Abstract
Introduction
Despite improvements in medical science and public health, mortality of community-acquired pneumonia (CAP) has barely changed throughout the last 15 years. The current SARS-CoV-2 pandemic has once again highlighted the central importance of acute respiratory infections to human health. The “network of excellence on Community Acquired Pneumonia” (CAPNETZ) hosts the most comprehensive CAP database worldwide including more than 12,000 patients. CAPNETZ connects physicians, microbiologists, virologists, epidemiologists, and computer scientists throughout Europe. Our aim was to summarize the current situation in CAP research and identify the most pressing unmet needs in CAP research.
Methods
To identify areas of future CAP research, CAPNETZ followed a multiple-step procedure. First, research members of CAPNETZ were individually asked to identify unmet needs. Second, the top 100 experts in the field of CAP research were asked for their insights about the unmet needs in CAP (Delphi approach). Third, internal and external experts discussed unmet needs in CAP at a scientific retreat.
Results
Eleven topics for future CAP research were identified: detection of causative pathogens, next generation sequencing for antimicrobial treatment guidance, imaging diagnostics, biomarkers, risk stratification, antiviral and antibiotic treatment, adjunctive therapy, vaccines and prevention, systemic and local immune response, comorbidities, and long-term cardio-vascular complications.
Conclusion
Pneumonia is a complex disease where the interplay between pathogens, immune system and comorbidities not only impose an immediate risk of mortality but also affect the patients’ risk of developing comorbidities as well as mortality for up to a decade after pneumonia has resolved. Our review of unmet needs in CAP research has shown that there are still major shortcomings in our knowledge of CAP.
Similar content being viewed by others
Introduction
In 1918, Sir William Osler observed that pneumonia had replaced tuberculosis as the leading cause of death in Europe and described pneumonia as the ‘‘Captain of the men of death’’ [1].
Even one century later, pneumonia remains a major health concern and lower respiratory tract infections continue to be the leading infectious cause of death with more than 2.3 million deaths and more than 91 million years of life lost in 2016 [2]. With the emergence of the SARS-CoV-2 pandemic the central importance of acute respiratory infections to human health has once again been highlighted.
Pneumonia is defined as an acute infection of the pulmonary parenchyma and it is commonly classified by the “pneumonia triad” into community-acquired pneumonia (CAP) as the most common form of acquisition, hospital-acquired pneumonia (HAP) including ventilator-associated pneumonia (VAP) and pneumonia in the immunocompromised host [3, 4]. The clinical presentation and severity of pneumonia is diverse and usually categorized as mild, moderate or severe in major guidelines [5,6,7].
The annual incidence of CAP requiring hospitalization ranges from 1.1 to 8.9 per 1000 inhabitants [8,9,10,11] and the 30-day readmission rate ranges from 12 to 25% [12,13,14,15]. In patients with CAP who do not need hospital admission the mortality rate is ≤ 1% [16,17,18] while in hospitalized patients CAP the short-term mortality ranges from 8 to 14% [8, 10, 11, 19,20,21,22,23]. Further, several studies have shown that long-term mortality is excessive after CAP [24,25,26,27,28,29]. This underlines that CAP imposes a significant impact on the healthcare system and because of the aging population and the associated increase in comorbidities predisposing for CAP, it is likely that CAP will continue to be a major health issue in the years to come.
In 1999, the German Ministry of Education and Research published a call to initiate an excellence competition for competence centres in infectious diseases. Through this call the “network of excellence on Community Acquired Pneumonia” (CAPNETZ) was founded in 2001 [30]. CAPNETZ connects physicians, microbiologists, virologists, epidemiologists and computer scientists within clinical centres in Germany, Switzerland, Austria, The Netherlands, Denmark and Italy [31]. Today CAPNETZ offers the most comprehensive CAP database worldwide with an associated biobank for samples and pathogens including more than 12,000 patients [31]. Currently, the CAPNETZ database contains information on adult patients and consequently the pneumonia research within CAPNETZ has been focusing on adults. Pneumonia in children is also a major issue but an entity of its mown due to different pathogens, less burden of comorbidities etc. Recognizing the significance of pneumonia in children CAPNETZ has expanded their collaboration and begun inclusion of children into the pedCAPNETZ cohort [32]. The pedCAPNETZ cohort is still under construction and therefore the focus of this study is on adults only.
To discuss and identify which future research areas should have the highest priority in adult CAP research, CAPNETZ invited both internal and external CAP experts to participate in a 2-day scientific retreat. This paper summarizes the main research topics discussed, and highlights areas of future research, which deserve high priority to improve the understanding of CAP in order to develop novel prophylactic and therapeutic measures and ultimately reduce the burden of CAP.
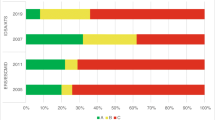
Procedures
The identification of unmet needs in CAP research followed a four-step procedure as depicted in Fig. 1. In brief, research members of CAPNETZ were asked to identify important issues to be addressed within basic, clinical and translational research. Then the top 100 experts in the field of CAP research were asked for their insights about the unmet needs in CAP research (Delphi approach). The top 100 experts were determined by CAPNETZ as the researchers with the most publications in the web of knowledge database over the past 5 years marked with “community-acquired pneumonia”. Only original publications, reviews and editorials were taken into consideration. Thirty-three of the 100 experts contributed with their views on the unmet needs in CAP research. Finally, the identified unmet needs in CAP research were discussed at a 2-day scientific retreat.
Since the SARS-CoV-2 pandemic emerged after the scientific retreat was held no unmet needs where identified prior to the meeting. However, due to the significant impact of the SARS-CoV-2 pandemic, sections on the Covid-19 disease have been added post hoc.
Results
Identified topics covering unmet needs in CAP research
Detection of causative pathogens
Current setting
Defining the causative pathogen in patients with pneumonia is relevant for ensuring the best-suited antimicrobial treatment. However, microbial diagnosis of pneumonia is still based on culture in most hospitals worldwide and a causative pathogen is only detected in the minority of patients. In a recent CAPNETZ study, bacteraemia rates in CAP were 0.5% in outpatients, 7.8% in hospitalized patients, 12.4% in patients admitted to an intensive care unit (ICU), and a relevant proportion of patients with bacteraemia and CAP (34.6%) was afebrile [33]. With the rapid emergence of novel diagnostic techniques (e.g. isothermic multiplex-PCRs for point of care testing, microbiome analysis, host transcriptomics and metagenomics), the question arises if these techniques will provide an added value to the currently available and established diagnostic methods and whether they will change management.
Unmet needs
Define an improved gold standard for microbial diagnosis of community-acquired pneumonia: Currently, microscopy and culture of lower respiratory tract specimens as well as blood cultures, detection of urine antigen detection and serology are routinely used to complement thorax imaging results in diagnosing pneumonia. However, most tests (particularly serology) lack sensitivity and specificity, while tests with a high sensitivity, such as PCR for non-influenza respiratory viruses may currently not properly translate into clinical relevance [34, 35]. No internationally accepted standard for microbiological tests in CAP has been defined, both in terms of including novel PCR-based techniques but also regarding the quality of the required respiratory samples [36]. There is a need for a consented diagnostic standard that also serves as comparison for new diagnostic techniques [37].
Next generation sequencing for guidance of antimicrobial treatment
Current setting
With the emergence of resistant or multidrug resistant (MDR) pathogens and increasing knowledge about potentially harmful or protective microbiomes [38], antibiotic management is becoming more complex [39]. Antibiotic stewardship is, therefore, a key priority [40] fostering pathogen directed treatment and avoiding excessive empiric broad spectrum antimicrobial therapy that increases the risk of complications, antibiotic resistance and mortality.
Metagenomics offers a potential solution. Most studies utilizing “microbiome” or metagenomics techniques to date have used target gene approaches such as sequencing amplicons of the 16s rRNA subunit [41]. As a more rapid technique, nanopore sequencing allows a much more in-depth data acquisition and analysis of viral and bacterial pathogens in real time [42]. The INHALE study from the UK showed that nanopore sequencing could provide results within 6 h of sampling from sputum with 96.6% sensitivity compared to culture [42]. This method also presented data on antibiotic resistance genes. Currently, methods to comprehensively describe bacterial, fungal and viral pathogens as well as the underlying microbiome in the same sample are still limited but technology is advancing rapidly.
Unmet needs
Metagenomic research has, to date, been conducted in relatively small studies in limited geographical locations [42]. Much larger studies are required to fully understand the limitations and added value of metagenomic approaches.
Studies show that molecular techniques out-perform culture in identification of bacterial pathogens [38, 42], but studies to demonstrate that implementation of these techniques improves clinical practice are lacking. There are remarkably few studies in which antibiotic choice, antibiotic duration or antibiotic spectrum are reduced or improved by the implementation of such techniques. Randomized controlled trials should be conducted to demonstrate the value of new techniques to improve CAP management.
Clinicians are not bioinformatics-scientists. Therefore, automated informatics tools that can rapidly analyse sequencing data and provide results to clinicians in a usable format are required. Antibiotic resistance genes may be detected by sequencing but their relationship to phenotypic resistance in bacteria is not always known, particularly in Gram-negatives.
Imaging diagnostics
Current setting
The primary role of imaging in CAP is to confirm the clinical diagnosis. The major diagnostic challenges are the correct identification of opacities and consolidations as being evoked by infectious versus non-infectious differential diagnoses. Different methods are available with chest radiography being the most abundantly used [43]. However, its low sensitivity and specificity leads to a high false negative and false positive rate, respectively, depending on the infiltrate’s position [44, 45]. Computer tomography (CT), therefore, is a useful addition to conventional radiography because of three-dimensional imaging with enhanced spatial resolution [44,45,46,47,48]. Due to higher radiation exposure and costs, however, CT is currently only used in selected cases [43, 49]. Further, lung ultrasonography may be an adjuvant resource to accurately diagnose CAP [50].
