Abstract
Backgorund
Tissue-engineered tracheal grafts (TETG) can be recellularized by the host or pre-seeded with host-derived cells. However, the impact of airway disease on the recellularization process is unknown.
Methods
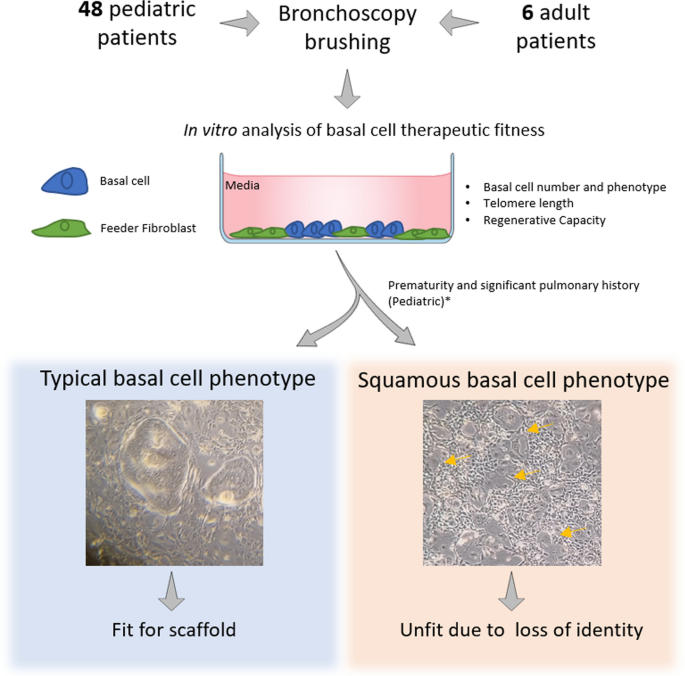
In this study, we determined if airway disease alters the regenerative potential of the human tracheobronchial epithelium (hTBE) obtained by brushing the tracheal mucosa during clinically-indicated bronchoscopy from 48 pediatric and six adult patients.
Results
Our findings revealed that basal cell recovery and frequency did not vary by age or region. At passage 1, all samples produced enough cells to cellularize a 3.5 by 0.5 cm2 graft scaffold at low cell density (~ 7000 cells/cm2), and 43.75% could cellularize a scaffold at high cell density (~ 100,000 cells/cm2). At passage 2, all samples produced the number of cells required for both recellularization models. Further evaluation revealed that six pediatric samples (11%) and three (50%) adult samples contained basal cells with a squamous basal phenotype. These cells did not form a polarized epithelium or produce differentiated secretory or ciliated cells. In the pediatric population, the squamous basal cell phenotype was associated with degree of prematurity (< 28 weeks, 64% vs. 13%, p = 0.02), significant pulmonary history (83% vs. 34%, p = 0.02), specifically with bronchopulmonary dysplasia (67% vs. 19%, p = 0.01), and patients who underwent previous tracheostomy (67% vs. 23%, p = 0.03).
Conclusions
In summary, screening high-risk pediatric or adult population based on clinical risk factors and laboratory findings could define appropriate candidates for airway reconstruction with tracheal scaffolds.
Level of evidence. Level III Cohort study.
Graphical Abstract
Similar content being viewed by others
Background
Laryngotracheal stenosis (LTS), defined as soft tissue narrowing of the proximal airway, currently has an estimated incidence of 0.6-2% [1,2,3]. The causes of LTS can be multifactorial in nature. In the pediatric and adult populations, acquired stenosis is most commonly secondary to prolonged intubation, tracheostomy, systemic disease, trauma, infection, or idiopathic causes [4, 5]. Surgical management of LTS can range from tracheostomy to endoscopic and open approaches [1]. Despite advancements in endoscopic and open techniques, there are significant limits to current clinical approaches.
Long-segment tracheal defects are defined as > 50% in adults and > 30% in children [6]. These defects cannot be repaired primarily because they require replacement tissue that is not currently available. A myriad of bioengineering approaches have created scaffolds that recapitulate the biological and mechanical properties of the native trachea [7, 8]. The success of these scaffolds is dependent in part on rapid epithelialization, which restores mucociliary clearance and prevents infection and inflammation [9]. However, the optimal method for reepithelialization is unknown.
