Abstract
Background
Coronary artery disease (CAD) is a common comorbidity of chronic obstructive pulmonary disease (COPD). However, data related to the impact of CAD on outcomes of acute exacerbation of COPD (AECOPD) are limited and whether the relationship depends on sex remains unknown. Our aim was to determine the impact of comorbid CAD on clinical outcomes among men and women with AECOPD.
Methods
We used data from the acute exacerbation of chronic obstructive pulmonary disease inpatient registry (ACURE) study, which is a nationwide observational real-world study conducted between September 2017 and February 2020 at 163 centers in patients admitted with AECOPD as their primary diagnosis. Patients were stratified according to the presence or absence of CAD in men and women. The primary outcomes were the length of hospital stay and economic burden during hospitalization.
Results
Among 3906 patients included in our study, the prevalence of CAD was 17.0%, and it was higher in women than in men (19.5% vs. 16.3%; P = 0.034). Age and other cardiovascular diseases were common factors associated with comorbid CAD in men and women, while body-mass index, cerebrovascular disease, and diabetes were determinants in men and pre-admission use of long-acting beta-adrenoceptor agonist and home oxygen therapy were protective factors in women. Only in men, patients with CAD had a longer length of hospital stay (median 10.0 vs. 9.0 days, P < 0.001), higher total cost during hospitalization (median $1502.2 vs. $1373.4, P < 0.001), and more severe COPD symptoms at day 30 compared to those without CAD. No significant difference was found in women. Comorbid CAD showed no relationship with 30-day readmission or death regardless of sex. In our real-world study, mortality/readmission risk within 30 days increased in patients with previous frequent hospitalizations and poorer pulmonary function.
Conclusions
In hospitalized AECOPD patients, comorbid CAD was significantly associated with poorer short-term outcomes in men. Clinicians should have heightened attention for men with comorbid CAD to achieve an optimal management of AECOPD patients.
Similar content being viewed by others
Background
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality worldwide that induces a considerable economic and social burden [1]. Comorbidities are common at any severity of COPD that may have a significant impact on disease process [1]. Among hospitalized population with an acute exacerbation of COPD (AECOPD) and severe airflow limitation, severe coronary artery disease (CAD) is present in about one-third of patients [2]. Moreover, patients with reduced lung function are at higher risk of developing CAD [3]. Early identification and proper management of these patients might improve the prognosis and reduce the risk of death.
Patients with COPD and CAD have specific clinical characteristics including more frequent respiratory symptoms, worse health status, and higher medication expenditure [4,5,6]. However, researches about the impact of comorbid CAD on clinical outcomes in AECOPD patients are limited. A single center historical cohort study including 507 separate hospital admissions for AECOPD reported that comorbid CAD was associated with longer length of stay, greater risk of intensive care unit (ICU) admission, and death [7]. This study has a relatively small sample size and did not investigate the impact of CAD on symptoms, economic burden of hospitalization, and future exacerbations or mortality among AECOPD patients.
Many studies have shown differences between men and women regarding the prevalence and clinical characteristics of comorbidities such as cardiovascular disease (CVD), bronchiectasis, and metabolic syndrome in COPD [8,9,10]. A multicenter study of patients hospitalized for COPD exacerbations showed that women had a lower prevalence of CAD but presented more chronic heart failure [11]. Instead, a 10-year study in subjects hospitalized due to COPD in Beijing reported that the prevalence of CAD decreased with years in men but increased in women, and reached to be similar between men and women at the end of the study [12]. The burden of CAD in the current Chinese AECOPD population remains unclear. Furthermore, scarce data exist in analyzing the sex-related differences in AECOPD outcomes according to the presence or absence of CAD.
This multicenter real-world study aimed to investigate the predictors of comorbid CAD in AECOPD patients according to sex and assess the effect of CAD on the length of hospital stay, healthcare costs, and change of symptom score during hospitalization in men and women among patients admitted for AECOPD. We additionally aimed to study whether the contribution of comorbid CAD to symptoms and readmissions or death within 30 days after discharge differed by sex and explore the factors associated with readmissions or death after 30 days.
