Abstract
Rationale
Electronic (e)-cigarettes are popular among youth and cigarette smokers attempting to quit. Studies to date have focused on the utility of e-cigarettes as a smoking cessation tool, but the biological effects are largely unknown.
Objectives
To identify transcriptomic differences in the blood and sputum of e-cigarette users compared to conventional cigarettes smokers and healthy controls and describe biological pathways affected by these tobacco products.
Methods
Cross-sectional analysis of whole blood and sputum RNA-sequencing data from 8 smokers, 9 e-cigarette users (e-cigs) and 4 controls. Weighted gene co-network analysis (WGCNA) identified gene module associations. Ingenuity Pathway Analysis (IPA) identified canonical pathways associated with tobacco products.
Main results
In blood, a three-group comparison showed 16 differentially expressed genes (DEGs); pair-wise comparison showed 7 DEGs between e-cigs and controls, 35 DEGs between smokers and controls, and 13 DEGs between smokers and e-cigs. In sputum, 438 DEGs were in the three-group comparison. In pair-wise comparisons, there were 2 DEGs between e-cigs and controls, 270 DEGs between smokers and controls, and 468 DEGs between smokers and e-cigs. Only 2 genes in the smokers vs. control comparison overlapped between blood and sputum. Most gene modules identified through WGCNA associated with tobacco product exposures also were associated with cotinine and exhaled CO levels. IPA showed more canonical pathways altered by conventional cigarette smoking than by e-cigarette use.
Conclusion
Cigarette smoking and e-cigarette use led to transcriptomic changes in both blood and sputum. However, conventional cigarettes induced much stronger transcriptomic responses in both compartments.
Similar content being viewed by others
Introduction
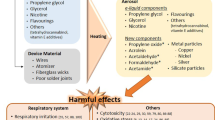
The use of e-cigarettes or “vaping” is popular among adolescents, young adults as well as former and current cigarette smokers [1]. Although e-cigarettes with nicotine are a potential tool for smoking cessation, their effectiveness remains controversial [2], [3]. The benefit of switching from conventional tobacco to e-cigarettes relies on the notion that they are less harmful than combustible cigarettes. Whereas smoke from cigarettes contains 4,000–7,000 chemicals, with many known harmful toxicants and carcinogens, e-cigarette aerosols contain many fewer (50–120) chemicals [4]. Nevertheless, epidemiological studies have linked e-cigarette use with pulmonary diseases known to occur with conventional cigarette smoking, namely bronchitis, COPD, hypersensitivity pneumonitis, eosinophilic pneumonia, lipoid pneumonia, and asthma [5,6,7], and in 2019, the Center for Disease Control and Prevention (CDC) identified a novel disease caused by vaping: e-cigarette or vaping product use-associated lung injury (EVALI) [8]. Beyond our clinical experience, little is known about the effects of e-cigarette use on the respiratory system, particularly when compared to conventional tobacco.
There are several reports from both in vitro and human subject studies showing that exposure to e-cigarette aerosols (commonly referred to as “vapor”) leads to significant changes in gene expression by airway epithelial cells [9,10,11]. However, to our knowledge, there are no reports regarding the effects of e-cigarette use on gene expression in immune cells in human airways. There are scarce reports of gene expression in sputum of healthy smokers, and the most robust, which was funded by the tobacco industry, showed that cigarette smoking alters two biological pathways: (1) the xenobiotic response and oxidative stress; and (2) immune related responses [12]. More recently, a study of inflammatory markers in the sputum of e-cigarette users showed that newer generation e-cigarettes (4th generation) may cause more immunosuppression than prior e-cigarette devices; nevertheless, the effects of e-cigarettes on human airway and systemic immunity remain unclear.
The goals of this work were to identify biological pathways differentially regulated in the blood and sputum of e-cigarette users when compared to cigarette smokers (CS) and healthy controls and to shed light on how exposure to these tobacco products may lead to respiratory diseases. Our primary hypothesis was that these two disparate inhalants would lead to gene expression changes in the sputum and the circulation reflecting homeostatic changes in multiple biological pathways contrasting with those induced by conventional tobacco.
Methods
Human subjects
Sixty-five participants were enrolled between May 1, 2017, and March 1, 2020 (Fig. 1). Inclusion criteria included age 18–55 years old plus exclusive daily use of e-cigarettes or conventional cigarettes for at least one year. Exclusion criteria included use of prescription medications (excluding birth control pills); previously diagnosed pulmonary disease; emergency room visits or hospitalization within the prior year; pregnancy; history of allergic rhinitis/rhinosinusitis, chemical exposure (including dust and wood) or an adverse reaction to albuterol; and current use of cigars, pipes, hookah, chewing tobacco or other tobacco products, marijuana, cocaine, or illicit drugs. We used these stringent criteria to avoid misclassification and residual bias, as older subjects may have greater significant undiagnosed comorbidities, while other noxious exposures, such as viral infections or allergies, could affect the biological pathways similarly to the use of tobacco products. All subjects underwent informed consent. This study was approved by the University of Connecticut Institutional Review Board.