We demonstrated that host-derived basal cells regenerate a surface airway epithelium (SAE) on a partially decellularized tracheal scaffold [10]. This process requires 7–14 days and could be accelerated by pre-seeding the scaffold with patient-derived cells. Ex vivo methods of cell seeding include the use of induced pluripotent stem cell-derived basal cells and primary airway stem cells (basal cells) [11]. Although both cell types can be expanded using current cell culture technology, the quality of the cell therapy product is likely to be dependent on the initial cell inoculum.
Patients with long-segment tracheal defects can suffer from chronic airway disease, a situation that may compromise the regenerative potential of the host’s basal cells. In particular, stenotic regions of the airway exhibit abnormal epithelial morphology, including basal cell dysplasia [12, 13]. We reported that the lifespan of the tracheobronchial basal cell is ~ 40 population doublings [14], which is consistent with the Hayflick limit [15]. Stem cell frequency decreases during wound healing and in vitro expansion, resulting in reduced regenerative potential [16, 17]. These decrements are associated with a decrease in the number of clone-forming stem cells, accumulation of cells with shortened telomeres, and suboptimal production of differentiated secretory and ciliated cells [18]. Thus, a critical question is whether tracheobronchial stem cells from patients with airway disease have sufficient regenerative potential to support the cellularization of a graft and the production of a functional epithelium. We addressed this issue by assessing the phenotype and function of basal cells that were recovered from the airways of normal donors and those with chronic lung disease.
Methods
Approvals
This study was approved by the institutional review boards of two tertiary-level pediatric and adult hospitals (Nationwide Children’s Hospital IRB STUDY00000847, Ohio State University 2021N0027). Pediatric and adult patients undergoing scheduled direct laryngoscopy and bronchoscopy (DLB) were voluntarily recruited. Demographics of the patients recruited were recorded.
Tracheal airway epithelial cell isolation
Our methods are similar to those previously described [16, 18]. Briefly, endotracheal brush biopsies were collected using a cytology brush (Medical Packing Corporation, Camarillo, CA). Under direct visualization, the cytology brush was advanced and spun in a focal region of the trachea five times for approximately 10 s.
Cells were liberated from the brushes using mechanical agitation in phosphate-buffered saline (PBS) supplemented with 10 µM β-mercaptoethanol (Acros Organics, NJ), 5 mM EDTA (Thermo Fisher, Waltham, MA), and 5 mM EGTA (Thermo Fisher, Waltham, MA). Cells were pelleted by centrifugation (2500 rpm, 5 min) and resuspended in 1 mL red blood cell lysis buffer (Invitrogen/Thermo Scientific, Waltham, MA) for 5 min. Lysis was then terminated by dilution with PBS (1:10) and the cells were repelleted. Cell pellets were then resuspended in culture medium (see below).
Tracheal airway epithelial culture timeline
Cells were cultured using the modified conditional reprogramming culture (mCRC) method [19]. Accordingly, the cells were co-cultured on a feeder layer of irradiated NIH-3T3 fibroblasts (ATCC #CRL-1658) with F-medium (Fmed) supplemented with Rho-kinase inhibitor, Y-27632 (10 µM). Cultures were supplemented with an antibiotic/antifungal cocktail, which was reduced to 50% concentration on day 2 and discontinued on day 4 of culture. Culture medium was changed on a Monday-Wednesday-Friday schedule, and the plates were monitored for basal cell colony development. Cultures were discarded if colonies were not observed on culture day 14. Successful cultures (p0) were expanded at passage 1 (p1) and cryopreserved as frozen stocks at passage 2 (p2).
Cytospin
Cytospin preparations (20,000 cells per slide) were prepared as previously described [14, 20], fixed with 10% neutral-buffered formalin (NBF) for 10 min at room temperature, and stained for Keratin 5 (Covance Innovative Antibodies, Rabbit, 1:1000) and Keratin 14 (Thermo Scientific, Mouse, 1:500). Slides were counterstained with 1 µg/ml 4′,6-diamidino-2-phenylindole (DAPI). Images of at least 200 nucleated cells were acquired using Zeiss Imager.Z1 fluorescent microscope (Zeiss) and quantified using ImageJ software.
Clone-forming cell frequency assay
Clone-forming Cell Frequency (CFCF) was determined using a limiting dilution method that has been previously described [21] and modified for use with airway tissues [14]. Passage one cells were distributed to wells of a 96-well plate using two-fold dilution from 100 cells/well to 1 cell/well. Six replicates were seeded for each cell input. Following 9 days of culture, cells were fixed with NBF, and stained with Giemsa stain. Wells were scored as positive or negative for the development of colonies. Linear regression analysis was used to calculate the CFCF.
