Abstract
Background
Which patients should receive dual therapy as initial treatment for chronic obstructive pulmonary disease (COPD) is only loosely defined. We evaluated if a lower forced expiratory volume in 1 s (FEV1) identifies a population more likely to benefit from dual therapy than monotherapy among group B COPD patients in whom Global initiative for Chronic Obstructive Pulmonary Disease (GOLD) recommends monotherapy as initial treatment.
Methods
This was a patient-level pooled analysis of phase-3 randomized controlled trials involving dual bronchodilators. Study patients were classified into two groups based on the FEV1 of 50% of the predicted value (GOLD I/II versus GOLD III/IV). We evaluated the efficacy of dual versus monotherapy (long-acting beta-2 agonist [LABA] or long-acting muscarinic antagonist [LAMA]) between these two groups in the following outcomes: changes in trough FEV1, the St. George’s Respiratory Questionnaire (SGRQ) score, the proportion of SGRQ responders, time to first exacerbation, and risk of adverse events.
Results
A total of 14,449 group B patients from 12 studies were divided into GOLD III/IV (n = 8043) or GOLD I/II group (n = 6406). In the GOLD III/IV group, dual therapy was significantly more effective in improving FEV1, reducing SGRQ scores, and achieving a higher proportion of SGRQ responders compared with either LABA or LAMA. Dual therapy also showed a significantly longer time to first exacerbation compared with LABA in the GOLD III/IV group. In contrast, in the GOLD I/II group, the benefits of dual therapy over monotherapy were less consistent. Although dual therapy resulted in significantly higher FEV1 than either LABA or LAMA, it did not show significant differences in the SGRQ score and proportion of SGRQ responders as compared with LABA. The time to first exacerbation was also not significantly different between dual therapy and either LABA or LAMA in the GOLD I/II group.
Conclusions
Dual therapy demonstrated benefits over monotherapy more consistently in patients with lower FEV1 than those with higher FEV1.
Similar content being viewed by others
Background
Chronic obstructive pulmonary disease (COPD) is one of the major causes of chronic morbidity and mortality worldwide [1,2,3]. It is characterized by irreversible airflow limitation and respiratory symptoms such as cough, sputum, and dyspnea [4]. The severity of airflow limitation is represented by forced expiratory volume at 1 s (FEV1). Although the importance of FEV1 is acknowledged, it does not determine treatment according to the Global initiative for Chronic Obstructive Lung Disease (GOLD) document [4]. GOLD classifies COPD patients and guides initial treatments based on symptom severity and exacerbation frequency [5, 6].
GOLD group B represents symptomatic patients with a low risk of exacerbation. According to the GOLD recommendations, the initial treatment choice is a long-acting bronchodilator, either a long-acting beta-2 agonist (LABA) or long-acting muscarinic antagonist (LAMA), with no preference between the two [6]. Dual therapy with LABA/LAMA is recommended as a step-up option [6]. Given that LABA and LAMA have different mechanisms of action [7, 8], dual therapy may provide greater benefits in terms of lung function improvement and symptom relief [9,10,11]. However, GOLD recommends dual therapy as an initial treatment only in patients with severe symptoms [6].
Considering that GOLD group B includes heterogeneous patients with a wide range of FEV1, some patients may not have a sufficient treatment response from LABA or LAMA alone. In particular, patients with a higher degree of airflow limitation at baseline may benefit from treatment more intensive than monotherapy. However, there has been no evaluation of whether the magnitude of treatment difference between dual and monotherapy varies according to the baseline FEV1 in group B patients. This study compared the effects of dual therapy and monotherapy in group B COPD patients according to FEV1 level (50% of the predicted value [%pred.]) to test the hypothesis that the population with a lower FEV1 level (GOLD grades III/IV) is more likely to benefit from dual therapy.
Methods
Data sources
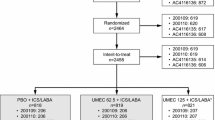
This study was a patient-level pooled analysis of phase-3 randomized controlled trials that evaluated the efficacy of a dual bronchodilator (LABA/LAMA) compared with either LABA or LAMA monotherapy. We obtained individual patient-level data from available trials provided by the sponsor companies. The dual bronchodilators of interest included glycopyrronium/indacaterol (Ultibro Breezehaler®, Novartis), umeclidinium/vilanterol (Anoro Ellipta®, GSK), and tiotropium/olodaterol (Spiolto Respimat®, Boehringer-Ingelheim). The study protocol was approved by the Institutional Review Board of Asan Medical Center (IRB No.: 2018-0298). The requirement for informed consent was waived due to the retrospective nature of the study.
