Abstract
Background
Although high-frequency percussive ventilation (HFPV) improves gas exchange, concerns remain about tissue overdistension caused by the oscillations and consequent lung damage. We compared a modified percussive ventilation modality created by superimposing high-frequency oscillations to the conventional ventilation waveform during expiration only (eHFPV) with conventional mechanical ventilation (CMV) and standard HFPV.
Methods
Hypoxia and hypercapnia were induced by decreasing the frequency of CMV in New Zealand White rabbits (n = 10). Following steady-state CMV periods, percussive modalities with oscillations randomly introduced to the entire breathing cycle (HFPV) or to the expiratory phase alone (eHFPV) with varying amplitudes (2 or 4 cmH2O) and frequencies were used (5 or 10 Hz). The arterial partial pressures of oxygen (PaO2) and carbon dioxide (PaCO2) were determined. Volumetric capnography was used to evaluate the ventilation dead space fraction, phase 2 slope, and minute elimination of CO2. Respiratory mechanics were characterized by forced oscillations.
Results
The use of eHFPV with 5 Hz superimposed oscillation frequency and an amplitude of 4 cmH2O enhanced gas exchange similar to those observed after HFPV. These improvements in PaO2 (47.3 ± 5.5 vs. 58.6 ± 7.2 mmHg) and PaCO2 (54.7 ± 2.3 vs. 50.1 ± 2.9 mmHg) were associated with lower ventilation dead space and capnogram phase 2 slope, as well as enhanced minute CO2 elimination without altering respiratory mechanics.
Conclusions
These findings demonstrated improved gas exchange using eHFPV as a novel mechanical ventilation modality that combines the benefits of conventional and small-amplitude high-frequency oscillatory ventilation, owing to improved longitudinal gas transport rather than increased lung surface area available for gas exchange.
Similar content being viewed by others
Background
Under general anesthesia and in critically ill patients, intermittent positive pressure ventilation is applied regularly to guarantee oxygen supply and promote carbon dioxide elimination. While maintaining physiologic lung ventilation in patients with healthy lungs is feasible, various pulmonary disorders pose challenges to health care professionals to guarantee adequate gas exchange during invasive ventilatory support. Particularly, diseases with decreased functional residual capacity and/or decreased lung compliance observed in obese patients [1, 2] or in those with acute respiratory distress syndrome (ARDS) [3, 4] require continuous adjustment of the ventilation strategy to maintain appropriate gas exchange. Furthermore, gas exchange abnormalities during mechanical ventilation have been seen in clinical situations associated with significant lung restriction and impaired gas exchange, such as during laparoscopic surgery in patients with capnoperitoneum [5, 6] or bariatric surgery [7].
Despite significant advancements in respiratory management, these increasingly common medical disorders continue to place a strain on healthcare systems by increasing the incidence of perioperative respiratory complications [8]. As a result, there is an urgent need to enhance ventilation support modalities without posing additional stress and strain on lung tissues. To enhance gas exchange, high-frequency percussive ventilation (HFPV) based on a combination of conventional and high-frequency oscillatory ventilation has been proposed [9] and applied subsequently in experimental and clinical studies [10,11,12,13,14,15]. This modality combines the benefits of conventional tidal expansions to maintain the lung open with high-frequency fluctuations facilitating axial gas mixing [16] and alveolar recruitment [12]. Despite improved gas exchange, superimposing the high-frequency component on conventional ventilation during inspiration results in higher peak pressures and tissues overdistension or lower tidal volumes in pressure control mode. Thus, the net benefit of this modality has been challenged [17, 18].
We hypothesize that using the high-frequency component during the expiration phase merely preserves the advantage of percussive ventilation without raising the peak inspiratory pressure and the combination of frequencies can reduce dynamic parenchymal strain and mechanical power [19,20,21], so preserving the lung from excessive stress. We contrasted this novel expiratory high-frequency percussive ventilation (eHFPV) with the whole-cycle HFPV and conventional mechanical ventilation to test this hypothesis. We aimed at assessing whether this eHFPV improved oxygen delivery and carbon dioxide (CO2) clearance in an experimental model of induced hypoxia and hypercapnia. Simulation research was also conducted to evaluate the effects of lung size on the oscillatory pressure transmission from the airway opening to the alveolar compartment in order to determine the extent to which our findings may be extended to other species.
Methods
Ethical considerations
This study was approved by the National Food Chain Safety and Animal Health Directorate of Csongrád County, Hungary (No. XXXII/149/2020) on March 10, 2020. The procedures were implemented in compliance with the guidelines of the Scientific Committee of Animal Experimentation of the Hungarian Academy of Sciences (updated Law and Regulations on Animal Protection: 40/2013. [II. 14.], the Government of Hungary), and European Union Directive 2010/63/EU on the protection of animals used for scientific purposes. The results were reported in line with the Animal Research Reporting of In Vivo Experiments (ARRIVE) guidelines.