Population Doubling Level calculation
Population Doubling Level was calculated as: PDL = 3.32 (logXe – logXb), where Xe is the basal cell number obtained at passage and Xb is the basal cell number plated (https://www.atcc.org/resources/culture-guides/animal-cell-culture-guide). Cells were stained with trypan blue and counted using a hemacytometer [15].
Relative telomere length determination
Telomere length was determined based on previously published methods [22, 23] with minor modifications [17]. Specifically, cells were recoverd using the double trypsinization method. Genomic DNA (gDNA) was purified from 50,000 cells using the DNeasy Blood & Tissue Kit (Qiagen Cat# 69506) and quantified using a Nanodrop 2000 spectrophometer (ThermoFisher, Welmington, DE). Both the telomere and 36B4 single copy gene control assays used 40 ng gDNA/reaction. Targets were amplified using previously reported standards and primers [22]. For the telomere assay, the magnesium concentration in the PowerSYBR Green Master Mix (Applied Biosystems Cat# 4367659) was lowered to a final concentration of 0.9625 mM through the addition of 0.5 M EDTA (0.0385 µL per 20 µL reaction). Previously published cycling parameters for telomeres [23] and 36B4 [22] were used. Jurkat (ATCC) and U1301 (human T-cell leukemia cell line (Sigma Cat# 01051619) were used as short and long telomere controls, respectively. A standard curve was generated for each experiment and was used to insure a linear relationship between DNA input and telomere length. Prior to analysis, the telomere standards were incubated at 95 °C with shaking for 5 min, and immediately placed on ice. Three technical replicates were generated for each standard curve point and biological sample. Relative telomere length was calculated according to the Telomere/Single copy gene control (T/S) ratio.
Flow cytometry
Human basal cells were resuspended at 10^7 cells/mL in BSA staining buffer (BD Pharmingen Cat# 554657). The cells were stained with APC-anti-CD151 (Biolegends Cat# 350406, 1:20) and EFlour 450-anti-CD49f (Invitrogen Ref# 48-0495-82, 1:20) for 30 min on ice. The cells were then washed with BSA staining buffer, fixed in NBF, and analyzed on a BD Pharmingen Fortessa-5 laser flow cytometer. Unstained cells served as a negative control. Flow data was analyzed using FlowJo.
Correlation of clinical and culture phenotype
Univariate chi-squared and t-test analyses were used to compare patient demographic and clinical characteristics between those who did and did not have squamous basal cells. Clinical characteristics included prematurity; significant pulmonary, cardiac, gastrointestinal, and/or neurological history; known chromosomal abnormalities; congenital defects in the head and neck (including supraglottic, glottic, subglottic, tracheal stenosis); and history of airway surgery. Prematurity was coded as an ordinal variable per World Health Organization guidelines, with a moderate to late preterm group (gestational age between 32 and 37 weeks), a very preterm group (28 to 32 weeks), and an extremely preterm group (less than 28 weeks).
Statistical analysis
All statistical calculations were conducted with Stata 17.0 (College Station, TX). Summary data are presented as the mean and standard deviation. Symbols represent the values from individual donors. Sample size is noted in the figure legends. Normally-distributed data were assessed by student’s t-test or 2-way ANOVA. Skewed data sets were assessed using the ROUT method and analyzed using GraphPad Prism, version 9.0.0 (GraphPad Software Inc., CA). A significance threshold of 0.05 was used. Specific analysis details for each data set and corresponding N for each experimental set are indicated in the figure legends.
Power analysis
Power analyses were completed with our pediatric population (total sample size of 48 patients), demonstrating that with our univariate chi-squared analyses with an error probability of 0.05 and power of 0.8, we would be able to detect a large effect size (r = 0.49). In our adult population (total sample size of 6 patients) with similar power analyses, we would be able to detect an effect size of 0.78. In order to detect a medium effect size (r = 0.3), we would need a total sample size of 143 patients in each of the pediatric and adult cohorts.
Results
Pediatric donor characteristics
This study included 48 pediatric patients and 6 adult patients. Male pediatric donors comprised 67% (N = 31) of the cohort and had a mean age of 3.5 years (standard deviation, S.D., 3.7 years). The mean female pediatric donor age was 3.4 (S.D. 3.5 years). The mean age did not vary for the two groups (p = 0.85). Mean body mass index (BMI) percentile was 51.6 (SE = 35). Prematurity was the most common comorbidity (62%, N = 30). Bronchoscopy was commonly performed for recurrent croup (N = 8, 17%), stridor (N = 8, 17%), or in conjunction with other surgical procedures (N = 6, 13%), including adenotonsillectomy for obstructive sleep apnea (N = 3, 50%). Full patient demographic information for the pediatric population is presented in Table 1.