Diagrammatic representation of the study cohort and workflow. A total of 65 participants were enrolled in the study; all underwent exhaled carbon monoxide (eCO) measurement, spirometry, sputum induction with hypertonic saline, and blood draw. Adequate (i.e., with less than 10% squamous cells) sputum samples were obtained from 33 subjects. Good quality RNA (RNA integrity numbers (RIN) > 7) was obtained from 23 samples, which then were matched with whole blood RNAs from the same subjects to comprise our final study cohort. Following RNA-Seq and principal component analysis, additional samples were excluded (see main text and Fig. 2) before in-depth analysis of differentially expressed genes. Only smokers and controls with eCO of < 5 ppm were included in the final analysis
Sputum induction, blood collection and RNA extraction and processing
All 65 participants underwent exhaled carbon monoxide (eCO) measurement, spirometry and sputum induction with hypertonic saline [13]. In brief, subjects were asked to blow their nose and to complete three 7-minute cycles of inhalation of 3%, 4%, and 5% hypertonic sodium chloride delivered by an ultrasonic nebulizer (DeVilbiss®). At the end of each cycle subjects were encouraged to expectorate into a sterile cup; samples were processed within 15 min of collection. Sputum plugs were selected, and then cellular and aqueous compartments were separated using dithiothreitol (DTT) and centrifugation as previously described [13], [14]. Cell viability was determined by trypan blue exclusion. Total cell counts were determined by hemocytometer, and final differentials were performed on Wright-Giemsa stained Cytospin® slides of ≥200 cells 15,16,17,18. Sputum samples with greater than 10% squamous cells were excluded as higher squamous cells concentration may reflect salivary contamination and may impact biomarker measurements [19], [20]. Aqueous phase was aliquoted and stored at -80 °C; cell pellets were stored at -80 °C in RNAlater®. YKL-40, TNF-alpha, interleukin (IL)-6, IL-33, IL-8, IL-10, and IL-13 were measured using the commercially available Magnetic Luminex Assay (R&D Systems Inc., Minneapolis, MN) and Bio-Plex 200 reader (BioRad Laboratories, Hercules, CA). All samples were tested in duplicate as described elsewhere [21]. RNA extraction was performed using the miRNAeasy and RNeasy MinElute kits (Qiagen) according to manufacturer instructions. Phlebotomy was performed and blood underwent automated cell blood count by the clinical laboratory, and RNA extraction and analysis via PAXgene® RNA tubes (BD Biosciences) and PAXgene blood RNA kit (Qiagen).
RNA-Sequencing and qRT-PCR experiments
RNA from sputum and blood was analyzed on an Agilent TapeStation 4200 (Agilent Technologies) using the RNA High Sensitivity assay. Only samples with ribosomal integrity numbers (RIN) values above 7.0 were considered for library preparation. Samples from blood and sputum were processed as one batch respectively. RNA samples were prepared for mRNA-Sequencing by the University of Connecticut Genomic Core Facility (Institute for System Genomics) using the Illumina TruSeq Stranded mRNA Sample Preparation kit, following the manufacturer’s protocol. Samples were combined into one sequencing pool and run as one sample on an Illumina HiSeq 2500 as paired end 100 bp reads. 100 ng of sputum RNA was reversed transcribed to synthesize cDNA to then perform real time PCR using Applied BioSystems 7900HT system as directed by manufacturer. Commercially available primer/probes were used for validation (see Supplemental Table 1). Relative levels of each gene were normalized against four control genes (HPRT, 18s, ACTIN and GAPDH). All sequencing data presented in this publication have been deposited in NCBI’s Gene Expression Omnibus and are accessible through GEO Series accession number GSE223736.
Statistical analysis and bioinformatics approach
Participant characteristics were analyzed using chi-square for categorical variables and non-parametric methods for continuous variables. A two-tail p < 0.05 was considered significant. For differential gene expression an adjusted (Benjamini and Hochberg [BH] method) p-value of ≤ 0.05 was considered significant. Quality control of the fastq files was performed using FASTQC [22]. BBDuk [23] was used to remove hemoglobin contamination from the blood samples. The reads were mapped to gencode.v38 release (GRCh38.p13 Release 38) using Salmon [24]. R version 4.1.2 was used for the statistical analysis [25]. For the analysis of the qRT-PCR we log-transformed and plotted the data as a heatmap using R software pheatmap package (Version 1.0.12). R packages DESeq2 (1.32.0), tximport (1.20.0), Salmon (version 1.5.2) and WGCNA (1.4.1717) 26,27,28,29 were used for quantification and analysis of the RNA-sequencing data. A cut-off of 95% quantile was used to subset the genes for Weighted Gene Co-expression Network Analysis (WGCNA). WGCNA was performed in a signed network and soft thresholds to the similarity matrix with the best power chosen to simulate a scale free network. Three WGCNA were performed using the differentially gene expression of the following three comparisons: (1) E-cigarettes vs. controls, (2) Cigarette vs. controls and (3) Cigarette vs. E-cigarettes. The gene clusters/modules from the WGCNA were further related with the metadata and phenotypical characteristics of interest, including eCO level, cotinine exposure, pulmonary function tests and cell counts in both blood and sputum. Canonical pathways were generated through the use of Ingenuity Pathway Analysis® (IPA) (Qiagen) [30].
Results
Population and biological samples
Study participants
A total of 65 participant were enrolled in our study [18]. Details and demographic characteristics of this entire cohort have been reported elsewhere [13]. Adequate (i.e., less than 10% squamous cells) sputum samples were obtained from 33 subjects. Good quality RNA (RIN ≥ 7) was obtained from 23 samples, which were matched with whole blood RNAs (also RIN ≥ 7) from the same subjects to comprise our final study cohort (Fig. 1). The demographic characteristics of these 23 subjects are presented in Table 1. Nine subjects used e-cigarettes exclusively daily with a median of 2 years, while 8 subjects were exclusive daily conventional smokers with a median of 13 pack-years. There were no significant differences among groups with respect to age, marital status, race, oxygen saturation, or systolic blood pressure. We did not find any significant differences in the selected inflammatory markers (cytokines) measured in the population in both sputum and serum (Supplemental Table 2). As expected, cigarettes smokers (CS) had significantly higher eCO levels when compared to e-cigarette users and controls (Median 11.0 vs. 1.1 and 1.5 ppm respectively [p = 0.004]). All subjects had normal and comparable airflow as measured by spirometry. Serum cotinine and nicotine dependence, assessed using the PENN (E) Cigarette Dependence Index, were similar for e-cigarette users and CS (Median 95.3 vs. 68.2 and 5.0 [p = 0.271] and 15.5 vs. 15.0 [p = 0.532] respectively). Among E-cigarette users, six used 4th generation e-cigarettes, including JUUL®, and all reported using “e-juice” containing nicotine concentrations greater than 10 mg/ml. Menthol and fruity flavors were the most common flavors reported, with four subjects using each (Supplemental Table 3).