Individual patient-level clinical trial data are available to outside researchers through ClinicalStudyDataRequest.com (CSDR). CSDR is a consortium of global pharmaceutical companies including, GlaxoSmithKline, Astellas Pharma, Bayer, Novartis, Roche, and Boehringer-Ingelheim, as well as academic research funders, including the Bill & Melinda Gates Foundation, the UK Medical Research Council, and The Wellcome Trust [12]. It was launched in 2013 to facilitate data sharing among independent investigators [12] by providing deidentified raw global clinical trial data from multiple sponsors [13]. Our study proposal was submitted via a web-based portal to the CSDR’s Independent Review Panel for a review of scientific importance and qualification of the research team. Data was analyzed in a closed system provided by CSDR with in-built statistical software. Data outside of CSDR could not be merged with data provided by CSDR.
Eligibility criteria
We requested data from phase-3 randomized controlled trials that evaluated the efficacy of a dual bronchodilator (glycopyrronium/indacaterol, umeclidinium/vilanterol, or tiotropium/olodaterol) in COPD patients. The research had to meet the following criteria: (1) compare dual and single bronchodilators with/without a placebo arm, (2) a parallel design, (3) duration of longer than eight weeks, and (4) outcomes include changes in trough FEV1, St. George's Respiratory Questionnaire (SGRQ) total score, risk of acute exacerbation, or adverse events. Studies were excluded if: (1) the comparator was not relevant to the study purpose (e.g., comparison between dual and inhaled corticosteroid (ICS)/LABA; (2) the dual bronchodilator was not given as a fixed-dose combination; (3) it was performed on patients who were not responsive to monotherapy; and (4) information regarding baseline symptom levels (modified Medical Research Council [mMRC] grade, COPD assessment test [CAT] or SGRQ score) and previous exacerbation were not adequately addressed. We submitted the study proposal to CSDR on March 15, 2018, and gained access to the requested data on January 2, 2019.
A total of 12 studies were included in this study (Additional file 1: Figure S1). The list of included studies and the types of study endpoints are described in Additional file 1: Table S1. Briefly, all studies measured trough FEV1 and the development of adverse events. Total scores of SGRQ and acute exacerbation were evaluated in 8 and 10 studies, respectively.
Study patients
All of the studies shared common inclusion criteria. Patients were diagnosed with COPD by spirometry (post-bronchodilator FEV1/forced vital capacity < 0.7), aged 40 years or older, and had a smoking history of more than 10 pack-years [7, 10, 11, 14,15,16,17,18]. The baseline characteristics of each treatment arm (excluding the placebo arm) in the 12 studies are shown in Additional file 1: Table S2.
This study included patients who belonged to group B according to the 2017 GOLD classification criteria. To classify patients into one of the four groups (A, B, C, and D), we determined symptom severity at the time of inclusion and the number of exacerbations in the previous year. If the baseline CAT score or mMRC grade was not provided, a baseline SGRQ score of 25 was used as a cutoff value as suggested by GOLD [5]. Additional file 1: Table S3 shows which criteria (CAT score, mMRC grade, and SGRQ score) were used in each study. Exacerbation was defined as an acute worsening of the patient’s respiratory symptoms beyond normal day-to-day variations requiring a change in medication. According to the 2017 GOLD classification criteria, patients who experienced none or one exacerbation not requiring hospitalization during the previous year were included in the study.
Study outcomes
We divided study patients into GOLD I/II group (FEV1 ≥ 50%pred.) and GOLD III/IV group (FEV1 < 50%pred.) based on their baseline FEV1 level. We evaluated whether the efficacy of dual versus monotherapy differs between these two groups on the following outcomes: change in the trough FEV1, change in the SGRQ total score, the proportion of SGRQ responders, time to first exacerbation, and the risk of adverse events. A change in the trough FEV1 was the difference between pre-dose FEV1 values at baseline and at the end of each study as shown in Additional file 1: Table S4. An SGRQ responder was defined as a patient who achieved a minimum clinically important difference (MCID) threshold of 4 points.