Animal preparation
Male New Zealand White rabbits (n = 10, weight: 2.0–2.5 kg) were sedated with an intramuscular injection of xylazine (5 mg/kg, CP-Xylazine; CP-Pharma, Burgdorf, Germany). An ear vein was cannulated with a 24-gage catheter (Abbocath, Abbott Medical, Baar/Zug, Switzerland) for drug delivery. Anesthesia was then induced and maintained through continuous intravenous infusions of propofol (10 mg/kg/h), fentanyl (5 µg/kg/h), and midazolam (0.2 mg/kg/h). Tracheotomy was performed under local anesthesia (subcutaneous injection of 0.5% lidocaine), and a 3.5-mm ID and 7-cm long uncuffed tube (Portex; Smiths Medical, Kent, UK) was inserted into the trachea. Rabbits were connected to a custom-made blower-driven ventilator and ventilated with room air (ventilation frequency, 20–25/min; tidal volume, 7 ml/kg; positive end-expiratory pressure [PEEP], 3 cmH2O; inspiratory-to-expiratory ratio, 1:2). A femoral artery and femoral vein were catheterized for drug delivery, blood sample collection, and blood pressure monitoring. After ensuring appropriate anesthesia depth, neuromuscular blockade was maintained via continuous infusion of atracurium (0.6 mg/kg/h, Tracrium; Aspen Pharma, Dublin, Ireland). The mean arterial pressure, heart rate, and electrocardiogram were monitored continuously during the experiment. A rectal probe was applied to monitor the body temperature, which was maintained at 38 °C–39 °C using a thermostatic heating pad (Harvard Apparatus, South Natick, MA, USA).
Performing mechanical ventilation
The custom-made blower-driven ventilator was tailored to suit the delivery of the driving pressure in the conventional pressure control mode, as it allowed superposition of the high-frequency signals over the conventional pressure excursions in a controlled manner (Fig. 1). The required changes in the airway pressure pattern during the different mechanical ventilation modalities were generated by controlling the rotation speed of the blower with custom-made software. During conventional mechanical ventilation, the constant rotation speed of the blower was altered periodically to provide the required RR and VT. When HFPV or eHFPV were applied, the rotation speed of the blower was modulated by adding the frequency of the oscillatory component required in order to deliver these complex pressure waveforms.
Scheme of the experimental setup. A custom-made blower-driven ventilator was used to deliver the driving pressure during conventional pressure-controlled ventilation, and it also allowed superposition of the high-frequency signals over the conventional pressure excursions. The rotation speed of the blower was controlled by a custom-made software to deliver the changes in the airway pressure required for the different mechanical ventilation modalities. Volumetric capnograms were recorded by using a mainstream CO2 sensor in series with a screen pneumotachograph (PTG)
Blood gas analyses
For blood gas analyses, 0.1 ml of arterial blood samples were collected under each experimental condition. Partial pressures of oxygen (PaO2) and CO2 (PaCO2) along with oxygen saturation (SaO2) were measured by using a point-of-care blood analyzer system (Epoc Reader and Host; Epocal, Inc., Ottawa, ON, Canada).
Volumetric capnography
Intra-tidal changes in the CO2 concentration were measured with a pediatric mainstream sensor connected to a data acquisition unit (Capnogard®; Novametrix, Andover, MA, USA). Central airflow was sensed by a screen pneumotachograph (11-mm ID, PNT3500; Hans Rudolph, Inc., Shawnee, KS, USA) that was connected to a differential pressure transducer (model 24PCEFA6D; Honeywell, Charlotte, NC, USA). Both the signals were digitized at a sampling rate of 256 Hz and then analyzed with a custom-made software. Volumetric capnogram curves were generated from the intra-tidal changes in CO2 concentration and the volume signals derived by integration of the airflow data were simultaneously recorded.
The inflection point of phase 2 was localized as the maximum of the first derivative of the volumetric capnogram curve. The maximum of the third derivatives of the capnogram before and after this inflection point were identified, and this range was considered as a capnogram phase 2 [22], which reflects mixed emptying of the airway-alveolar spaces. Phase 3 of the capnogram curves, which represents the expiration of the alveolar gas compartment, was defined as the range from the end of phase 2 until the end of expiration. Capnogram phase 2 slope (S2V) was derived by fitting a linear regression line to 5 points around the inflection point. Fowler’s anatomic dead space (VDF) was defined as the gas volume expired until the inflection point in phase 2 [23]. CO2 volume eliminated in a minute (V’CO2) was calculated as the product of expired CO2 within a breathing cycle (VCO2) and the ventilation frequency. VCO2 was obtained by integrating the expiratory phases of the volumetric capnogram curve within each ventilation cycle. Since the application of the HFPV and eHFPV caused substantial fluctuation in phase 3 of the capnogram (e.g., Fig. 3), the shape factors and dead space parameters related to this segment were significantly biased and not extracted accordingly.