Blood sample characteristics
Controls had a lower proportion of circulating neutrophils when compared to CS (60.9 vs. 48.3% [p = 0.028]) and e-cigarette users (60.9 vs. 55.9% [p = 0.043]) but a three-group comparison was not significant (Table 2). There were no other significant differences among other circulating blood cells, total white blood cells (WBCs), platelet count or hemoglobin concentration.
Characteristics of Induced Sputum
Although the amount of sputum produced and processed from healthy controls tended to be lower (Median 80.0 mg) than that from CS (125 mg) and e-cigarette users (130 mg), this was not statistically significant (Table 2). Similarly, there were no differences in total number of cells, viability, or proportion of neutrophils, macrophages, lymphocytes, eosinophils, and bronchial epithelial cells which is consistent with what other studies have reported [31], [32].
RNA-Seq Quality Control
Quality control of the RNA-Seq data was acceptable for all whole blood (hereinafter referred to as blood) samples except from one e-cigarette user, which was removed from further analysis (Fig. 2A). RNA-Seq quality controls showed that all sputum samples were acceptable for further analysis. Surprisingly, principal component analysis showed that two e-cigarette user samples clustered with CS. Although these subjects identified as exclusive e-cigarette users, their eCO levels were greater than 4 ppm (9 and 19 ppm), suggesting in retrospect that they are dual users. Thus, these subject samples were also removed from further transcriptomic analysis (Fig. 2B).
Principal component analysis reveals outliers and dual users. Principal component analysis (PCA) of RNA-Seq data from all (A) blood samples and (C) sputum samples. (A) A single e-cigarette blood sample was deemed as an outlier (black arrow) and excluded from further blood analysis (note this sample was retained in the sputum group). (C) Two sputum samples from e-cigarette users (black arrows) were observed to cluster with samples from smokers. Analysis of exhaled carbon monoxide in these subjects reveled levels of more than 5 ppm, suggesting that they likely were dual e-cigarette and tobacco users. Samples from these subjects were excluded from further analysis for both blood and sputum. PCA plots for (B) blood and (D) sputum following exclusion of outliers and dual users
Transcriptomic differences in blood
Differentially expressed genes in blood
A three-group comparison (Likelihood Ratio Test [LRT]) showed 16 differentially expressed genes (DEGs) (Supplemental Table 4). Eleven genes (RMRP, LCN8, RBPMS2, WASHC1, ZNF703, STON2, IGHV7-4-1, ICAM4, CHRNA2, SAMD14, ATF5) were overexpressed and 5 genes (WDR27, CBSL, RP11-807H22.10, SIX4, HERC2P2) were underexpressed. No specific biological pathways were overrepresented with this set of genes.
DEGs in the blood of E-cigarette users vs. controls
Comparison of e-cigarette users and controls revealed 7 DEGs in blood (Fig. 3A-B, Supplemental Table 4). Three genes (UTS2, IGHG3, and IGLC3) were underexpressed, while 4 (PI4KAP1, RNF112, TG, and IQSEC3) were overexpressed in e-cigarette users. Similar to the above comparison there were no specific biological pathways overrepresented with these genes.
Increased numbers of differentially expressed genes in the blood of cigarettes smokers vs. e-cigarette users. (A) Heatmap showing significant (log2 fold change |≥1 and p≤ 0.005) combined genes from pairwise comparisons in blood (cigarette smokers, Cig; e-cigarette users, E-cigs; and controls, Cont). (B, C and E) Volcano plots of DEGs in blood from pairwise comparisons between (B) e-cigarette users (E-cigs) and controls, (C) cigarette smokers and controls, and (E) cigarette smokers and E-cigarette users (E-cigs). (D) Venn diagram representing the number of DEGs that overlap between each comparison
DEGS in the blood of cigarette smokers vs. controls
In contrast to the e-cigarettes vs. controls, CS had a more robust effect on blood gene expression with 35 DEGs (Supplement Table 4; Fig. 3A C). Three of these (IQSEC3, TG and UTS2) also were differentially expressed in the comparison between e-cigarette users and controls (Fig. 3D). Expression of these genes correlated with the use of tobacco products, with IQSEC3 and TG overexpressed and UTS2 underexpressed in blood of tobacco product users as compared to controls (Fig. 3B-C).
DEGS in the blood of cigarette smokers vs. E-cigarette users
Comparison of CS to e-cigarette users revealed 13 DEGs (see supplemental Tables 4, Fig. 3E). Eight genes were overexpressed (LCN8, RBPMS2, ICAM4, CHRNA2, STON2, WASHC1, EGF, ZNF703) in the blood of CS when compared to e-cigarette users. Zinc Finger Protein 703 (ZNF703) also was overexpressed in CS compared to controls (Fig. 3D). Although no biological pathways were enriched by these genes, in the blood CS had greater transcriptomic changes than e-cigarette users and controls.
Transcriptomic differences in sputum
DEGs in the sputum
Comparison of all 3 groups (LRT) revealed a total of 438 differentially expressed genes (Supplemental Table 4). And similar to the DEG analysis of the blood, these differences were driven mostly by CS.