Unmet needs
Pathogen prediction through imaging analysis: Although radiographic findings do currently not allow the diagnosis of a specific pathogen, a differential diagnosis may be possible using radiological pattern recognition. Deep learning approaches may help to identify patterns that are indicative of specific viral or bacterial CAP. Integrating clinical data available at time of diagnosis may further improve such an approach.
Pre-test probability for general practitioners for chest radiography: Although chest radiographs are routinely used, the efficacy as a diagnostic tool has not been determined. The reduction of unnecessary chest radiographs particularly in the outpatient setting would decrease healthcare costs, and radiation exposure. However, even in the “Prospective Cough Complication Cohort Study (3C)”, where patients with acute cough received chest radiographs, the positive predictive value of at least one of four clinical signs of CAP (temperature > 37.8 °C, crackles on auscultation, oxygen saturation < 95%, heart rate > 100/min) for a radiography-confirmed pneumonia was low at around 20% [51]. In another European multicentre study including more than 3000 patients with acute cough, the addition of C-reactive protein > 30 mg/l to clinical signs of pneumonia (absence of runny nose and presence of breathlessness, crackles and diminished breath sounds on auscultation, tachycardia, and fever) improved the diagnostic classification [52]. However, further enhancing the pre-test probability for CAP would be necessary to provide a more reliable guide to general practitioners to identify patients with respiratory tract infections other than CAP where radiographs are not necessary.
Biomarkers
Current setting
Biomarkers may be an effective way to identify patients with severe infection and to monitor and eventually predict the course of infection. In CAP, biomarkers may be indicators of inflammation (local or systemic), may be released specifically after lung injury due to infection or originate from the genome of either the host or the pathogens. Numerous biomarkers have been investigated including pro-atrial natriuretic peptide [53], pro-vasopressin [53], cortisol [54], glucose [55], glycaemic gap [56], neutrophil extracellular traps [57], proadrenomedullin [58], Angiopoietin [59] etc. [60, 61] but C-reactive protein and procalcitonin remain the most widely used biomarkers [60] even though they both have well known shortcomings [60]. Additionally, cardiac troponins, biomarkers for cardiac injury, may identify patients with cardiac complications of CAP that need special attention during follow-up [62, 63]. Since coronary artery calcium (CAC), a marker of coronary atherosclerotic burden, is higher in patients already at increased atherosclerotic cardiovascular risk after pneumonia as compared to similar patients without a pneumonia event, assessment of CAC by CT may also be of predictive value [64].
Unmet needs
As the research on immune-modulatory therapies intensifies, so will the search for the appropriate biomarkers for severity and treatment response [65]. However, the heterogeneity among patients with CAP in terms of onset of symptoms, clinical presentation, severity of disease, causative pathogen(s), comorbidities, genetic disposition etc. is vast. The discovery of a single common biomarker for CAP is therefore unlikely. Instead, combining the different sources of “biomarkers” into a systems-medicine approach reflects the complexity of CAP and could provide new insights, accurate clinical diagnosis, prediction of the severity of disease and help targeting specific adjuvant treatments. The recent advances in the field of metabolomics, genomics, epigenomics, transcriptomics, proteomics and microbiomics offer respective opportunities [60, 66].
Risk stratification
Current setting
Identifying low risk-patients that can be treated in an outpatient setting enhances patient satisfaction and reduces costs. CRB-65 is frequently used as a first step but should be supplemented by oxygenation status, assessment of instable comorbidities and functional parameters [67]. Identifying high-risk patients allows early application of intensified management, prevents organ failure and, thereby, improves prognosis. ATS/IDSA minor criteria supplemented by lactate are recommended tools [68, 69]. Recommendations for early high-risk stratification are available but have not yet been fully implemented. Although there is a five percent risk of death within the first post-discharge weeks [70], there is only limited data available on risk stratification to predict post-discharge complications.
Unmet needs
Harmonization with sepsis risk stratification and implementation of prediction tools: Sepsis is a major complication in CAP. Current sepsis recommendations employ a risk stratification strategy with similarities to CAP risk stratification by using a simple screening score (quickSOFA, qSOFA) and a more specific high-risk prediction score (SOFA) [71]. However, the scores and respective breakpoints (e.g. respiratory rate in qSOFA vs. CRB-65) are different from those recommended for CAP [72]. Moreover, the qSOFA with a cut off of ≥ 2 misses more than half of CAP patients whose condition will deteriorate during the course of the disease [73]. For optimal implementation of risk stratification concepts in busy emergency departments a harmonization of both concepts is needed, and prospective (cluster-randomized) clinical studies to implement recommendations with clinical outcome endpoints are necessary.
Individualization of management-based risk stratification: Today, medicine is heading towards the broad application of state-of-the-art medical technologies including “omics” approaches, which might allow more tailored treatment approaches based on a better understanding of a patient’s individual state of health [74]. In addition, machine learning could provide algorithms that predict the patient’s individual risk to deteriorate and will allow monitoring treatment responses based on routinely measured markers [75].
Risk factors for and management strategies against early post-discharge complications: Studies show high re-admission or even early death rate after discharge from hospital because of CAP [12, 76]. So far, only little information is available on risk factors for post-discharge events, including infection- and non-infection-related complications, re-hospitalization or death. There is the need to determine the different affected patient groups and to define target groups that require interventions.
Stratification strategy for the coverage of multidrug resistant pathogens: In Europe, MDR pathogens are rare in CAP, but still can complicate the choice of empiric antibiotic therapies and may result in poor outcomes [77]. However, optimal individual MDR risk prediction is not known as existing scores lack accuracy and external validation.
Antiviral and antibiotic treatment
Current setting
The early initiation of antibiotic therapy has been shown to provide a survival benefit [78]. Treatment is typically started empirically, prior to the identification of the causative pathogen. Bacteria are considered to be the primary causative pathogens in CAP and antibiotics are the mainstay of CAP treatment.
Treatment guidelines differ for outpatients and only little information is available on CAP-outpatients. In the hospital, either antibiotic monotherapy or combination therapy is applied but up to now no significant differences in outcome apart from adverse effects have been observed [79]. Most antibiotics are administered systemically, either through intravenous or oral application. The role of aerosolized antibiotics has so far been only investigated for hospital-acquired (HAP) and ventilator-associated pneumonia, but not for CAP [80].
Viral pathogens are increasingly recognized as a cause of pneumonia, especially among immunocompromised patients. Although more than 20 viruses have been linked with CAP, antiviral drugs were only available for the treatment of influenza or respiratory syncytial virus (RSV) pneumonia [81] before COVID-19. Since the occurrence of SARS-CoV-2 existing antiviral drugs such as Remdesivir and lopinavir–ritonavir have been evaluated for the treatment of Covid-19 [82]. However, lopinavir–ritonavir has not shown any beneficial effect in treating Covid-19 and the effect of Remdesivir in treating Covid-19 is still questionable [82]. The specifically developed antiviral Paxlovid may hold promise but peer-reviewed data are currently lacking [83].
Secondary bacterial pneumonia is frequently observed in viral pneumonia [84, 85] and influenza patients often receive preventive antibiotic treatment [86]. However, the pathophysiologic mechanisms promoting a co-infection with bacterial and viral pathogens are not fully understood. Notably, the frequency of bacterial co-infections in Covid-19 patients appears to be low [87].
Unmet needs
Monitoring of ß-lactam antibiotic and macrolide antibiotic treatment and development of resistance: ß-lactams have been the “antibiotic backbone” of antimicrobial therapy of pneumonia for decades [88]. However, increasing resistance rates are beginning to limit the utility of this antibiotic class. Drug-resistant Gram-negative pathogens associated with pneumonia have been identified with increasing frequency and a variety of resistance patterns. Among the “atypical” agents there is also several reports of increasing macrolide resistance in M. pneumoniae infections throughout the world [89,90,91]. Antibiotic resistances show a broad variety between regions. Treatment guidelines, therefore, need to be updated and validated based on local epidemiological data [92].
Development of new antibiotics vs. improved usage of available antibiotics: Although the number of newly approved antibiotics has tripled in the past 6 years after a 90% decrease between 1983 and 2012, MDR bacteria pose an increasing threat [93]. Mis- and overuse of empirically prescribed broad-spectrum antibiotics have led to a significant increase in resistance although a great diversity has been observed in different countries [94]. The timely differentiation between bacterial and viral pneumonia may support the physician in avoiding medically not indicated antibiotic administration. In CAP, development of new antibiotics and improving diagnostic-guided therapy is warranted.
Overview of the treatment of CAP in an outpatient setting: A high proportion of CAP patients is treated in an outpatient setting [52, 70]. A comprehensive overview of existing real-life principles that guide treatment in an outpatient setting will allow the formulation of improved guidelines taking the medical environment and available methods into account.
Adjunctive therapy
Current setting
An excessive inflammatory response seems to be partly responsible for treatment failure in some patients and has been associated with poor clinical outcomes [95]. Different immunomodulatory and barrier-enhancing agents have been discussed and tested for potential adjunctive therapy to antimicrobial agents in the treatment of CAP. Classical approaches have focused on corticosteroids and immunoglobulins [95], while the effects of adrenomedullin and angiopoietin-1 have been investigated in more experimental approaches [59, 96]. Especially corticosteroids have been the subject of potential adjuncts to conventional CAP treatment [95]. They are the most used anti-inflammatory drugs and modulate a wide range of physiological processes, but their efficacy has been discussed controversially in CAP treatment [97]. In hospitalized patients with Covid-19 and who requires oxygen, corticosteroid treatment improves survival [98] and is therefore recommended [82].