Ventilation monitoring
The pressure signal at the airway opening was recorded during the entire ventilation period. Tidal volume (VT), and minimum (Pmin), maximum (Pmax), and mean airway pressures (Pmean) were derived from these signals under steady-state conditions.
Measurement of respiratory mechanics
The forced oscillatory measurement of airway and respiratory tissue mechanics have been detailed previously [24]. Briefly, the custom-made blower-driven ventilator generated a small-amplitude (less than ± 1 cmH2O) pseudo-random signal containing 23 sinusoidal components ranging from 0.5 to 20.75 Hz during short apneic periods (8 s) that was interposed into the mechanical ventilation. Oscillatory airflow was measured with a screen pneumotachograph (11-mm ID, PNT3500; Hans Rudolph, Inc.) connected to a differential pressure transducer (model 24PCEFA6D; Honeywell), and tracheal pressure (Ptr) was sensed with an identical pressure transducer relative to the atmosphere. The input impedance spectra of the respiratory system (Zrs) were calculated as Zrs = P/V′. The input impedance of the tracheal tube and the connections also were measured with applying a reduced oscillatory amplitude in the open circuit that corresponds to the oscillatory amplitude employed in vivo, and the value obtained was subtracted from the Zrs spectra before further analyses.
The mechanical properties of the airways and respiratory tissues were determined by model fitting through minimizing of the weighted difference in the measured and modeled spectra. The well-validated model [25] contained a frequency-independent airway resistance (Raw) and inertance connected in series to a constant-phase tissue compartment incorporating damping (G) and elastance (H) parameters [26]. Since the frequency-independent resistive component of the chest wall is negligible in rabbits [27], the parameter Raw mainly represents the flow resistance of the conducting airways. Parameters G and H signify the resistive (i.e., damping or energy loss) and elastic (i.e., stiffness) characteristics of the respiratory tissues.
Simulation study to model pressure transmission
A simulation study using a lumped-element model of the respiratory system was performed to estimate how the lung size affects the transmission ratio of the high-frequency oscillatory pressures from the airway opening (Pao) to the alveoli (Palv). The details and results of the simulation are provided in Additional file 1.
Experimental protocol
The scheme of the experimental protocol is demonstrated in Fig. 2. Hyperinflation was performed before initiating the protocol to standardize the volume history by maintaining an airway pressure of 25 cmH2O for 5 s. The animals were initially ventilated by conventional pressure-controlled ventilation (CMV). Normocapnia was maintained in phase 1 of the protocol by maintaining CMV, and the measurements were performed by analyzing blood gas, recording the volumetric capnogram and ventilation curves, and collecting forced oscillatory data epochs. To assess the ability of the novel ventilation strategy toward improving gas exchange, hypoxia and hypercapnia were induced by decreasing the ventilation frequency so as to attain a target PaCO2 of 53–56 mmHg during conventional ventilation. After establishing stable ventilation and hemodynamic conditions, another data set for blood gas, volumetric capnography, ventilation, and forced oscillations was collected while CMV was maintained (CMV1). Percussive ventilation modes were then initiated by randomly setting the oscillatory amplitude (2 or 4 cmH2O) or frequency (5 or 10 Hz) added either to the entire breathing cycle (HFPV) or to the expiratory phase alone (eHFPV). A 5-min period was allowed for the ventilation to reach a steady-state condition, and another set of data was collected under CMV and identical percussive ventilation to that of the earlier phase of the protocol. This randomized sequence was continued during the maintenance of hypercapnia until all percussive ventilation settings with amplitudes of 2 and 4 cmH2O and frequencies of 5 and 10 Hz were completed for both HFPV and eHFPV.
Experimental protocol scheme. Measurements were initially made under normocapnic conditions (baseline) and continued during the maintenance of hypoxia and hypercapnia by decreasing the ventilation frequency. Four sequences including a high-frequency percussive ventilation (HFPV) and an expiratory high-frequency percussive ventilation (eHFPV), each preceded by a conventional mechanical ventilation (CMV), was then performed. Both HFPV and eHFPV were applied by randomly setting the oscillatory amplitude (2 or 4 cmH2O) and the oscillatory frequency (5 or 10 Hz). BG: blood gas; Vcap: volumetric capnography; Vent: recording the mechanical ventilation pressure/volume parameters; FOT: forced oscillations
Statistical analysis
The scatter of the values of the measured variables was presented as half-width of the 95% confidence interval. Blood gas, capnographic, and ventilation variables were compared by 2-way repeated measures analyses of variance with ventilation mode (CMV, HFPV, and eHFPV) and experimental stages (amplitude and frequency settings) as independent within-subject factors. Pairwise comparisons were performed via post hoc t-tests with Holm–Sidak corrections. Sample size was estimated to detect 10% difference in the primary outcome variable PaCO2 by using a power of 0.8 and 2-sided α error of 0.05. The estimation resulted in a desired sample size of 9 animals in each group, based on the blood gas data obtained in our earlier study under similar experimental conditions [28]. Statistical tests were performed within the R environment with the lme4 [29] and lsmeans [30] program packages. p < 0.05 was considered to indicate statistical significance and all p values were 2-sided.