DEGs in the sputum of E-cigarette users vs. controls
Only 2 genes were differentially expressed (PMEL and TBC1D3F) between e-cigarette users and controls (Fig. 4A-B). PMEL, a gene involved in lymphangioleiomyomatosis (LAM) [33] was underexpressed. TBC1D3F, which is involved on macropinocytosis and tissue repair [34] was overexpressed in the sputum of e-cigarette users.
Increased numbers of differentially expressed genes in the sputum of cigarettes smokers vs. e-cigarette users. (A) Heatmap showing significant (log2 fold change |≥1 and p≤ 0.005) combined genes from pairwise comparisons in sputum (cigarette smokers, Cig; e-cigarette users, E-cigs; and controls, Cont). (B, C and E) Volcano plots of DEGs in sputum from pairwise comparisons between (B) e-cigarette users (E-cigs) and controls, (C) cigarette smokers and controls, and (E) cigarette smokers and E-cigarette users (E-cigs). (D) Venn diagram representing the number of DEGs that overlap between each comparison
DEGs in the sputum of cigarette smokers vs. controls
A total of 270 genes were differentially expressed in the sputum between CS and controls (Fig. 4C and Supplemental Table 4). Interestingly, of these 270 genes, 2 (THBS1 and SPOCD1, (Supplemental Fig. 1 and Supplemental Table 5) were overexpressed in both the blood and sputum of CS compared to controls. There was no overlap with genes differentially expressed between e-cigarette users and controls (Fig. 4D). Overexpressed genes in this set were overrepresented in biological pathways that encompass processes from oxidation reduction, xenobiotic metabolism, to anatomic structure development, while underexpressed genes were enriched for biological pathways involved in the inflammatory and immune response.
DEGs in the sputum of cigarette smokers vs. E-cigarette users
Comparison of CS to e-cigarette users revealed 468 differentially expressed genes in sputum (Fig. 4E and Supplemental Table 4). One hundred and forty-three genes overlapped with genes differentially expressed in the sputum of CS compared with controls (Fig. 4D). Overexpressed genes were overrepresented in biological processes involved mostly in cellular response to stimulus, cell proliferation, tube morphogenesis and oxidative stress, while underexpressed genes were overrepresented in biological pathways associated with the inflammatory and immune response similarly to the comparison between CS and controls.
We compared our findings with published proteomics studies of the sputum of tobacco users [32], [35], [36] (See Supplemental Fig. 2 and Supplemental Table 6). We found the overlap of 23 genes/proteins with those studies. Some of these genes, such as those involved in neutrophil degranulation and antimicrobial humoral response (C3, CLU, B2M, LIZ, CSF1R, and S100A8), response to external stimuli (G6PD, NQO1, and ALDH3A1), and endocytosis (CLU, C3, and B2M), are involved in biological processes affected by exposure to tobacco. We also performed qRT-PCR of selected genes from sputum to validate our findings; results are presented in Supplemental Fig. 3.
WGCNA analysis and IPA
To determine whether specific gene networks were associated with phenotypic features and tobacco product exposure we performed Weighted Gene Correlation Network Analysis (WGCNA) of the blood and sputum. Gene modules that demonstrated association with a relevant trait then were analyzed using IPA.
Blood WGCNA and IPA
Multiple gene modules were associated with clinical traits including pack year history, cotinine concentration, and multiple blood cell population counts (Supplemental Tables 9 and Fig. 5A-C). Serum cotinine was associated with the Turquoise module in both e-cigarette users (R = 0.7, p = 0.01) and CS (R = 0.6, p = 0.05), suggesting that in the blood these genes are affected by nicotine exposure. Two modules were significantly associated to CS when compared to controls (Magenta and Turquoise [R = 0.64 and 0.60, p = 0.03 and 0.04 respectively]) (Fig. 5B). The genes in these modules were enriched in biological pathways associated with xenobiotic metabolism, oxidative stress, and pulmonary healing (Supplemental Table 7).
Weighted gene co-expression network analysis identifies modules and canonical pathways associated with type of tobacco product and clinical traits. (A-E and I) Heatmaps showing WGCNA gene modules associated with phenotypic characteristics, including the type of tobacco product exposure (last column in each heatmap) for pairwise comparison in the blood and sputum. (F-G and J-L) Bar plots highlighting IPA canonical pathways from the gene modules associated with the tobacco product type in sputum for (F-H) cigarettes versus controls and (J-L) e-cigarettes versus cigarettes
One module (Green module R = 0.58, p = 0.05) was associated with e-cigarettes when compared to controls (Fig. 5A) but no significant biological pathways were identified through IPA. (Supplemental Table 7). However, when we compared CS to e-cigarette users, 3 modules were significantly associated with e-cigarette use (Turquoise, Green and Yellow [R = 0.52, -0.49, -0.67 and p = 0.04, 0.05 and 0.02 respectively]) with genes that enriched in several biological pathways including ferroptosis, eNOs, macropinocytsis and EGF signaling, suggesting that those pathways were differently affected by type of tobacco product.
Sputum WGCNA and IPA
Like our analysis of blood samples, multiple gene modules were associated with serum cotinine and eCO suggesting that these gene modules are highly involved in pathways associated to tobacco use (see Fig. 5, Supplemental Tables 8 and 9). When compared to controls, cigarette smoking was associated with 4 gene modules (Magenta, Black, Green-Yellow and Yellow [R = -0.8, 0.75, 0.87 and − 0.77, p = < 0.01, < 0.01, < 0.01 and < 0.01 respectively]). The genes in these modules were overrepresented in biological pathways related to xenobiotic metabolism, oxidative stress response, aryl hydrocarbon receptor (AHR) signaling, coronavirus replication and Th1/Th2 activation (Supplemental Table 8). The comparison between e-cigarettes and controls, showed that one gene module was associated with e-cigarette use (Red [R = -0.54, p-value = 0.05]), with genes involved in the SNARE and synaptogenesis signaling pathways which regulates vesicles fusion and exocytosis, matching other in vitro reports from bronchial epithelial cells [37]. By contrast the comparison between CS and e-cigarettes users in the sputum showed 5 gene modules correlated with type of product use (Black, Magenta, Yellow, Red and Green [R = -0.9, -0.5, 0.77 and 0.49 with p-value = < 0.01, < 0.01, < 0.01, < 0.01 and 0.01 respectively]). Genes from these modules are overrepresented in multiple biological pathways including hepatic fibrosis, xenobiotic response, nicotine degradation, inhibition of metalloproteases, atherosclerosis, and COPD (Supplemental Tables 8 and 9). Suggesting that the type of tobacco product has different effects on these biological processes and how they may lead to disease.