Statistical analysis
A professional statistician (JB Lee) performed all statistical analyses. A generalized linear mixed model using stratified study-effects or random study-effects was used to sum up individual patient-level data. For continuous variables, such as a change in trough FEV1 and SGRQ score from baseline, a linear mixed model with random effects was applied with an adjusted multiple treatment comparison. The least-squares mean change from baseline values for each treatment group were reported with their associated standard errors and a 95% confidence interval (CI). For binary data, we used a generalized linear mixed model with Penalized Quasi-likelihood estimation. The odds ratio and 95% CI were estimated for the binary data. Cox’s proportional hazard model with random effects was used to summarize time to the first exacerbation. The hazard ratio (HR) and the corresponding 95% CI were then estimated. All p-values were two-tailed, and p-values < 0.05 were considered statistically significant. All analyses were performed using the Statistical Analysis System (SAS) statistical software package, version 9.4. SAS Institute Inc., Cary, NC, USA.
Results
Baseline characteristics of the study patients
We identified 20204 patients who received either dual or monotherapy of a long-acting bronchodilator from 12 studies. Among them, 14449 patients were classified as group B based on the 2017 GOLD classification criteria. Table 1 describes the baseline clinical characteristics of all group B patients and according to the baseline FEV1 level. The GOLD III/IV group accounted for 55.7% (n = 8043) of all study patients. Their mean age was 64.7 years and the mean FEV1 value was 35.1%pred. In the GOLD I/II group, the mean age and mean FEV1 values were 64.6 years and 54.6%pred., respectively. Among the patients who received dual therapy, the number of patients treated with tiotropium/olodaterol was the highest, followed by umeclidinium/vilanterol in both groups. Tiotropium was the most frequently administered bronchodilator monotherapy in both groups.
Trough FEV 1
In both the GOLD I/II and GOLD III/IV groups, dual therapy resulted in mean FEV1 improvement greater than MCID of 100 mL, whereas monotherapy did not (Table 2). The difference in the treatment effect between dual and monotherapy was statistically significant in both the GOLD I/II and GOLD III/IV groups, as shown in Fig. 1. Dual therapy provided a significantly greater FEV1 improvement than monotherapy, regardless of the comparator, LABA or LAMA (all p-values < 0.001).
SGRQ total score
Table 3 shows the changes in the SGRQ total score following dual or monotherapy. Although dual therapy resulted in a greater reduction in the SGRQ score than monotherapy did, the difference between the two treatments had a different pattern in the GOLD I/II and GOLD III/IV groups. In the GOLD III/IV group, dual therapy reduced the SGRQ score by 7.63 points and was consistently, significantly greater than LABA (treatment difference, 2.12; p = 0.001) and LAMA monotherapy (treatment difference, 1.79; p < 0.001) as shown in Fig. 2. In the GOLD I/II group, however, dual therapy was significantly better than LAMA (treatment difference, 1.12; p = 0.048), but not LABA (treatment difference, 0.33; p = 0.868).
Difference between dual therapy vs. monotherapy in change from baseline in SGRQ score. CI confidence interval, GOLD Global initiative for Chronic Obstructive Lung Disease, LABA long-acting beta-2 agonist, LAMA long-acting muscarinic antagonist, LSM least squares mean, SGRQ St. George’s Respiratory Questionnaire
SGRQ responders
Figure 3 shows the proportion of SGRQ responders in the GOLD I/II and GOLD III/IV groups. Similar to the changes in the SGRQ score, there was a different benefit pattern of dual therapy versus monotherapy, depending on the baseline FEV1 level. In the GOLD III/IV group, dual therapy resulted in a significantly higher proportion of SGRQ responders than both LABA and LAMA monotherapy. The treatment difference between dual vs. LABA and LAMA were 9.86% (95% CI 5.62–14.10; p < 0.001) and 8.21% (95% CI 4.81–11.62; p < 0.001), respectively. In the GOLD I/II group, dual therapy was significantly better than LAMA (treatment difference, 5.93%; 95% CI 2.44–9.41; p = 0.001), but not LABA monotherapy (treatment difference 0.52%, 95% CI − 3.96 to 4.99; p = 0.821).