Results
The baseline blood gas, capnographic, ventilation, and respiratory mechanical parameters are summarized in Table 1. Before inducing hypercapnia and hypoxia, all parameters were within normal limits.
Figure 3 depicts typical tracheal pressure signals during application of CMV, HFPV, and eHFPV in a rabbit by introducing 10 Hz pressure fluctuations with a pressure amplitude of 2 cmH2O applied. The reduction in VDF and S2V is shown by the corresponding representative volumetric capnogram curves.
Left: Changes in the airway opening pressure during conventional mechanical ventilation (CMV, black), during high-frequency percussive ventilation (HFPV, blue) and an expiratory high-frequency percussive ventilation (eHFPV, red) (10 Hz oscillatory frequency administered with an amplitude of 2 cmH2O) obtained in a representative rabbit. Right: corresponding volumetric capnogram curve
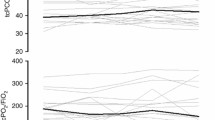
Figure 4 depicts the absolute values of the parameters acquired from arterial blood gas analyses during the different protocol stages, as well as their relative variations between the ventilation modes. The superposition of high-frequency oscillations throughout the whole ventilation cycle had a significant effect on the absolute values of PaCO2, PaO2, and SaO2, regardless of the frequency or amplitude of the high-frequency component (p < 0.001 for all). Improvements in gas exchange were also observed when a high-frequency signal with an amplitude of 4 cmH2O and frequency of 5 Hz was applied in the expiratory phase only (p < 0.001 for all). While such improvement was evidenced in oxygenation indices (PaO2 and SaO2) at a frequency of 10 Hz (p < 0.01 for both), there was only a tendency for a significant increase in CO2 clearance at 10 Hz (p = 0.1).
Arterial blood gas parameters during hypoxia and hypercapnia with normal mechanical ventilation (CMV, open symbols on the left), during high-frequency percussive ventilation (HFPV, blue filled symbols on the right) and during expiratory high-frequency percussive ventilation (eHFPV, red filled symbols on the right). Characters in the legend denote the oscillatory amplitude (2 or 4 cmH2O), the superposed frequency (5 or 10 Hz), and its application phase (E: expiratory phase only; IE: entire breathing cycle). PaO2: arterial partial pressure of oxygen, PaOC2: arterial partial pressure of carbon dioxide, SaO2: arterial oxygen saturation. *p < 0.05 between HFPV or eHFPV vs. the corresponding CMV
Figure 5 depicts the absolute values of ventilation parameters acquired by mainstream capnography and their relative variations between ventilation modes. HFPV improved capnography parameters (VDF/VT, S2V and V’CO2) independent of amplitude or frequency applied (p < 0.001 for all). While VCO2 elevated at all amplitudes and frequencies used during eHFPV (p < 0.001), this ventilation modality only improved VDF/VT and S2V at higher oscillatory amplitudes (p < 0.05 for all).
Parameters obtained via mainstream capnography during hypoxia and hypercapnia with normal mechanical ventilation (CMV, open symbols on the left), during high-frequency percussive ventilation (HFPV, blue filled symbols on the right) and during expiratory high-frequency percussive ventilation (eHFPV, red filled symbols on the right). Characters in the legend denote the oscillatory amplitude (2 or 4 cmH2O), the superposed frequency (5 or 10 Hz), and its application phase (E, expiratory phase only; IE, entire breathing cycle). VDF/VT: anatomical dead space fraction according to Fowler, S2V: phase 2 slope, V’CO2: minute elimination of carbon dioxide. *p < 0.05 between HFPV or eHFPV vs. the corresponding CMV
Additional file 1: Table S1 shows the relative differences in respiratory mechanical parameters between conventional and percussive ventilation modalities (Additional file 1). In comparison to CMV, neither HFPV nor eHFPV showed a significant effect on any airway or respiratory tissue parameters.
Figure 6 summarizes the parameters representing the delivered VT and corresponding airway opening pressures for the various ventilation strategies. At any experimental stage, there was no difference in VT and Pmean. The decreases in Pmin during all forms of percussive ventilation mirrored the negative ramifications of high-frequency pressure fluctuations at the airway opening. Pmax was only enhanced with HFPV because the oscillations in this modality persisted during the inspiratory phase.
Tidal volume and ventilation pressures obtained during hypoxia and hypercapnia with normal mechanical ventilation (CMV, open symbols on the left), during high-frequency percussive ventilation (HFPV, blue filled symbols on the right) and during expiratory high-frequency percussive ventilation (eHFPV, red filled symbols on the right). Characters in the legend denote the oscillatory amplitude (2 or 4 cmH2O), the superposed frequency (5 or 10 Hz), and its application phase (E, expiratory phase only; IE, entire breathing cycle). Pmean: mean airway opening pressure, Pmax: maximum airway opening pressure, Pmin: minimum airway opening pressure, VT: tidal volume. *p < 0.05 between HFPV or eHFPV vs. the corresponding CMV
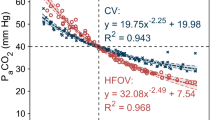
Additional file 1 describe the relationship between lung size and the ratio of alveolar and airway opening pressures (Palv/Pao) derived from the simulations. Palv/Pao showed a rapid decline with FRC rising until around 400 ml, when it plateaued at roughly 45% and 25% for oscillation frequencies of 5 and 10 Hz, respectively.