Discussion
The purpose of our study was to characterize transcriptomic changes in the sputum and blood of cigarette smokers compared to e-cigarette users and controls. We discovered that cigarette smoking is the main driver of transcriptomic differences between the three groups, with a much stronger impact in the airways than blood. Gene modules associated with type of tobacco product exposure were highly associated with levels of eCO and/or with cotinine concentration, both of which were highest in smokers. These findings support the overarching conclusion that cigarette smoking is likely to perturb more biological processes than e-cigarettes, however, this does not imply that e-cigarettes are harmless or safer than conventional cigarettes.
In fact, several genes were differentially expressed in blood and sputum of e-cigarette users compared to controls. These transcriptomic changes support the hypothesis that chronic use of e-cigarettes can lead to biologically significant changes and, potentially contribute to pulmonary diseases. For example, one of the two genes differentially expressed in the sputum of e-cigarette users, TBC1D3F, has been implicated in the differentiation of macrophages and vesicle function and trafficking [38], [39] suggesting that vaping may lead to dysfunction of these immune cells in the airways. The other gene (PMEL) encodes for a protein that is highly expressed by cells associated with pulmonary lymphangioleiomyomatosis, a potentially lethal cystic lung disease [33], [40]. Furthermore, PMEL is a component of the melanosome, a type of lysosome-related organelle that is dysfunctional in patients with Hermansky-Pudlak, an inherited fibrotic pulmonary disease [41]. However, it is unknown as to how changes in the expression of PMEL may influence pulmonary disease development secondary to e-cigarette exposure.
Our study also showed that two genes (SPOCD1 and THBS1) were differentially overexpressed in sputum and blood among CS when compared to controls. SPOCD1 has been implicated in pi-RNA-directed DNA methylation, with at least two prior studies linking it with smoke exposure 42,43,44, and THBS1 is an integral component of the extracellular matrix where it regulates cell migration, cytoskeletal organization, cell proliferation and apoptosis, and plays a role in the regulation of inflammation and modulation of reactive oxygen species [45], [46]. Changes in DNA-methylation and expression of THBS1 have been associated with atherosclerosis and cancer among smokers, while other reports have linked overexpression of THBS1 with higher lung cancer survival [47], [48]. Taken together, these genes may aid our understanding of how cigarette smoking can lead to systemic disease from its effects in the respiratory system.
Our findings in sputum resemble those reported by others demonstrating that smoking cigarettes induces a xenobiotic and oxidative stress response and activation of immune-related genes [35], [36]. However, in contrast with data from shotgun proteomics of sputum [32], we did not see evidence of an altered innate immune response or dysfunctional neutrophils in the sputum of e-cigarette users. Furthermore, our analytical approach allowed us to detect misclassification bias and, using only transcriptomics, we were able to distinguish exclusive e-cigarette users from likely dual users or subjects exposed to smoke. Two other strengths of our study are that only high-quality specimens were used for RNA sequencing as RNA degradation could significantly impact RNA-seq analysis [49], and we recruited subjects with no known history of significant comorbidities, including atopy or asthma. Our subjects also underwent spirometry that confirmed normal air flow with no evidence of obstructive pulmonary disease. A recent study also demonstrated that exposure to e-cigarettes affects the immune homeostasis of the respiratory airways and that this is altered by the generation of e-cigarette [31]. A significant difference with that report is our exclusion of sputum samples with greater than 10% squamous cells. Furthermore, the majority of our study participants (66%) were users of fourth generation e-cigarette devices which reflects the current trends of e-cigarette use in the US [50], [51].
Our findings in the blood are similar to those reported by Tommasi et al., in that cigarette smoking induced more transcriptomic changes in blood leukocytes than vaping, although we did not find a dysregulation of mitochondria-specific genes as reported in their study perhaps due to differences in the cell composition studied (PBMCs vs. whole blood) [52]. Our study shows that cigarette smoking generates a greater transcriptomic response in the respiratory system and in blood than e-cigarettes. However, further studies are necessary to better characterize the long-term clinical significance of these gene expression differences to properly support the use of e-cigarettes as a viable harm reduction strategy for cigarette smokers.
Our study does have limitations, including the relatively small sample size. This was associated with the COVID-19 pandemic hindering recruitment of subjects for a study in which nebulized saline was used for sputum induction and concerns of aerosolization of viral particles. This limitation affects our ability to perform subgroup analysis based on e-cigarette brands, type of device (or generation), nicotine concentration or flavors. Furthermore, we did not collect the time of last use of the tobacco product, but we assume that our results reflect a steady state in the airways and blood as one would expect in chronic tobacco use as subjects reported daily use of their tobacco product for at least one year. In addition, since we are analyzing bulk RNA-Seq on samples with a complex cellular composition, lowly expressed transcripts or highly expressed transcripts in low prevalence cells may have been missed. We did not collect data on secondhand smoke exposure either, which could potentially affect our findings. Indeed, one healthy control had elevated cotinine serum levels (but a normal eCO level), although this is not necessarily proof of tobacco exposure [53], [54]. Nonetheless, our results are valuable as they provide early evidence of specific transcripts in the airways and the blood associated with e-cigarette use in contrast to cigarette smoking.