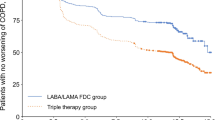
Time to first exacerbation
The mean exacerbation rates per 6 months are shown in Additional file 1: Table S5. Briefly, the exacerbation rates were 0.212, 0.188, 0.176 per 6 months in the LABA, LAMA, and dual therapy arm, respectively, in the GOLD III/IV group. In the GOLD I/II group, the rates were 0.139, 0.122, 0.108, in patients treated with LABA, LAMA, and dual therapy, respectively.
Figure 4 shows the time to first exacerbation in patients who received dual therapy and those who received LABA or LAMA monotherapy. A different pattern was observed in the GOLD I/II and GOLD III/IV groups. In the GOLD III/IV group, dual therapy showed a significantly longer time to first exacerbation compared with LABA (HR, 1.311; 95% CI 1.113–1.544; p = 0.001), although there was no significant difference as compared with LAMA monotherapy. In the GOLD I/II group, dual therapy did not show any significant difference compared to both LABA and LAMA monotherapy.
Adverse events
There was no significant difference in the risk of any adverse events between dual and monotherapy in both the GOLD I/II and GOLD III/IV groups (Fig. 5).
Discussion
This study compared the effects of dual therapy and monotherapy according to the baseline FEV1 level in GOLD group B patients using patient-level data from phase-3 randomized controlled trials. We found that the benefit of dual therapy over monotherapy was more prominent in the GOLD III/IV group. In the GOLD III/IV group, dual therapy was consistently more effective than LABA or LAMA in improving FEV1, reducing the SGRQ score, and achieving a higher proportion of SGRQ responders, and also resulted in a longer time to exacerbation compared with LABA. In contrast, in the GOLD I/II group, the benefit of dual therapy was less consistently shown in the study outcomes.
The purpose of COPD treatment is to reduce respiratory symptoms and prevent exacerbations [6]. Optimal treatment should be provided in order to achieve this goal. It remains undetermined if LABA or LAMA monotherapy is sufficient enough for group B COPD patients. In a previous study, the level of symptom burden was investigated in patients who were on maintenance treatment with LABA or LAMA alone [19]. Several domains of a respiratory questionnaire revealed greater impairment, including more dyspnea, in patients with FEV1 < 50%pred. than in those with ≥ 50%pred. Hence, there is a need to determine if patients with more severe airflow limitations require more intensive treatment than is currently recommended. In another study, patients who initiated maintenance therapy with a single bronchodilator showed a significantly shorter time to escalation to triple therapy (ICS/LABA/LAMA) than those who started treatment with a dual bronchodilator [20]. This may indirectly indicate a higher risk of additional treatment requirement in patients receiving monotherapy.
Given that the magnitude of FEV1 improvement was similar in the GOLD I/II and GOLD III/IV groups, it is interesting that the benefit of dual therapy over monotherapy regarding health-related quality of life appeared differently in the groups. An increase in FEV1 does not always indicate better results in patient-reported outcomes. For example, a previous study found that the proportion of SGRQ responders was not very different between indacaterol/glycopyrronium (63.7%) and indacaterol (63.0%), although indacaterol/glycopyrronium showed a significantly greater increase in trough FEV1 than indacaterol (1.45 L vs. 1.38 L; p < 0.001) [9]. One explanation for the difference shown in our study could be that patients who have less severe airflow limitations may not perceive the benefit of greater bronchodilation provided by dual therapy. Instead, in the GOLD I/II group, non-bronchodilator effects, such as enhanced mucociliary clearance, may have an important role in reducing SGRQ scores and preventing exacerbation [21]. As these effects are delivered by both dual therapy and monotherapy, the benefits of dual therapy over monotherapy might have appeared smaller in this group.
One may argue that the treatment difference in the SGRQ total score between dual therapy and monotherapy might not be large enough to be translated into a significant clinical benefit. However, the proportion of SGRQ responder was approximately 10% greater with dual therapy than either monotherapy in the GOLD III/IV patients. In the GOLD I/II group, dual therapy was significantly associated with a greater proportion of SGRQ responders than LAMA but the difference was smaller than that shown in the GOLD III/IV patients. These results indicate that patients with lower FEV1 are more likely to benefit from dual therapy than monotherapy in terms of health-related quality of life. Given that there was no significant difference in adverse events and dual therapy was associated with greater FEV1 improvement, the advantage of dual therapy in GOLD III/IV needs to be highlighted.