Discussion
The current study evaluated the usefulness of a novel ventilation approach based on the application of a high-frequency oscillatory component solely to the expiratory phase of invasive conventional single-frequency mechanical ventilation. The efficacy of this expiratory high-frequency percussive ventilation to increase O2 delivery and CO2 elimination with a 5 Hz oscillation frequency applied with a 4 cmH2O amplitude was demonstrated in rabbits with healthy lungs. These benefits in gas exchange were associated with decreased ventilation dead space and capnogram phase 2 slope, as well as enhanced CO2 minute elimination. This beneficial profile was not associated with alterations in the airway or respiratory tissue mechanics.
To satisfy the growing demand for improved ventilation assistance, many alternative types of mechanical ventilation have been developed. While PEEP elevation reduces pulmonary complications and improves patient outcomes [28, 31], this strategy is not without limits. High PEEP potentially increases stress and strain on lung tissues, and the reduced venous return and cardiac output, along with permissive hypercapnia [32], may result in cardiovascular impairment [33]. Another approach is application of variable tidal volume and frequencies based on prerecorded physiologic breathing patterns. The advantage of physiologically variable ventilation on respiratory mechanics, gas exchange, and lung inflammatory outcomes were established in healthy lungs [28], but not in severely injured lungs [33]. High-frequency oscillatory ventilation (HFOV) has been considered particularly in newborns but failed to demonstrate a benefit in adults particularly in the presence of ARDS characterized by a non-homogeneous insult, due to the risk for developments of distinct areas with cyclic hyper- and hypoinflation [1]. Alternatively, application of multi-frequency oscillatory ventilation in pediatric animal models of lung injury revealed improvements in oxygenation and CO2 elimination [20, 34] providing a clinical perspective to this ventilation modality as an advancement of HFOV.
CMV was coupled with superimposed constant-pressure fluctuations in our investigation, either throughout the whole ventilation cycle or during the expiratory phase. This approach combines the benefits of conventional tidal expansions to maintain the lung open with the high-frequency oscillations of HFOV. Previously, high oscillatory amplitudes were overlaid on conventional waveforms to apply HFPV [10,11,12,13,14,15]. Percussive ventilation with oscillatory amplitudes of 10–20 cmH2O improved gas exchange by enabling alveolar recruitment at the expense of greater peak inspiratory pressure [12]. With the use of modest amplitude oscillations, we were able to increase gas exchange in the current investigation (up to 5 to 10 times smaller than those applied previously during HFPV). As a result, our findings suggest that high frequencies delivered at significantly lower amplitudes are still effective at increasing gas exchange. While applying multi-frequency oscillatory ventilation with high frequencies (5–15 Hz) improved lung recruitment via a dithering effect to keep lung units open [34], the lack of improvements in respiratory mechanics (Additional file 1: Table S1) with HFPV and eHFPV waveforms with lower frequencies suggests that the enhanced gas exchange is not due to alveolar recruitment. Alternatively, the reduced VDF and S2V indicates augmentation of longitudinal gas transport via HFOV processes (Fig. 5), such as inducing asymmetric velocity profile, pendelluft, turbulence, molecular diffusion, and collateral ventilation [16]. Combining multiple frequencies in mechanical ventilation waveform may also improve gas exchange due to the highly frequency-dependent nature of how flow is heterogeneously distributed throughout the airway tree [19, 35,36,37]. Accordingly, these mechanisms have added value to the advantage of maintaining bulk flow and alveolar recruitment supplied by the CMV waveform component of HFPV and eHFPV.
The primary finding of the present study is the ability of eHFPV to improve gas exchange but when higher amplitude (4 cmH2O) and the lower oscillatory frequency (5 Hz) were superimposed on the conventional expiratory waveform. This oscillation amplitude was high enough to augment longitudinal gas transport, and the 5 Hz frequency was low enough to diminish the intrapulmonary shunting effect (Fig. 2S), resulting in better gas exchange. The improved axial gas mixing drained the alveolar CO2 gas content. In this context, the expired tidal volume can be considered virtually higher than the conventional inspiratory tidal volume. Likewise, oscillation is anticipated to restore the alveolar O2 fraction during expiration. During expiration, the intraluminal gas transfer can increase gas exchange without increasing inspiratory or expiratory pressures. Unlike in HFPV, this improvement during eHFPV did not result in an increase in peak inspiratory pressure (Fig. 6). High peak inspiratory pressure is the major cause of ventilator-induced lung injury (VILI) because it causes overdistension in the airway and alveolar compartments, resulting in the release of proinflammatory cytokines [38, 39]. Using oscillations solely during expiration to avoid excessive peak inspiratory pressure may protect against VILI, especially in lungs with restrictive diseases. This potentially protective feature of eHFPV takes on added significance in light of previous findings demonstrating that not only is increased alveolar stress and strain responsible for the inflammatory response in VILI, but excessive airway distensions also trigger proinflammatory bronchial responses, contributing to ventilator-induced lung injury [38].