Further, due to the hyperinflammation state seen in some patients with Covid-19 several immunomodulatory agents, with the intend to block the inflammatory pathway, have been evaluated [82, 99]. Fare from all has proven effective but in hospitalized patients with Covid-19 and in need of oxygen treatment, IL-6 inhibitors may reduce the risk of mechanical ventilation or death [82]. Likewise treatment with Janus kinase (JAK) inhibitors may reduce the risk of respiratory failure and death [100, 101]. Inhibition of the IL-1 pathway may also be associated with reduced mortality in patients with Covid-19 [102] although conflicting results exists [103, 104].
As the understanding of the underlying pathophysiology improves, specifically tailored agents for immunomodulatory therapy will likely help to avoid adverse outcomes for specific patient groups.
Unmet needs
Identification of patients that benefit most from macrolides: In addition to antimicrobial effects, macrolides also have an immunomodulatory effect [105, 106]. Several studies have suggested a benefit of adding macrolides to a β-lactam in the empirical treatment, although the existing literature is conflicting [105, 107,108,109]. It is largely unclear, which patient groups benefit most from an adjunctive macrolide therapy since the effects of macrolides appear to be influenced by the presence of bacteria [106, 110] and by the susceptibility of the host to develop cardiac side effects associated with macrolide treatment [111].
A recent CAPNETZ study has used a machine learning approach to identify patients who benefit most from macrolide treatment [112]. Such a personalized approach is important for improved management and disease outcome. However, results need to be confirmed in a randomized controlled trial.
Immunoglobulins: Immunoglobulins have been proposed as a promising adjunctive therapy option for severe sepsis, but have only been investigated in small studies [113]. Both, IgG and IgM levels have been shown to be higher during convalescence in pneumonia [114]. Additionally, patients with severe CAP admitted to ICU showed lower levels of immunoglobulins than non-ICU patients [115]. Since therapeutic formulations of immunoglobulins are available further insights into the changes of serum levels of immunoglobulins and IgG subclasses during the course of the disease are of scientific and therapeutic interest.
Pathogen-directed strategies: In addition to antibiotic treatment, a pathogen-directed strategy may include blockers of pathogenicity, virulence, or toxins. These may be small molecule inhibitors or monoclonal antibodies [116]. Additional use of adoptive cell therapy might be possible as well as the use of phages or phage products. In the ongoing pandemic of Covid-19 treatment with monoclonal antibodies against the SARS-CoV-2 spike protein may reduce the risk of Covid-19-related hospitalization and death in ambulatory patients [117] and in hospitalized patients with Covid-19 and who are seronegative, treatment with monoclonal antibodies may reduce mortality [118].
Host-directed strategies: Alternative strategies comprise of specifically stimulating early local immune responses against pathogens, dampening particular components of the local and systemic immune responses to avoid tissue injury, increasing tissue resilience and improving resolution of inflammation and tissue repair.
Vaccines and prevention
Current setting
Vaccines against pneumococci and influenza virus, the most frequent bacterial and viral causes of CAP, are available. Influenza vaccination has been shown to reduce the number of severe CAP cases and improved overall long-term survival in patients with CAP during influenza seasons [119]. The known mechanistic link between cardiovascular events and pneumonia may be the cause for the reported cardioprotective effect of vaccines against influenza and pneumococci [120,121,122].
Recently, a quadrivalent influenza vaccine that includes both influenza B lines, i.e. Yamagata and Victoria, has been made available for clinical use [123]. It has already been recommended as the primary influenza vaccine instead of the trivalent influenza vaccines in several countries. The investigational universal influenza vaccine candidate, FLU-v, has entered phase 3 clinical trials [124] after demonstrating immunogenicity and safety in a recent phase 2b study [125].
Two types of pneumococcal vaccines are used: pneumococcal conjugate vaccines (PCVs) and pneumococcal polysaccharide vaccines (PPVs). Although PPV has been shown to prevent pneumococcal bacteraemia, its protective effect against non-invasive pneumococcal pneumonia and its effectiveness in the immune-compromised host are limited [126,127,128]. Infant vaccination programs with PCV have substantially decreased the contained serotypes by herd protection effects [129]. However, the decrease of vaccine serotypes was compensated by non-vaccine serotypes (replacement effect), that comprised sometimes even the same pneumococcal clone, which has switched its capsule to another serotype to evade the selective pressure of the vaccine [130]. Furthermore, strong herd protection effects in invasive and non-invasive pneumococcal CAP seen after the global implementation of the 7-valent conjugate vaccine (PCV7) [129, 131] were not reproduced after substitution of PCV7 by the 13-valent conjugate vaccine (PCV13) [132, 133]. Particularly, serotype 3, which was included into PCV13, seems not to be affected by herd protection effects. Serotype 3 has been associated with disease severity, i.e. higher rate of patients with hospital admission and oxygen support, and has become one of the leading serotypes in adult CAP [133, 134]. The decreased efficacy against serotype 3 as well as the lack of herd protection of this major serotype is not completely understood. One plausible hypothesis includes capsular shedding after binding of antibodies [135].
Unmet needs
Optimal use for pneumococcal polysaccharide vaccines and pneumococcal conjugate vaccines: Although the two vaccines PPV23 and PCV13 share some serotypes they generate different immune responses [136]. While both vaccines generate antibodies against pneumococcal capsular antigens, only PCV13 induces a T-cell-dependent response. The broad landscape of different pneumococcal vaccination recommendation worldwide (i.e. PPV or PCV or “sequential vaccination” with PCV followed by PPV) reflects uncertainty on the optimal use of these vaccines. Furthermore, simultaneous application of both pneumococcal vaccines (PCV and PPV) is currently investigated for the first time in an ongoing randomized controlled trial to improve immunological response (pneumococcal serotype specific B-cells and humoral immune response) in the elderly [137]. More research is needed on the topic to provide vaccination recommendations especially for patients with certain underlying medical conditions such as respiratory, hepatic or renal comorbidities and immunosuppression as well as the optimal time for re-vaccination [138].
Novel vaccines: Like a universal influenza vaccine, a serotype independent pneumococcal vaccine would decrease the global CAP burden tremendously. Currently, a 15-valent PCV was announced in the US and a 20-valent PCV is close to market license [139]. However, experience with PCV7 and PCV13 have shown that pneumococcal evolution is highly dynamic and that non-vaccine serotypes will emerge and fill the niche created by PCV-induced reduction of vaccine serotypes. Since the inclusion of even more serotypes into a novel vaccine is limited, a serotype independent vaccine targeting e.g. surface proteins would represent a major breakthrough [140]. Also, a more effective—even singular—vaccine against serotype 3 would decrease the burden of CAP tremendously.
The progress in microbiological diagnostics—and also the recent SARS-CoV-2 pandemics- has uncovered the burden of non-influenza respiratory viruses in CAP. Particularly, RSV seems to expose a substantial burden on adult CAP. Therefore, a RSV vaccine is highly desirable but remains a challenge [141], since earlier RSV vaccines had no efficacy and even seemed to aggravate disease [142].
Systemic and local immune response
Current setting
In order to facilitate a rapid and efficient immune response against invading microbial pathogens, the lung combines different defence strategies including anatomic, mechanical, humoral, and cellular mechanisms aiming towards the rapid expulsion of pathogens [143]. The lung is a fragile organ that is finely designed for gas exchange, so that an excessive immune response may itself be damaging and lead to irreparable tissue damage that might be lethal [144, 145]. Many anti-inflammatory strategies have failed to improve survival in pneumonia [146]. It seems that more specific anti-inflammatory strategies, subphenotyping of patients, and precise timing are crucial to achieve beneficial modulation of the inflammatory response. Differences in immune responses may result from genetic predispositions that influence immunomodulation [147, 148]. Deciphering the mechanisms of inflammatory response in respiratory infection would allow the identification of different inflammatory phenotypes.
Unmet needs
Determination of different inflammatory phenotypes for personalized medicine: Despite sharing the same underlying pathogen, in some patients CAP manifests as a serious disease while in others the course of disease is mild. The susceptibility to infection as well as CAP severity is most likely a phenotypical trait determined by uncountable pathogen- and host-specific factors, including polymorphisms in many collaborating genes in otherwise healthy persons [149], immunosenescence, pregnancy, lung diseases, immunodeficiency, and specific therapies for preceding diseases or the CAP itself, to name a few. Therefore, specific conditions need specific strategies for promising personalized adjunctive immunomodulatory therapy.
Pulmonary long-term consequences of CAP: While most patients return to normal lung function following pneumonia within weeks to months, some fail to recover ad integrum due to pleura-involvement or parenchymal alteration, and some may be at an increased risk of developing chronic non-infectious lung inflammation including cryptogenic organizing pneumonia (COP) and idiopathic pulmonary fibrosis (IPF) after an episode of pneumonia. The early identification of these patients would allow taking timely countermeasures. For this, specific markers (of clinical course, lung function, imaging, biomarkers, etc.) and therapeutic strategies need to be identified. Therefore, a deeper patho-mechanistic understanding of the pulmonary long-term sequelae of CAP is needed.