Adult donor characteristics
Six adult donors were recruited for this study. The cohort was 50% (N = 3) male, with mean age of 55 years (SE 13.2 years). 50% (N = 3) of the patients underwent direct laryngoscopy (DL) for subglottic stenosis and 33% (N = 2) for tracheal stenosis. The final patient had a normal airway and was recruited as a healthy control. Additional patient characteristics of the adult population are detailed in Table 2.
Basal cell number and phenotype
Cytospin slides were generated from uncultured cells and stained for a pan-basal cell marker keratin 5 (K5) and a marker of basal cell activation keratin 14 (K14) (Fig. 1A). Regardless of age (pediatric vs. adult) or region sampled (normal vs. stenosis), basal cell number (K5+) and activation status (K5/K14+) were similar (Fig. 1B). These data indicate that the brush biopsy protocol recovered similar numbers of basal cells and that these metrics did not vary by age or region (Fig. 1C).
Similar basal cell yield and expansion potential in brush biopsies. A Representative immunostaining of cytospin-recovered cells demonstrates positive staining of basal cell markers (K5, green) and (K14, red) in pediatric (p0 n = 5, p2 n = 3) and adult (p0 n = 6, p2 n = 4) samples, after brushing from normal (p0 n = 6, p2 n = 4), and stenotic regions (p0 n = 5, p2 n = 3) at passage 0 (left panel) and passage 2 (right panel). B Bar graph showing the percentage of positive cells over total cell counts (DAPI, blue) count divided by age or C region of sample collection. Bars represent mean ± DLB: direct laryngoscopy and bronchoscopy S.D. Statistical analysis was performed using 2-way ANOVA with multiple-comparison test. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
As the brush biopsy contains a heterogenous population of epithelial cells including differentiated mucous-producing and ciliated cell types, cell isolates were cultured using the mCRC method which selects for basal cells. To determine if age or the region of airway stenosis sampling influenced basal cell expansion in vitro, cytospins were generated from passage 2 cells and stained for K5 and K14 (Fig. 1A). The percentage of basal cells increased with passage. Basal cell number (K5 + only) and activation state (K5/K14+) did not vary as a function of age (Fig. 1B) or airway region sampled (Fig. 1C).
Regenerative capacity
To estimate the therapeutic potential of cells that are recovered by brush biopsy, we determined the clone forming cell frequency at passage 1. This study used the limiting dilution assay and results were reported as the Clone-forming Cell Frequency (CFCFx1000, Fig. 2A). The mean CFCF was 195 +/- 210 (n = 33 donors). This value was lower than the CFCFx1000 for basal cells that were isolated by digestion of explanted tracheal tissue [24]. The pediatric and adult groups and the normal or stenotic sampling sites had similar numbers of clone forming cells.
Regenerative capacity of pediatric and adult basal cells. A Bar graph represents the Clone-forming Cell Frequency of pediatric and adult basal cells after 1 passage in culture (n = 30). B Prediction of the number of cells recovered after 1 or 2 passages in culture (n = 48) able to cellularize a scaffold at low density (LowD) or high density (HighD). C Bar graph of the in vitro population doubling after 1 or 2 passages in culture (p1 n = 35, p2 n = 35). D Relative telomere length of the basal cells of pediatric (n = 48), and adult (n = 6) donors divided by E Normal (n = 59) and stenotic (n = 18) region. Bars represent mean ± S.D. Statistical analysis was performed using paired, 2-tailed Student’s t-test
To determine if these clone forming cells could be amplified, they were passaged and cell yield was determined (Fig. 2B). These results were benchmarked against a scaffold that would be used for the reconstruction of a pediatric airway [25]. At passage 1, all samples contained sufficient cells to cellularize a 3.5 by 0.5 cm2 graft scaffold at low cell density (~ 7000 cells/cm^2) and 98% could cellularize a scaffold at high cell density (~ 100,000 cells/cm^2). At passage 2, all samples contained sufficient cells for both recellularization models.
To determine if these cells had reserve regenerative potential, we first calculated the number of populations doublings [15]. At passage 1, most samples underwent 0–5 population doublings (Fig. 2C). However, cell number did not increase in 13 samples. At passage 2, all samples underwent 4 population doublings. The total number of population doublings was ~ 25% of basal cell life-span [20].