Methods
Study design and patients
This study analyzed data from the acute exacerbation of chronic obstructive pulmonary disease inpatient registry (ACURE) study. The ACURE study is an ongoing, nationwide multicenter, observational patient registry designed to investigate the clinical characteristics, treatments, and prognoses of Chinese patients admitted for AECOPD in a real-world setting. It started from September 2017 and planned to recruit 7600 hospitalized COPD patients due to exacerbation with a 3-year follow-up. Details of the ACURE study design have been previously described [13]. The study was approved by the ethics committee of China-Japan Friendship Hospital (No. 2015-88) and informed consent was obtained from all involved participants. This study was conducted in accordance with the Declaration of Helsinki.
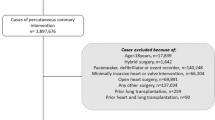
Data on February 25th, 2020 (Phase I) in the ACURE study from 163 centers were reviewed in our study. The eligibility criteria for AECOPD patients were: (1) ≥ 18 years old; (2) inpatients with a primary diagnosis of AECOPD; (3) the presence of post-bronchodilator forced expiratory volume in 1 s (FEV1)/forced vital capacity (FVC) ratio < 0.70 at baseline. Patients were excluded if they participated in other clinical trials or withdrew the informed consent. The flow chart of patient enrollment is shown in Fig. 1. We grouped the study population according to sex and the status of CAD.
Measurements
At admission, we extracted the baseline characteristics including age, sex, body-mass index (BMI), smoking status, the number of hospital or emergency admissions in the previous year, symptoms, modified Medical Research Council (mMRC) dyspnea grade, COPD Assessment Test (CAT) score, pulmonary function, pre-admission medications, and pre-admission non-drug therapy. Data on heart rate, respiratory rate, blood tests, drug treatment, intensive care unit (ICU) admission, length of hospital stay, total cost during hospitalization, and CAT score at discharge were all collected. Total costs were shown in US dollars using the average exchange rate in 2019 (one US dollar was equivalent to 6.90 yuan). We recorded the mMRC dyspnea grade, CAT score, and St George’s Respiratory Questionnaire (SGRQ) score at day 30 after discharge and readmissions or death within 30 days following discharge.
Comorbidities confirmed based on patient history, symptoms, and relevant examinations or former diagnoses according to the historical clinical records were also reviewed, including respiratory disease (asthma, bronchiectasis, lung cancer, pulmonary artery hypertension, sleep apnea syndrome, and pneumonia), CVD (CAD, hypertension, acute or chronic heart failure, and arrhythmia), digestive disease (gastroesophageal reflux disease, peptic ulcer, and chronic gastritis), cerebrovascular disease, endocrine and metabolic disease (diabetes and osteoporosis), and other malignant tumors. CAD was defined as stable angina pectoris, unstable angina pectoris, and myocardial infarction in accordance with relevant diagnostic criteria [14,15,16] or former diagnosis of CAD.
Outcomes
The primary outcomes were the length of hospital stay and cost during hospitalization. The secondary outcomes were the change of CAT score at discharge compared to admission, mMRC dyspnea grade at day 30, CAT score at day 30, SGRQ score at day 30, all-cause readmission or death within 30 days, and AECOPD readmission within 30 days.
Statistical analyses
Medians (interquartile range, IQR) or means (standard deviation, SD) were used to describe continuous data, and frequencies (percentage) were calculated for categorical data. The continuous variables were compared using the Mann–Whitney U test and categorical variables were compared using the chi-squared test or Fisher’s exact test. Multivariate logistic regression analyses (baseline variables were considered if they showed a P-value < 0.10 in univariate analyses) were performed to identify independent risk factors associated with comorbid CAD in men and women.