Extra-pulmonary long-term consequences of CAP (see also “Long-term cardio-vascular complications”): Severe pulmonary and systemic inflammation upon lung infection may result in long-term sequelae regarding organ dysfunction, vascular pathology, and neuromuscular function. Some patho-mechanistic links have been proposed, e.g. direct cardiac damage by bacterial invasion into the myocardium and formation of microscopic lesions finally leading to cardiac scarring [150] and a causal relationship between pulmonary inflammation and atherosclerotic plaque formation in systemic arteries [151]. However, many key patho-mechanisms by which pneumonia may trigger or promote subsequent organ dysfunction remain unclear. The complexity of the interplay between pulmonary inflammation and distant organ pathology and the relatively long timeframes render preclinical as well as clinical investigations in this field challenging. Nevertheless, the emerging evidence for the relevance of long-term sequelae for patient outcome and the probability for potentially effective secondary prophylactic measures warrant intense joint scientific efforts.
Comorbidities
Current setting
Pre-existing comorbidities including chronic respiratory, cardiovascular diseases and diabetes mellitus are frequent in the elderly population and increase the risk of CAP as well as mortality [152, 153]. Immunosenescence and therapies with immunosuppressive agents increase the number of immunosuppressed patients. Immunosuppression has been recognized as an independent risk factor for CAP [9]. Although the prevalence of different comorbidities in CAP patients has been evaluated across several studies, data on their impact on the course of the disease as well as their management during CAP are limited. Furthermore, most of the international guidelines on CAP management clearly state that the proposed recommendations do not apply to patients with immunosuppression [5]. International and observational studies on immunocompromised patients are limited or consider only a single specific risk factor. A direct implication of this scenario is the possible underestimation of the real prevalence of immunosuppression with a higher rate of treatment failure or an overestimation and overuse of wide-spectrum antibiotics.
Unmet needs
Treatment guidelines for immunocompromised patients: Up to 29% of hospitalized patients with CAP have some level of immunosuppression [154] and it is foreseeable that this population will expand in the following years. These patients may be at risk of both the “core” CAP pathogens and opportunistic microorganisms. Unfortunately, such patients are often excluded from pneumonia studies resulting in a marked knowledge gap concerning causative pathogens, performance of existing prognostic risk scores and performance of advanced diagnostic such as metagenomics among others. Immunocompromised patients do not form a homogeneous group in terms of underlying disease, treatment and severity of immunosuppression and the different immunosuppression states in the context of CAP need to be defined. It is possible that severely immunocompromised patients with CAP may benefit from adjunctive therapies to enhance specific functions of the immune system. Therefore, future studies need to focus on patients with risk factors for immunodeficiency in order to provide clinicians with recommendations for the management of immunocompromised patients with CAP.
Treatment guidelines for patients on special medication (i.e. patients on chronic steroids, biological drugs and cancer patients): Patients suffering from pre-existing lung diseases such as asthma or COPD are often treated with either inhaled or systemic corticosteroids [155]. Although these drugs reduce inflammation and might prevent exacerbations, the impact of the routine use of corticosteroids on CAP patients has not been investigated to full extent [156]. Biological drugs targeting tumour immune evasive pathways for the treatment of lung cancer [157] may guide different treatment regimens of CAP due to a changed immune status in these patients. With the ever-increasing number of patients suffering from pre-existing lung disease, it will be necessary to develop adjusted guidelines and treatment recommendations.
Influence of CAP on dementia and neurological damage: As in sepsis, during the acute phase of pneumonia, confusion is frequently observed [158, 159]. Evidence suggests that delirium may hasten cognitive deterioration in people with pre-existing dementia. Since pneumonia is primarily a disease of older patients there is the possibility that an episode of pneumonia will cause neurological damage and that the early onset of worsening of pre-existing dementia is a long-term consequence of CAP that has been overlooked so far.
Long-term cardio-vascular complications
Current setting
Hospitalized CAP patients have an increased risk of major acute and long-term cardiovascular complications (i.e. new/worsening heart failure, new/worsening arrhythmias, myocardial infarctions and/or strokes) [151, 160], which are associated with a 60% increase in short-term mortality [161]. Mortality remains increased even in long-term survivors of pneumonia [27, 162], an effect that has at least in part been attributed to an increased risk for cardiovascular diseases such as heart failure or atherosclerosis [151, 163, 164]. As a result of both acute and long-term effects, the ensuing risk for cardiovascular events associated with pneumonia is similar to or higher as compared to classic cardiovascular risk factors such as smoking or diabetes [165]. The underlying pathophysiological processes, however, are so far largely unclear.
Unmet needs
Spectrum, incidence and outcome of cardio-vascular disease after pneumonia: While there is clearly emerging evidence from epidemiological and preclinical studies for the association of pneumonia with both short- and long-term cardiovascular events, a comprehensive analysis of the various clinical manifestations (e.g. systolic or diastolic heart failure, arrhythmias, atherosclerotic and ischemic events) of cardiovascular disease (CVD), their incidence at different time points following a pneumonia event, and their association with outcome is as yet lacking, but would be critical to develop better diagnostic tools and ultimately tailor interventional trials.
Patients at increased risk of developing cardio-vascular disease after pneumonia: Patients with pre-existing chronic CVD have the strongest risk, followed by patients with common comorbidities including chronic obstructive pulmonary disease (COPD), ischemic heart disease, and diabetes [160]. The influence of these risk factors prior to the event of pneumonia, however, has not been stratified. Similarly, genetic traits associated with an increased risk for CVD after pneumonia have so far not been assessed. Furthermore, most studies focus so far on short-term outcomes of CAP. Cardiovascular complications associated with CAP may occur up to 10 years or more after the event of pneumonia. It would be helpful to stratify known cardiovascular risk factors to identify patients at an increased risk of developing CVD as early as possible and to develop therapeutic interventions to reduce the incidence of cardiac complications following CAP. Similarly, it would be helpful to identify microbial characteristics, and/or markers of pneumonia severity and host response that may predict association with CVD and CVD-related mortality [166].
Prevention of cardio-vascular disease after pneumonia: At present, our understanding of the patho-mechanisms that drive acute and chronic CVD following pneumonia is at best rudimentary. Discussed mechanisms include but are not limited to invasion of microbes such as S. pneumoniae into the myocardium with formation of microscopic lesions [150], or dissemination of inflammatory cells or pro-inflammatory mediators and extracellular vesicles driving inflammatory cardiomyopathic syndromes or formation and destabilization of atherosclerotic plaques [151]. A detailed in-depth understanding of these mechanisms by comparative systems medicine approaches in patient cohorts and preclinical models is required to inform the development and testing of targeted interventions to prevent CVD in patients-at-risk and/or in specific responder subgroups and as such, to create personalized therapeutic approaches.
Conclusion
Pneumonia has been known as the leading infectious cause of death for more than a century and many attempts have been made to change this fact. However, the mortality of CAP has barely changed in the last 50 years and the Covid-19 pandemic has once again highlighted the central importance of acute respiratory infections to human health. Pneumonia is not just an infection of the lung but a complex disease where the interplay between the pathogen(s), immune system and comorbidities not only impose an immediate risk of mortality but also affect the patients’ risk of developing comorbidities as well as mortality for up to a decade after the pneumonia has resolved. Despite the importance of pneumonia on human health and the fact that many of the identified topics have been focus points for several years, our review of unmet needs in CAP research has shown that there are still major shortcomings in our knowledge of CAP. The poor evidence base that exists for most clinical decisions in acute respiratory infections can no longer be considered acceptable and a co-ordinated focus and investment into research on acute respiratory infections is now needed.
Take home message
Unmet needs have been identified for diagnostics, risk stratification, treatment, adjunctive therapy, and prevention. Major knowledge gaps include immune response, role of comorbidities, and long-term cardio-vascular complications.
Availability of data and materials
Not applicable.
Abbreviations
- CVD:
-
Cardiovascular disease
- CAP:
-
Community-acquired pneumonia
- CT:
-
Computer tomography
- CAC:
-
Coronary artery calcium
- COPD:
-
Chronic obstructive pulmonary disease
- COP:
-
Cryptogenic organizing pneumonia
- HAP:
-
Hospital-acquired pneumonia
- IPF:
-
Idiopathic pulmonary fibrosis
- ICU:
-
Intensive care unit
- JAK:
-
Janus kinase
- MDR:
-
Multidrug resistant
- CAPNETZ:
-
Network of excellence on Community Acquired Pneumonia
- PCVs:
-
Pneumococcal conjugate vaccines
- PPVs:
-
Pneumococcal polysaccharide vaccines
- qSOFA:
-
Quick SOFA
- RSV:
-
Respiratory syncytial virus
- VAP:
-
Ventilator-associated pneumonia
- PCV7:
-
7-Valent conjugate vaccine
- PCV13:
-
13-Valent conjugate vaccine
References
Osler W, McCrae T. The principles and practice of medicine. New York, London: D. Appleton and company; 1920. http://archive.org/details/principlesandpr00mccrgoog. Accessed 15 May 2019.
Wang H, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, et al. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1084–150.
Chalmers JD, Pletz MW, Aliberti S. European respiratory monograph community-acquired pneumonia. European Respiratory Society; 2014.
Aliberti S, Cruz CSD, Amati F, Sotgiu G, Restrepo MI. Community-acquired pneumonia. Lancet. 2021;398:906–19.
Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200:e45–67.
Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Jeune IL, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64:iii1–55.
Ewig S, Höffken G, Kern W, Rohde G, Flick H, Krause R, et al. Behandlung von erwachsenen Patienten mit ambulant erworbener Pneumonie und Prävention—Update 2016. Pneumologie. 2016;70:151–200.
Egelund GB, Jensen AV, Andersen SB, Petersen PT, Lindhardt BØ, von Plessen C, et al. Penicillin treatment for patients with community-acquired pneumonia in Denmark: a retrospective cohort study. BMC Pulm Med. 2017;17:66.