The time to first exacerbation appeared to be significantly longer with dual therapy than with LABA monotherapy in the GOLD III/IV group, although no difference was found when compared to LAMA monotherapy. In the GOLD I/II group, there was no significant difference in dual therapy vs. LABA or LAMA. Noninferiority of LAMA as compared with dual therapy in terms of exacerbation is consistent with the GOLD document, which recommends LAMA as an initial treatment for patients who frequently develop exacerbation [12, 18, 22]. However, for those who are symptomatic but have a low risk of exacerbation, the desired treatment goals may be an improved health-related quality of life and reduced symptoms rather than a reduced exacerbation. Therefore, the importance of dual therapy should not be underestimated in symptomatic patients. In line with this, dual therapy is indicated in patients with more impaired lung function (FEV1 less than 50%) according to the expert recommendation in the recently published Czech guidelines [23].
The population more likely to benefit from starting treatment with a dual bronchodilator has only been loosely defined [24]. In a previous study, Martinez et al. showed that patients with a higher symptom burden, represented as CAT score ≥ 20, are more likely to benefit from dual bronchodilator treatment than monotherapy. The treatment difference between dual and monotherapy in the SGRQ score changes and the use of rescue medication was greatest in those with a CAT score ≥ 20 [24]. Accordingly, GOLD reserves dual bronchodilator treatment for highly symptomatic patients [5]. However, it should be noted that patients with lower lung function may underestimate their symptom burden due to unconsciously restricted physical activity [25, 26]. This will potentially lead to undertreatment in patients with a high degree of airflow limitation. In contrast, FEV1 is an objective parameter that can be used simply in treatment decisions.
The proportion of patients with FEV1 < 50%pred. in group B is not negligible. There were 8043 patients with an FEV1 less than 50%pred., accounting for 55.7% of our study subjects. These patients would have been classified as group D if the 2011 GOLD classification criteria were applied. Since FEV1 is no longer considered in patient classification, a substantial proportion of patients have shifted from high-risk to low-risk groups [27,28,29,30,31,32]. Previously, Tudoric et al. analyzed data from a study of 3361 COPD patients in central and eastern Europe [27]. They reported that 20.4% of the entire cohort moved from group D to group B according to the revised classification system. In another study that retrospectively analyzed 1053 COPD patients, the proportion of group D decreased by more than half (from 34.2 to 11.6%), whereas group B increased from 40.6 to 63.2% [29]. In large COPD cohorts such as ECLIPSE, Copenhagen, and the COPD gene cohort, the proportion of patients classified as group D by FEV1 alone was higher than those classified by frequent exacerbation history [33, 34]. Given these findings, there may be a considerable number of patients in GOLD group B who can benefit from early dual therapy.
We should address the limitations of our study to better understand the results. First, we did not include studies that evaluated the efficacy of aclidinium/formoterol (Duaklir Genuair®, AstraZeneca), glycopyrronium/formoterol (Bevespi Aerosphere®, AstraZeneca), and other clinically available dual bronchodilators. The corresponding pharmaceutical company (AstraZeneca) was not part of CSDR, and their data were not available. Further, there is a concern that twice- and once-daily medications differ in efficacy [35]. In fact, a previous meta-analysis found less FEV1 improvement with aclidinium/formoterol than with glycopyrronium/indacaterol or umeclidinium/vilanterol [36]. Second, the study patients included those who received ICS. The study outcomes might have been affected by not only the bronchodilator treatment but also ICS. However, in a recent study performed in non-ICS users, dual therapy resulted in greater lung function improvement and a significant reduction in clinically important deterioration than monotherapy [37]. Third, only one study (DYNAGITO) evaluated the acute exacerbation risk as a primary outcome. Although 9 of the 12 studies provided data on the development of acute exacerbation, except for DYNAGITO, they were not powered for this outcome. Of note, DYNAGITO included the greatest number of patients, and the acute exacerbation results might have been derived largely from DYNAGITO. Fourth, several outcomes were assessed in this study, but the problem of multiplicity was not considered. Although there is relatively less need to adjust for multiplicity in post-hoc studies, the results should be interpreted with caution. Lastly, we did not assess the cost-effectiveness of dual therapy. However, several previous studies have found that dual bronchodilators are cost-effective in COPD patients [38,39,40]. Particularly in South Korea, the costs are almost similar between dual and single bronchodilators.