In summary, cigarette smoking and e-cigarette vaping led to significant transcriptomic changes in the airways and the blood of their users. This transcriptomic impact is higher among CS than e-cigarette users. Some of the transcriptomic changes among e-cigarette users are associated with vesicle trafficking and macropynocitosis, biological functions that are fundamental for proper macrophage function and airway immune response. More research is urgently needed to better characterize the long-term effects of these transcriptomic changes in relationship to tobacco product use.
Data Availability
The database generated for this study is available by request. For inquiries, please email corresponding author.
References
Mayer M, Reyes-Guzman C, Grana R, Choi K, Freedman ND. Demographic characteristics, cigarette smoking, and e-Cigarette Use among US adults. JAMA Netw Open. 2020;3(10):e2020694–4. https://doi.org/10.1001/jamanetworkopen.2020.20694.
Hartmann-Boyce J, McRobbie H, Lindson N, et al. Electronic cigarettes for smoking cessation. Cochrane Database of Systematic Reviews. 2021;410.1002/14651858.CD010216.pub5.
Chen R, Pierce JP, Leas EC, et al. Effectiveness of e-cigarettes as aids for smoking cessation: evidence from the PATH study cohort, 2017–2019. Tob Control. 2022;tobaccocontrol–2021. https://doi.org/10.1136/tobaccocontrol-2021-056901.
Goniewicz ML, Knysak J, Gawron M, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control 2014/03//. 2014;23(2):133–9. https://doi.org/10.1136/tobaccocontrol-2012-050859.
Perez MF, Atuegwu NC, Oncken C, Mead EL, Mortensen EM. Association between electronic cigarette use and asthma in never-smokers. Ann Am Thorac Soc Nov. 2019;16(11):1453–6. https://doi.org/10.1513/AnnalsATS.201904-338RL.
Perez MF, Atuegwu NC, Mead EL, Oncken C, Mortensen EM. Adult E-Cigarettes use Associated with a self-reported diagnosis of COPD. Int J Environ Res Public Health Oct. 2019;16(20). https://doi.org/10.3390/ijerph16203938.
Bhatta DN, Glantz SA. Association of E-Cigarette Use with respiratory disease among adults: a longitudinal analysis. Am J Prev Med Feb. 2020;58(2):182–90. https://doi.org/10.1016/j.amepre.2019.07.028.
Perrine CG, Pickens CM, Boehmer TK, et al. Characteristics of a Multistate Outbreak of Lung Injury Associated with E-cigarette Use, or Vaping - United States, 2019. MMWR Morb Mortal Wkly Rep Oct. 2019;4(39):860–4. https://doi.org/10.15585/mmwr.mm6839e1.
Martin EM, Clapp PW, Rebuli ME, et al. E-cigarette use results in suppression of immune and inflammatory-response genes in nasal epithelial cells similar to cigarette smoke. Am J Physiol Lung Cell Mol Physiol 2016/07//. 2016;311(1):L135–44. https://doi.org/10.1152/ajplung.00170.2016.
Herr C, Tsitouras K, Niederstrasser J, et al. Cigarette smoke and electronic cigarettes differentially activate bronchial epithelial cells. Respir Res Mar. 2020;12(1):67. https://doi.org/10.1186/s12931-020-1317-2.
Corbett SE, Nitzberg M, Moses E, et al. Gene expression alterations in the bronchial epithelium of e-Cigarette users. Chest. 2019;156(4):764–73. https://doi.org/10.1016/j.chest.2019.05.022.
Titz B, Sewer A, Schneider T et al. Alterations in the sputum proteome and transcriptome in smokers and early-stage COPD subjects. Journal of Proteomics. 2015/10/14/ 2015;128:306–320. https://doi.org/10.1016/j.jprot.2015.08.009.
Perez MF, Atuegwu NC, Mortensen EM, Oncken C. The inflammatory biomarker YKL-40 is elevated in the serum, but not the sputum, of E-cigarette users. Exp Lung Res Feb-Mar. 2021;47(2):55–66. https://doi.org/10.1080/01902148.2020.1847216.
Weiszhar Z, Horvath I. Induced sputum analysis: step by step. Breathe. 2013-06-01 00:00:00 2013;9(4):300–306. https://doi.org/10.1183/20734735.042912.
Pizzichini E, Pizzichini MM, Kidney JC, et al. Induced sputum, bronchoalveolar lavage and blood from mild asthmatics: inflammatory cells, lymphocyte subsets and soluble markers compared. Eur Respir J Apr. 1998;11(4):828–34.
Yan X, Chu JH, Gomez J, et al. Noninvasive analysis of the sputum transcriptome discriminates clinical phenotypes of asthma. Am J Respir Crit Care Med May. 2015;15(10):1116–25. https://doi.org/10.1164/rccm.201408-1440OC.
Strober W. Trypan Blue Exclusion Test of Cell Viability. Curr Protoc Immunol. Nov 2 2015;111:A3 B 1–3. https://doi.org/10.1002/0471142735.ima03bs111.
An Atlas of Induced Sputum. An aid for research and diagnosis. Encyclopedia of Visual Medicine Series. 1st ed. Informa Healthcare; 2003.
Pedersen F, Trinkmann F, Abdo M, et al. Influence of cell quality on inflammatory biomarkers in COPD Sputum Supernatant. Int J Chron Obstruct Pulmon Dis. 2021;16:487–93. https://doi.org/10.2147/copd.S284938.