Torres A, Peetermans WE, Viegi G, Blasi F. Risk factors for community-acquired pneumonia in adults in Europe: a literature review. Thorax. 2013;68:1057–65.
Ewig S, Birkner N, Strauss R, Schaefer E, Pauletzki J, Bischoff H, et al. New perspectives on community-acquired pneumonia in 388 406 patients. Results from a nationwide mandatory performance measurement programme in healthcare quality. Thorax. 2009;64:1062–9.
Søgaard M, Nielsen RB, Schønheyder HC, Nørgaard M, Thomsen RW. Nationwide trends in pneumonia hospitalization rates and mortality, Denmark 1997–2011. Respir Med. 2014;108(8):1214–22.
Petersen PT, Egelund GB, Jensen AV, Andersen SB, Pedersen MF, Rohde G, et al. Associations between biomarkers at discharge and co-morbidities and risk of readmission after community-acquired pneumonia: a retrospective cohort study. Eur J Clin Microbiol Infect Dis. 2018;37(6):1–9.
Jasti H, Mortensen EM, Obrosky DS, Kapoor WN, Fine MJ. Causes and risk factors for rehospitalization of patients hospitalized with community-acquired pneumonia. Clin Infect Dis. 2008;46:550–6.
Shorr AF, Zilberberg MD, Reichley R, Kan J, Hoban A, Hoffman J, et al. Readmission following hospitalization for pneumonia: the impact of pneumonia type and its implication for hospitals. Clin Infect Dis. 2013;57:362–7.
Micek ST, Lang A, Fuller BM, Hampton NB, Kollef MH. Clinical implications for patients treated inappropriately for community-acquired pneumonia in the emergency department. BMC Infect Dis. 2014;14:61.
Fine MJ, Smith MA, Carson CA, et al. Prognosis and outcomes of patients with community-acquired pneumonia: a meta-analysis. JAMA. 1996;275:134–41.
Carratala J, Fernández-Sabé N, Ortega L, Castellsagué X, Rosón B, Dorca J, et al. Outpatient care compared with hospitalization for community-acquired pneumonia: a randomized trial in low-risk patients. Ann Intern Med. 2005;142:165–72.
Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–82.
Arnold FW, Wiemken TL, Peyrani P, Ramirez JA, Brock GN. Mortality differences among hospitalized patients with community-acquired pneumonia in three world regions: results from the community-acquired pneumonia organization (CAPO) international cohort study. Respir Med. 2013;107:1101–11.
Metersky ML, Waterer G, Nsa W, Bratzler DW. Predictors of in-hospital vs postdischarge mortality in pneumonia. Chest. 2012;142:476–81.
Fine MJ, Stone RA, Singer DE, Coley CM, Marrie TJ, Lave JR, et al. Processes and outcomes of care for patients with community-acquired pneumonia: results from the pneumonia patient outcomes research team (PORT) cohort study. Arch Intern Med. 1999;159:970–80.
Lindenauer PK, Lagu T, Shieh M-S, Pekow PS, Rothberg MB. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA. 2012;307:1405–13.
Ramirez JA, Wiemken TL, Peyrani P, Arnold FW, Kelley R, Mattingly WA, et al. Adults hospitalized with pneumonia in the united states: incidence, epidemiology, and mortality. Clin Infect Dis. 2017;65:1806–12.
Bruns AHW, Oosterheert JJ, Cucciolillo MC, El Moussaoui R, Groenwold RHH, Prins JM, et al. Cause-specific long-term mortality rates in patients recovered from community-acquired pneumonia as compared with the general Dutch population. Clin Microbiol Infect. 2011;17:763–8.
Koivula I, Stén M, Mäkelä P. Prognosis after community-acquired pneumonia in the elderly: a population-based 12-year follow-up study. Arch Intern Med. 1999;159:1550–5.
Brancati FL, Chow JW, Wagener MM, Vacarello SJ, Yu VL. Is pneumonia really the old man’s friend? Two-year prognosis after community-acquired pneumonia. Lancet. 1993;342:30–3.
Mortensen EM, Kapoor WN, Chang C-CH, Fine MJ. Assessment of mortality after long-term follow-up of patients with community-acquired pneumonia. Clin Infect Dis. 2003;37:1617–24.
Yende S, D’Angelo G, Kellum JA, Weissfeld L, Fine J, Welch RD, et al. Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med. 2008;177:1242–7.
Johnstone J, Eurich DT, Majumdar SR, Jin Y, Marrie TJ. Long-term morbidity and mortality after hospitalization with community-acquired pneumonia: a population-based cohort study. Medicine. 2008;87:329–34.
Welte T, Suttorp N, Marre R. CAPNETZ—community-acquired pneumonia competence network. Infection. 2004;32:234–8.
CAPNETZ. https://www.capnetz.de/html/capnetz/lccs. Accessed 29 Nov 2017.
pedCAPNETZ. http://www.capnetz.de/html/pedcapnetz/project. Accessed 18 May 2022.
Forstner C, Patchev V, Rohde G, Rupp J, Witzenrath M, Welte T, et al. Rate and predictors of bacteremia in afebrile community-acquired pneumonia. Chest. 2019;157(3):529–39.
Lutfiyya MN, Henley E, Chang LF, Reyburn SW. Diagnosis and treatment of community-acquired pneumonia. AFP. 2006;73:442–50.
Self WH, Williams DJ, Zhu Y, Ampofo K, Pavia AT, Chappell JD, et al. Respiratory viral detection in children and adults: comparing asymptomatic controls and patients with community-acquired pneumonia. J Infect Dis. 2016;213:584–91.
Prendki V, Huttner B, Marti C, Mamin A, Fubini PE, Meynet MP, et al. Accuracy of comprehensive PCR analysis of nasopharyngeal and oropharyngeal swabs for CT-scan-confirmed pneumonia in elderly patients: a prospective cohort study. Clin Microbiol Infect. 2019;25:1114–9.
File TM Jr. New diagnostic tests for pneumonia: what is their role in clinical practice? Clin Chest Med. 2011;32:417–30.
Torres A, Lee N, Cilloniz C, Vila J, der Eerden MV. Laboratory diagnosis of pneumonia in the molecular age. Eur Respir J. 2016;48:1764–78.
Chalmers JD, Rother C, Salih W, Ewig S. Healthcare-associated pneumonia does not accurately identify potentially resistant pathogens: a systematic review and meta-analysis. Clin Infect Dis. 2014;58:330–9.
Aliberti S, Cilloniz C, Chalmers JD, Zanaboni AM, Cosentini R, Tarsia P, et al. Multidrug-resistant pathogens in hospitalised patients coming from the community with pneumonia: a European perspective. Thorax. 2013;68:997–9.
Faner R, Sibila O, Agustí A, Bernasconi E, Chalmers JD, Huffnagle GB, et al. The microbiome in respiratory medicine: current challenges and future perspectives. Eur Respir J. 2017;49:1602086.
Charalampous T, Kay GL, Richardson H, Aydin A, Baldan R, Jeanes C, et al. Nanopore metagenomics enables rapid clinical diagnosis of bacterial lower respiratory infection. Nat Biotechnol. 2019;37:783–92.
Franquet T. Imaging of pneumonia: trends and algorithms. Eur Respir J. 2001;18:196–208.
Self WH, Courtney DM, McNaughton CD, Wunderink RG, Kline JA. High discordance of chest X-ray and CT for detection of pulmonary opacities in ED patients: implications for diagnosing pneumonia. Am J Emerg Med. 2013;31:401–5.
Claessens Y-E, Debray M-P, Tubach F, Brun A-L, Rammaert B, Hausfater P, et al. Early chest computed tomography scan to assist diagnosis and guide treatment decision for suspected community-acquired pneumonia. Am J Respir Crit Care Med. 2015;192:974–82.
Haga T, Fukuoka M, Morita M, Cho K, Tatsumi K. Computed tomography for the diagnosis and evaluation of the severity of community-acquired pneumonia in the elderly. Intern Med. 2016;55:437–41.
Nazerian P, Volpicelli G, Vanni S, Gigli C, Betti L, Bartolucci M, et al. Accuracy of lung ultrasound for the diagnosis of consolidations when compared to chest computed tomography. Am J Emerg Med. 2015;33:620–5.
Reissig A, Copetti R, Mathis G, Mempel C, Schuler A, Zechner P, et al. Lung ultrasound in the diagnosis and follow-up of community-acquired pneumonia: a prospective, multicenter, diagnostic accuracy study. Chest. 2012;142:965–72.
Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, et al. Radiological Society of North America expert consensus statement on reporting chest CT findings related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. J Thorac Imaging. 2020. https://doi.org/10.1097/RTI.0000000000000524.
Llamas-Álvarez AM, Tenza-Lozano EM, Latour-Pérez J. Diaphragm and lung ultrasound to predict weaning outcome: systematic review and meta-analysis. Chest. 2017;152:1140–50.
Moore M, Stuart B, Little P, Smith S, Thompson MJ, Knox K, et al. Predictors of pneumonia in lower respiratory tract infections: 3C prospective cough complication cohort study. Eur Respir J. 2017;50:1700434.
van Vugt SF, Broekhuizen BDL, Lammens C, Zuithoff NPA, de Jong PA, Coenen S, et al. Use of serum C reactive protein and procalcitonin concentrations in addition to symptoms and signs to predict pneumonia in patients presenting to primary care with acute cough: diagnostic study. BMJ. 2013. https://doi.org/10.1136/bmj.f2450.