Finally, we used telomere length as a surrogate for biological age [26]. DNA was recovered from cryopreserved p2 cells (48 pediatric and 5 adult subjects). Telomere length was analyzed using a modified PCR assay and is presented as the relative telomere length [17]. Since telomere length varies as a function of chronological age and has been associated with lung diseases [27], we evaluated pediatric and adult samples separately. At passage 2, the relative telomere length for pediatric samples was 2.3+/-0.42, and 41% of samples were in the short telomere range (the samples with a value </=1, Fig. 2D). Relative telomere length in adult samples was 1.6+/-0.3 and most samples were in the short telomere range (Fig. 2D). No significant differences were detected between normal or stenotic samples (Fig. 2E). Collectively, these data indicate that the airways of pediatric and adult 54 donors have sufficient regenerative capacity to recellularize an airway scaffold.
Alteration of basal cell identity: squamous basal cells
Culture morphology was qualitatively assessed at p1. Typical basal cells (normal phenotype) formed discrete colonies on the fibroblast feeder layer that were generally spherical or ovoid in shape and had distinct edges. Normal phenotype colonies required extensive trypsin exposure to remove them from the culture plate and to dissociate the cells into a single-cell suspension for passage and handling. Most pediatric donor collections yielded basal cell colonies of typical phenotype (59 of 69 samples, 85.5%, Fig. 3A). These cells expressed high levels of K5 and K14 (Fig. 3B, C).
Identification of squamous basal cells. A Normal tracheal basal cell colonies under 10x magnification form discrete colonies with distinct edges. Representative immunofluorescence staining demonstrates high levels of K5 (green) and K14 (red), markers associated with airway epithelial stem cells, at low B and high C magnification. Representative double staining with epithelial cell markers CD151 (α-CD151-APC) and CD49f (α-CD49f-eFlour-450) in normal D and stenotic E regions. F Squamous metaplasia cells under 10x magnification exhibit a diffuse growth pattern and no discrete edges.Representative immunofluorescence staining demonstrates high levels of K5 (green) and K14 (red), markers associated with airway epithelial stem cells, at low H and high I magnification. Representative double staining with epithelial cell markers CD151 (α-CD151-APC) and CD49f (α-CD49f-eFlour-450) in normal I and stenotic J regions
In contrast, squamous basal cells (Fig. 3F) were observed as morphological variants at p1. These colonies exhibited a diffuse lattice-like structure with poorly defined boundaries and expressed lower levels of K5 than typical cells (Fig. 3H, I). Both the number of K5 positive cells and the intensity of the staining were decreased relative to cells recovered from typical morphology colonies. Abnormal cells grew more rapidly than typical basal cells and were easily dislodged with trypsin. Ten cultures originating from seven pediatric patients (14.5%) contained squamous basal cell colonies at passage 1. Samples containing these abnormal cells were excluded from the previous data sets (Figs. 1, 2 and 3).
Cell phenotype was further evaluated using flow cytometry. Cells with a typical phenotype demonstrated high expression of the markers CD151 and CD49f (Fig. 3D, E), which are commonly expressed on epithelial basal cells [13]. In contrast, cells with the squamous basal cell phenotype had decreased or absent expression of these markers (Fig. 3K–J). Squamous basal cells from pediatric and adult donors exhibited similar morphology and marker expression profiles.
A meta-analysis demonstrated that the presence of squamous basal cells correlated with the degree of prematurity, with 67% (N = 4) from donors having a history of extreme prematurity (< 28 weeks, vs. 5% [N = 2], p = 0.001, see Table 3. Squamous basal cell isolates were also associated with significant pulmonary history (83% vs. 31%, p = 0.013), specifically bronchopulmonary dysplasia (67% vs. 17%, p = 0.006), as well as airway surgery (67% vs. 26%, p = 0.045), specifically tracheostomy placement (67% vs. 21%, p = 0.02). The presence of squamous basal cells was not associated with a history of laryngotracheal reconstruction or balloon dilation (33% vs. 10%, p = 0.1; 33% vs. 14%, p = 0.24; respectively). Subglottic stenosis as assessed by direct laryngoscopy and bronchoscopy approached significance (50% vs. 17%, p = 0.06).