The degree of improvement in gas exchange during percussive ventilation modes is determined by the efficiency with which the high-frequency component is delivered to the lung periphery [40]. High-frequency oscillations are attenuated by the resistive and elastic losses in the airways and gas-filled compartments, which are all dependent largely on lung size via complex mechanisms. Reduced shunting caused by narrower airspaces and less compliant tissue compartments in a smaller lung favors oscillatory signal transmission to the alveoli. Elevated resistive losses, on the other hand, reduce the oscillatory component of HFPV and eHFPV more significantly in smaller lungs. Our simulation study using representative values to characterize lung volumes and respiratory mechanics indicated that as lung size increased, so did the loss of oscillatory signal (Additional file 1: Fig. S2). As a result, more efficient transport of the high-frequency component to the alveolar spaces might be expected in smaller lungs (i.e., sizes in neonates and small children). This finding is consistent with the more evident benefit of HFOV in neonates and children without substantial ventilation heterogeneities, and also explains the controversy over the efficacy of HFOV in adults [1]. Subsequently, eHFPV may also be particularly beneficial in smaller lungs. However, our simulation study demonstrated that the oscillatory signal can be transmitted to the alveolar spaces of adult lungs with around 45% (5 Hz) and 25% (10 Hz) efficiency, indicating the presence of a gas exchange improvement even in adult-sized lungs.
The magnitude of changes in the gas exchange outcomes is noteworthy. While the improvements in PaCO2, PaO2, and SaO2 were statistically highly significant, the magnitude of changes was relatively modest (~ 10%–20%). Nevertheless, even small differences in these critical parameters can have a significant influence on the development of a gas exchange abnormality [2, 41]. Accordingly, prognosis for patient outcome may be fundamentally affected even by small favorable differences in clinical situations involving a progressive decline in gas exchange, such as in patients with acute lung injury and ARDS [41].
Conclusions
In summary, our findings demonstrate the efficacy of HFPV in improving gas exchange even when its oscillatory component is markedly smaller in amplitude than applied conventionally. The reduced ventilation dead space, capnogram phase 2 slope, and enhanced minute elimination of CO2 were not associated with changes in respiratory mechanics, suggesting that augmented longitudinal gas transport was involved rather than an increased lung surface available for gas exchange. In an additional effort to reduce lung overdistension, a novel mechanical ventilation modality based only on the superposition of a high-frequency oscillatory component during the expiratory phase of the conventional waveform was developed. This modality, termed as expiratory high-frequency percussive ventilation (eHFPV), enhanced oxygen delivery and CO2 removal by carefully selecting oscillatory frequency and amplitude without increasing lung expansion. Our findings suggest that ventilation with eHFPV has the potential to reduce hypoxemia and hypercapnia without increasing the driving pressure at the airway opening. Confirmation of our findings in subsequent trials has the promise to facilitate modification of already existing HFPV ventilators to extend their abilities with the eHFPV modality.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CMV:
-
Conventional mechanical ventilation
- eHFPV:
-
Expiratory high-frequency percussive ventilation
- FRC:
-
Functional residual capacity
- G:
-
Tissue damping
- H:
-
Tissue elastance
- HFOV:
-
High-frequency oscillatory ventilation
- HFPV:
-
High-frequency percussive ventilation
- PaO2 :
-
Arterial partial pressures of oxygen
- PaCO2 :
-
Arterial partial pressures of carbon dioxide
- Palv:
-
Alveolar pressure
- Pao:
-
Airway opening pressure
- PEEP:
-
Positive end-expiratory pressure
- Pmin :
-
Minimum airway pressure
- Pmax :
-
Maximum airway pressure
- Pmean :
-
Mean airway pressures
- Ptr:
-
Tracheal pressure
- Raw:
-
Airway resistance
- S2V:
-
Capnogram phase 2 slope
- SaO2 :
-
Arterial oxygen saturation
- V’CO2 :
-
CO2 volume eliminated in a minute
- VCO2 :
-
Expired CO2 within a breathing cycle
- VDF:
-
Fowler’s anatomic dead space
- VILI:
-
Ventilator-induced lung injury
- VT:
-
Tidal volume
References
Nguyen AP, Schmidt UH, MacIntyre NR. Should high-frequency ventilation in the adult be abandoned? Respir Care. 2016;61:791–800.