Krüger S, Papassotiriou J, Marre R, Richter K, Schumann C, von Baum H, et al. Pro-atrial natriuretic peptide and pro-vasopressin to predict severity and prognosis in community-acquired pneumonia. Intensive Care Med. 2007;33:2069–78.
Kolditz M, Höffken G, Martus P, Rohde G, Schütte H, Bals R, et al. Serum cortisol predicts death and critical disease independently of CRB-65 score in community-acquired pneumonia: a prospective observational cohort study. BMC Infect Dis. 2012;12:90.
Lepper PM, Ott S, Nuesch E, von Eynatten M, Schumann C, Pletz MW, et al. Serum glucose levels for predicting death in patients admitted to hospital for community acquired pneumonia: prospective cohort study. BMJ. 2012;344: e3397.
Jensen AV, BaunbækEgelund G, Bang Andersen S, Petersen PT, Benfield T, Witzenrath M, et al. The glycemic gap and 90-day mortality in community-acquired pneumonia. A prospective cohort study. Ann ATS. 2019;16:1518–26.
Ebrahimi F, Giaglis S, Hahn S, Blum CA, Baumgartner C, Kutz A, et al. Markers of neutrophil extracellular traps predict adverse outcome in community-acquired pneumonia: secondary analysis of a randomised controlled trial. Eur Respir J. 2018;51:1701389.
Krüger S, Ewig S, Giersdorf S, Hartmann O, Suttorp N, Welte T. Cardiovascular and inflammatory biomarkers to predict short- and long-term survival in community-acquired pneumonia. Am J Respir Crit Care Med. 2010;182:1426–34.
Gutbier B, Neuhauß A-K, Reppe K, Ehrler C, Santel A, Kaufmann J, et al. Prognostic and pathogenic role of angiopoietin-1 and -2 in pneumonia. Am J Respir Crit Care Med. 2018;198:220–31.
Karakioulaki M, Stolz D. Biomarkers in pneumonia—beyond procalcitonin. Int J Mol Sci. 2019;20:2004.
Holub M, Džupová O, Růžková M, Stráníková A, Bartáková E, Máca J, et al. Selected biomarkers correlate with the origin and severity of sepsis. Mediat Inflamm. 2018;2018:7028267.
Vestjens SMT, Spoorenberg SMC, Rijkers GT, Grutters JC, Ten Berg JM, Noordzij PG, et al. High-sensitivity cardiac troponin T predicts mortality after hospitalization for community-acquired pneumonia. Respirology. 2017;22(5):1000–6.
Frencken JF, van Baal L, Kappen TH, Donker DW, Horn J, van der Poll T, et al. Myocardial injury in critically ill patients with community-acquired pneumonia. A cohort study. Ann Am Thorac Soc. 2019;16:606–12.
Corrales-Medina VF, Dwivedi G, Taljaard M, Petrcich W, Lima JA, Yende S, et al. Coronary artery calcium before and after hospitalization with pneumonia: the MESA study. PLoS ONE. 2018;13: e0191750.
Kox WJ, Volk T, Kox SN, Volk H-D. Immunomodulatory therapies in sepsis. Intensive Care Med. 2000;26:S124–8.
Waterer G. Community-acquired pneumonia: genomics, epigenomics, transcriptomics, proteomics, and metabolomics. Semin Respir Crit Care Med. 2012;33:257–65.
Kolditz M, Ewig S, Schütte H, Suttorp N, Welte T, Rohde G. Assessment of oxygenation and comorbidities improves outcome prediction in patients with community-acquired pneumonia with a low CRB-65 score. J Intern Med. 2015;278:193–202.
Lim WS, Smith DL, Wise MP, Welham SA. British thoracic society community acquired pneumonia guideline and the NICE pneumonia guideline: how they fit together. Thorax. 2015;70:698–700.
Frenzen FS, Kutschan U, Meiswinkel N, Schulte-Hubbert B, Ewig S, Kolditz M. Admission lactate predicts poor prognosis independently of the CRB/CURB-65 scores in community-acquired pneumonia. Clin Microbiol Infect. 2018;24:306.e1-306.e6.
Kolditz M, Tesch F, Mocke L, Höffken G, Ewig S, Schmitt J. Burden and risk factors of ambulatory or hospitalized CAP: a population based cohort study. Respir Med. 2016;121:32–8.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315:801–10.
Kolditz M, Scherag A, Rohde G, Ewig S, Welte T, Pletz M, et al. Comparison of the qSOFA and CRB-65 for risk prediction in patients with community-acquired pneumonia. Intensive Care Med. 2016;42:2108–10.
Jiang J, Yang J, Jin Y, Cao J, Lu Y. Role of qSOFA in predicting mortality of pneumonia. Medicine (Baltimore). 2018;97: e12634.
Antcliffe DB, Burnham KL, Al-Beidh F, Santhakumaran S, Brett SJ, Hinds CJ, et al. Transcriptomic signatures in sepsis and a differential response to steroids. From the VANISH randomized trial. Am J Respir Crit Care Med. 2019;199:980–6.
Delahanty RJ, Alvarez J, Flynn LM, Sherwin RL, Jones SS. Development and evaluation of a machine learning model for the early identification of patients at risk for sepsis. Ann Emerg Med. 2019;73:334–44.
Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the hospital readmissions reduction program with mortality among medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA. 2018;320:2542–52.
Ewig S, Kolditz M, Pletz MW, Chalmers J. Healthcare-associated pneumonia: is there any reason to continue to utilize this label in 2019? Clin Microbiol Infect. 2019;25:1173–9.
Lee JS, Giesler DL, Gellad WF, Fine MJ. Antibiotic therapy for adults hospitalized with community-acquired pneumonia: a systematic review. JAMA. 2016;315:593–602.
Pakhale S, Mulpuru S, Verheij TJ, Kochen MM, Rohde GG, Bjerre LM. Antibiotics for community-acquired pneumonia in adult outpatients. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.CD002109.pub4.
Schreiber MP, Shorr AF. Inhaled antibiotics for the treatment of pneumonia. Curr Opin Pulm Med. 2019;25:289–93.
Dandachi D, Rodriguez-Barradas MC. Viral pneumonia: etiologies and treatment. J Investig Med. 2018;66:957–65.
Chalmers JD, Crichton ML, Goeminne PC, Cao B, Humbert M, Shteinberg M, et al. Management of hospitalised adults with coronavirus disease 2019 (COVID-19): a European Respiratory Society living guideline. Eur Respir J. 2021;57:2100048.
Graham F. Daily briefing: Pfizer’s COVID pill looks promising. Nature. 2021. https://doi.org/10.1038/d41586-021-03379-5.
Martin-Loeches I, van Someren GF, Schultz MJ. Bacterial pneumonia as an influenza complication. Curr Opin Infect Dis. 2017;30:201–7.
Deinhardt-Emmer S, Haupt KF, Garcia-Moreno M, Geraci J, Forstner C, Pletz M, et al. Staphylococcus aureus pneumonia: preceding influenza infection paves the way for low-virulent strains. Toxins (Basel). 2019;11:734.
Cawcutt K, Kalil AC. Pneumonia with bacterial and viral coinfection. Curr Opin Crit Care. 2017;23:385–90.
Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26:1622–9.
Bell BG, Schellevis F, Stobberingh E, Goossens H, Pringle M. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis. 2014;14:13.
Yamazaki T, Kenri T. Epidemiology of Mycoplasma pneumoniae infections in Japan and therapeutic strategies for macrolide-resistant M. pneumoniae. Front Microbiol. 2016;7:693.
Peuchant O, Ménard A, Renaudin H, Morozumi M, Ubukata K, Bébéar CM, et al. Increased macrolide resistance of Mycoplasma pneumoniae in France directly detected in clinical specimens by real-time PCR and melting curve analysis. J Antimicrob Chemother. 2009;64:52–8.
Diaz MH, Benitez AJ, Winchell JM. Investigations of Mycoplasma pneumoniae infections in the United States: trends in molecular typing and macrolide resistance from 2006 to 2013. J Clin Microbiol. 2015;53:124–30.
Bassetti M, Welte T, Wunderink RG. Treatment of Gram-negative pneumonia in the critical care setting: is the beta-lactam antibiotic backbone broken beyond repair? Crit Care. 2016;20:1–9.
Nielsen TB, Brass EP, Gilbert DN, Bartlett JG, Spellberg B. Sustainable discovery and development of antibiotics—is a nonprofit approach the future? N Engl J Med. 2019;381:503–5.
Arancibia F, Ruiz M. Risk factors for drug-resistant cap in immunocompetent patients. Curr Infect Dis Rep. 2017;19:11.
Sibila O, Rodrigo-Troyano A, Torres A. Nonantibiotic adjunctive therapies for community-acquired pneumonia (corticosteroids and beyond): where are we with them? Semin Respir Crit Care Med. 2016;37:913–22.
Stefan H, Martin W, Bernd S, Andreas H, Mathias K, Matthias K, et al. Adrenomedullin reduces endothelial hyperpermeability. Circ Res. 2002;91:618–25.
Chalmers JD. Corticosteroids for community-acquired pneumonia: a critical view of the evidence. Eur Respir J. 2016;48:984–6.
Sterne JAC, Murthy S, Diaz JV, Slutsky AS, Villar J, Angus DC, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19. JAMA. 2020;324:1–13.
COVID-19: management in hospitalized adults—UpToDate. https://www.uptodate.com/contents/covid-19-management-in-hospitalized-adults?search=Interleukin%201%20antagonists%20covid§ionRank=1&usage_type=default&anchor=H3001451751&source=machineLearning&selectedTitle=3~150&display_rank=3#H3001451751. Accessed 6 Jan 2022.