Cox proportional hazard regression model was used to determine variables associated with all-cause readmission or death within 30 days or AECOPD readmission within 30 days. We included the following clinically significant variables when studying potential in the univariate analyses: sex, status of CAD, age, BMI, smoking status, hospital admissions in the previous year, mMRC dyspnea grade and CAT score at admission, post-bronchodilator FEV1% predicted, comorbidities, blood gas, neutrophil-to-lymphocyte ratio (NLR), eosinophil count, N-terminal pro-B-type natriuretic peptide (NT-proBNP), C-reactive protein (CRP), procalcitonin (PCT), and drug treatment during hospitalization. Each variable was initially tested individually before we added those variables having a univariate association (P < 0.10) to the multivariate model. All analyses were carried out using the software IBM-SPSS statistics 25. Unless stated otherwise, a two-sided P-value < 0.05 was considered statistically significant.
Results
Baseline characteristics
Of the 3906 subjects included in the study, 664 (17.0%) had comorbid CAD. Baseline characteristics of the study patients are shown in Table 1. AECOPD patients combined with CAD were older, more likely to be ex-smokers, and had a higher BMI. Moreover, comorbid CAD was associated with increased cough, a higher CAT score, and more cardiovascular, cerebrovascular, and diabetic comorbidities. There was no difference in the post-bronchodilator FEV1% predicted, although the median FEV1/FVC ratio seemed to be higher in patients with CAD.
The prevalence of CAD was 16.3% in men and 19.5% in women (P = 0.034) (Table 1). The age and prevalence of cardiovascular and diabetic comorbidities were higher in patients with CAD for both men and women. However, in men, BMI and the proportion of ex-smokers and patients with increased cough or cerebrovascular comorbidity were significantly higher in subjects with CAD than in those without CAD, which was not the case in women. Compared with men, women used less long-acting muscarinic receptor antagonist (LAMA), long-acting beta-adrenoceptor agonist (LABA), and inhaled corticosteroids (ICS) before admission (all P < 0.001). Further analyses showed that only in women, comorbid CAD was associated with less use of pre-admission LAMA and LABA (Table 1).
Examinations and treatments during hospitalization
As for laboratory tests during hospitalization, patients with CAD had higher values of eosinophils, blood urea nitrogen, creatinine, blood glucose, and NT-proBNP. During hospitalization, short-acting bronchodilator (SABD), LABA, ICS, and systemic corticosteroids were all prescribed more often to patients without CAD than to those with CAD. Patients with comorbid CAD had a higher rate of ICU admission (P = 0.022). Details are shown in Table 2.
Only in men, comorbid CAD was significantly related to higher levels of eosinophils, creatinine, blood glucose, and NT-proBNP (Table 2). As for treatments during hospitalization, in men, patients with CAD were less likely to be prescribed SABD than those without (P = 0.042), but the difference was not statistically significant between the two groups in women (P = 0.277). Additionally, the rate of ICU admission was higher in cases with CAD compared to those without in men (P = 0.013) but similar between the two groups in women (P = 1.000) (Table 2).
Sex differences in the predictors of comorbid CAD
In men, age, BMI, hypertension, heart failure, arrhythmia, cerebrovascular disease, and diabetes were independently associated with the prevalence of CAD in AECOPD patients (Table 3). However, in women, multivariate analysis indicated that cerebrovascular disease and diabetes were weakly linked to comorbid CAD. Pre-admission use of LABA and home oxygen therapy indicated a lower possibility of comorbid CAD in women (Table 3).
Clinical outcomes during hospitalization
For all patients enrolled in our study, comorbid CAD was associated with a longer length of hospital stay and higher total cost (Table 4). In men, the median time in hospital was significantly longer in those with CAD than in those without CAD (median 10.0 days vs. 9.0 days, P < 0.001), whereas no statistical difference was found between the two groups in women (Table 4). Similarly, the total cost during hospitalization was significantly higher only in men with CAD than in those without CAD (median $1502.2 vs. $1373.4, P < 0.001) (Table 4). In particular, medicine fee in men was numerically higher for those with CAD (Fig. 2A). However, in women, almost all types of costs during hospitalization showed no significant differences between the two groups (Fig. 2B). As for the change of CAT score at discharge compared to admission, only men showed a significant difference between those with and without CAD (Table 4).