Cooke CR, Kahn JM, Caldwell E, Okamoto VN, Heckbert SR, Hudson LD, Rubenfeld GD. Predictors of hospital mortality in a population-based cohort of patients with acute lung injury. Crit Care Med. 2008;36:1412–20.
Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey AJ, Adhikari NKJ, Amato MBP, Branson R, Brower RG, et al. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195:1253–63.
Howell MD, Davis AM. Management of ARDS in adults. JAMA. 2018;319:711–2.
Spadaro S, Karbing DS, Mauri T, Marangoni E, Mojoli F, Valpiani G, Carrieri C, Ragazzi R, Verri M, Rees SE, Volta CA. Effect of positive end-expiratory pressure on pulmonary shunt and dynamic compliance during abdominal surgery. Br J Anaesth. 2016;116:855–61.
Valenza F, Chevallard G, Fossali T, Salice V, Pizzocri M, Gattinoni L. Management of mechanical ventilation during laparoscopic surgery. Best Pract Res Clin Anaesthesiol. 2010;24:227–41.
Thorell A, MacCormick AD, Awad S, Reynolds N, Roulin D, Demartines N, Vignaud M, Alvarez A, Singh PM, Lobo DN. Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg. 2016;40:2065–83.
Odor PM, Bampoe S, Gilhooly D, Creagh-Brown B, Moonesinghe SR. Perioperative interventions for prevention of postoperative pulmonary complications: systematic review and meta-analysis. BMJ. 2020;368: m540.
Harf A, Le Gall R, Chang HK. Mechanical ventilation with superimposed high frequency oscillation in the normal rat. Respir Physiol. 1983;54:31–40.
Butler AD, Dominick CL, Yehya N. High frequency percussive ventilation in pediatric acute respiratory failure. Pediatr Pulmonol. 2021;56:502–8.
Korzhuk A, Afzal A, Wong I, Khusid F, Worku B, Gulkarov I. High-frequency percussive ventilation rescue therapy in morbidly obese patients failing conventional mechanical ventilation. J Intensive Care Med. 2020;35:583–7.
Godet T, Jabaudon M, Blondonnet R, Tremblay A, Audard J, Rieu B, Pereira B, Garcier JM, Futier E, Constantin JM. High frequency percussive ventilation increases alveolar recruitment in early acute respiratory distress syndrome: an experimental, physiological and CT scan study. Crit Care. 2018;22:3.
Chung KK, Wolf SE, Renz EM, Allan PF, Aden JK, Merrill GA, Shelhamer MC, King BT, White CE, Bell DG, et al. High-frequency percussive ventilation and low tidal volume ventilation in burns: a randomized controlled trial. Crit Care Med. 2010;38:1970–7.
Derdak S, Mehta S, Stewart TE, Smith T, Rogers M, Buchman TG, Carlin B, Lowson S, Granton J. Multicenter Oscillatory Ventilation For Acute Respiratory Distress Syndrome Trial Study I: high-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial. Am J Respir Crit Care Med. 2002;166:801–8.
Allan PF, Osborn EC, Chung KK, Wanek SM. High-frequency percussive ventilation revisited. J Burn Care Res. 2010;31:510–20.
Pillow JJ. High-frequency oscillatory ventilation: mechanisms of gas exchange and lung mechanics. Crit Care Med. 2005;33:S135-141.
Al Ashry HS, Mansour G, Kalil AC, Walters RW, Vivekanandan R. Incidence of ventilator associated pneumonia in burn patients with inhalation injury treated with high frequency percussive ventilation versus volume control ventilation: a systematic review. Burns. 2016;42:1193–200.
Spapen H, De Regt J, van Gorp V, Honore PM. High-frequency percussive ventilation in acute respiratory distress syndrome: knocking at the door but can it be let in? Crit Care. 2018;22:55.
Herrmann J, Tawhai MH, Kaczka DW. Parenchymal strain heterogeneity during oscillatory ventilation: why two frequencies are better than one. J Appl Physiol. 1985;2018(124):653–63.
Herrmann J, Gerard SE, Shao W, Hawley ML, Reinhardt JM, Christensen GE, Hoffman EA, Kaczka DW. Quantifying regional lung deformation using four-dimensional computed tomography: a comparison of conventional and oscillatory ventilation. Front Physiol. 2020;11:14.
Herrmann J, Tawhai MH, Kaczka DW. Strain, strain rate, and mechanical power: an optimization comparison for oscillatory ventilation. Int J Numer Method Biomed Eng. 2019;35: e3238.
Tusman G, Scandurra A, Bohm SH, Suarez-Sipmann F, Clara F. Model fitting of volumetric capnograms improves calculations of airway dead space and slope of phase III. J Clin Monit Comput. 2009;23:197–206.
Fowler WS. Lung function studies; the respiratory dead space. Am J Physiol. 1948;154:405–16.
Fodor GH, Balogh AL, Sudy R, Ivankovits-Kiss O, Babik B, Petak F. Dopamine ameliorates bronchoconstriction induced by histaminergic and cholinergic pathways in rabbits. Respir Physiol Neurobiol. 2019;259:156–61.