Hamid Q, Kelly MM, Linden M, et al. Methods of sputum processing for cell counts, immunocytochemistry and < em > in situ hybridisation. Eur Respir J. 2002;20(37 suppl):19s–23s. https://doi.org/10.1183/09031936.02.00001902.
Perez MF, Atuegwu NC, Mortensen EM, Oncken C. The inflammatory biomarker YKL-40 is elevated in the serum, but not the sputum, of E-cigarette users. Exp Lung Res. 2020;1–12. https://doi.org/10.1080/01902148.2020.1847216.
Andres S, FastQC:. A Quality Control Tool for High Throughput Sequence Data [Online]. Accessed 07/12, 2021. http://www.bioinformatics.babraham.ac.uk/projects/fastqc/.
JGI DoE, BBTools. Accessed 07/12, 2021. https://jgi.doe.gov/data-and-tools/bbtools/.
Patro R, Duggal G, Love MI, Irizarry RA, Kingsford C. Salmon provides fast and bias-aware quantification of transcript expression. Nat Methods. 2017;14(4):417–9. https://doi.org/10.1038/nmeth.4197.
R: A language and environment for statistical computing. R Foundation for Statistical Computing. ; 2021. https://www.R-project.org/.
R: A language and environment for statistical computing. 2020. https://www.R-project.org.
Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15(12). https://doi.org/10.1186/s13059-014-0550-8.
Soneson C, Love MI, Robinson MD. Differential analyses for RNA-seq: transcript-level estimates improve gene-level inferences. F1000Research. 2016;4:1521. https://doi.org/10.12688/f1000research.7563.2.
Langfelder P, Horvath S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinformatics. 2008;9(1):559. https://doi.org/10.1186/1471-2105-9-559. 12/29 2008.
Krämer A, Green J, Pollard J, Tugendreich S. Causal analysis approaches in Ingenuity Pathway Analysis. Bioinformatics. 2014;30(4):523–30. https://doi.org/10.1093/bioinformatics/btt703.
Hickman E, Payton A, Duffney P, et al. Biomarkers of Airway Immune Homeostasis Differ significantly with generation of E-Cigarettes. Am J Respir Crit Care Med Nov. 2022;15(10):1248–58. https://doi.org/10.1164/rccm.202202-0373OC.
Reidel B, Radicioni G, Clapp P, et al. E-Cigarette Use causes a unique innate Immune response in the lung involving increased neutrophilic activation and altered mucin secretion. Am J Respir Crit Care Med Oct. 2017;20. https://doi.org/10.1164/rccm.201708-1590OC.
Guo M, Yu JJ, Perl AK, et al. Single-cell transcriptomic analysis identifies a unique pulmonary lymphangioleiomyomatosis cell. Am J Respir Crit Care Med Nov. 2020;15(10):1373–87. https://doi.org/10.1164/rccm.201912-2445OC.
Qin S, Dorschner RA, Masini I, et al. TBC1D3 regulates the payload and biological activity of extracellular vesicles that mediate tissue repair. Faseb j May. 2019;33(5):6129–39. https://doi.org/10.1096/fj.201802388R.
Titz B, Sewer A, Schneider T, et al. Alterations in the sputum proteome and transcriptome in smokers and early-stage COPD subjects. J Proteom Oct. 2015;14:128:306–20. https://doi.org/10.1016/j.jprot.2015.08.009.
Takahashi K, Pavlidis S, Ng Kee Kwong F, et al. Sputum proteomics and airway cell transcripts of current and ex-smokers with severe asthma in U-BIOPRED: an exploratory analysis. Eur Respir J. 2018;51(5):1702173. https://doi.org/10.1183/13993003.02173-2017.
Ghosh A, Coakley RC, Mascenik T, et al. Chronic E-Cigarette exposure alters the human bronchial epithelial proteome. Am J Respir Crit Care Med Jul. 2018;1(1):67–76. https://doi.org/10.1164/rccm.201710-2033OC.
Qin S, Dorschner RA, Masini I, et al. TBC1D3 regulates the payload and biological activity of extracellular vesicles that mediate tissue repair. FASEB J. 2019;33(5):6129–39. https://doi.org/10.1096/fj.201802388R.
Leung CCT, Wong CKC. Characterization of stanniocalcin-1 expression in macrophage differentiation. Transl Oncol Jan. 2021;14(1):100881. https://doi.org/10.1016/j.tranon.2020.100881.
Matsumoto Y, Horiba K, Usuki J, Chu SC, Ferrans VJ, Moss J. Markers of cell proliferation and expression of melanosomal antigen in lymphangioleiomyomatosis. Am J Respir Cell Mol Biol Sep. 1999;21(3):327–36. https://doi.org/10.1165/ajrcmb.21.3.3693.
Nguyen T, Wei ML. Characterization of Melanosomes in Murine Hermansky–Pudlak Syndrome: Mechanisms of Hypopigmentation. Journal of Investigative Dermatology. 2004/02/01/ 2004;122(2):452–460. https://doi.org/10.1046/j.0022-202X.2004.22117.x.
Zoch A, Auchynnikava T, Berrens RV, et al. SPOCD1 is an essential executor of piRNA-directed de novo DNA methylation. Nature. 2020;584(7822):635–9. https://doi.org/10.1038/s41586-020-2557-5. /08/01 2020.
Gupta A, Sasse SK, Gruca MA, Sanford L, Dowell RD, Gerber AN. Deconvolution of multiplexed transcriptional responses to wood smoke particles defines rapid aryl hydrocarbon receptor signaling dynamics. J Biol Chem Oct. 2021;297(4):101147. https://doi.org/10.1016/j.jbc.2021.101147.
Otto JM, Gizer IR, Ellingson JM, Wilhelmsen KC. Genetic variation in the exome: Associations with alcohol and tobacco co-use. Psychol Addict Behav. 2017;31(3):354–66. https://doi.org/10.1037/adb0000270.