Clinical outcomes within 30 days after discharge
A total of 2407 (61.6%) patients had follow-up data within 30 days after discharge. Baseline characteristics were largely similar among patients with and without follow-up data (see Additional file 1: Table S1). Subjects with comorbid CAD had a higher mMRC dyspnea grade at day 30 than those without CAD in both men and women, but only in men, comorbid CAD was associated with a higher CAT score at day 30 (Table 4). No significant difference was found for the SGRQ score (Table 4).
The 30-day all-cause readmission or death and AECOPD readmission occurred in 3.4% and 2.4% of the 2407 patients, respectively. The all-cause readmission or death rates and the AECOPD readmission rates showed no differences between patients with and without CAD regardless of sex (Table 4). Cox regression analyses showed that sex and CAD were not statistically significant risk factors for all-cause readmission or death (Table 5) or AECOPD readmission (see Additional file 1: Table S2). Further analysis indicated that the number of hospital admissions ≥ 2 in the previous year contributed independently to a higher risk of readmission or death, whereas higher FEV1% predicted had a protective effect against 30-day readmission or death.
Discussion
To the best of our knowledge, this is the first and largest study using real-world data to investigate sex differences in AECOPD outcomes according to the presence or absence of CAD. We found that 17.0% of patients admitted with AECOPD had concomitant CAD and this frequency was higher in women in our study. The predictors of comorbid CAD showed obvious sex difference. In addition, only in men, comorbid CAD was associated with a longer length of hospital stay and higher total cost. For women, comorbid CAD did not significantly influence the clinical outcomes. Sex and CAD were not relevant to readmissions or death within 30 days after discharge.
COPD characterized by low-grade systemic inflammation plays a role in the development or acceleration of CVD [17]. A large meta-analysis reported that COPD patients had a two times higher risk of CAD [18]. However, CAD prevalence rates in COPD patients range from 3 to 64% [18], partly due to the different severity of COPD and also because pulmonary symptoms can mimic and mask the symptoms of CVD leading to misdiagnosis or missed diagnosis. Although studies have showed that exacerbations confer an increased risk of subsequent cardiovascular events [19], data about the prevalence of CAD in AECOPD are limited. The prevalence rate in this study was similar to 17.0% reported by Almagro et al. [11], but lower than 28.8% reported by Aliyali et al. who recruited older participants aged over 50 in their study [7]. Contrary to the results found by Almagro et al. [11], the prevalence of CAD in our study was higher in women than in men. This might be related to insufficient pre-admission treatment in women including the use of LABA and home oxygen therapy acting as protective factors against comorbid CAD. In fact, a study in hospitalized COPD patients in China has reported that for CAD, the prevalence in men decreased and that for women increased year by year, which could be partly explained by the increase of occupational exposure and social or psychological stress in women [12].
Common cardiovascular risk factors including age, BMI, hypertension, and diabetes were also independently associated with the prevalence of CAD in men admitted for AECOPD in our study. The results were in line with the findings of Bellocchia et al. that age and BMI were predictive factors of CAD, although their study recruited patients with stable COPD [20]. In addition, both hypertension and diabetes can cause structural alterations of lung and heart tissue due to systemic inflammation or oxidative stress, which were highly associated not only with the development of CVD but also with the pathogenesis of COPD [21]. Moreover, cerebrovascular disease and other types of CVD might be independently associated with comorbid CAD considering a number of shared risk factors (e.g., age and obesity) between them.
In women, the role of BMI, cerebrovascular disease, and diabetes became less important when assessing the risk of comorbid CAD. Similarly, a large study based on 2046 stable COPD patients reported that in men, age, BMI, smoking status, mMRC, energy, and pulmonary function were related to cardiac disease, while in women the predictors only included age [8]. Of note, we found pre-admission use of LABA and home oxygen therapy were protective factors against comorbid CAD in women but showed no relationship with comorbid CAD in men. Although evidence for the safety of LABA in patients with concomitant COPD and CVD is less definitive, many studies including randomized controlled trials and post-hoc analyses have concluded that LABA administration does not increase the risk of cardiovascular events in patients with COPD [22, 23]. There are also data suggesting that LABA can produce a positive impact on reducing the risk of CVD. An interventional, randomized, double-blind clinical trial showed that a clinically relevant improvement of dyspnea with indacaterol was associated with a significant increase of the right ventricular compliance indexes [24]. Inhaled LABA also had direct benefits on pulmonary haemodynamics [25] and reduced exacerbations in COPD patients [26], which could lead to an increased risk of CVD [19]. The reason for different roles of LABA in men and women was not clear but might be partly explained by the sex differences in response to LABA.