Lutchen KR, Hantos Z, Petak F, Adamicza A, Suki B. Airway inhomogeneities contribute to apparent lung tissue mechanics during constriction. J Appl Physiol. 1996;80:1841–9.
Hantos Z, Daroczy B, Suki B, Nagy S, Fredberg JJ. Input impedance and peripheral inhomogeneity of dog lungs. J Appl Physiol. 1985;1992(72):168–78.
Sudy R, Fodor GH, Dos Santos RA, Schranc A, Tolnai J, Habre W, Petak F. Different contributions from lungs and chest wall to respiratory mechanics in mice, rats, and rabbits. J Appl Physiol. 1985;2019(127):198–204.
Walesa M, Bayat S, Albu G, Baudat A, Petak F, Habre W. Comparison between neurally-assisted, controlled, and physiologically variable ventilation in healthy rabbits. Br J Anaesth. 2018;121:918–27.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48.
Lenth RV. Least-squares means: the R package lsmeans. J Stat Softw. 2016;69:1–33.
Fodor GH, Habre W, Balogh AL, Sudy R, Babik B, Petak F. Optimal crystalloid volume ratio for blood replacement for maintaining hemodynamic stability and lung function: an experimental randomized controlled study. BMC Anesthesiol. 2019;19:21.
Barnes T, Zochios V, Parhar K. Re-examining permissive hypercapnia in ARDS: a narrative review. Chest. 2018;154:185–95.
Fodor GH, Bayat S, Albu G, Lin N, Baudat A, Danis J, Petak F, Habre W. Variable ventilation is equally effective as conventional pressure control ventilation for optimizing lung function in a rabbit model of ARDS. Front Physiol. 2019;10:803.
Kaczka DW, Herrmann J, Zonneveld CE, Tingay DG, Lavizzari A, Noble PB, Pillow JJ. Multifrequency oscillatory ventilation in the premature lung: effects on gas exchange, mechanics, and ventilation distribution. Anesthesiology. 2015;123:1394–403.
Allen JL, Fredberg JJ, Keefe DH, Frantz ID 3rd. Alveolar pressure magnitude and asynchrony during high-frequency oscillations of excised rabbit lungs. Am Rev Respir Dis. 1985;132:343–9.
Allen JL, Frantz ID 3rd, Fredberg JJ. Regional alveolar pressure during periodic flow. Dual manifestations of gas inertia. J Clin Invest. 1985;76:620–9.
Herrmann J, Tawhai MH, Kaczka DW. Regional gas transport in the heterogeneous lung during oscillatory ventilation. J Appl Physiol. 1985;2016(121):1306–18.
RespoNickles HT, Sumkauskaite M, Wang X, Wegner I, Puderbach M, Kuebler WM. Mechanical ventilation causes airway distension with proinflammatory sequelae in mice. Am J Physiol Lung Cell Mol Physiol. 2014;307:L27-37.
Monjezi M, Jamaati H, Noorbakhsh F. Attenuation of ventilator-induced lung injury through suppressing the pro-inflammatory signaling pathways: a review on preclinical studies. Mol Immunol. 2021;135:127–36.
Herrmann J, Lilitwat W, Tawhai MH, Kaczka DW. High-frequency oscillatory ventilation and ventilator-induced lung injury: size does matter. Crit Care Med. 2020;48:e66–73.
Esteve F, Lopez-Delgado JC, Javierre C, Skaltsa K, Carrio ML, Rodriguez-Castro D, Torrado H, Farrero E, Diaz-Prieto A, Ventura JL, Manez R. Evaluation of the PaO2/FiO2 ratio after cardiac surgery as a predictor of outcome during hospital stay. BMC Anesthesiol. 2014;14:83.
Acknowledgements
The authors thank Orsolya Ivánkovitsné-Kiss for the excellent technical assistance.
Funding
Open access funding provided by University of Szeged. This work was supported by Hungarian Basic Research Council Grants (OTKA-NKFIH K138032).
Author information
Authors and Affiliations
Contributions
Study concept: FP, BB, RLD, WH. Study design: FP, WH, RLD. Data collection: PF, GHF, ÁS, RS. Data analyses: FP, GHF, ÁS, RS, ÁLB, ADSR, DB. Statistical evaluation: FP, GHF. Simulation study: FP, ÁLB. Data interpretation: FP, BB, ADSR, SB, RLD, WH. Manuscript drafting: FP, RLD, WH. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the National Food Chain Safety and Animal Health Directorate of Csongrád County, Hungary (No. XXXII/149/2020) on March 10, 2020.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Details of the simulation study and additional data for respiratory mechanics.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Peták, F., Fodor, G.H., Schranc, Á. et al. Expiratory high-frequency percussive ventilation: a novel concept for improving gas exchange. Respir Res 23, 283 (2022). https://doi.org/10.1186/s12931-022-02215-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-022-02215-2