et al. Brief Research Report: serum clara cell 16 kDa protein levels are increased in patients hospitalized for severe SARS-CoV-2 or sepsis infection. Front Immunol. 2022;13:1037115.
Zhu W, Liu Y, Zhang W, Fan W, Wang S, Gu JH, Sun H, Liu F. Selenomethionine protects hematopoietic stem/progenitor cells against cobalt nanoparticles by stimulating antioxidant actions and DNA repair functions. Aging. 2021;13(8):11705–26.
Andersson L, Hedbrant A, Bryngelsson IL, Persson A, Johansson A, Ericsson A, Vihlborg P, Sjögren B, Särndahl E, Stockfelt L, et al. Respiratory health and inflammatory markers-exposure to Cobalt in the Swedish Hard Metal Industry. J Occup Environ Med. 2020;62(10):820–9.
Lv BB, Yang CL, Tan ZX, Zheng L, Li MD, Jiang YL, Liu L, Tang MM, Hua DX, Yang J, et al. Association between cadmium exposure and pulmonary function reduction: potential mediating role of telomere attrition in chronic obstructive pulmonary disease patients. Ecotoxicol Environ Saf. 2023;251:114548.
Jiang YL, Fei J, Cao P, Zhang C, Tang MM, Cheng JY, Zhao H, Fu L. Serum cadmium positively correlates with inflammatory cytokines in patients with chronic obstructive pulmonary disease. Environ Toxicol. 2022;37(1):151–60.
Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Criner GJ, Frith P, Halpin DMG, Han M, et al. Global strategy for the diagnosis, management, and Prevention of Chronic Obstructive Lung Disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164.
Pu Z, Wang W, Xie H, Wang W. Apolipoprotein C3 (ApoC3) facilitates NLRP3 mediated pyroptosis of macrophages through mitochondrial damage by accelerating of the interaction between SCIMP and SYK pathway in acute lung injury. Int Immunopharmacol. 2024;128:111537.
Li Y, Dai M, Wang L, Wang G. Polysaccharides and glycosides from Aralia Echinocaulis protect rats from arthritis by modulating the gut microbiota composition. J Ethnopharmacol. 2021;269:113749.
Huang JH, Tao L, Wu Y, He W, Wang JX, Chen X, Fu L. Cobalt exposure and dyslipidemia in elderly population: the mediating role of systemic inflammation and lipid peroxidation. Environ Sci Pollut Res Int. 2023;30(17):50402–11.
Zheng L, Jiang YL, Fei J, Cao P, Zhang C, Xie GF, Wang LX, Cao W, Fu L, Zhao H. Circulatory cadmium positively correlates with epithelial-mesenchymal transition in patients with chronic obstructive pulmonary disease. Ecotoxicol Environ Saf. 2021;215:112164.
Al-Abcha A, Wang L, Reilly MJ, Rosenman KD. Work-related asthma in cobalt-exposed workers. J Asthma. 2021;58(8):1032–41.
Adams TN, Butt YM, Batra K, Glazer CS. Cobalt related interstitial lung disease. Respir Med. 2017;129:91–7.
Broeckaert F, Bernard A. Clara cell secretory protein (CC16): characteristics and perspectives as lung peripheral biomarker. Clin Exp Allergy. 2000;30(4):469–75.
Zhou Y, Mu G, Liu Y, Xiao L, Ma J, Wang B, Shi T, Tan A, Yuan J, Chen W. Urinary polycyclic aromatic hydrocarbon metabolites, Club cell secretory protein and lung function. Environ Int. 2018;111:109–16.
Lomas DA, Silverman EK, Edwards LD, Miller BE, Coxson HO, Tal-Singer R. Evaluation of serum CC-16 as a biomarker for COPD in the ECLIPSE cohort. Thorax. 2008;63(12):1058–63.
Rong B, Fu T, Gao W, Li M, Rong C, Liu W, Liu H. Reduced serum concentration of CC16 is Associated with Severity of Chronic Obstructive Pulmonary Disease and contributes to the diagnosis and Assessment of the Disease. Int J Chron Obstruct Pulmon Dis. 2020;15:461–70.
Kirkham PA, Barnes PJ. Oxidative stress in COPD. Chest. 2013;144(1):266–73.
Hirano T, Matsunaga K, Sugiura H, Minakata Y, Koarai A, Akamatsu K, Ichikawa T, Furukawa K, Ichinose M. Relationship between alveolar nitric oxide concentration in exhaled air and small airway function in COPD. J Breath Res. 2013;7(4):046002.
Wang Y, Fei J, Xu J, Cheng ZY, Ma YC, Wu JH, Yang J, Zhao H, Fu L. Associations of the serum KL-6 with severity and prognosis in patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Lung. 2024; 202(3): 245–55.
Zhao YY, Cao CL, Liu YL, Wang J, Li SY, Li J, Deng Y. Genetic analysis of oxidative and endoplasmic reticulum stress responses induced by cobalt toxicity in budding yeast. Biochim Biophys Acta Gen Subj. 2020;1864(3):129516.
Jeong J, Han Y, Poland CA, Cho WS. Response-metrics for acute lung inflammation pattern by cobalt-based nanoparticles. Part Fibre Toxicol. 2015;12:13.
Acknowledgements
Not applicable.
Funding
This study was supported by National Natural Science Foundation of China (82270071), Anhui Provincial Clinical Research Transformation Project (202204295107020014, 202204295107020056), Research Funds of Center for Big Data and Population Health of IHM (JKS2023010), Anhui Provincial Health Research Foundation (AHWJ2022b033, AHWJ2021b091), University Natural Science Research Project of Anhui Province (2023AH030117), Anhui Provincial Medical and Health Key Specialty Construction Project ([2021]273), Anhui Medical University Foundation (2021xkj159), Talent Project of Colleges and Universities in Anhui Province (gxyp2021169), National Natural Science Foundation Incubation Program of the Second Affiliated Hospital of Anhui Medical University (2019GQFY06, 2020GQFY05), Key Developmental Program of Anhui Province (2022i01020003), and Opening Foundation of Anhui Province Key Laboratory of Clinical and Preclinical Research in Respiratory Disease (HX2022D01).
Author information
Authors and Affiliations
Contributions
Fei Tang, Hong-Yan Liu, Qi-Yuan He, Ying Liu: Methodology, Investigation. Li-Ping Lv, Jun Fei: Conceptualization, Methodology, Resources. Lin Fu: Conceptualization, Validation, Investigation, Writing - Review & Editing, Visualization, Project administration, Funding acquisition.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
In accordance with the Declaration of Helsinki, the Ethics Committee of Second Affiliated Hospital of Anhui Medical University (YJ-YX2021-146) approved the studies involving humans. All participators provided informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tang, F., Liu, HY., He, QY. et al. Cobalt exposure and pulmonary function reduction in chronic obstructive pulmonary disease patients: the mediating role of club cell secretory protein. Respir Res 25, 324 (2024). https://doi.org/10.1186/s12931-024-02950-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-024-02950-8