Squamous basal cells were observed in one adult patient with subglottic stenosis and two patients with tracheal stenosis. Adult samples containing these abnormal cells were excluded from the previous data sets (Figs. 1, 2 and 3). The presence of squamous basal cells did not correlate with direct laryngoscopy findings (subglottic stenosis 50% vs. tracheal stenosis 100% vs. control 0%; p = 0.2) including aspiration, obstructive sleep apnea (OSA), past airway surgery, or current/previous tracheostomy (all p > 0.05).
Discussion
Our study revealed that the airways of pediatric and adult donors have sufficient regenerative capacity to recellularize an airway scaffold. However, we identified squamous basal cells in a subset of donors and associated their presence with chronic lung disease and tracheostomy in the pediatric population.
The basal cell is the tissue-specific stem cell of the conducting airway epithelium [28]. Common pediatric airway diseases including bronchopulmonary dysplasia [29] and laryngotracheal stenosis [30] can result in epithelial injury from mechanical ventilation, direct trauma, infection, and inflammation. Repeated injury causes selective activation of basal cells [17] and promotes proliferation. These events can lead to terminal differentiation and squamous metaplasia [31,32,33].
In conditions such as chronic obstructive pulmonary disease (COPD), pathologic remodeling of the airway epithelium includes squamous metaplasia. This condition is likely to be the result of environmental exposures and a chronic inflammatory response and is thought to contribute to poor ciliary function and mucus clearance [28]. Sustained pathogeneic squamous phenotype has been associated with the pathophysiology of tracheobronchial disorders with unknwon etiology, accompanied by recurrent infections, nodules formation, and absence of normal ciliated respiratory epithelium [34]. Squamous metaplasia has also been reported in the proximal airways following intubation and tracheostomy placement. Although the clinical implications of squamous metaplasia remain unclear [13], McKeon’s group identified a squamous basal cell subtype that self-renewed and retained its phenotype across multiple passages and after transplantation into immunocompromised mice [31]. We identified similar cells in our cohort and report that they are more prevalent in pediatric patients with bronchopulmonary dysplasia, subglottic stenosis, and those who underwent tracheostomy placement.
The association between bronchopulmonary dysplasia and squamous basal cells requires further study. The observed correlations may be a consequence of direct trauma to the airway during intubation and surgery in combination with free radical changes from prolonged intubation. It is also possible that the squamous metaplasia phenotype is congenitally predisposed in certain pediatric patients, although the relationship was not clearly demonstrated [13]. If substantiated, this predisposition would explain why premature patients have significantly higher rates of squamous basal cells compared to their full-term peers [35].
Future directions
The rise of tissue engineering has provided promising techniques with the intention of creating viable tracheal replacement grafts [8, 36, 37]. Successful grafting not only requires an optimal cell source and scaffold for integration but also the appropriate cellular microenvironment for complete epithelialization [8]. Although our data indicate that brush biopsy cells have significant therapeutic potential, a subset of samples contained squamous basal cells that do not regenerate the epithelium. Further studies could determine if cell rejuvenation methods would improve the performance of samples with low-performance metrics.
Study limitations
We recognize that our understanding of the squamous basal cell phenotype is limited by sample size and that the study may be underpowered to detect smaller effect sizes, particularly those related to tracheal stenosis. We also acknowledge that our cross-sectional study design could be enhanced by a longitudinal study. Finally, we understand that our sampling method may have underestimated the frequency of squamous basal cells in pediatric and adult airways.
Conclusions
Our data suggest that screening high-risk pediatric or adult population based on clinical risk factors and laboratory findings could define appropriate candidates for airway reconstruction with tracheal scaffolds.
Availability of data and materials
Not applicable.
References
Raol N, Rogers D, Setlur J, Hartnick CJ. Comparison of hybrid laryngotracheal reconstruction to traditional single- and double-stage laryngotracheal reconstruction. Otolaryngol Head Neck Surg. 2015;152:524–9.
Choi SS, Zalzal GH. Changing trends in neonatal subglottic stenosis. Otolaryngology–Head and Neck Surgery. 2000;122:61–3.
Walner DL, Loewen MS, Kimura RE. Neonatal subglottic stenosis–incidence and trends. Laryngoscope. 2001;111:48–51.
Lewis S, Earley M, Rosenfeld R, Silverman J. Systematic review for surgical treatment of adult and adolescent laryngotracheal stenosis. Laryngoscope. 2017;127:191–8.
Lorenz RR. Adult laryngotracheal stenosis: etiology and surgical management. Curr Opin Otolaryngol Head Neck Surg. 2003;11:467–72.