In our study, comorbid CAD was associated with poorer short-term outcomes. This was consistent with previous studies. Aliyali et al. reported that the median length of stay was 7 days in patients with CAD versus 6 days for patients without CAD and the adjusted odds ratio for the risk of ICU admission in patients with CAD was 2.97 [7]. Another study analyzing stable-state data of 386 subjects from the London COPD Cohort showed that patients with CAD had significantly worse health status, lower exercise capacity, and more dyspnea as well as longer exacerbations [5]. However, as far as we know, no research has investigated the sex-related differences in the effect of comorbid CAD on AECOPD outcomes. We found that only in men, comorbid CAD was associated with a higher rate of ICU admission and longer length of hospital stay. The following reasons may account for the poorer outcomes in men with CAD. For the population in the ACURE study, only in men, patients with CAD had a higher level of NT-proBNP proposed as a marker of left ventricular and endothelial dysfunction and early mortality in patients with AECOPD [27]. The proportion of patients prescribed SABD during hospitalization was significantly lower in men with CAD than those without. Less use of SABDs, which were recommended as the initial bronchodilators for AECOPD [1], could result in inadequate symptom control.
Several studies demonstrated a substantial economic burden associated with comorbid CVD among COPD patients. In a nationally representative population of COPD adults in the United States, presence of CVD was associated with higher annual healthcare expenditure and resource utilization [28]. A population study using health administrative data for over 7 million people in Canada reported that individuals with COPD had more health service claims including higher claim rates of emergency department visits and hospitalizations for CVD compared to the general population [29].
The impact of comorbid CAD on the economic burden during an AECOPD and whether it differs by sex remain unclear. Our study showed that patients with CAD had a higher economic burden of hospitalization than those without CAD, but the difference was significant only in men. In particular, accounting for the highest proportion of total cost, medicine fee was also numerically higher in men with CAD. This might be related to their serious conditions indicated by the higher rate of ICU admission and longer length of hospital stay.
In our analyses, COPD symptoms assessed by the CAT score and mMRC dyspnea grade were more severe in patients with CAD at day 30, especially in men with CAD, although the decreases of CAT score during hospitalization were more significant among patients with CAD. No relationship was found between comorbid CAD and all-cause readmission or death or AECOPD readmission within 30 days regardless of sex. To our best knowledge, there is no relevant research comparing the risk of readmission or death after 30 days between AECOPD patients with and without comorbid CAD.
A prospective observational study in 2887 COPD patients enrolled from primary care claimed that there was no difference in the annualized rate of AECOPD and mortality between those with or without CVD during the 24-month follow-up period and sensitivity analyses for each CVD diagnosis also did not show any relationship between individual CVD and the incidence of exacerbations [30]. Patel et al. recruiting patients from the London COPD Cohort conducted a prospective evaluation of exacerbations in those who had completed symptom diaries for ≥ 1 year and reported a longer duration but not an increased frequency of AECOPD in patients with CAD [5]. However, when the follow-up period was extended to more than 5 years, data from two population-based cohorts showed that the presence of respiratory impairment and comorbid CVD predicted higher mortality and higher risk of all-cause hospitalization [31]. In addition, in our real-world study with relatively recent recruitment of AECOPD patients, variables associated with a higher risk of 30-day readmission or death were frequent hospitalizations and lower FEV1% predicted.
Indeed, data on differences between the sexes in COPD with comorbidities are scarce. In patients with COPD, it has been suggested that there are substantial differences between men and women in airway anatomy, with women exhibiting smaller lumina and disproportionately thicker airway walls than men [32]. Furthermore, important differences in biology, genetic susceptibility to airway damage, and lung microbiome have been reported [33]. These differences between men and women with COPD may have a role in differently influencing the characteristics of COPD comorbidities. In fact, the protective role of estrogens in regulating the contractility of airway smooth muscles [34] and in the cardiovascular system [35] probably reduces the adverse effects of comorbid CAD on women. The potential differences in prognosis and complicated mechanisms need to be further studied.