In conclusion, dual therapy showed more consistent benefits over monotherapy in the GOLD III/IV group than in the GOLD I/II group. Among group B COPD patients, those with lower FEV1 may benefit from more intensive treatment.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CAT:
-
COPD assessment test
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CSDR:
-
Clinical Study Data Request
- FEV1 :
-
Forced expiratory volume in 1 s
- GOLD:
-
Global initiative for Chronic Obstructive Lung Disease
- HR:
-
Hazard ratio
- ICS:
-
Inhaled corticosteroid
- LABA:
-
Long-acting beta-2 agonist
- LAMA:
-
Long-acting muscarinic antagonist
- MCID:
-
Minimum clinically important difference
- mMRC:
-
Modified Medical Research Council
- SGRQ:
-
St. George’s Respiratory Questionnaire
References
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128.
Lopez-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology. 2016;21:14–23.
Svedsater H, Roberts J, Patel C, Macey J, Hilton E, Bradshaw L. Life impact and treatment preferences of individuals with asthma and chronic obstructive pulmonary disease: results from qualitative interviews and focus groups. Adv Ther. 2017;34:1466–81.
Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Chen R, Decramer M, Fabbri LM, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Eur Respir J. 2017;195:557–82.
Global Strategy for Diagnosis, Management, and Prevention of COPD. https://goldcopd.org/wp-content/uploads/2017/02/wms-GOLD-2017-FINAL.pdf. Accessed 1 Jan 2021.
Global Strategy for Prevention, Diagnosis and Management of COPD. https://goldcopd.org/gold-reports/. Accessed 1 Jan 2021.
Buhl R, Maltais F, Abrahams R, Bjermer L, Derom E, Ferguson G, Fležar M, Hébert J, McGarvey L, Pizzichini E, et al. Tiotropium and olodaterol fixed-dose combination versus mono-components in COPD (GOLD 2–4). Eur Respir J. 2015;45:969–79.
Tashkin DP, Ferguson GT. Combination bronchodilator therapy in the management of chronic obstructive pulmonary disease. Respir Res. 2013;14:49.
Bateman ED, Ferguson GT, Barnes N, Gallagher N, Green Y, Henley M, Banerji D. Dual bronchodilation with QVA149 versus single bronchodilator therapy: the SHINE study. Eur Respir J. 2013;42:1484–94.
Donohue JF, Maleki-Yazdi MR, Kilbride S, Mehta R, Kalberg C, Church A. Efficacy and safety of once-daily umeclidinium/vilanterol 62.5/25 mcg in COPD. Respir Med. 2013;107:1538–46.
Singh D, Ferguson GT, Bolitschek J, Grönke L, Hallmann C, Bennett N, Abrahams R, Schmidt O, Bjermer L. Tiotropium + olodaterol shows clinically meaningful improvements in quality of life. Respir Med. 2015;109:1312–9.
www.clinicalstudydatarequest.com. Accessed 1 Jan 2021.
Nisen P, Rockhold F. Access to patient-level data from GlaxoSmithKline clinical trials. N Engl J Med. 2013;369:475–8.
Ferguson GT, Taylor AF, Thach C, Wang Q, Schubert-Tennigkeit AA, Patalano F, Banerji D. Long-term maintenance bronchodilation with indacaterol/glycopyrrolate versus indacaterol in moderate-to-severe COPD patients: the FLIGHT 3 study. Chronic Obstr Pulm Dis. 2016;3:716–28.
Mahler DA, Kerwin E, Ayers T, FowlerTaylor A, Maitra S, Thach C, Lloyd M, Patalano F, Banerji D. FLIGHT1 and FLIGHT2: efficacy and safety of QVA149 (indacaterol/glycopyrrolate) versus its monocomponents and placebo in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015;192:1068–79.
Maleki-Yazdi MR, Kaelin T, Richard N, Zvarich M, Church A. Efficacy and safety of umeclidinium/vilanterol 62.5/25 mcg and tiotropium 18 mcg in chronic obstructive pulmonary disease: results of a 24-week, randomized, controlled trial. Respir Med. 2014;108:1752–60.
Decramer M, Anzueto A, Kerwin E, Kaelin T, Richard N, Crater G, Tabberer M, Harris S, Church A. Efficacy and safety of umeclidinium plus vilanterol versus tiotropium, vilanterol, or umeclidinium monotherapies over 24 weeks in patients with chronic obstructive pulmonary disease: results from two multicentre, blinded, randomised controlled trials. Lancet Respir Med. 2014;2:472–86.