Grillo HC. Surgery of the Trachea and Bronchi. BC Decker; 2004.
Dhasmana A, Singh A, Rawal S. Biomedical grafts for tracheal tissue repairing and regeneration tracheal tissue engineering: an overview. J Tissue Eng Regen Med. 2020;14:653–72.
Chiang T, Pepper V, Best C, Onwuka E, Breuer CK. Clinical translation of tissue Engineered Trachea grafts. Ann Otol Rhinol Laryngol. 2016;125:873–85.
Pepper V, Best CA, Buckley K, Schwartz C, Onwuka E, King N, White A, Dharmadhikari S, Reynolds SD, Johnson J, et al. Factors influencing poor outcomes in synthetic tissue-Engineered Tracheal replacement. Otolaryngol Head Neck Surg. 2019;161:458–67.
Tan ZH, Dharmadhikari S, Liu L, Yu J, Shontz KM, Stack JT, Breuer CK, Reynolds SD, Chiang T. Regeneration of tracheal neotissue in partially decellularized scaffolds. NPJ Regen Med. 2023;8:35.
Wagner DE, Bonvillain RW, Jensen T, Girard ED, Bunnell BA, Finck CM, Hoffman AM, Weiss DJ. Can stem cells be used to generate new lungs? Ex vivo lung bioengineering with decellularized whole lung scaffolds. Respirology. 2013;18:895–911.
Malleske DT, Hayes D Jr., Lallier SW, Hill CL, Reynolds SD. Regulation of human airway epithelial tissue stem cell differentiation by β-Catenin, P300, and CBP. Stem Cells. 2018;36:1905–16.
Mithal A, Emery JL. Squamous metaplasia of the tracheal epithelium in children. Thorax. 1976;31:167–71.
Ghosh M, Helm KM, Smith RW, Giordanengo MS, Li B, Shen H, Reynolds SD. A single cell functions as a tissue-specific stem cell and the in vitro niche-forming cell. Am J Respir Cell Mol Biol. 2011;45:459–69.
Hayflick L, Moorhead PS. The serial cultivation of human diploid cell strains. Exp Cell Res. 1961;25:585–621.
Hayes D Jr., Rayner RE, Hill CL, Alsudayri A, Tadesse M, Lallier SW, Parekh H, Brock GN, Cormet-Boyaka E, Reynolds SD. Airway epithelial stem cell chimerism in cystic fibrosis lung transplant recipients. J Cyst Fibros. 2021;20:165–72.
Ghosh M, Hill CL, Alsudayri A, Lallier SW, Hayes D Jr, Wijeratne S, Tan ZH, Chiang T, Mahoney JE, Carraro G, et al. Repeated injury promotes tracheobronchial tissue stem cell attrition. STEM CELLS Transl Med. 2021;10:1696–713.
Kelly NA, Shontz KM, Bergman M, Manning AM, Reynolds SD, Chiang T. Biobanked tracheal basal cells retain the capacity to differentiate. Laryngoscope Investig Otolaryngol. 2022;7:2119–25.
Reynolds SD, Rios C, Wesolowska-Andersen A, Zhuang Y, Pinter M, Happoldt C, Hill CL, Lallier SW, Cosgrove GP, Solomon GM, et al. Airway progenitor clone formation is enhanced by Y-27632-Dependent changes in the transcriptome. Am J Respir Cell Mol Biol. 2016;55:323–36.
Cole BB, Smith RW, Jenkins KM, Graham BB, Reynolds PR, Reynolds SD. Tracheal basal cells: a facultative progenitor cell pool. Am J Pathol. 2010;177:362–76.
Taswell C. Limiting dilution assays for the determination of immunocompetent cell frequencies. I. Data analysis. J Immunol. 1981;126:1614–9.
O’Callaghan N, Dhillon V, Thomas P, Fenech M. A quantitative real-time PCR method for absolute telomere length. Biotechniques. 2008;44:807–9.
Hsieh AYY, Saberi S, Ajaykumar A, Hukezalie K, Gadawski I, Sattha B, Côté HCF. Optimization of a relative telomere length assay by Monochromatic Multiplex Real-Time quantitative PCR on the LightCycler 480: sources of variability and Quality Control considerations. J Mol Diagn. 2016;18:425–37.
Hayes D Jr., Kopp BT, Hill CL, Lallier SW, Schwartz CM, Tadesse M, Alsudayri A, Reynolds SD. Cell therapy for cystic fibrosis lung disease: regenerative basal cell amplification. Stem Cells Transl Med. 2019;8:225–35.