Marconi VC, Ramanan AV, de Bono S, Kartman CE, Krishnan V, Liao R, et al. Efficacy and safety of baricitinib for the treatment of hospitalised adults with COVID-19 (COV-BARRIER): a randomised, double-blind, parallel-group, placebo-controlled phase 3 trial. Lancet Respir Med. 2021;9:1407–18.
Guimarães PO, Quirk D, Furtado RH, Maia LN, Saraiva JF, Antunes MO, et al. Tofacitinib in patients hospitalized with Covid-19 pneumonia. N Engl J Med. 2021;385:406–15.
Kyriazopoulou E, Poulakou G, Milionis H, Metallidis S, Adamis G, Tsiakos K, et al. Early treatment of COVID-19 with anakinra guided by soluble urokinase plasminogen receptor plasma levels: a double-blind, randomized controlled phase 3 trial. Nat Med. 2021;27:1752–60.
Caricchio R, Abbate A, Gordeev I, Meng J, Hsue PY, Neogi T, et al. Effect of canakinumab vs placebo on survival without invasive mechanical ventilation in patients hospitalized with severe COVID-19: a randomized clinical trial. JAMA. 2021;326:230–9.
Tharaux PL, Pialoux G, Pavot A, Mariette X, Hermine O, Resche-Rigon M, Porcher R, Ravaud P, Bureau S, Dougados M, Tibi A. Effect of anakinra versus usual care in adults in hospital with COVID-19 and mild-to-moderate pneumonia (CORIMUNO-ANA-1): a randomised controlled trial. Lancet Respir Med. 2021;9:295–304.
Aliberti S, Chalmers JD, Pletz MW. Anti-infectives and the lung. 2017. https://doi.org/10.1183/2312508X.erm7517. Accessed 25 May 2018.
Kanoh S, Rubin BK. Mechanisms of action and clinical application of macrolides as immunomodulatory medications. Clin Microbiol Rev. 2010;23:590–615.
Postma DF, van Werkhoven CH, van Elden LJR, Thijsen SFT, Hoepelman AIM, Kluytmans JAJW, et al. Antibiotic treatment strategies for community-acquired pneumonia in adults. N Engl J Med. 2015;372:1312–23.
Ito A, Ishida T, Tachibana H, Tokumasu H, Yamazaki A, Washio Y. Azithromycin combination therapy for community-acquired pneumonia: propensity score analysis. Sci Rep. 2019;9:1–8.
Okumura J, Shindo Y, Takahashi K, Sano M, Sugino Y, Yagi T, et al. Mortality in patients with community-onset pneumonia at low risk of drug-resistant pathogens: impact of β-lactam plus macrolide combination therapy. Respirology. 2018;23:526–34.
Wunderink RG, Mandell L. Adjunctive therapy in community-acquired pneumonia. Semin Respir Crit Care Med. 2012;33:311–8.
Postma DF, Spitoni C, van Werkhoven CH, van Elden LJR, Oosterheert JJ, Bonten MJM. Cardiac events after macrolides or fluoroquinolones in patients hospitalized for community-acquired pneumonia: post-hoc analysis of a cluster-randomized trial. BMC Infect Dis. 2019;19:1–12.
König R, Cao X, Oswald M, Forstner C, Rohde G, Rupp J, et al. Macrolide combination therapy for hospitalised CAP patients? An individualised approach supported by machine learning. Eur Respir J. 2019;54:1900824.
Welte T, Dellinger RP, Ebelt H, Ferrer M, Opal SM, Singer M, et al. Efficacy and safety of trimodulin, a novel polyclonal antibody preparation, in patients with severe community-acquired pneumonia: a randomized, placebo-controlled, double-blind, multicenter, phase II trial (CIGMA study). Intensive Care Med. 2018;44:438–48.
de la Torre MC, Bolíbar I, Vendrell M, de Gracia J, Vendrell E, Rodrigo MJ, et al. Serum immunoglobulins in the infected and convalescent phases in community-acquired pneumonia. Respir Med. 2013;107:2038–45.
de la Torre MC, Torán P, Serra-Prat M, Palomera E, Güell E, Vendrell E, et al. Serum levels of immunoglobulins and severity of community-acquired pneumonia. BMJ Open Respir Res. 2016;3(1): e000152.
Wienhold S-M, Lienau J, Witzenrath M. Towards inhaled phage therapy in western Europe. Viruses. 2019;11:295.
Dougan M, Nirula A, Azizad M, Mocherla B, Gottlieb RL, Chen P, et al. Bamlanivimab plus etesevimab in mild or moderate Covid-19. N Engl J Med. 2021;385:1382–92.
Group RC, Horby PW, Mafham M, Peto L, Campbell M, Pessoa-Amorim G, et al. Casirivimab and imdevimab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021. https://doi.org/10.1101/2021.06.15.21258542v1.
Tessmer A, Welte T, Schmidt-Ott R, Eberle S, Barten G, Suttorp N, et al. Influenza vaccination is associated with reduced severity of community-acquired pneumonia. Eur Respir J. 2011;38:147–53.
Udell JA, Zawi R, Bhatt DL, Keshtkar-Jahromi M, Gaughran F, Phrommintikul A, et al. Association between influenza vaccination and cardiovascular outcomes in high-risk patients: a meta-analysis. JAMA. 2013;310:1711–20.
Chiang M-H, Wu H-H, Shih C-J, Chen Y-T, Kuo S-C, Chen T-L. Association between influenza vaccination and reduced risks of major adverse cardiovascular events in elderly patients. Am Heart J. 2017;193:1–7.
Fröbert O, Götberg M, Erlinge D, Akhtar Z, Christiansen EH, MacIntyre CR, et al. Influenza vaccination after myocardial infarction: a randomized, double-blind, placebo-controlled, multicenter trial circulation. Am Heart Assoc. 2021;144:1476–84.
Pletz MW, Rohde GG, Welte T, Kolditz M, Ott S. Advances in the prevention, management, and treatment of community-acquired pneumonia. Research. 2016. https://doi.org/10.12688/f1000research.7657.1.
Abbasi J. FLU-v, a universal flu vaccine candidate, advances in trial. JAMA. 2020;323:1336.
Pleguezuelos O, Dille J, de Groen S, Oftung F, Niesters HGM, Islam MA, et al. Immunogenicity, safety, and efficacy of a standalone universal influenza vaccine, FLU-v, in healthy adults. Ann Intern Med. 2020;172:453–62.
Moberley S, Holden J, Tatham DP, Andrews RM. Vaccines for preventing pneumococcal infection in adults. Cochrane Database Syst Rev. 2013;2013:CD000422.
Suzuki M, Dhoubhadel BG, Ishifuji T, Yasunami M, Yaegashi M, Asoh N, et al. Serotype-specific effectiveness of 23-valent pneumococcal polysaccharide vaccine against pneumococcal pneumonia in adults aged 65 years or older: a multicentre, prospective, test-negative design study. Lancet Infect Dis. 2017;17:313–21.
French N, Nakiyingi J, Carpenter LM, Lugada E, Watera C, Moi K, et al. 23–valent pneumococcal polysaccharide vaccine in HIV-1-infected Ugandan adults: double-blind, randomised and placebo controlled trial. Lancet. 2000;355:2106–11.
Pilishvili T, Lexau C, Farley MM, Hadler J, Harrison LH, Bennett NM, et al. Sustained reductions in invasive pneumococcal disease in the era of conjugate vaccine. J Infect Dis. 2010;201:32–41.
Makarewicz O, Lucas M, Brandt C, Herrmann L, Albersmeier A, Rückert C, et al. Whole genome sequencing of 39 invasive Streptococcus pneumoniae sequence type 199 isolates revealed switches from serotype 19A to 15B. PLoS ONE. 2017;12: e0169370.
Pletz MW, Ewig S, Rohde G, Schuette H, Rupp J, Welte T, et al. Impact of pneumococcal vaccination in children on serotype distribution in adult community-acquired pneumonia using the serotype-specific multiplex urinary antigen detection assay. Vaccine. 2016;34:2342–8.
Rodrigo C, Bewick T, Sheppard C, Greenwood S, Mckeever TM, Trotter CL, et al. Impact of infant 13-valent pneumococcal conjugate vaccine on serotypes in adult pneumonia. Eur Respir J. 2015;45:1632–41.
Forstner C, Kolditz M, Kesselmeier M, Ewig S, Rohde G, Barten-Neiner G, et al. Pneumococcal conjugate serotype distribution and predominating role of serotype 3 in German adults with community-acquired pneumonia. Vaccine. 2019;38(5):1129–36.
LeBlanc JJ, ElSherif M, Ye L, MacKinnon-Cameron D, Ambrose A, Hatchette TF, et al. Streptococcus pneumoniae serotype 3 is masking PCV13-mediated herd immunity in Canadian adults hospitalized with community acquired pneumonia: a study from the serious outcomes surveillance (SOS) network of the Canadian immunization research network (CIRN). Vaccine. 2019;37:5466–73.
Azarian T, Mitchell PK, Georgieva M, Thompson CM, Ghouila A, Pollard AJ, et al. Global emergence and population dynamics of divergent serotype 3 CC180 pneumococci. PLoS Pathog. 2018;14: e1007438.
Pletz MW, Maus U, Krug N, Welte T, Lode H. Pneumococcal vaccines: mechanism of action, impact on epidemiology and adaption of the species. Int J Antimicrob Agents. 2008;32:199–206.