Kale A, Rogers NM, Ghimire K. Thrombospondin-1 CD47 signalling: from mechanisms to Medicine. Int J Mol Sci. 2021;22(8):4062.
Adams JC, Lawler J. The thrombospondins. The International Journal of Biochemistry & Cell Biology. 2004/06/01/ 2004;36(6):961–968. https://doi.org/10.1016/j.biocel.2004.01.004.
Sayols-Baixeras S, Lluís-Ganella C, Subirana I et al. Identification of a new locus and validation of previously reported loci showing differential methylation associated with smoking. The REGICOR study. Epigenetics. 2015/12/02 2015;10(12):1156–65. https://doi.org/10.1080/15592294.2015.1115175.
Weng T-Y, Wang C-Y, Hung Y-H, Chen W-C, Chen Y-L, Lai M-D. Differential expression pattern of THBS1 and THBS2 in Lung Cancer: clinical outcome and a systematic-analysis of microarray databases. PLoS ONE. 2016;11(8):e0161007–7. https://doi.org/10.1371/journal.pone.0161007.
Gallego Romero I, Pai AA, Tung J, Gilad Y. RNA-seq: impact of RNA degradation on transcript quantification. BMC Biology 2014/05/30. 2014;12(1):42. https://doi.org/10.1186/1741-7007-12-42.
Cooper M, Park-Lee E, Ren C, Cornelius M, Jamal A, Cullen KA. Notes from the Field: E-cigarette Use among Middle and High School Students - United States, 2022. MMWR Morb Mortal Wkly Rep Oct. 2022;7(40):1283–5. https://doi.org/10.15585/mmwr.mm7140a3.
Barrington-Trimis JL, Gibson LA, Halpern-Felsher B, et al. Type of E-Cigarette device used among adolescents and young adults: findings from a pooled analysis of eight studies of 2166 Vapers. Nicotine Tob Res. 2017;20(2):271–4. https://doi.org/10.1093/ntr/ntx069.
Tommasi S, Pabustan N, Li M, Chen Y, Siegmund KD, Besaratinia A. A novel role for vaping in mitochondrial gene dysregulation and inflammation fundamental to disease development. Sci Rep. 2021/11/23 2021;11(1):22773. https://doi.org/10.1038/s41598-021-01965-1.
Jacob P, St Helen G, Yu L, et al. Biomarkers of exposure for dual use of electronic cigarettes and combustible cigarettes: Nicotelline, NNAL, and total nicotine equivalents. Nicotine Tob Res Jun. 2020;12(7):1107–13. https://doi.org/10.1093/ntr/ntz235.
Davis RA, Stiles MF, deBethizy JD, Reynolds JH. Dietary nicotine: a source of urinary cotinine. Food Chem Toxicol Dec. 1991;29(12):821–7. https://doi.org/10.1016/0278-6915(91)90109-k.
Acknowledgements
The authors want to thank Dr. Justin Radolf for his kind support and significant amount of time discussing, reading, and editing the manuscript.
Funding
(1) Scholars in Medicine – seed grant, Department of Medicine, University of Connecticut. (2) Seed grant Institute for Systems Genomics. (3) Clinical Research Center, University of Connecticut. (4) PRIDE – AIRE, NHLBI small project grant. (5) R01 CA207491 Minority Supplement. (6) NIH NHLBI K24 HL155884 (LCA). (7) NIH NIAID R01 AI141609.
Author information
Authors and Affiliations
Contributions
Study design: MFP, LCA, AW. Data Collection: MFP, EMM. Methodology: MFP, EMM, MY, SP. Data Analysis: MFP, MY, SP, AW. Visualization: MFP, MY, SP, AW. Drafting of the Manuscript: MFP, EMM, LCA, AW. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the University of Connecticut Institutional Review Board (17-045-2). All participants provided written consent.
Consent for publication
Not Applicable.
Competing interests
The authors report no conflict of interest or competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Fig. 1.
Overlap of differentially expressed genes in blood and sputum of smokers. Venn diagram of differentially expressed genes in blood and sputum of cigarette smokers when compared to controls. [https://doi.org/10.6084/m9.figshare.19878268 under embargo, private link: https://figshare.com/s/778ecc2fce40553bfdb1]. Supplemental Fig. 2. Overlap with published proteomics data from sputum of healthy users exposed to different tobacco products. We compared DEGs from all comparisons (p < 0.05) from our data (RNA) with published significantly different proteins from the sputum of healthy e-cigarette (E-Cigs) or healthy cigarette (Cig) users. A total of 23 genes/proteins overlapped with other publications, 12 with reports from E-cigarette users and 19 from smokers. Supplemental Figure 3. qRT-PCR of selected genes in sputum. Relative levels of each gene were normalized against four control genes (HPRT, 18s, ACTIN and GAPDH). ANOVA was use to compare all three groups and Dunnett’s test was used to test pair comparisons. *=p < 0.05, **=p < 0.01, ***=p < 0.001. A. Data were log10 transformed and plotted as a heatmap. B. Presented as the relative fold change when compared to the four control genes. Supplemental Fig. 4. Weighted gene co-expression network analysis gene modules associated with tobacco product type. (A-E) heatmaps of genes present in sputum WGCNA modules significantly associated with tobacco product type (e-cigarettes versus cigarettes). [https://doi.org/10.6084/m9.figshare.19878268 under embargo, private link: https://figshare.com/s/778ecc2fce40553bfdb1]
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Perez, M.F., Yurieva, M., Poddutoori, S. et al. Transcriptomic responses in the blood and sputum of cigarette smokers compared to e-cigarette vapers. Respir Res 24, 134 (2023). https://doi.org/10.1186/s12931-023-02438-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-023-02438-x