Griscom NT, Wohl ME. Dimensions of the growing trachea related to age and gender. AJR Am J Roentgenol. 1986;146:233–7.
Fasching CL. Telomere length measurement as a clinical biomarker of aging and disease. Crit Rev Clin Lab Sci. 2018;55:443–65.
Adegunsoye A, Newton CA, Oldham JM, Ley B, Lee CT, Linderholm AL, Chung JH, Garcia N, Zhang D, Vij R, et al. Telomere length associates with chronological age and mortality across racially diverse pulmonary fibrosis cohorts. Nat Commun. 2023;14:1489.
Rock JR, Randell SH, Hogan BL. Airway basal stem cells: a perspective on their roles in epithelial homeostasis and remodeling. Dis Model Mech. 2010;3:545–56.
Davidson LM, Berkelhamer SK. Bronchopulmonary dysplasia: chronic lung disease of infancy and long-term pulmonary outcomes. J Clin Med. 2017;6:4.
Redondo-Sedano J, Antón-Pacheco JL, Valverde RM, Díaz ML, Paredes CL, Guardia LM, Alelu RM, Huerta IJ, Gordo MIB, Fraile AG. Laryngeal stenosis in children: types, grades and treatment strategies. J Pediatr Surg. 2019;54:1933–7.
McKeon F. p63 and the epithelial stem cell: more than status quo? Genes Dev. 2004;18:465–9.
Reynolds SD, Hill CL, Alsudayri A, Lallier SW, Wijeratne S, Tan ZH, Chiang T, Cormet-Boyaka E. Assemblies of JAG1 and JAG2 determine tracheobronchial cell fate in mucosecretory lung disease. JCI Insight. 2022;7:15.
Araya J, Cambier S, Markovics JA, Wolters P, Jablons D, Hill A, Finkbeiner W, Jones K, Broaddus VC, Sheppard D, et al. Squamous metaplasia amplifies pathologic epithelial-mesenchymal interactions in COPD patients. J Clin Invest. 2007;117:3551–62.
Hong Y, Shan S, Gu Y, Huang H, Zhang Q, Han Y, Dong Y, Liu Z, Huang M, Ren T. Malfunction of airway basal stem cells plays a crucial role in pathophysiology of tracheobronchopathia osteoplastica. Nat Commun. 2022;13:1309.
Knaneh-Monem H, Osterbauer B, Hochstim C. Tracheal squamous metaplasia in children with endotracheal intubation or tracheostomy. Int J Pediatr Otorhinolaryngol. 2021;140:110549.
Elliott MJ, Butler CR, Varanou-Jenkins A, Partington L, Carvalho C, Samuel E, Crowley C, Lange P, Hamilton NJ, Hynds RE, et al. Tracheal replacement therapy with a stem cell-seeded graft: lessons from compassionate use application of a GMP-Compliant tissue-Engineered Medicine. Stem Cells Transl Med. 2017;6:1458–64.
Martinod E, Chouahnia K, Radu DM, Joudiou P, Uzunhan Y, Bensidhoum M, Santos Portela AM, Guiraudet P, Peretti M, Destable MD, et al. Feasibility of bioengineered tracheal and bronchial reconstruction using stented aortic matrices. JAMA. 2018;319:2212–22.
Funding
National Institutes of Health, Grant/Award Number: NHLBI R01HL157039.
Author information
Authors and Affiliations
Contributions
LZ; KS; SR and TC wrote the main manuscript. LZ; NK; KM; JC, LM; AM; SR and TC contributed to the main manuscript. JC; LZ; NK; KM; JS; and CH prepared figures and tables. LZ; NK; KM; CH; JS; JC; LM; AM; SR and TC contributed to the data analysis. KM; CH and JS contributed to experimentation. JC; LM; AM; SR and TC served as scientific advisors. All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review boards of two tertiary-level pediatric and adult hospitals (Nationwide Children’s Hospital IRB STUDY00000847, Ohio State University 2021N0027). Pediatric and adult patients undergoing scheduled direct laryngoscopy and bronchoscopy (DLB) were voluntarily recruited. Demographics of the patients recruited were recorded.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, L., Kelly, N., Shontz, K.M. et al. Airway disease decreases the therapeutic potential of epithelial stem cells. Respir Res 25, 28 (2024). https://doi.org/10.1186/s12931-024-02667-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-024-02667-8