Pletz M. Sequential versus simultaneous vaccination with pneumococcal conjugate vaccine (prevenar 13) and pneumococcal polysaccharide vaccine (pneumovax 23) in elderly: immunological memory and antibody levels. clinicaltrials.gov; 2021. Report No. NCT02637583. https://clinicaltrials.gov/ct2/show/NCT02637583.
Green C, Moore CA, Mahajan A, Bajaj K. A simple approach to pneumococcal vaccination in adults. J Glob Infect Dis. 2018;10:159–62.
Oligbu G. Higher valent pneumococcal conjugate vaccines: is it a roller coaster? AIMS Public Health. 2020;7:29–32.
Lagousi T, Basdeki P, Routsias J, Spoulou V. Novel protein-based pneumococcal vaccines: assessing the use of distinct protein fragments instead of full-length proteins as vaccine antigens. Vaccines (Basel). 2019;7:E9.
Green CA, Drysdale SB, Pollard AJ, Sande CJ. Vaccination against respiratory syncytial virus. Vaccines Older Adults Curr Pract Future Oppor. 2020;43:182–92.
Ponnuraj EM, Springer J, Hayward AR, Wilson H, Simoes EAF. Antibody-dependent enhancement, a possible mechanism in augmented pulmonary disease of respiratory syncytial virus in the bonnet monkey model. J Infect Dis. 2003;187:1257–63.
Boyton RJ, Openshaw PJ. Pulmonary defences to acute respiratory infection. Br Med Bull. 2002;61:1–12.
Sun X, Wang T, Cai D, Hu Z, Chen J, Liao H, et al. Cytokine storm intervention in the early stages of COVID-19 pneumonia. Cytokine Growth Factor Rev. 2020;53:38–42.
Crane MJ, Lee KM, FitzGerald ES, Jamieson AM. Surviving deadly lung infections: innate host tolerance mechanisms in the pulmonary system. Front Immunol. 2018;9:1421.
Müller-Redetzky H, Lienau J, Suttorp N, Witzenrath M. Therapeutic strategies in pneumonia: going beyond antibiotics. Eur Respir Rev. 2015;24:516–24.
Smelaya TV, Belopolskaya OB, Smirnova SV, Kuzovlev AN, Moroz VV, Golubev AM, et al. Genetic dissection of host immune response in pneumonia development and progression. Sci Rep. 2016;6:1–12.
Wang X, Guo J, Wang Y, Xiao Y, Wang L, Hua S. Genetic variants of interferon regulatory factor 5 associated with the risk of community-acquired pneumonia. Gene. 2018;679:73–80.
Kloek AT, Brouwer MC, van de Beek D. Host genetic variability and pneumococcal disease: a systematic review and meta-analysis. BMC Med Genom. 2019;12:130.
Reyes LF, Restrepo MI, Hinojosa CA, Soni NJ, Anzueto A, Babu BL, et al. Severe pneumococcal pneumonia causes acute cardiac toxicity and subsequent cardiac remodeling. Am J Respir Crit Care Med. 2017;196:609–20.
Brack MC, Lienau J, Kuebler WM, Witzenrath M. Cardiovascular sequelae of pneumonia. Curr Opin Pulm Med. 2019;25:257–62.
Aliberti S, Ramirez J, Cosentini R, Valenti V, Voza A, Rossi P, et al. Acute myocardial infarction versus other cardiovascular events in community-acquired pneumonia. ERJ Open Res. 2015. https://doi.org/10.1183/23120541.00020-2015.
Jensen AV, Faurholt-Jepsen D, Egelund GB, Andersen SB, Petersen PT, Benfield T, et al. Undiagnosed diabetes mellitus in community-acquired pneumonia: a prospective cohort study. Clin Infect Dis. 2017;65:2091–8.
Aliberti S, Di Pasquale M, Zanaboni AM, Cosentini R, Brambilla AM, Seghezzi S, et al. Stratifying risk factors for multidrug-resistant pathogens in hospitalized patients coming from the community with pneumonia. Clin Infect Dis. 2012;54:470–8.
Di Pasquale MF, Sotgiu G, Gramegna A, Radovanovic D, Terraneo S, Reyes LF, et al. Prevalence and etiology of community-acquired pneumonia in immunocompromised patients. Clin Infect Dis. 2019;68:1482–93.
Scholl T, Kiser TH, Vondracek SF. Evaluation of systemic corticosteroids in patients with an acute exacerbation of COPD and a diagnosis of pneumonia. Chronic Obstr Pulm Dis. 2018;5:57–65.
Zugazagoitia J, Molina-Pinelo S, Lopez-Rios F, Paz-Ares L. Biological therapies in nonsmall cell lung cancer. Eur Respir J. 2017;49:1601520.
Faverio P, Aliberti S, Bellelli G, Suigo G, Lonni S, Pesci A, et al. The management of community-acquired pneumonia in the elderly. Eur J Intern Med. 2014;25:312–9.
Aliberti S, Bellelli G, Belotti M, Morandi A, Messinesi G, Annoni G, et al. Delirium symptoms during hospitalization predict long-term mortality in patients with severe pneumonia. Aging Clin Exp Res. 2015;27:523–31.
Restrepo MI, Reyes LF. Pneumonia as a cardiovascular disease. Respirology. 2018;23:250–9.
Corrales-Medina VF, Musher DM, Shachkina S, Chirinos JA. Acute pneumonia and the cardiovascular system. Lancet. 2013;381:496–505.
Eurich DT, Marrie TJ, Minhas-Sandhu JK, Majumdar SR. Ten-year mortality after community-acquired pneumonia. A prospective cohort. Am J Respir Crit Care Med. 2015;192:597–604.
Eurich DT, Marrie TJ, Minhas-Sandhu JK, Majumdar SR. Risk of heart failure after community acquired pneumonia: prospective controlled study with 10 years of follow-up. BMJ. 2017;356: j413.
Jaw JE, Tsuruta M, Oh Y, Schipilow J, Hirano Y, Ngan DA, et al. Lung exposure to lipopolysaccharide causes atherosclerotic plaque destabilisation. Eur Respir J. 2016;48:205–15.
Corrales-Medina VF, Alvarez KN, Weissfeld LA, Angus DC, Chirinos JA, Chang C-CH, et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA. 2015;313:264–74.
Dela Cruz CS, Wunderink RG, Christiani DC, Cormier SA, Crothers K, Doerschuk CM, et al. Future research directions in pneumonia. NHLBI working group report. Am J Respir Crit Care Med. 2018;198:256–63.
Acknowledgements
CAPNETZ is a multidisciplinary approach to better understand and treat patients with community-acquired pneumonia. The network has only been made possible by the contribution of many investigators. We are especially indebted to the work of the investigators in the local clinical centres (LCC) that established and maintained contact with all practitioners, physicians, and respiratory specialists cooperating within the network. The members of the CAPNETZ study group are as follows:
M. Dreher, C. Cornelissen (Aachen); W. Knüppel (Bad Arolsen); D. Stolz (Basel, Switzerland); N. Suttorp, M. Niebank, A. Mikolajewska, M. Witzenrath, W. Pankow, S. Gläser, D. Thiemig (Berlin); M. Prediger, S. Schmager (Cottbus); M. Kolditz, B. Schulte-Hubbert, S. Langner (Dresden); G. Rohde, C. Bellinghausen (Frankfurt); M. Panning (Freiburg); C. Hoffmann (Hamburg); T. Welte, J. Freise, G. Barten, W. Kröner, M. Nawrocki, J. Naim, T. Illig, N. Klopp (Hannover); M. Pletz, C. Kroegel, B. Schleenvoigt, C. Forstner, A. Moeser (Jena); D. Drömann, P. Parschke, K. Franzen, J. Rupp, N. Käding (Lübeck); M. Wouters, K. Walraven, D. Braeken (Maastricht, The Netherlands); C. Spinner (Munich); A. Zaruchas (Paderborn); Schaberg, D. Heigener, I. Hering (Rotenburg/Wümme); W. Albrich, F. Waldeck, F. Rassouli, S. Baldesberger (St. Gallen, Switzerland); S. Stenger, M. Wallner (Ulm); H. Burgmann, L. Traby (Vienna); and all study nurses.
We sincerely thank the international CAP experts for their important and invaluable feedback. Without their contribution, this work would not have been possible.
Funding
Open Access funding enabled and organized by Projekt DEAL. CAPNETZ was funded by a German Federal Ministry of Education and Research grant (01KI07145) 2001–2011 and is supported by the German Center for Lung Research (DZL).
Author information
Authors and Affiliations
Contributions
GBN, as part of CAPNETZ, was responsible for organizing the meeting. AVJ was responsible for grouping the views from the invited researchers into headlines for discussion at the scientific retreat. CD took minutes during the scientific retreat which was used for drafting the individual sections. The individual sections were then drafted by one of the participants of the scientific retreat as follows; Detection of causative pathogens (JR), Next generation sequencing for guidance of antimicrobial treatment (JDC), Imaging diagnostics (SD), Biomarkers (DS). Risk stratification (MK), Antiviral and antibiotic treatment (GR), Adjunctive therapy (NS), Vaccines and prevention (MWP, CB), Systemic and local immune response (MW), Comorbidities (SA), Long-term cardio-vascular complications (WMK). AVJ and MWP reviewed the individual sections and prepared the first draft. All authors reviewed the draft manuscript. All authors were responsible for the decision to publish the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interests relevant to the content of the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pletz, M.W., Jensen, A.V., Bahrs, C. et al. Unmet needs in pneumonia research: a comprehensive approach by the CAPNETZ study group. Respir Res 23, 239 (2022). https://doi.org/10.1186/s12931-022-02117-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-022-02117-3