The strength of our study was that we used real-world data from the ACURE study which was the first and largest registry of hospitalized AECOPD patients in China. Our analyses provided a comprehensive overview of the clinical characteristics and outcomes of in-hospital AECOPD patients. Moreover, all patients had a diagnosis of COPD confirmed by spirometry at baseline. This study also had several limitations. First, data on treatments for CAD before and during hospitalization were unavailable in the ACURE study, which could also affect clinical outcomes. Second, patients in our study might be admitted to the hospital at different periods of their exacerbations and there was no accurate data regarding when their symptoms started. Some patients might be admitted earlier in their exacerbation course, which potentially confounded the results. However, this real-world study reflected the realities of patients requiring hospitalization and provided valuable information for clinical practice. Such data collection will be planned in our future studies. Third, there were missing data (e.g., blood gas) in a portion of patients. Fourth, not all patients in our study had follow-up data within 30 days after discharge. However, the baseline characteristics were largely similar between those with or without follow-up data, making selective bias less likely. Finally, no long-term prognostic analysis was performed because the ACURE study is still ongoing with only the 30-day data available.
Conclusions
Using data from a large AECOPD cohort, we revealed the different role of clinical characteristics in men and women in evaluating the risk of comorbid CAD. For men hospitalized for AECOPD, comorbid CAD was associated with a higher rate of ICU admission, longer length of hospital stay, higher economic burden of hospitalization, and more severe COPD symptoms at day 30. No significant difference was found in women. Comorbid CAD showed no relationship with 30-day readmission or death regardless of sex. Clinicians should have heightened attention for men with comorbid CAD to achieve an optimal management of AECOPD patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CAD:
-
Coronary artery disease
- COPD:
-
Chronic obstructive pulmonary disease
- AECOPD:
-
Acute exacerbation of COPD
- ACURE:
-
Acute exacerbation of chronic obstructive pulmonary disease inpatient registry
- ICU:
-
Intensive care unit
- CVD:
-
Cardiovascular disease
- FEV1:
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- BMI:
-
Body-mass index
- mMRC:
-
Modified Medical Research Council
- CAT:
-
COPD assessment test
- SGRQ:
-
St George’s respiratory questionnaire
- IQR:
-
Interquartile range
- SD:
-
Standard deviation
- NLR:
-
Neutrophil-to-lymphocyte ratio
- NT-proBNP:
-
N-terminal pro-B-type natriuretic peptide
- CRP:
-
C-reactive protein
- PCT:
-
Procalcitonin
- LAMA:
-
Long-acting muscarinic receptor antagonist
- LABA:
-
Long-acting beta-adrenoceptor agonist
- ICS:
-
Inhaled corticosteroids
- SAS:
-
Sleep apnea syndrome
- OCS:
-
Oral corticosteroids
- SABD:
-
Short-acting bronchodilator
- PaO2:
-
Partial pressure of oxygen
- PaCO2:
-
Partial pressure of carbon dioxide
- WBCs:
-
White blood cells
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- BUN:
-
Blood urea nitrogen
- Cr:
-
Creatinine
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
References
Committee GE. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease (2021 REPORT). http://goldcopd.com. Accessed Nov 2020.
Leong P, Bardin PG. The untreated treatable trait: cardiovascular disease in COPD exacerbations. Respirology. 2021;26(5):413–5.
Lee HM, Liu MA, Barrett-Connor E, Wong ND. Association of lung function with coronary heart disease and cardiovascular disease outcomes in elderly: the Rancho Bernardo study. Respir Med. 2014;108(12):1779–85.
Yangui F, Touil A, Antit S, Zakhama L, Charfi MR. COPD prevalence in smokers with stable ischemic heart disease: a cross-sectional study in Tunisia. Respir Med. 2021;179:106335.