Calverley PMA, Anzueto AR, Carter K, Grönke L, Hallmann C, Jenkins C, Wedzicha J, Rabe KF. Tiotropium and olodaterol in the prevention of chronic obstructive pulmonary disease exacerbations (DYNAGITO): a double-blind, randomised, parallel-group, active-controlled trial. Lancet Respir Med. 2018;6:337–44.
Dransfield MT, Bailey W, Crater G, Emmett A, O’Dell DM, Yawn B. Disease severity and symptoms among patients receiving monotherapy for COPD. Prim Care Respir J. 2011;20:46–53.
Hahn B, Hull M, Blauer-Peterson C, Buikema AR, Ray R, Stanford RH. Rates of escalation to triple COPD therapy among incident users of LAMA and LAMA/LABA. Respir Med. 2018;139:65–71.
Beeh KM, Burgel PR, Franssen FME, Lopez-Campos JL, Loukides S, Hurst JR, Fležar M, Ulrik CS, Di Marco F, Stolz D, et al. How do dual long-acting bronchodilators prevent exacerbations of chronic obstructive pulmonary disease? Am J Respir Crit Care Med. 2017;196:139–49.
Wedzicha JA, Decramer M, Ficker JH, Niewoehner DE, Sandstrom T, Taylor AF, D’Andrea P, Arrasate C, Chen H, Banerji D. Analysis of chronic obstructive pulmonary disease exacerbations with the dual bronchodilator QVA149 compared with glycopyrronium and tiotropium (SPARK): a randomised, double-blind, parallel-group study. Lancet Respir Med. 2013;1:199–209.
Zatloukal J, Brat K, Neumannova K, Volakova E, Hejduk K, Kocova E, Kudela O, Kopecky M, Plutinsky M, Koblizek V. Chronic obstructive pulmonary disease—diagnosis and management of stable disease; a personalized approach to care, using the treatable traits concept based on clinical phenotypes. Position paper of the Czech Pneumological and Phthisiological Society. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2020;164:325–56.
Martinez FJ, Fabbri LM, Ferguson GT, Orevillo C, Darken P, Martin UJ, Reisner C. Baseline symptom score impact on benefits of glycopyrrolate/formoterol metered dose inhaler in COPD. Chest. 2017;152:1169–78.
Mathioudakis AG, Chatzimavridou-Grigoriadou V, Evangelopoulou E, Mathioudakis GA. Chronic bronchitis: an objective diagnosis of exclusion. Eur Respir J. 2012;40:1305 (author reply 1305-1306).
Haroon S, Adab P, Riley RD, Fitzmaurice D, Jordan RE. Predicting risk of undiagnosed COPD: development and validation of the TargetCOPD score. Eur Respir J. 2017;49:1602191.
Tudoric N, Koblizek V, Miravitlles M, Valipour A, Milenkovic B, Barczyk A, Somfay A, Zykov K, Kostov K, Zbozinkova Z, et al. GOLD 2017 on the way to a phenotypic approach? Analysis from the Phenotypes of COPD in Central and Eastern Europe (POPE) Cohort. Eur Respir J. 2017;49:1602518.
Le LAK, Johannessen A, Hardie JA, Johansen OE, Gulsvik A, Vikse BE, Bakke P. Prevalence and prognostic ability of the GOLD 2017 classification compared to the GOLD 2011 classification in a Norwegian COPD cohort. Int J Chron Obstruct Pulmon Dis. 2019;14:1639–55.
Hsieh MJ, Huang SY, Yang TM, Tao CW, Cheng SL, Lee CH, Kuo PH, Wu YK, Chen NH, Hsu WH, et al. The impact of 2011 and 2017 Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD) guidelines on allocation and pharmacological management of patients with COPD in Taiwan: Taiwan Obstructive Lung Disease (TOLD) study. Int J Chron Obstruct Pulmon Dis. 2018;13:2949–59.
Kobayashi S, Hanagama M, Ishida M, Sato H, Ono M, Yamanda S, Yamada M, Aizawa H, Yanai M. Clinical characteristics and outcomes in Japanese patients with COPD according to the 2017 GOLD classification: the Ishinomaki COPD Network Registry. Int J Chron Obstruct Pulmon Dis. 2018;13:3947–55.