Patel ARC, Donaldson GC, Mackay AJ, Wedzicha JA, Hurst JR. The impact of ischemic heart disease on symptoms, health status, and exacerbations in patients with COPD. Chest. 2012;141(4):851–7.
Rysiak E, Prokop I, Zaręba I, Mróz RM. Estimates of medication expenditure for ischemic heart disease accompanying chronic obstructive pulmonary disease. Adv Exp Med Biol. 2018;1114:49–55.
Aliyali M, Mehravaran H, Abedi S, Sharifpour A, Yazdani CJ. Impact of comorbid ischemic heart disease on short-term outcomes of patients hospitalized for acute exacerbations of COPD. Tanaffos. 2015;14(3):165–71.
Trudzinski FC, Kellerer C, Jörres RA, Alter P, Lutter JI, Trinkmann F, et al. Gender-specific differences in COPD symptoms and their impact for the diagnosis of cardiac comorbidities. Clin Res Cardiol. 2021;
Sánchez-Muñoz G, Lopez-de-Andrés A, Hernández-Barrera V, Jiménez-García R, Pedraza-Serrano F, Puente-Maestu L, et al. Bronchiectasis in patients hospitalized with acute exacerbation of COPD in Spain: influence on mortality, hospital stay, and hospital costs (2006–2014) according to gender. PLoS ONE. 2019;14(1):e0211222.
Choi HS, Rhee CK, Park YB, Yoo KH, Lim SY. Metabolic syndrome in early chronic obstructive pulmonary disease: gender differences and impact on exacerbation and medical costs. Int J Chron Obstruct Pulmon Dis. 2019;14:2873–83.
Almagro P, López García F, Cabrera FJ, Montero L, Morchón D, Díez J, et al. Comorbidity and gender-related differences in patients hospitalized for COPD. The ECCO study. Respir Med. 2010;104(2):253–9.
Cui H, Miao DM, Wei ZM, Cai JF, Li Y, Liu AM, et al. Prevalence of cardiovascular disease in subjects hospitalized due to chronic obstructive pulmonary disease in Beijing from 2000 to 2010. J Geriatr Cardiol. 2012;9(1):5–10.
Pei Z, Sun Y, Wang S, Chen Y, Yang T, Huang K, et al. Estimating mortality among inpatients with acute exacerbation of chronic obstructive pulmonary disease using registry data. NPJ Prim Care Respir Med. 2020;30(1):28.
Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34(38):2949–3003.
Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130(25):e344-426.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Corlateanu A, Covantev S, Mathioudakis AG, Botnaru V, Siafakas N. Prevalence and burden of comorbidities in chronic obstructive pulmonary disease. Respir Investig. 2016;54(6):387–96.
Chen W, Thomas J, Sadatsafavi M, FitzGerald JM. Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(8):631–9.
Kunisaki KM, Dransfield MT, Anderson JA, Brook RD, Calverley PMA, Celli BR, et al. Exacerbations of chronic obstructive pulmonary disease and cardiac events. A post hoc cohort analysis from the SUMMIT randomized clinical trial. Am J Respir Crit Care Med. 2018;198(1):51–7.
Bellocchia M, Masoero M, Ciuffreda A, Croce S, Vaudano A, Torchio R, et al. Predictors of cardiovascular disease in asthma and chronic obstructive pulmonary disease. Multidiscip Respir Med. 2013;8(1):58.
Crisan L, Wong N, Sin DD, Lee HM. Karma of cardiovascular disease risk factors for prevention and management of major cardiovascular events in the context of acute exacerbations of chronic obstructive pulmonary disease. Front Cardiovasc Med. 2019;6:79.
Vestbo J, Anderson JA, Brook RD, Calverley PM, Celli BR, Crim C, et al. Fluticasone furoate and vilanterol and survival in chronic obstructive pulmonary disease with heightened cardiovascular risk (SUMMIT): a double-blind randomised controlled trial. Lancet. 2016;387(10030):1817–26.
Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Cardiovascular events in patients with COPD: TORCH study results. Thorax. 2010;65(8):719–25.
Santus P, Radovanovic D, Di Marco S, Valenti V, Raccanelli R, Blasi F, et al. Effect of indacaterol on lung deflation improves cardiac performance in hyperinflated COPD patients: an interventional, randomized, double-blind clinical trial. Int J Chron Obstruct Pulmon Dis. 2015;10:1917–23.
Cazzola M, Mantero A, Santus P, Carlucci P, Mondoni M, Bosotti L, et al. Doppler echocardiographic assessment of the effects of inhaled long-acting beta2-agonists on pulmonary artery pressure in COPD patients. Pulm Pharmacol Ther. 2007;20(3):258–64.
Geake JB, Dabscheck EJ, Wood-Baker R, Cates CJ. Indacaterol, a once-daily beta2-agonist, versus twice-daily beta2-agonists or placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;1(1):Cd010139.
Kheir F, Salerno DA. Brain natriuretic peptide measurement in patients with COPD and cardiovascular disease. Chest. 2013;144(3):1081.
Jafar Z, Valero-Elizondo J, Saeed GJ, Acquah I, Yahya T, Mahajan S, et al. Association of cardiovascular risk profile with healthcare expenditure and resource utilization in chronic obstructive pulmonary disease, with and without atherosclerotic cardiovascular disease. Am J Prev Cardiol. 2020;3:100084.
Gershon AS, Mecredy GC, Guan J, Victor JC, Goldstein R, To T. Quantifying comorbidity in individuals with COPD: a population study. Eur Respir J. 2015;45(1):51–9.
Jones PW, Mullerova H, Agusti A, Decramer M, Adamek L, Raillard A, et al. Cardiovascular disease does not predict exacerbation rate or mortality in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197(3):400–3.
Mannino DM, Thorn D, Swensen A, Holguin F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J. 2008;32(4):962–9.
Martinez FJ, Curtis JL, Sciurba F, Mumford J, Giardino ND, Weinmann G, et al. Sex differences in severe pulmonary emphysema. Am J Respir Crit Care Med. 2007;176(3):243–52.
Matera MG, Ora J, Calzetta L, Rogliani P, Cazzola M. Sex differences in COPD management. Expert Rev Clin Pharmacol. 2021;14(3):323–32.
Bhallamudi S, Connell J, Pabelick CM, Prakash YS, Sathish V. Estrogen receptors differentially regulate intracellular calcium handling in human nonasthmatic and asthmatic airway smooth muscle cells. Am J Physiol Lung Cell Mol Physiol. 2020;318(1):L112–24.
Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol Sex Differ. 2017;8(1):33.
Acknowledgements
We would like to thank all participants in ACURE study for collecting the data of this clinical study.
Funding
This work was supported by the Major Program of National Natural Science Foundation of China (82090010, 82090011), National Key R&D Program of China (2018YFC1315100), CAMS Innovation Fund for Medical Sciences (2020-I2M-2-008), Respiratory Disease Clinical Research Public Welfare Program of China Song Qingling Foundation (2018MZFC-032), and the Fundamental Research Funds for the Central Universities of Central South University (No. 2021zzts0389).
Author information
Authors and Affiliations
Contributions
Concept and design of the study by YCu, YCh, TY, CL, KH, and CW. Data collection and management by YCu, ZZh, YM, CL, XM, KH, YZ, XR, JL, TY, YCh, and CW. Statistical analysis by YCu, ZZh, CL, XM, and YZ. Drafting of the manuscript by YCu. Review and final approval of the manuscript by all the authors. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of China-Japan Friendship Hospital (No. 2015-88) and informed consent was obtained from all involved participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Baseline characteristics of the patients with or without follow-up data. Table S2. Univariate and multivariate Cox regression analyses of factors associated with AECOPD readmission within 30 days.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cui, Y., Zhan, Z., Ma, Y. et al. Clinical and economic burden of comorbid coronary artery disease in patients with acute exacerbation of chronic obstructive pulmonary disease: sex differences in a nationwide cohort study. Respir Res 23, 28 (2022). https://doi.org/10.1186/s12931-022-01945-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-022-01945-7