Sun L, Chen Y, Wu R, Lu M, Yao W. Changes in definition lead to changes in the clinical characteristics across COPD categories according to GOLD 2017: a national cross-sectional survey in China. Int J Chron Obstruct Pulmon Dis. 2017;12:3095–102.
Cabrera López C, Casanova Macario C, Marín Trigo JM, Torres JP, Sicilia Torres R, González JM, Polverino F, Divo M, Pinto Plata V, Zulueta JJ, Celli B. Comparison of the 2017 and 2015 Global Initiative for Chronic Obstructive Lung Disease Reports. Impact on grouping and outcomes. Am J Respir Crit Care Med. 2018;197:463–9.
Han MK, Muellerova H, Curran-Everett D, Dransfield MT, Washko GR, Regan EA, Bowler RP, Beaty TH, Hokanson JE, Lynch DA, et al. GOLD 2011 disease severity classification in COPDGene: a prospective cohort study. Lancet Respir Med. 2013;1:43–50.
Agusti A, Hurd S, Jones P, Fabbri LM, Martinez F, Vogelmeier C, Vestbo J, Rodriguez-Roisin R. FAQs about the GOLD 2011 assessment proposal of COPD: a comparative analysis of four different cohorts. Eur Respir J. 2013;42:1391–401.
Kornmann O, Dahl R, Centanni S, Dogra A, Owen R, Lassen C, Kramer B. Once-daily indacaterol versus twice-daily salmeterol for COPD: a placebo-controlled comparison. Eur Respir J. 2011;37:273–9.
Calzetta L, Rogliani P, Matera MG, Cazzola M. A systematic review with meta-analysis of dual bronchodilation with LAMA/LABA for the treatment of stable COPD. Chest. 2016;149:1181–96.
Maltais F, Bjermer L, Kerwin EM, Jones PW, Watkins ML, Tombs L, Naya IP, Boucot IH, Lipson DA, Compton C, et al. Efficacy of umeclidinium/vilanterol versus umeclidinium and salmeterol monotherapies in symptomatic patients with COPD not receiving inhaled corticosteroids: the EMAX randomised trial. Respir Res. 2019;20:238.
van Boven JF, Kocks JW, Postma MJ. Cost-effectiveness and budget impact of the fixed-dose dual bronchodilator combination tiotropium-olodaterol for patients with COPD in the Netherlands. Int J Chron Obstruct Pulmon Dis. 2016;11:2191–201.
Miravitlles M, Galdiz JB, Huerta A, Villacampa A, Carcedo D, Garcia-Rio F. Cost-effectiveness of combination therapy umeclidinium/vilanterol versus tiotropium in symptomatic COPD Spanish patients. Int J Chron Obstruct Pulmon Dis. 2016;11:123–32.
Hoogendoorn M, Corro Ramos I, Baldwin M, Luciani L, Fabron C, Detournay B, Rutten-van Molken M. Long-term cost-effectiveness of the fixed-dose combination of tiotropium plus olodaterol based on the DYNAGITO trial results. Int J Chron Obstruct Pulmon Dis. 2019;14:447–56.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Y-MO was responsible for the conception and design of the study. Y-MO also served as a guarantor and takes full responsibility for the content of this manuscript, including the data and analyses. Y-MO, JBL, and JK made substantial contributions to the concept and design of the study. JBL performed the statistical analyses. JK, JSL, and SWL made substantial contributions to the analysis and interpretation of data. JK wrote the first draft of the manuscript. All authors discussed the results and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the amended Declaration of Helsinki and the protocol was approved by the Institutional Review Board of Asan Medical Center (2018-0298). Informed consent was waived due to the retrospective nature of the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. List of included studies and their endpoints. Table S2. Baseline patient characteristics (excluding placebo arms) included in the 12 studies. Table S3. Criteria used to classify symptom severity in each study. Table S4. Changes in the trough FEV1 (L) according to the treatment arm in each study and treatment difference between dual and monotherapy. Table S5. Rates of acute exacerbation per 6 months in patients treated with dual or monotherapy of LABA and/or LAMA. Figure S1. Study flow diagram.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kang, J., Lee, J.S., Lee, S.W. et al. Dual versus monotherapy with bronchodilators in GOLD group B COPD patients according to baseline FEV1 level: a patient-level pooled analysis of phase-3 randomized clinical trials. Respir Res 22, 55 (2021). https://doi.org/10.1186/s12931-021-01648-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-021-01648-5